Primary Peritonitis Secondary to Streptococcus pyogenes in a Young Female Adult—A Case Report and Literature Review
Abstract
1. Introduction
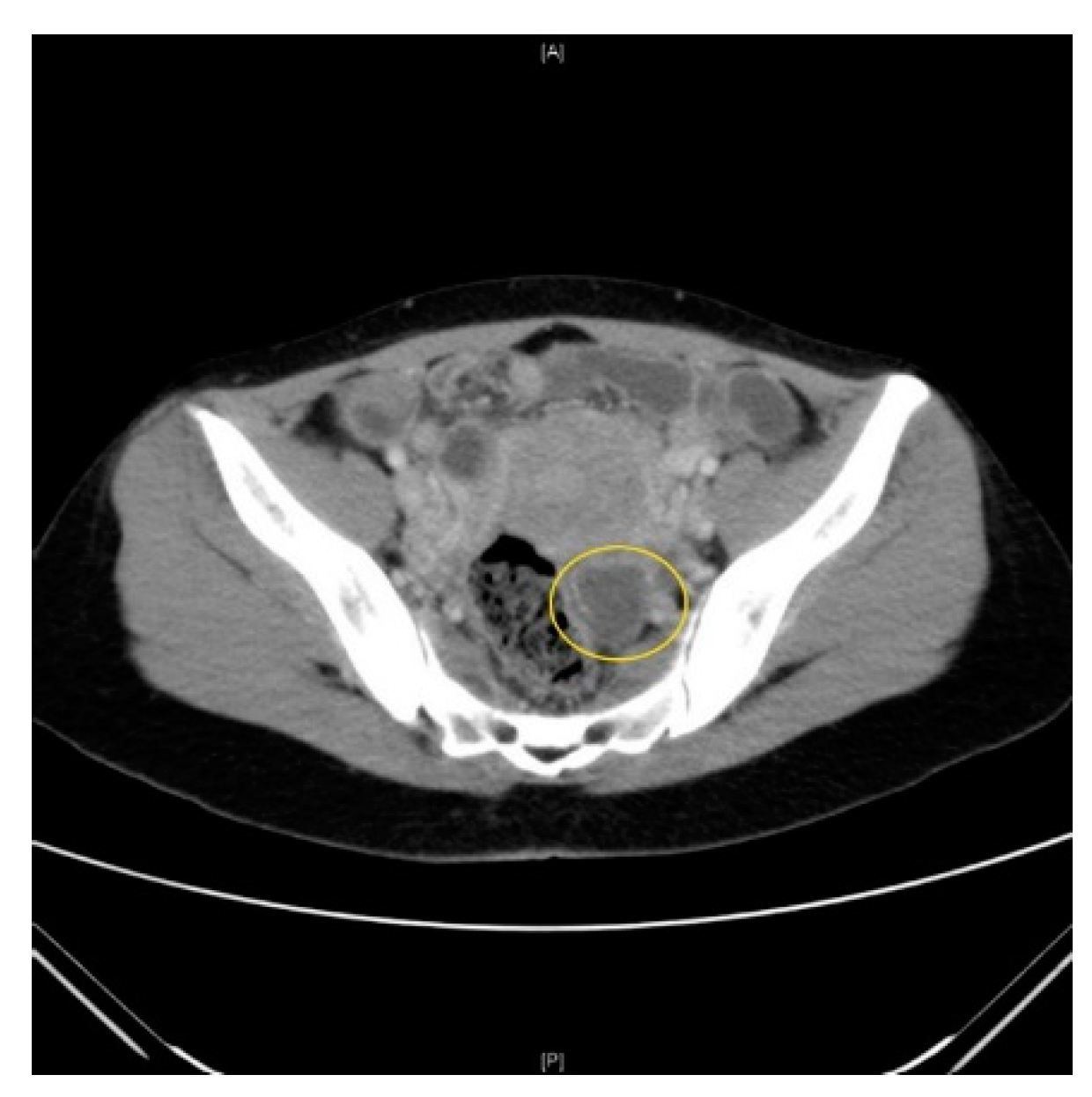
2. Case Presentation
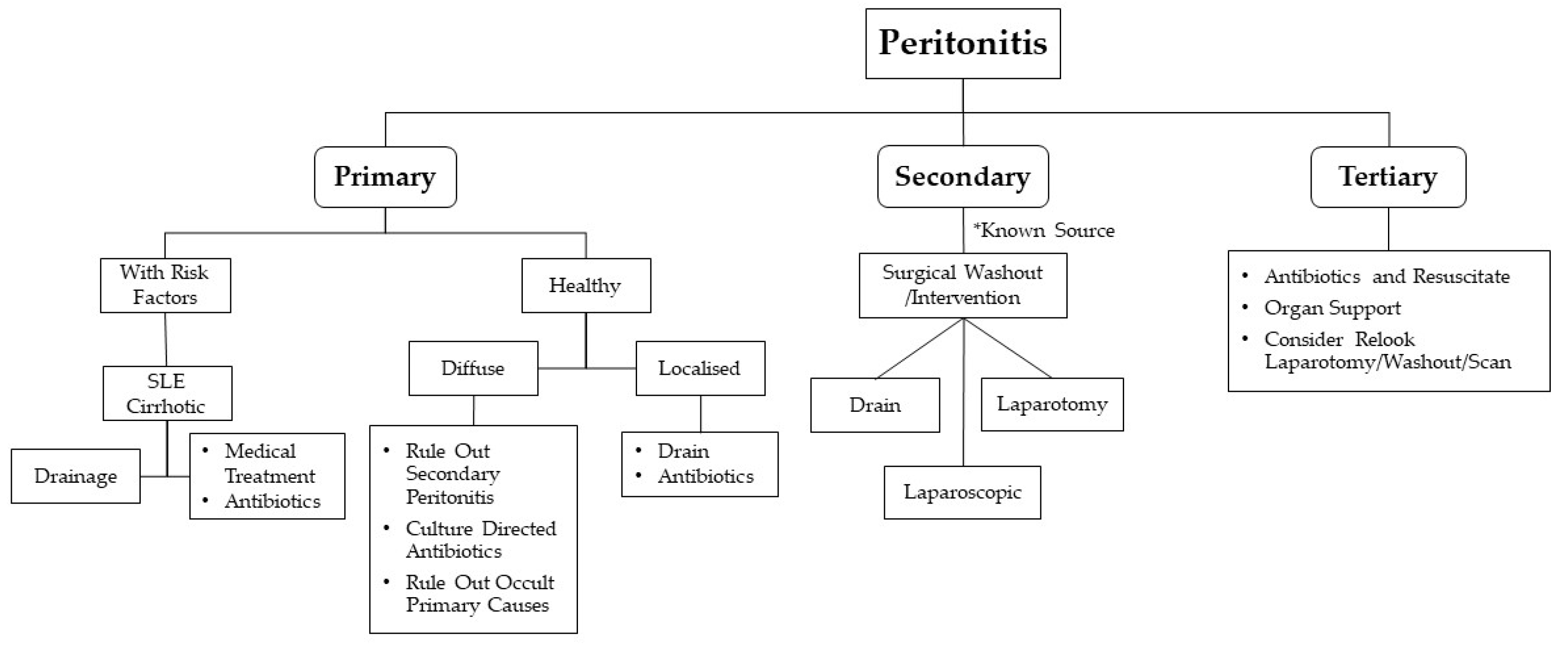
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Khilji, M.F. Primary Peritonitis—A Forgotten Entity. Eur. J. Pediatric Surg. Rep. 2015, 3, 27–29. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ross, A.; Shoff, H.W. Toxic Shock Syndrome. StatPearls. Available online: http://www.ncbi.nlm.nih.gov/books/NBK459345/ (accessed on 22 September 2020).
- Gupta, S.K.; Mishra, S.P.; Tiwary, S.K.; Mishra, M. An introduction of Tertiary Peritonitis. J. Emerg. Trauma Shock. 2014, 7, 121–123. [Google Scholar] [CrossRef] [PubMed]
- Koulaouzidis, A.; Bhat, S.; Karagiannidis, A.; Tan, W.C.; Linaker, B.D. Spontaneous bacterial peritonitis. Postgrad. Med. J. 2007, 83, 379–383. [Google Scholar] [CrossRef] [PubMed]
- Guarner, C.; Soriano, G. Bacterial translocation and its consequences in patients with cirrhosis. Eur. J. Gastroenterol. Hepatol. 2005, 17, 27–31. [Google Scholar] [CrossRef]
- Lipsky, P.E. Spontaneous peritonitis and systemic lupus erythematosus. Importance of accurate diagnosis of gram-positive bacterial infections. JAMA 1975, 232, 929–931. [Google Scholar] [CrossRef]
- Horina, J.H.; Hammer, H.F.; Reisinger, E.C.; Enzinger, G.F.; Holzer, H.; Krejs, G.J. Spontaneous Bacterial Peritonitis in a Hemodialysis Patient with Systemic Lupus erythematosus. Nephron 1993, 65, 633–635. [Google Scholar] [CrossRef]
- Kiziltaş, S.; Imeryüz, N.; Gürcan, T.; Siva, A.; Saip, S.; Dumankar, A.; Kalayci, C.; Ulusoy, N.B. Corticosteroid therapy augments gastroduodenal permeability to sucrose. Am. J. Gastroenterol. 1998, 93, 2420–2425. [Google Scholar] [CrossRef]
- Cereto, F.; Molina, I.; González, A.; Del Valle, O.; Esteban, R.; Guardia, J.; Genescà, J. Role of immunosuppression in the development of quinolone-resistant Escherichia coli spontaneous bacterial peritonitis and in the mortality of E. coli spontaneous bacterial peritonitis. Aliment. Pharmacol. Ther. 2003, 17, 695–701. [Google Scholar] [CrossRef]
- Tan, E.K.; Shelat, V.G.; Tserng, T.L.; Chiu, M.T. Peritoneo-cutaneous fistula secondary to skin excoriation from a large chronic incisional hernia. Ann. Acad. Med. Singap. 2010, 39, 872–873. [Google Scholar]
- Lantsberg, S.; Rachinsky, I.; Boguslavsky, L. Tubo-ovarian Abscess. Clin. Nucl. Med. 1999, 24, 796. [Google Scholar] [CrossRef]
- Barnham, M.; Holm, S.E. Serious Streptococcus pyogenes disease. Clin. Microbiol. Infect. 1997, 3, 250–260. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Micha, J.; Goldstein, B.; Rettenmaier, M.; Brown, J.; Bock, B. Spontaneous bacterial peritonitis following treatment for cervical carcinoma. Int. J. Gynecol. Cancer 2006, 16, 908–911. [Google Scholar] [CrossRef] [PubMed]
- Malota, M.; Felbinger, T.W.; Ruppert, R.; Nüssler, N.C. Group A Streptococci: A rare and often misdiagnosed cause of spontaneous bacterial peritonitis in adults. Int. J. Surg. Case Rep. 2015, 6, 251–255. [Google Scholar] [CrossRef]
- Litaka, D.; Ochi, F.; Nakashima, S.; Fujiyama, J.; Masuyama, M. Treatment with antibodies against primary group A streptococcal peritonitis: A case report and a review of the literature. Medicine 2017, 96, e9498. [Google Scholar]
- Holden, R.; Wilmer, A.; Kollman, T. Primary Peritonitis due to Group A Streptococcus in a Previously Healthy Pediatric Patient. Can. J. Infect. Dis. Med. Microbiol. 2012, 23, e69–e70. [Google Scholar] [CrossRef] [PubMed]
- Borgia, S.M.; Low, D.E.; Andrighetti, S.; Rau, N.V. Group A streptococcal sepsis secondary to peritonitis and acute pelvic inflammatory disease. Eur. J. Clin. Microbiol. Infect. Dis. 2001, 20, 437–439. [Google Scholar] [CrossRef]
- Toquero, M.Z.; Flores, J.B. Secondary peritonitis due to rupture of pyometra in cervical cancer. Ginecol. Obstet. Mex. 2005, 73, 618–621. [Google Scholar]
- Sartelli, M.; Chichom-Mefire, A.; Labricciosa, F.M.; Hardcastle, T.; Abu-Zidan, F.M.; Adesunkanmi, A.K.; Ansaloni, L.; Bala, M.; Balogh, Z.J.; Beltrán, M.A.; et al. The management of intra-abdominal infections from a global perspective: 2017 WSES guidelines for management of intra-abdominal infections. World J. Emerg. Surg. 2017, 12, 36. [Google Scholar] [CrossRef]
- Robinson, E.D.; Volles, D.F.; Kramme, K.; Mathers, A.J.; Sawyer, R.G. Collaborative Antimicrobial Stewardship for Surgeons. Infect. Dis. Clin. N. Am. 2020, 34, 97–108. [Google Scholar] [CrossRef]
- Vuilleumier, H.; Halkic, N. Streptococcal toxic shock syndrome revealed by a peritonitis. Case report and review of the literature. Swiss Surg. 2001, 7, 25–27. [Google Scholar] [CrossRef]
- Legras, A.; Lodico, R.; Ferre, R.; Valleur, P.; Pautrat, K. Primary peritonitis due to Streptococcus A: Laparoscopic treatment. J. Visc. Surg. 2011, 148, e315–e317. [Google Scholar] [CrossRef] [PubMed]
- Cortese, F.; Fransvea, P.; Saputelli, A.; Ballardini, M.; Baldini, D.; Gioffre, A.; Marcello, R.; Sganga, G. Streptococcus pneumoniae primary peritonitis mimicking acute appendicitis in an immunocompetent patient: A case report and review of the literature. J. Med. Case Rep. 2019, 13, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Miyoshi-Akiyama, T.; Ikebe, T.; Watanabe, H.; Uchiyama, T.; Kirikae, T.; Kawamura, Y. Use of DNA Arrays to Identify a Mutation in the Negative Regulator, csrR, Responsible for the High Virulence of a Naturally Occurring Type M3 Group A Streptococcus Clinical Isolate. J. Infect. Dis. 2006, 193, 1677–1684. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ikebe, T.; Ato, M.; Matsumura, T.; Hasegawa, H.; Sata, T.; Kobayashi, K.; Watanabe, H. Highly Frequent Mutations in Negative Regulators of Multiple Virulence Genes in Group A Streptococcal Toxic Shock Syndrome Isolates. PLoS Pathog. 2010, 6, e1000832. [Google Scholar] [CrossRef] [PubMed]
- Kaneko, M.; Maruta, M.; Shikata, H.; Hanayama, M.; Ikebe, T. Acute abdomen due to group A streptococcus bacteremia caused by an isolate with a mutation in the csrS gene. J. Infect. Chemother. 2015, 21, 816–819. [Google Scholar] [CrossRef] [PubMed]
- Ikebe, T.; Matsumura, T.; Nihonmatsu, H.; Ohya, H.; Okuno, R.; Mitsui, C.; Kawahara, R.; Kameyama, M.; Sasaki, M.; Shimada, N.; et al. Spontaneous mutations in Streptococcus pyogenes isolates from streptococcal toxic shock syndrome patients play roles in virulence. Sci. Rep. 2016, 6, 28761. [Google Scholar] [CrossRef]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aw, A.E.Y.; Lee, J.W.K.; Tay, K.V. Primary Peritonitis Secondary to Streptococcus pyogenes in a Young Female Adult—A Case Report and Literature Review. Infect. Dis. Rep. 2021, 13, 26-32. https://doi.org/10.3390/idr13010005
Aw AEY, Lee JWK, Tay KV. Primary Peritonitis Secondary to Streptococcus pyogenes in a Young Female Adult—A Case Report and Literature Review. Infectious Disease Reports. 2021; 13(1):26-32. https://doi.org/10.3390/idr13010005
Chicago/Turabian StyleAw, Avelyn E. Y., James W. K. Lee, and Kon Voi Tay. 2021. "Primary Peritonitis Secondary to Streptococcus pyogenes in a Young Female Adult—A Case Report and Literature Review" Infectious Disease Reports 13, no. 1: 26-32. https://doi.org/10.3390/idr13010005
APA StyleAw, A. E. Y., Lee, J. W. K., & Tay, K. V. (2021). Primary Peritonitis Secondary to Streptococcus pyogenes in a Young Female Adult—A Case Report and Literature Review. Infectious Disease Reports, 13(1), 26-32. https://doi.org/10.3390/idr13010005




