Abstract
Ebstein anomaly is a rare heterogeneous congenital heart defect (CHD) with a largely unknown etiology. We present a 6-year-old girl with Ebstein anomaly, atrial septum defect, hypoplastic right ventricle, and persistent left superior vena cava who has a de novo intragenic ~403 kb deletion of the GDP-mannose 4,6-dehydratase (GMDS) gene. GMDS is located on chromosome 6p25.3 and encodes the rate limiting enzyme in GDP-fucose synthesis, which is used to fucosylate many proteins, including Notch1, which plays a critical role during mammalian cardiac development. The GMDS locus has sporadically been associated with Ebstein anomaly (large deletion) and tetralogy of Fallot (small deletion). Given its function and the association with CHD, we hypothesized that loss-of-function of, or alterations in, GMDS could play a role in the development of Ebstein anomaly. We collected a further 134 cases with Ebstein anomaly and screened them for genomic aberrations of the GMDS locus. No additional GMDS genomic aberrations were identified. In conclusion, we describe a de novo intragenic GMDS deletion associated with Ebstein anomaly. Together with previous reports, this second case suggests that GMDS deletions could be a rare cause for congenital heart disease, in particular Ebstein anomaly.
1. Introduction
Ebstein anomaly is a rare congenital heart defect in which the tricuspid valve is malformed and displaced downward into the right ventricle.
It accounts for less than 1% of all congenital heart diseases. Older studies reported a live birth prevalence of Ebstein anomaly of around 1:200,000 [1], but more recent population studies have reported a lower birth prevalence of around 1:20,000 [2,3,4]. This has been attributed to different factors, i.e., earlier and better diagnoses [5], better technology, and differences in ascertainment methods and classifications [5,6].
The clinical presentation of Ebstein anomaly varies widely and depends on the degree of anatomic abnormalities. Additional cardiac anomalies, such as patent foramen ovale, atrial septum defect, pulmonary stenosis or atresia, and ventricular septum defect, are often present in cases with Ebstein anomaly [7]. Approximately 20% of cases with Ebstein anomaly have extra-cardiac malformations suggesting that the cardiac defect could be part of a genetic syndrome [2]. The etiology of Ebstein anomaly is largely unknown. Epidemiologic studies have reported associations between Ebstein anomaly and environmental factors, such as peri-conceptional exposure to pesticides and varnishes as well as maternal infections and maternal health conditions [2,3,7]. In addition, familial recurrence and identification of genetic variants segregating with this congenital disorder also suggest a genetic component [8,9]. Although Ebstein anomaly has been sporadically described in genetic syndromes, including Down, CHARGE, Noonan, and Cornelia de Lange syndrome [10,11,12,13], a consistent association between Ebstein anomaly and a distinct genetic condition has not yet been identified [10]. Pathogenic variants in three genes (MYH7, NKX2-5, and GATA4) and different copy number variants have been described in cases with Ebstein anomaly but only account for a small proportion of cases [6,13,14,15]. In 2016, Sicko et al. performed a genome-wide investigation of copy number variants in a cohort of 47 cases with isolated Ebstein anomaly [6]. They identified several (new) candidate copy number variants, including one intragenic GMDS deletion of approximately 345 kb on chromosome 6p25.3.
Here, we report a second case of Ebstein anomaly associated with a de novo 403 kb intragenic GMDS deletion. Additionally, we analyzed a further 134 cases with isolated Ebstein anomaly for abnormalities in the GMDS genomic locus, specifically copy number variants.
2. Materials and Methods
2.1. Clinical Data
The patient was enrolled at Amsterdam UMC in Amsterdam, the Netherlands. The parents provided written consent for research use of their data, and the study was conducted in accordance with the Declaration of Helsinki. Clinical data were retrieved from the patient’s records. A total of 134 additional patients were evaluated from the Netherlands and the patient’s island of origin. We obtained genomic DNA from 129 cases with the main clinical diagnosis of either Ebstein malformation, congenital pulmonary valve stenosis, or tricuspid atresia. These cases were collected through the Dutch national biobank of adult cases with congenital heart defects (CONCOR) [16]. Subsequently, we screened these cases for copy number variants (CNVs) in GMDS using digital droplet PCR for three locations across the whole GMDS locus, including the previously identified deletion. Using this method, we could positively identify the deletion in the proband, validating the array-CGH results. From the same Caribbean island, genomic DNA from five cases with Ebstein anomaly was analyzed. Under Dutch law, assessment of the study protocol by our ethics committee was not required since only genetic and clinical data collected during regular patient care were used. This is specifically explained for (Dutch) research involving the CONCOR registry and DNA-bank [16,17].
2.2. Array-CGH
Copy number profiling was performed on DNA isolated from peripheral blood using 180 K (Amadid #023363) Human Genome CGH Microarray slides from Agilent Technologies (Version 5.1, Santa Clara, CA, USA) according to the manufacturer’s protocols. The results were classified with Cartagenia BENCH software 5.1. (Cartagenia, Leuven, Belgium).
2.3. Next-Generation Sequencing Targeted Panel
In addition, a next-generation sequencing (NGS) targeted structural heart disease gene panel was performed, which consisted of 46 genes, including Noonan-syndrome related genes (BRAF, KRAS, LZTR1, MAP2K1, NRAS, PTPN11, RAF1, RASA2, RIT1, SOS1, and SOS2).
2.4. CNV Detection Using Droplet Digital PCR (ddPCR)
For ddPCR, the QX200 Droplet Digital PCR system (Bio-Rad, Hercules, CA, USA) was used. The ddPCR reaction was performed in a 21 μL volume consisting of 10 μL 2× ddPCR Supermix for Probes (No UDP) (Bio-Rad), 1 μL 20× target primers/probe mix (FAM), 1 μL 20× reference primers/probe mix, 1 μL (5U) Hind111 restriction enzyme (New England Biolabs, Ipswich, MA, USA), and 1 μL DNA sample at 20 ng/μL. The mixture was loaded into a DG8 cartridge (Bio-Rad) together with 70 μL of droplet generation oil (Bio-Rad) and covered with a DG8 gasket. After processing the droplets in the droplet generator, the samples were transferred to a 96-well PCR plate. PCR amplification was carried out in a T11 Touch thermal cycler (Bio-Rad). The cycling protocol was as follows: 95 °C for 10 min, 40 cycles of 94 °C for 30 s and 60 °C for 1 min followed by an infinite 15-degree hold. After PCR, the plate was loaded on the QX200 droplet reader (Bio-Rad). Data were analyzed using QuantaSoft Analysis Pro software Version 1.2 (Bio-Rad).
3. Results
3.1. The Clinical Description of the Affected Patient Is Presented in This Section
The female index case was born to healthy Caribbean parents after an uneventful pregnancy of 37.5 weeks. She had a birth weight of 3200 g (50th centile), length of 51 cm (85th centile), and head circumference of 32.5 cm (10th centile). On the second day of life, she was admitted to the neonatology ward due to cyanosis with a heart rate of 125/min, respiratory rate of 40/min, and oxygen saturation of 84%. Echocardiography revealed an Ebstein anomaly with an atrial septal defect, hypoplastic right ventricle, and persistent left superior vena cava. Treatment with prostaglandin E2 and nasal continuous positive airway pressure was started. She was then referred to a tertiary pediatric heart center in Colombia for surgery.
The patient underwent a Starnes procedure, atrio-septostomy, closure of the pulmonary valve, and placement of a 3.5 mm Blalock–Taussig shunt. She experienced postoperative complications, including renal failure and paralysis of the diaphragm. At the age of one year, she had a follow-up surgery consisting of a bidirectional Glenn shunt. She suffered from bronchiolitis, pneumonia, and asthma and required a gastrostomy tube for feeding. At the age of 9 months, she was examined by a clinical geneticist. At that time, her height was 65 cm (2nd centile), weight was 6820 g (15th centile), and head circumference was 42 cm (15th centile). Dysmorphological examination showed hypertelorism, mid face hypoplasia, long philtrum, uplifted earlobes, and an anteriorly placed anus (Figure 1). An abdominal ultrasound was performed at the age of 10 months to exclude additional organ abnormalities.

Figure 1.
Photograph of the index patient at four years of age. Hypertelorism, long flat philtrum, and mid face hypoplasia can be recognized.
At the age of 4 years, she developed severe cyanosis caused by an aorta-pulmonary collateral, which was closed by intervention. Because of severe pulmonary hypertension, completion of Fontan circulation was not feasible. She had divergent eyes, a difference in size of the globe, and a right nasolacrimal duct stenosis. She also had delayed motor and speech development and developed convulsions at the age of one year. EEG showed occipital epileptic activity for which anti-epileptic therapy was started.
Because of left-sided hypotonia at the age of 2 years, a CT of the brain was performed, which showed no abnormalities. This has resolved spontaneously.
3.2. Molecular and Cytogenetic Studies
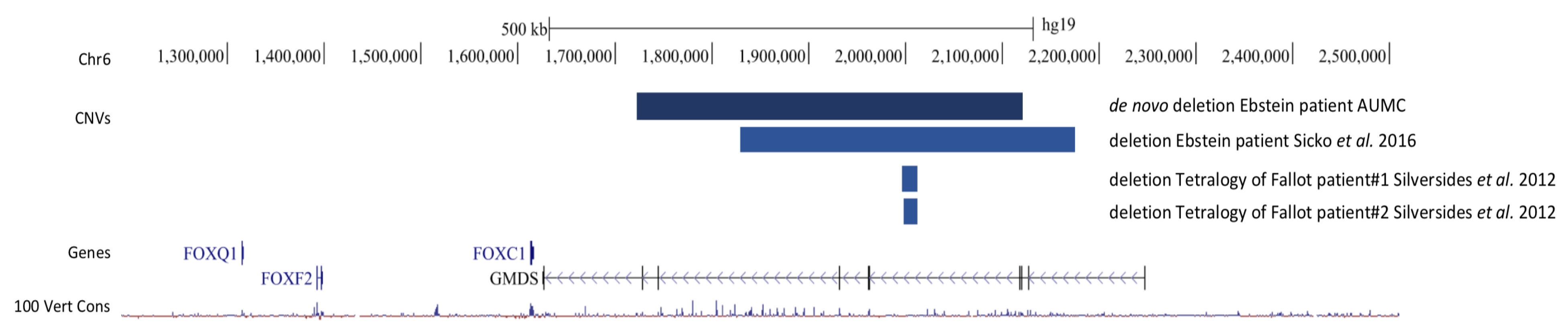
An array-CGH was performed. The Agilent Bench Lab CNV Version 5.1 180 K array-CGH showed a de novo deletion on chromosome 6p25.3 of ~403 kb (Figure 2) and a maternally inherited duplication in Xq27.2 of ~316 kb (arr [GRCh37] 6p25.3(1727928_2131157) x1 dn, Xq27.2(140693307_141009050) x3 mat, in accordance with the ISCN 2020 nomenclature [18]. No (likely) pathogenic variants were identified in the NGS gene panel.
Figure 2.
GMDS genomic locus (hg19), demonstrating the location of surrounding genes and the location of both the de novo deletion from the index patient and the previously published GMDS deletion by Sicko et al. [6] and Silversides et al. [19].
3.3. Genetic Investigations in Large Ebstein Anomaly Cohort
Genetic investigations in 129 Ebstein cases from the CONCOR data revealed no additional deletions or duplications.
3.4. Genetic Investigations in Caribbean Ebstein Cohort
In the five Caribbean cases with Ebstein anomaly, SNP arrays were performed, but none of them showed a 6p25.3 deletion. One patient had a 16q23.1 deletion, but unfortunately, her parents refused testing, and the other patients all had normal SNP array results.
4. Discussion
We report a patient with Ebstein anomaly, a rare, heterogeneous congenital heart defect with largely unknown etiology. Although Ebstein anomaly has been associated with pathogenic variants in a handful of genes and various copy number variants, these account for only a small proportion of cases [4,11,12,13]. We demonstrate here that the index patient has a large, intragenic, and de novo deletion in GMDS that is likely associated with the patient’s phenotype. GMDS encodes a short-chain mannose dehydrogenase protein (GDP-mannose 4,6-dehydratase) that catalyzes the first step in a molecular process called fucosylation, which has a function in many processes important in development [20]. GMDS is a key player in fucosylation as it is the rate-limiting enzyme [20]. Although no pathogenic human single nucleotide variations have been reported for GMDS, a case with Ebstein anomaly and a comparable large intragenic GMDS deletion has been recently reported [6]. The inheritance of that deletion was not reported. Both these large intragenic deletions are predicted to lead to loss-of-function of GMDS as they remove a large part of the GMDS coding region. In addition, two patients with Tetralogy of Fallot (TOF), a rare congenital heart disease, have been described to harbor a smaller deletion (of unknown inheritance) in the same region as the two Ebstein patients [19] (see Figure 2). These TOF-associated deletions, however, do not delete any GMDS coding parts, making it difficult to predict their effect. Nonetheless, based on our results coupled with the cases described above, we hypothesize that GMDS, or the GMDS locus, is important for normal (cardiac) development. Animal experiments corroborate this as GMDS knockout mice have an abnormal cranium and snout morphology [21], while Song et al. demonstrated that a GMDS missense variant in zebrafish results in disturbed neural development and reduced Notch signaling (see below) [22]. Together, this indicates that GMDS or its products have a role in normal development. One possible mechanism by which GMDS might be involved in development comes from its role as a major player in protein glycosylation (specifically fucosylating). It is known that protein glycosylation regulates various functions and physicochemical properties and that it plays a critical role in maintaining homeostasis. However, alterations of glycosylation are associated with the development and aggravation of many diseases [23]. This raises the possibility that altered glycosylation could lead to congenital heart disease as observed in our patient and the other three reported intragenic GMDS deletion patients. A possible link between congenital heart disease and altered glycosylation might be that a group of key proteins in (cardiac) development, the Notch proteins, are actually fucosylated [24]. Indeed, reduced fucose levels result in decreased Notch1 activation [23,24], a key player in cardiac development [25,26].
The importance of Notch1 in cardiac development is underscored by the fact that it is one of the most frequently mutated genes in patients with congenital heart disease, and that Notch1 KO mice demonstrate a plethora of congenital heart disease phenotypes [26]. One hypothesis could therefore be that GMDS haploinsufficiency leads to decreased GDP-fucose production, which in turn affects fucosylation of Notch1, thereby reducing its activity, resulting in cardiac anomalies. Alternatively, it is also possible that the intragenic deletions not only impact GMDS but also its nearest neighbor FOXC1, a forkhead transcription factor [27] located just 10 kb from the last GMDS exon. FOXC1 is an essential component of mesodermal [27] and neural crest development [27], both important for heart development [28,29]. While FOXC1 is not affected by any of the deletions directly, it is possible that disruption of conserved enhancer sequences within the GMDS locus also affects the regulation of (spatial-temporal) expression of FOXC1. FOXC1-knockout mice present with a variety of phenotypes, including congenital heart disease, and demonstrate abnormal valve development, which is part of the Ebstein anomaly, suggesting that altered expression of FOXC1 may cause developmental problems of the heart [29]. An additional possibility is that GMDS locus deletions have an impact on multiple neighboring genes and thereby cause the phenotype. Regardless, further investigation into the mechanism of how intragenic GMDS deletions can lead to disease is needed.
Given the link between GMDS and congenital heart disease, we collected a cohort of 134 Ebstein and Ebstein like cases, in which we investigated the GMDS locus for additional aberrations. No deletions or duplication were identified in this cohort, suggesting that GMDS intragenic aberrations are a relatively rare cause of Ebstein anomaly.
In addition to Ebstein anomaly, our index case also presented with seizures and dysmorphic facial features. This is in contrast to the other large GMDS intragenic deletion case, where the Ebstein anomaly was reported as an isolated condition [11]. However, as no additional clinical details were reported, it is possible that minor birth defects, such as dysmorphic features, and/or developmental delay were present in that patient. Alternatively, the difference in phenotype could also be caused by differences in genetic background and/or the difference in size and location of the GMDS intragenic deletions. With regard to the two cases with smaller GMDS deletions associated with tetralogy of Fallot [19,22], the patients in that study were grouped into syndromic vs. non-syndromic. However, it is unclear in which group these two cases with GMDS deletions fall. Taken together, there is a degree of phenotypic diversity with regard to the heart phenotype of GMDS intragenic deletion carriers, while the extent of extra-cardiac phenotypes is still unclear.
5. Conclusions
In summary, we report a patient with Ebstein anomaly with a de novo intragenic GMDS deletion. This locus has previously been sporadically associated with Ebstein anomaly and tetralogy of Fallot. We hypothesize that (large) deletions of this locus lead to loss of function of GMDS, which affects fucosylation, and in turn interferes with downstream developmental signaling molecules (e.g., Notch1) that are dependent on fucosylation for proper function. Given all the evidence, we conclude that GMDS intragenic deletions can be associated with rare cases of congenital heart disease.
Author Contributions
The first authors contributed equally: S.M.L.-A.-N. and E.A.V.; Patient’s Clinical Care and Follow-up: S.M.L.-A.-N. and E.A.; Conceptualization: S.M.L.-A.-N., E.A.V., M.M.v.H., A.V.P. and J.P.v.T.; Data curation: E.A.V., M.M.v.H., A.V.P., L.T.v.d.V. and J.P.v.T.; Funding Acquisition: not applicable; Project Administration: S.M.L.-A.-N., E.A.V. and M.M.v.H.; Writing; S.M.L.-A.-N., E.A.V., M.M.v.H., A.V.P. and J.P.v.T.; Review and editing: all the authors. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Under Dutch law, assessment of the study protocol by our ethics committee was not indicated since only genetic and clinical data collected during regular patient care were used. For Dutch research involving CONCOR-data, this is explained on their website https://concor.net/en/aboutconcor/methodology.html (accessed on 1 June 2022).
Informed Consent Statement
The parents provided written consent for research use of their data. For Dutch research involving CONCOR-data, this is explained in https://pubmed.ncbi.nlm.nih.gov/16121765/ and on their website https://concor.net/en/aboutconcor/methodology.html (accessed on 1 June 2022).
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy reasons.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Attenhofer Jost, C.; Connolly, H.; Dearani, J.; Edwards, W.; Danielson, G. Ebstein’s Anomaly. Circulation 2007, 115, 227–285. [Google Scholar] [CrossRef]
- Correa-Villasenor, A.; Ferencz, C.; Neill, C.A.; Wilson, P.D.; Boughman, J.A. Ebstein’s malformation of the tricuspid valve: Genetic and environmental factors. The Baltimore-Washington Infant Study Group. Teratology 1994, 50, 137–147. [Google Scholar] [CrossRef]
- Lupo, P.J.; Langlois, P.H.; Mitchell, L.E. Epidemiology of Ebstein anomaly: Prevalence and patterns in Texas, 1999–2005. Am. J. Med. Genet. Part A 2011, 155, 1007–1014. [Google Scholar] [CrossRef]
- Pradat, P.; Francannet, C.; Harris, J.; Robert, E. The epidemiology of cardiovascular defects, part I: A study based on data from three large registries of congenital malformations. Pediatr. Cardiol. 2003, 24, 195–221. [Google Scholar] [CrossRef] [PubMed]
- Boyle, B.; Garne, E.; Loane, M.; Addor, M.-C.; Arriola, L.; Cavero-Carbonell, C.; Gatt, M.; Lelong, N.; Lynch, C.; Nelen, V.; et al. The changing epidemiology of Ebstein’s anomaly and its relationship with maternal mental health conditions: A European registry-based study. Cardiol. Young 2017, 27, 677–685. [Google Scholar] [CrossRef]
- Sicko, R.J.; Browne, M.L.; Rigler, S.L.; Druschel, C.M.; Liu, G.; Fan, R.; Romitti, P.A.; Caggana, M.; Kay, D.M.; Brody, L.C.; et al. Genetic Variants in Isolated Ebstein Anomaly Implicated in Myocardial Development Pathways. PLoS ONE 2016, 11, e0165174. [Google Scholar] [CrossRef] [PubMed]
- Yuan, S.M. Ebstein’s Anomaly: Genetics, Clinical Manifestations, and Management. Pediatr. Neurol. 2017, 58, 211–215. [Google Scholar] [CrossRef]
- Fesslova, V.; Brankovic, J.; Lalatta, F.; Villa, L.; Meli, V.; Piazza, L.; Ricci, C. Recurrence of congenital heart disease in cases with familial risk screened prenatally by echocardiography. J. Pregnancy 2011, 2011, 368067. [Google Scholar] [CrossRef] [PubMed]
- Hirono, K.; Hata, Y.; Ibuki, K.; Yoshimura, N. Familial Ebstein’s anomaly, left ventricular noncompaction, and ventricular septal defect associated with an MYH7 mutation. J. Thorac. Cardiovasc. 2014, 148, e223–e226. [Google Scholar] [CrossRef]
- Siehr, S.; Punn, R.; Priest, J.; Lowenthal, A. Ebstein anomaly and Trisomy 21: A rare association. Ann. Pediatr. Cardiol. 2014, 7, 67–69. [Google Scholar] [CrossRef]
- Pierpont, M.E.; Basson, C.T.; Benson, D.W., Jr.; Gelb, B.D.; Giglia, T.M.; Goldmuntz, E.; McGee, G.; Sable, D.A.; Srivastava, D.; Webb, C.L. Genetic Basis for Congenital Heart Defects: A Scientific Statement from the American Heart Association Congenital Cardiac Defects Committee, Council on Cardiovascular Disease in the Young. Circulation 2007, 115, 3015–3038. [Google Scholar] [CrossRef] [PubMed]
- Vanderhauwaert, L.G.; Fryns, J.P.; Dumoulin, M.; Logghe, N. Cardiovascular malformations in Turner’s and Noonan’s syn-drome. BHJ 1978, 40, 500–509. [Google Scholar] [CrossRef] [PubMed]
- Digilio, M.C.; Bernardini, L.; Lepri, F.R.; Giuffrida, M.G.; Guida, V.; Baban, A.; Versacci, P.; Capolino, R.; Torres, B.; De Luca, A.; et al. Ebstein anomaly: Genetic heterogeneity and association with microdeletions 1p36 and 8p23.1. Am. J. Med. Genet. Part A 2011, 155, 2196–2202. [Google Scholar] [CrossRef]
- Giannakou, A.; Sicko, R.J.; Zhang, W.; Romitti, P.; Browne, M.L.; Caggana, M.; Brody, L.C.; Jelliffe-Pawlowski, L.; Shaw, G.M.; Kay, D.M.; et al. Copy number variants in Ebstein anomaly. PLoS ONE 2017, 12, e0188168. [Google Scholar] [CrossRef] [PubMed]
- Postma, A.V.; van Engelen, K.; van de Meerakker, J.; Rahman, T.; Probst, S.; Baars, M.J.; Bauer, U.; Pickardt, T.; Sperling, S.R.; Berger, F.; et al. Mutations in the Sarcomere Gene MYH7 in Ebstein Anomaly. Circ. Cardiovasc. Genet. 2011, 4, 43–50. [Google Scholar] [CrossRef] [PubMed]
- Vander Velde, E.; Vriend, J.W.J.; Mannens, M.; Uiterwaal, C.; Brand, R.; Mulder, B.J.M. NEW STUDY CONCOR, an initiative towards a national registry and DNA-bank of patients with congenital heart disease in the Netherlands- Rationale, design, and first results. Eur. J. Epidemiol. 2005, 20, 549–557. [Google Scholar] [CrossRef]
- Available online: https://concor.net/en/aboutconcor/methodology.html (accessed on 27 December 2022).
- Chen, G.; Yu, X.; Zhang, M.; Zheng, A.; Wang, Z.; Zuo, Y.; Liang, Q.; Jiang, D.; Chen, Y.; Zhao, L.; et al. Inhibition of Euchromatic Histone Lysine Methyltransferase 2 (EHMT2) Suppresses the Proliferation and Invasion of Cervical Cancer Cells. Cytogenet. Genome Res. 2019, 158, 205–212. [Google Scholar] [CrossRef]
- Silversides, C.K.; Lionel, A.C.; Costain, G.; Merico, D.; Migita, O.; Liu, B.; Yuen, T.; Rickaby, J.; Thiruvahindrapuram, B.; Marshall, C.R.; et al. Rare Copy Number Variations in Adults with Tetralogy of Fallot Implicate Novel Risk Gene Pathways. PLOS Genet. 2012, 8, e1002843. [Google Scholar] [CrossRef]
- Becker, D.J.; Lowe, J.B. Fucose: Biosynthesis and biological function in mammals. Glycobiology 2003, 13, 41R–53R. [Google Scholar] [CrossRef]
- Available online: http://www.informatics.jax.org/allele/MGI:4363597 (accessed on 1 June 2022).
- Song, Y.; Willer, J.R.; Scherer, P.C.; Panzer, J.A.; Kugath, A.; Skordalakes, E.; Gregg, R.G.; Willer, G.B.; Balice-Gordon, R.J. Neural and synaptic defects in slytherin, a zebrafish model for human congenital disorders of glycosylation. PLoS ONE 2010, 5, e13743. [Google Scholar] [CrossRef]
- Moloney, D.J.; Panin, V.M.; Johnston, S.H.; Chen, J.; Shao, L.; Wilson, R.; Wang, Y.; Stanley, P.; Irvine, K.D.; Haltiwanger, R.S.; et al. Fringe is a glycosyltransferase that modifies Notch. Nature 2000, 406, 369–375. [Google Scholar] [CrossRef] [PubMed]
- MacGrogan, D.; Luna-Zurita, L.; de la Pompa, J.L. Notch Signaling in Cardiac Valve Development and Disease. Birth Defects Res. Part A Clin. Mol. Teratol. 2011, 91, 449–459. [Google Scholar] [CrossRef]
- Niessen, K.; Karsan, A. Notch signaling in cardiac development. Circ. Res. 2008, 102, 1169–1181. [Google Scholar] [CrossRef] [PubMed]
- Fahed, A.C.; Gelb, B.D.; Seidman, J.G.; Seidman, C.E. Genetics of Congenital Heart Disease. The Glass Half Empty. Circ. Res. 2013, 112, 707–720. [Google Scholar] [CrossRef] [PubMed]
- George, R.M.; Maldonado-Velez, G.; Firulli, A.B. The heart of the neural crest: Cardiac neural crest cells in development and regeneration. Development 2020, 147, dev188706. [Google Scholar] [CrossRef] [PubMed]
- Hong, H.K.; Lass, J.H.; Chakravarti, A. Pleiotropic skeletal and ocular phenotypes of the mouse mutation congenital hydro-cephalus (ch/Mf1) arise from a winged helix/forkhead transcriptionfactor gene. Hum. Mol. Genet. 1999, 8, 625–637. [Google Scholar] [CrossRef]
- Seo, S.; Kume, T. Forkhead transcription factors, Foxc1 and Foxc2, are required for the morphogenesis of the cardiac outflow tract. Dev. Biol. 2006, 296, 421–436. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).