Anemia in Newly Diagnosed Pediatric Patients with Inflammatory Bowel Disease
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Patients
2.2. Statistical Methods
2.3. Ethics
3. Results
3.1. Characteristics of the Study Population
3.2. Prevalence of Anemia
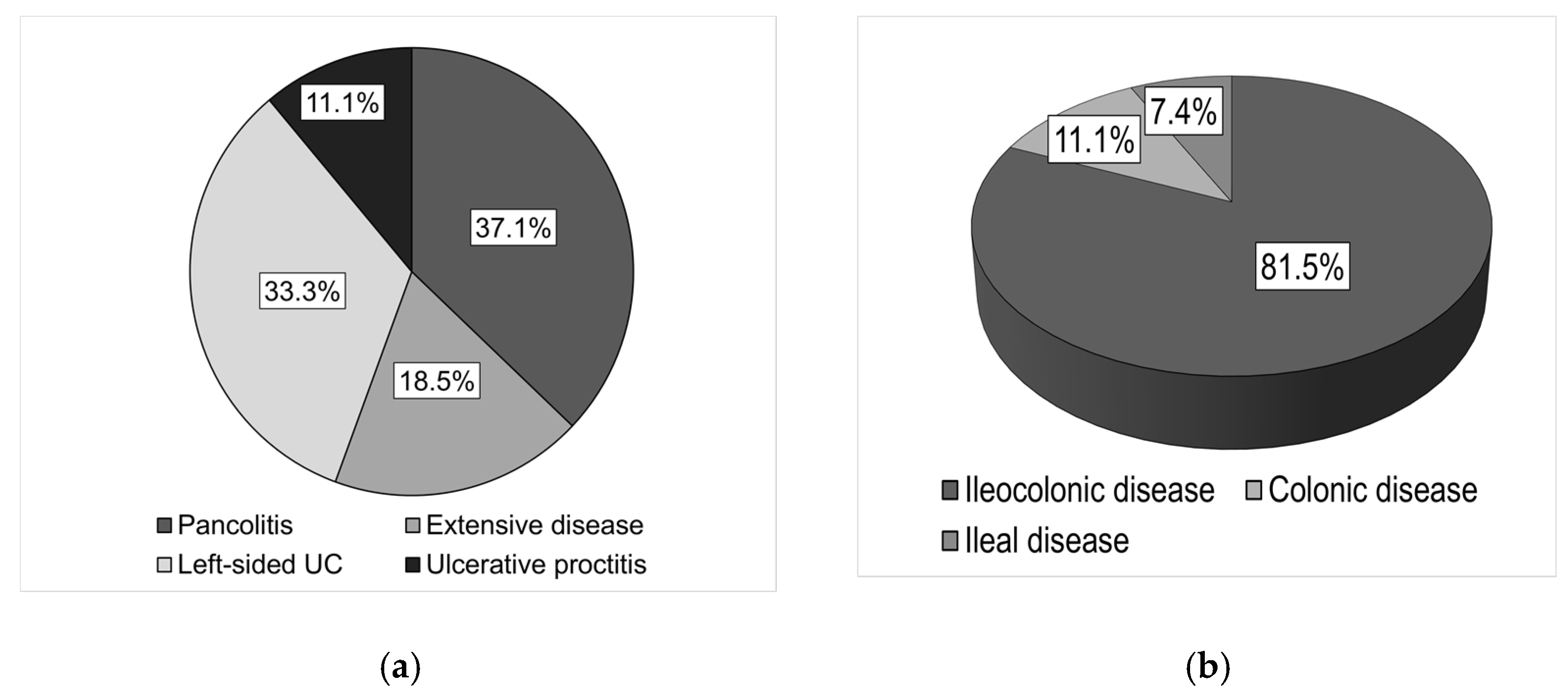
3.3. Association between the Prevalence of Anemia and Disease Extent
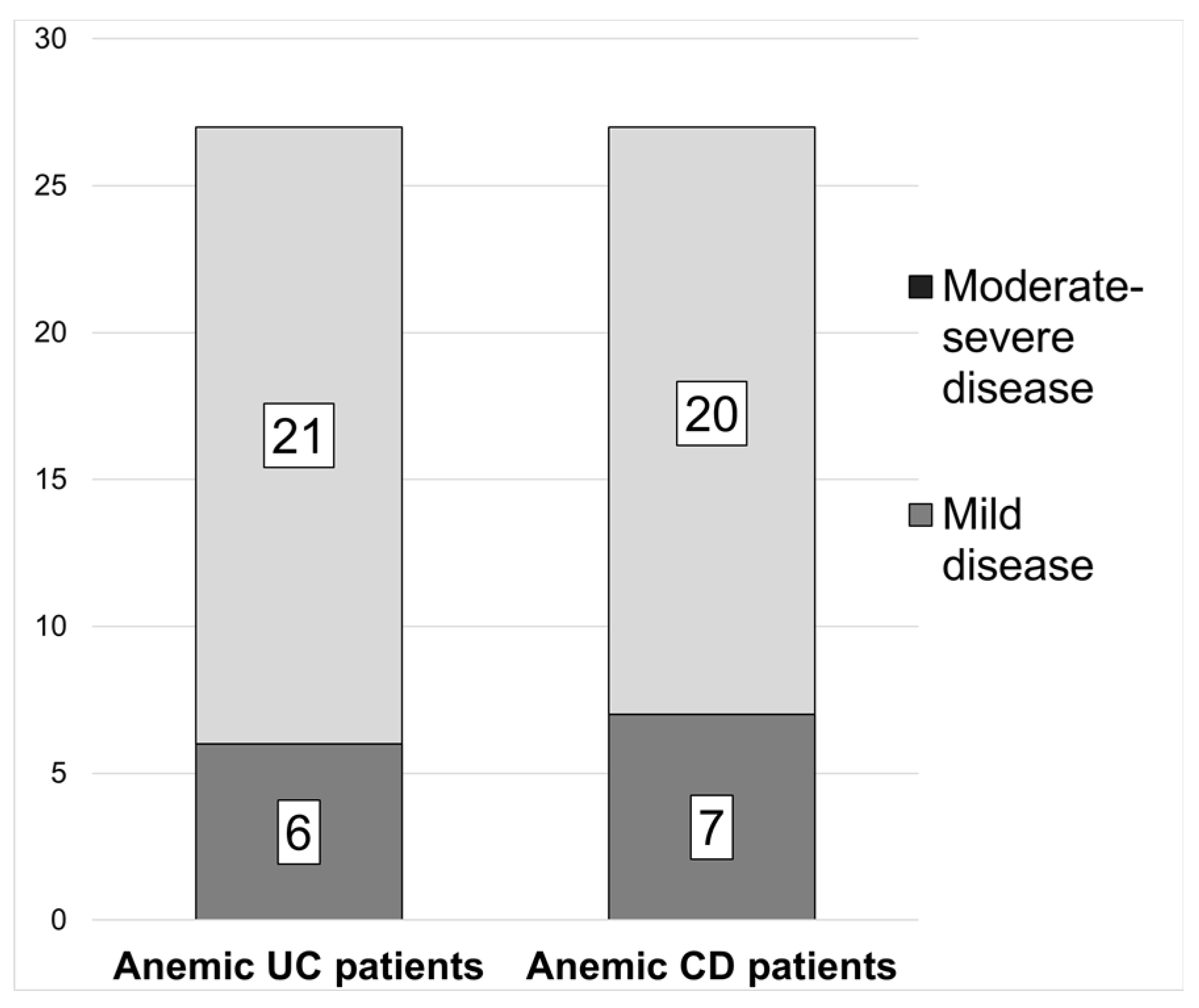
3.4. Association between the Prevalence of Anemia and Disease Severity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Gasche, C. Anemia in IBD: The overlooked villain. Inflamm. Bowel Dis. 2000, 6, 142–150. [Google Scholar] [CrossRef] [PubMed]
- Kulnigg, S.; Gasche, C. Systematic review: Managing anaemia in Crohn’s disease. Aliment. Pharmacol. Ther. 2006, 24, 1507–1523. [Google Scholar] [CrossRef]
- Gisbert, J.P.; Gomollón, F. Common misconceptions in the diagnosis and management of anemia in inflammatory bowel disease. Am. J. Gastroenterol. 2008, 103, 1299–1307. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, O.H.; Ainsworth, M.; Coskun, M.; Weiss, G. Management of Iron-Deficiency Anemia in Inflammatory Bowel Disease: A Systematic Review. Medicine 2015, 94, e963. [Google Scholar] [CrossRef]
- Guagnozzi, D.; Lucendo, A.J. Anemia in inflammatory bowel disease: A neglected issue with relevant effects. World J. Gastroenterol. 2014, 20, 3542–3551. [Google Scholar] [CrossRef] [PubMed]
- Dignass, A.U.; Gasche, C.; Bettenworth, D.; Birgegård, G.; Danese, S.; Gisbert, J.P.; Gomollon, F.; Iqbal, T.; Katsanos, K.; Koutroubakis, I.; et al. European Crohn’s and Colitis Organisation [ECCO]. European consensus on the diagnosis and management of iron deficiency and anaemia in inflammatory bowel diseases. J. Crohns Colitis 2015, 9, 211–222. [Google Scholar] [CrossRef]
- Goyal, A.; Zheng, Y.; Albenberg, L.G.; Stoner, N.L.; Hart, L.; Alkhouri, R.; Hampson, K.; Ali, S.; Cho-Dorado, M.; Goyal, R.K.; et al. Anemia in Children With Inflammatory Bowel Disease: A Position Paper by the IBD Committee of the North American Society of Pediatric Gastroenterology, Hepatology and Nutrition. J. Pediatr. Gastroenterol. Nutr. 2020, 71, 563–582. [Google Scholar] [CrossRef] [PubMed]
- Ferrante, M.; Penninckx, F.; De Hertogh, G.; Geboes, K.; D’Hoore, A.; Noman, M.; Vermeire, S.; Rutgeerts, P.; Van Assche, G. Protein-losing enteropathy in Crohn’s disease. Acta Gastroenterol. Belg. 2006, 69, 384–389. [Google Scholar] [CrossRef]
- Levine, A.; Koletzko, S.; Turner, D.; Escher, J.C.; Cucchiara, S.; de Ridder, L.; Kolho, K.L.; Veres, G.; Russell, R.K.; Paerregaard, A.; et al. European Society of Pediatric Gastroenterology, Hepatology, and Nutrition. ESPGHAN revised Porto criteria for the diagnosis of inflammatory bowel disease in children and adolescents. J. Pediatr. Gastroenterol. Nutr. 2014, 58, 795–806. [Google Scholar] [CrossRef] [Green Version]
- Levine, A.; Griffiths, A.; Markowitz, J.; Wilson, D.C.; Turner, D.; Russell, R.K.; Fell, J.; Ruemmele, F.M.; Walters, T.; Sherlock, M.; et al. Pediatric modification of the Montreal classification for inflammatory bowel disease: The Paris classification. Inflamm. Bowel Dis. 2011, 17, 1314–1321. [Google Scholar] [CrossRef]
- Turner, D.; Otley, A.R.; Mack, D.; Hyams, J.; de Bruijne, J.; Uusoue, K.; Walters, T.D.; Zachos, M.; Mamula, P.; Beaton, D.E.; et al. Development, validation, and evaluation of a pediatric ulcerative colitis activity index: A prospective multicenter study. Gastroenterology 2007, 133, 423–432. [Google Scholar] [CrossRef]
- Hyams, J.S.; Ferry, G.D.; Mandel, F.S.; Gryboski, J.D.; Kibort, P.M.; Kirschner, B.S.; Griffiths, A.M.; Katz, A.J.; Grand, R.J.; Boyle, J.T.; et al. Development and validation of a pediatric Crohn’s disease activity index. J. Pediatr. Gastroenterol. Nutr. 1991, 12, 439–447. [Google Scholar] [CrossRef]
- Danko, I.; Weidkamp, M. Correction of Iron Deficiency Anemia With Intravenous Iron Sucrose in Children With Inflammatory Bowel Disease. J. Pediatr. Gastroenterol. Nutr. 2016, 63, e107–e111. [Google Scholar] [CrossRef]
- Lopes, A.; Azevedo, S. Anemia and IBD: Current Status and Future Prospectives. In Current Topics in Anaemia, 1st ed.; Khan, J., Ed.; IntechOpen Limited: London, UK, 2018. [Google Scholar] [CrossRef]
- Goodhand, J.R.; Kamperidis, N.; Rao, A.; Laskaratos, F.; McDermott, A.; Wahed, M.; Naik, S.; Croft, N.M.; Lindsay, J.O.; Sanderson, I.R.; et al. Prevalence and management of anemia in children, adolescents, and adults with inflammatory bowel disease. Inflamm. Bowel Dis. 2012, 18, 513–519. [Google Scholar] [CrossRef]
- Aljomah, G.; Baker, S.S.; Schmidt, K.; Alkhouri, R.; Kozielski, R.; Zhu, L.; Baker, R.D. Anemia in Pediatric Inflammatory Bowel Disease. J. Pediatr. Gastroenterol. Nutr. 2018, 67, 351–355. [Google Scholar] [CrossRef]
- Wiskin, A.E.; Fleming, B.J.; Wootton, S.A.; Beattie, R.M. Anaemia and iron deficiency in children with inflammatory bowel disease. J. Crohns Colitis 2012, 6, 687–691. [Google Scholar] [CrossRef] [Green Version]
- Pels, L.P.; Van de Vijver, E.; Waalkens, H.J.; Uitentuis, J.; Gonera-de Jong, G.; van Overbeek, L.A.; Norbruis, O.F.; Rings, E.H.; van Rheenen, P.F. Slow hematological recovery in children with IBD-associated anemia in cases of “expectant management”. J. Pediatr. Gastroenterol. Nutr. 2010, 51, 708–713. [Google Scholar] [CrossRef]
- Sjöberg, D.; Holmström, T.; Larsson, M.; Nielsen, A.L.; Holmquist, L.; Rönnblom, A. Anemia in a population-based IBD cohort (ICURE): Still high prevalence after 1 year, especially among pediatric patients. Inflamm. Bowel Dis. 2014, 20, 2266–2270. [Google Scholar] [CrossRef]
- de Laffolie, J.; Laass, M.W.; Scholz, D.; Zimmer, K.P.; Buderus, S.; CEDATA-GPGE Study Group. Prevalence of Anemia in Pediatric IBD Patients and Impact on Disease Severity: Results of the Pediatric IBD-Registry CEDATA-GPGE®. Gastroenterol. Res. Pract. 2017, 2017, 8424628. [Google Scholar] [CrossRef] [Green Version]
- Rempel, J.; Grover, K.; El-Matary, W. Micronutrient Deficiencies and Anemia in Children with Inflammatory Bowel Disease. Nutrients 2021, 13, 236. [Google Scholar] [CrossRef]
- Høivik, M.L.; Reinisch, W.; Cvancarova, M.; Moum, B.; IBSEN Study Group. Anaemia in inflammatory bowel disease: A population-based 10-year follow-up. Aliment. Pharmacol. Ther. 2014, 39, 69–76. [Google Scholar] [CrossRef]
- Gerasimidis, K.; Barclay, A.; Papangelou, A.; Missiou, D.; Buchanan, E.; Tracey, C.; Tayler, R.; Russell, R.K.; Edwards, C.A.; McGrogan, P. The epidemiology of anemia in pediatric inflammatory bowel disease: Prevalence and associated factors at diagnosis and follow-up and the impact of exclusive enteral nutrition. Inflamm. Bowel Dis. 2013, 19, 2411–2422. [Google Scholar] [CrossRef]
- Parra, R.S.; Feitosa, M.R.; Ferreira, S.D.C.; Rocha, J.J.R.D.; Troncon, L.E.A.; FÉres, O. Anemia and iron deficiency in inflammatory bowel disease patients in a referral center in brazil: Prevalence and risk factors. Arq. Gastroenterol. 2020, 57, 272–277. [Google Scholar] [CrossRef]
- Revel-Vilk, S.; Tamary, H.; Broide, E.; Zoldan, M.; Dinari, G.; Zahavi, I.; Yaniv, I.; Shamir, R. Serum transferrin receptor in children and adolescents with inflammatory bowel disease. Eur. J. Pediatr. 2000, 159, 585–589. [Google Scholar] [CrossRef]
| Age | Healthy Hb, g/L | Mild Anemia Hb, g/L | Moderate Anemia Hb, g/L | Severe Anemia Hb, g/L |
|---|---|---|---|---|
| 6–59 months | ≥110 | 100–109 | 70–99 | <70 |
| 5–11 years | ≥115 | 110–114 | 80–109 | <80 |
| 12–14 years | ≥120 | 110–119 | 80–109 | <80 |
| Non-pregnant females (≥15 years) | ≥120 | 110–119 | 80–109 | <80 |
| Pregnant females | ≥110 | 100–109 | 70–99 | <70 |
| Males (≥15 years) | ≥130 | 110–129 | 80–109 | <80 |
| All n = 80 | Crohn’s Disease n = 35 | Ulcerative Colitis n = 45 |
|---|---|---|
| Gender, n (%) | ||
| Male | 19 (23.75) | 23 (28.75) |
| Female | 16 (20.0) | 22 (27.5) |
| Age at diagnosis, median (range) | 15 years | 15 years |
| (7–17 years) | (2-17 years) | |
| Disease duration before diagnosis, median (range) | 5 months | 3 months |
| (2 weeks–180 months) | (2 weeks–24 months) | |
| Disease location, n (%) | ||
| Ileal (L1) | 5 (14.3) | |
| Colonic (L2) | 4 (11.4) | |
| Ileocolonic (L3) | 26 (74.3) | |
| Upper disease proximal to ligament of Treitz (L4a) | 14 (40.0) | |
| Upper disease distal to ligament of Treitz (L4b) | 3 (8.6) | |
| Disease behavior, n (%) | ||
| Non-stricturing, non-penetrating (B1) | 23 (65.7) | |
| Stricturing (B2) | 6 (17.2) | |
| Penetrating (B3) | 2 (5.7) | |
| Stricturing and penetrating (B2B3) | 4 (11.4) | |
| Perianal disease (p) | 6 (17.2) | |
| Growth, n (%) | ||
| No evidence of growth delay (G0) | 31 (88.6) | |
| Growth delay (G1) | 4 (11.4) | |
| Disease activity at diagnosis, n (%) | ||
| Mild | 9 (25.7) | |
| Moderate to severe | 26 (74.3) | |
| Disease extent, n (%) | ||
| Ulcerative proctitis (E1) | 9 (20.0) | |
| Left-sided UC (E2) | 13 (28.9) | |
| Extensive colitis (E3) | 6 (13.3) | |
| Pancolitis (E4) | 17 (37.8) | |
| Disease severity, n (%) | ||
| Never severe (S0) | 30 (66.7) | |
| Ever severe (S1) | 15 (33.3) | |
| Disease activity at diagnosis, n (%) | ||
| Mild | 11 (24.4) | |
| Moderate | 21 (46.7) | |
| Severe | 13 (28.9) | |
| Anemia at diagnosis, n (%) | ||
| Yes | 27 (77.1) | 27 (60.0) |
| No | 8 (22.9) | 18 (40.0) |
| Prevalence of iron deficiency in anemic patients at diagnosis, n (%) | ||
| Yes | 21 (77.8) | 20 (74.1) |
| No | 6 (22.2) | 7 (25.9) |
| CD Patients | UC Patients | |||
|---|---|---|---|---|
| n = 35 | Hb g/L (±SD) | n = 45 | Hb g/L (±SD) | |
| With anemia, n (%) | 27 (77.1) | 110.3 (±14.6) | 27 (60.0) | 97.4 (±15.7) |
| Mild | 16 (59.3) | 119.2 (±5.8) | 7 (25.9) | 117 (±7.7) |
| Moderate | 10 (37.0) | 100.8 (±8.5) | 18 (66.7) | 93 (±8.7) |
| Severe | 1 (3.7) | 63.0 (NA) | 2 (7.4) | 68.5 (±6.3) |
| Without anemia, n (%) | 8 (22.9) | 133.8 (±7.3) | 18 (40.0) | 135.8 (±15.3) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shentova-Eneva, R.; Kofinova, D.; Hadzhiyski, P.; Yaneva, P.; Lazarova, E.; Baycheva, M. Anemia in Newly Diagnosed Pediatric Patients with Inflammatory Bowel Disease. Gastroenterol. Insights 2021, 12, 376-383. https://doi.org/10.3390/gastroent12040036
Shentova-Eneva R, Kofinova D, Hadzhiyski P, Yaneva P, Lazarova E, Baycheva M. Anemia in Newly Diagnosed Pediatric Patients with Inflammatory Bowel Disease. Gastroenterology Insights. 2021; 12(4):376-383. https://doi.org/10.3390/gastroent12040036
Chicago/Turabian StyleShentova-Eneva, Rayna, Denitza Kofinova, Petyo Hadzhiyski, Penka Yaneva, Elena Lazarova, and Mila Baycheva. 2021. "Anemia in Newly Diagnosed Pediatric Patients with Inflammatory Bowel Disease" Gastroenterology Insights 12, no. 4: 376-383. https://doi.org/10.3390/gastroent12040036
APA StyleShentova-Eneva, R., Kofinova, D., Hadzhiyski, P., Yaneva, P., Lazarova, E., & Baycheva, M. (2021). Anemia in Newly Diagnosed Pediatric Patients with Inflammatory Bowel Disease. Gastroenterology Insights, 12(4), 376-383. https://doi.org/10.3390/gastroent12040036






