Examining State Policies and Administrative Factors as Determinants of Consumer-Reported Unmet Service Needs in Publicly Funded Home- and Community-Based Services in the United States
Abstract
1. Introduction
2. Methods
2.1. Data Source and Survey Methods
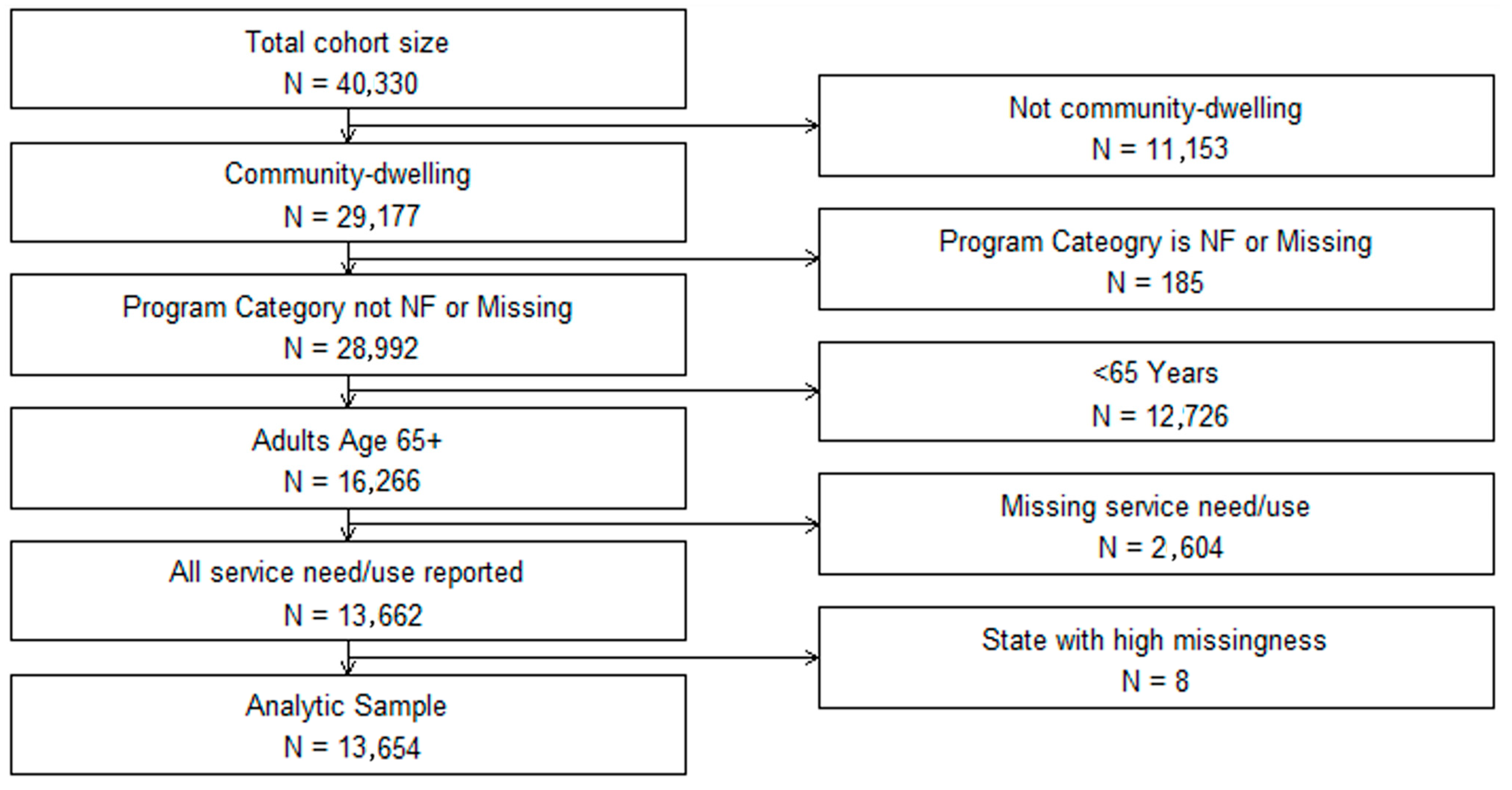
2.2. Study Population
2.3. Dependent Variable: Unmet HCBS Needs
2.4. Independent Variable: State-Level Factors
2.5. Independent Variable: Consumer-Level Factors
2.6. Statistical Analyses
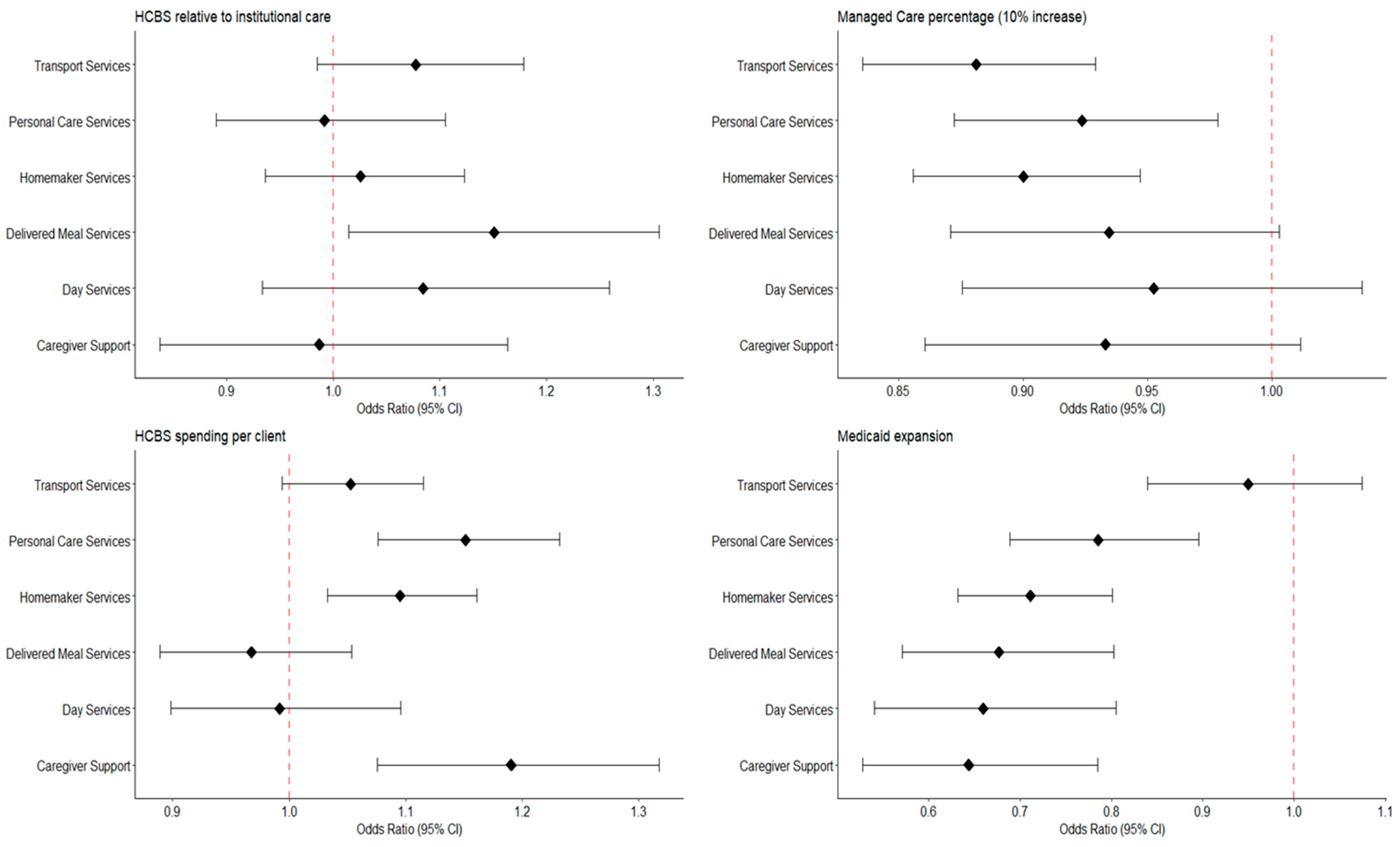
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mann, D.R.; Ross, J.; Wysocki, A. Medicaid Section 1915(c) Waiver Programs Annual Expenditures and Beneficiaries Report: Analysis of CMS 372 Annual Reports, 2018–2019; Mathematica: Chicago, IL, USA, 2023. Available online: https://www.medicaid.gov/sites/default/files/2023-10/cms-372-report-2018-2019.pdf (accessed on 15 July 2024).
- Casado, B.L.; Lee, S.E. Access barriers to and unmet needs for home- and community-based services among older Korean Americans. Home Health Care Serv. Q. 2012, 31, 219–242. [Google Scholar] [CrossRef] [PubMed]
- Konetzka, R.T.; Jung, D.H.; Gorges, R.J.; Sanghavi, P. Outcomes of Medicaid home- and community-based long-term services relative to nursing home care among dual eligibles. Health Serv. Res. 2020, 55, 973–982. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Murray, C.; Eckstein, M.; Lipson, D.; Wysocki, A. Medicaid Long Term Services and Supports Annual Expenditures Report: Federal Fiscal Year 2020; Mathematica: Chicago, IL, USA, 2023. Available online: https://www.medicaid.gov/sites/default/files/2023-10/ltssexpenditures2020.pdf (accessed on 15 July 2024).
- Tyler, D.A.; Fennell, M.L. Rebalance Without the Balance: A Research Note on the Availability of Community-Based Services in Areas Where Nursing Homes Have Closed. Res. Aging. 2017, 39, 597–611. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Murray, C.; Tourtellotte, A.; Lipson, D.; Wysocki, A. Medicaid Long Term Services and Supports Annual Expenditures Report: Federal Fiscal Year 2019; Mathematica: Chicago, IL, USA, 2021. Available online: https://www.medicaid.gov/medicaid/long-term-services-supports/downloads/ltssexpenditures2019.pdf (accessed on 15 July 2024).
- Segelman, M.; Intrator, O.; Li, Y.; Mukamel, D.; Veazie, P.; Temkin-Greener, H. HCBS Spending and Nursing Home Admissions for 1915(c) Waiver Enrollees. J. Aging Soc. Policy 2017, 29, 395–412. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Temkin-Greener, H.; Simning, A.; Konetzka, R.T.; Cai, S. Medicaid home- and community-based services and discharge from skilled nursing facilities. Health Serv. Res. 2021, 56, 1156–1167. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wang, S.; Yan, D.; Temkin-Greener, H.; Cai, S. Nursing home admissions for persons with dementia: Role of home- and community-based services. Health Serv. Res. 2021, 56, 1168–1178. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cheng, Z.; Mutoniwase, E.; Cai, X.; Li, Y. Higher levels of state funding for Home- and Community-Based Services linked to better state performances in Long-Term Services and Supports. Health Serv. Res. 2024, 59, e14288. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- CMS Releases First-Ever Home- and Community-Based Services Quality Measure Set. Centers for Medicare & Medicaid Services. 2022. Available online: https://www.cms.gov/newsroom/press-releases/cms-releases-first-ever-home-and-community-based-services-quality-measure-set (accessed on 15 July 2024).
- Chong, N.; Akobirshoev, I.; Caldwell, J.; Kaye, H.S.; Mitra, M. The relationship between unmet need for home and community-based services and health and community living outcomes. Disabil. Health J. 2022, 15, 101222. [Google Scholar] [CrossRef]
- Li, Y.; Liu, X. The Effect of Home Care Poverty on the Activities of Daily Living among Older Adults in China: A Propensity Score Matching Study. Iran. J. Public Health. 2023, 52, 2325–2332. [Google Scholar] [CrossRef]
- Shippee, T.P.; Bucy, T.I.; Parikh, R.R.; Wolf, J.M.; Shewmaker, P.; Mulcahy, J.F.; Skarphol, T.; Giordano, S.; Isvan, N.; Jutkowitz, E. Service Utilization and Consumer-Reported Unmet Needs in Medicaid Home- and Community-Based Services for Older Adults. J. Aging Soc. Policy 2024, 16, 1–15. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Fabius, C.D.; Parikh, R.; Wolf, J.M.; Giordano, S.; Fashaw-Walters, S.; Jutkowitz, E.; Shippee, T. Racial and ethnic differences in unmet needs among older adults receiving publicly-funded home and community-based services. J. Am. Geriatr. Soc. 2024, 72, 3520–3529. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Shippee, T.P.; Duan, Y.; Baker, Z.G.; Parikh, R.; Bucy, T.; Jutkowitz, E. Measuring Consumer-Reported Quality of Life Among Recipients of Publicly Funded Home- and Community-Based Services: Implications for Health Equity. J. Aging Health 2024, 24, 8982643241267378. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bhaumik, D.; Wallace, J.; Grabowski, D.C.; Schlesinger, M.J. The Impact of Introducing Managed Care Intermediaries for Long-Term Services and Supports. Health Serv. Res. 2025, 60, e14462. [Google Scholar] [CrossRef] [PubMed]
- Arku, D.; Felix, M.; Warholak, T.; Axon, D.R. Program of All-Inclusive Care for the Elderly (PACE) versus Other Programs: A Scoping Review of Health Outcomes. Geriatrics 2022, 7, 31. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Keohane, L.M.; Zhou, Z.; Stevenson, D.G. Aligning Medicaid and Medicare Advantage Managed Care Plans for Dual-Eligible Beneficiaries. Med. Care Res. Rev. 2022, 79, 207–217. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mellor, J.; Cunningham, P.; Britton, E.; Walker, L. Use of Home and Community-Based Services After Implementation of Medicaid Managed Long Term Services and Supports in Virginia. J. Aging Soc. Policy 2024, 36, 1026–1044. [Google Scholar] [CrossRef] [PubMed]
- IPRO. Core Medicaid and MLTSS: External Quality Review Annual Technical Report; New Jersey Department of Human Services Division of Medical Assistance and Health Services: Trenton, NJ, USA, 2023. Available online: https://www.nj.gov/humanservices/dmahs/news/2023%20Core%20Medicaid-MLTSS%20Annual%20Technical%20Report.pdf (accessed on 24 June 2025).
- Arora, K.; Rochford, H.; Todd, K.; Kaskie, B. Medicaid managed care in Iowa: Experiences of older adults and people with disabilities. Disabil. Health J. 2021, 14, 100975. [Google Scholar] [CrossRef]
- Williamson, H.J.; Perkins, E.A.; Levin, B.L.; Baldwin, J.A.; Lulinski, A.; Armstrong, M.I.; Massey, O.T. Implementation of Medicaid Managed Long-Term Services and Supports for Adults With Intellectual and/or Developmental Disabilities in Kansas. Intellect. Dev. Disabil. 2017, 55, 84–96. [Google Scholar] [CrossRef] [PubMed]
- Kaye, H.S. Toward a model long-term services and supports system: State policy elements. Gerontologist 2014, 54, 754–761. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Waymouth, M.; Siconolfi, D.; Friedman, E.M.; Saliba, D.; Ahluwalia, S.C.; Shih, R.A. Barriers and Facilitators to Home- and Community-Based Services Access for Persons With Dementia and Their Caregivers. J. Gerontol. B Psychol. Sci. Soc. Sci. 2023, 78, 1085–1097. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sommers, B.D.; Arntson, E.; Kenney, G.M.; Epstein, A.M. Lessons from early Medicaid expansions under health reform: Interviews with Medicaid officials. Medicare Medicaid Res. Rev. 2013, 3, mmrr.003.04.a02. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Soni, A.; Griffith, K.N. The Protective Role of Medicaid Expansion for Low-Income People During the COVID-19 Pandemic. Health Serv. Res. 2025, 60 (Suppl. 2), e14444. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- McGarry, B.E.; Grabowski, D.C. Medicaid home and community-based services spending for older adults: Is there a “woodwork” effect? J. Am. Geriatr. Soc. 2023, 71, 3143–3151. [Google Scholar] [CrossRef] [PubMed]
- Muramatsu, N.; Campbell, R.T. State expenditures on home and community based services and use of formal and informal personal assistance: A multilevel analysis. J. Health Soc. Behav. 2002, 43, 107–124. [Google Scholar] [CrossRef] [PubMed]
- Muramatsu, N.; Yin, H.; Hedeker, D. Functional declines, social support, and mental health in the elderly: Does living in a state supportive of home and community-based services make a difference? Soc. Sci. Med. 2010, 70, 1050–1058. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yates, M.; Gonzalez-Smith, J.; Li, K.; Wang, A.; Saunders, R.R. Value-Based State-Directed Payments in Medicaid Managed Care. JAMA Health Forum. 2025, 6, e251666. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Damberg, C.L.; Sorbero, M.E.; Lovejoy, S.L.; Martsolf, G.R.; Raaen, L.; Mandel, D. Measuring Success in Health Care Value-Based Purchasing Programs: Findings from an Environmental Scan, Literature Review, and Expert Panel Discussions. Rand Health Q. 2014, 4, 9. [Google Scholar] [PubMed] [PubMed Central]
- Yang, Y.; Lee, A.R.; Rapp, T.; Chen, R.; Glymour, M.M.; Torres, J.M. State home and community-based services expenditures and unmet care needs in the United States: Has everyone benefitted equally? Health Serv. Res. 2024, 59, e14269. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Miller, K.E.M.; Thunell, J. The critical role of Medicaid home- and community-based services in meeting the needs of older adults in the United States. Health Serv. Res. 2024, 59, e14290. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
| Feature | Program of All-Inclusive Care for the Elderly (PACE) | Older Americans Act (OAA) | Managed Long-Term Services and Supports (Managed LTSS) | Medicaid Waiver LTSS (e.g., HCBS Waivers) |
|---|---|---|---|---|
| Program Type | A comprehensive, all-in-one healthcare program that combines medical and long-term care services into a single coordinated system. Example: InnovAge and Johns Hopkins ElderPlus. | A framework for discretionary grants that provides funding to states and communities for a wide range of social services for older adults. Example: Title III nutrition and caregiver programs managed by Area Agencies on Aging (AAAs). | A Medicaid-funded program in which states have a contract with managed care organizations (MCOs) to deliver long-term services and supports through a capitated payment system. Example: Arizona Long Term Care System (ALTCS). | A Medicaid option that allows states to waive certain federal requirements (e.g., institutional care mandates) in order to provide long-term services and support in home- and community-based settings. Example: New York’s OPWDD 1915(c) waiver for individuals with developmental disabilities. |
| Eligibility | Specific and strict. Participants must be at least 55 years old, certified by their state as needing a nursing home level of care, and able to live safely in the community at the time of enrollment. Example: PACE enrollment criteria require nursing-home level certification. | Broad. Services are generally available to people aged 60 and older, with a focus on those with the greatest economic or social need. Example: Meals on Wheels prioritizes homebound seniors with limited income or support. | Varies by state, but typically available to Medicaid-eligible individuals who need nursing home level of care and enroll in a managed care plan. Example: Florida Managed Medical Assistance LTC program serves Medicaid beneficiaries needing institutional-level care. | Varies by waiver and state. Typically limited to individuals who meet Medicaid income requirements and have a nursing home level of care need, but who can be served safely in the community. Example: California’s HCBS waiver for adults with disabilities and frail elders. |
| Funding | A managed care plan funded by fixed capitated payments from Medicare and Medicaid. The PACE provider receives a set amount per participant and is responsible for all their health and long-term care needs. Example: Dual-eligible PACE participants receive joint Medicare–Medicaid funding. | Funded through discretionary appropriations from Congress. The money is distributed to states and AAAs, which contract with local service providers. Example: Title III-B funds support transportation services through community nonprofits. | States receive federal Medicaid matching funds and pay MCOs a capitated rate to manage and deliver LTSS. Example: Texas STAR + PLUS uses capitated payments to MCOs for LTSS delivery. | Jointly funded by state and federal Medicaid dollars through Section 1915(c) or other waivers. Example: Wisconsin Family Care waiver funded with blended state and federal Medicaid dollars. |
| Service Delivery | An interdisciplinary team coordinates and provides all necessary medical and social services through a single PACE center. Services include adult day care, primary care, home care, and transportation. Example: PACE day health centers integrating clinic, therapy, and meals. | Community-based programs. Services are delivered by a network of providers, typically managed by AAAs, and are not necessarily integrated under a single entity. Example: Congregate meal programs run through senior centers. | Services are delivered through contracted provider networks managed by MCOs. Care coordination is typically required, but integration varies by state and plan. Example: MCO care coordinators in New Jersey’s Managed LTSS oversee both medical and support services. | Services are delivered through approved community-based providers. States have flexibility in designing benefits and provider networks, but services are not necessarily integrated. Example: Home health agencies delivering waiver-funded personal assistance. |
| Scope of Services | All-inclusive. Covers a full continuum of medical and support services, including hospital care, prescriptions, and long-term care, to keep participants independent for as long as possible. Example: PACE covers hospitalizations, medications, and LTSS under one plan. | Provides grants for specific programs, such as congregate and home-delivered meals, transportation, and caregiver support. It does not cover a participant’s full medical care like PACE does. Example: Title III-C funding supports Meals on Wheels programs. | Broader than OAA, narrower than PACE. Includes LTSS such as personal care, home modifications, and sometimes integrated medical care, depending on the state. Example: Minnesota’s MLTSS programs integrate acute and LTSS under MCOs. | Focused on LTSS, particularly home- and community-based services such as personal assistance, respite care, habilitation, adult day health, and case management. Does not usually cover all medical services. Example: Colorado’s HCBS waiver funds respite and habilitation services but not hospital care. |
| Focus | Keeping frail, high-need older adults who would otherwise require a nursing home in their community. A strong emphasis is placed on preventive care to reduce hospitalizations. Example: PACE prevents nursing home placement for dual-eligibles. | Supporting the health, independence, and well-being of older adults through a variety of social services. Example: OAA-funded transportation helps older adults maintain independence. | Promoting cost-effective care delivery and better outcomes by shifting LTSS into managed care arrangements, with a focus on integration, efficiency, and quality oversight. Example: Tennessee’s CHOICES program emphasizes cost savings and care integration. | Expanding access to community-based alternatives to institutional care, with emphasis on flexibility, consumer choice, and supporting individuals in the least restrictive setting possible. Example: HCBS waivers reduce nursing home use by funding in-home supports. |
| Characteristic | N = 13,654 1 |
|---|---|
| State-Level Factors | |
| HCBS spending relative to institutional care spending (ratio) | 1.24 (0.90, 2.03) |
| Percentage of Medicaid beneficiaries in managed care | 0.84 (0.80, 0.95) |
| Average HCBS spending per client | $18,500 ($12,600, $28,300) |
| Medicaid expansion | 7758 (57%) |
| Consumer-Level Factors | |
| Age (years; median [IQR]) | 77 (71, 84) |
| Female (vs. not Female) | 9791 (72%) |
| ADRD diagnosis | 2059 (17%) |
| Physical Disability | 6995 (58%) |
| Developmental Disability | 1088 (9%) |
| Brain Injury | 1455 (12%) |
| Mental Health Condition | 2634 (20%) |
| Multiple Chronic Conditions | 3500 (26%) |
| Funding Program | |
| Medicaid-A&D Waiver | 4008 (29%) |
| Managed LTSS | 4507 (33%) |
| PACE | 621 (5%) |
| OAA | 3386 (25%) |
| Other | 1132 (8%) |
| Medicare Enrollee | 11,093 (91%) |
| Have Legal Guardian | 1141 (10%) |
| Marital Status | |
| Single | 1567 (13%) |
| Married/Domestic Partner | 2570 (21%) |
| Separated/Divorced | 3053 (25%) |
| Widowed | 4985 (41%) |
| ZIP Code RUCA Classification | |
| Metropolitan | 9669 (72%) |
| Micropolitan | 2065 (15%) |
| Rural | 658 (5%) |
| Small town | 1085 (8%) |
| Living Arrangement | |
| Alone | 6569 (53%) |
| Family | 5305 (43%) |
| Other | 602 (5%) |
| Race/Ethnicity | |
| White | 7931 (60%) |
| Black or African-American | 3025 (23%) |
| Hispanic or Latino | 1347 (10%) |
| Other/Multiracial/Multiethnic | 930 (7%) |
| Overall Health | |
| Poor | 2501 (19%) |
| Fair | 5236 (39%) |
| Good | 4075 (30%) |
| Very Good | 1344 (10%) |
| Excellent | 334 (2%) |
| Proxy | 1780 (13%) |
| Service Use | |
| Personal Care Services | 6491 (48%) |
| Homemaker Services | 2961 (22%) |
| Delivered Meal Services | 4157 (30%) |
| Day Services | 1051 (7.7%) |
| Transport Services | 1075 (7.9%) |
| Caregiver Support | 757 (5.5%) |
| Characteristic | Logistic Model |
|---|---|
| Adjusted Odds Ratio (95% CI) | |
| State-Level Factors | |
| HCBS spending relative to institutional care spending | 1.19 (1.11, 1.28) *** |
| Percentage of Medicaid beneficiaries in managed care (per 10% increase) | 0.92 (0.89, 0.96) *** |
| HCBS spending per client | 1.00 (0.96, 1.05) |
| Medicaid expansion | 0.80 (0.73, 0.87) *** |
| Consumer-Level Factors | |
| Funding Program | |
| Medicaid-A&D waiver | referent |
| Managed LTSS | 0.67 (0.61, 0.74) *** |
| OAA | 1.11 (1.00, 1.24) |
| PACE | 0.39 (0.31, 0.49) *** |
| Other | 0.91 (0.78, 1.06) |
| Female (vs. not Female) | 1.00 (0.92, 1.09) |
| Marital Status | |
| Single | referent |
| Married/Domestic Partner | 0.97 (0.83, 1.13) |
| Separated/Divorced | 1.21 (1.06, 1.38) ** |
| Widowed | 0.99 (0.87, 1.13) |
| ZIP Code RUCA Classification | |
| Metropolitan | referent |
| Micropolitan | 0.80 (0.71, 0.89) *** |
| Rural | 0.73 (0.61, 0.88) ** |
| Small town | 0.87 (0.75, 1.00) |
| Living Arrangement | |
| Alone | referent |
| Family | 1.03 (0.93, 1.14) |
| Other | 0.77 (0.64, 0.94) ** |
| Race/Ethnicity | |
| White | referent |
| Black or African-American | 1.06 (0.96, 1.18) |
| Hispanic or Latino | 1.15 (1.00, 1.33) |
| Other/Multiracial/Multiethnic | 1.36 (1.16, 1.59) *** |
| Overall Health | |
| Poor | referent |
| Fair | 0.67 (0.61, 0.75) *** |
| Good | 0.48 (0.43, 0.54) *** |
| Very Good | 0.40 (0.34, 0.46) *** |
| Excellent | 0.32 (0.24, 0.43) *** |
| Medicare Enrollee (yes vs. no) | 1.40 (1.21, 1.62) *** |
| Have Legal Guardian (yes vs. no) | 0.90 (0.76, 1.05) |
| ADRD diagnosis (yes vs. no) | 1.13 (1.01, 1.28) * |
| Physical Disability (yes vs. no) | 1.12 (1.03, 1.22) ** |
| Developmental Disability (yes vs. no) | 0.95 (0.79, 1.15) |
| Brain Injury (yes vs. no) | 1.16 (0.99, 1.37) |
| Mental Health Condition (yes vs. no) | 1.39 (1.27, 1.53) *** |
| Proxy (yes vs. no) | 0.99 (0.87, 1.12) |
| Characteristic | GEE Model |
|---|---|
| Adjusted Odds Ratio (95% CI) | |
| State-level factors | |
| HCBS relative to institutional care | 1.19 (0.85, 1.69) |
| Percentage of Medicaid beneficiaries in managed care (10% increase) | 0.92 (0.79, 1.08) |
| HCBS spending per client | 1.00 (0.81, 1.23) |
| Medicaid expansion | 0.80 (0.54, 1.19) |
| Administrative Factor- Funding Program | |
| Medicaid-A&D waiver | referent |
| Managed LTSS | 0.67 (0.47, 0.96) * |
| OAA | 1.11 (0.72, 1.70) |
| PACE | 0.39 (0.27, 0.57) *** |
| Other Programs | 0.91 (0.61, 1.36) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Market Access Society. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Parikh, R.R.; Shippee, T.P.; Langworthy, B.; Wang, Z.; Giordano, S.; Jutkowitz, E. Examining State Policies and Administrative Factors as Determinants of Consumer-Reported Unmet Service Needs in Publicly Funded Home- and Community-Based Services in the United States. J. Mark. Access Health Policy 2025, 13, 51. https://doi.org/10.3390/jmahp13040051
Parikh RR, Shippee TP, Langworthy B, Wang Z, Giordano S, Jutkowitz E. Examining State Policies and Administrative Factors as Determinants of Consumer-Reported Unmet Service Needs in Publicly Funded Home- and Community-Based Services in the United States. Journal of Market Access & Health Policy. 2025; 13(4):51. https://doi.org/10.3390/jmahp13040051
Chicago/Turabian StyleParikh, Romil R., Tetyana P. Shippee, Benjamin Langworthy, Zheng Wang, Stephanie Giordano, and Eric Jutkowitz. 2025. "Examining State Policies and Administrative Factors as Determinants of Consumer-Reported Unmet Service Needs in Publicly Funded Home- and Community-Based Services in the United States" Journal of Market Access & Health Policy 13, no. 4: 51. https://doi.org/10.3390/jmahp13040051
APA StyleParikh, R. R., Shippee, T. P., Langworthy, B., Wang, Z., Giordano, S., & Jutkowitz, E. (2025). Examining State Policies and Administrative Factors as Determinants of Consumer-Reported Unmet Service Needs in Publicly Funded Home- and Community-Based Services in the United States. Journal of Market Access & Health Policy, 13(4), 51. https://doi.org/10.3390/jmahp13040051






