Extra-Axial Cavernous Angioma: A Case Report and Review of the Literature
Abstract
1. Introduction
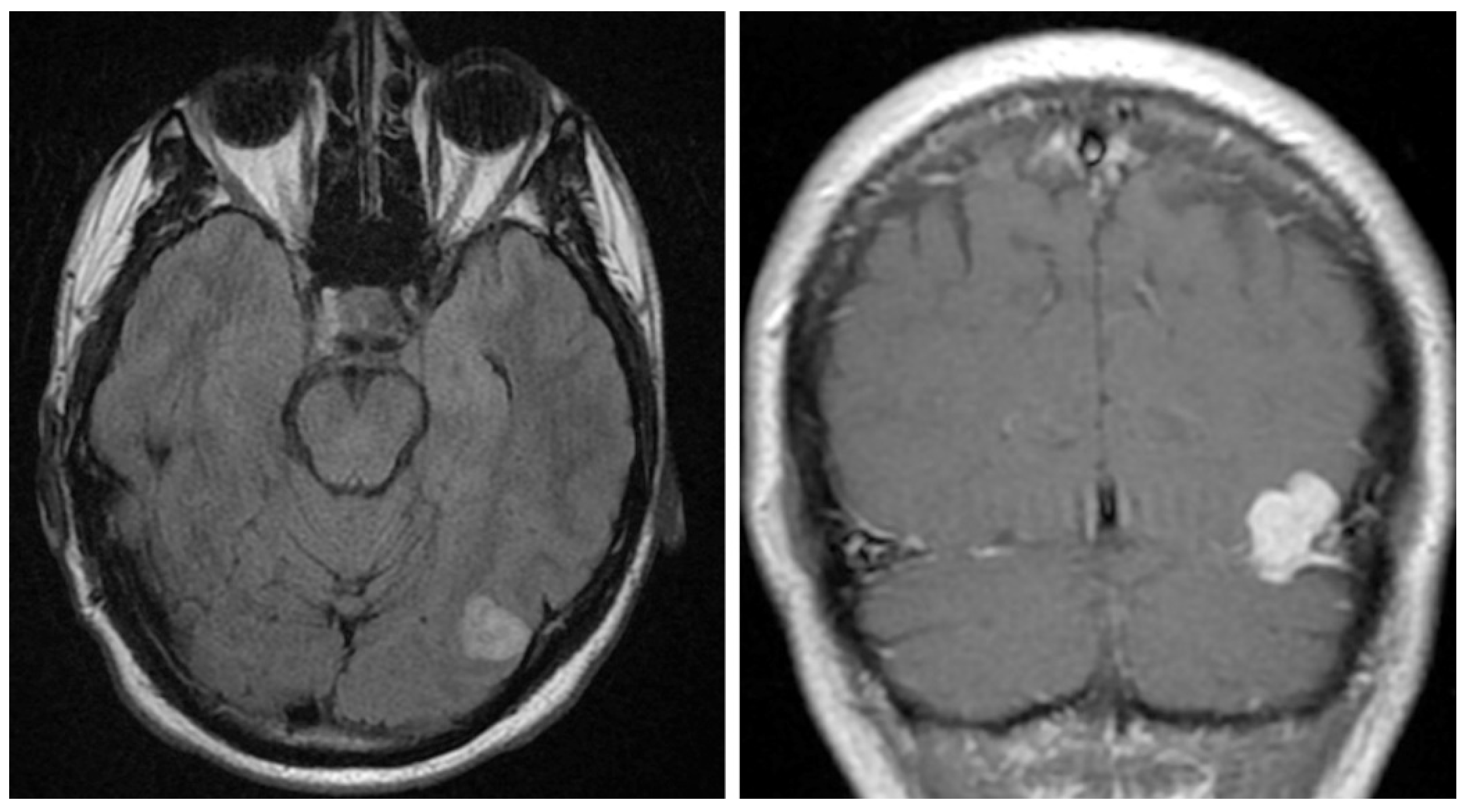
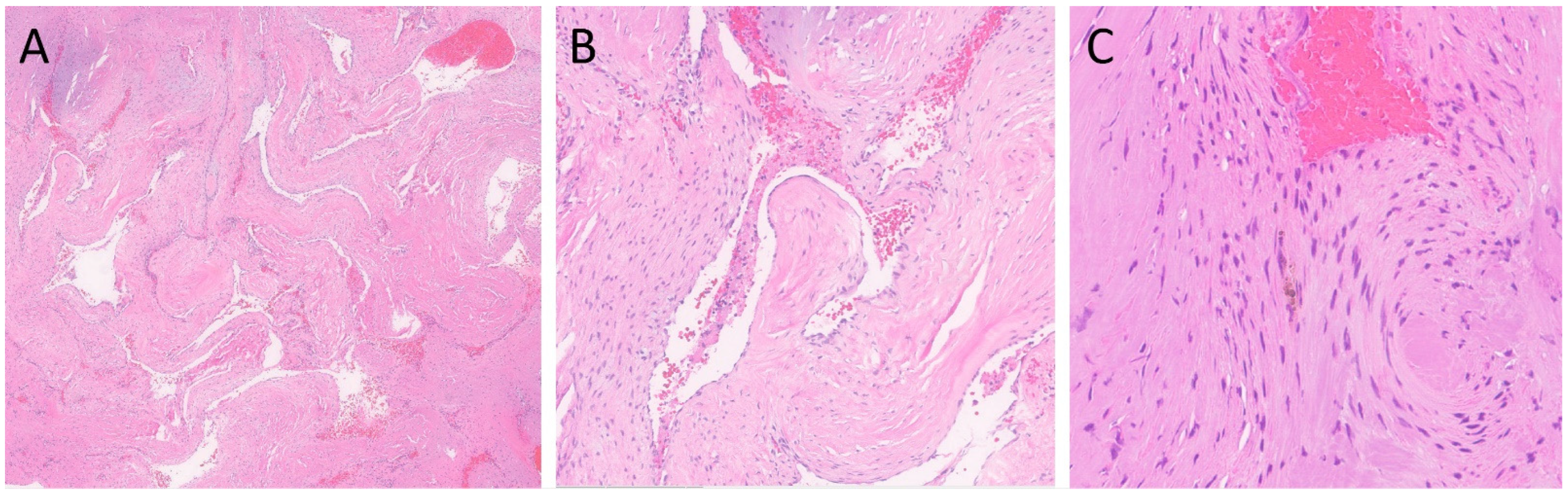
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Uzunoglu, I.; Guvenc, G.; Kizmazoglu, C.; Aydin, H.E.; Kaya, I.; Rezanko, T.A.; Yuceer, N. Cavernous Angioma Mimicking Meningioma. J. Craniofac. Surg. 2019, 30, e218–e220. [Google Scholar] [CrossRef]
- Oommen, A.; Pratap, T.; Chandi, S.; Jalal, M.J.A. Parasellar extra-axial cavernoma mimicking meningioma: A case report. Neuroimmunol. Neuroinflamm. 2017, 4, 16–19. [Google Scholar] [CrossRef]
- Biondi, A.; Clemenceau, S.; Dormont, D.; Deladoeuille, M.; Ricciardi, G.K.; Mokhtari, K.; Sichez, J.P.; Marsault, C. Intracranial extra-axial cavernous (HEM) angiomas: Tumors or vascular malformations? J. Neuroradiol. 2002, 29, 91–104. [Google Scholar]
- Luschka, H. Cavernöse Blutgeschwuelste des Gehirns. Arch. Path. Arch. Path Anat. 1853, 6, 458. [Google Scholar] [CrossRef]
- Vogler, R.; Castillo, M. Dural cavernous angioma: MR features. AJNR Am. J. Neuroradiol. 1995, 16, 773–775. [Google Scholar] [PubMed]
- Simonin, A.; Passaplan, C.; Sancho, S.; Rusconi, A.; Otten, P. Giant Extra-Axial Cavernous Angioma of the Falx: Case Report. Neurosurgery 2019, 84, E211–E214. [Google Scholar] [CrossRef] [PubMed]
- Kashlan, O.N.; Sack, J.A.; Ramnath, S. Cavernous Angioma of the Dural Convexity Mimicking a Meningioma. Austin Neurosurg. Open Access 2014, 1, 1019. [Google Scholar]
- Mori, H.; Koike, T.; Endo, S.; Takii, Y.; Uzuka, T.; Takahashi, H.; Ito, J.; Tanaka, R. Tentorial cavernous angioma with profuse bleeding. Case report. J. Neurosurg. Pediatr. 2009, 3, 37–40. [Google Scholar] [CrossRef]
- Robinson, J.R.; Awad, I.A.; Little, J.R. Natural history of the cavernous angioma. J. Neurosurg. 1991, 75, 709–714. [Google Scholar] [CrossRef]
- Bancroft, J.D.; Stevens, A. Theory and Practice of Histological Techniques, 3rd ed.; Churchill Livingstone: Edinburgh, Scotland; New York, NY, USA, 2008. [Google Scholar]
- Namba, S. Extracerebral cavernous hemangioma of the middle cranial fossa. Surg. Neurol. 1983, 19, 379–388. [Google Scholar] [CrossRef]
- Saldaña, C.J.; Zimman, H.; Alonso, P.; Mata, P.R. Neonatal cavernous hemangioma of the dura mater: Case report. Neurosurgery 1991, 29, 602–605. [Google Scholar] [CrossRef]
- Canevini, P.; Farneti, A.; Flauto, U. Report of a Case of Cavernous Hemangioma of the Dura Mater in a 2-Day Old Newborn. Folia Hered. Pathol. 1963, 12, 163–166. [Google Scholar]
- Moritake, K.; Handa, H.; Nozaki, K.; Tomiwa, K. Tentorial cavernous angioma with calcification in a neonate. Neurosurgery 1985, 16, 207–211. [Google Scholar] [CrossRef]
- Gross, B.A.; Lin, N.; Du, R.; Day, A.L. The natural history of intracranial cavernous malformations. Neurosurg. Focus 2011, 30, E24. [Google Scholar] [CrossRef]
- Lewis, A.I.; Tew, J.M.; Jr Payner, T.D.; Yeh, H.S. Dural cavernous angiomas outside the middle cranial fossa: A report of two cases. Neurosurgery 1994, 35, 498–504. [Google Scholar] [CrossRef]
- Tarabay, A.; Rocca, A.; Maeder, P.; Simonin, A.; Messerer, M.; Daniel, R.T. Extra-Axial Cavernoma of the Cerebellopontine Angle: A Case Study and Review of Literature. World Neurosurg. 2019, 128, 415–421. [Google Scholar] [CrossRef] [PubMed]
- Tsutsumi, S.; Yasumoto, Y.; Saeki, H.; Ito, M. Cranial dural cavernous angioma. Clin. Neuroradiol. 2014, 24, 155–159. [Google Scholar] [CrossRef] [PubMed]
- Sasani, M.; Bayhan, M.; Cakiroglu, G.; Ozer, A.F. Extra Axial Cavernous Hemangioma of the Cerebellopontine Angle With Intratumor Hemorrhage: Case Report and Review. Neurosurg. Q. 2010, 20, 23–26. [Google Scholar] [CrossRef]
- Kunishio, K.; Sunami, N.; Yamamoto, Y.; Satoh, T.; Asari, S.; Ohtsuki, Y. A case of convexity cavernous hemangioma associated with meningioma. No Shinkei Geka 1986, 14, 1487–1491. [Google Scholar]
- Quattrocchi, K.B.; Kissel, P.; Ellis, W.G.; Frank, E.H. Cavernous angioma of the tentorium cerebelli. Case Rep. J. Neurosurg. 1989, 71, 935–937. [Google Scholar] [CrossRef]
- Hwang, S.W.; Pfannl, R.M.; Wu, J.K. Convexity dural cavernous malformation with intradural and extradural extension mimicking a meningioma: A case report. Acta Neurochir. 2009, 151, 79–83. [Google Scholar] [CrossRef]
- Riant, F.; Bergametti, F.; Ayrignac, X.; Boulday, G.; Tournier-Lasserve, E. Recent insights into cerebral cavernous malformations: The molecular genetics of CCM. FEBS J. 2010, 277, 1070–1075. [Google Scholar] [CrossRef] [PubMed]
- Bhatia, S.; O’Neill, B.R.; Pu, F.; Aziz, K. Giant tentorial cavernous hemangioma: Case report and review of literature. Clin. Neurol. Neurosurg. 2011, 113, 937–942. [Google Scholar] [CrossRef] [PubMed]
- van Lindert, E.J.; Tan, T.C.; Grotenhuis, J.A.; Wesseling, P. Giant cavernous hemangiomas: Report of three cases. Neurosurg. Rev. 2007, 30, 83–92. [Google Scholar] [CrossRef]
- Yamada, S.; Nakase, H.; Nakagawa, I.; Nishimura, F.; Motoyama, Y.; Park, Y.S. Cavernous malformations in pregnancy. Neurol. Med. Chir. 2013, 53, 555–560. [Google Scholar] [CrossRef]
- Haber, J.S.; Kesavabhotla, K.; Ottenhausen, M.; Bodhinayake, I.; Dinkin, M.J.; Segal, A.Z.; Lee, Y.M.; Boockvar, J.A. Conservative management of cavernous sinus cavernous hemangioma in pregnancy. J. Neurosurg. 2014, 120, 1309–1312. [Google Scholar] [CrossRef]
- Ishii, K.; Tanei, T.; Kato, T.; Naito, T.; Tsukamoto, E.; Okada, K.; Hasegawa, T. Dural-based Cavernous Malformation at the Temporal Convexity Presenting with Hemorrhage in a Pregnant Woman: Case Report. NMC Case Rep. J. 2021, 8, 69–73. [Google Scholar] [CrossRef] [PubMed]
- Weigel, J.; Neher, M.; Schrey, M.; Wünsch, P.H.; Steiner, H.H. Collision Tumor Composed of Meningioma and Cavernoma. J. Korean Neurosurg. Soc. 2017, 60, 102–107. [Google Scholar] [CrossRef]
- Kilani, M.; Darmoul, M.; Hammedi, F.; Ben Nsir, A.; Hattab, M.N. Cavernous hemangioma of the skull and meningioma: Association or coincidence? Case Rep. Neurol. Med. 2015, 2015, 716837. [Google Scholar] [CrossRef]
- Dubovoy, A.V.; Jafarov, V.M.; Voronina, E.I. Supratentorial dural-based collision of cavernoma and meningioma: A case report. Chin. Neurosurg. J. 2018, 4, 17. [Google Scholar] [CrossRef]
- Bteich, F.; Kassab, C.; El Hage, G.; Moussa, R.; Abadjian, G.A.; Bou-Nassif, R. Atypical Presentation of Parietal Convexity Dural-Based Cavernous Hemangioma: A Case Report and Review of Literature. World Neurosurg. 2019, 128, 403–407. [Google Scholar] [CrossRef] [PubMed]
- Simard, J.M.; Garcia-Bengochea, F.; Ballinger, W.E., Jr.; Mickle, J.P.; Quisling, R.G. Cavernous angioma: A review of 126 collected and 12 new clinical cases. Neurosurgery 1986, 18, 162–172. [Google Scholar] [CrossRef] [PubMed]
- Dörner, L.; Buhl, R.; Hugo, H.H.; Jansen, O.; Barth, H.; Mehdorn, H.M. Unusual locations for cavernous hemangiomas: Report of two cases and review of the literature. Acta Neurochir. 2005, 147, 1091–1096. [Google Scholar] [CrossRef] [PubMed]
- Del Curling, O., Jr.; Kelly, D.L., Jr.; Elster, A.D.; Craven, T.E. An analysis of the natural history of cavernous angiomas. J. Neurosurg. 1991, 75, 702–708. [Google Scholar] [CrossRef]
- Li, G.; Zhai, X.; Zhang, Y.; Liang, P.; Wu, X.; Hou, K. Dural-Based Cavernous Malformation at the Cerebral Convexity: Report of Two Pediatric Patients. World Neurosurg. 2018, 112, 81–85. [Google Scholar] [CrossRef]
- Suzuki, K.; Kamezaki, T.; Tsuboi, K.; Kobayashi, E. Dural cavernous angioma causing acute subdural hemorrhage--case report. Neurol. Med. Chir. 1996, 36, 580–582. [Google Scholar] [CrossRef] [PubMed]
- Jadik, S.; Stan, A.C.; Dietrich, U.; Pietilä, T.A.; Elsharkawy, A.E. Intraparenchymal meningioma mimicking cavernous malformation: A case report and review of the literature. J. Med. Case Rep. 2014, 8, 467. [Google Scholar] [CrossRef]
- Puca, A.; Colosimo, C.; Tirpakova, B.; Lauriola, L.; Di Rocco, F. Cavernous hemangioma extending to extracranial, intracranial, and orbital regions. Case report. J. Neurosurg. 2004, 101, 1057–1060. [Google Scholar] [CrossRef]
- Ghanta, R.K.; Tangella, P.; Koti, K.; Dandamudi, S. A rare case of an extra-axial cavernous angioma in the cerebellopontine angle. J. Neurosci. Rural. Pract. 2013, 4, 210–212. [Google Scholar]
- Shen, W.C.; Chenn, C.A.; Hsue, C.T.; Lin, T.Y. Dural cavernous angioma mimicking a meningioma and causing facial pain. J. Neuroimaging 2000, 10, 183–185. [Google Scholar] [CrossRef]
- Melone, A.G.; Delfinis, C.P.; Passacantilli, E.; Lenzi, J.; Santoro, A. Intracranial extra-axial cavernous angioma of the cerebellar falx. World Neurosurg. 2010, 74, 501–504. [Google Scholar] [CrossRef]
- Revuelta, R.; Teixeira, F.; Rojas, R.; Juambelz, P.; Romero, V.; Valdes, J. Cavernous hemangiomas of the dura mater at the convexity. Report of a case and therapeutical considerations. Neurosurg. Rev. 1994, 17, 309–311. [Google Scholar] [CrossRef] [PubMed]
- Zabramski, J.M.; Wascher, T.M.; Spetzler, R.F.; Johnson, B.; Golfinos, J.; Drayer, B.P.; Brown, B.; Rigamonti, D.; Brown, G. The natural history of familial cavernous malformations: Results of an ongoing study. J. Neurosurg. 1994, 80, 422–432. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Liu, J.P.; You, C.; Mao, Q. Convexity dural cavernous haemangioma mimicking meningioma: A case report. Br. J. Neurosurg. 2016, 30, 345–347. [Google Scholar] [CrossRef]
- Eisenberg, M.B.; Al-Mefty, O.; DeMonte, F.; Burson, G.T. Benign nonmeningeal tumors of the cavernous sinus. Neurosurgery 1999, 44, 949–954. [Google Scholar] [CrossRef]
- Zhu, W.-Z.; Qi, J.-P.; Zhan, C.-J.; Shu, H.-G.; Zhang, L.; Wang, C.-Y.; Xia, L.-M.; Hu, J.-W.; Feng, D.-Y. Magnetic resonance susceptibility weighted imaging in detecting intracranial calcification and hemorrhage. Chin. Med. J. 2008, 121, 2021–2025. [Google Scholar] [CrossRef]
- Yonezawa, U.; Ikawa, F.; Hamasaki, O.; Hidaka, T.; Kurokawa, Y.; Onuma, H. A case of cavernous angioma at the convexity in the dura mater: Characteristics of images in the literature. No. Shinkei. Geka 2014, 42, 731–735. [Google Scholar]
- Kim, J.-S.; Yang, S.-H.; Kim, M.-K.; Hong, Y.-K. Cavernous Angioma in the Falx Cerebri: A Case Report. JKMS 2006, 21, 950–953. [Google Scholar] [CrossRef]
- Seo, Y.; Fukuoka, S.; Sasaki, T.; Takanashi, M.; Hojo, A.; Nakamura, H. Cavernous sinus hemangioma treated with gamma knife radiosurgery: Usefulness of SPECT for diagnosis—Case report. Neurol. Med. Chir. 2000, 40, 575–580. [Google Scholar] [CrossRef]
- Turan, A.; Unlu, H.A.; Yigit, H.; Yilmaz, O.; Yakut, Z.I. Intrasellar Cavernous Hemangioma: MRI Findings of a Very Rare Lesion. J. Med. Cases 2013, 4, 719–721. [Google Scholar] [CrossRef]
- Rigamonti, D.; Pappas, C.T.; Spetzler, R.F.; Johnson, P.C. Extracerebral cavernous angiomas of the middle fossa. Neurosurgery 1990, 27, 306–310. [Google Scholar] [CrossRef]
- Shi, J.; Hang, C.; Pan, Y.; Liu, C.; Zhang, Z. Cavernous hemangiomas in the cavernous sinus. Neurosurgery. 1999, 45, 1308–1313. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Li, P.; Zhang, X.J.; Xu, Y.Y.; Wang, W. Gamma Knife Surgery for Cavernous Sinus Hemanginoma: A Report of 32 Cases. World Neurosurg. 2016, 94, 18–25. [Google Scholar] [CrossRef]
- Chuang, C.C.; Jung, S.M.; Yang, J.T.; Chang, C.N.; Pai, P.C. Intrasellar cavernous hemangioma. J. Clin. Neurosci. 2006, 13, 672–675. [Google Scholar] [CrossRef] [PubMed]
- Meyer, F.B.; Lombardi, D.; Scheithauer, B.; Nichols, D.A. Extra-axial cavernous hemangiomas involving the dural sinuses. J. Neurosurg. 1990, 73, 187–192. [Google Scholar] [CrossRef]
- Kamrin, R.B.; Buchsbaum, H.W. Large vascular malformations of the brain not visualized by serial angiography. Arch. Neurol. 1965, 13, 413–420. [Google Scholar] [CrossRef] [PubMed]
- Sansone, M.E.; Liwnicz, B.H.; Mandybur, T.I. Giant pituitary cavernous hemangioma: Case report. J. Neurosurg. 1980, 53, 124–126. [Google Scholar] [CrossRef]
- Buonaguidi, R.; Canapicci, R.; Mimassi, N.; Ferdeghini, M. Intrasellar cavernous hemangioma. Neurosurgery 1984, 14, 732–734. [Google Scholar] [CrossRef] [PubMed]
- Sawamura, Y.; de Tribolet, N. Cavernous hemangioma in the cavernous sinus: Case report. Neurosurgery 1990, 26, 126–128. [Google Scholar] [CrossRef]
- Mitsuhashi, T.; Hashimoto, R.; Nagahama, S.; Nagata, Y. Intrasellar cavernous angioma in neurofibromatosis. Hum. Pathol. 1991, 22, 623–624. [Google Scholar] [CrossRef]
- Chhang, W.H.; Khosla, V.K.; Radotra, B.D.; Kak, V.K. Large cavernous haemangioma of the pituitary fossa: A case report. Br. J. Neurosurg. 1991, 5, 627–629. [Google Scholar] [CrossRef]
- Lombardi, D.; Giovanelli, M.; de Tribolet, N. Sellar and parasellar extra-axial cavernous hemangiomas. Acta Neurochir. 1994, 130, 47–54. [Google Scholar] [CrossRef]
- Cobbs, C.S.; Wilson, C.B. Intrasellar cavernous hemangioma. Case report. J. Neurosurg. 2001, 94, 520–522. [Google Scholar] [CrossRef]
- Jeon, S.C.; Yi, J.S.; Yang, J.H.; Lee, I.W. Intrasellar Cavernous Hemangioma. J. Korean Neurosurg. Soc. 2004, 36, 163–165. [Google Scholar]
- Ma, L.C.; Li, W.Y.; Chen, W.Q.; Wu, Y.K. Intrasellar cavernous hemangioma. Neurol. India 2014, 62, 95–96. [Google Scholar] [CrossRef]
- Wu, X.; Yu, H.; Zhao, G.; Wang, L.; Liu, Y.; Li, Y. Intrasellar Cavernous Hemangioma: A Case Report and Literature Review. Transl. Neurosci. Clin. 2017, 3, 111–115. [Google Scholar] [CrossRef]
- Das, S.; Ang, L.C.; Ramsay, D. Intrasellar cavernous hemangioma presenting as pituitary adenoma: A report of two cases and review of the literature. Clin. Neuropathol. 2018, 37, 64–67. [Google Scholar] [CrossRef]
- Al-Sharydah, A.; Al-Suhibani, S.; Al-Jubran, S.; Al-Abdulwahhab, A.; Al-Bar, M.; Al-Jehani, H.; Al-Issawi, W. Endoscopic management of Atypical sellar cavernous hemangioma: A case report and review of the literature. Int. J. Surg. Case Rep. 2018, 42, 161–164. [Google Scholar] [CrossRef]
- Chibbaro, S.; Cebula, H.; Ganau, M.; Gubian, A.; Todeschi, J.; Lhermitte, B.; Proust, F.; Noel, G. Multidisciplinary management of an intra-sellar cavernous hemangioma: Case report and review of the literature. J. Clin. Neurosci. 2018, 52, 135–138. [Google Scholar] [CrossRef]
- Pan, X.; Shen, J.; Ma, Y.; Lou, H.; Weng, Y.; Zhan, R. Imaging characteristics of Intrasellar cavernous hemangioma: A case report. Medicine 2020, 99, e23405. [Google Scholar] [CrossRef]
- Al-Saiari, S.; Al-Orabi, K.; Farag, A.; Brinji, Z.; Azzouz, A.; Mohammed, T.; Mushtaq, D.; Hamouda, W. Intrasellar cavernous hemangiomas: A case report with a comprehensive review of the literature. Surg. Neurol. Int. 2021, 12, 58. [Google Scholar] [CrossRef]
- Okada, J.; Hara, M.; Takeuchi, K. Dural haemangioma with extracranial component. Acta Neurochir. 1977, 36, 111–115. [Google Scholar] [CrossRef]
- Ito, J.; Konno, K.; Sato, I.; Kameyama, S.; Takeda, S. Convexity cavernous hemangioma, its angiographic and CT findings. Report of a case (author’s transl). No Shinkei 1978, 30, 737–747. [Google Scholar]
- Perry, J.R.; Tucker, W.S.; Chui, M.; Bilbao, J.M. Dural cavernous hemangioma: An under-recognized lesion mimicking meningioma. Can. J. Neurol. Sci. 1993, 20, 230–233. [Google Scholar]
- McKechnie, S.; Harper, C.; Besser, M. Durally-based occipital cavernous haemangioma indistinguishable from meningioma. J. Clin. Neurosci. 1998, 5, 105–108. [Google Scholar] [CrossRef]
- Hyodo, A.; Yanaka, K.; Higuchi, O.; Tomono, Y.; Nose, T. Giant interdural cavernous hemangioma at the convexity: Case. illustration. J. Neurosurg. 2000, 92, 503. [Google Scholar] [CrossRef]
- Joshi, V.; Muzumdar, D.; Dange, N.; Goel, A. Supratentorial convexity dural-based cavernous hemangioma mimicking a meningioma in a child. Pediatr. Neurosurg. 2009, 45, 141–145. [Google Scholar] [CrossRef]
- Sakakibara, Y.; Matsumori, T.; Taguchi, Y.; Koizumi, H. Supratentorial high convexity intradural extramedullary cavernous angioma: Case report. Neurol. Med. Chir. 2010, 50, 328–329. [Google Scholar] [CrossRef]
- Di Vitantonio, H.; De Paulis, D.; Ricci, A.; Marzi, S.; Dehcordi, S.R.; Galzio, R.J. Cavernous hemangioma of the dura mater mimicking meningioma. Surg. Neurol. Int. 2015, 6 (Suppl. 13), S375–S378. [Google Scholar]
- Pelluru, P.K.; Rajesh, A.; Uppin, M.S. Dural-based giant cavernous hemangioma mimicking a meningioma: Lessons learnt. Neurol. India 2017, 65, 1173–1176. [Google Scholar]
- Bhide, A.; Velho, V.; Pujari, M.; Jain, N. Dural-Based Cavernous Hemangioma Mimicking Convexity Meningioma—Case Report. Indian J. Neurosurg. 2018, 7, 280–283. [Google Scholar] [CrossRef]
- Li, Z.; Wang, C.; Ma, L.; Wu, C.; Zhao, Y.; Jiang, Z. Multiple nodular dural cavernous angiomas occluding superior sagittal sinus and destructing calvarium: Case report and literature review. J. Clin. Neurosci. 2018, 58, 218–221. [Google Scholar] [CrossRef] [PubMed]
- Fracasso, L. Considerazioni su un caso di angioma della falce. Riv. Patol. Nerv. Ment. 1947, 68, 214–226. [Google Scholar]
- Kaga, A.; Isono, M.; Mori, T.; Kusakabe, T.; Okada, H.; Hori, S. Cavernous angioma of falx cerebri; case report. No Shinkei Geka 1991, 19, 1079–1083. [Google Scholar] [PubMed]
- McCormick, W.F.; Boulter, T.R. Vascular malformations (“angiomas”) of the dura mater. J. Neurosurg. 1966, 25, 309–311. [Google Scholar] [CrossRef]
- Huber, P. Vascular abnormalities and vascular tumors of the A. carotis externa and of the dura. Fortschr. Geb. Rontgenstr. Nuklearmed. 1968, 109, 325–335. [Google Scholar] [CrossRef]
- Matsumoto, M.; Kikuchi, H.; Nagata, I.; Yamagata, S. A case of tentorial cavernous angioma. No Shinkei Geka 1988, 16, 403–407. [Google Scholar] [PubMed]
- Lee, A.G.; Parrish, R.G.; Goodman, J.C. Homonymous hemianopsia due to a dural cavernous hemangioma. J. Neuroophthalmol. 1998, 18, 250–254. [Google Scholar] [CrossRef]
- Yoshimura, J.; Tsukamoto, Y.; Sano, M.; Hasegawa, H.; Nishino, K.; Saito, A.; Fukuda, M.; Okamoto, K.; Fujii, Y. Successful removal of a huge hypervascular tentorial cavernous angioma after preoperative endovascular embolization. J. Neurosurg. Pediatr. 2014, 14, 43–47. [Google Scholar] [CrossRef]
- Iplikçioğlu, A.C.; Benli, K.; Bertan, V.; Ruacan, S. Cystic cavernous hemangioma of the cerebellopontine angle: Case report. Neurosurgery 1986, 19, 641–642. [Google Scholar] [CrossRef]
- Goel, A.; Achwal, S.; Nagpal, R.D. Dural cavernous haemangioma of posterior cranial fossa. J. Postgrad. Med. 1993, 39, 222–223. [Google Scholar] [PubMed]
- Brunori, A.; Chiappetta, F. Cystic extra-axial cavernoma of the cerebellopontine angle. Surg. Neurol. 1996, 46, 475–476. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.; Rowed, D.W.; Cheung, G.; Ang, L.C. Cavernous malformation presenting as an extra-axial cerebellopontine angle mass: Case report. Neurosurgery 1997, 40, 187–190. [Google Scholar] [PubMed]
- Ferrante, L.; Acqui, M.; Trillò, G.; Antonio, M.; Nardacci, B.; Celli, P. Cavernous angioma of the VIIIth cranial nerve. A case report. Neurosurg. Rev. 1998, 21, 270–276. [Google Scholar] [CrossRef] [PubMed]
- Vajramani, G.V.; Devi, B.I.; Hegde, T.; Srikanth, S.G.; Shankar, S.K. Cystic cavernous malformation of the cerebellopontine angle. Clin. Neurol. Neurosurg. 1998, 100, 133–137. [Google Scholar] [CrossRef]
- Beskonakli, E.; Kaptanoglu, E.; Okutan, O.; Solaroglu, I.; Taskin, Y. Extra-axial cavernomas of the cerebellopontine angle involving the seventh-eighth nerve complex. Neurosurg. Rev. 2002, 25, 222–224. [Google Scholar] [CrossRef] [PubMed]
- Deshmukh, V.R.; Albuquerque, F.C.; Zabramski, J.M.; Spetzler, R.F. Surgical management of cavernous malformations involving the cranial nerves. Neurosurgery 2003, 53, 352–357. [Google Scholar] [CrossRef] [PubMed]
- Stevenson, C.B.; Johnson, M.D.; Thompson, R.C. Cystic cavernous malformation of the cerebellopontine angle. Case illustration. J. Neurosurg. 2005, 103, 931. [Google Scholar] [CrossRef]
- Albanese, A.; Sturiale, C.L.; D’Alessandris, Q.G.; Capone, G.; Maira, G. Calcified extra-axial cavernoma involving lower cranial nerves: Technical case report. Neurosurgery 2009, 64 (Suppl. 3), onsE135–onsE136. [Google Scholar] [CrossRef]
- Engh, J.A.; Kostov, D.; Martin MB, S.; Yeaney, G.; Rothfus, W.; Hirsch, B.; Kassam, A.B. Cavernous malformation tumors: A case study and review of the literature. Otol. Neurotol. 2010, 31, 294–298. [Google Scholar] [CrossRef]
- Huang, H.; Xu, K.; Qu, L.; Li, Y.; Yu, J. Cystic cavernous malformation of the cerebellopontine angle: Case report and literature review. World J. Surg. Oncol. 2011, 9, 36. [Google Scholar] [CrossRef] [PubMed]
- Otani, N.; Wada, K.; Sakakibara, F.; Takeuchi, S.; Nagatani, K. A cystic haemorrhagic lesion located in the cerebellopontine angle cistern. J. Clin. Neurosci. 2012, 19, 1608. [Google Scholar] [CrossRef] [PubMed]
- Wu, B.; Liu, W.; Zhao, Y. Coexistence of extra-axial cavernous malformation and cerebellar developmental venous anomaly in the cerebellopontine angle. World Neurosurg. 2012, 78, e5–e9. [Google Scholar] [CrossRef] [PubMed]
- Ito, M.; Kamiyama, H.; Nakamura, T.; Nakajima, H.; Tokugawa, J. Dural cavernous hemangioma of the cerebellar falx. Neurol. Med. Chir. 2009, 49, 410–412. [Google Scholar] [CrossRef]

| Article | Year | Age (Years) | Gender | Clinical Features | Location | Management | Outcome | |
|---|---|---|---|---|---|---|---|---|
| 1. | Kamrin et al. [57] | 1965 | 46 | Female |
|
| Surgery | Death (11 days after surgery) |
| 2. | Sansone et al. [58] | 1980 | 72 | Female |
|
| Autopsy | - |
| 3. | Buonaguidi et al. [59] | 1984 | 50 | Male |
|
| Surgery | Recurrence after 8 years (reoperation) |
| 4. | Sawamura et al. [60] | 1990 | 45 | Female |
| Surgery |
| |
| 5. | Mitsuhashi et al. [61] | 1991 | 45 | Female |
|
| Surgery | Transcalvarial brain herniation and death (during surgery) |
| 6. | Chhang et al. [62] | 1991 | 48 | Male |
|
|
| Uneventful postoperative course |
| 7. | Lombardi et al. [63] | 1994 | 41 | Female |
|
| Surgery | - |
| 8. | Cobbs et al. [64] | 2001 | 41 | Male |
| Sella (right part) | Surgery |
|
| 9. | Biondi et al. [3] (Case 1) | 2002 | 24 | Female |
| Left cavernous sinus | Surgery | No clinical worsening |
| 10. | Biondi et al. [3] (Case 2) | 2002 | - | - |
| - | Surgery | No clinical worsening |
| 11. | Biondi et al. [3] (Case 3) | 2002 | - | - |
| - | Surgery | No clinical worsening |
| 12. | Biondi et al. [3] (Case 4) | 2002 | 38 | Female |
| Left cavernous sinus |
| No clinical worsening |
| 13. | Jeon et al. [65] | 2004 | 63 | Male |
|
| Surgery | Improvement of hyponatremia |
| 14. | Chuang et al. [55] | 2006 | 62 | Female |
|
| Surgery | Improvement of diplopia |
| 15. | Turan et al. [51] | 2013 | 32 | Female | Blurred vision |
| Surgery | Transient diabetes insipidus |
| 16. | Ma et al. [66] | 2014 | - | - |
|
| Surgery | - |
| 17. | Oommen et al. [2] | 2017 | 50 | Male |
| Left parasellar area | Surgery | Asymptomatic |
| 18. | Wu et al. [67] | 2017 | 64 | Female |
|
| Surgery | Improvement of visual acuity |
| 19. | Das et al. [68] (Case 1) | 2018 | 66 | Female |
|
| Surgery | - |
| 20. | Das et al. [68] (Case 2) | 2018 | 48 | Female |
|
| Surgery | - |
| 21. | Al-Sharydah et al. [69] | 2018 | 43 | Male |
|
|
| Hypothyroidism |
| 22. | Chibbaro et al. [70] | 2018 | 49 | Male |
|
|
| Further lesion shrinkage is stable after five years of follow-up |
| 23. | Pan et al. [71] | 2020 | 55 | Female | Intermittent dizziness | Intrasellar | Surgery |
|
| 24. | Al-Saiari et al. [72] | 2021 | 49 | Female |
|
|
|
|
| Article | Year | Age (Years) | Gender | Clinical Features | Location | Management | Outcome | |
|---|---|---|---|---|---|---|---|---|
| 1. | Canevini et al. [13] | 1963 | Neonate | - | - | - | - | - |
| 2. | Okada et al. [73] | 1977 | 35 | Male |
| Left supraorbital area | Surgery | - |
| 3. | Ito et al. [74] | 1978 | - | - | - | Parietal convexity | - | - |
| 4. | Kunishio et al. [20] | 1986 | 61 | Female |
| Convexity | Surgery | - |
| 5. | Saldana et al. [12] | 1991 | Neonate | Male |
| Mass abutting the inner table of the skull in the frontoparietal region | Surgery | Uneventful postoperative course |
| 6. | Perry et al. [75] | 1993 | 77 | Female |
| Left parietal convexity | Surgery | Uneventful recovery |
| 7. | Revuelta et al. [43] | 1994 | 66 | Male |
| Left occipito-temporal gyrus | Surgery | Uneventful postoperative course |
| 8. | Lewis et al. [16] | 1994 | 36 | Female |
| Right parietal convexity | Surgery |
|
| 9. | Vogler et al. [5] | 1995 | 35 | Male |
| Right parietal occipital | Surgery | - |
| 10. | Suzuki et al. [37] | 1996 | 78 | Female |
| Frontal convexity | Surgery | Successful surgery, but without complete recovery of consciousness |
| 11. | McKechnie et al. [76] | 1998 | 47 | Female |
| Convexity of the right occipital lobe (lateral to the falx) | Surgery | Transient mild decrease in the visual acuity of the left eye (resolved by discharge) |
| 12. | Hyodo et al. [77] | 2000 | 77 | Male | Consciousness disturbance | Right parieto-occipital convexity | Surgery | - |
| 13. | Shen et al. [41] | 2000 | 18 | Female |
| Left parietal lobe | Surgery | Unremarkable |
| 14. | Puca et al. [39] | 2004 | 32 | Female |
| Parietal convexity |
| |
| 15. | Hwang et al. [22] | 2009 | 61 | Male |
| Right frontal convexity | Surgery | - |
| 16. | Joshi et al. [78] | 2009 | 15 | Male | Headache (left parietal region) | Left parieto-occipital convexity | Surgery | Asymptomatic |
| 17. | Sakakibara [79] | 2010 | 59 | Male | Neurological deficits | Left parieto-occipital convexity | Surgery | Resolution of numbness |
| 18. | Yonezawa et al. [48] | 2014 | 78 | Female | Headache | Convexity | Surgery | - |
| 19. | Kashlan et al. [7] | 2014 | 56 | Male |
| Left occipital convexity | Surgery |
|
| 20. | Di Vitantonio H et al. [80] | 2015 | 30 | Female | Progressive left frontal headache | Left frontal | Surgery | Asymptomatic |
| 21. | Wang et al. [45] | 2015 | 37 | Female | Sensory disturbance of the right limbs | Left parietal | No recurrence | |
| 22. | Pelluru et al. [81] | 2018 | 26 | Male |
| Left temporoparietal | Surgery | Asymptomatic |
| 23. | Bhide et al. [82] | 2018 | 22 | Female |
| Right frontal convexity | Surgery |
|
| 24. | Li et al. [83] | 2018 | 33 | Male |
|
| Surgery | Stable residual lesions at a three-month follow-up |
| 25. | Dubovoy et al. [31] | 2018 | 63 | Female |
| Supratentorial, frontal convexity | Surgery |
|
| 26. | Biteich et al. [32] | 2019 | 67 | Male |
| Left frontoparietal | Surgery |
|
| 27. | Ishii et al. [28] | 2021 | 29 | Female |
| Left temporal | Surgery | No recurrence |
| Article | Year | Age (Years) | Gender | Clinical Features | Location | Management | Outcome | |
|---|---|---|---|---|---|---|---|---|
| 1. | Fracasso et al. [84] | 1947 | 47 | Female | - | - | - | - |
| 2. | Kaga et al. [85] | 1991 | 62 | Female |
| Beneath the falx cerebri | Surgery | - |
| 3. | Biondi et al. [3] | 2002 | 63 | Female |
| Anterior third of the flax | Surgery | No clinical worsening |
| 4. | Dorner et al. [34] | 2005 | 37 | Male |
| Right frontal | Surgery | Discharged for further psychiatric management |
| 5. | Kim et al. [49] | 2006 | 22 | Female |
| Right frontal | Surgery | - |
| 6. | Simonin et al. [6] | 2018 | 61 | Female |
| Frontobasal lesion | Surgery |
|
| 7. | Uzunoglu et al. [1] | 2019 | 58 | Male |
| Posterior interhemispheric fissure near the posterior part of the corpus callosum splenium | Surgery | - |
| Article | Year | Age (Years) | Gender | Clinical Features | Location | Management | Outcome | |
|---|---|---|---|---|---|---|---|---|
| 1. | McCormic et al. [86] | 1966 | 52 | Male |
| Right leaf of the tentorium cerebelli | Autopsy | - |
| 2. | McCormic et al. [86] | 1966 | 54 | Male | Death due to suppurative cholangitis, liver necrosis, and uremia | Right leaf of the tentorium | Autopsy | - |
| 3. | Huber [87] | 1968 | 28 | Female | Headache | - | Surgery | - |
| 4. | Moritake et al. [14] | 1985 | Fetus/Neonate | Female |
| Right tentorium cerebelli | Surgery |
|
| 5. | Matsumoto et al. [88] | 1988 | 61 | Female |
| Left tentorium cerebelli | Surgery | - |
| 6. | Quattrocchi et al. [21] | 1989 | 63 | Male |
| Tentorium cerebelli | Surgery | Uneventful postoperative course |
| 7. | Lee et al. [89] | 1998 | 53 | Male |
| Surgery | ||
| 8. | Van Lindert et al. [25] | 2006 | 36 | Female |
| Temporoparietal lesion in the right hemisphere with transtentorial extension in the right cerebellar hemisphere | Surgery |
|
| 9. | Mori et al. [8] | 2009 | 15 | Male |
| Right cerebellar tentorium with extension to the supratentorial and infratentorial spaces | Surgery | Transient left homonymous hemianopia |
| 10. | Bhatia et al. [24] | 2011 | 60 | Male |
| Tentorial mass, with its bulk primarily in the posterior fossa | Surgery | Resolution of neurologic deficits |
| 11. | Yoshimura et al. [90] | 2014 | 15 | Female |
| Right occipital and suboccipital regions, both the supra- and infratentorial spaces |
|
|
| Article | Year | Age (Years) | Gender | Clinical Features | Location | Management | Outcome | |
|---|---|---|---|---|---|---|---|---|
| 1. | Iplikcioglu et al. [91] | 1986 | 30 | Female |
| Left CPA | Surgery |
|
| 2. | Goel et al. [92] | 1993 | 60 | Male | Episodic ataxia of left-sided limbs | Lateral part of the left cerebellar hemisphere | Surgery | Uneventful postoperative course |
| 3. | Brunoni et al. [93] | 1996 | 60 | Male |
| Left CPA | Surgery | - |
| 4. | Kim et al. [94] | 1997 | 32 | Male |
| CPA without internal auditory canal involvement | Surgery | Resolution of facial paresis |
| 5. | Ferrante et al. [95] | 1998 | 24 | Female |
| Right CPA | Surgery |
|
| 6. | Vajramani et al. [96] | 1998 | 46 | Male |
| Right CPA | Surgery |
|
| 7. | Benkonakli et al. [97] (Case 1) | 2002 | 19 | Male |
| Involvement of the seventh-eighth nerve complex | Surgery | Persistent facial hypoesthesia |
| 8. | Benkonakli et al. [97] (Case 2) | 2002 | 25 | Male |
| Right CPA | Surgery | Good condition |
| 9. | Deshmukh et al. [68] (Case 1) | 2003 | 76 | Male |
| Left CN VII/CN VIII | Surgery |
|
| 10. | Deshmukh et al. [98] (Case 2) | 2003 | 53 | Male |
| Left CPA, Left CN VII/CN VIII | Surgery |
|
| 11. | Stevenson et al. [99] | 2005 | 57 | Male |
| Right CPA | Surgery |
|
| 12. | Albanese et al. [100] | 2009 | 48 | Male |
| Lower third of the right CPA cistern | Surgery | Significant improvement in voice tone |
| 13. | Sasani et al. [19] | 2010 | 16 | Female | Headache | Right cerebellopontine angle | Surgery |
|
| 14. | Engh et al. [101] | 2010 | 16 | Female |
| Left cerebellopontine angle | Surgery |
|
| 15. | Huang et al. [102] | 2011 | 50 | Male |
| Cerebellopontine angle | Surgery | Resolution of symptoms |
| 16. | Otani et al. [103] | 2012 | 74 | Female |
| Cerebellopontine angle cistern | Surgery | Hearing could not be recovered |
| 17. | Wu et al. [104] | 2012 | 36 | Male |
| Left cerebellopontine angle cistern | Surgery |
|
| 18. | Ghanta et al. [40] | 2013 | 50 | Male |
| Left cerebellopontine angle | Surgery | Significant recovery of the lower cranial nerve palsy |
| 19. | Tarabay et al. [17] | 2019 | 44 | Female |
| Right cerebellopontine angle | Surgery |
|
| Article | Year | Age (Years) | Gender | Clinical Features | Location | Management | Outcome | |
|---|---|---|---|---|---|---|---|---|
| 1. | Ito et al. [105] | 2009 | 47 | Male |
| Posterior cranial fossa arising attached to the cerebellar falx | Surgery | Unremarkable postoperative course |
| 2. | Melone et al. [42] | 2010 | 58 | Male | An episode of mental confusion | Posterior cranial fossa arising from the cerebellar falx | Surgery | Uneventful postoperative course |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hassanzadeh, S.; Gao, L.; Alvarado, A.M.; Camarata, P.J.; Lakis, N.S.; Haeri, M. Extra-Axial Cavernous Angioma: A Case Report and Review of the Literature. Neurol. Int. 2024, 16, 162-185. https://doi.org/10.3390/neurolint16010010
Hassanzadeh S, Gao L, Alvarado AM, Camarata PJ, Lakis NS, Haeri M. Extra-Axial Cavernous Angioma: A Case Report and Review of the Literature. Neurology International. 2024; 16(1):162-185. https://doi.org/10.3390/neurolint16010010
Chicago/Turabian StyleHassanzadeh, Shakiba, Linlin Gao, Anthony M. Alvarado, Paul J. Camarata, Nelli S. Lakis, and Mohammad Haeri. 2024. "Extra-Axial Cavernous Angioma: A Case Report and Review of the Literature" Neurology International 16, no. 1: 162-185. https://doi.org/10.3390/neurolint16010010
APA StyleHassanzadeh, S., Gao, L., Alvarado, A. M., Camarata, P. J., Lakis, N. S., & Haeri, M. (2024). Extra-Axial Cavernous Angioma: A Case Report and Review of the Literature. Neurology International, 16(1), 162-185. https://doi.org/10.3390/neurolint16010010





