Medical Therapy Versus Percutaneous Coronary Intervention in Patients with Myocardial Bridging from a National Population-Based Cohort Study: The Use of Big Data Analytics
Abstract
1. Introduction
2. Methods
2.1. Data Source
2.2. Study Population
2.3. Study Outcomes and Definitions
2.4. Statistical Analysis
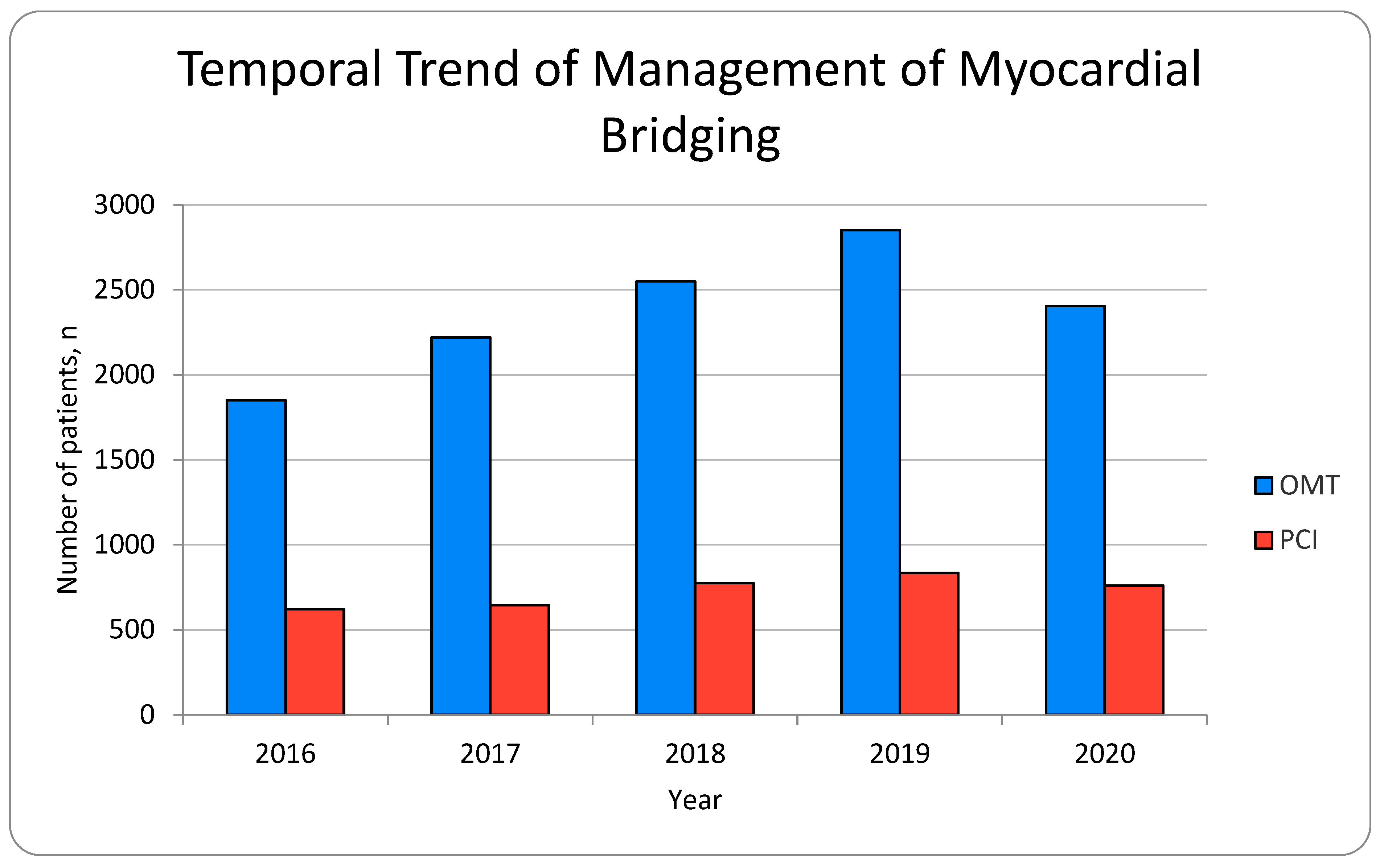
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Evbayekha, E.O.; Nwogwugwu, E.; Olawoye, A.; Bolaji, K.; Adeosun, A.A.; Ajibowo, A.O.; Nsofor, G.C.; Chukwuma, V.N.; Shittu, H.O.; Onuegbu, C.A.; et al. A Comprehensive Review of Myocardial Bridging: Exploring Diagnostic and Treatment Modalities. Cureus 2023, 15, e43132. [Google Scholar] [CrossRef] [PubMed]
- Moore, P.; Murdock, P.; Ramanathan, A.; Sathyamoorthy, M. A Contemporary Review of the Genomic Associations of Coronary Artery Myocardial Bridging. Genes 2023, 14, 2175. [Google Scholar] [CrossRef]
- Yang, T.L.; Ting, J.; Lin, M.R.; Chang, W.C.; Shih, C.M. Identification of Genetic Variants Associated with Severe Myocardial Bridging through Whole-Exome Sequencing. J. Pers. Med. 2023, 13, 1509. [Google Scholar] [CrossRef] [PubMed]
- Sternheim, D.; Power, D.A.; Samtani, R.; Kini, A.; Fuster, V.; Sharma, S. Myocardial Bridging: Diagnosis, Functional Assessment, and Management: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2021, 78, 2196–2212. [Google Scholar] [CrossRef]
- Tandar, A.; Whisenant, B.K.; Michaels, A.D. Stent fracture following stenting of a myocardial bridge: Report of two cases. Catheter. Cardiovasc. Interv. 2008, 71, 191–196. [Google Scholar] [CrossRef]
- Srinivasan, M.; Prasad, A. Metal fatigue in myocardial bridges: Stent fracture limits the efficacy of drug-eluting stents. J. Invasive Cardiol. 2011, 23, E150–E152. [Google Scholar]
- Broderick, T.M.; Kereiakes, D.J.; Whang, D.D.; Toltzis, R.J.; Abbottsmith, C.W. Myocardial Bridging May Predispose to Coronary Perforation During Rotational Atherectomy. J. Invasive Cardiol. 1996, 8, 161–163. [Google Scholar] [PubMed]
- Zhang, M.; Kang, W.C.; Moon, C.I.; Han, S.H.; Ahn, T.H.; Shin, E.K. Coronary artery perforation following implantation of a drug-eluting stent rescued by deployment of a covered stent in symptomatic myocardial bridging. Korean Circ. J. 2010, 40, 148–151. [Google Scholar] [CrossRef]
- Agrawal, H.; Mery, C.M.; Sexson, T.S.K.; Fraser, C.D.; McKenzie, E.D.; Qureshi, A.M.; Molossi, S. Familial clustering of cardiac conditions in patients with anomalous aortic origin of a coronary artery and myocardial bridges. Cardiol. Young 2018, 28, 1099–1105. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, E.R.; Klues, H.G.; vom Dahl, J.; Klein, I.; Krebs, W.; Hanrath, P. Functional characteristics of myocardial bridging. A combined angiographic and intracoronary Doppler flow study. Eur. Heart J. 1997, 18, 434–442. [Google Scholar] [CrossRef]
- Klues, H.G.; Schwarz, E.R.; vom Dahl, J.; Reffelmann, T.; Reul, H.; Potthast, K.; Schmitz, C.; Minartz, J.; Krebs, W.; Hanrath, P. Disturbed intracoronary hemodynamics in myocardial bridging: Early normalization by intracoronary stent placement. Circulation 1997, 96, 2905–2913. [Google Scholar] [CrossRef] [PubMed]
- Corban, M.T.; Hung, O.Y.; Eshtehardi, P.; Rasoul-Arzrumly, E.; McDaniel, M.; Mekonnen, G.; Timmins, L.H.; Lutz, J.; Guyton, R.A.; Samady, H. Myocardial bridging: Contemporary understanding of pathophysiology with implications for diagnostic and therapeutic strategies. J. Am. Coll. Cardiol. 2014, 63, 2346–2355. [Google Scholar] [CrossRef]
- Lee, M.S.; Chen, C.H. Myocardial Bridging: An Up-to-Date Review. J. Invasive Cardiol. 2015, 27, 521–528. [Google Scholar] [PubMed]
- Attaran, S.; Moscarelli, M.; Athanasiou, T.; Anderson, J. Is coronary artery bypass grafting an acceptable alternative to myotomy for the treatment of myocardial bridging? Interact. Cardiovasc. Thorac. Surg. 2013, 16, 347–349. [Google Scholar] [CrossRef]
- Pratt, J.W.; Michler, R.E.; Pala, J.; Brown, D.A. Minimally invasive coronary artery bypass grafting for myocardial muscle bridging. Heart. Surg. Forum 1999, 2, 250–253. [Google Scholar]
- Ernst, A.; Bulum, J.; Šeparović, H.J.; Lovrić, B.M.; Strozzi, M. Five-year angiographic and clinical follow-up of patients with drug-eluting stent implantation for symptomatic myocardial bridging in absence of coronary atherosclerotic disease. J. Invasive Cardiol. 2013, 25, 586–592. [Google Scholar] [PubMed]
- Tsujita, K.; Maehara, A.; Mintz, G.S.; Doi, H.; Kubo, T.; Castellanos, C.; Liu, J.; Yang, J.; Oviedo, C.; Franklin-Bond, T.; et al. Impact of myocardial bridge on clinical outcome after coronary stent placement. Am. J. Cardiol. 2009, 103, 1344–1348. [Google Scholar] [CrossRef]
- Hao, Z.; Xinwei, J.; Ahmed, Z.; Huanjun, P.; Zhanqi, W.; Yanfei, W.; Chunhong, C.; Chan, Z.; Liqiang, F. The Outcome of Percutaneous Coronary Intervention for Significant Atherosclerotic Lesions in Segment Proximal to Myocardial Bridge at Left Anterior Descending Coronary Artery. Int. Heart. J. 2018, 59, 467–473. [Google Scholar] [CrossRef]
- Schwarz, E.R.; Klues, H.G.; vom Dahl, J.; Klein, I.; Krebs, W.; Hanrath, P. Functional, angiographic and intracoronary Doppler flow characteristics in symptomatic patients with myocardial bridging: Effect of short-term intravenous beta-blocker medication. J. Am. Coll. Cardiol. 1996, 27, 1637–1645. [Google Scholar] [CrossRef]
- Haager, P.K.; Schwarz, E.R.; vom Dahl, J.; Klues, H.G.; Reffelmann, T.; Hanrath, P. Long term angiographic and clinical follow up in patients with stent implantation for symptomatic myocardial bridging. Heart 2000, 84, 403–408. [Google Scholar] [CrossRef]
- Shen, L.; Xu, K.; Zhang, W.; Zheng, X.; He, B. Drug-Coated Balloon Treatment for ACS Induced by Myocardial Bridging: An Intravascular Ultrasound-Guided PCI. CJC Open 2021, 3, 372–375. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, E.R.; Gupta, R.; Haager, P.K.; vom Dahl, J.; Klues, H.G.; Minartz, J.; Uretsky, B.F. Myocardial bridging in absence of coronary artery disease: Proposal of a new classification based on clinical-angiographic data and long-term follow-up. Cardiology 2009, 112, 13–21. [Google Scholar] [CrossRef]
| Variables | Medical Therapy | PCI | Total | p-Value | ||
|---|---|---|---|---|---|---|
| Number of patients, n | 11,875 | % | 3635 | % | 15,510 | |
| Age | 64.53 ± 15.04 | 65.86 ± 12.83 | 0.019 | |||
| Female | 3695 | 31.12 | 970 | 26.69 | 4665 | 0.0223 |
| Race | 0.0002 | |||||
| White | 7595 | 63.96 | 2580 | 70.98 | 10,175 | |
| Black | 1705 | 14.36 | 355 | 9.77 | 2060 | |
| Hispanic | 1140 | 9.60 | 250 | 6.88 | 1390 | |
| Asian or Pacific Islander | 480 | 4.04 | 100 | 2.75 | 580 | |
| Native American | 45 | 0.38 | 35 | 0.96 | 80 | |
| Other | 430 | 3.62 | 155 | 4.26 | 585 | |
| Missing | 480 | 3.62 | 160 | 4.40 | ||
| Hospital Bed Size | 0.9295 | |||||
| Small | 1920 | 16.17 | 605 | 16.64 | 2525 | |
| Medium | 3125 | 26.32 | 935 | 25.72 | 4060 | |
| Large | 6830 | 57.52 | 2095 | 57.63 | 8925 | |
| Hospital Teaching Status | 0.0071 | |||||
| Rural | 520 | 4.38 | 215 | 5.91 | 735 | |
| Urban Non-teaching | 2080 | 17.52 | 790 | 21.73 | 2870 | |
| Urban Teaching | 9275 | 78.11 | 2630 | 72.35 | 11,905 | |
| Admission | ||||||
| Elective | 2350 | 19.81 | 485 | 13.36 | 2835 | 0.0001 |
| Primary payment coverage | 0.00 | 0.00 | 0.0835 | |||
| Medicare | 6695 | 56.38 | 1950 | 53.65 | 8645 | |
| Medicaid | 1300 | 10.95 | 300 | 8.25 | 1600 | |
| Private insurance | 3130 | 26.36 | 1095 | 30.12 | 4225 | |
| Self-pay | 345 | 2.91 | 140 | 3.85 | 485 | |
| No charge | 45 | 0.38 | 15 | 0.41 | 60 | |
| Other | 350 | 2.95 | 130 | 3.58 | 480 | |
| Missing | 10 | 2.95 | 5 | 3.58 | ||
| Median household income, USD | 0.231 | |||||
| 1–28,999 | 3190 | 26.86 | 1000 | 27.51 | 4190 | |
| 29,000–35,999 | 3115 | 26.23 | 1050 | 28.89 | 4165 | |
| 36,000–46,999 | 2880 | 24.25 | 760 | 20.91 | 3640 | |
| 47,000+ | 2425 | 20.42 | 765 | 21.05 | 3640 | |
| Missing | 265 | 2.23 | 60 | 1.65 | ||
| Hospital Region | 0.3563 | |||||
| Northeast | 1805 | 15.20 | 500 | 13.76 | 2305 | |
| Midwest | 3020 | 25.43 | 840 | 23.11 | 3860 | |
| South | 4615 | 38.86 | 1530 | 42.09 | 6145 | |
| West | 2435 | 20.51 | 765 | 21.05 | 3200 | |
| Comorbidities | ||||||
| Congestive heart failure | 4995 | 42.06 | 1480 | 40.72 | 6475 | 0.5264 |
| Cardiac arrhythmias | 5790 | 48.76 | 1520 | 41.82 | 7310 | 0.0012 |
| Valvular heart diseases | 2725 | 22.95 | 520 | 14.31 | 3245 | <0.001 |
| Pulmonary circulatory disorders | 1235 | 10.40 | 245 | 6.74 | 1480 | 0.0036 |
| Peripheral vascular disease | 2610 | 21.98 | 545 | 14.99 | 3155 | <0.001 |
| HTN, uncomplicated | 4765 | 40.13 | 1805 | 49.66 | 6570 | <0.001 |
| HTN, complicated | 4835 | 40.72 | 1225 | 33.70 | 6060 | 0.0008 |
| Paralysis | 170 | 1.43 | 30 | 0.83 | 200 | 0.2055 |
| Other neurologic disorders | 1050 | 8.84 | 200 | 5.50 | 1250 | 0.0042 |
| Chronic lung disease | 3135 | 26.40 | 675 | 18.57 | 3810 | <0.001 |
| DM, uncomplicated | 1545 | 13.01 | 635 | 17.47 | 2180 | 0.0026 |
| DM, complicated | 2020 | 17.01 | 625 | 17.19 | 2645 | 0.9101 |
| Hypothyroidism | 1430 | 12.04 | 415 | 11.42 | 1845 | 0.6506 |
| CKD | 2675 | 22.53 | 630 | 17.33 | 3305 | 0.0027 |
| Liver disease | 545 | 4.59 | 210 | 5.78 | 755 | 0.1937 |
| Peptic ulcer disease | 100 | 0.84 | 15 | 0.41 | 115 | 0.2386 |
| Lymphoma | 55 | 0.46 | 15 | 0.41 | 70 | 0.8586 |
| Metastatic cancer | 130 | 1.09 | 40 | 1.10 | 170 | 0.9897 |
| Solid tumor | 390 | 3.28 | 95 | 2.61 | 485 | 0.3693 |
| Rheumatologic disorders | 800 | 6.74 | 130 | 3.58 | 930 | 0.0018 |
| Coagulopathy | 1465 | 12.34 | 225 | 6.19 | 1690 | 0 |
| Obesity | 2525 | 21.26 | 775 | 21.32 | 3300 | 0.9743 |
| Weight loss | 580 | 4.88 | 50 | 1.38 | 630 | <0.001 |
| Fluid and electrolyte disorders | 3660 | 30.82 | 805 | 22.15 | 4465 | <0.001 |
| Blood loss anemia | 85 | 0.72 | 30 | 0.83 | 115 | 0.7635 |
| Deficiency anemia | 475 | 4.00 | 130 | 3.58 | 605 | 0.606 |
| Alcohol abuse | 450 | 3.79 | 115 | 3.16 | 565 | 0.4317 |
| Drug abuse | 500 | 4.21 | 170 | 4.68 | 670 | 0.5964 |
| Psychoses | - | - | - | - | - | - |
| Depression | 1225 | 10.32 | 310 | 8.53 | 1535 | 0.1562 |
| Smoking | 2280 | 19.20 | 1005 | 27.65 | 3285 | <0.001 |
| Prior MI | 2400 | 20.21 | 725 | 19.94 | 3125 | 0.8779 |
| Prior PCI | 170 | 1.43 | 35 | 0.96 | 205 | 0.332 |
| Prior CABG | 1055 | 8.88 | 205 | 5.64 | 1260 | 0.1462 |
| AMI | 3520 | 29.64 | 2650 | 72.90 | 6170 | <0.001 |
| Outcomes | Medical Therapy | PCI | p-Value | Adjusted OR | Lower Limit | Upper Limit | p-Value | ||
|---|---|---|---|---|---|---|---|---|---|
| Number of patients | 11,875 | % | 3635 | % | |||||
| Mortality | 325 | 2.74 | 165 | 4.54 | 0.0151 | 1.39 | 0.81 | 2.40 | 0.232 |
| Cardiac arrest | 290 | 2.44 | 145 | 3.99 | 0.0285 | 1.68 | 0.94 | 3.03 | 0.083 |
| Cardiogenic shock | 590 | 4.97 | 365 | 10.04 | 0 | 2.04 | 1.40 | 2.99 | 0 |
| Use of MCS | |||||||||
| LVAD | 45 | 0.38 | 170 | 4.68 | 0 | 15.22 | 5.54 | 41.79 | 0 |
| IABP | 230 | 1.94 | 245 | 6.74 | 0 | 2.24 | 1.34 | 3.74 | 0.002 |
| ECMO | 30 | 0.25 | 15 | 0.41 | 0.5055 | - | - | - | - |
| AKI | 2370 | 19.96 | 595 | 16.37 | 0.0317 | 0.93 | 0.70 | 1.23 | 0.595 |
| Cost of hospitalization, USD | 27,787 ± 32,418 | - | 30,884 ± 25,100 | - | 0.009 | - | - | - | - |
| Length of stay, days | 6.13 ± 6.57 | - | 4.53 ± 5.25 | - | <0.001 | - | - | - | - |
| Variables | Odds Ratio | Lower Limit | Upper Limit | p-Value |
|---|---|---|---|---|
| Smoking | 1.61 | 1.31 | 1.97 | 0 |
| Prior MI | 0.77 | 0.62 | 0.95 | 0.015 |
| Depression | 0.66 | 0.49 | 0.88 | 0.004 |
| Prior CABG | 0.57 | 0.40 | 0.80 | 0.001 |
| Psychosis | 0.35 | 0.10 | 1.27 | 0.11 |
| Drug abuse | 0.95 | 0.63 | 1.43 | 0.797 |
| Nutrional deficiency anemia | 0.84 | 0.54 | 1.31 | 0.435 |
| Blood loss anemia | 0.74 | 0.26 | 2.11 | 0.568 |
| Weight loss | 0.43 | 0.26 | 0.70 | 0.001 |
| Coagulopathy | 0.84 | 0.64 | 1.12 | 0.232 |
| Rheumatological disorders | 0.92 | 0.65 | 1.30 | 0.64 |
| Lymphoma | 0.27 | 0.05 | 1.50 | 0.135 |
| Peptic ulcer disease | 0.26 | 0.07 | 1.01 | 0.051 |
| CKD | 0.74 | 0.58 | 0.95 | 0.019 |
| Hypothyroidism | 0.88 | 0.67 | 1.15 | 0.334 |
| Diabetes, uncomplicated | 1.16 | 0.91 | 1.48 | 0.223 |
| Chronic lung disease | 0.65 | 0.52 | 0.80 | 0 |
| Other neurological disorders | 0.72 | 0.53 | 0.99 | 0.045 |
| Hypertension, complicated | 1.32 | 1.03 | 1.70 | 0.027 |
| Hypertension, uncomplicated | 1.11 | 0.89 | 1.37 | 0.366 |
| Peripheral vascular disease | 0.69 | 0.56 | 0.86 | 0.001 |
| Pulmonary circulatory disorders | 0.55 | 0.40 | 0.76 | 0 |
| Valvular heart diseases | 0.82 | 0.66 | 1.02 | 0.07 |
| Cardiac arrhythmia | 0.85 | 0.72 | 1.01 | 0.062 |
| Median household income | ||||
| 1–28,999 | Ref | |||
| 29,000–35,999 | 1.17 | 0.94 | 1.47 | 0.163 |
| 36,000–46,999 | 0.91 | 0.72 | 1.14 | 0.408 |
| 47,000+ | 0.93 | 0.72 | 1.19 | 0.565 |
| Elective admission | 0.17 | 0.13 | 0.23 | 0 |
| Primary payer method | ||||
| Medicare | Ref | |||
| Medicaid | 1.00 | 0.72 | 1.38 | 0.977 |
| Private insurance | 1.48 | 1.19 | 1.86 | 0.001 |
| Self-pay | 1.49 | 0.90 | 2.47 | 0.12 |
| No charge | 1.01 | 0.28 | 3.61 | 0.988 |
| Other | 2.06 | 1.30 | 3.27 | 0.002 |
| Hospital region | ||||
| Northeast | Ref | |||
| Midwest | 1.14 | 0.87 | 1.50 | 0.349 |
| South | 1.05 | 0.82 | 1.36 | 0.683 |
| West | 1.46 | 1.10 | 1.93 | 0.008 |
| Hospital teaching status | ||||
| Rural | Ref | |||
| Urban Non-teaching | 0.70 | 0.46 | 1.05 | 0.085 |
| Urban Teaching | 0.69 | 0.47 | 1.01 | 0.058 |
| Hospital bed size | ||||
| Small | Ref | |||
| Medium | 0.85 | 0.66 | 1.11 | 0.242 |
| Large | 0.82 | 0.64 | 1.04 | 0.1 |
| Race | ||||
| White | Ref | |||
| Black | 0.79 | 0.62 | 1.02 | 0.067 |
| Hispanic | 0.84 | 0.63 | 1.13 | 0.25 |
| Asian or Pacific Islander | 1.04 | 0.70 | 1.55 | 0.838 |
| Native American | 3.76 | 1.22 | 11.56 | 0.021 |
| Other | 0.85 | 0.54 | 1.33 | 0.472 |
| Female | 0.75 | 0.62 | 0.91 | 0.003 |
| Age | 1.01 | 1.00 | 1.02 | 0.031 |
| Mortality | Odds Ratio | Lower Limit | Upper Limit | p-Value |
|---|---|---|---|---|
| AMI | 4.09 | 2.58 | 6.49 | <0.001 |
| Drug abuse | 0.60 | 0.17 | 2.07 | 0.418 |
| Blood loss anemia | 0.86 | 0.12 | 5.96 | 0.876 |
| Fluid and electrolyte disorders | 2.28 | 1.45 | 3.59 | <0.001 |
| Obesity | 0.42 | 0.21 | 0.82 | 0.011 |
| Coagulopathy | 1.81 | 1.07 | 3.07 | 0.027 |
| Peptic ulcer disease | 5.23 | 1.11 | 24.62 | 0.036 |
| Liver disease | 4.76 | 2.63 | 8.59 | <0.001 |
| CKD | 2.32 | 1.29 | 4.19 | 0.005 |
| Other neurological disorders | 3.32 | 1.96 | 5.60 | <0.001 |
| Hypertension, complicated | 0.53 | 0.25 | 1.11 | 0.094 |
| Hypertension, uncomplicated | 0.94 | 0.46 | 1.91 | 0.867 |
| Cardiac arrhythmias | 2.53 | 1.54 | 4.16 | <0.001 |
| Congestive heart failure | 1.83 | 1.04 | 3.24 | 0.037 |
| Hospital region | ||||
| Northeast | ||||
| Midwest | 1.13 | 0.55 | 2.33 | 0.734 |
| South | 1.13 | 0.57 | 2.22 | 0.726 |
| West | 1.29 | 0.62 | 2.67 | 0.496 |
| Age | 1.02 | 1.00 | 1.03 | 0.091 |
| Variables | Odds Ratio | Lower Limit | Upper Limit | p-Value |
|---|---|---|---|---|
| AMI | 3.44 | 1.90 | 6.24 | 0 |
| Prior MI | 0.51 | 0.21 | 1.26 | 0.146 |
| Prior PCI | 2.16 | 0.24 | 19.35 | 0.491 |
| Depression | 0.51 | 0.13 | 1.92 | 0.317 |
| Fluid and electrolyte disorders | 2.02 | 1.15 | 3.54 | 0.014 |
| Obesity | 0.41 | 0.16 | 1.02 | 0.055 |
| Coagulopathy | 1.87 | 0.98 | 3.58 | 0.059 |
| Solid tumour | 1.00 | |||
| Liver disease | 3.09 | 1.33 | 7.14 | 0.009 |
| CKD | 1.90 | 0.98 | 3.70 | 0.059 |
| Other neurological disorders | 3.67 | 1.82 | 7.40 | 0 |
| Hypertension, uncomplicated | 1.22 | 0.54 | 2.74 | 0.637 |
| Peripheral vascular disease | 1.67 | 0.95 | 2.95 | 0.076 |
| Pulmonary circulatory disorders | 1.16 | 0.49 | 2.77 | 0.738 |
| Valvular heart diseases | 1.16 | 0.64 | 2.11 | 0.615 |
| Cardiac arrhythmias | 2.85 | 1.50 | 5.44 | 0.001 |
| Congestive heart failure | 1.18 | 0.60 | 2.32 | 0.642 |
| Median household income | ||||
| 1–28,999 | ||||
| 29,000–35,999 | 0.62 | 0.30 | 1.32 | 0.215 |
| 36,000–46,999 | 0.79 | 0.39 | 1.60 | 0.509 |
| 47,000+ | 0.44 | 0.18 | 1.08 | 0.074 |
| Elective | 0.45 | 0.16 | 1.28 | 0.137 |
| Hospital bed size | ||||
| Small | Ref | |||
| Medium | 3.16 | 1.14 | 8.75 | 0.027 |
| Large | 1.90 | 0.73 | 4.94 | 0.188 |
| Age | 1.02 | 0.99 | 1.04 | 0.204 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Krittanawong, C.; Ang, S.P.; Padilla, F.A.; Qadeer, Y.K.; Wang, Z.; Gaibazzi, N.; Sharma, S.K.; Lavie, C.J.; Schaff, H.V.; Schwarz, E.R. Medical Therapy Versus Percutaneous Coronary Intervention in Patients with Myocardial Bridging from a National Population-Based Cohort Study: The Use of Big Data Analytics. Cardiogenetics 2025, 15, 10. https://doi.org/10.3390/cardiogenetics15020010
Krittanawong C, Ang SP, Padilla FA, Qadeer YK, Wang Z, Gaibazzi N, Sharma SK, Lavie CJ, Schaff HV, Schwarz ER. Medical Therapy Versus Percutaneous Coronary Intervention in Patients with Myocardial Bridging from a National Population-Based Cohort Study: The Use of Big Data Analytics. Cardiogenetics. 2025; 15(2):10. https://doi.org/10.3390/cardiogenetics15020010
Chicago/Turabian StyleKrittanawong, Chayakrit, Song Peng Ang, Fernando Alexis Padilla, Yusuf Kamran Qadeer, Zhen Wang, Nicola Gaibazzi, Samin K. Sharma, Carl J. Lavie, Hartzell V. Schaff, and Ernst R. Schwarz. 2025. "Medical Therapy Versus Percutaneous Coronary Intervention in Patients with Myocardial Bridging from a National Population-Based Cohort Study: The Use of Big Data Analytics" Cardiogenetics 15, no. 2: 10. https://doi.org/10.3390/cardiogenetics15020010
APA StyleKrittanawong, C., Ang, S. P., Padilla, F. A., Qadeer, Y. K., Wang, Z., Gaibazzi, N., Sharma, S. K., Lavie, C. J., Schaff, H. V., & Schwarz, E. R. (2025). Medical Therapy Versus Percutaneous Coronary Intervention in Patients with Myocardial Bridging from a National Population-Based Cohort Study: The Use of Big Data Analytics. Cardiogenetics, 15(2), 10. https://doi.org/10.3390/cardiogenetics15020010








