Non-Invasive Methods for the Prediction of Spontaneous Bacterial Peritonitis in Patients with Cirrhosis
Abstract
1. Introduction
2. Serum Biomarkers
2.1. Procalcitonin
2.2. C-Reactive Protein
2.3. Homocysteine
2.4. Interferon-γ-Induced Protein
3. Hematological Indices
3.1. Neutrophil-to-Lymphocyte Ratio
3.2. Mean Platelet Volume
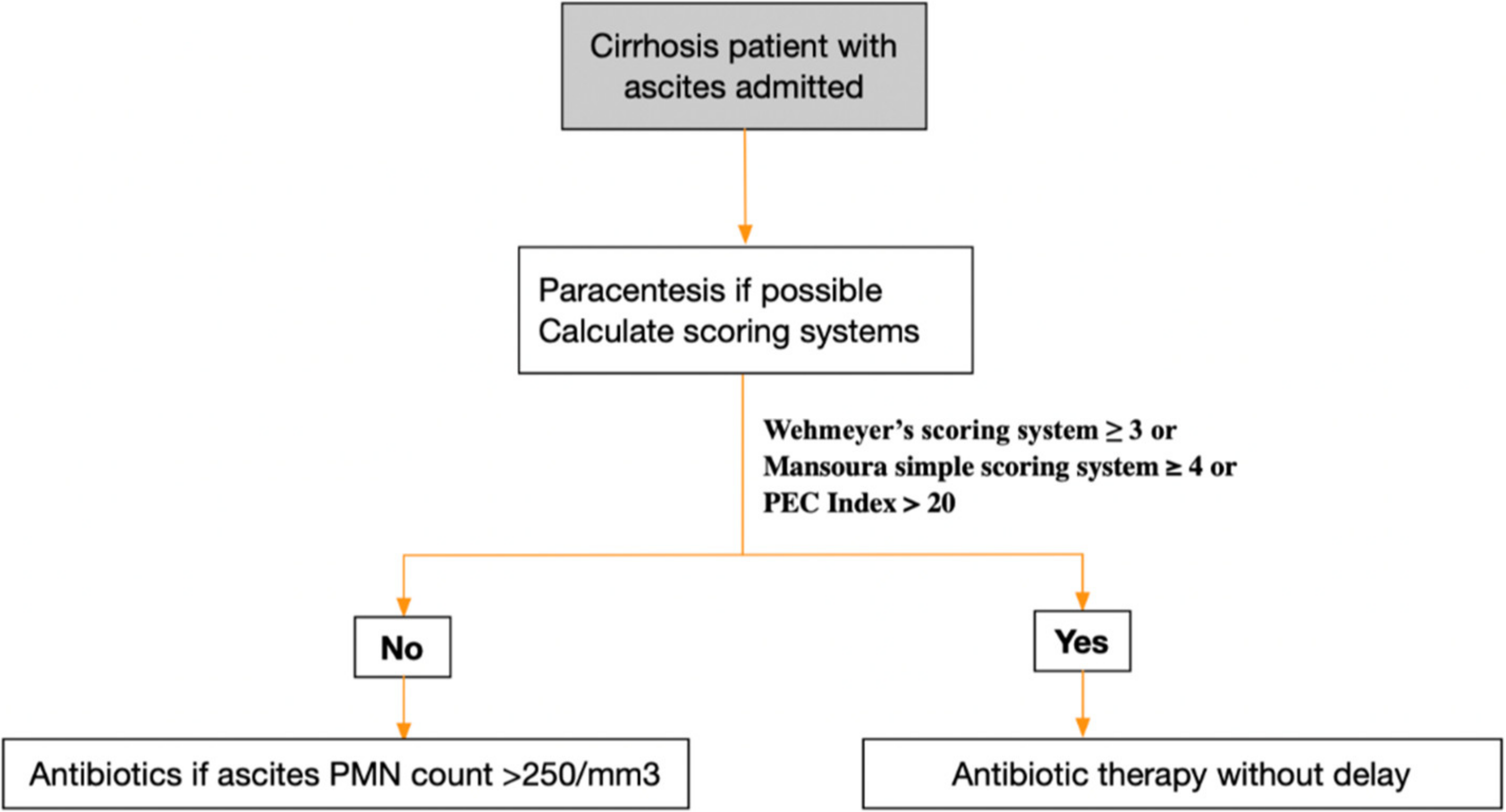
4. Models for Prediction of SBP
4.1. Scoring System including Age, CRP, and Platelet Count
4.2. Mansoura Simple Scoring System
4.3. PEC Index
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- European Association for the Study of the Liver. EASL Clinical Practice Guidelines for the management of patients with decompensated cirrhosis. J. Hepatol. 2018, 69, 406–460. [Google Scholar] [CrossRef] [PubMed]
- Piano, S.; Singh, V.; Caraceni, P.; Maiwall, R.; Alessandria, C.; Fernandez, J.; Soares, E.C.; Kim, D.J.; Kim, S.E.; Marino, M.; et al. Epidemiology and effects of bacterial infections in patients with cirrhosis worldwide. Gastroenterology 2019, 156, 1368–1380.e10. [Google Scholar] [CrossRef] [PubMed]
- Aithal, G.P.; Palaniyappan, N.; China, L.; Härmälä, S.; Macken, L.; Ryan, J.M.; Wilkes, E.A.; Moore, K.; Leithead, J.A.; Hayes, P.C.; et al. Guidelines on the management of ascites in cirrhosis. Gut 2021, 70, 9–29. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.J.; Tsukamoto, M.M.; Mathur, A.K.; Ghomri, Y.M.; Hou, L.A.; Sheibani, S.; Runyon, B.A. Delayed paracentesis is associated with increased in-hospital mortality in patients with spontaneous bacterial peritonitis. Am. J. Gastroenterol. 2014, 109, 1436–1442. [Google Scholar] [CrossRef] [PubMed]
- Biggins, S.W.; Angeli, P.; Garcia-Tsao, G.; Ginès, P.; Ling, S.C.; Nadim, M.K.; Wong, F.; Kim, W.R. Diagnosis, evaluation, and management of ascites and hepatorenal syndrome. Hepatology 2021, 74, 1014–1048. [Google Scholar] [CrossRef]
- Orman, E.S.; Hayashi, P.H.; Bataller, R.; Barritt, A.S., IV. Paracentesis is associated with reduced mortality in patients hospitalized with cirrhosis and ascites. Clin. Gastroenterol. Hepatol. 2014, 12, 496–503.e1. [Google Scholar] [CrossRef]
- Titó, L.; Rimola, A.; Ginès, P.; Llach, J.; Arroyo, V.; Rodés, J. Recurrence of spontaneous bacterial peritonitis in cirrhosis: Frequency and predictive factors. Hepatology 1988, 8, 27–31. [Google Scholar] [CrossRef]
- Thalheimer, U.; Triantos, C.K.; Samonakis, D.N.; Patch, D.; Burroughs, A.K. Infection, coagulation, and variceal bleeding in cirrhosis. Gut 2005, 54, 556–563. [Google Scholar] [CrossRef]
- Dam, G.; Vilstrup, H.; Watson, H.; Jepsen, P. Proton pump inhibitors as a risk factor for hepatic encephalopathy and spontaneous bacterial peritonitis in patients with cirrhosis with ascites. Hepatology 2016, 64, 1265–1272. [Google Scholar] [CrossRef]
- Rahimkhani, M.; Einollahi, N.; Khavari Daneshvar, H.; Dashti, N. Survey of serum procalcitonin in cirrhotic patients. Acta Medica Iranica 2013, 51, 153–156. [Google Scholar]
- Connert, S.; Stremmel, W.; Elsing, C. Procalcitonin is a valid marker of infection in decompensated cirrhosis. Z. Gastroenterol. 2003, 41, 165–170. [Google Scholar] [CrossRef]
- Spahr, L.; Morard, I.; Hadengue, A.; Vadas, L.; Pugin, J. Procalcitonin is not an accurate marker of spontaneous bacterial peritonitis in patients with cirrhosis. Hepato-Gastroenterol. 2001, 48, 502–505. [Google Scholar]
- Spahr, L.; Morard, I.; Hadengue, A.; Vadas, L.; Pugin, J. Serum and ascitic procalcitonin levels in cirrhotic patients with spontaneous bacterial peritonitis: Diagnostic value and relationship to pro-inflammatory cytokines. Intensive Care Med. 2000, 26, 1082–1088. [Google Scholar]
- Su, D.H.; Zhuo, C.; Liao, K.; Cheng, W.B.; Cheng, H.; Zhao, X.F. Value of serum procalcitonin levels in predicting spontaneous bacterial peritonitis. Hepato-Gastroenterol. 2013, 60, 641–646. [Google Scholar]
- Yang, Y.; Li, L.; Qu, C.; Zeng, B.; Liang, S.; Luo, Z.; Wang, X.; Zhong, C. Diagnostic accuracy of serum procalcitonin for spontaneous bacterial peritonitis due to end-stage liver disease: A meta-analysis. Medicine 2015, 94, e2077. [Google Scholar] [CrossRef] [PubMed]
- Lobo, S.M.; Lobo, F.R.; Bota, D.P.; Lopes-Ferreira, F.; Soliman, H.M.; Mélot, C.; Vincent, J.L. C-reactive protein levels correlate with mortality and organ failure in critically ill patients. Chest 2003, 123, 2043–2049. [Google Scholar] [CrossRef]
- Baidoshvili, A.; Nijmeijer, R.; Lagrand, W.K.; Hack, C.E.; Niessen, H.W. Localisation of C reactive protein in infarcted tissue sites of multiple organs during sepsis. J. Clin. Pathol. 2002, 55, 152–153. [Google Scholar] [CrossRef] [PubMed]
- Póvoa, P. C-reactive protein: A valuable marker of sepsis. Intensive Care Med. 2002, 28, 235–243. [Google Scholar] [CrossRef]
- Li, C.H.; Yang, R.B.; Pang, J.H.; Chang, S.S.; Lin, C.C.; Chen, C.H.; Chen, H.Y.; Chiu, T.F. Procalcitonin as a biomarker for bacterial infections in patients with liver cirrhosis in the emergency department. Acad. Emerg. Med. 2011, 18, 121–126. [Google Scholar] [CrossRef]
- Lin, Z.Y.; Chuang, W.L.; Dai, C.Y.; Yu, M.L.; Chen, S.C.; Hsieh, M.Y.; Wang, L.Y.; Tsai, J.F.; Chang, W.Y. Clinical application of serum C-reactive protein measurement in the detection of bacterial infection in patients with liver cirrhosis. Kaohsiung J. Med. Sci. 2002, 18, 121–126. [Google Scholar]
- Pieri, G.; Agarwal, B.; Burroughs, A.K. C-reactive protein and bacterial infection in cirrhosis. Ann. Gastroenterol. 2014, 27, 113. [Google Scholar] [PubMed]
- Wu, H.; Chen, L.; Sun, Y.; Meng, C.; Hou, W. The role of serum procalcitonin and C-reactive protein levels in predicting spontaneous bacterial peritonitis in patients with advanced liver cirrhosis. Pak. J. Med. Sci. 2016, 32, 1484. [Google Scholar] [CrossRef]
- Cekin, Y.; Cekin, A.H.; Duman, A.; Yilmaz, U.; Yesil, B.; Yolcular, B.O. The role of serum procalcitonin levels in predicting ascitic fluid infection in hospitalized cirrhotic and non-cirrhotic patients. Int. J. Med. Sci. 2013, 10, 1367. [Google Scholar] [CrossRef]
- Fiskerstrand, T.; Refsum, H.; Kvalheim, G.; Ueland, P.M. Homocysteine and other thiols in plasma and urine: Automated determination and sample stability. Clin. Chem. 1993, 39, 263–271. [Google Scholar] [CrossRef] [PubMed]
- Mirković, D.; Majkić-Singh, N.; Ignjatović, S. Homocysteine: Chemistry, metabolism and roles in pathophysiology processes. Jugosl. Med. Biohemija 2003, 22, 127–140. [Google Scholar] [CrossRef]
- Abdel-Razik, A.; Eldars, W.; Elhelaly, R.; Eldeeb, A.A.; Abdelsalam, M.; El-Wakeel, N.; Aboulmagd, A. Homocysteine: A new diagnostic marker in spontaneous bacterial peritonitis. Eur. J. Gastroenterol. Hepatol. 2018, 30, 779–785. [Google Scholar] [CrossRef] [PubMed]
- Guo, S.J.; Jia, L.Q.; Hu, Q.J.; Long, H.Y.; Pang, C.S.; Wen, F.Q. Diagnostic accuracy of interferon gamma-induced protein 10 for tuberculosis: A meta-analysis. Int. J. Clin. Exp. Med. 2014, 7, 93. [Google Scholar]
- Lighter, J.; Rigaud, M.; Eduardo, R.; Peng, C.H.; Pollack, H. Latent tuberculosis diagnosis in children by using the QuantiFERON-TB Gold In-Tube test. Pediatrics 2009, 123, 30–37. [Google Scholar] [CrossRef]
- Kim, J.K.; Chon, C.Y.; Kim, J.H.; Kim, Y.J.; Cho, J.H.; Bang, S.M.; Ahn, S.H.; Han, K.H.; Moon, Y.M. Changes in serum and ascitic monocyte chemotactic protein-1 (MCP-1) and IL-10 levels in cirrhotic patients with spontaneous bacterial peritonitis. J. Interferon Cytokine Res. 2007, 27, 227–230. [Google Scholar] [CrossRef]
- Abdel-Razik, A.; Mousa, N.; Elbaz, S.; Eissa, M.; Elhelaly, R.; Eldars, W. Diagnostic utility of interferon gamma-induced protein 10 kDa in spontaneous bacterial peritonitis: Single-center study. Eur. J. Gastroenterol. Hepatol. 2015, 27, 1087–1093. [Google Scholar] [CrossRef]
- Xue, T.C.; Zhang, L.; Xie, X.Y.; Ge, N.L.; Li, L.X.; Zhang, B.H.; Ye, S.L.; Ren, Z.G. Prognostic significance of the neutrophil-to-lymphocyte ratio in primary liver cancer: A meta-analysis. PLoS ONE 2014, 9, e96072. [Google Scholar] [CrossRef] [PubMed]
- Cai, Y.J.; Dong, J.J.; Dong, J.Z.; Yang, N.B.; Song, M.; Wang, Y.Q.; Chen, Y.P.; Lin, Z.; Shi, K.Q. Neutrophil-lymphocyte ratio predicts hospital-acquired bacterial infections in decompensated cirrhosis. Clin. Chim. Acta 2017, 469, 201–207. [Google Scholar] [CrossRef] [PubMed]
- Mousa, N.; Besheer, T.; Abdel-Razik, A.; Hamed, M.; Deiab, A.G.; Sheta, T.; Eldars, W. Can combined blood neutrophil to lymphocyte ratio and C-reactive protein be used for diagnosis of spontaneous bacterial peritonitis? Br. J. Biomed. Sci. 2018, 75, 71–75. [Google Scholar] [CrossRef]
- Popoiag, R.E.; Suceveanu, A.I.; Suceveanu, A.P.; Micu, S.I.; Voinea, F.; Mazilu, L.; Petcu, L.C.; Panaitescu, E.; Cozaru, G.; Fierbințeanu-Braticevici, C. Predictors of spontaneous bacterial peritonitis in Romanian adults with liver cirrhosis: Focus on the neutrophil-to-lymphocyte ratio. Exp. Ther. Med. 2021, 22, 983. [Google Scholar] [CrossRef]
- Semple, J.W.; Italiano, J.E.; Freedman, J. Platelets and the immune continuum. Nat. Rev. Immunol. 2011, 11, 264–274. [Google Scholar] [CrossRef]
- Kilciler, G.; Genc, H.; Tapan, S.; Ors, F.; Kara, M.; Karadurmus, N.; Ercin, C.N.; Karslioglu, Y.; Kilic, S.; Bagci, S.; et al. Mean platelet volume and its relationship with carotid atherosclerosis in subjects with non-alcoholic fatty liver disease. Upsala J. Med. Sci. 2010, 115, 253–259. [Google Scholar] [CrossRef] [PubMed]
- Thompson, C.B.; Jakubowski, J.A.; Quinn, P.G.; Deykin, D.; Valeri, C.R. Platelet size and age determine platelet function independently. Blood 1984, 63, 1372–1375. [Google Scholar] [CrossRef]
- Kaser, A.; Brandacher, G.; Steurer, W.; Kaser, S.; Offner, F.A.; Zoller, H.; Theurl, I.; Widder, W.; Molnar, C.; Ludwiczek, O.; et al. Interleukin-6 stimulates thrombopoiesis through thrombopoietin: Role in inflammatory thrombocytosis. Blood J. Am. Soc. Hematol. 2001, 98, 2720–2725. [Google Scholar] [CrossRef]
- Abdel-Razik, A.; Eldars, W.; Rizk, E. Platelet indices and inflammatory markers as diagnostic predictors for ascitic fluid infection. Eur. J. Gastroenterol. Hepatol. 2014, 26, 1342–1347. [Google Scholar] [CrossRef]
- Gálvez-Martínez, M.; Servín-Caamaño, A.I.; Pérez-Torres, E.; Salas-Gordillo, F.; Rivera-Gutiérrez, X.; Higuera-de la Tijera, F. Mean platelet volume as a novel predictor of systemic inflammatory response in cirrhotic patients with culture-negative neutrocytic ascites. World J. Hepatol. 2015, 7, 1001. [Google Scholar] [CrossRef]
- Abdelkader, A.H.; Jouda, A.A. The role of mean platelet volume in the diagnosis of spontaneous bacterial peritonitis. Afro-Egypt. J. Infect. Endem. Dis. 2019, 9, 193–198. [Google Scholar] [CrossRef]
- Elkafoury, R.M.; Kobtan, A.A.; Attia, T.E.; Abdelhamed, A.H. Study of platelet indices in cirrhotic patients with spontaneous bacterial peritonitis. Tanta Med. J. 2018, 46, 8. [Google Scholar] [CrossRef]
- Wehmeyer, M.H.; Krohm, S.; Kastein, F.; Lohse, A.W.; Lüth, S. Prediction of spontaneous bacterial peritonitis in cirrhotic ascites by a simple scoring system. Scand. J. Gastroenterol. 2014, 49, 595–603. [Google Scholar] [CrossRef] [PubMed]
- Metwally, K.; Fouad, T.; Assem, M.; Abdelsameea, E.; Yousery, M. Predictors of spontaneous bacterial peritonitis in patients with cirrhotic ascites. J. Clin. Transl. Hepatol. 2018, 6, 372. [Google Scholar] [CrossRef]
- Abdel-Razik, A.; Mousa, N.; Abdel-Aziz, M.; Elsherbiny, W.; Zakaria, S.; Shabana, W.; Abed, S.; Elhelaly, R.; Elzehery, R.; Eldars, W.; et al. Mansoura simple scoring system for prediction of spontaneous bacterial peritonitis: Lesson learnt. Eur. J. Gastroenterol. Hepatol. 2019, 31, 1017–1024. [Google Scholar] [CrossRef]
- Elsadek, H.M.; Elhawari, S.A.; Mokhtar, A. A novel serum index for accurate diagnosis of spontaneous bacterial peritonitis in cirrhotic patients without other infections. Egypt. Liver J. 2020, 10, 10. [Google Scholar] [CrossRef]
| Parameter | “Cut-Off” | Scoring Points |
|---|---|---|
| Age | >60 years | 1 |
| Platelet count | ≤100,000/µL | 1 |
| C-reactive protein | >60 mg/L | 2 |
| SBP Scoring System | SBP Negative (%) | SBP Positive (%) |
|---|---|---|
| 0 | 100 | 0 |
| 1 | 94.5 | 5.5 |
| 2 | 72.4 | 27.6 |
| 3 | 25 | 75 |
| 4 | 15.4 | 84.6 |
| 5 | 0 | 100 |
| Parameter | “Cut-Off” | Scoring Points |
|---|---|---|
| Age | ≥55 years | 1 |
| MPV | ≥8.5 fl | 1 |
| NLR | ≥2.5 | 1 |
| CRP | ≥40 mg/L | 2 |
| Cut-Off | Specificity (%) | Sensitivity (%) | NPV (%) | PPV (%) |
|---|---|---|---|---|
| 1 | 30.8 | 88.2 | 95.1 | 14.8 |
| 2 | 60.8 | 79.4 | 95.6 | 21.6 |
| 3 | 97.1 | 58.7 | 92.4 | 79.4 |
| 4 | 97.8 | 55.8 | 90.8 | 85.3 |
| 5 | 100 | 14.7 | 89.6 | 100 |
| Non-Invasive Test | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | LR (+) | LR (−) | AUROC |
|---|---|---|---|---|---|---|---|
| PCT [15] | 79–87 | 82%–89 | 4.94 | 0.22 | 0.92 | ||
| CRP [22] | 75 | 61.2 | 0.613 | ||||
| Hcy [26] | 95.1 | 89.3 | 68.2 | 99.2 | 0.932 | ||
| IP-10 [30] | 91 | 89 | 97 | 95 | 0.912 | ||
| NLR [34] | 98.61 | 81.94 | 0.963 | ||||
| MPV [40] | 84 | 82 | 83 | 84 | 0.9 | ||
| Wehmeyer’s Scoring system [43] | 29.4 | 100 | 100 | 83.1 | 0.68 | ||
| Mansoura simple scoring system [45] | 55.8 | 97.8 | 85.3 | 90.8 | 0.795 | ||
| PEC Index [46] | 98.33 | 96.67 | 0.977 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cao, N.H.; Ho, P.T.; Bui, H.H.; Vo, T.D. Non-Invasive Methods for the Prediction of Spontaneous Bacterial Peritonitis in Patients with Cirrhosis. Gastroenterol. Insights 2023, 14, 170-177. https://doi.org/10.3390/gastroent14020013
Cao NH, Ho PT, Bui HH, Vo TD. Non-Invasive Methods for the Prediction of Spontaneous Bacterial Peritonitis in Patients with Cirrhosis. Gastroenterology Insights. 2023; 14(2):170-177. https://doi.org/10.3390/gastroent14020013
Chicago/Turabian StyleCao, Ngoc Huynh, Phat Tan Ho, Hoang Huu Bui, and Thong Duy Vo. 2023. "Non-Invasive Methods for the Prediction of Spontaneous Bacterial Peritonitis in Patients with Cirrhosis" Gastroenterology Insights 14, no. 2: 170-177. https://doi.org/10.3390/gastroent14020013
APA StyleCao, N. H., Ho, P. T., Bui, H. H., & Vo, T. D. (2023). Non-Invasive Methods for the Prediction of Spontaneous Bacterial Peritonitis in Patients with Cirrhosis. Gastroenterology Insights, 14(2), 170-177. https://doi.org/10.3390/gastroent14020013






