Malignant Transformation of Heterotopic Pancreatic Tissue in a Patient with BRCA2 Mutation
Abstract
1. Introduction
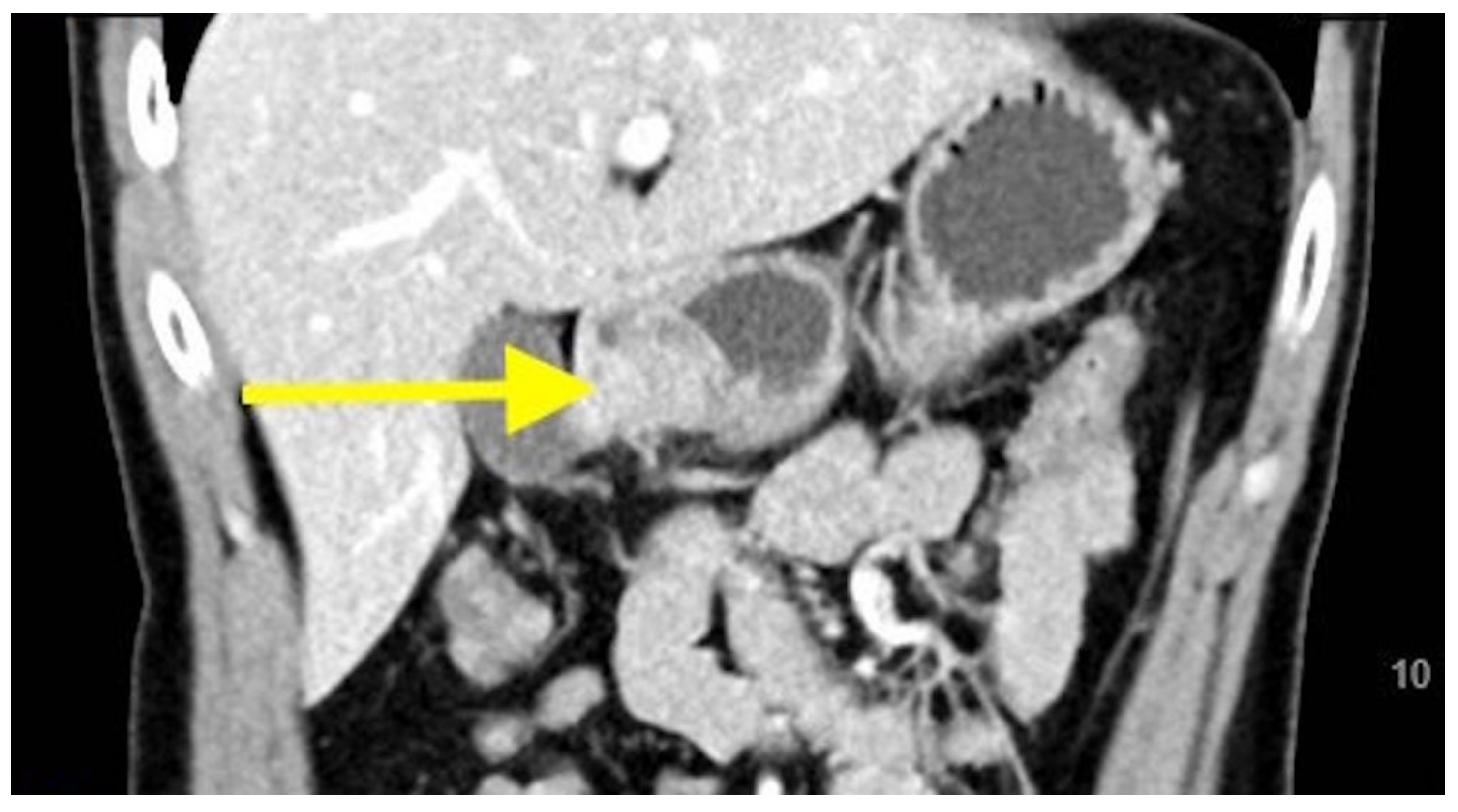
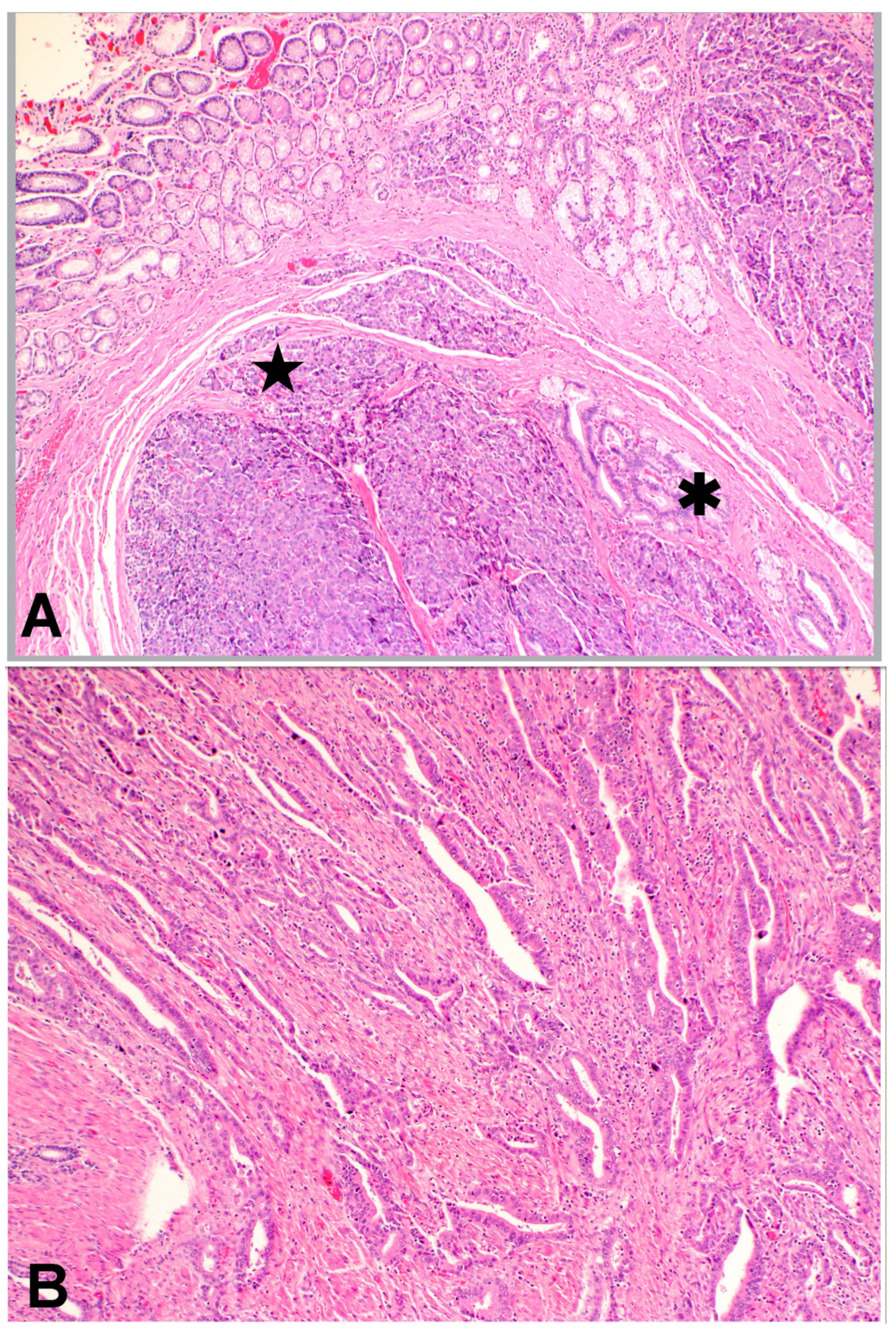
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hunt, V.C. Meckel’s diverticulum containing abberant pancreas. Arch. Surg. 1934, 28, 425–439. [Google Scholar] [CrossRef]
- Goodarzi, M.; Rashid, A.; Maru, D. Invasive ductal adenocarcinoma arising from pancreatic heterotopia in rectum: Case report and review of literature. Hum. Pathol. 2010, 41, 1809–1813. [Google Scholar] [CrossRef] [PubMed]
- Stock, C.; Keutgen, X.M.; Pisapia, D.; Crawford, C.; Zarnegar, R. Heterotopic pancreatic neoplasm presenting as an obstructing mass at the fourth portion of the duodenum. JOP 2011, 12, 241–243. [Google Scholar] [PubMed]
- Ulrych, J.; Fryba, V.; Skalova, H.; Krska, Z.; Krechler, T.; Zogala, D. Premalignant and malignant lesions of the heterotopic pancreas in the esophagus: A case report and review of the literature. J. Gastrointest. Liver Dis. 2015, 24, 235–239. [Google Scholar] [CrossRef] [PubMed]
- Kung, J.W.; Brown, A.; Kruskal, J.B.; Goldsmith, J.D.; Pedrosa, I. Heterotopic pancreas: Typical and atypical imaging findings. Clin. Radiol. 2010, 65, 403–407. [Google Scholar] [CrossRef]
- Song, D.E.; Kwon, Y.; Kim, K.R.; Oh, S.T.; Kim, J.S. Adenocarcinoma arising in gastric heterotopic pancreas: A case report. J. Korean Med. Sci. 2004, 19, 145–148. [Google Scholar] [CrossRef] [PubMed]
- Herold, G.; Kraft, K. Adenocarcinoma arising from ectopic gastric pancreas: Two case reports with a review of the literature. Z. Gastroenterol. 1995, 33, 260–264. [Google Scholar]
- Yamaoka, Y.; Yamaguchi, T.; Kinugasa, Y.; Shiomi, A.; Kagawa, H.; Yamakawa, Y.; Numata, M.; Sugimoto, S.; Imai, K.; Hotta, K.; et al. Adenocarcinoma arising from jejunal ectopic pancreas mimicking peritoneal metastasis from colon cancer: A case report and literature review. Surg. Case Rep. 2015, 1, 114. [Google Scholar] [CrossRef][Green Version]
- Guillou, L.; Nordback, P.; Gerber, C.; Schneider, R.P. Ductal adenocarcinoma arising in a heterotopic pancreas situated in a hiatal hernia. Arch. Pathol. Lab. Med. 1994, 118, 568–571. [Google Scholar]
- Endo, S.; Saito, R.; Ochi, D.; Yamada, T.; Hirose, M.; Hiroshima, Y.; Yamamoto, Y.; Ueno, T.; Hasegawa, N.; Moriwaki, T.; et al. Effectiveness of an endoscopic biopsy procedure using EUS-FNA and EMR-C for diagnosing adenocarcinoma arising from ectopic pancreas: Two case reports and a literature review. Intern. Med. 2014, 53, 1055–1062. [Google Scholar] [CrossRef][Green Version]
- Safi, F.; Schlosser, W.; Falkenreck, S.; Beger, H.G. Prognostic value of CA 19-9 serum course in pancreatic cancer. Hepatogastroenterology 1998, 45, 253–259. [Google Scholar] [PubMed]
- Yasuda, K.; Nakajima, M.; Yoshida, S.; Kiyota, K.; Kawai, K. The diagnosis of submucosal tumors of the stomach by endoscopic ultrasonography. Gastrointest. Endosc. 1989, 35, 10–15. [Google Scholar] [CrossRef]
- Matsushita, M.; Hajiro, K.; Okazaki, K.; Takakuwa, H. Gastric aberrant pancreas: EUS analysis in comparison with the histology. Gastrointest. Endosc. 1999, 49, 493–497. [Google Scholar] [CrossRef]
- Matsuki, M.; Gouda, Y.; Ando, T.; Matsuoka, H.; Morita, T.; Uchida, N.; Kuriyama, S. Adenocarcinoma arising from aberrant pancreas in the stomach. J. Gastroenterol. 2005, 40, 652–656. [Google Scholar] [CrossRef] [PubMed]
- The Breast Cancer Linkage Consortium. Cancer risks in BRCA2 mutation carriers. J. Natl. Cancer Inst. 1999, 91, 1310–1316. [Google Scholar] [CrossRef] [PubMed]
- Iqbal, J.; Ragone, A.; Lubinski, J.; Lynch, H.T.; Moller, P.; Ghadirian, P.; Foulkes, W.D.; Armel, S.; Eisen, A.; Neuhausen, S.L.; et al. The incidence of pancreatic cancer in BRCA1 and BRCA2 mutation carriers. Br. J. Cancer 2012, 107, 2005–2009. [Google Scholar] [CrossRef]
- Goggins, M.; Schutte, M.; Lu, J.; Moskaluk, C.A.; Weinstein, C.L.; Petersen, G.M.; Yeo, C.J.; Jackson, C.E.; Lynch, H.T.; Hruban, R.H.; et al. Germline BRCA2 gene mutations in patients with apparently sporadic pancreatic carcinomas. Cancer Res. 1996, 56, 5360–5364. [Google Scholar] [PubMed]
- Phelan, C.M.; Lancaster, J.M.; Tonin, P.; Gumbs, C.; Cochran, C.; Carter, R.; Ghadirian, P.; Perret, C.; Moslehi, R.; Dion, F.; et al. Mutation analysis of the BRCA2 gene in 49 site-specific breast cancer families. Nat. Genet. 1996, 13, 120–122. [Google Scholar] [CrossRef]
- Couch, F.J.; Johnson, M.R.; Rabe, K.G.; Brune, K.; de Andrade, M.; Goggins, M.; Rothenmund, H.; Gallinger, S.; Klein, A.; Petersen, G.M.; et al. The prevalence of BRCA2 mutations in familial pancreatic cancer. Cancer Epidemiol. Biomark. Prev. 2007, 16, 342–346. [Google Scholar] [CrossRef]
- Jeng, K.S.; Yang, K.C.; Kuo, S.H. Malignant degeneration of heterotopic pancreas. Gastrointest. Endosc. 1991, 37, 196–198. [Google Scholar] [CrossRef]
- Hickman, D.M.; Frey, C.F.; Carson, J.W. Adenocarcinoma arising in gastric heterotopic pancreas. West. J. Med. 1981, 135, 57–62. [Google Scholar] [PubMed]
- Kaneko, T.; Ohara, M.; Okamura, K.; Fujiwara-Kuroda, A.; Miyasaka, D.; Yamabuki, T.; Takahashi, R.; Komuro, K.; Suzuoki, M.; Iwashiro, N.; et al. Adenocarcinoma arising from an ectopic pancreas in the duodenum: A case report. Surg. Case Rep. 2019, 5, 126. [Google Scholar] [CrossRef] [PubMed]
- Fukino, N.; Oida, T.; Mimatsu, K.; Kuboi, Y.; Kida, K. Adenocarcinoma arising from heterotopic pancreas at the third portion of the duodenum. World J. Gastroenterol. 2015, 21, 4082–4088. [Google Scholar] [CrossRef] [PubMed]
- Conroy, T.; Desseigne, F.; Ychou, M.; Bouche, O.; Guimbaud, R.; Becouarn, Y.; Adenis, A.; Raoul, J.L.; Gourgou-Bourgade, S.; de la Fouchardiere, C.; et al. FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. N. Engl. J. Med. 2011, 364, 1817–1825. [Google Scholar] [CrossRef] [PubMed]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yeo, D.X.W.; Goh, N.; Chuah, K.L.; Amitbhai, S.K.; Oo, A.M.; Ahmed, A.K.S.; Nath, K.A. Malignant Transformation of Heterotopic Pancreatic Tissue in a Patient with BRCA2 Mutation. Gastroenterol. Insights 2021, 12, 10-16. https://doi.org/10.3390/gastroent12010002
Yeo DXW, Goh N, Chuah KL, Amitbhai SK, Oo AM, Ahmed AKS, Nath KA. Malignant Transformation of Heterotopic Pancreatic Tissue in a Patient with BRCA2 Mutation. Gastroenterology Insights. 2021; 12(1):10-16. https://doi.org/10.3390/gastroent12010002
Chicago/Turabian StyleYeo, Danson Xue Wei, Nicholette Goh, Khoon Leong Chuah, Sanghvi Kaushal Amitbhai, Aung Myint Oo, Abdul Kareem Saleem Ahmed, and Koura Aaryan Nath. 2021. "Malignant Transformation of Heterotopic Pancreatic Tissue in a Patient with BRCA2 Mutation" Gastroenterology Insights 12, no. 1: 10-16. https://doi.org/10.3390/gastroent12010002
APA StyleYeo, D. X. W., Goh, N., Chuah, K. L., Amitbhai, S. K., Oo, A. M., Ahmed, A. K. S., & Nath, K. A. (2021). Malignant Transformation of Heterotopic Pancreatic Tissue in a Patient with BRCA2 Mutation. Gastroenterology Insights, 12(1), 10-16. https://doi.org/10.3390/gastroent12010002



