Is the Healthcare Industry Ready for Digital Twins? Examining the Opportunities and Challenges
Abstract
1. Introduction
1.1. Background
1.2. Research Motivation (Gaps)
- How does Digital Twin technology improve individualised patient treatments and care quality?
- What is the role of Digital Twin technology in accurately predicting patient responses to medical interventions?
- What are the significant challenges of integrating Digital Twin technology into healthcare?
2. Methodology
2.1. Study Design
2.2. Integrative Review Method
2.3. Key Terms
2.4. Search Strategy
- Resources and databases: This study primarily utilised ProQuest due to its wide coverage of peer-reviewed journals across healthcare, technology, and interdisciplinary fields relevant to Digital Twin applications. PubMed, Scopus, Web of Science, and ProQuest’s advanced filtering features also supported focused searches aligned with the study’s inclusion criteria. To complement this, Google Scholar was used to broaden the search and capture additional literature, particularly emerging studies, grey literature, and articles that may not be indexed in discipline-specific databases. The combined use of these platforms ensured both depth and breadth in identifying relevant and diverse sources across the Digital Twin and healthcare literature.
- Using “key terms”: Affiliated with study concentrations, the key terms applied were “Digital Twin”, “Technology improvements”, “Healthcare”, “Impact”, “Customised treatment”, “Virtual models”, “Patient treatment”, and “Applications”. These were chosen to screen Digital Twin technology’s potential and its implementation in healthcare circumstances, mainly focusing on patients’ treatment outcomes and innovative applications of the technologies.
- Boolean finding operators: These strings were applied to construct the finding sequences and advance the search area as required. The key Boolean search operator used was (“Digital Twins” AND “Healthcare” AND “Patient”).
- Inclusion criteria: Once the early results, articles’ headings, sub-headings, and abstracts were systematically assessed for pertinence to the research topic, the adoption of Digital Twin models in healthcare contexts, individualised patient care and treatment approaches, and measurable results were included in the inclusion criteria. Studies that were conducted for non-medically related conditions and lacked information about practical treatment outcomes were excluded.
- Manual citation validation: To supplement database searches, backward reference searching (also known as manual citation checking) was conducted. This involved reviewing the reference lists of key articles to identify additional relevant studies that were not retrieved through the initial search queries. This method helped uncover frequently cited foundational works and ensured a more comprehensive and representative literature base.
- Search modifications and duplications: This search approach was constantly sophisticated during the analysis. The search phrases were altered based on initial outcomes, ensuring a detailed and concentrated set of articles appropriate to the research aims.
2.5. Eligibility Criteria (Inclusion and Exclusion)
2.6. Screening and Selection
2.7. Data Analysis Techniques
3. Literature Review
3.1. Conceptualisation and Terms
3.2. Study Overview
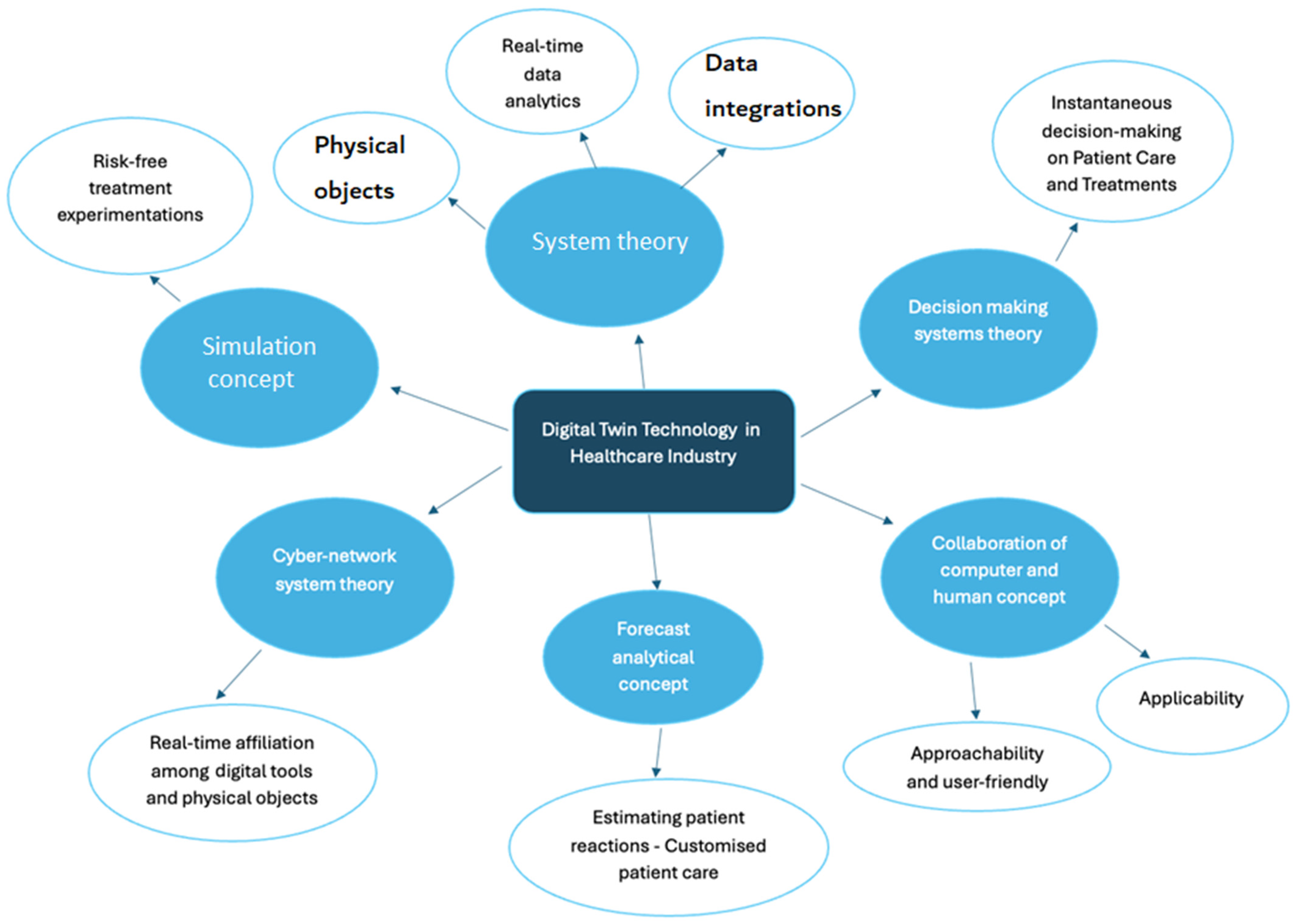
3.3. Theories and Theoretical Models in Previous Research
4. Findings
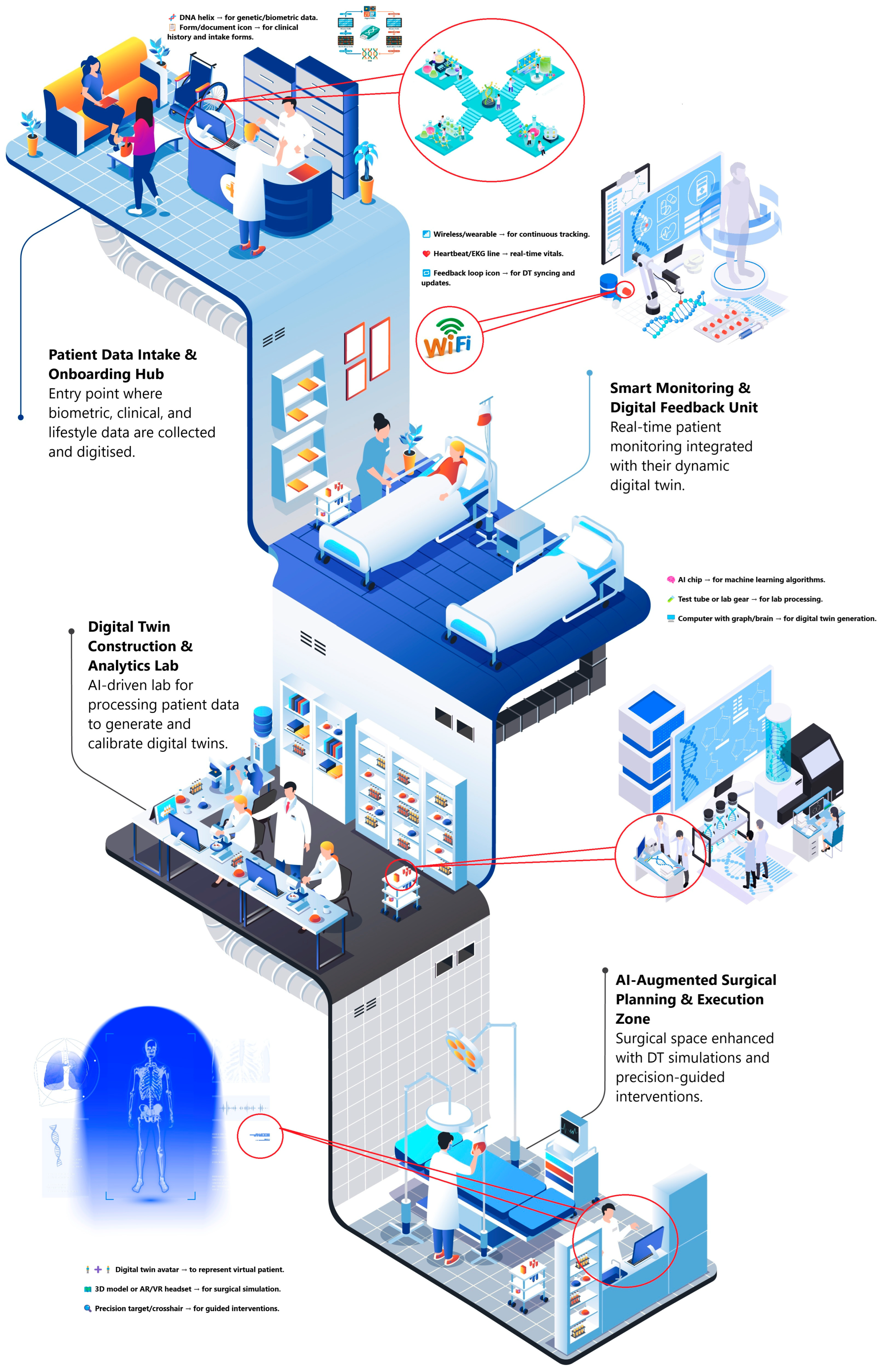
4.1. Conceptual Insights
4.2. Ethical and Organisational Challenges to DT Adoption
4.3. Personalised Medicine and Treatment
4.4. Predictive Analytics for Patient Care
4.5. Extended Reality and Artificial Intelligence for Advanced Treatments
4.6. Data Privacy and Safety Issues
4.7. Legislation and Technological Limitations
4.8. Ethical Considerations of Artificial Intelligence-Related Decisions
4.9. Methodological Approaches in a Targeted Subset of Articles on Digital Twin Applications
4.10. Research Gaps in the Literature
5. Theoretical and Practical Contributions
5.1. Theoretical Contribution
5.2. Practical Contribution
5.3. Limitations and Future Studies
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| Term | Definition | References |
|---|---|---|
| Digital Twin | A Digital Twin technology is a virtual model of a real human being that assists healthcare experts to identify and obtain significant insights, optimise medical treatments and practices, and provide customised individual care and treatment by adopting multiple data sources. | [25,39] |
| Healthcare | A system designed for diagnosing, treating, anticipating, and controlling patient’s medical conditions, concentrated on enhancing well-being and supporting high-quality healthcare practices. | [8,40] |
| Personalised Treatment | Healthcare method which customises the clinical involvements based on each patient’s particular conditions, needs, and characteristics, leveraging innovative technologies like artificial intelligence and Digital Twins to optimise medical care effectiveness. | [41,44] |
| Technology Advancements | The adoption and enhancements of advanced technologies to increase results and effectiveness in clinical and health sciences, confronting problems such as system interoperability and cybersecurity. | [36,42] |
| Patient Treatment Outcome | The clinical consequences and impacts for patients, mainly considering disease progress and its efficiency of involvements. | [45,56] |
| Virtual Models | Digital replicas that operate as alike counterparts to real physical objects, mirroring their exact attributes and behaviours. These virtual stimulations are coupled to real-time active data, allowing for virtual realities and evaluation to optimise comprehension and informed decisions in diverse implementations in healthcare. | [39,54] |
| Impacts | Digital Twins’ considerable impacts on various areas, specifically in the healthcare sector, in terms of transmuting practices, increasing understanding, and fostering innovative adoptions in response to the benefits and challenges created through digitalisation practices. | [37,57] |
| Applications | Digital Twins’ practical utilisations in research studies and healthcare contexts for virtualising and copying biological procedures and patients’ health situations. | [59,60] |
References
- Safa, E.; Asan, O. Digital Twins for Managing Health Care Systems: Rapid Literature Review. J. Med. Internet Res. 2022, 24, e37641. [Google Scholar] [CrossRef]
- Kulkarni, C.; Quraishi, A.; Mohan, R.; Shabaz, M.; Khan, M.A.; Varma, R.A.; Keshta, I.; Soni, M.; Byeon, H. Hybrid disease prediction approach leveraging digital twin and metaverse technologies for health consumer. BMC Med. Inform. Decis. Mak. 2024, 24, 92. [Google Scholar] [CrossRef]
- Cellina, M.; Cè, M.; Alì, M.; Irmici, G.; Ibba, S.; Caloro, E.; Fazzini, D.; Oliva, G.; Papa, S. Digital Twins: The New Frontier for Personalized Medicine? Appl. Sci. 2023, 13, 7940. [Google Scholar] [CrossRef]
- Palaniappan, R.; Surendran, S. A Digital Twin Approach for deepened Classification of Patients with Hepatitis, Fibrosis and Cirrhosis. J. Phys. Conf. Ser. 2022, 2335, 012034. [Google Scholar] [CrossRef]
- Johnson, Z.; Saikia, M.J. Digital Twins for Healthcare Using Wearables. Bioengineering 2024, 11, 606. [Google Scholar] [CrossRef]
- Katsoulakis, E.; Wang, Q.; Wu, H.; Shahriyari, L.; Fletcher, R.; Liu, J.; Achenie, L.; Liu, H.; Jackson, P.; Xiao, Y. Digital twins for health: A scoping review. NPJ Digit. Med. 2024, 7, 77. [Google Scholar] [CrossRef] [PubMed]
- Rudnicka, Z.; Proniewska, K.; Perkins, M.; Pregowska, A. Cardiac Healthcare Digital Twins Supported by Artificial Intelligence-Based Algorithms and Extended Reality—A Systematic Review. Electronics 2024, 13, 866. [Google Scholar] [CrossRef]
- Dang, J.; Lal, A.; Montgomery, A.; Flurin, L.; Litell, J.; Gajic, O.; Rabinstein, A. Developing DELPHI expert consensus rules for a digital twin model of acute stroke care in the neuro critical care unit. BMC Neurol. 2023, 23, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Chu, Y.; Li, S.; Tang, J.; Wu, H. The potential of the Medical Digital Twin in diabetes management: A review. Front. Med. 2023, 10, 1178912. [Google Scholar] [CrossRef]
- Laubenbacher, R.; Niarakis, A.; Helikar, T.; An, G.; Shapiro, B.; Malik-Sheriff, R.S.; Sego, T.J.; Knapp, A.; Macklin, P.; Glazier, J.A. Building digital twins of the human immune system: Toward a roadmap. NPJ Digit. Med. 2022, 5, 64. [Google Scholar] [CrossRef]
- Mohapatra, S.; Bose, S. An appraisal of literature for design and implementation of developing a framework for digital twin and validation through case studies. Health Technol. 2020, 10, 1229–1237. [Google Scholar] [CrossRef]
- Vallée, A. Digital twin for healthcare systems. Front. Digit. Health 2023, 5, 1253050. [Google Scholar] [CrossRef] [PubMed]
- Avanzato, R.; Beritelli, F.; Lombardo, A.; Ricci, C. Lung-DT: An AI-Powered Digital Twin Framework for Thoracic Health Monitoring and Diagnosis. Sensors 2024, 24, 958. [Google Scholar] [CrossRef] [PubMed]
- Konopik, J.; Wolf, L.; Schöffski, O. Digital twins for breast cancer treatment—An empirical study on stakeholders’ perspectives on potentials and challenges. Health Technol. 2023, 13, 1003–1010. [Google Scholar] [CrossRef]
- Turab, M.; Jamil, S. A comprehensive survey of digital twins in healthcare in the era of metaverse. BioMedInformatics 2023, 3, 563–584. [Google Scholar] [CrossRef]
- Wickramasinghe, N.; Ulapane, N.; Andargoli, A.; Shuakat, N.; Nguyen, T.; Zelcer, J.; Vaughan, S. Digital twin of patient in clinical workflow. Proc. R. Soc. Vic. 2023, 135, 72–80. [Google Scholar] [CrossRef]
- Machado, T.M.; Berssaneti, F.T. Literature review of digital twin in healthcare. Heliyon 2023, 9, e19390. [Google Scholar] [CrossRef]
- Cronin, M.A.; George, E. The why and how of the integrative review. Organ. Res. Methods 2023, 26, 168–192. [Google Scholar] [CrossRef]
- Battistone, M.J.; Kemeyou, L.; Varpio, L. The Theoretical Integrative Review—A Reader’s Guide. J. Grad. Med. Educ. 2023, 15, 449–452. [Google Scholar] [CrossRef]
- Harari, M.B.; Parola, H.R.; Hartwell, C.J.; Riegelman, A. Literature searches in systematic reviews and meta-analyses: A review, evaluation, and recommendations. J. Vocat. Behav. 2020, 118, 103377. [Google Scholar] [CrossRef]
- McCrae, N.; Blackstock, M.; Purssell, E. Eligibility criteria in systematic reviews: A methodological review. Int. J. Nurs. Stud. 2015, 52, 1269–1276. [Google Scholar] [CrossRef]
- Chigbu, U.E.; Atiku, S.O.; Du Plessis, C.C. The science of literature reviews: Searching, identifying, selecting, and synthesising. Publications 2023, 11, 2. [Google Scholar] [CrossRef]
- Neuendorf, K.A. Content analysis and thematic analysis. In Advanced Research Method; Routledge: Oxfordshire, UK, 2018. [Google Scholar]
- Moztarzadeh, O.; Mohammad, J.; Saleh, S.; Jamshidi, A.; Baghalipour, N.; Mona Malekzadeh, M.; Hauer, L. Metaverse and Healthcare: Machine Learning-Enabled Digital Twins of Cancer. Bioengineering 2023, 10, 455. [Google Scholar] [CrossRef]
- Meijer, C.; Uh, H.W.; El Bouhaddani, S. Digital Twins in Healthcare: Methodological Challenges and Opportunities. J. Pers. Med. 2023, 13, 1522. [Google Scholar] [CrossRef] [PubMed]
- Iqbal, J.D.; Krauthammer, M.; Biller-Andorno, N. The Use and Ethics of Digital Twins in Medicine. J. Law Med. Ethics 2022, 50, 583–596. [Google Scholar] [CrossRef]
- Zalake, M. Doctors’ perceptions of using their digital twins in patient care. Sci. Rep. 2023, 13, 21693. [Google Scholar] [CrossRef] [PubMed]
- Pei-hua, H.; Ki-hun, K.; Schermer, M. Ethical Issues of Digital Twins for Personalized Health Care Service: Preliminary Mapping Study. J. Med. Internet Res. 2022, 24, e33081. [Google Scholar] [CrossRef]
- Duan, H.; Gao, S.; Yang, X.; Li, Y. The development of a digital twin concept system. Digit. Twin 2025, 2, 10. [Google Scholar] [CrossRef]
- Privacy Commissioner. Privacy Act 2020: Privacy Principles. Privacy Commissioner New Zealand. 2020. Available online: https://www.privacy.org.nz/privacy-act-2020/privacy-principles/ (accessed on 18 August 2025).
- Abdullayev, K.; Gorvett, O.; Sochiera, A.; Laidlaw, L.; Chico, T.; Manktelow, M.; Buckley, O.; Condell, J.; Richard Van, A.; Diaz, V.; et al. Stakeholder perspectives on contributors to delayed and inaccurate diagnosis of cardiovascular disease and their implications for digital health technologies: A UK-based qualitative study. BMJ Open 2024, 14, e080445. [Google Scholar] [CrossRef]
- Hu, W.; Zhang, T.; Deng, X.; Liu, Z.; Tan, J. Digital twin: A state-of-the-art review of its enabling technologies, applications and challenges. J. Intell. Manuf. Spec. Equip. 2021, 2, 1–34. [Google Scholar] [CrossRef]
- Sharma, A.; Kosasih, E.; Zhang, J.; Brintrup, A.; Calinescu, A. Digital Twins: State of the art theory and practice, challenges, and open research questions. J. Ind. Inf. Integr. 2022, 30, 100383. [Google Scholar] [CrossRef]
- Winter, P.D.; Chico, T.J.A. Using the Non-Adoption, Abandonment, Scale-Up, Spread, and Sustainability (NASSS) Framework to Identify Barriers and Facilitators for the Implementation of Digital Twins in Cardiovascular Medicine. Sensors 2023, 23, 6333. [Google Scholar] [CrossRef] [PubMed]
- Ferlito, B.; De Proost, M.; Segers, S. Navigating the Landscape of Digital Twins in Medicine: A Relational Bioethical Inquiry. Asian Bioeth. Rev. 2024, 16, 471–481. [Google Scholar] [CrossRef] [PubMed]
- Vidovszky, A.A.; Fisher, C.K.; Loukianov, A.D.; Smith, A.M.; Tramel, E.W.; Walsh, J.R.; Ross, J.L. Increasing acceptance of AI-generated digital twins through clinical trial applications. Clin. Transl. Sci. 2024, 17, e13897. [Google Scholar] [CrossRef]
- Lehmann, J.; Lorenz, G.; Browne, R.; Ogawa, T.; Kokubun, K.; Taki, Y.; Jokinen, K.; Janboecke, S.; Lohr, C.; Wieching, R.; et al. Digital Twins for Supporting Ageing Well: Approaches in Current Research and Innovation in Europe and Japan. Sustainability 2024, 16, 3064. [Google Scholar] [CrossRef]
- Tzachor, A.; Sabri, S.; Richards, C.E.; Schlüter, M.; Ruckelshaus, M.; Creutzig, F. Potential and limitations of digital twins to achieve the Sustainable Development Goals. Nat. Sustain. 2022, 5, 822–829. [Google Scholar] [CrossRef]
- Armeni, P.; Polat, I.; De Rossi, L.M.; Diaferia, L.; Meregalli, S.; Gatti, A. Digital Twins in Healthcare: Is It the Beginning of a New Era of Evidence-Based Medicine? A Critical Review. J. Pers. Med. 2022, 12, 1255. [Google Scholar] [CrossRef]
- Adibi, S.; Rajabifard, A.; Shojaei, D.; Wickramasinghe, N. Enhancing Healthcare through Sensor-Enabled Digital Twins in Smart Environments: A Comprehensive Analysis. Sensors 2024, 24, 2793. [Google Scholar] [CrossRef]
- Sun, T.; Wang, J.; Moran, S.; Liu, X.; Huang, H.; Zhang, J.; Zhang, W.; Li, Z. The Digital Twin: A Potential Solution for the Personalized Diagnosis and Treatment of Musculoskeletal System Diseases. Bioengineering 2023, 10, 627. [Google Scholar] [CrossRef]
- Vasiliu-Feltes, I.; Mylrea, M.; Christina Yan, Z.; Tyler Cohen, W.; Thornley, B. Impact of Blockchain-Digital Twin Technology on Precision Health, Pharmaceutical Industry, and Life Sciences Conv2X 2023 Report. Blockchain Healthc. Today 2023, 6. Available online: https://blockchainhealthcaretoday.com/index.php/journal/article/view/281 (accessed on 18 August 2025). [CrossRef]
- Coorey, G.; Figtree, G.A.; Fletcher, D.F.; Snelson, V.J.; Vernon, S.T.; Winlaw, D.; Grieve, S.M.; McEwan, A.; Yang, J.Y.H.; Qian, P.; et al. The health digital twin to tackle cardiovascular disease—A review of an emerging interdisciplinary field. NPJ Digit. Med. 2022, 5, 126. [Google Scholar] [CrossRef]
- Sahal, R.; Alsamhi, S.H.; Brown, K.N. Personal Digital Twin: A Close Look into the Present and a Step towards the Future of Personalised Healthcare Industry. Sensors 2022, 22, 5918. [Google Scholar] [CrossRef] [PubMed]
- Tardini, E.; Zhang, X.; Canahuate, G.; Wentzel, A.; Mohamed, A.S.R.; Lisanne Van, D.; Fuller, C.D.; Marai, G.E. Optimal Treatment Selection in Sequential Systemic and Locoregional Therapy of Oropharyngeal Squamous Carcinomas: Deep Q-Learning With a Patient-Physician Digital Twin Dyad. J. Med. Internet Res. 2022, 24, e29455. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Hu, H.; Wu, S. Opportunities and challenges of digital twin technology in healthcare. Chin. Med. J. 2023, 136, 2895–2896. [Google Scholar] [CrossRef] [PubMed]
- Md Shafiqur Rahman, J.; Emillia Vann, Y.; Ilodibe, A.; Eldabi, T. Ethical and Quality of Care-Related Challenges of Digital Health Twins in Older Care Settings: Protocol for a Scoping Review. JMIR Res. Protoc. 2024, 13, e51153. [Google Scholar] [CrossRef] [PubMed]
- Volkov, I.; Radchenko, G.; Tchernykh, A. Digital Twins, Internet of Things and Mobile Medicine: A Review of Current Platforms to Support Smart Healthcare. Program. Comput. Softw. 2021, 47, 578–590. [Google Scholar] [CrossRef]
- Drummond, D.; Coulet, A. Technical, Ethical, Legal, and Societal Challenges With Digital Twin Systems for the Management of Chronic Diseases in Children and Young People. J. Med. Internet Res. 2022, 24, e39698. [Google Scholar] [CrossRef]
- Lee, J.-H.; Lee, H.-L.; Park, I.-Y.; On, S.-W.; Byun, S.-H.; Yang, B.-E. Effectiveness of creating digital twins with different digital dentition models and cone-beam computed tomography. Sci. Rep. 2023, 13, 10603. [Google Scholar] [CrossRef]
- Adel, A.; HSAlani, N. Human-Centric Collaboration and Industry 5.0 Framework in Smart Cities and Communities: Fostering Sustainable Development Goals 3, 4, 9, and 11 in Society 5.0. Smart Cities 2024, 7, 1723–1775. [Google Scholar] [CrossRef]
- Kolokotroni, E.; Abler, D.; Ghosh, A.; Tzamali, E.; Grogan, J.; Georgiadi, E.; Büchler, P.; Radhakrishnan, R.; Byrne, H.; Sakkalis, V.; et al. A Multidisciplinary Hyper-Modeling Scheme in Personalized In Silico Oncology: Coupling Cell Kinetics with Metabolism, Signaling Networks, and Biomechanics as Plug-In Component Models of a Cancer Digital Twin. J. Pers. Med. 2024, 14, 475. [Google Scholar] [CrossRef]
- Cho, R.-Y.; Soo-Hwan, B.; Sang-Min, Y.; Hee-Ju, A.; Yoo-Sung, N.; Park, I.-Y.; Sung-Woon, O.; Jong-Cheol, K.; Byoung-Eun, Y. Comparative Analysis of Three Facial Scanners for Creating Digital Twins by Focusing on the Difference in Scanning Method. Bioengineering 2023, 10, 545. [Google Scholar] [CrossRef]
- Gazerani, P. Intelligent Digital Twins for Personalized Migraine Care. J. Pers. Med. 2023, 13, 1255. [Google Scholar] [CrossRef]
- Kaul, R.; Ossai, C.; Forkan, A.R.M.; Jayaraman, P.P.; Zelcer, J.; Vaughan, S.; Wickramasinghe, N. The role of AI for developing digital twins in healthcare: The case of cancer care. Wiley Interdiscip. Rev. Data Min. Knowl. Discov. 2023, 13, e1480. [Google Scholar] [CrossRef]
- Cen, S.; Gebregziabher, M.; Moazami, S.; Azevedo, C.J.; Pelletier, D. Toward precision medicine using a “digital twin” approach: Modeling the onset of disease-specific brain atrophy in individuals with multiple sclerosis. Sci. Rep. 2023, 13, 16279. [Google Scholar] [CrossRef] [PubMed]
- Hassani, H.; Huang, X.; MacFeely, S. Impactful Digital Twin in the Healthcare Revolution. Big Data Cogn. Comput. 2022, 6, 83. [Google Scholar] [CrossRef]
- Ebiloma, D.O.; Aigbavboa, C.O.; Anumba, C. Towards Digital Twin Maintenance Management of Health Facilities in Nigeria: The Need for Maintenance Documentation. Buildings 2023, 13, 1339. [Google Scholar] [CrossRef]
- Emmert-Streib, F.; Yli-Harja, O. What Is a Digital Twin? Experimental Design for a Data-Centric Machine Learning Perspective in Health. Int. J. Mol. Sci. 2022, 23, 13149. [Google Scholar] [CrossRef]
- Chakshu Neeraj, K.; Sazonov, I.; Nithiarasu, P. Towards enabling a cardiovascular digital twin for human systemic circulation using inverse analysis. Biomech. Model. Mechanobiol. 2021, 20, 449–465. [Google Scholar] [CrossRef]
- Yeman, R. The Application of Agile to Large-Scale, Safety-Critical, Cyber-Physical Systems. Ph.D. Thesis, Colorado State University, Fort Collins, CO, USA, 2025. [Google Scholar]
- Basaure, V. Models in medicine: The digital twin for health. Ser. Selección De Textos 2025, 10, 3–16. [Google Scholar] [CrossRef]
- Botín-Sanabria, D.M.; Mihaita, A.S.; Peimbert-García, R.E.; Ramírez-Moreno, M.A.; Ramírez-Mendoza, R.A.; Lozoya-Santos, J.D.J. Digital twin technology challenges and applications: A comprehensive review. Remote Sens. 2022, 14, 1335. [Google Scholar] [CrossRef]
- Fagherazzi, G. Deep Digital Phenotyping and Digital Twins for Precision Health: Time to Dig Deeper. J. Med. Internet Res. 2020, 22, e16770. [Google Scholar] [CrossRef] [PubMed]
- Calcaterra, V.; Pagani, V.; Zuccotti, G. Digital Twin: A Future Health Challenge in Prevention, Early Diagnosis and Personalisation of Medical Care in Paediatrics. Int. J. Environ. Res. Public Health 2023, 20, 2181. [Google Scholar] [CrossRef] [PubMed]
- Corrin, L.; Thompson, K.; Hwang, G.-J.; Lodge, J.M. The importance of choosing the right keywords for educational technology publications. Australas. J. Educ. Technol. 2022, 38, 1–8. [Google Scholar] [CrossRef]
- Adel, A.; Alani, N.H.S.; Jan, T. Factories of the future in industry 5.0—Softwarization, servitization, and industrialization. Internet Things 2024, 24, 101431. [Google Scholar] [CrossRef]
- Sigawi, T.; Yaron, I. Using Constrained-Disorder Principle-Based Systems to Improve the Performance of Digital Twins in Biological Systems. Biomimetics 2023, 8, 359. [Google Scholar] [CrossRef]
- John, L.K. Harnessing Cloud Infrastructure for DevOps Excellence. Int. J. Comput. Exp. Sci. Eng. 2025, 11, 2. [Google Scholar] [CrossRef]
- Papachristou, K.; Katsakiori, P.F.; Papadimitroulas, P.; Strigari, L.; Kagadis, G.C. Digital Twins’ Advancements and Applications in Healthcare, Towards Precision Medicine. J. Pers. Med. 2024, 14, 1101. [Google Scholar] [CrossRef]
- Mousavi, V.; Rashidi, M.; Mohammadi, M.; Samali, B. Evolution of Digital Twin Frameworks in Bridge Management: Review and Future Directions. Remote Sens. 2024, 16, 1887. [Google Scholar] [CrossRef]




| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Peer-reviewed journal articles | Non-peer-reviewed sources such as opinion pieces, editorials, and conference abstracts without full papers |
| Published between 2019 and 2024 | Articles published before 2019 |
| Focus on the adoption or application of Digital Twins in healthcare settings | Articles focused on Digital Twins in non-healthcare domains, such as Digital Twins in manufacturing, aerospace, etc. |
| Discusses clinical relevance, patient care, implementation, or ethical/technical aspects of DT in healthcare | Articles lacking methodological transparency or practical relevance |
| Written in English | Articles published in other languages |
| Available as full text | Abstract-only records or inaccessible publications |
| Model/Concept | Typical DT-in-Healthcare Use | Supported Reference | How is it Used in the Cited Work |
|---|---|---|---|
| System Theory | Integrating real-time data, sensors, and physical entities into one cohesive “patient–twin” system | Katsoulakis et al., 2024 [6]; Laubenbacher et al., 2022 [10] | Both papers describe DT platforms as systems of systems that continuously blend clinical and cyber data streams |
| Simulation Concept | Risk-free experimentation and virtual trials | Rudnicka et al., 2024 [7]; Avanzato et al., 2024 [13] | Cardiac DT and lung DT frameworks run thousands of simulated treatment scenarios before real-world application |
| Cyber-Network System Theory (CPS) | Tight, real-time coupling of IoT devices with their digital replicas | Dang et al., 2023 [8]; Mohapatra and Bose, 2020 [11] | Both describe DTs as cyber–physical systems where bedside devices feed live data to the twin for ICU decision support |
| Forecast Analytical Concept | AI/ML models that predict disease progression or therapy response | Chu et al., 2023 [9]; Vallée 2023 [12] | Diabetes DTs and system-level DTs rely on ML forecasts to adjust insulin or resource allocation proactively |
| Human–Computer Collaboration Concept | Clinician + DT co-decision workflows, XR visualisation for operators | Konopik et al., 2023 [14]; Wickramasinghe et al., 2023 [16] | Both papers study how clinicians interact with DT dashboards and XR overlays to fine-tune cancer and workflow decisions |
| Decision-Making System Theory | Real-time, data-driven clinical decision support layers atop the DT | Dang et al., 2023 [8]; Turab and Jamil, 2023 [15] | Stroke DT Delphi rules and metaverse-enabled DTs highlight algorithmic triage and automated alerts for rapid action |
| Supporting Reference | Risk Description | Likelihood | Impact | Mitigation Strategy | Responsible Party |
|---|---|---|---|---|---|
| [26] | Data privacy breach | High | Critical | Enforce strict data encryption and access control | IT Security Officer |
| [11] | Incompatibility with legacy systems | Medium | High | Use middleware or APIs for integration | Systems Integration Manager |
| [6] | Patient data inaccuracies | High | High | Regular data audits and validation protocols | Data Analyst |
| [27] | Lack of clinician training on DT use | Medium | Medium | Conduct regular training sessions | HR & Clinical Trainer |
| [28] | Ethical concerns regarding AI-based decision-making | High | High | Establish an ethics review committee | Compliance & Ethics Officer |
| [29] | High cost of implementation | Medium | High | Seek phased rollout and apply for innovation grants | Finance & Project Manager |
| [30] | Regulatory non-compliance (e.g., privacy laws) | Low | Critical | Regular legal audits, compliance documentation | Legal Advisor |
| [31] | Resistance from staff or clinicians | Medium | Medium | Awareness campaigns and stakeholder involvement | Change Management Lead |
| [32] | Cybersecurity threats | High | Critical | Employ multi-layered cyber defence systems | Cybersecurity Team |
| [33] | Over-reliance on DTs, reducing human judgement | Medium | High | Maintain hybrid decision models with human oversight | Clinical Governance Lead |
| [34] | Interoperability issues across departments | Medium | High | Standardise data protocols and integration frameworks | IT Architect |
| [35] | Legal liabilities from incorrect DT simulations | Low | High | Test extensively and ensure liability insurance | Legal & Risk Team |
| [36] | Misinterpretation of predictive analytics | Medium | Medium | Provide guidelines for data interpretation | Data Science Lead |
| [37] | Inequitable patient access to DT-powered care | Medium | High | Develop policies for inclusive access | Policy Advisor |
| [38] | Environmental risks from tech infrastructure | Low | Medium | Opt for green IT solutions and e-waste management | Sustainability Officer |
| Study | Focus Area | Methodology | Key Findings |
|---|---|---|---|
| [6] | Digital Twins’ wide range of use in healthcare | Comprehensive literature analysis | Investigates the use of DTs in clinical systems, outlining gaps in forecasting analytics and adoption issues |
| [23] | Combination of metaverse and DTs in cancer therapy | Comprehensive case-study methodology integrated with an analytical approach | Discussing ML-powered DT models in cancer treatment, showcasing their part in metaverse for delivering advanced and collaborative patient care |
| [14] | Digital Twins’ application in breast cancer therapy | Semi-structured interviews with 14 breast cancer patients | Illustrates DTs’ challenges and concerns in breast cancer, indicating technological, operational, and ethical considerations |
| [45] | Digital Twins in cancer care | Deep Q-learning model | Highlights the potential of DTs for enhanced therapy choice, indicating the impacts of AI in customised patient treatments |
| [9] | Digital Twin use in diabetes control | Comprehensive mixed methodology | Explains DTs’ ability for tailored control over diabetes, including customising care based on patient reaction prediction |
| [27] | Doctor’s understanding about Digital Twins in patient treatments | Reflexive thematic–qualitative approach | Analyses about practitioners’ understanding of DT models, highlighting issues about data safety, privacy, and potential harm to doctors’ autonomy |
| [41] | Musculoskeletal detection and treatment using DTs | Case study | Evaluates how DTs function for customised diagnosis and care in musculoskeletal issues, showing the high-level opportunities in orthopaedics |
| [44] | Personal Digital Twin (PDT) utilisation in healthcare | Literature review | Assesses the ability of PDT models in optimising personalised treatment, analysing limitations in data privacy and administrative processes across the tailored clinical practices |
| [8] | Smart medical frameworks using artificial intelligence | Quantitative and qualitative methodologies using the DELPHI Consensus technique | Discusses the health system using AI and its capability to assist tailored patient care, highlighting DTs key role in smart and innovative healthcare settings |
| Medical Field | Use Case | Technology Integrated | Clinical Function | Impact | Limitations/Challenges | Reference |
|---|---|---|---|---|---|---|
| Cardiology | Heart model simulation | IoT + AI + XR | Diagnosis and risk modelling | Better diagnosis, risk prediction | Data integration and real-time synchronisation | [8] |
| Oncology | Breast cancer treatment personalisation | ML, VR | Predictive modelling | Tailored chemo protocols | Model bias and scalability | [24] |
| Diabetes | Continuous glucose monitoring + predictive modelling | Wearables + AI | Real-time monitoring | Adaptive insulin delivery | Privacy concerns with wearable data | [9] |
| Orthopaedics | Musculoskeletal simulations | XR, sensor integration | Biomechanical modelling | Biomechanical optimisation | High sensor precision requirement | [41] |
| Smart Environments | Real-time clinical assessments | AI, ML, IoT | Ambient monitoring | Continuous patient monitoring | Security vulnerabilities in smart networks | [40] |
| General Medicine | Prediction of treatment outcomes | AI, simulation | Decision support | Evidence-based treatment planning | Interpretability of AI decisions | [39] |
| Healthcare Systems | Resource optimisation | IoT + AI | Operational management | Improved efficiency and responsiveness | Interoperability issues with legacy systems | [1] |
| Personalised Care | Predictive analytics for treatment planning | AI, blockchain | Individualised therapy | Tailored treatment suggestions | Ethical concerns with data ownership | [44] |
| Respiratory Care | Lung disease diagnostics | IoT sensors + ML | Diagnostic imaging | Real-time chest X-ray analysis | Need for robust image training datasets | [13] |
| Elderly Care | Health monitoring for seniors | HDT + AI | Geriatric monitoring | Support for independent living | Limited device access in low-income settings | [47] |
| Paediatrics | Child-specific device regulation | Custom IoT devices | Paediatric screening | Improved safety and diagnostics | Usability concerns with younger patients | [49] |
| Policy and Regulation | Ethical frameworks for DTs | AI, consent Protocols | Health governance | Safer data governance | Jurisdictional variation in laws | [28] |
| Doctor Representation | Digital Twins of Doctors (DTDs) | Simulation + data modelling | Training and simulation | Medical expertise replication | Concerns about autonomy and over-reliance | [27] |
| Breast Oncology | Stakeholder engagement in DT adoption | VR + digital modelling | Stakeholder-centred design | Improved patient-centred care | Varying stakeholder concerns | [14] |
| Diagnostics | Virtual patient replication | ML, simulation | Virtual trials | Advanced diagnosis accuracy | Model validity and generalisation | [45] |
| Chronic Disease | Individualised treatment response prediction | Wearables + ML | Long-term care Management | Optimised chronic care | Sensor fatigue and system calibration | [44] |
| Neuroscience | Simulation of neural activities | AI, predictive analytics | Cognitive disorder Modelling | Improved cognitive care strategies | Difficulty simulating complex neural behaviour | [36] |
| Migraine Care | Pattern analysis of triggers | Digital logs + AI | Preventative care | Personalised trigger avoidance plans | Need for long-term user input | [54] |
| General Practice | Clinician adaptation to DTs | Survey + thematic analysis | Attitude research | Awareness of DTs’ limitations | Sample size limitations | [27] |
| Public Health | Privacy regulations in digital health | Legal frameworks + AI | Data ethics and regulation | Stronger data control | Disparities in data law enforcement | [46] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sasitharasarma, S.; Alani, N.H.S.; Wisker, Z.L. Is the Healthcare Industry Ready for Digital Twins? Examining the Opportunities and Challenges. Future Internet 2025, 17, 386. https://doi.org/10.3390/fi17090386
Sasitharasarma S, Alani NHS, Wisker ZL. Is the Healthcare Industry Ready for Digital Twins? Examining the Opportunities and Challenges. Future Internet. 2025; 17(9):386. https://doi.org/10.3390/fi17090386
Chicago/Turabian StyleSasitharasarma, Srinivasini, Noor H. S. Alani, and Zazli Lily Wisker. 2025. "Is the Healthcare Industry Ready for Digital Twins? Examining the Opportunities and Challenges" Future Internet 17, no. 9: 386. https://doi.org/10.3390/fi17090386
APA StyleSasitharasarma, S., Alani, N. H. S., & Wisker, Z. L. (2025). Is the Healthcare Industry Ready for Digital Twins? Examining the Opportunities and Challenges. Future Internet, 17(9), 386. https://doi.org/10.3390/fi17090386







