Abstract
Pancreatitis is the most common complication following endoscopic retrograde cholangio-pancreatography (ERCP). With the progress of research in many drugs and technologies, promising efficacy has been achieved in preventing post-ERCP pancreatitis (PEP). Recently, combined prevention has received more attention in order to further reduce the incidence of PEP. However, there is no review about the combined prevention of PEP. This review summarizes the medication and ERCP techniques that are used to prevent PEP and emphasizes that appropriate combination prevention approaches should be based on risk stratification.
1. Introduction
Endoscopic retrograde cholangio-pancreatography (ERCP) is an important procedure to diagnose and treat hepatobiliary and pancreatic diseases. Pancreatitis is one of the most common and severe complications after ERCP, with the reported incidence ranging from 3.47% to 9.70% in recent studies [1,2]. The generally accepted definition of post-ERCP pancreatitis (PEP) was advanced by Cotton et al. in 1991 [3], which included the new or exacerbating pancreatic-type abdominal pain, accompanied by serum amylase exceeding at least three times the upper limit of the normal value occurring within 24 h post-ERCP, as well as hospital admission duration for more than one day. The severity of PEP was also defined according to the consensus criteria, which is shown in Table 1. In addition, Banks et al. [4] proposed the classification of acute pancreatitis which was used in some studies. Although differences in the criteria for defining PEP and severity classification are likely to influence the reported rates, the majority of PEP is assumed to be mild. In contrast, severe pancreatitis has a lower incidence, but still is a major contributing factor in the death of patients.

Table 1.
Severity grading of PEP.
The majority of relevant references in this review use the Cotton et al. consensus to define PEP. The mechanism of post-ERCP pancreatitis (PEP) is still unclear, which could be associated with mechanical injury, thermal injury, chemical or allergic injury, etc. These factors activate proteolytic enzymes within acinar cells, ultimately leading to cellular injury and autodigestion of the pancreas [5]. Recently, various research is being conducted to explain the mechanism and etiologies of PEP. This review mainly introduces the precautionary measures to prevent PEP.
2. Risk Factors
The risk factors related to PEP have been investigated in many studies and systematic reviews, and some patient-related risk factors (e.g., female, previous PEP, previous pancreatitis, and sphincter of Oddi dysfunction) and procedure-related risk factors (e.g., difficult cannulation, pancreatic injection, precut sphincterotomy, and non-prophylactic pancreatic duct stent) have been confirmed [6,7,8,9,10,11]. The presence of multiple factors can have a cumulative effect. Typically, patients without the above risk factors were defined as low-risk. High-risk patients were identified as patients who met one or more of the above risk factors factors [12]. In addition, there are a number of other risk factors that we need to consider, for example the research of Deenadayalu VP et al. showed that obesity increases the risk of PEP (OR = 1.143; p = 0.002) [13], and other earlier studies also found that using pancreatotoxic drugs (including estrogen, azathioprine, valproic acid, mesalazine, morphine derivatives, and prednisone) in the preoperative period of ERCP significantly increased the risk of PEP (OR = 3.7, p = 0.04) [14]. However, the use of BMI and drugs is not involved in the recent meta-analysis because of the lack of relevant clinical studies. In addition, several studies [15,16,17] have shown that the incidence of PEP progressively decreases with age and middle-aged people have a higher incidence and mortality. The pathophysiology behind that observance remains unclear. One explanation could be reduced levels of pancreatic enzyme secretion or more advanced atrophy of the pancreas in older patients [16,17].
Because of the high incidence of PEP in high-risk patients, early identification and the implementation of therapeutic strategies for high-risk patients is critical to avoid the occurrence of PEP [18,19]. Additionally, further investigations of novel risk factors of PEP are highly warranted. The risk factors of PEP are shown in Table 2.

Table 2.
Risk factors for PEP.
3. Prevention
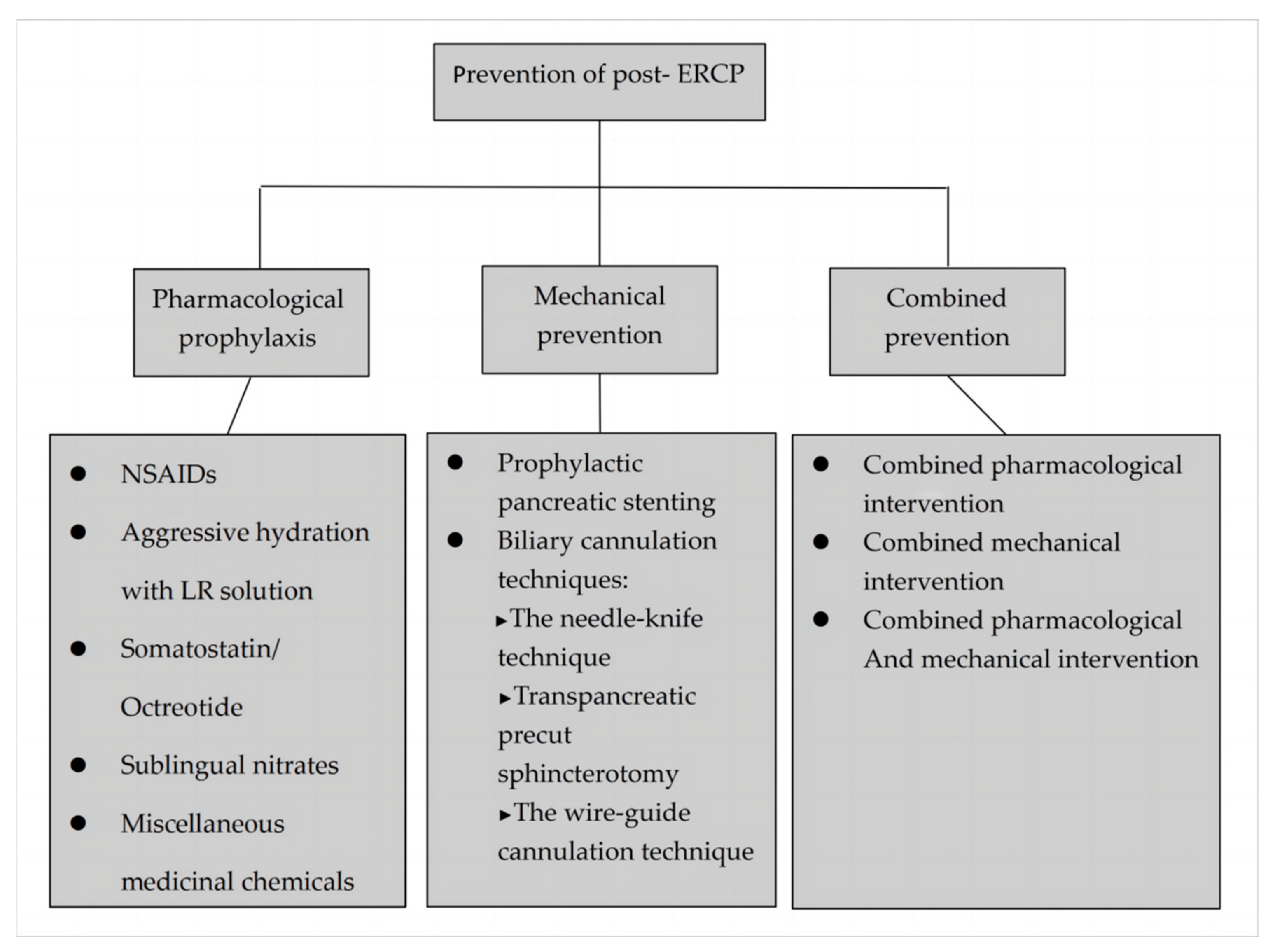
The prevention of PEP has been studied for decades, and some breakthroughs have been made in pharmacological and technological prevention measures which are discussed below in detail (Figure 1).
Figure 1.
Methods for prevention of post-ERCP pancreatitis.
3.1. Pharmacological Prophylaxis
Pharmacological prophylaxis was routinely given to patients who performed ERCP. As an ideal strategy for the prevention of PEP, medication also should have the following advantages: (1) effective and safe; (2) easily available and simple to use; (3) inexpensive. Numerous drugs to prevent PEP have been studied, including nonsteroid anti-inflammatory drugs (NSAIDs), nitroglycerin, somatostatin, octreotide, gabexate, steroids, heparin, allopurinol, etc.
3.1.1. Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
As an inexpensive, safe, and easily administered drug, NSAIDs have been the most attractive agents against PEP in the past decade. NSAIDs are potent inhibitors of prostaglandins, phospholipase A2, and neutrophil-endothelial interaction, which might prevent PEP by inhibiting synthesis of prostaglandin and interrupting the inflammatory cascade of pancreatitis [20,21,22]. A large meta analysis [23] (6 RCTs, 1300 patients) further confirmed the efficacy of NSAIDs for preventing PEP (OR: 0.46, 95% CI: 0.32–0.65, p < 0.0001). At present, there are four common routes of NSAIDs administration including intravenous injection, intramuscular injection, oral administration, and rectal suppositories. Furthermore, rectal NSAIDs administration is the most widely used due to its advantages of less gastrointestinal irritation and rapid absorption [21]. In addition, compared with other routes, rectal NSAIDs administration indicates a better clinical response in the prevention of PEP. Diclofenac and indomethacin are the main NSAIDs which have been studied and applied in clinics widely. In 2008, Elmunzer et al. [24] performed a meta-analysis (four RCTs, 912 patients) which demonstrated that rectal NSAIDs may significantly reduce the incidence of PEP (RR = 0.36, 95% CI: 0.22–0.60). However, data recruited from only four RCTs are too small to be entirely convincing. Numerous studies have shown that rectal NSAIDs have less side effects, which shows their own unique advantage. Traditionally, clinicians often use 100 mg of rectal diclofenac or rectal indomethacin immediately before ERCP in all patients without contraindications to NSAID administration.
Furthermore, Ding et al. [25] (10 RCTs, 2269 patients) found that the rectal route of NSAIDs administration seems to be more effective than other routes. A recent meta analysis has confirmed the effects of rectal NSAIDs; however, controversy still remains in the prevention of moderate to severe PEP. The study by Yang et al. [26], (12 RCTs, 3989 patients) showed that NSAIDs reduce the risk of moderate to severe PEP(RR = 0.44, 95% CI: 0.28–0.69, p < 0.01). In contrast, the study of Li et al. [27] (9 RCTs, 1883 patients) revealed that NSAIDs had no effect on the development of moderate to severe pancreatitis (RR = 0.79, 95% CI: 0.52–1.18). Thus, the effectiveness of NSAIDs for PEP prevention needs to be further evaluated. Beyond that, with gradual intense study, there are some major problems that demand discussion and emphasis, such as dosages of NSAIDs, type and timing of administration, etc. The most frequent dosage of diclofenac or indomethacin was 100 mg, which was mostly based on clinical experience. However, there is still no confirmed information about the appropriate dosage to prevent PEP. Some studies have applied certain reference values to observe the efficacy in prevention of PEP. A retrospective study [28] in Japan showed that 50 mg rectal diclofenac had superiority over the 25 mg dose in preventing PEP, which suggested that the effectiveness of NSAIDs for PEP may be dose-dependent. The latest trial [29] showed that 200 mg rectal indomethacin had no superiority over the standard 100 mg regimen in preventing PEP, which suggested that more NSAID doses are not always better. In addition, the timing of administration of rectal NSAIDs is equally important. Although Yang et al.’s subgroup analyses showed that the timing of administration (pre-or post-ERCP) and NSAID type (indomethacin or diclofenac) could not affect rectal NSAIDs’ preventive effects, more relevant research results are still lacking. This is a reminder that although remarkable achievements have been made in NSAIDs, there are still many issues to be resolved and additional experimental investigations are needed.
3.1.2. Somatostatin/Octreotide
Somatostatin and its synthetic analogue octreotide decreases pancreatic enzyme secretion by inhibiting cholecystokinin (CCK) and secretin. Earlier studies have shown that they can decrease the secretion of pancreatic enzymes, and reduce intraductal pressure and possibly proteolysis [30,31,32,33]. Although somatostatin and octreotide have been extensively investigated for the chemoprophylaxis of PEP, early studies have shown conflicting results regarding the preventive effect of somatostatin or octreotide on PEP [34,35,36].
In 2007, a meta-analysis [34] that included 16 trials compared the administration of somatostatin to controls for the incidence of pancreatitis. While pancreatitis occurred in 7.3% of controls compared with 5.3% of patients treated with somatostatin, this difference was not statistically significant (OR = 0.73; 95% CI: 0.54–1.006). However, a meta-analysis by Rudin et al. [36] (7 RCTs, 3130 patients) reported conflicting results showing that long-term somatostatin infusion significantly reduced the incidence of PEP. Similarly, in 2008, a systematic review (15 trials, 2621 patients) also did not find any benefit in favor of treatment with octreotide (OR = 0.78, 95% CI: 0.57–1.08, p = 0.49) [35]. In contrast, a meta-analysis by Zhang et al. [37] (17 RCTs, 2784 patients) showed that a sufficient dose (≥0.5 mg) of octreotide (OR = 0.45, 95% CI: 0.28–0.73, p = 0.001) was more effective in preventing PEP than a dose of <0.5 mg octreotide (OR = 1.23, 95% CI: 0.80–1.91, p = 0.35). These different results let us speculate that the preventive effect of somatostatin or octreotide may correlate directly with the dose. Furthermore, this speculation was confirmed in subsequent research. A meta-analysis of Omata et al. [38] (17 RCTs, 3818 patients) revealed that high doses of somatostatin or octreotide have a significant effect on the prevention of PEP. In recent years, several subgroup analyses have shown that when a long-term infusion or high-dose somatostatin therapy is used, the incidence of PEP is significantly reduced [39,40,41]. Thus, in accordance with current research, using high doses of somatostatin or octreotide to prevent PEP seems to be a viable option.
3.1.3. Sublingual Nitrates
Glyceryl trinitrate (GTN) as a nitricoxide donor can relax the sphincter of Oddi (SOD) and decrease SOD pressure [42]. It has been used to induce papillary dilation so far in clinicals. GTN for the prevention of PEP was confirmed in the earlier meta-analysis [43,44,45]. The most common adverse events were headache and transient hypotension, noted more frequently in trials with sublingual or intravenous delivery. Compared with other therapeutic agents that might possibly be used to reduce the frequency of PEP, the GTN has a number of advantages such as feasibility, low cost, and mild side effects.
In 2013, Ding et al. [46] performed a meta-analysis (12 RCTs, 2649 patients), which showed that the incidence of PEP was significantly reduced by GTN treatment (RR = 0.67, 95% CI: 0.52–0.87). However, GTN administration did not decrease the incidence of moderate to severe PEP (RR = 0.70, 95% CI: 0.42–1.15). After subgroup analyses, they suggested that the advantage of sublingual GTN (RR = 0.47) was greater than topical and transdermal application (RR = 1.00, RR = 0.78, respectively). The latest studies, combining NSAIDs with sublingual nitrates to prevent PEP have also achieved good results. Hence, ESGE (2019) also suggested administration of 5 mg sublingual GTN before ERCP in patients for the prevention of PEP (weak recommendation, moderate quality evidence). Further clinical trials are still required to explore the effectiveness of nitroglycerin in the prevention of PEP.
3.1.4. Aggressive Hydration with Lactated Ringer’s Solution
As the pancreatic inflammatory response causes vasodilation with intravascular volume depletion and organ hypoperfusion, perioperative aggressive hydration has attracted immense attention. Perioperative aggressive hydration can maintain pancreatic microperfusion, which can effectively delay the pancreatic inflammation and ultimately reduce the incidence of PEP [4,47]. The evidence supporting aggressive hydration fluid type to prevent PEP is unclear. Most studies have used Lactated Ringer’s (LR) solution as the preferred hydration fluid. The possible reason is that intravenous hydration with normal saline can potentiate acidosis and activate pancreatic enzymes. However, LR solution has more pH-balanced properties, which can prevent hyperchloremic metabolic acidosis [48]. The total amount of fluid used for aggressive hydration is 35–45 mL/kg, administered within 8–10 h.
The meta-analysis by Wu et al. [49] (3 RCTs, 722 patients) showed that the aggressive hydration treatment reduced the incidence of PEP (OR = 0.29; 95% CI: 0.16–0.53) and slightly shortened the length of hospital stay. The latest meta-analysis (9 RCTs, 2094 patients), including two RCTs from the above study, confirmed the previous result [50]. At the same time, the risk analysis showed that aggressive hydration reduced the risk of PEP (OR = 0.44, 95% CI: 0.28–0.69, p = 0.0004). The studies of hydration with Lactate Ringer’ s solution are showed in Table 3. However, the side effects of aggressive hydration are also obvious. Hydration volume overload may aggravate the circulatory system burden n resulting in a higher incidence of peripheral edema. Furthermore, the study of Grunwald et al. [51] showed that an increase in the amount of IV fluids administered during ERCP may increase the risk of PEP. In addition, the latest randomized prospective multicenter trial by De-Madaria et al. [52] regarding early aggressive hydration in the management of acute pancreatitis demonstrated that early aggressive fluid resuscitation resulted in a higher incidence of fluid overload without improvement in clinical outcomes of pancreatitis patients (adjusted RR, 2.85; 95% CI: 1.36–5.94, p = 0.004). Therefore, fluid overload risk should be taken into account in aggressive fluid resuscitation. Furthermore, more research is needed before the routine use of aggressive hydration to prevent PEP.

Table 3.
The project of hydration with Lactate Ringer’s solution.
3.1.5. Miscellaneous Medicinal Chemicals
Some potentially effective drugs have also been used to prevent PEP, but the results were not very satisfactory. Hereby, we have mentioned a brief summary of other drugs.
Corticosteroid is an anti-inflammatory hormone that may reduce inflammatory response during the initial steps of autodigestive cascade and relieve exudation or edema [53]. Previous studies showed that corticosteroid is able to increase the activity of C1-antipro-tease inhibitor [54], inhibiting synthesis of phospholipaseA2 [55,56]. It is suggested that corticosteroid may be used to prevent PEP. However, in 1999, a controlled prospective study [57] (535 patients) showed that the advantage of hydrocortisone is similar to placebo in preventing PEP (the incidence of PEP: 5.7% vs. 4.9%). Later, a larger study [58] (1115 patients) arrived at a similar conclusion that prophylactic orally administered corticosteroid did not reduce the frequency or severity of PEP. In 2008, Zheng et al. [59] performed a meta-analysis (7 RCTs, 2632 patients) indicating that there were no beneficial effects of corticosteroid on PEP (OR = 1.13, 95% CI: 0.89–1.44, p = 0.32). Thus, the use of corticosteroids for preventing PEP is not recommended.
Nifedipine is a widely used calcium channel inhibitor that acts on L-type calcium channels and may reduce the basal pressure of the sphincter of Oddi and the contraction amplitude and duration of the sphincter [60]. However, nifedipine has not been effective in current clinical studies. In 2002, Prat et al. [61] performed a double-blind randomized trial (nifedipine 76 patients, placebo 79 patients), which not only failed to demonstrate that nifedipine has a significant effect in preventing PEP (The rate of PEP: 13.2% vs. 17.7%, p = 0.4; respectively), but also showed that nifedipine did not reduce the frequency of difficult cannulation (OR = 3.78, 95% CI: 1.25–11.45). So far, there have been no clinical trials to support the benefits of nifedipine in preventing PEP.
Lidocaine has been shown to minimize the increase in cholecystokinin (CCK) after the diversion of the pancreatic-biliary stream [62,63]. However, the preventive effect of PEP is not significant [64].
There is evidence that heparin has anti-inflammatory effects [65,66]. However, low-dose heparin was ineffective in two previous clinical trials [67,68].
Allopurinol is a structural isomer of hypoxanthine, which has the effect of inhibiting xanthine oxidase. Allopurinol may prevent capillary injury, which is an early event regulated by oxygen-derived free radicals in the pathogenesis of acute pancreatitis [69]. However, several studies confirmed that prophylactic allopurinol was not useful for preventing PEP. In 2008, Bai et al. performed a meta-analysis [70] (4 RCTs, 1730 patients), which showed that the RR of allopurinol was 0.86 (95% CI: 0.42–1.77, p = 0.68), and the subgroup analyses showed that doses of allopurinol did not affect the results. In the same year, a larger meta-analysis [71] (6 RCTs, 1 554 patients) confirmed that prophylactic allopurinol was not effective in reducing the incidence of PEP (RR=0.74, 95% CI: 0.37–1.48, p = 0.40). The most recent study [72] (RR = 0.75, 95% CI: 0.39–1.42) confirmed this result again, so this option is not recommended.
Protease inhibitors can inhibit the activation of proteolytic enzymes and play an important role in the recognized pathogenesis of PEP [73]. Several clinical trials have shown that gabexate mesylate or ulinastatin seems to be effective in preventing PEP [74,75,76,77,78,79]. However, a subsequent meta-analysis showed that protease inhibitors had no significant effect on preventing PEP (OR: 0.65–0.67) [80,81]. It even did not have any beneficial effects on hyperamylasemia and abdominal pain after ERCP. As protease inhibitors are expensive and less effective, these agents may not be practical in routine clinical use.
3.2. Mechanical Prevention
Some mechanical preventive measures during the ERCP have also achieved good results. Below, we will mainly introduce the measures of handling difficult cannulation and prophylactic pancreatic stenting.
3.2.1. Prophylactic Pancreatic Stenting
Pancreatic duct (PD) stent placement is a substitute drainage pathway, which can maintain the patency of pancreatic drainage. PD stents are commonly made of polyethylene, which is sometimes mixed with vinyl or other softer materials, and typically have side holes [82,83,84]. In addition, clinicians have been updating PD stents to make it easily deployable without causing stent-induced ductal or parenchymal pancreatic damage. An early meta-analysis [85] (3 RCTs, 258 patients) showed that the risk of PEP in patients with PD stent was significantly reduced (OR = 0.18, 95% CI: 0.07–0.47, p = 0.001). However, the sample size of the three studies included was too small to allow a proper conclusion regarding the effects of treatment. Two subsequent meta-analyses (8 RCTs, 680 patients [86]; 14RCTs, 1 541 patients [87], respectively) confirmed that pancreatic stent placement after ERCP reduced the risk of PEP (RR = 0.32, p < 0.001 and RR = 0.39; p < 0.001, respectively).
In 2015, Fan et al. performed a larger meta-analysis [83] (15 RCTs, 1606 patients), which had more comprehensive data compared to the previous studies. The meta analysis showed that pancreatic stent placement after ERCP had a significantly lower incidence of PEP (OR = 0.35, 95% CI: 0.25–0.49, p < 0.00001). Furthermore, the subgroup analysis demonstrated that it could effectively decrease the incidence of complications and shorter hospital stay in high-risk patients. A recent meta-analysis [88] (11 RCTs, 1475 patients) obtained the same results (OR = 0.32, 95% CI: 0.23–0.45). Although pancreatic-stent placement decreases the incidence of PEP, this endoscopic maneuver also has been related to complications and additional costs. A cost-effectiveness analysis [89] showed that the use of prophylactic pancreatic stenting only for high-risk patients was the most cost-effective strategy.
At present, there is a controversy about the optimal size and length of the PD stent. Clinically, 3–5 Fr pancreatic stents have been used most widely, which may result in less ductal irritation and may spontaneously dislodge more frequently than larger-diameter ones. Some clinical trials [84,90,91] have shown that when placing a PD stent to prevent PEP, using small-caliber stents (3 Fr, 4 Fr, or 5 Fr) can minimize PD injury and promote spontaneous dislodgment. However, placing small luminal diameter stents is technically more difficult, as it can occlude early resulting in the compromise of pancreatic duct drainage, and leading to an increase in the risk of pancreatitis. In 2011, Zolotarevsky et al. [92] reported that the placement of a 5-Fr compared with a 3-Fr PS for PEP prophylaxis was easier and faster and required fewer wires. The most recent meta-analysis [93] showed that 5-Fr stents were superior to 3-Fr in preventing PEP. Therefore, for prophylactic pancreatic stenting, we suggest the use of a short 5-Fr pancreatic stent in high-risk patients.
3.2.2. Biliary Cannulation
Selective biliary intubation is the initial step to successfully enter the biliary tract during ERCP. Even an experienced endoscopist may fail in 10–15% cases [94]. Some studies [95,96,97] have indicated that every new attempt to cannulate through the papilla or repeat cannulation of the pancreatic duct increases the risk of PEP. Repeated cannulation attempts may result in ductal injury or injury to the ampulla. At the same time, in the standard contrast agent injection method, the inadvertent injection of a contrast agent into the pancreatic duct may cause chemical damage to the pancreas. Therefore, several supplementary techniques have been developed to overcome the difficult cannulation, including the needle-knife technique, the double guide-wire technique, and the technique trans pancreatic sphincterotomy (TPS) [98,99].
3.2.3. Needle-Knife Precut Sphincterotomy
The needle-knife technique was first described in the early 1980s, including needle-knife papillotomy (NKP) and needle-knife fistulotomy (NKF) [100,101]. Initial studies have found this technique to be an independent risk factor for the development of PEP [102,103,104], but it is more likely that the increased risk of PEP stems from the prolonged cannulation attempts with resultant papillary edema, stressing the importance of implementing alternative techniques earlier rather than later to reduce the incidence of PEP [105,106,107]. In 2014, a systemic review and meta-analysis by Choudhary et al. [108] suggested that needle-knife fistulotomy significantly lowered the risk of PEP (OR = 0.27, 95% CI: 0.09–0.82; p = 0.02) by an absolute risk reduction of 5%. Therefore, NKF has been recommended as the preferred technique for difficult biliary cannulation by current guidelines [12]. Although needle-knife precut sphincterotomy greatly increases the efficiency of biliary cannulation [109], the technique also carries the risk of postoperative complications (including bleeding, perforation, and cholangitis), ideally performed by experienced endoscopists [110].
3.2.4. Transpancreatic Precut Sphincterotomy (TPS)
TPS was first described by Goff in 1995. As the technical accessibility is not so complicated and the incision depth is easier to control, TPS may be a simple way to find the way to bile duct compared with needle-knife sphincterotomy [111]. A retrospective study in Taiwan [112] showed that TPS had an acceptable success rate (83.0% vs. 74.2%, p = 0.34) and a similar PEP rate (16.1% vs. 6.4%, p = 0.17) compared with needle-knife therapy. Although there is no evidence that TPS is superior to needle-knife therapy, it is relatively easier for young endoscopists to learn this technique. In a word, it is a promising operative approach.
3.2.5. The Wire-Guide Cannulation (WGC) Technique
The WGC technique is an alternative to the standard contrast agent injection method, which can increase the success rate and reduce the risk of PEP [113,114,115]. The guidewire technology uses a soft-tipped guidewire to cannulate the bile duct, which is believed to potentially limit papillary trauma and need for precut sphincterotomies. In addition, this technique avoids the injection of a contrast medium into PD and prevents submucosal injection in the papilla, further reducing the risk of pancreatitis [116,117].
In 2009, a meta-analysis [118] (5 RCTs, 1762 patients) showed that the use of the guide wire-assisted cannulation technique not only increased the primary cannulation rate (OR = 2.05, 95% CI: 1.27–3.31), but also reduced the need for the precut technique (the guide wire-assisted cannulation technique compared with the standard-method: 10.3 vs. 14.7%, respectively). Furthermore, the guide wire to achieve deep biliary cannulation significantly reduced the risk of PEP (RR = 0.23, 95% CI: 0.13–0.41).
In 2013, Tse et al. [119] performed a larger meta-analysis (12 RCTs, 3450 patients) and reached similar conclusions that the guide wire assisted cannulation technique and resulted in a greater primary cannulation rate (RR = 1.07, 95% CI: 1.00–1.15), fewer precut sphincterotomies (RR = 0.75, 95% CI: 0.60–0.95), and a significant reduction in PEP (RR = 0.51, 95% CI: 0.32–0.82).
According to current studies, the use rate of WGC cannulation is increasing when performing ERCP. In addition, the double-guidewire technique (DGT) also seems to be a good cannulation measure [120,121,122]. It has been postulated that the DGT can increase the success rate of cannulation and reduce the risk of PEP [123,124]. Although the current research results are controversial in some aspects [125,126], in 2020, the ESGE recommended the DGT with prophylactic pancreatic stenting to address difficult biliary cannulation [12].
4. Combined Prevention
Combined prevention has actually been extensively used in high-risk patients. Clinicians generally use rectal NSAIDs and prophylactic pancreatic stenting to prevent PEP in high-risk patients, and the treatment effect is obvious. However, for low-risk patients, prophylactic pancreatic stenting is not an efficient and cost-effective approach. Therefore, we think that PEP-related risk factors should be used to stratify risk among patients better before the procedure, which would help physicians decide on preventative measures, such as drug prophylaxis or PD stenting.
For low-risk patients, clinicians emphasize the use of pharmacological treatment to prevent PEP, which is generally accepted for their obvious advantages such as good efficacy and a cheaper price. Based on the current research, we found that the use of rectal NSAIDs alone cannot completely prevent PEP and the use of other drugs only, such as GTN and somatostatin/ octreotide, also have some limitations. Thus, we suggest the combination of multiple drugs to prevent PEP in low-risk patients.
So far, the combined prevention of multiple drugs has shown effective results in the latest clinical trials, which is a good start. The result confirms further investigations are worthy and needed. In 2014, Sotoudehmanesh et al. [127] performed a randomized, double-blind controlled trial (300 patients) to evaluate the efficacy of the combination of indomethacin and sublingual nitrates compared with indomethacin alone to prevent PEP. The experimental results were pleasantly surprising. Rectal indomethacin plus sublingual nitrate significantly reduced the incidence of PEP compared with indomethacin alone (6.7% vs. 15.3%, RR = 0.39, 95% CI: 0.18–0.86, p = 0.016). In addition, adding drugs did not increase drug-related adverse effects. The latest trial [128] (886 patients) obtained similar results that rectal diclofenac plus sublingual nitrate significantly reduced the incidence of PEP compared with diclofenac alone (5.6% vs. 9.5%, RR = 0.59, 95% CI: 0.37–0.95, p = 0.03). Although some patients developed hypotension and headache in the combined group, they were significantly relieved after simple treatment. Furthermore, the relative benefit of additional sublingual nitrate had a tendency to decline according to the number of risk factors for PEP. Due to it being simple, inexpensive, and well tolerated, the combination of rectally administered NSAIDs and sublingual nitrate should be an ideal pharmacologic prophylaxis in low-risk patients (moderate quality evidence).
In addition, there are other drug combinations being studied. The study of Katsinelos et al. [129] (540 patients) demonstrated that the preventive effect of rectal diclofenac plus somatostatin was better than that of rectal diclofenac alone (low quality evidence). In the multivariate analysis, pretreatment with diclofenac plus somatostatin significantly reduced the risk of PEP (OR = 0.423, 95% CI: 0.201–0.889, p = 0.023). Hajalikhani et al. [130] compared the preventive effects of diclofenac and aggressive hydration by LR (n = 107) with diclofenac alone (n = 112). Although the results showed that there was no significant difference between them (0.9% vs. 2.7%, p = 0.622), the serum levels of pancreatic enzymes in the combination group were significantly lower than those of diclofenac alone group at 2 h, 8 h, and 24 h after ERCP (p < 0.001 at all levels). The author believes that this result may be caused by the low overall PEP rate and the small sample size of the trial. A previous randomized, double-blind trial [131] (192 high risk patients) showed that LR plus indomethacin had a lower PEP rate (6% vs. 21%, p = 0.04) and a lower readmission rate (2% vs. 13%; p = 0.03) compared with normal saline plus placebo. Although these results cannot confirm the superiority of NSAIDs plus LR, they showed that the combination of NSAIDs and aggressive hydration to prevent PEP is feasible. Excitingly, the latest network meta-analysis [132] (24 studies, 11,321 patients) showed that indomethacin plus LR solution, followed by diclofenac plus nitrate and indomethacin plus normal saline, are the most efficacious combinations of pharmacological agents for the prevention of PEP (low quality evidence).
These experimental results undoubtedly bring confidence to the combination of drugs to prevent PEP. However, it is not the case that increasing the type of drug use can greatly improve the preventive effect. For example, a latest meta-analysis of rectal indomethacin plus topical epinephrine to prevent PEP (3 RCTs, 2244 patients) showed that this combination had no more advantage than rectal indomethacin alone (RR = 1.15, 95% CI: 0.62–2.2) [133]. This is an indication that the combination of drugs to prevent PEP is not simply adding drugs to improve the preventive effect. There are many questions to be considered in combined prevention, including which drugs should be combined, whether the dose of combined drug should be changed, whether the adverse drug reactions of the combined drug are obvious, etc. At present, there are few large-scale clinical trials in this area, and we hope that more large-sample studies can be published. Clinically, effective drug combinations use are worthy of promotion in low-risk patients.
For high-risk patients, factors that promote the occurrence of PEP are diverse and complex, combining drugs with mechanical prophylaxis to prevent PEP in high-risk patients is necessary, with PD stenting being the recommended option (Table 4).

Table 4.
Summary of benefit of various pharmacological agents and mechanical measures for prevention of PEP.
At present, the most commonly used mechanical prophylaxis to prevent PEP in high-risk patients is PD stenting, which is recommended in most patients with difficult cannulation, suspected sphincter dysfunction, history of post-ERCP pancreatitis, or in those with other risk factors. Most of the studies of PD stenting to prevent PEP were conducted before the routine use of pharmacological prophylaxis including indomethacin (high quality evidence). In addition to this, an atraumatic and efficient method of cannulation needs to be used in difficult intubation cases, such as the WGC technique, TPS, or needle-knife precut sphincterotomy. Until further evidence are available, it is advisable to combine pharmacological with mechanical prophylaxis in high-risk cases (moderate quality evidence).
5. Conclusions
With the development and application of ERCP, the burden caused by its complications is undoubtedly the most important contraindication in the implementation of ERCP. With the aim of reducing the incidence of PEP, the development of a combined prevention is necessary and inevitable. The purpose of this review was to describe current research on the prevention of PEP and to value the reasonable combination of multiple drugs and mechanical measures in the prevention of PEP. We expect that future updates and more high-quality studies will identify the optimal combination regimen that reduces the incidence of PEP.
Author Contributions
Y.Z. and Y.F. drafted and edited the manuscript. Y.Z., Y.L., and Y.F. provided critical revisions of the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Andriulli, A.; Loperfido, S.; Napolitano, G.; Niro, G.; Valvano, M.R.; Spirito, F.; Pilotto, A.; Forlano, R. Incidence rates of post-ERCP complications: A systematic survey of prospective studies. Am. J. Gastroenterol. 2007, 102, 1781–1788. [Google Scholar] [CrossRef]
- Kochar, B.; Akshintala, V.S.; Afghani, E.; Elmunzer, B.J.; Kim, K.J.; Lennon, A.M.; Khashab, M.A.; Kalloo, A.N.; Singh, V.K. Incidence, severity, and mortality of post-ERCP pancreatitis: A systematic review by using randomized, controlled trials. Gastrointest. Endosc. 2015, 81, 143–149. [Google Scholar] [CrossRef] [PubMed]
- Cotton, P.B.; Lehman, G.; Vennes, J.; Geenen, J.E.; Russell, R.C.; Meyers, W.C.; Liguory, C.; Nickl, N. Endoscopic sphincterotomy complications and their management: An attempt at consensus. Gastrointest. Endosc. 1991, 37, 383–393. [Google Scholar] [CrossRef] [PubMed]
- Banks, P.A.; Bollen, T.L.; Dervenis, C.; Gooszen, H.G.; Johnson, C.D.; Sarr, M.G.; Tsiotos, G.G.; Vege, S.S. Acute Pancreatitis Classification Working Group. Classification of acute pancreatitis—2012: Revision of the Atlanta classification and definitions by international consensus. Gut 2013, 62, 102–111. [Google Scholar] [CrossRef] [PubMed]
- Pezzilli, R.; Romboli, E.; Campana, D.; Corinaldesi, R. Mechanisms involved in the onset of post-ERCP pancreatitis. JOP 2002, 3, 162–168. [Google Scholar]
- Cheng, C.L.; Sherman, S.; Watkins, J.L.; Barnett, J.; Freeman, M.; Geenen, J.; Ryan, M.; Parker, H.; Frakes, J.T.; Fogel, E.L.; et al. Risk factors for post-ERCP pancreatitis: A prospective multicenter study. Am. J. Gastroenterol. 2006, 101, 139–147. [Google Scholar] [CrossRef]
- Cotton, P.B.; Garrow, D.A.; Gallagher, J.; Romagnuolo, J. Risk factors for complications after ERCP: A multivariate analysis of 11,497 procedures over 12 years. Gastrointest. Endosc. 2009, 70, 80–88. [Google Scholar] [CrossRef]
- Christoforidis, E.; Goulimaris, I.; Kanellos, I.; Tsalis, K.; Demetriades, C.; Betsis, D. Post-ERCP pancreatitis and hyperamylasemia: Patient-related and operative risk factors. Endoscopy 2002, 34, 286–292. [Google Scholar] [CrossRef]
- Cheon, Y.K.; Cho, K.B.; Watkins, J.L.; McHenry, L.; Fogel, E.L.; Sherman, S.; Lehman, G.A. Frequency and severity of post-ERCP pancreatitis correlated with extent of pancreatic ductal opacification. Gastrointest. Endosc. 2007, 65, 385–393. [Google Scholar] [CrossRef]
- Chen, J.-J.; Wang, X.-M.; Liu, X.-Q.; Li, W.; Dong, M.; Suo, Z.-W.; Ding, P.; Li, Y. Risk factors for post-ERCP pancreatitis: A systematic review of clinical trials with a large sample size in the past 10 years. Eur. J. Med. Res. 2014, 19, 26. [Google Scholar] [CrossRef]
- Ding, X.; Zhang, F.; Wang, Y. Risk factors for post-ERCP pancreatitis: A systematic review and meta-analysis. Surgeon 2015, 13, 218–229. [Google Scholar] [CrossRef]
- Dumonceau, J.-M.; Kapral, C.; Aabakken, L.; Papanikolaou, I.S.; Tringali, A.; Vanbiervliet, G.; Beyna, T.; Dinis-Ribeiro, M.; Hritz, I.; Mariani, A.; et al. ERCP-related adverse events: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy 2020, 52, 127–149. [Google Scholar] [CrossRef]
- Fujisawa, T.; Kagawa, K.; Hisatomi, K.; Kubota, K.; Sato, H.; Nakajima, A.; Matsuhashi, N. Obesity with abundant subcutaneous adipose tissue increases the risk of post-ERCP pancreatitis. J. Gastroenterol. 2016, 51, 931–938. [Google Scholar] [CrossRef]
- Perney, P.; Berthier, E.; Pageaux, G.P.; Hillaire-Buys, D.; Roques, V.; Fabbro-Peray, P.; Melki, M.; Hanslik, B.; Bauret, P.; Larrey, D.; et al. Are drugs a risk factor of post-ERCP pancreatitis? Gastrointest. Endosc. 2003, 58, 696–700. [Google Scholar] [CrossRef]
- Day, L.W.; Lin, L.; Somsouk, M. Adverse events in older patients undergoing ERCP: A systematic review and meta-analysis. Endosc. Int. Open 2014, 2, E28–E36. [Google Scholar] [CrossRef]
- Finkelmeier, F.; Tal, A.; Ajouaou, M.; Filmann, N.; Zeuzem, S.; Waidmann, O.; Albert, J. ERCP in elderly patients: Increased risk of sedation adverse events but low frequency of post-ERCP pancreatitis. Gastrointest. Endosc. 2015, 82, 1051–1059. [Google Scholar] [CrossRef]
- Lukens, F.J.; Howell, D.A.; Upender, S.; Sheth, S.G.; Jafri, S.-M.R. ERCP in the Very Elderly: Outcomes Among Patients Older than Eighty. Am. J. Dig. Dis. 2009, 55, 847–851. [Google Scholar] [CrossRef]
- Huibregtse, K. Complications of Endoscopic Sphincterotomy and Their Prevention. N. Engl. J. Med. 1996, 335, 961–963. [Google Scholar] [CrossRef]
- Freeman, M.L. Adverse outcomes of ERCP. Gastrointest. Endosc. 2002, 56, S273–S282. [Google Scholar] [CrossRef]
- Mäkelä, A.; Kuusi, T.; Schröder, T. Inhibition of serum phospholipase-A2 in acute pancreatitis by pharmacological agents in vitro. Scand J Clin Lab Invest. 1997, 57, 401–407. [Google Scholar] [CrossRef]
- Davies, N.M.; Anderson, K.E. Clinical phamacokinetics of diclofenac. Therapeutic insights and pitfalls. Clin. Pharamakokinet. 1997, 33, 184–213. [Google Scholar] [CrossRef] [PubMed]
- Sotoudehmanesh, R.; Khatibian, M.; Kolahdoozan, S.; Ainechi, S.; Malboosbaf, R.; Nouraie, M. Indomethacin may reduce the incidence and severity of acute pancreatitis after ERCP. Am. J. Gastroenterol. 2007, 102, 978–983. [Google Scholar] [CrossRef] [PubMed]
- Dai, H.F.; Wang, X.W.; Zhao, K. Role of nonsteroidal anti-inflammatory drugs in the prevention of post-ERCP pancreatitis: A meta-analysis. Hepatobiliary Pancreat. Dis. Int. 2009, 8, 11–16. [Google Scholar] [PubMed]
- Elmunzer, B.J.; Waljee, A.K.; Elta, G.H.; Taylor, J.R.; Fehmi, S.M.A.; Higgins, P.D.R. A meta-analysis of rectal NSAIDs in the prevention of post-ERCP pancreatitis. Gut 2008, 57, 1262–1267. [Google Scholar] [CrossRef] [PubMed]
- Ding, X.; Chen, M.; Huang, S.; Zhang, S.; Zou, X. Nonsteroidal anti-inflammatory drugs for prevention of post-ERCP pancreatitis: A meta-analysis. Gastrointest. Endosc. 2012, 76, 1152–1159. [Google Scholar] [CrossRef]
- Yang, C.; Zhao, Y.; Li, W.; Zhu, S.; Yang, H.; Zhang, Y.; Liu, X.; Peng, N.; Fan, P.; Jin, X. Rectal nonsteroidal anti-inflammatory drugs administration is effective for the prevention of post-ERCP pancreatitis: An updated meta-analysis of randomized controlled trials. Pancreatology 2017, 17, 681–688. [Google Scholar] [CrossRef]
- Li, X.; Tao, L.P.; Wang, C.H. Effectiveness of nonsteroidal anti-inflammatory drugs in prevention of post-ERCP pancreatitis: A meta-analysis. World J. Gastroenterol. 2014, 20, 12322–12329. [Google Scholar] [CrossRef]
- Yoshihara, T.; Horimoto, M.; Kitamura, T.; Osugi, N.; Ikezoe, T.; Kotani, K.; Sanada, T.; Higashi, C.; Yamaguchi, D.; Ota, M.; et al. 25 mg versus 50 mg dose of rectal diclofenac for prevention of post-ERCP pancreatitis in Japanese patients: A retrospective study. BMJ Open 2015, 5, e006950. [Google Scholar] [CrossRef]
- Fogel, E.L.; Lehman, G.A.; Tarnasky, P.; Cote, G.; Schmidt, S.E.; Waljee, A.K.; Higgins, P.D.R.; Watkins, J.L.; Sherman, S.; Kwon, R.S.Y.; et al. US Cooperative for Outcomes Research in Endoscopy (USCORE). Rectal indometacin dose escalation for prevention of pancreatitis after endoscopic retrograde cholangiopancreatography in high-risk patients: A double-blind, randomised controlled trial. Lancet Gastroenterol. Hepatol. 2020, 5, 132–141. [Google Scholar] [CrossRef]
- Raptis, S.; Schlegel, W.; Lehmann, E.; Dollinger, H.C.; Zoupas, C. Effects of somatostatin on the exocrine pancreas and the release of duodenal hormones. Metabolism 1978, 27, 1321–1328. [Google Scholar] [CrossRef]
- Dollinger, H.C.; Raptis, S.; Pfeiffer, E.F. Effects of somatostatin on exocrine and endocrine pancreatic function stimulated by intestinal hormones in man. Horm. Metab. Res. 1976, 8, 74–78. [Google Scholar] [CrossRef]
- Schlegel, W.; Raptis, S.; Harvey, R.F.; Oliver, J.M.; Pfeiffer, E.F. Inhibition of cholecystokinin-pancreozymin release by somatostatin. Lancet 1977, 2, 166–168. [Google Scholar] [CrossRef]
- Foster, E.; Leung, J. Pharmacotherapy for the prevention of post-ERCP pancreatitis. Am. J. Gastroenterol. 2007, 102, 52–55. [Google Scholar] [CrossRef]
- Andriulli, A.; Leandro, G.; Federici, T.; Ippolito, A.; Forlano, R.; Iacobellis, A.; Annese, V. Prophylactic administration of somatostatin or gabexate does not prevent pancreatitis after ERCP: An updated meta-analysis. Gastrointest. Endosc. 2007, 65, 624–632. [Google Scholar] [CrossRef]
- Bai, Y.; Gao, J.; Zou, D.W.; Li, Z.S. Prophylactic octreotide administration does not prevent post-endoscopic retrograde cholangiopancreatography pancreatitis: A meta-analysis of randomized controlled trials. Pancreas 2008, 37, 241–256. [Google Scholar] [CrossRef]
- Rudin, D.; Kiss, A.; Wetz, R.V.; Sottile, V.M. Somatostatin and gabexate for post-endoscopic retrograde cholangiopancreatography pancreatitis prevention: Meta-analysis of randomized placebo-controlled trials. J. Gastroenterol. Hepatol. 2007, 22, 977–983. [Google Scholar] [CrossRef]
- Zhang, Y.; Chen, Q.B.; Gao, Z.Y.; Xie, W.F. Meta-analysis: Octreotide prevents post-ERCP pancreatitis, but only at sufficient doses. Aliment. Pharmacol. Ther. 2009, 29, 1155–1164. [Google Scholar] [CrossRef]
- Omata, F.; Deshpande, G.; Tokuda, Y.; Takahashi, O.; Ohde, S.; Carr-Locke, D.L.; Jacobs, J.L.; Mine, T.; Fukui, T. Meta-analysis: Somatostatin or its long-acting analogue, octreotide, for prophylaxis against post-ERCP pancreatitis. J. Gastroenterol. 2010, 45, 885–895. [Google Scholar] [CrossRef]
- Qin, X.; Lei, W.S.; Xing, Z.X.; Shi, F. Prophylactic effect of somatostatin in preventing Post-ERCP pancreatitis: An updated meta-analysis. Saudi J. Gastroenterol. 2015, 21, 372–378. [Google Scholar]
- Hu, J.; Li, P.L.; Zhang, T.; Chen, J.P.; Hu, Y.J.; Yu, Z.; Wang, J.P.; Zhu, D.; Tong, X.F. Role of Somatostatin in Preventing Post-endoscopic Retrograde Cholangiopancreatography (ERCP) Pancreatitis: An Update Meta-analysis. Front. Pharmacol. 2016, 7, 489. [Google Scholar] [CrossRef]
- Wang, G.; Xiao, G.; Xu, L.; Qiu, P.; Li, T.; Wang, X.; Wen, P.; Wen, J.; Xiao, X. Effect of somatostatin on prevention of post-endoscopic retrograde cholangiopancreatography pancreatitis and hyperamylasemia: A systematic review and meta-analysis. Pancreatology 2018, 18, 370–378. [Google Scholar] [CrossRef]
- Luman, W.; Pryde, A.; Heading, R.C.; Palmer, K.R. Topical glyceryltrinitrate relaxes the sphincter of Oddi. Gut 1997, 40, 541–543. [Google Scholar] [CrossRef]
- Shao, L.M.; Chen, Q.Y.; Chen, M.Y.; Cai, J.T. Nitroglycerin in the prevention of post-ERCP pancreatitis: A meta-analysis. Dig. Dis. Sci.. 2010, 55, 1–7. [Google Scholar] [CrossRef]
- Chen, B.; Fan, T.; Wang, C.-H. A meta-analysis for the effect of prophylactic GTN on the incidence of post-ERCP pancreatitis and on the successful rate of cannulation of bile ducts. BMC Gastroenterol. 2010, 10, 85. [Google Scholar] [CrossRef]
- Bai, Y.; Xu, C.; Yang, X.; Gao, J.; Zou, D.-W.; Li, Z.-S. Glyceryl trinitrate for prevention of pancreatitis after endoscopic retrograde cholangiopancreatography: A meta-analysis of randomized, double-blind, placebo-controlled trials. Endoscopy 2009, 41, 690–695. [Google Scholar] [CrossRef]
- Ding, J.; Jin, X.; Pan, Y.; Liu, S.; Li, Y. Glyceryl trinitrate for prevention of post-ERCP pancreatitis and improve the rate of cannulation: A meta-analysis of prospective, randomized, controlled trials. PLoS ONE 2013, 8, e75645. [Google Scholar] [CrossRef]
- Wall, I.; Badalov, N.; Baradarian, R.; Iswara, K.; Li, J.J.; Tenner, S. Decreased mortality in acute pancreatitis related to early aggressive hydration. Pancreas 2011, 40, 547–550. [Google Scholar] [CrossRef]
- Wu, B.U.; Hwang, J.Q.; Gardner, T.H.; Repas, K.; Delee, R.; Yu, S.; Smith, B.; Banks, P.A.; Conwell, D.L. Lactated Ringer’s solution reduces systemic inflammation compared with saline in patients with acute pancreatitis. Clin. Gastroenterol. Hepatol. 2011, 9, 710–717. [Google Scholar] [CrossRef]
- Wu, D.; Wan, J.; Xia, L.; Chen, J.; Zhu, Y.; Lu, N. The Efficiency of Aggressive Hydration With Lactated Ringer Solution for the Prevention of Post-ERCP Pancreatitis: A Systematic Review and Meta-analysis. J. Clin. Gastroenterol. 2017, 51, e68–e76. [Google Scholar] [CrossRef]
- Radadiya, D.; Devani, K.; Arora, S.; Charilaou, P.; Brahmbhatt, B.; Young, M.; Reddy, C. Peri-Procedural Aggressive Hydration for Post Endoscopic Retrograde Cholangiopancreatography (ERCP) Pancreatitis Prophylaxsis: Meta-analysis of Randomized Controlled Trials. Pancreatology 2019, 19, 819–827. [Google Scholar] [CrossRef]
- Grunwald, D.; Wadhwa, V.; Sawhney, M.S. Hemodynamic Variation and Intravenous Fluids Administered During ERCP and the Association With Post-ERCP Pancreatitis. Pancreas 2016, 45, 293–297. [Google Scholar] [CrossRef] [PubMed]
- de-Madaria, E.; Buxbaum, J.L.; Maisonneuve, P.; García García de Paredes, A.; Zapater, P.; Guilabert, L.; Vaillo-Rocamora, A.; Rodríguez-Gandía, M.Á.; Donate-Ortega, J.; Lozada-Hernández, E.E.; et al. Aggressive or Moderate Fluid Resuscitation in Acute Pancreatitis. N. Engl. J. Med. 2022, 387, 989–1000. [Google Scholar] [CrossRef] [PubMed]
- Steinberg, W.; Tenner, S. Acute pancreatitis. N. Engl. J. Med. 1994, 330, 1198–1210. [Google Scholar] [CrossRef] [PubMed]
- Lasser, E.C.; Lang, J.H.; Lyon, S.G.; Hamblin, A.E.; Howard, M. Glucocorti-coid-induced elevations of C1-esterase inhibitor: A mechanism for protection against lethal dose range contrast challenge in rabbits. Investig. Radiol. 1981, 16, 20–23. [Google Scholar] [CrossRef] [PubMed]
- Bettinger, J.R.; Grendell, J.H. Intracellular events in the pathogenesis of acute pancreatitis. Pancreas 1991, 6 (Suppl. 1), S2–S6. [Google Scholar] [CrossRef]
- Weiner, G.R.; Geenen, J.E.; Hogan, W.J.; Catalano, M.F. Use of corticosteroids in the prevention of post-ERCP pancreatitis. Gastrointest. Endosc. 1995, 42, 579–583. [Google Scholar] [CrossRef]
- De Palma, G.D.; Catanzano, C. Use of corticosteriods in the prevention of post-ERCP pancreatitis: Results of a controlled prospective study. Am. J. Gastroenterol. 1999, 94, 982–985. [Google Scholar] [CrossRef]
- Sherman, S.; Blaut, U.; Watkins, J.L.; Barnett, J.; Freeman, M.; Geenen, J.; Ryan, M.; Parker, H.; Frakes, J.T.; Fogel, E.L.; et al. Does prophylactic administration of corticosteroid reduce the risk and severity of post-ERCP pancreatitis: A randomized, prospective, multicenter study. Gastrointest. Endosc. 2003, 58, 23–29. [Google Scholar] [CrossRef]
- Zheng, M.-H.; Bai, J.; Yuan, B.; Lin, F.; You, J.; Lu, M.; Gong, Y.; Chen, Y. Meta-analysis of prophylactic corticosteroid use in post-ERCP pancreatitis. BMC Gastroenterol. 2008, 8, 6. [Google Scholar] [CrossRef]
- Guelrud, M.; Mendoza, S.; Rossiter, G.; Ramirez, L.; Barkin, J. Effect of nifedipine on sphincter of Oddi motor activity: Studies in healthy volunteers and patients with biliary dyskinesia. Gastroenterology 1988, 95, 1050–1055. [Google Scholar] [CrossRef]
- Prat, F.; Amaris, J.; Ducot, B.; Bocquentin, M.; Fritsch, J.; Choury, A.D.; Pelletier, G.; Buffet, C. Nifedipine for prevention of post-ERCP pancreatitis: A prospective, double-blind randomized study. Gastrointest. Endosc. 2002, 56, 202–208. [Google Scholar] [CrossRef]
- Karlstrom, L.; Cassuto, J.; Jodal, M.; Lundgren, O. The importance of the enteric nervous system for the bile-salt-induced secretion in the small intestine of the rat. Scand. J. Gastroenterol. 1983, 18, 117–123. [Google Scholar] [CrossRef]
- Louie, D.S.; May, D.; Miller, P.; Owyang, C. Cholecystokinin mediates feedback regulation of pancreatic enzyme secretion in rats. Am. J. Physiol. 1986, 250, G252–G259. [Google Scholar] [CrossRef]
- Schwartz, J.J.; Lew, R.J.; Ahmad, N.A.; Shah, J.N.; Ginsberg, G.G.; Kochman, M.L.; Brensinger, C.M.; Long, W.B. The effect of lidocaine sprayed on the major duodenal papilla on the frequency of post-ERCP pancreatitis. Gastrointest. Endosc. 2004, 59, 179–184. [Google Scholar] [CrossRef]
- Salas, A.; Sans, M.; Soriano, A.; Reverter, J.C.; Anderson, D.C.; Piqué, J.M.; Panés, J. Heparin attenuates TNF-alpha induced inflammatory response through a CD11b dependent mechanism. Gut 2000, 47, 88–96. [Google Scholar] [CrossRef]
- Tyrrell, D.J.; Horne, A.P.; Holme, K.R.; Page, C.P. Heparin in inflammation: Potential therapeutic applications beyond anti-coagulation. Adv. Pharmacol. 1999, 46, 151–208. [Google Scholar]
- Barkay, O.; Niv, E.; Santo, E.; Bruck, R.; Hallak, A.; Konikoff, F.M. Low-dose heparin for the prevention of post-ERCP pancreatitis: A randomized placebo-controlled trial. Surg. Endosc. 2008, 22, 1971–1976. [Google Scholar] [CrossRef]
- Rabenstein, T.; Fischer, B.; Wießner, V.; Schmidt, H.; Radespiel-Tröger, M.; Hochberger, J.; Mühldorfer, S.; Nusko, G.; Messmann, H.; Schölmerich, J.; et al. Low–molecular-weight heparin does not prevent acute post-ERCP pancreatitis. Gastrointest. Endosc. 2004, 59, 606–613. [Google Scholar] [CrossRef]
- Sanfey, H.; Bulkley, G.; Cameron, J.L. Pathogenesis of acute pancreatitis: Role of oxygen-derived free radicals in the pathogenesis. Surg. Forum. 1983, 33, 222–224. [Google Scholar] [CrossRef]
- Bai, Y.; Gao, J.; Zhang, W.; Zou, D.; Li, Z. Meta-analysis: Allopurinol in the prevention of postendoscopic retrograde cholangiopancreatography pancreatitis. Aliment. Pharmacol. Ther. 2008, 28, 557–564. [Google Scholar] [CrossRef]
- Zheng, M.; Chen, Y.; Bai, J.; Xin, Y.; Pan, X.; Zhao, L. Meta-analysis of prophylactic allopurinol use in post-endoscopic retrograde cholangiopancreatography pancreatitis. Pancreas 2008, 37, 247–253. [Google Scholar] [CrossRef] [PubMed]
- Cao, W.L.; Yan, W.S.; Xiang, X.H.; Chen, K.; Xia, S.H. Prevention effect of allopurinol on post-endoscopic retrograde cholangiopancreatography pancreatitis: A meta-analysis of prospective randomized controlled trials. PLoS ONE 2014, 9, e107350. [Google Scholar] [CrossRef] [PubMed]
- Di Francesco, V.; Mariani, A.; Angelini, G.; Masci, E.; Frulloni, L.; Talamini, G.; Passaretti, S.; Testoni, P.; Cavallini, G. Effects of gabexate mesilate, a protease inhibitor, on human sphincter of Oddi motility. Dig. Dis. Sci. 2002, 47, 741–745. [Google Scholar] [CrossRef] [PubMed]
- Cavallini, G.; Tittobello, A.; Frulloni, L.; Masci, E.; Mariana, A.; Di Francesco, V. Gabexate for the prevention of pancreatic damage related to endoscopic retrograde cholangiopancreatography. Gabexate in digestive endoscopy--Italian Group. N. Engl. J. Med. 1996, 335, 919–923. [Google Scholar] [CrossRef] [PubMed]
- Masci, E.; Cavallini, G.; Mariani, A.; Frulloni, L.; Testoni, P.A.; Curioni, S.; Tittobello, A.; Uomo, G.; Costamagna, G.; Zambelli, S.; et al. Gabexate in Digestive Endoscopy-Italian Group II. Comparison of two dosing regimens of gabexate in the prophylaxis of post-ERCP pancreatitis. Am. J. Gastroenterol. 2003, 98, 2182–2186. [Google Scholar] [CrossRef]
- Xing, G.S.; Wu, S.M.; Zhang, X.W.; Ge, Z.Z. Clinical trial of gabexate in the prophylaxis of post-endoscopic retrograde cholangiopan-creatography pancreatitis. Braz. J. Med. Biol. Res. 2006, 39, 85–90. [Google Scholar] [CrossRef]
- Tsujino, T.; Komatsu, Y.; Isayama, H.; Hirano, K.; Sasahira, N.; Yamamoto, N.; Toda, N.; Ito, Y.; Nakai, Y.; Tada, M.; et al. Ulinastatin for pancreatitis after endoscopic retrograde cholangiopancreatography: A randomized, controlled trial. Clin. Gastroenterol. Hepatol. 2005, 3, 376–383. [Google Scholar] [CrossRef]
- Fujishiro, H.; Adachi, K.; Imaoka, T.; Hashimoto, T.; Kohge, N.; Moriyama, N.; Suetsugu, H.; Kawashima, K.; Komazawa, Y.; Ishimura, N.; et al. Ulinastatin shows preventive effect on post-endoscopic retrograde cholangiopancreatography pancreatitis in a multicenter prospective randomized study. J. Gastroenterol. Hepatol. 2006, 21, 1065–1069. [Google Scholar] [CrossRef]
- Ueki, T.; Otani, K.; Kawamoto, K.; Shimizu, A.; Fujimura, N.; Sakaguchi, S.; Matsui, T. Comparison between ulinastatin and gabexate mesylate for the prevention of post-endoscopic retrograde cholangiopancreatography pancreatitis: A prospective, randomized trial. J. Gastroenterol. 2007, 42, 161–167. [Google Scholar] [CrossRef]
- Zheng, M.H.; Bai, J.L.; Meng, M.B.; Chen, Y.P. Gabexate mesylate in the prevention of post-endoscopic retrograde cholangiopancreatography pancreatitis: A systematic review and meta-analysis update. Curr. Ther. Res. Clin. Exp. 2008, 69, 288–304. [Google Scholar] [CrossRef]
- Zheng, M.-H.; Chen, Y.; Yang, X.; Li, J.; Zhang, Y.; Zeng, Q. Gabexate in the prophylaxis of post-ERCP pancreatitis: A meta-analysis of randomized controlled trials. BMC Gastroenterol. 2007, 7, 6. [Google Scholar] [CrossRef]
- Lella, F.; Bagnolo, F.; Colombo, E.; Bonassi, U. A simple way of avoiding post-ERCP pancreatitis. Gastrointest. Endosc. 2004, 59, 830–834. [Google Scholar] [CrossRef]
- Fan, J.-H.; Qian, J.-B.; Wang, Y.-M.; Shi, R.-H.; Zhao, C.-J. Updated meta-analysis of pancreatic stent placement in preventing post-endoscopic retrograde cholangiopancreatography pancreatitis. World J. Gastroenterol. 2015, 21, 7577–7583. [Google Scholar] [CrossRef]
- Chahal, P.; Tarnasky, P.R.; Petersen, B.T.; Topazian, M.D.; Levy, M.J.; Gostout, C.J.; Baron, T.H. Short 5Fr vs long 3Fr pancreatic stents in patients at risk for post-endoscopic retrograde cholangiopancreatography pancreatitis. Clin. Gastroenterol. Hepatol. 2009, 7, 834–839. [Google Scholar] [CrossRef]
- Singh, P.; Das, A.; Isenberg, G.; Wong, R.C.; Sivak, M.V.; Agrawal, D.; Chak, A. Does prophylactic pancreatic stent placement reduce the risk of post-ERCP acute pancreatitis? A meta-analysis of controlled trials. Gastrointest. Endosc. 2004, 60, 544–550. [Google Scholar] [CrossRef]
- Mazaki, T.; Masuda, H.; Takayama, T. Prophylactic pancreatic stent placement and post-ERCP pancreatitis: A systematic review and meta-analysis. Endoscopy 2010, 42, 842–853. [Google Scholar] [CrossRef]
- Mazaki, T.; Mado, K.; Masuda, H.; Shiono, M. Prophylactic pancreatic stent placement and post-ERCP pancreatitis: An updated meta-analysis. J. Gastroenterol. 2014, 49, 343–355. [Google Scholar] [CrossRef]
- Sugimoto, M.; Takagi, T.; Suzuki, R.; Konno, N.; Asama, H.; Sato, Y.; Irie, H.; Watanabe, K.; Nakamura, J.; Kikuchi, H.; et al. Pancreatic stents to prevent post-endoscopic retrograde cholangiopancreatography pancreatitis: A meta-analysis. World J. Meta-Anal. 2019, 7, 249–258. [Google Scholar] [CrossRef]
- Das, A.; Singh, P.; Sivak, M.V., Jr.; Chak, A. Pancreatic-stent placement for prevention of post-ERCP pancreatitis: A cost-effectiveness analysis. Gastrointest. Endosc. 2007, 65, 960–968. [Google Scholar] [CrossRef]
- Rashdan, A.; Fogel, E.L.; McHenry, L.; Sherman, S.; Temkit, M.; Lehman, G.A. Improved stent characteristics for prophylaxis of post-ERCP pancreatitis. Clin. Gastroenterol. Hepatol. 2004, 2, 322–329. [Google Scholar] [CrossRef]
- Lee, T.H.; Moon, J.H.; Choi, H.J.; Han, S.H.; Cheon, Y.K.; Cho, Y.D.; Park, S.-H.; Kim, S.-J. Prophylactic temporary 3F pancreatic duct stent to prevent post-ERCP pancreatitis in patients with a difficult biliary cannulation: A multicenter, prospective, randomized study. Gastrointest. Endosc. 2012, 76, 578–585. [Google Scholar] [CrossRef]
- Zolotarevsky, E.; Fehmi, S.M.; Anderson, M.A.; Schoenfeld, P.S.; Elmunzer, B.J.; Kwon, R.S.; Piraka, C.R.; Wamsteker, E.J.; Scheiman, J.M.; Korsnes, S.J.; et al. Prophylactic 5-Fr pancreatic duct stents are superior to 3-Fr stents: A randomized controlled trial. Endoscopy 2011, 43, 325–330. [Google Scholar] [CrossRef]
- Afghani, E.; Akshintala, V.S.; Khashab, M.A.; Law, J.K.; Hutfless, S.M.; Kim, K.J.; Lennon, A.M.; Kalloo, A.N.; Singh, V.K. 5-Fr vs. 3-Fr pancreatic stents for the prevention of post-ERCP pancreatitis in high-risk patients: A systematic review and network meta-analysis. Endoscopy 2014, 46, 573–580. [Google Scholar] [CrossRef]
- Freeman, M.L. Adverse outcomes of endoscopic retrograde cholangiopancreatography: Avoidance and management. Gastrointest. Endosc. Clin. N. Am. 2003, 13, 775–798. [Google Scholar] [CrossRef]
- Freeman, M.L.; DiSario, J.A.; Nelson, D.B.; Fennerty, M.B.; Lee, J.G.; Bjorkman, D.J.; Overby, C.S.; Aas, J.; Ryan, M.E.; Bochna, G.S.; et al. Risk factors for post-ERCP pancreatitis: A prospective, multicenter study. Gastrointest. Endosc. 2001, 54, 425–434. [Google Scholar] [CrossRef] [PubMed]
- Huibregste, K.K.M. Endoscopic retrograde cholangiopancreatography, endoscopic sphincterotomy and endoscopic biliary and pancreatic drainage. In Textbook of Gastroenterology; Yamada, T., Ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 1995; pp. 2590–2617. [Google Scholar]
- Bailey, A.; Bourke, M.; Williams, S.; Walsh, P.; Murray, M.; Lee, E.; Kwan, V.; Lynch, P. A prospective randomized trial of cannulation technique in ERCP: Effects on technical success and post-ERCP pancreatitis. Endoscopy 2008, 40, 296–301. [Google Scholar] [CrossRef] [PubMed]
- Pécsi, D.; Farkas, N.; Hegyi, P.; Balaskó, M.; Czimmer, J.; Garami, A.; Illés, A.; Mosztbacher, D.; Pár, G.; Párniczky, A.; et al. Transpancreatic sphincterotomy has a higher cannulation success rate than needle-knife precut papillotomy—A meta-analysis. Endoscopy 2017, 49, 874–887. [Google Scholar] [CrossRef] [PubMed]
- Freeman, M.L.; Guda, N.M. ERCP cannulation: A review of reported techniques. Gastrointest. Endosc. 2005, 61, 112–125. [Google Scholar] [CrossRef] [PubMed]
- Siegel, J. Precut Papillotomy: A method to improve success of ERCP and Papillotomy. Endoscopy 1980, 12, 130–133. [Google Scholar] [CrossRef]
- Saritas, U.; Ustundag, Y.; Harmandar, F. Precut sphincterotomy: A reliable salvage for difficult biliary cannulation. World J. Gastroenterol. 2013, 19, 1–7. [Google Scholar] [CrossRef]
- Masci, E.; Mariani, A.; Curioni, S.; Testoni, P.A. Risk factors for pancreatitis following endoscopic retrograde cholangiopancreatography: A meta-analysis. Endoscopy 2003, 35, 830–834. [Google Scholar]
- Vandervoort, J.; Soetikno, R.M.; Tham, T.C.; Wong, R.C.; Ferrari, A.P., Jr.; Montes, H.; Roston, A.D.; Slivka, A.; Lichtenstein, D.R.; Ruymann, F.W.; et al. Risk factors for complications after performance of ERCP. Gastrointest. Endosc. 2002, 56, 652–656. [Google Scholar] [CrossRef]
- Testoni, P.A.; Giussani, A.; Vailati, C.; Testoni, S.; Di Leo, M.; Mariani, A. Precut sphincterotomy, repeated cannulation and post-ERCP pancreatitis in patients with bile duct stone disease. Dig. Liver Dis. 2011, 43, 792–796. [Google Scholar] [CrossRef]
- Bailey, A.A.; Bourke, M.J.; Kaffes, A.J.; Byth, K.; Lee, E.Y.; Williams, S.J. Needle-knife sphincterotomy: Factors predicting its use and the relationship with post-ERCP pancreatitis (with video). Gastrointest. Endosc. 2010, 71, 266–271. [Google Scholar] [CrossRef]
- Testoni, P.A.; Testoni, S.; Giussani, A. Difficult biliary cannulation during ERCP: How to facilitate biliary access and minimize the risk of post-ERCP pancreatitis. Dig. Liver Dis. 2011, 43, 596–603. [Google Scholar] [CrossRef]
- Swan, M.P.; Alexander, S.; Moss, A.; Williams, S.J.; Ruppin, D.; Hope, R.; Bourke, M.J. Needle knife sphincterotomy does not increase the risk of pancreatitis in patients with difficult biliary cannulation. Clin. Gastroenterol. Hepatol. 2013, 11, 430–436. [Google Scholar] [CrossRef]
- Choudhary, A.; Winn, J.; Siddique, S.; Arif, M.; Arif, Z.; Hammoud, G.M.; Puli, S.R.; Ibdah, J.A.; Bechtold, M.L. Effect of precut sphincterotomy on post-endoscopic retrograde cholangiopancreatography pancreatitis: A systematic review and meta-analysis. World J. Gastroenterol. 2014, 20, 4093–4101. [Google Scholar] [CrossRef]
- Aronson, N.; Flamm, C.R.; Bohn, R.L.; Mark, D.H.; Speroff, T. Evidence-based assessment: Patient, procedure, or operator factors associated with ERCP complications. Gastrointest. Endosc. 2002, 56, S294–S302. [Google Scholar] [CrossRef]
- Chan, T.T.; Chew, M.C.H.; Tang, R.S.Y. Troubleshooting Difficult Bile Duct Access: Advanced ERCP Cannulation Techniques, Percutaneous Biliary Drainage, or EUS-Guided Rendezvous Technique? Gastroenterol. Insights 2021, 12, 405–422. [Google Scholar] [CrossRef]
- Catalano, M.F.; Linder, J.D.; Geenen, J.E. Endoscopic transpancreatic papillary septotomy for inaccessible obstructed bile ducts: Comparison with standard pre-cut papillotomy. Gastrointest. Endosc. 2004, 60, 557–561. [Google Scholar] [CrossRef]
- Liang, K.-S.; Chen, C.-C.; Liao, W.-C.; Kuo, Y.-T.; Tseng, L.-W.; He, W.-T.; Wang, H.-P. Comparison between transpancreatic sphincterotomy and needle-knife fistulotomy in difficulty biliary access, a retrospective study in Taiwan. BMC Gastroenterol. 2020, 20, 194. [Google Scholar] [CrossRef] [PubMed]
- Artifon, E.L.; Sakai, P.; Cunha, J.E.; Halwan, B.; Ishioka, S.; Kumar, A. Guidewire Cannulation Reduces Risk of Post-ERCP Pancreatitis and Facilitates Bile Duct Cannulation. Am. J. Gastroenterol. 2007, 102, 2147–2153. [Google Scholar] [CrossRef] [PubMed]
- Lee, T.H.; Park, D.H.; Park, J.Y.; Kim, E.O.; Lee, Y.S.; Park, J.H.; Lee, S.H.; Chung, I.K.; Kim, H.S.; Park, S.H.; et al. Can wire-guided cannulation prevent post-ERCP pancreatitis? A prospective randomized trial. Gastrointest. Endosc. 2009, 69, 444–449. [Google Scholar] [CrossRef] [PubMed]
- Nambu, T.; Ukita, T.; Shigoka, H.; Omuta, S.; Maetani, I. Wire-guided selective cannulation of the bile duct with a sphincterotome: A prospective randomized comparative study with the standard method. Scand. J. Gastroenterol. 2011, 46, 109–115. [Google Scholar] [CrossRef] [PubMed]
- Nakai, Y.; Isayama, H.; Tsujino, T.; Sasahira, N.; Hirano, K.; Kogure, H.; Sasaki, T.; Kawakubo, K.; Yagioka, H.; Yashima, Y.; et al. Impact of introduction of wire-guided cannulation in therapeutic biliary endoscopic retrograde cholangiopancreatography. J. Gastroenterol. Hepatol. 2011, 26, 1552–1558. [Google Scholar] [CrossRef]
- Cheung, J.; Tsoi, K.K.; Quan, W.L.; Lau, J.Y.; Sung, J.J. Guidewire versus conventional contrast cannulation of the common bile duct for the prevention of post-ERCP pancreatitis: A systematic review and meta-analysis. Gastrointest. Endosc. 2009, 70, 1211–1219. [Google Scholar] [CrossRef]
- Cennamo, V.; Fuccio, L.; Zagari, R.M.; Eusebi, L.H.; Ceroni, L.; Laterza, L.; Fabbri, C.; Bazzoli, F. Can a Wire-Guided Cannulation Technique Increase Bile Duct Cannulation Rate and Prevent Post-ERCP Pancreatitis?: A Meta-Analysis of Randomized Controlled Trials. Am. J. Gastroenterol. 2009, 104, 2343–2350. [Google Scholar] [CrossRef]
- Tse, F.; Yuan, Y.; Moayyedi, P.; Leontiadis, G.I. Guide wire-assisted cannulation for the prevention of post-ERCP pancreatitis: A systematic review and meta-analysis. Endoscopy 2013, 45, 605–618. [Google Scholar] [CrossRef]
- Gyökeres, T.; Duhl, J.; Varsányi, M.; Schwab, R.; Burai, M.; Pap, A. Double guide wire placement for endoscopic pancreaticobiliary procedures. Endoscopy 2003, 35, 95–96. [Google Scholar] [CrossRef]
- Maeda, S.; Hayashi, H.; Hosokawa, O.; Dohden, K.; Hattori, M.; Morita, M.; Kidani, E.; Ibe, N.; Tatsumi, S. Prospective Randomized Pilot Trial of Selective Biliary Cannulation Using Pancreatic Guide-Wire Placement. Endoscopy 2003, 35, 721–724. [Google Scholar] [CrossRef]
- Gotoh, Y.; Tamada, K.; Tomiyama, T.; Wada, S.; Ohashi, A.; Satoh, Y.; Higashizawa, T.; Miyata, T.; Ido, K.; Sugano, K. A new method for deep cannulation of the bile duct by straightening the pancreatic duct. Gastrointest. Endosc. 2001, 53, 820–822. [Google Scholar] [CrossRef]
- Tse, F.; Yuan, Y.; Moayyedi, P.; Leontiadis, G.I.; Barkun, A.N. Double-guidewire technique in difficult biliary cannulation for the prevention of post-ERCP pancreatitis: A systematic review and meta-analysis. Endoscopy 2016, 49, 15–26. [Google Scholar] [CrossRef]
- Dumonceau, J.M.; Devière, J.; Cremer, M. A new method of achieving deep cannulation of the common bile duct during endoscopic retrograde cholangiopancreatography. Endoscopy 1998, 30, S80. [Google Scholar] [CrossRef]
- Eminler, A.T.; Parlak, E.; Koksal, A.S.; Toka, B.; Uslan, M.I. Wire-guided cannulation over a pancreatic stent method increases the need for needle-knife precutting ın patients with difficult biliary cannulations. Gastrointest. Endosc. 2018, 89, 301–308. [Google Scholar] [CrossRef]
- Freeman, M.L.; Guda, N.M. Prevention of post-ERCP pancreatitis: A comprehensive review. Gastrointest. Endosc. 2004, 59, 845–864. [Google Scholar] [CrossRef]
- Sotoudehmanesh, R.; Eloubeidi, M.A.; Asgari, A.A.; Farsinejad, M.; Khatibian, M. A randomized trial of rectal indomethacin and sublingual nitrates to prevent post-ERCP pancreatitis. Am. J. Gastroenterol. 2014, 109, 903–909. [Google Scholar] [CrossRef]
- Tomoda, T.; Kato, H.; Ueki, T.; Akimoto, Y.; Hata, H.; Fujii, M.; Harada, R.; Ogawa, T.; Wato, M.; Takatani, M.; et al. Combination of Diclofenac and Sublingual Nitrates Is Superior to Diclofenac Alone in Preventing Pancreatitis After Endoscopic Retrograde Cholangiopancreatography. Gastroenterology 2019, 156, 1753–1760. [Google Scholar] [CrossRef]
- Katsinelos, P.; Fasoulas, K.; Paroutoglou, G.; Chatzimavroudis, G.; Beltsis, A.; Terzoudis, S.; Dimou, E.; Zavos, C.; Kaltsa, A.; Kountouras, J. Combination of diclofenac plus somatostatin in the prevention of post-ERCP pancreatitis: A randomized, double-blind, placebo-controlled trial. Endoscopy 2011, 44, 53–59. [Google Scholar] [CrossRef]
- Hajalikhani, M.; Emami, M.H.; Khodadoostan, M.; Shavakhi, A.; Rezaei, M.; Soluki, R. Combination of diclofenac and aggressive hydration for the prevention of post-ERCP pancreatitis. Gastroenterol. Hepatol. Bed. Bench. 2018, 11, 319–324. [Google Scholar]
- Mok, S.R.S.; Ho, H.C.; Shah, P.; Patel, M.; Gaughan, J.P.; Elfant, A.B. Lactated Ringer’s solution in combination with rectal indomethacin for prevention of post-ERCP pancreatitis and readmission: A prospective randomized, double-blinded, placebo-controlled trial. Gastrointest. Endosc. 2017, 85, 1005–1013. [Google Scholar] [CrossRef]
- Oh, H.C.; Kang, H.; Park, T.Y.; Choi, G.J.; Lehman, G.A. Prevention of post-endoscopic retrograde cholangiopancreatography pancreatitis with a combination of pharmacological agents based on rectal non-steroidal anti-inflammatory drugs: A systematic review and network meta-analysis. J. Gastroenterol. Hepatol. 2021, 36, 1403–1413. [Google Scholar] [CrossRef] [PubMed]
- Aziz, M.; Ghanim, M.; Sheikh, T.; Sharma, S.; Ghazaleh, S.; Fatima, R.; Khan, Z.; Lee-Smith, W.; Nawras, A. Rectal indomethacin with topical epinephrine versus indomethacin alone for preventing Post-ERCP pancreatitis—A systematic review and meta-analysis. Pancreatology 2020, 20, 356–361. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).