Abdominal Pain—Beyond Colonic Lipoma Intussusception
Abstract
1. Introduction
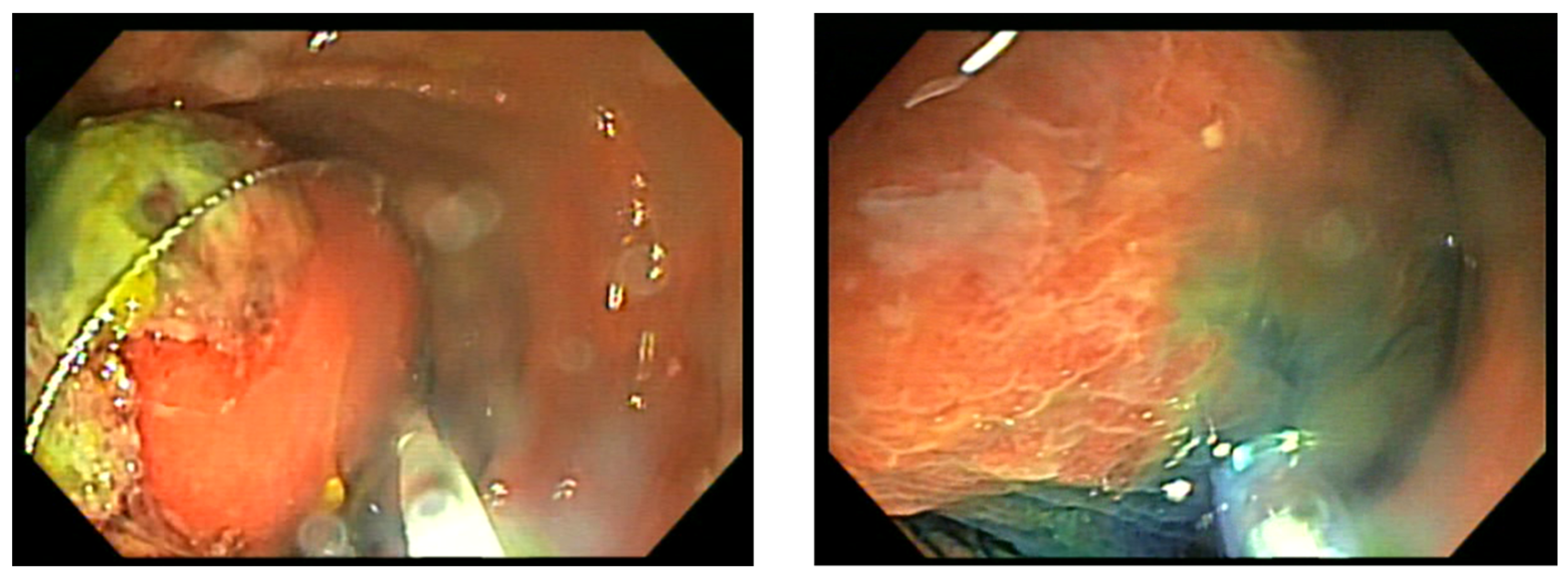
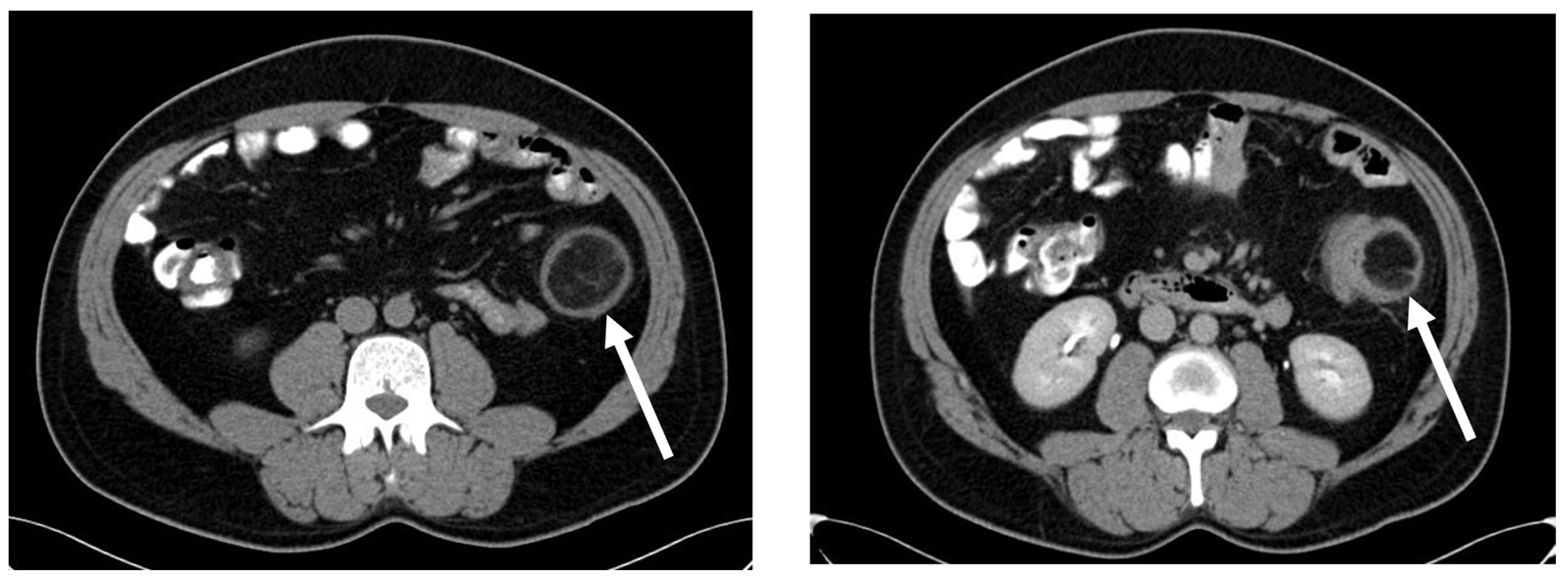
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ryan, J.; Martin, J.E.; Pollock, D.J. Fatty tumours of the large intestine: A clinicopathological review of 13 cases. Br. J. Surg. 2005, 76, 793–796. [Google Scholar] [CrossRef]
- Zhang, H.; Cong, J.C.; Chen, C.S.; Qiao, L.; Liu, E.Q. Submucous colon lipoma: A case report and review of the literature. World J. Gastroenterol. WJG 2005, 11, 3167. [Google Scholar] [CrossRef]
- Nallamothu, G.; Adler, D.G. Large colonic lipomas. Gastroenterol. Hepatol. 2011, 7, 490–492. [Google Scholar]
- Gould, D.J.; Anne Morrison, C.; Liscum, K.R.; Silberfein, E.J. A lipoma of the transverse colon causing intermittent obstruction: A rare cause for surgical intervention. Gastroenterol. Hepatol. 2011, 7, 487–490. [Google Scholar]
- Farfour, A.N.; AbuOmar, N.A.; Alsohaibani, F.I. Large lipoma of the ascending colon: A case report and review of literature. J. Surg. Case Rep. 2020, 2020, rjaa354. [Google Scholar] [CrossRef]
- Rogers, S.O.; Lee, M.C.; Ashley, S.W. Giant colonic lipoma as lead point for intermittent colo-colonic intussusception. Surgery 2002, 131, 687–688. [Google Scholar] [CrossRef]
- Paškauskas, S.; Latkauskas, T.; Valeikaite, G.; Paršeliunas, A.; Švagždys, S.; Saladžinskas, Ž.; Tamelis, A.; Pavalkis, D. Colonic intussusception caused by colonic lipoma: A case report. Medicina 2010, 46, 477. [Google Scholar] [CrossRef] [PubMed]
- Miloudi, N.; Hefaiedh, R.; Khalfallah, M. Giant lipoma of the transverse colon causing colo-colonic intussusceptions. J. Visc. Surg. 2012, 149, 421–422. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.C.; Hu, K.Q.; Jiang, Y. A 4-cm lipoma of the transverse colon causing colonic intussusception: A case report and literature review. Oncol. Lett. 2014, 8, 1090–1092. [Google Scholar] [CrossRef] [PubMed]
- Vishnu, J.; Kapil, N.; Pe, V.; Patnaik, P. Giant colonic lipoma remains a surgeon’s domain: A report of two cases. Cureus 2023, 15, e43488. [Google Scholar] [CrossRef]
- Sapalidis, K.; Laskou, S.; Kosmidis, C.; Passos, I.; Mantalobas, S.; Michalopoulos, N.; Alexandrou, V.; Koimtzis, G.; Koulouris, C.; Katsaounis, A.; et al. Symptomatic colonic lipomas: Report of two cases and a review of the literature. SAGE Open Med. Case Rep. 2019, 7, 2050313X19830477. [Google Scholar] [CrossRef]
- Bronswijk, M.; Vandenbroucke, A.M.; Bossuyt, P. Endoscopic treatment of large symptomatic colon lipomas: A systematic review of efficacy and safety. United Eur. Gastroenterol. J. 2020, 8, 1147–1154. [Google Scholar] [CrossRef]
- An, H.H.; Duong, T.T.; Van Truong, N.; Van Quoc, L.; Son, V.N.; Thang, N.V.P.; Van Thach, N.; Cuong, D.D.; Duc, N.M. A large lipoma of the descending colon: A rare case report. Radiol. Case Rep. 2021, 16, 3396–3399. [Google Scholar] [CrossRef]
- Târcoveanu, E.; Chifan, M.; Veisa, E.; Epure, O.; Florea, N. Colonic lipoma. Chirurgia 2000, 95, 353–357. [Google Scholar]
- Ullah, S.; Ahmed, H.; Jehangir, E. Giant colonic lipoma presenting with intermittent intestinal obstruction. J. Coll. Physicians Surg. Pak. 2012, 22, 792–793. [Google Scholar]
- Crocetti, D.; Sapienza, P.; Sterpetti, A.V.; Paliotta, A.; Gori, A.D.; Pedullà, G.; Toma, G.D. Surgery for Symptomatic Colon Lipoma: A Systematic Review of the Literature. Anticancer Res. 2014, 34, 6271–6276. [Google Scholar]
- Popa, B.; Ilie, M.; Sandru, V.; Hortopan, M.; Beuran, M.; Constantinescu, G. Endoscopic resection of a giant colonic lipoma causing severe anemia. J. Gastrointestin. Liver Dis. 2015, 24, 142. [Google Scholar] [CrossRef] [PubMed]
- Yano, Y.; Yamaguchi, T.; Imai, M.; Toyama, K.; Toguchi, K.; Hirabayashi, K. A Case of Giant Lipoma of the Transverse Colon with Intussusception Treated by Laparoscopic Surgery: A Review of 36 Cases Reported in the Japanese Literature. Nihon Gekakei Rengo Gakkaishi J. Jpn. Coll. Surg. 2019, 44, 753–760. [Google Scholar] [CrossRef]
- Ozen, O.; Guler, Y.; Yuksel, Y. Giant colonic lipoma causing intussusception: CT scan and clinical findings. Pan Afr. Med. J. 2019, 32, 27. [Google Scholar] [PubMed]
- Sagar, J.; Kumar, V.; Shah, D.K. Meckel’s diverticulum: A systematic review. J. R. Soc. Med. 2006, 99, 501–505. [Google Scholar] [CrossRef] [PubMed]
- Hansen, C.C.; Søreide, K. Systematic review of epidemiology, presentation, and management of Meckel’s diverticulum in the 21st century. Medicine 2018, 97, e12154. [Google Scholar] [CrossRef]
- Zani, A.; Eaton, S.; Rees, C.M.; Pierro, A. Incidentally detected Meckel diverticulum: To resect or not to resect? Ann. Surg. 2008, 247, 276–281. [Google Scholar] [CrossRef] [PubMed]
- UpToDate. Meckel’s Diverticulum. Available online: https://www.uptodate.com/contents/meckels-diverticulum (accessed on 30 December 2023).
- Park, J.J.; Wolff, B.G.; Tollefson, M.K.; Walsh, E.E.; Larson, D.R. Meckel diverticulum: The Mayo Clinic experience with 1476 patients (1950–2002). Ann. Surg. 2005, 241, 529–533. [Google Scholar] [CrossRef]
- Dumper, J.; Mackenzie, S.; Mitchell, P.; Sutherland, F.; Quan, M.L.; Mew, D. Complications of Meckel’s diverticula in adults. Can. J. Surg. 2006, 49, 353–357. [Google Scholar]
- Groebli, Y.; Bertin, D.; Morel, P. Meckel’s diverticulum in adults: Retrospective analysis of 119 cases and historical review. Eur. J. Surg. 2001, 167, 518–524. [Google Scholar] [PubMed]
- Huang, C.C.; Lai, M.W.; Hwang, F.M.; Yeh, Y.C.; Chen, S.Y.; Kong, M.S.; Lai, J.Y.; Chen, J.C.; Ming, Y.C. Diverse presentations in pediatric Meckel’s diverticulum: A review of 100 cases. Pediatr. Neonatol. 2014, 55, 369–375. [Google Scholar] [CrossRef]
- Mackey, W.C.; Dineen, P. A fifty year experience with Meckel’s diverticulum. Surg. Gynecol. Obstet. 1983, 156, 56–64. [Google Scholar] [PubMed]
- Zulfikaroglu, B.; Ozalp, N.; Zulfikaroglu, E.; Ozmen, M.M.; Tez, M.; Koc, M. Is incidental Meckel’s diverticulum resected safely? N. Z. Med. J. 2008, 121, 39–44. [Google Scholar]
- Robijn, J.; Sebrechts, E.; Miserez, M. Management of incidentally found Meckel’s diverticulum a new approach: Resection based on a Risk Score. Acta Chir. Belg. 2006, 106, 467–470. [Google Scholar] [CrossRef]
- Mukai, M.; Takamatsu, H.; Noguchi, H.; Fukushige, T.; Tahara, H.; Kaji, T. Does the external appearance of a Meckel’s diverticulum assist in choice of the laparoscopic procedure? Pediatr. Surg. Int. 2002, 18, 231–233. [Google Scholar] [CrossRef]
- Varcoe, R.L.; Wong, S.W.; Taylor, C.F.; Newstead, G.L. Diverticulectomy is inadequate treatment for short Meckel’s diverticulum with heterotopic mucosa. ANZ J. Surg. 2004, 74, 869–872. [Google Scholar] [CrossRef] [PubMed]
- Blouhos, K.; Boulas, K.A.; Tsalis, K.; Barettas, N.; Paraskeva, A.; Kariotis, I.; Keskinis, C.; Hatzigeorgiadis, A. Meckel’s diverticulum in adults: Surgical concerns. Front. Surg. 2018, 5, 55. [Google Scholar] [CrossRef] [PubMed]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dascalu, R.-I.; Constantinescu, G.; Scafa, A.; Plotogea, O.-M.; Sandru, V.; Rinja, E.M.; Jichitu, A.; Ilie, M. Abdominal Pain—Beyond Colonic Lipoma Intussusception. Gastroenterol. Insights 2024, 15, 213-220. https://doi.org/10.3390/gastroent15010015
Dascalu R-I, Constantinescu G, Scafa A, Plotogea O-M, Sandru V, Rinja EM, Jichitu A, Ilie M. Abdominal Pain—Beyond Colonic Lipoma Intussusception. Gastroenterology Insights. 2024; 15(1):213-220. https://doi.org/10.3390/gastroent15010015
Chicago/Turabian StyleDascalu, Raluca-Ioana, Gabriel Constantinescu, Alexandru Scafa, Oana-Mihaela Plotogea, Vasile Sandru, Ecaterina Mihaela Rinja, Alexandra Jichitu, and Madalina Ilie. 2024. "Abdominal Pain—Beyond Colonic Lipoma Intussusception" Gastroenterology Insights 15, no. 1: 213-220. https://doi.org/10.3390/gastroent15010015
APA StyleDascalu, R.-I., Constantinescu, G., Scafa, A., Plotogea, O.-M., Sandru, V., Rinja, E. M., Jichitu, A., & Ilie, M. (2024). Abdominal Pain—Beyond Colonic Lipoma Intussusception. Gastroenterology Insights, 15(1), 213-220. https://doi.org/10.3390/gastroent15010015





