Abstract
With the increasing pipeline of cell and gene therapies (CGTs) and the expected surge in the number of approvals, understanding the market access landscape becomes crucial for timely patient access. This study evaluates the challenges Dutch stakeholders encounter in CGT market access, offering insights for improving time-to-patient access. A traditional literature review was conducted to identify market access challenges and solutions for CGTs. Based on the findings, participants for semi-structured interviews, designed using an interview guide adapted to the Dutch context, were selected to capture diverse perspectives on market access. This review included 124 relevant articles out of 2449, covering several aspects of market access of CGTs. Subsequently, interviews with 16 stakeholders from academia, patient advocacy groups, manufacturers, health insurers, payers, hospital pharmacists, healthcare practitioners, and the Association of Innovative Medicines were conducted. Stakeholders identified challenges and proposed solutions for reimbursement package management, clinical trials, health economics, payment models, and procedural and organisational aspects. Thematic analysis revealed unique country-specific challenges and solutions in the Netherlands. This research provides insights into these challenges and potential solutions, emphasising the need for collaborative efforts among stakeholders to develop practical and multidisciplinary measures to improve the market access landscape for CGTs in the country.
1. Introduction
Despite the surge in the availability of cell and gene therapies (CGTs) over the past two decades, only a limited number of CGTs received reimbursement shortly after European Medicines Agency (EMA) approval. Nevertheless, considering a growing pipeline of products in clinical trials, the number of these approvals is anticipated to increase in the near future as up to 21 cell therapy launches and 31 gene therapy launches are expected by 2024 [1,2]. The main challenges for the market access procedure in Europe are due to differences between regulatory and reimbursement assessments along with the unique nature of CGTs and include dealing with limited patient populations, conducting long-term clinical effectiveness and safety evaluation, managing differences in assessment frameworks among countries, determining the value of health outcomes, estimating costs, selecting appropriate discount rates, incorporating equity considerations, and addressing affordability [3,4,5,6,7,8,9]. These issues are discussed in the international literature, which also offers recommendations on how the guidelines on economic evaluation methodology need to be adapted to assess CGTs [3,7,9,10,11,12,13,14]. Several health technology assessment (HTA) agencies have adapted their guidelines to address challenges specifically associated with CGTs, recommending increasing thresholds for severe diseases (Sweden and Norway), adding disease severity measurement through quality-adjusted life years (QALYs) shortfall (the U.K.), and introducing cure models with conservative and optimistic scenarios and durability of effect threshold analyses (Institute for Clinical and Economic Review in the U.S.) [15,16,17,18].
As the number of market access and reimbursement submissions for CGTs grows, stakeholders, including HTA bodies, payers, insurers, and healthcare professionals, face increased pressure to assess these innovative treatments. The variations in regulatory landscapes across different countries underscore the importance of mapping the opportunities and difficulties associated with CGT assessments at the national level. In the Netherlands, for instance, 40% of new (orphan) drugs are not reimbursed. Of particular concern within this subset is the fact that around 70% of orphan drugs with conditional or exceptional registration fail to secure reimbursement [19]. Furthermore, the median duration from EMA registration to hospital availability consistently exceeds 300 days for all three categories including the following: orphan drugs, drugs subjected to restricted distribution, and those that underwent conditional or accelerated marketing authorisation procedures. In the Netherlands, this timeframe has shown an annual increase, signifying a continuous trend toward heightened scrutiny [20]. The Dutch approach differs from that of other European nations such as Germany, Denmark, the U.K., Austria, and Norway, where orphan drugs are more actively reimbursed [21]. The Netherlands serves as an example of a country with a stringent regulatory approach. This was further emphasised by the new Dutch cabinet, which, after assuming office in January 2022, announced that costly medicines (i.e., medicines with an annual expenditure of EUR 20 million or more for one or more new indications) will not receive automatic coverage. Instead, they will undergo assessment and potential price negotiations before inclusion in the insured package [22]. Additionally, compared with other countries, the availability of CGTs in the Netherlands remains limited, with treatments like Tecartus, Abecma, Carvykti, Skysona, Zynteglo, Casgevy, and Hemgenix not yet accessible to Dutch patients as of June 2024 [23,24,25,26]. Consequently, access to treatment options for patients with respective conditions such as multiple myeloma, mantle cell lymphoma, cerebral adrenoleukodystrophy, beta-thalassemia, sickle cell disease, and haemophilia B remains constrained.
The primary objective of comprehending the challenges and solutions in the Netherlands is to enhance the time-to-patient access. This study is specifically designed to evaluate the obstacles faced by Dutch stakeholders in the market access of CGTs, and insights gained from this research have the potential to benefit other countries grappling with similar issues in the gene therapy field. Ultimately, the research findings inform recommendations for enhancing time-to-patient access in the Netherlands and neighbouring European countries.
2. Materials and Methods
2.1. Literature Review
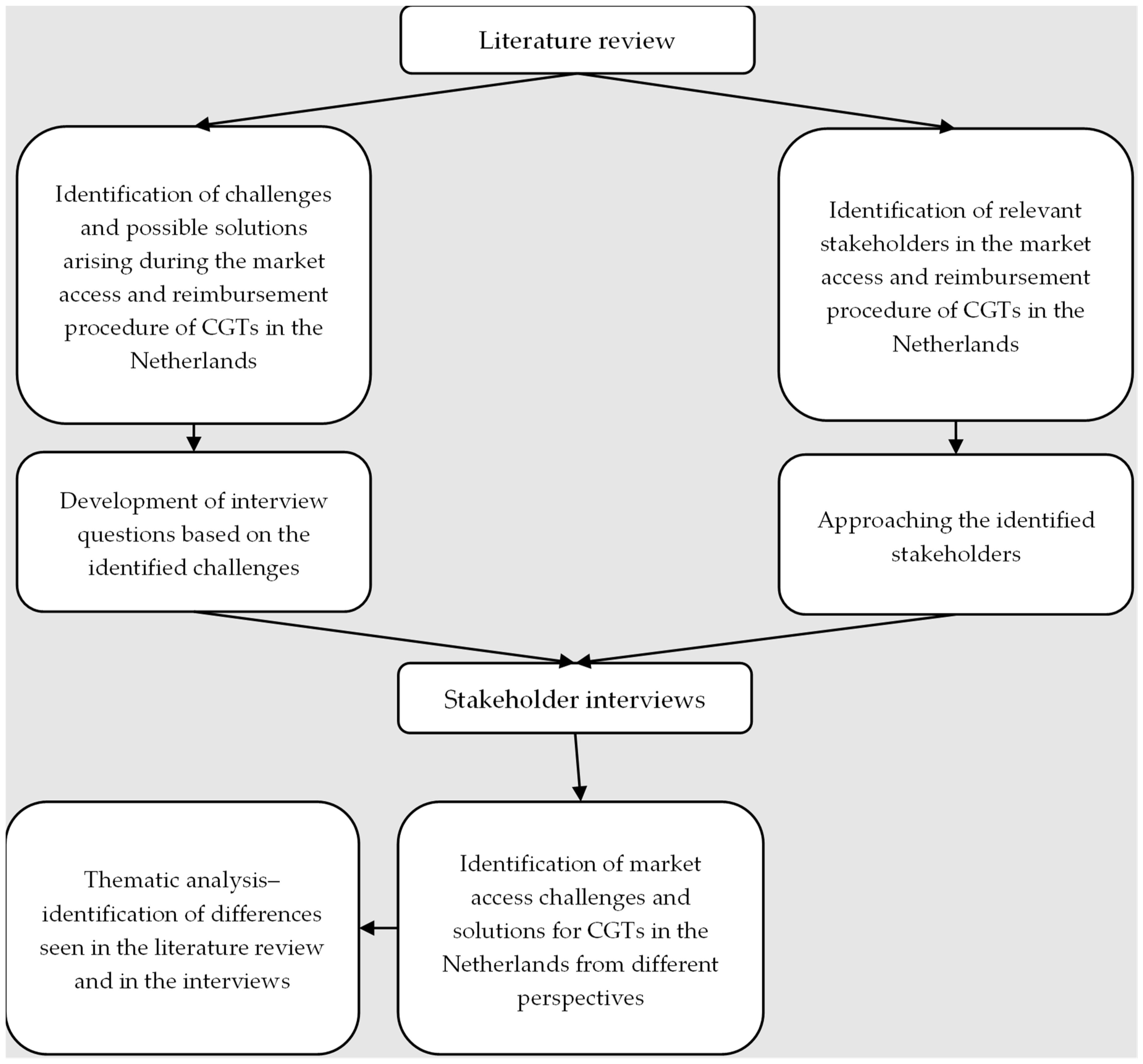
A pragmatic literature review was performed to identify market access challenges and solutions for CGTs. The traditional literature review method was chosen instead of a systematic review because it is better suited for qualitative research that aims to gain in-depth insights and generate hypotheses rather than test pre-determined ones [27]. This review included a grey literature search of HTA reports from the Dutch National Health Care Institute (ZIN; Dutch: Zorginstituut Nederland) and the National Institute for Health and Care Excellence (NICE) and other reports on trends in CGT market access in Europe, the U.S., and Canada. Based on the literature review, both the study sample and interview guide were further uncovered. Figure 1 depicts the methodology of this study in detail. The inclusion and exclusion criteria can be found in Appendix A Table A1.
Figure 1.
Methodology flowchart.
2.2. Study Sample
The type of participants for the interviews was identified from the (grey) literature review and selected based on their experiences and significant expertise related to the market access of CGTs in the Netherlands, ensuring a well-rounded understanding of the challenges and solutions, providing diverse viewpoints on the subject, and ensuring conceptual saturation.
2.3. Developing the Interview Guide
The findings identified in the literature review informed the development of the interview guide designed to elicit in-depth responses from participants regarding their experiences, perspectives, and potential solutions related to market access, with a clear emphasis on the Dutch context. The interview guide was structured around open-ended questions. This approach provided a framework for exploring participants’ insights and capturing a comprehensive understanding of market access dynamics. The structure was designed to encourage participants to provide detailed and insightful responses while allowing them the flexibility to express their unique perspectives.
2.4. Administering Semi-Structured Interviews
Semi-structured, in-depth, qualitative interviews with participants were conducted from January to April 2022 through video conference calls. These interviews were recorded with participant consent, and open-ended questions were used to explore the participants’ experiences and perspectives on challenges related to market access of CGTs. The transcripts of the interviews were summarised to capture short and clear messages and were later validated and sent to each participant. The summaries provided a written version of the data that was analysed to better understand the participants’ experiences and perspectives on market access of CGTs.
2.5. Analysing Data
The thematic analysis of the transcribed interviews involved identifying recurrent themes and patterns in the participants’ experiences and perspectives related to market access of CGTs in the Netherlands [28]. Initially, the data were thoroughly familiarised by reading the transcripts. The text was highlighted, and data were systematically coded into relevant themes. These codes were subsequently grouped into broader categories. Each theme was clearly defined and named, with detailed descriptions developed to outline their key features. The categories were synthesised and interpreted to generate meaningful insights, examine their relationships, and address the research objective. The analysis also compared the solutions proposed by stakeholders to those identified in the literature, tabulating differences and similarities to highlight new solutions and identify those not yet implemented in the Netherlands. By analysing interview data to capture all relevant themes, conceptual saturation was achieved.
3. Results
3.1. Literature Review
Out of the 2449 articles identified in the initial database searches, 124 relevant articles were selected for inclusion in this study. The following categories were identified in the literature review: clinical trial design, clinical evidence, health economics, reimbursement assessment, procedure, and organisation. The PRISMA flow diagram can be found in Figure A1 in Appendix A.
3.2. Study Sample
In total, 53 stakeholders were identified and contacted, of whom 16 agreed to the interview. There was an equal set of respondents from academia and patient advocacy groups, each accounting for 19% (three respondents), while manufacturers, health insurers, healthcare practitioners, and Association of Innovative Medicines members (Vereniging Innovatieve Geneesmiddelen, VIG) each represented 13% (two respondents) of the respondents. The lowest concentration was of hospital pharmacists and payers, representing 6% (one respondent) each.
3.3. Interview Guide
The interview guide focused on the following categories: reimbursement package, clinical trial design and assessment of the art and practice, health economics, payment models, procedure, and organisation. It can be found in Appendix A Table A2. The interviews lasted 45 min to one hour.
3.4. Views on the Reimbursement Package Management Challenges
Despite the benefits and facilitators of access, such as low budget impact and curative potentials, assessing CGTs presents several challenges, as acknowledged by all stakeholders in the interviews. Overall, 83% of respondents recognised the uncertainty in the long-term effectiveness of the therapy, 33% acknowledged the difficulty in comparing clinical data with standard care, 33% stressed the high burden associated with reimbursement procedure, 16% suggested there was a lack of designated centres of expertise and lack of clarity on whether the current reimbursement procedure is applicable for CGTs as those are therapies, not drugs, and another 16% highlighted the small patient populations and high prices of CGTs as considerable challenges to bear.
There was broad agreement on using RWE and long-term patient registries among academic HTA experts, the VIG, manufacturers, and health insurers. Both VIG and manufacturers suggested post-marketing reassessments based on phase IV studies and long-term data follow-up from clinical trials, respectively. Former payers advocated for the use of agreement mechanisms, emphasising that agreeing on Minimal Clinically Important Difference (MCID) should be a priority. Healthcare practitioners suggested permitting extrapolations based on mechanisms of action.
While the stakeholders acknowledged the difficulty in comparing clinical data with standard care, their approaches to addressing this challenge varied. The former payer emphasised the need to agree on MCID despite the inherent difficulty and offered the same advice for small patient populations in trials. Additionally, the payer recommended agreeing on a general level of uncertainty permitted by all the stakeholders. Health insurers recommended taking into account the additional costs of CGTs and comparing these to the total multi-year treatment costs of the current standard of care.
The stakeholders also stressed the high burden associated with the reimbursement procedure. Manufacturers suggested that ZIN should become more flexible. Healthcare practitioners recommended setting clear criteria for which patients should receive treatment and allowing health insurers to appoint Centres of Excellence (CoE).
Health insurers identified a lack of designated centres of expertise as a significant challenge. They suggested coming to an agreement with the relevant professional groups (beroepsgroep) to establish and designate these centres.
To address the high prices of CGTs, they suggested the development of new pricing models.
3.5. Views on the Clinical Trials, State-of-the-Art, and Science Challenges
The effectiveness and safety of CGTs are highly uncertain for a variety of reasons, according to all stakeholders. As much as 71% of the respondents suggested this is due to the relatively short-term duration of clinical trials, while another 57% argued that it is due to the single-arm study design. Additionally, 57% of the respondents mentioned that small patient populations in clinical trials contribute to this uncertainty. Finally, 29% mentioned that disease-specific and not generally applicable outcome measures also contribute to the overall uncertainty.
The stakeholders generally agreed on the importance of using real-world evidence (RWE) and long-term patient registries to address the short-term duration of clinical trials and the need for long-term data collection. Academic HTA experts, health insurers, and the VIG all advocated for using RWE and ensuring ongoing data collection through patient registries. Specifically, health insurers highlighted the necessity of using phase IV data and making it obligatory to track patients in registries, while VIG emphasised the legal enforcement of post-market authorisation studies. However, the stakeholders took differing approaches. Healthcare practitioners proposed permitting extrapolation based on the mechanism of action, offering a different perspective on managing the lack of long-term data.
To address the challenge posed by single-arm studies, the stakeholders agreed on the use of historical data and indirect comparators. Health insurers, VIG, and academic HTA experts all recognised the value of historical control groups, though health insurers noted the difficulty in achieving comparable populations due to different inclusion criteria. VIG further recommended the use of biomarkers alongside patient follow-ups to track disease progression and stressed the importance of informing patients. Academic HTA experts highlighted the feasibility of agreeing upfront on indirect comparators from the literature, a practice already in place in the Netherlands. The former payer suggested that HTA agencies could provide more detailed information on the requirements for indirect comparisons, emphasising the need for clearer guidelines.
To address the challenge posed by small patient populations, the stakeholders generally agreed on the need for robust study requirements and increasing sample sizes. The patient advocacy groups and VIG both emphasised the importance of more stringent study requirements and international collaboration to enhance sample sizes. They also highlighted the need for head-to-head studies with standard therapies to establish non-inferiority or superiority and for early dialogue between manufacturers and regulatory authorities to ensure trials meet necessary assessment criteria. Healthcare practitioners proposed outcome-based agreements as a solution to the issue of small patient populations, offering a different perspective on managing this challenge. Academic HTA experts suggested that allowing HTA agencies to provide input on study designs approved by the EMA would improve the relevance and comprehensiveness of the trials.
Lastly, the stakeholders agreed on the need for standardised outcome measures to address the challenge posed by disease-specific outcomes. The patient advocacy group called for the EMA/FDA to implement stricter requirements for similar outcome measures across different trials within the same indications. VIG underscored the issue by noting that current outcome measures are disease-specific and not generally applicable, implying the need for a more standardised approach
3.6. Views on Health Economics Challenges
All survey respondents identified challenges related to the health economics methodology specific to the Netherlands. Overall, 57% of those surveyed reported a lack of clarity regarding the appropriate use, indicating that if the drugs were in the trajectory of “appropriate use (in Dutch: “gepast gebruik”)”, it would be easier to monitor, collect data, and treat patients more effectively and cost-effective as a result. Another 57% of the respondents stated that traditional cost-effectiveness analyses (CEAs) did not represent CGTs, as they did not account for the unique costs or discounting methods required for CGTs. Additionally, 43% noted uncertainty in the long-term effects of CGTs, and 29% reported difficulty in accurately assessing the quality of life of CGT patients.
The stakeholders’ approaches to tackling the challenge related to appropriate use varied. Healthcare practitioners suggested collaborating with local HTA to establish MCID before national use and updating clinical guidelines. Health insurers proposed allowing professional associations to set up CoE and adhering to specific start criteria to assess patient suitability, particularly recommending a single CoE for small patient populations. The patient advocacy group emphasised good follow-up, clear criteria for starting treatment, and linking follow-up to a CoE for better patient assessment. The former payer advocated for using registries to improve appropriate use through ongoing monitoring and follow-up research.
Academic HTA experts recommended adapting CEAs to include specific elements of CGTs, such as hospital training and quality systems, to address the limitations of traditional CEAs. VIG suggested companies provide input on cost-effectiveness models, develop new discounting methods, and include cost-effectiveness analyses early in the process. Manufacturers stressed creating Diagnosis Treatment Combinations (DBCs; Dutch: Diagnose Behandel Combinaties) to cover administration, safety, and hospital stay requirements.
To address uncertainty in long-term effects, health insurers recommended adding conditional reimbursement or payment trajectories, and VIG recommended including cost-effectiveness in an early stage. To address the difficulty in accurately assessing QoL, the former payer advised monitoring patients extensively to establish accurate baselines and suggested setting up registries and CoEs for continuous long-term monitoring.
3.7. Views on Payment and Model Challenges
According to all interview respondents, there are issues related to payment and payment models for CGTs. High up-front costs were considered a significant challenge for 83% of the respondents, 67% mentioned that hospitals bear additional costs not included in the price of CGTs, 50% reported that it is difficult to establish a payment model as stakeholders cannot agree on MCID to reach reimbursement, and 17% stated that CGT patients are not evenly distributed among health insurers and can switch coverage after treatment. Additionally, a notable 17% of the respondents highlighted that flat discounts resulting from price negotiations are unsustainable because of their contribution to inconsistent pricing, lack of transparency, and fairness. Furthermore, this approach can create misaligned incentives, focusing on securing profitable agreements rather than addressing broader public health needs, thus impeding effective collaboration and partnership between pharmaceutical companies and governments.
Many of the stakeholders, including healthcare practitioners, the former payer, health insurers, the VIG, and manufacturers, advocated for various financial agreements to address this issue of high upfront costs. Different options for financial agreements included managed entry agreements with instalments proposed by health insurers, outcome-based payments or refunds for ineffective treatments suggested by healthcare practitioners and the former payer, and volume-based rebates recommended by manufacturers.
Additionally, health insurers recommend shifting phase III clinical research to real-life research to shorten registration times and reduce treatment costs. The former payer emphasised the need for agreement on outcome measures to make outcome-based agreements feasible.
To address the fact that hospitals bear additional costs that are not included in the price of CGTs, healthcare practitioners suggested including these additional costs in reimbursement. The former payer recommended covering and integrating these costs into DBCs and adjusting them accordingly. The VIG emphasised the need to standardise hospital requirements to treat patients with CGTs.
Regarding the challenge of agreeing on the MCID, the former payer proposed involving a third party, such as a professional association, to help set these thresholds and facilitate pricing agreements. They emphasised that outcome measures and MCID agreements should be linked to a patient registry and CoE. Academic HTA experts recommended using these payment models in combination with an early access program to increase availability and improve data collection, thereby reducing existing uncertainties.
To mitigate the uneven distribution of CGT patients among health insurers, health insurers proposed creating a joint fund to pay for CGT treatments, which would help distribute the financial burden more evenly.
Finally, to tackle the issue of unsustainable flat discounts resulting from price negotiations, health insurers suggested implementing risk-sharing and instalments to ensure more sustainable and transparent pricing models.
3.8. Views on Procedural and Organisational Challenges
According to the interview results, there are several challenges facing organisations, including bureaucratic and legislative issues. Specifically, 71% of the respondents reported that hospitals and academic groups face challenges related to legislation, certification, capacity, and equipment associated with CGTs. Academic centres must meet multiple manufacturers’ requirements and receive permission to work with CGTs, which is time-consuming. Pharmacists must fulfil requirements that are usually not feasible for a hospital pharmacist. Hospitals must purchase additional equipment and adhere to different quality control systems per manufacturer. In total, 57% of the respondents noted issues with the HTA process, such as extended time between marketing authorisation and market access, high costs due to separate reimbursement processes per country, lack of clear guidance on early access programs, and the absence of independent advice during ZIN assessment. Additionally, 29% of respondents cited challenges related to collecting RWE and low patient numbers due to low publicity and local data collection. Finally, 14% of the respondents mentioned that clinical guidelines are incomplete before or upon reimbursement.
To address the challenges related to legislation, certification, capacity, and equipment associated with CGTs, healthcare practitioners proposed creating a universal certificate/license for hospitals that covers all requirements and satisfies various manufacturers, preventing repeated assessments and audits. They also highlighted the DARE-NL platform, which ensures harmonised development, clinical testing, and sustained patient access through standardised practices across Dutch academic centres. The patient advocacy group suggested creating agreements in terms of accountability, spillage, and contracts, as well as arranging permission procedures per academic centre with a designated committee. Academic HTA experts recommended establishing a universal license/system that covers multiple products, encouraging manufacturers to fit their products into such a system. VIG emphasised the need for good coordination and upfront early dialogues to address the questions and needs of payers, healthcare practitioners, and patients, noting that they have already reduced the certification process time from one year to 28 days on paper.
Regarding the HTA process challenges, such as extended time between marketing authorisation and market access, high costs from separate reimbursement processes per country, the lack of clear guidance on early access programs, and the absence of independent advice during ZIN assessment, the stakeholders proposed various solutions. Health insurers suggested starting conversations before the product leaves the “lock” and arranging a central European process for registration and reimbursement. The patient advocacy group recommended clear discussions between hospitals and manufacturers about indications, finance, risks, insurance, and obligatory data collection during early access. They also emphasised the importance of proactive engagement with PAGs and allowing healthcare practitioners to comment earlier to align with PAGs. Furthermore, they called for academic centres to receive budget support for phase I and II research and to make it possible to register through the Central Committee on Research Involving Human Subjects only. The former payer questioned whether the responsibility should remain with private parties and suggested adding hospitals to the registration framework. Manufacturers recommended that ZIN should look at similar dossiers to expedite the assessment process.
To overcome challenges related to collecting RWE and low patient numbers due to low publicity and local data collection, the stakeholders proposed several solutions. Health insurers suggested setting up registries independently and on a European level to facilitate data collection. VIG recommended creating enthusiasm among healthcare practitioners and patients by explaining the treatment and seeking media attention to increase awareness. They also emphasised cooperation among healthcare practitioners to provide advice and pre-sort the designation of CoE, noting that often only one centre participates in trials in the Netherlands.
Lastly, to address the issue of incomplete clinical guidelines before or upon reimbursement, manufacturers proposed that professional associations should create better patient flows and estimations. They emphasised the importance of including new interventions in the guidelines before reimbursement.
3.9. Thematic Analysis of Interviews and the Literature Review
A thematic analysis of the challenges and recommendations identified in the literature review and interviews was conducted. In the context of the Netherlands, it was found that there were more country-specific challenges and solutions than those currently discussed in the literature. The detailed overview is presented in Table A3 and Table A4 in Appendix A. Notably, these include developing more robust data requirements as early as in dialogue with EMA. Establishing clear criteria for the CoEs is also critical to ensure these institutions are well-equipped to handle CGTs effectively.
Additionally, the stakeholders emphasised the importance of considering extra costs associated with CGTs, accounting for DBC costs. Integrating price negotiations and financial models early in the market access process was identified as a key strategy to mitigate potential delays and uncertainties. Furthermore, meaningful involvement of patient and clinician associations was underscored as essential for developing patient-centric and clinically relevant solutions.
Interestingly, the Dutch stakeholders did not mention certain recommendations discussed in the literature, such as increasing the willingness-to-pay threshold for health technologies like CGTs, integrating all elements in economic modelling using multi-criteria decision analyses, and establishing patient advocacy groups to advocate for the affordability and accessibility of CGTs.
4. Discussion
This paper sheds light on published challenges and solutions related to the market access of CGTs in the Netherlands, as seen from the stakeholders’ perspectives. This study conducted 16 interviews with stakeholders from various areas of expertise, including academia, patient advocacy groups, manufacturers, health insurers, healthcare practitioners, payers, hospital pharmacists, and VIG. The findings of this study summarise the stakeholders’ views on the readiness of HTA agencies to assess CGTs, long-term safety and effectiveness, health economics methodology, funding models, and other policies relevant to stakeholders. This article highlights common challenges all stakeholders face, such as uncertainty in long-term effectiveness, difficulties in comparing clinical data, high costs, lack of designated expertise centres, and small patient populations. Each stakeholder group has a different focus on addressing these issues, reflecting the complex dynamics and underscoring the need for a comprehensive discussion. The solutions to address the challenges include improving communication and collaboration, developing a regional strategy for RWE, establishing expertise centres, collecting RWE, establishing robust study requirements, developing new health economics methodologies, and introducing new payment models.
While this study offers a unique perspective, it has inherent limitations to its qualitative method. This study did not account for recent studies published after the literature review, and the reliance on spontaneous recall during interviews may affect the accuracy of the findings [6,14,29,30,31,32,33,34,35,36]. Although the data collection occurred a few years ago, the answers and our recommendations remain relevant because the common challenges are still faced and the proposed solutions continue to be necessary and applicable.
Despite these limitations, the consistent findings among different stakeholders strengthen the results and reduce the impact of recall bias. Although this study had a limited number of interviewees, which is common in qualitative research, the study design partly ensured the conceptual saturation of each stakeholder group when possible. Additionally, the number of respondents was deemed sufficient because of the high level of expertise and diverse perspectives each participant brought to this research. Their comprehensive knowledge and varied backgrounds ensured a rich, in-depth topic exploration. The findings of this study add to the numerous articles published on the topic, as they not only highlight the challenges faced by the stakeholders in the field but also present specific recommendations for improving market access of CGTs derived from the stakeholders’ interviews. Unlike many other articles that only address a single perspective and lack recommendations for collaboration among stakeholders, this study provides a comprehensive view of the situation in the Netherlands from different angles and perspectives. It emphasises the importance of a united approach to improving market access. It is important to note that while these findings are primarily applicable to the Netherlands, they can be relevant to countries with similar regulatory environments, such as Belgium, Ireland, and Luxembourg. It is recommended that future research initiate similar studies in other European countries to identify corresponding vulnerabilities and find opportunities for pan-European collaboration.
5. Conclusions
This research provides a novel exploration of market access challenges and solutions for CGTs in the Netherlands by integrating diverse stakeholder perspectives through comprehensive qualitative interviews, presenting realistic and achievable recommendations. It emphasises the importance of collaborative efforts among stakeholders in the coming years to mitigate these challenges and develop comprehensive multidisciplinary solutions. This manuscript could yield a call to action to initiate the process of creating tangible action plans to address these issues, providing a united starting point for all stakeholders to work together in improving patient access to CGTs in the Netherlands.
Author Contributions
Conceptualization, R.V., S.W., H.S.H. and M.J.P.; Data curation, R.V., S.W. and H.S.H.; Formal analysis, R.V., S.W. and H.S.H.; Investigation, S.W. and H.S.H.; Methodology, R.V., S.W. and H.S.H.; Project administration, R.V., S.W. and H.S.H.; Resources, S.W. and H.S.H.; Supervision, R.V. and C.B.; Validation, M.J.P. and C.B.; Visualization, R.V.; Writing—original draft, R.V. and C.B.; Writing—review & editing, R.V., S.W., H.S.H., M.J.P. and C.B. All authors have read and agreed to the published version of the manuscript.
Funding
Bayer Netherlands B.V.: PO2150850929 supported the research.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All the relevant data are provided in this article.
Acknowledgments
We thank Roma Kwiatkiewicz for medical writing and administrative support. Additionally, we thank Jeanni van Loon for her help preparing the interviews.
Conflicts of Interest
Rimma Velikanova, Sharon Wolters, and Hinko Hofstra work as consultants at Asc Academics B.V., which has received grants from Bayer Netherlands B.V. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results. Maarten Postma, and Cornelis Boersma declare no financial interest.
Appendix A

Table A1.
PICOS criteria for the inclusion and exclusion of studies.
Table A1.
PICOS criteria for the inclusion and exclusion of studies.
| Category | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| Population (P) | Any patient population that is eligible for CGT | Patient population not eligible for CGT |
| Intervention (I) | CGTs | Not CGT |
| Comparators (Cs) | Any | None |
| Outcomes (Os) | Challenges and solutions in CGT market access | Not discussing CGT market access challenges and solutions |
| Study design (S) | Any | None |
| Language | English or Dutch language | Non-English or non-Dutch language |
| Time limit | Published from 2016 to July 2021 1 | Studies published before 2016 |
| Country | Any | None |
CGT indicates Cell and Gene Therapy; PICOS indicates population, intervention, comparators, outcomes, study design, language, time limit, and country. 1 This period captures key regulatory approvals, reimbursement challenges, and early market experiences of gene and cell therapies. It includes the latest data and trends, reflecting the evolving market access landscape.
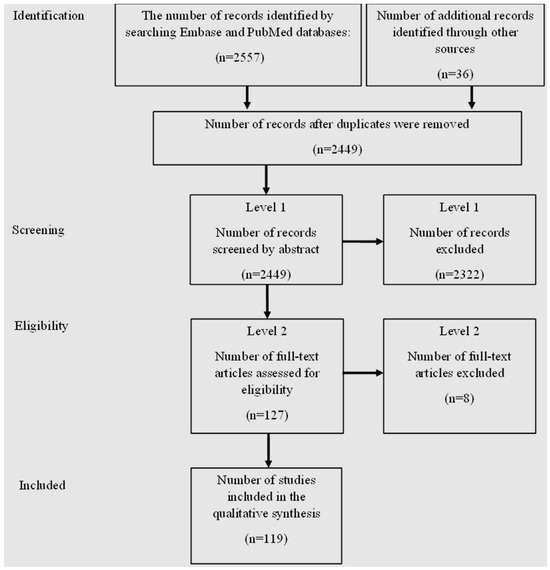
Figure A1.
The PRISMA flowchart.
Figure A1.
The PRISMA flowchart.

Table A2.
Interview guide.
Table A2.
Interview guide.
| Questions by Category |
| Introduction: We are conducting research on the market access challenges of CGTs in the Netherlands. The lead time for CGT medications is long due to additional challenges, and we hope this research will help streamline and accelerate the market access process. We aim to contribute to the structural access of patients to CGTs through these interviews. We have already identified a number of challenges in the literature, but we would like to identify the key challenges and potential solutions experienced by various parties involved in the Dutch practice through these interviews. We hope this will contribute to a future-proof package management as mentioned by ZIN to keep innovative care high quality, accessible, and affordable in the future. Finally, we would like to discuss possible solutions for the challenges, the transformations needed for this, and what the current state of affairs is. |
| Questions by Category |
| Open Questions |
|
|
|
|
| For the rest of the interview, we have divided the questions into the following topics: clinical CGT research, current state of science and practice, health economics, future-proof package management, funding, and procedures/organization. |
| Clinical Trial Challenges |
| Current clinical CGT studies have a number of shortcomings. |
|
|
|
|
|
| State of Science and Practice |
| CGTs obtain reimbursement through the same process as other therapies (conditional admission process or standard assessment from the sluice) |
|
|
|
|
| Health Economics |
|
|
|
|
|
|
|
| Future-Proof Package Management |
|
|
|
|
| Funding |
| CGTs are associated with high upfront costs. |
|
|
| Various innovative payment models can be used to reduce uncertainties/risk sharing or to spread payment over time. |
|
| What is the current state of affairs regarding the development of payment models that better fit CGT? (this is referred to in the July 2021 letter to parliament about future-oriented package management). |
|
|
|
| Procedural and Organizational Challenges |
|
|
| Closing |
|
|
CGT indicates Cell and Gene Therapy; ZIN indicates Zorginstituut Nederland (Dutch National Health Care Institute); RCT indicates Randomized Controlled Trial; RWE indicates real-world evidence; HTA indicates health technology assessment; DBC indicates Diagnose Behandel Combinatie (Diagnosis Treatment Combination); DOT indicates DBCs on their way to transparency; CEA indicates cost-effectiveness analysis.

Table A3.
Challenges identified from the literature review versus interviews.
Table A3.
Challenges identified from the literature review versus interviews.
| Challenges | Clinical Trial | Clinical Evidence—SvWP/Pakketbeheer | Health Economics | Payment Models | Value Assessment | Procedures & Organizational | |
|---|---|---|---|---|---|---|---|
| TLR/ Dutch Stakeholders | |||||||
| Overlapping challenges in TLR and Dutch stakeholders |
|
|
|
|
|
| |
| Additional Dutch challenges derived from interviews |
|
|
|
|
| ||
TLR indicates literature review; SvWP indicates Stand van de Wetenschap en Praktijk (State of Science and Practice); CoEs indicates Centers of Excelence; CGT indicates cell and gene therapy; ICER indicates Incremental Cost-Effectiveness Ratio; DRGs indicates Diagnosis-Related Groups; HICs indicates health insurers; CEA indicates cost-effectiveness analysis; RWE indicates real-world evidence; HRQoL indicates Health-Related Quality of Life; MCID indicates Minimal Clinically Important Difference; EMA indicates European Medicines Agency; ZIN indicates Zorginstituut Nederland (Dutch National Health Care Institute). Note: Red highlights indicate significant CGT challenges that are complex to overcome under current HTA and market access requirements in the Netherlands; amber challenges can be addressed with additional data or structural changes, while green challenges are more easily resolved through collaboration with stakeholders, focusing on procedural or organizational issues.

Table A4.
Solutions identified from the literature review versus interviews.
Table A4.
Solutions identified from the literature review versus interviews.
| Solutions | Clinical Trial | Clinical Evidence—SvWP/Pakketbeheer | Health Economics | Payment Models | Value Assessment | Procedures and Organisational | |
|---|---|---|---|---|---|---|---|
| TLR/ Dutch | |||||||
| Overlapping Proposed Solutions in TLR and Dutch stakeholders |
|
|
|
|
|
| |
| Proposed solution in TLR | - |
|
| ||||
| Additional Dutch proposed solutions |
|
|
|
|
|
| |
TLR indicates Literature Review; SvWP indicates Stand van de Wetenschap en Praktijk (State of Science and Practice); HTA indicates Health Technology Assessment; CGT indicates cell and gene therapy; RWE indicates real-world evidence; CoE(s) indicates Centre(s) of Excellence; EMA indicates European Medicines Agency; WTP indicates Willingness to Pay; Tx indicates Treatment; MCDA indicates Multi-Criteria Decision Analysis; CEA indicates cost-effectiveness analysis; MoA indicates the mechanism of action; FU indicates follow-up; HRQoL indicates Health-Related Quality of Life; PAG indicates patient advocacy group; MoH indicates Ministry of Health; HICs indicates health insurance; MNF indicates manufacturer; ZIN indicates Zorginstituut Nederland (Dutch National Health Care Institute); HCP indicates Health Care Provider; EPPs indicates Early Patient Programs; DRG indicates Diagnosis-Related Group. Note: Red highlights indicate significant CGT challenges that are complex to overcome under current HTA and market access requirements in the Netherlands; amber challenges can be addressed with additional data or structural changes, while green challenges are more easily resolved through collaboration with stakeholders, focusing on procedural or organisational issues.
References
- ClinicalTrials.gov. Available online: https://clinicaltrials.gov/ (accessed on 3 December 2023).
- Simon Alfano, A.G.; Alberto, L.; Pablo, S. Eight Imperatives for Launching Cell and Gene Therapies. Available online: https://www.mckinsey.com/industries/life-sciences/our-insights/eight-imperatives-for-launching-cell-and-gene-therapies (accessed on 20 January 2024).
- Aballéa, S.; Thokagevistk, K.; Velikanova, R.; Simoens, S.; Annemans, L.; Antonanzas, F.; Auquier, P.; François, C.; Fricke, F.-U.; Malone, D. Health economic evaluation of gene replacement therapies: Methodological issues and recommendations. J. Mark. Access Health Policy 2020, 8, 1822666. [Google Scholar] [CrossRef] [PubMed]
- Marsden, G.; Towse, A. Exploring the Assessment and Appraisal of Regenerative Medicines and Cell Therapy Products: Is the NICE Approach Fit for Purpose. Available online: https://www.ohe.org/publications/exploring-assessment-and-appraisal-regenerative-medicines-and-cell-therapy-products/ (accessed on 1 December 2023).
- Pochopień, M.; Paterak, E.; Clay, E.; Janik, J.; Aballea, S.; Biernikiewicz, M.; Toumi, M. An overview of health technology assessments of gene therapies with the focus on cost-effectiveness models. J. Mark. Access Health Policy 2021, 9, 2002006. [Google Scholar] [CrossRef] [PubMed]
- Pochopień, M.; Qiu, T.; Aballea, S.; Clay, E.; Toumi, M. Considering potential solutions for limitations and challenges in the health economic evaluation of gene therapies. Expert Rev. Pharmacoecon. Outcomes Res. 2021, 21, 1145–1158. [Google Scholar] [CrossRef] [PubMed]
- Hettle, R.; Corbett, M.; Hinde, S.; Hodgson, R.; Jones-Diette, J.; Woolacott, N.; Palmer, S. The assessment and appraisal of regenerative medicines and cell therapy products: An exploration of methods for review, economic evaluation and appraisal. Health Technol. Assess. 2017, 21, 1–204. [Google Scholar] [CrossRef] [PubMed]
- Hampson, G.; Towse, A.; Pearson, S.D.; Dreitlein, W.B.; Henshall, C. Gene therapy: Evidence, value and affordability in the US health care system. J. Comp. Eff. Res. 2018, 7, 15–28. [Google Scholar] [CrossRef] [PubMed]
- Jönsson, B.; Hampson, G.; Michaels, J.; Towse, A.; von der Schulenburg, J.-M.G.; Wong, O. Advanced therapy medicinal products and health technology assessment principles and practices for value-based and sustainable healthcare. Eur. J. Health Econ. 2019, 20, 427–438. [Google Scholar] [CrossRef] [PubMed]
- Drummond, M.F.; Neumann, P.J.; Sullivan, S.D.; Fricke, F.-U.; Tunis, S.; Dabbous, O.; Toumi, M. Analytic considerations in applying a general economic evaluation reference case to gene therapy. Value Health 2019, 22, 661–668. [Google Scholar] [CrossRef] [PubMed]
- Angelis, A.; Naci, H.; Hackshaw, A. Recalibrating health technology assessment methods for cell and gene therapies. Pharmacoeconomics 2020, 38, 1297–1308. [Google Scholar] [CrossRef] [PubMed]
- Coyle, D.; Durand-Zaleski, I.; Farrington, J.; Garrison, L.; Graf von der Schulenburg, J.-M.; Greiner, W.; Longworth, L.; Meunier, A.; Moutié, A.-S.; Palmer, S. HTA methodology and value frameworks for evaluation and policy making for cell and gene therapies. Eur. J. Health Econ. 2020, 21, 1421–1437. [Google Scholar] [CrossRef]
- Ten Ham, R.M.; Klungel, O.H.; Leufkens, H.G.; Frederix, G.W. A review of methodological considerations for economic evaluations of gene therapies and their application in literature. Value Health 2020, 23, 1268–1280. [Google Scholar] [CrossRef]
- Simoens, S.; De Groote, K.; Boersma, C. Critical reflections on reimbursement and access of advanced therapies. Front. Pharmacol. 2022, 13, 771966. [Google Scholar] [CrossRef] [PubMed]
- Svensson, M.; Nilsson, F.O.; Arnberg, K. Reimbursement decisions for pharmaceuticals in Sweden: The impact of disease severity and cost effectiveness. Pharmacoeconomics 2015, 33, 1229–1236. [Google Scholar] [CrossRef]
- Principles for Priority Setting in Health Care. Available online: https://www.regjeringen.no/contentassets/439a420e01914a18b21f351143ccc6af/en-gb/pdfs/stm201520160034000engpdfs.pdf (accessed on 23 January 2024).
- Changes We’re Making to Health Technology Evaluation. Available online: https://www.nice.org.uk/Media?Default/About/what-we-do/our-programmes/technology-appraisals/methods-processes-and-topic-selection-review-board-paper-appendix.docx (accessed on 23 January 2024).
- Adapted Value Assessment Methods for High-Impact “Single and Short-Term Therapies” (SSTs). Available online: https://icer.org/wp-content/uploads/2020/10/ICER_SST_FinalAdaptations_111219.pdf (accessed on 27 January 2024).
- Vergoeding Intramurale Geneesmiddelen: De Add-on Prestatie. Available online: http://www.hollandbio.nl/wp-content/uploads/2020/12/infographic-vergoeding-intramurale-geneesmiddelen_final.pdf (accessed on 11 June 2023).
- Vergoeding Intramurale Geneesmiddelen: Van EMA Registratie Tot Add-on. Available online: https://www.hollandbio.nl/wp-content/uploads/2023/02/infographic-vergoeding-intramurale-geneesmiddelen_versie-jan-2023.pdf (accessed on 10 June 2024).
- Ward, L.M.; Chambers, A.; Mechichi, E.; Wong-Rieger, D.; Campbell, C. An international comparative analysis of public reimbursement of orphan drugs in Canadian provinces compared to European countries. Orphanet J. Rare Dis. 2022, 17, 113. [Google Scholar] [CrossRef] [PubMed]
- Kuipers, E. Wijziging Beleidsregels voor de Toepassing van de Sluis voor dure Geneesmiddelen op Grond van Artikel 2.4a van het Besluit Zorgverzekering. 24 January 2023. Available online: https://open.overheid.nl/documenten/ronl-a04e9c698c6915588ffed5b381e5f2b7097c4bc6/pdf (accessed on 20 July 2023).
- Sluis Voor Dure Geneesmiddelen. Available online: https://www.zorginstituutnederland.nl/over-ons/programmas-en-samenwerkingsverbanden/horizonscan-geneesmiddelen/sluis-voor-dure-geneesmiddelen (accessed on 26 July 2023).
- Pakketadvies Sluisgeneesmiddel Ciltacabtagene Autoleucel (Carvykti®) Voor de Behandeling van Multipel Myeloom. Available online: https://www.zorginstituutnederland.nl/over-ons/publicaties/adviezen/2022/10/20/pakketadvies-sluisgeneesmiddel-ciltacabtagene-autoleucel-carvykti (accessed on 26 July 2023).
- Bluebird Bio Reports Second Quarter Financial Results and Provides Operational Update. Available online: https://investor.bluebirdbio.com/news-releases/news-release-details/bluebird-bio-reports-second-quarter-financial-results-and (accessed on 26 July 2023).
- Pakketadvies Sluisgeneesmiddel Atidarsagene Autotemcel (Libmeldy®) Voor de Behandeling van Metachromatische Leukodystrofie (MLD). Available online: https://www.zorginstituutnederland.nl/over-ons/publicaties/adviezen/2022/09/27/pakketadvies-sluisgeneesmiddel-atidarsagene-autotemcel-libmeldy (accessed on 26 May 2024).
- Paré, G.; Kitsiou, S. Methods for literature reviews. In Handbook of ehealth Evaluation: An Evidence-Based Approach; Lau, F., Kuziemsky, C., Eds.; University of Victoria: Victoria, BC, Canada, 2017. [Google Scholar]
- Kiger, M.E.; Varpio, L. Thematic analysis of qualitative data: AMEE Guide No. 131. Med. Teach. 2020, 42, 846–854. [Google Scholar] [CrossRef]
- Landfeldt, E. Gene therapy for neuromuscular diseases: Health economic challenges and future perspectives. J. Neuromuscul. Dis. 2022, 9, 675–688. [Google Scholar] [CrossRef] [PubMed]
- Qiu, T.; Pochopien, M.; Liang, S.; Saal, G.; Paterak, E.; Janik, J.; Toumi, M. Gene therapy evidence generation and economic analysis: Pragmatic considerations to facilitate fit-for-purpose health technology assessment. Front. Public Health 2022, 10, 773629. [Google Scholar] [CrossRef]
- Garrison, L.P.; Pezalla, E.; Towse, A.; Yang, H.; Faust, E.; Wu, E.Q.; Li, N.; Sawyer, E.K.; Recht, M. Hemophilia gene therapy value assessment: Methodological challenges and recommendations. Value Health 2021, 24, 1628–1633. [Google Scholar] [CrossRef] [PubMed]
- O’Hara, J.; Neumann, P.J.; Council, I.H.A.S. Health technology assessment for gene therapies in haemophilia. Haemophilia 2022, 28, 19–26. [Google Scholar] [CrossRef]
- de Labry-Lima, A.O.; Ponce-Polo, A.; García-Mochón, L.; Ortega-Ortega, M.; Pérez-Troncoso, D.; Epstein, D. Challenges for economic evaluations of advanced therapy medicinal products: A systematic review. Value Health 2023, 26, 138–150. [Google Scholar] [CrossRef]
- Sabatini, M.T.; Xia, T.; Chalmers, M. Pricing and market access challenges in the era of one-time administration cell and gene therapies. Pharm. Med. 2022, 36, 265–274. [Google Scholar] [CrossRef]
- Fornaro, G.; Drummond, M.; Ciani, O.; Jommi, C. P48 Are Health Technology Assessment (HTA) Bodies Responding to the Assessment Challenges Posed By Cell and Gene Therapies? Value Health 2022, 25, S297. [Google Scholar] [CrossRef]
- Toumi, M.; Dabbous, O.; Aballéa, S.; Drummond, M.F.; von der Schulenburg, J.-M.G.; Malone, D.C.; Neumann, P.J.; Sullivan, S.D.; Tunis, S. Recommendations for economic evaluations of cell and gene therapies: A systematic literature review with critical appraisal. Expert Rev. Pharmacoecon. Outcomes Res. 2023, 23, 483–497. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).