A Digital Health Platform for Remote and Multimodal Monitoring in Neurodegenerative Diseases
Abstract
1. Introduction
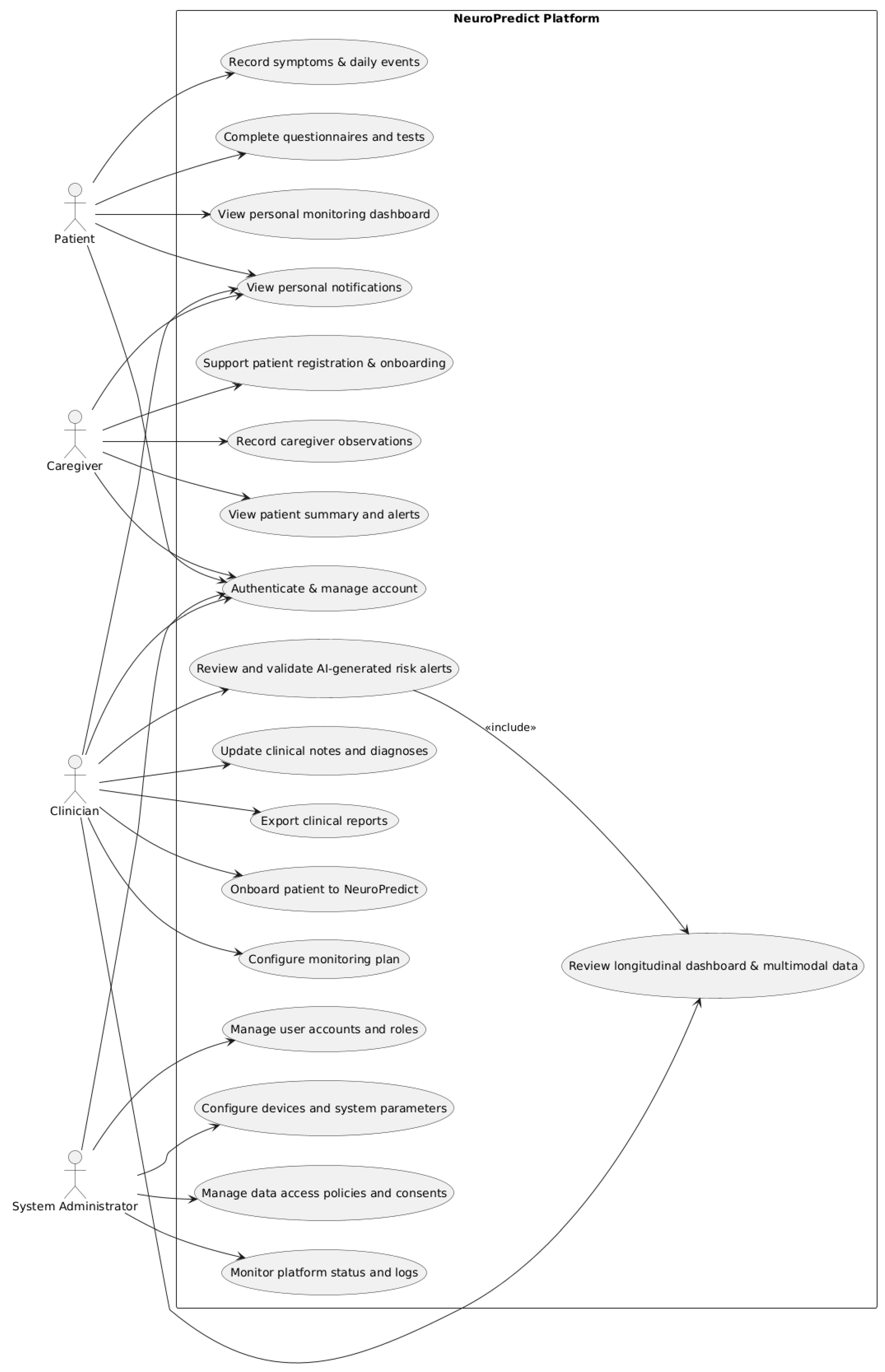
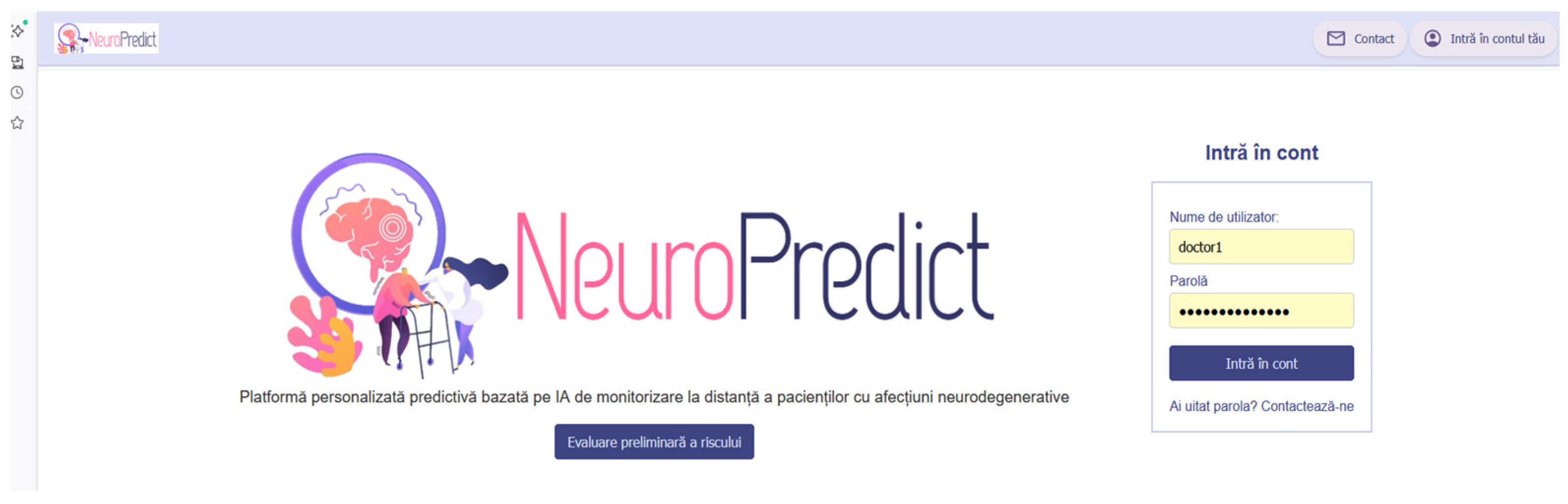
2. Materials and Methods
2.1. Platform Architecture and Technological Foundation
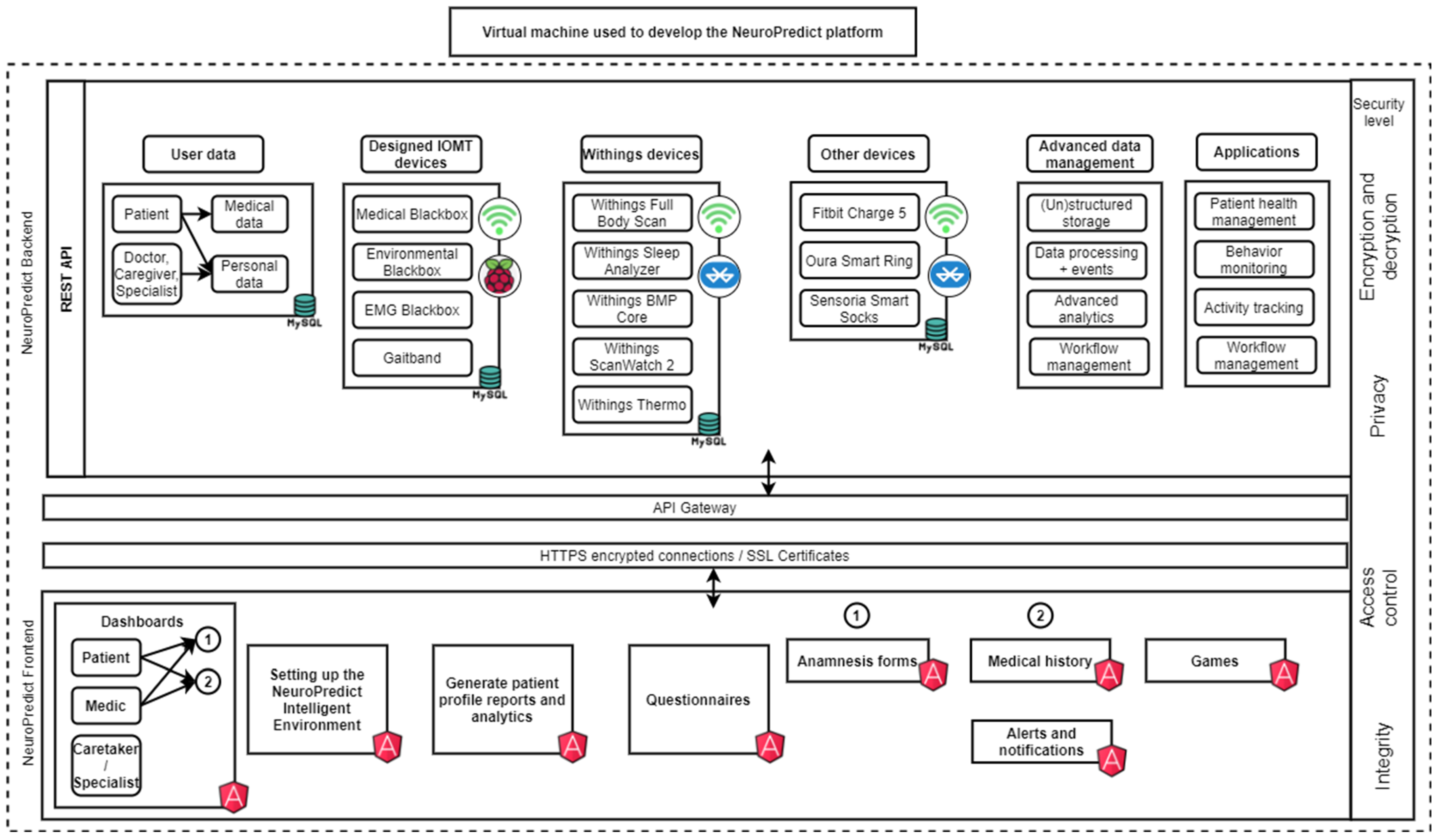
2.1.1. Platform Architecture
- Angular 17 and TypeScript 3.4 were used to build modular and scalable components (e.g., role-specific dashboards), which simplify data organization and user flow.
- Angular’s Reactive Extensions for JavaScript 7.8 library was used to handle data streams in real time, thus enabling health monitoring and the sending of alerts when thresholds are exceeded.
- Tailwnd CSS 3.4 and Sassy CSS (SCSS) 1.77 helped design coherent and visually attractive user interfaces.
- HTML5 and CSS3 were used to develop the structural foundation of the interface, facilitating navigation and good visual feedback.
- PHP 8.2 manages the interaction between the frontend and the database.
- C# 12.0 handles the core functionality for health data processing.
- C++ 20 was used for context, requiring high-performance computing like managing and analyzing complex physiological datasets.
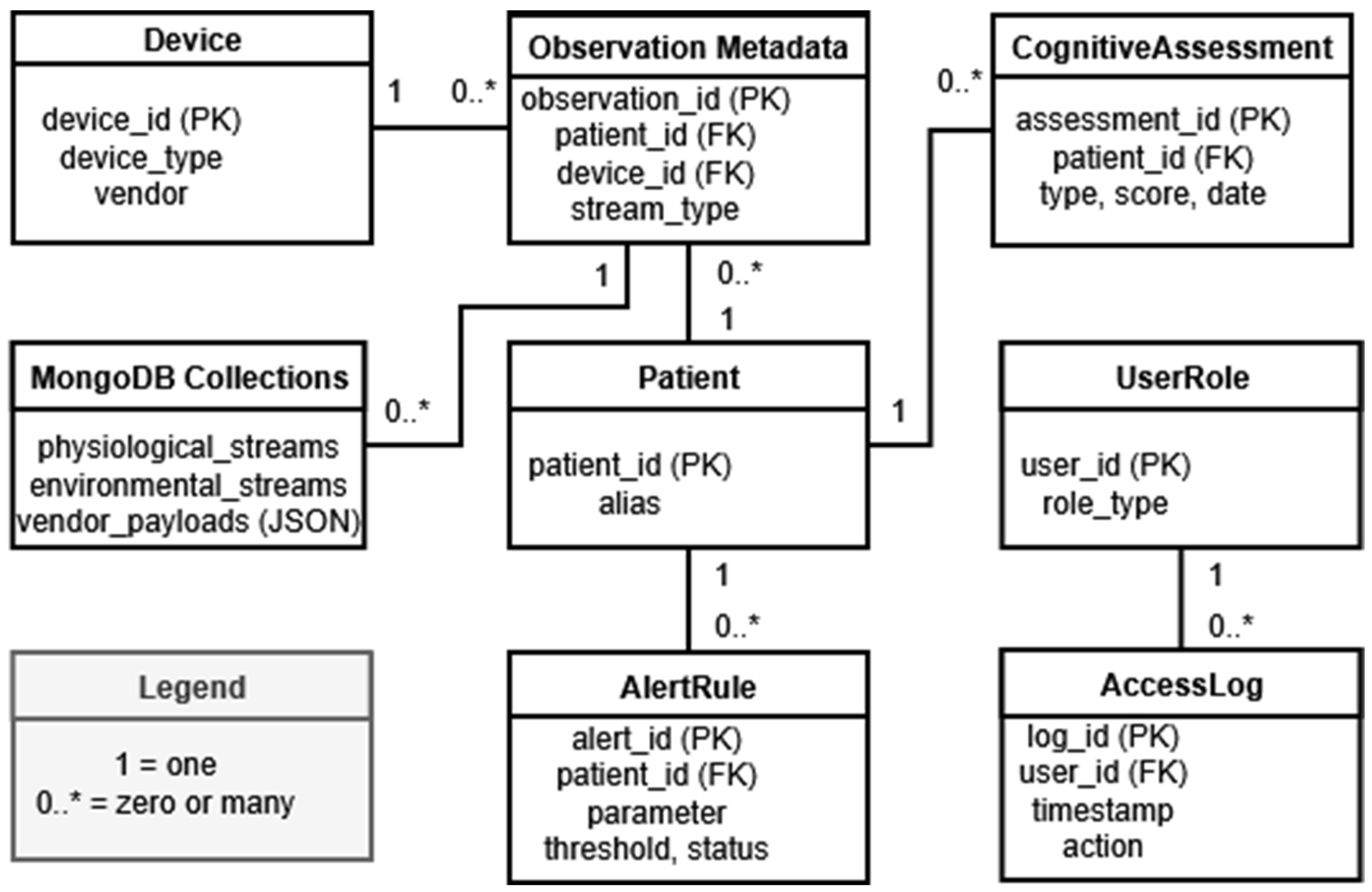
- MySQL 8.0 handles structured data, while MongoDB handles semi-structured or unstructured data, ensuring flexibility and scalability in storing real-time and big data.
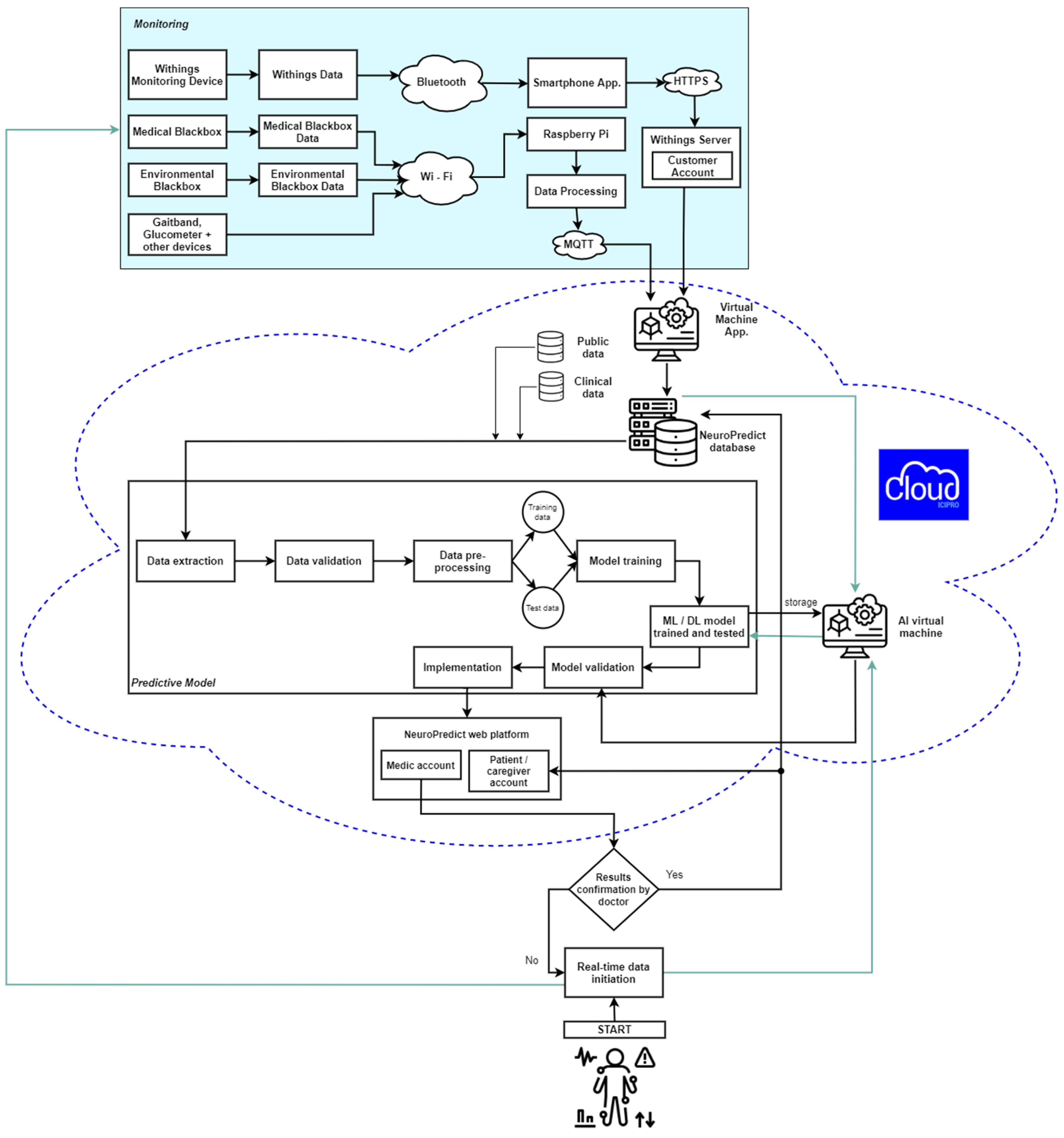
2.1.2. Infrastructure
- The Romanian national cloud service for public institutions (ICIPRO): A cloud service used for testing and experimentation within regulatory boundaries in Romanian public institutions.
- Microsoft Azure, under an infrastructure as a service (IaaS) model: A scalable cloud service for development, testing, and deployment.
2.1.3. Security and Privacy Principles
- Role-Based Access Control (RBAC), ensuring that users only have access to data and functionality that are relevant to their role, thus preventing unauthorized access.
- Encryption of all data exchanged between clients and servers using Transport Layer Security/Secure Sockets Layer (TLS/SSL) protocols, ensuring data integrity and confidentiality.
- Secure communication by using the HTTPS protocol, ensuring data integrity and confidentiality during transmission.
- Secure, stateless user authentication, using JSON Web Tokens (JWT).
2.2. Integration of IoMT Devices in the NeuroPredict Platform
2.2.1. Commercial Wearables
2.2.2. In-House Developed Devices
- The Medical “Blackbox” integrates electrocardiography (ECG) (AD8232), respiratory flow meters (SFM3300-D), peripheral capillary oxygen saturation (SpO2), and temperature probes [8,34]. It was developed on ESP32 and Raspberry Pi microcontrollers and supports local preprocessing and encrypted data transmission. On the NeuroPredict platform, it allows for continuous recording of cardiovascular and muscular signals.
- The Ambiental “Blackbox” records environmental data by integrating sensors for air quality (carbon dioxide (CO2), volatile organic compounds (VOC)), ambient temperature, humidity, light intensity, and motion. Such data are important when analyzing sleep quality, fatigue, and symptom changes in AD and PD [8,34].
- The EMG “Blackbox” is a dedicated electromyographic acquisition system which uses MyoWare 2.0 modules and wireless shields. It produces high-resolution EMG recordings, which are matched with accelerometer and gait signals and sent over ESP32 microcontrollers [35]. The EMG “Blackbox” has been tested for muscle activation analysis in a laboratory context.
- The Gaitband is a wearable device which includes accelerometers, gyroscopes, and pressure sensors to monitor gait in terms of its features [8,34]. It has a higher resolution and granularity than standard activity trackers, which allows it to be used to identify early changes in gait. This can help discover impairments that are not clinically visible and that are associated with disease progression in PD and MS [36,37,38].
2.2.3. Connectivity and Interoperability
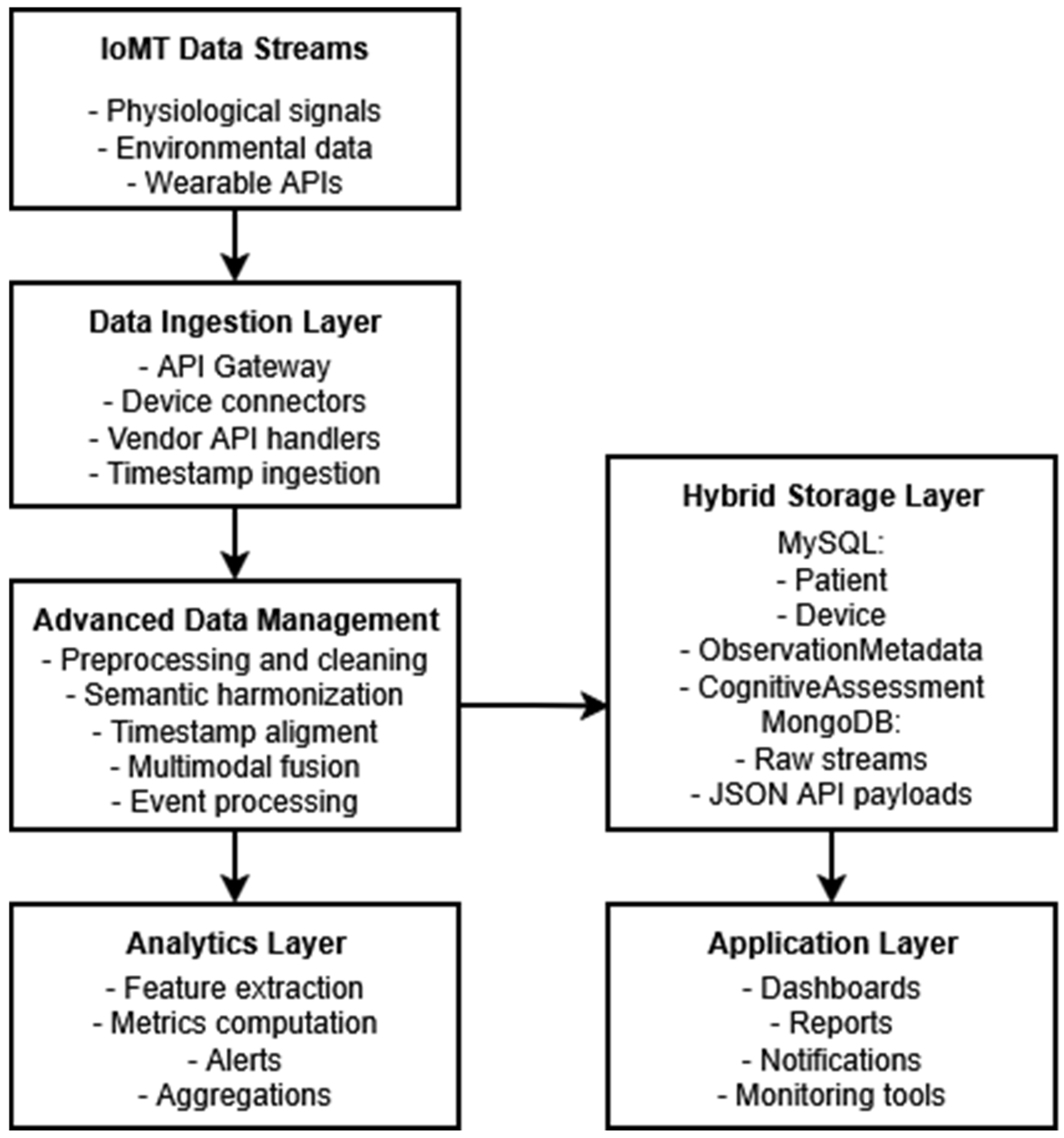
2.3. Multisource Data Collection, Preprocessing, and Secure Management
2.3.1. Multisource Data Collection and Integration
2.3.2. Data Transmission and Synchronization
2.3.3. Preprocessing Pipelines and Feature Extraction
- Initial Data Validation and Normalization: The received data are logically validated and made into a consistent predefined format to ensure their integrity and compatibility.
- Encryption Plans (Secure Hashing Algorithm (SHA) + Advanced Encryption Standard (AES)): The NeuroPredict platform uses SHA for data integrity and identity verification and AER for encrypting health data before storage.
- JWT: The architecture of the NeuroPredict platform includes mechanisms to separate user identities from sensitive data. JWT allows for secure, stateless authentication and secure token storage mechanisms integrated into the design to manage session integrity and access control.
2.3.4. Cloud Storage and Data Security
2.3.5. From Data Processing to Knowledge Extraction
- Daily summaries on heart rate, heart rate variability, and sleep metrics.
- Gait analysis and EMG metrics: preliminary processing pipelines for them are currently being evaluated in terms of reliability and clinical relevance using pilot data
2.3.6. User Interaction Interfaces
2.4. Human-Centered Design Considerations
3. Results
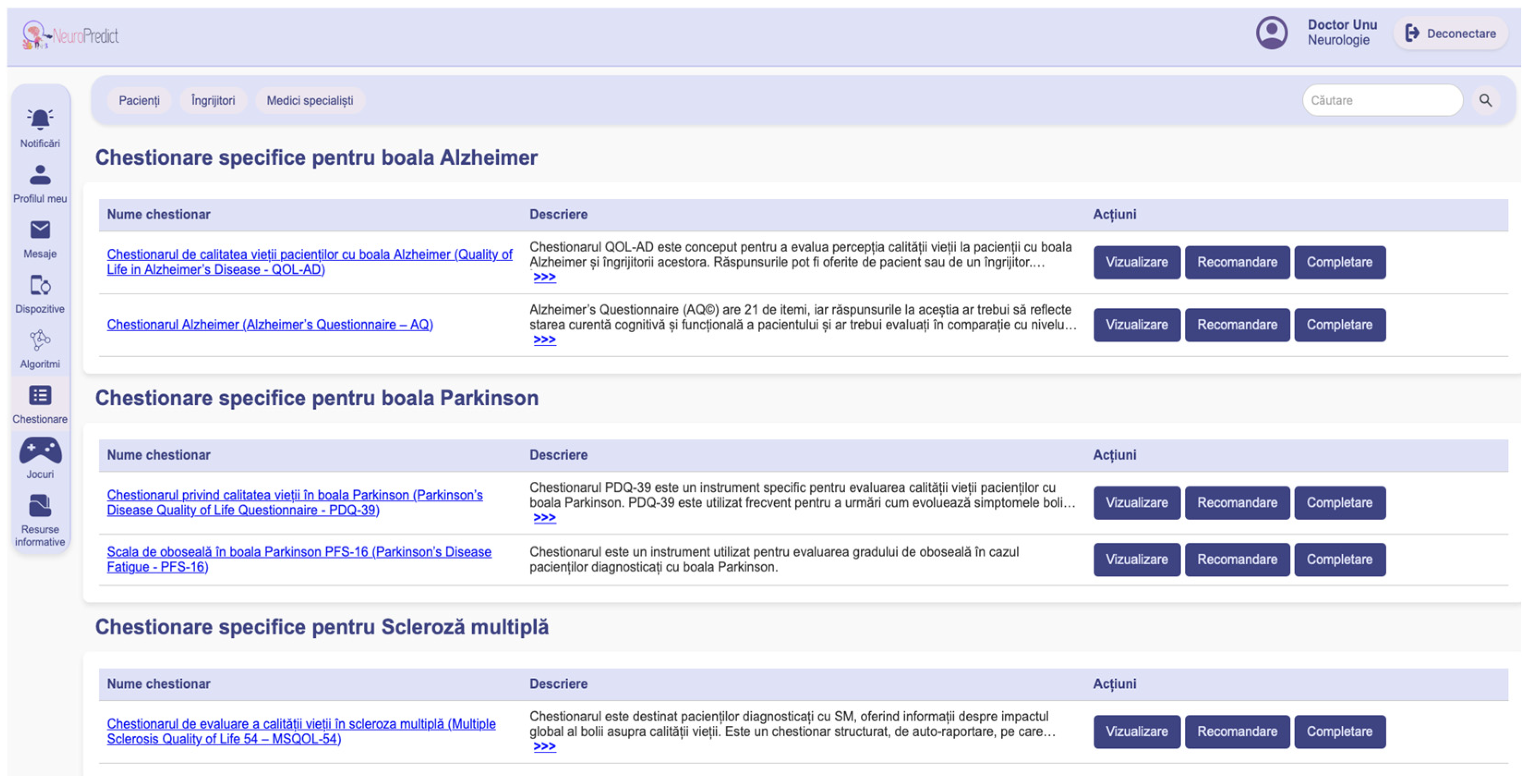
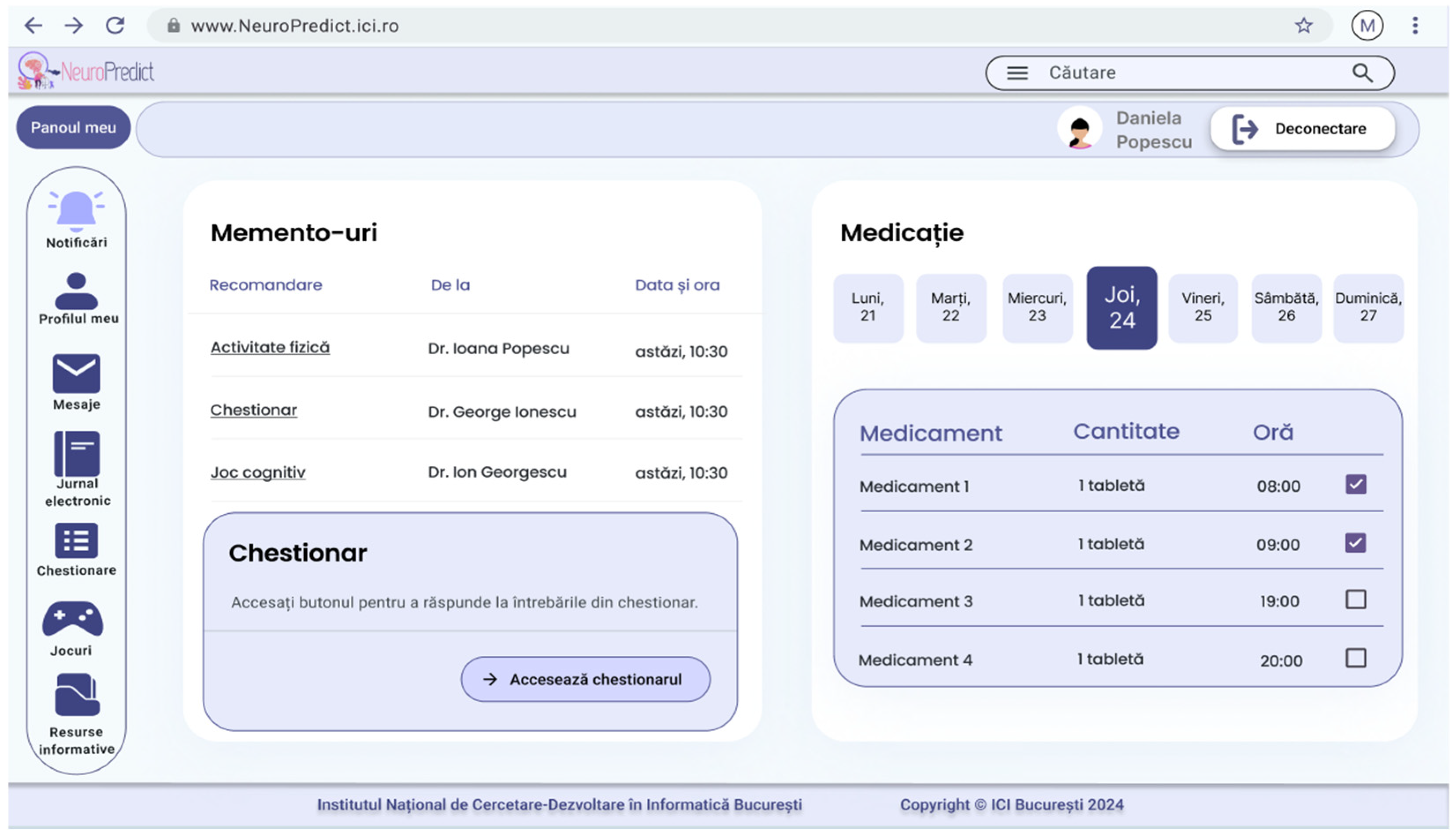
3.1. Dashboards
3.2. Cognitive and Behavioral Assessments
3.3. Patient Empowerment and Engagement
4. Discussion
4.1. Usability and Patient Empowerment
4.2. Related Work and Comparison with Related eHealth Approaches
4.3. Ethical and Regulatory Considerations
4.4. System Responsiveness and Future Extensions
4.5. Limitations and Current Maturity Level
5. Conclusions
- User interface/experience enhancements: Current plans include improving the platform’s responsiveness and its feedback mechanisms, such that the interaction between end-users across clinical and research domains can be facilitated. Ongoing usability testing will guide other improvements.
- Clinical validation planning: Once it reaches technical maturity, the NeuroPredict platform will undergo clinical evaluation at partner healthcare institutions. The aims will be to check its performance, diagnostic utility, and clinician acceptance.
- Regulatory compliance: The platform is already designed with compliance with the EU AI Act and certification as a high-risk AI system under healthcare classifications in mind. For example, for the latter, the platform already includes transparency mechanisms.
- EMR interoperability: The NeuroPredict platform will adopt healthcare data standards such as HL7 and FHIR, which will support its interoperability with EMR systems. This will enable its monitoring insights to be transmitted to the EMR, thus increasing its utility in clinical settings.
- Research platform for computational medicine: The NeuroPredict platform is also intended as a modular, extensible research platform that supports studies in computational medicine. It will be possible to extend it to integrate with other devices to collect different types of bio signal data and set it up with personalized health metrics for longitudinal patient monitoring.
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Abbreviations
| AAMI | Association for the Advancement of Medical Instrumentation |
| AD | Alzheimer’s disease |
| AES | Advanced Encryption Standard |
| AI | Artificial Intelligence |
| API | Application Programming Interface |
| BMI | Body Mass Index |
| CO2 | Carbon Dioxide |
| ECG | Electrocardiography |
| EMG | Electromyography |
| EMR | Electronic Medical Record |
| EU AI Act | European Union Artificial Intelligence Act |
| FDA | U.S. Food and Drug Administration |
| FHIR | Fast Healthcare Interoperability Resources |
| GDPR | General Data Protection Regulation |
| GSM | Global System for Mobile Communications |
| HL7 | Health Level Seven |
| HTTPS | Hypertext Transfer Protocol Secure |
| IaaS | Infrastructure as a Service |
| ICIPRO | Romanian National Cloud Service for Public Institutions |
| IoMT | Internet of Medical Things |
| ISO | International Organization for Standardization |
| IVDR | In Vitro Diagnostic Regulation |
| JSON | JavaScript Object Notation |
| JWT | JSON Web Token |
| MDR | Medical Device Regulation |
| MDCG | Medical Device Coordination Group |
| ML | Machine Learning |
| MMSE | Mini-Mental State Examination |
| MoCA | Montreal Cognitive Assessment |
| MS | Multiple Sclerosis |
| MQTT | Message Queuing Telemetry Transport |
| PD | Parkinson’s disease |
| RBAC | Role-Based Access Control |
| SHA | Secure Hash Algorithm |
| SpO2 | Peripheral Capillary Oxygen Saturation |
| SSL | Secure Sockets Layer |
| TLS | Transport Layer Security |
| TRL | Technology Readiness Level |
| VOC | Volatile Organic Compounds |
References
- European Commission. Directorate-General for Economic and Financial Affairs 2024 Ageing Report. Economic and Budgetary Projections for the EU Member States (2022–2070); European Commission: Brussels, Belgium, 2024. [Google Scholar]
- Hou, Y.; Dan, X.; Babbar, M.; Wei, Y.; Hasselbalch, S.G.; Croteau, D.L.; Bohr, V.A. Ageing as a Risk Factor for Neurodegenerative Disease. Nat. Rev. Neurol. 2019, 15, 565–581. [Google Scholar] [CrossRef]
- Junaid, M.; Ali, S.; Eid, F.; El-Sappagh, S.; Abuhmed, T. Explainable Machine Learning Models Based on Multimodal Time-Series Data for the Early Detection of Parkinson’s Disease. Comput. Methods Programs Biomed. 2023, 234, 107495. [Google Scholar] [CrossRef]
- Paraschiv, E.; Petrache, C.; Bica, O.; Vasilevschi, A. Fall Detection System: Continuous in-Home Monitoring of Parkinson’s Patients. In Proceedings of the 2022 E-Health and Bioengineering Conference (EHB), Iași, Romania, 17–18 November 2022; pp. 1–4. [Google Scholar]
- Stara, V.; Soraci, L.; Takano, E.; Kondo, I.; Möller, J.; Maranesi, E.; Luzi, R.; Riccardi, G.R.; Browne, R.; Dacunha, S.; et al. Intrinsic Capacity and Active and Healthy Aging Domains Supported by Personalized Digital Coaching: Survey Study Among Geriatricians in Europe and Japan on EHealth Opportunities for Older Adults. J. Med. Internet Res. 2023, 25, e41035. [Google Scholar] [CrossRef] [PubMed]
- Ianculescu, M.; Paraschiv, E.-A.; Alexandru, A. Addressing Mild Cognitive Impairment and Boosting Wellness for the Elderly through Personalized Remote Monitoring. Healthcare 2022, 10, 1214. [Google Scholar] [CrossRef] [PubMed]
- Kurlan, R.; Richard, I.H.; Papka, M.; Marshall, F. Movement Disorders in Alzheimer’s Disease: More Rigidity of Definitions Is Needed. Mov. Disord. 2000, 15, 24–29. [Google Scholar] [CrossRef] [PubMed]
- Sandulescu, V.; Ianculescu, M.; Valeanu, L.; Alexandru, A. Integrating IoMT and AI for Proactive Healthcare: Predictive Models and Emotion Detection in Neurodegenerative Diseases. Algorithms 2024, 17, 376. [Google Scholar] [CrossRef]
- Balakrishnan, A.; Medikonda, J.; Namboothiri, P.K.; Natarajan, M. Role of Wearable Sensors with Machine Learning Approaches in Gait Analysis for Parkinson’s Disease Assessment: A Review. Eng. Sci. 2022, 19, 5–19. [Google Scholar] [CrossRef]
- Antonini, A.; Reichmann, H.; Gentile, G.; Garon, M.; Tedesco, C.; Frank, A.; Falkenburger, B.; Konitsiotis, S.; Tsamis, K.; Rigas, G.; et al. Toward Objective Monitoring of Parkinson’s Disease Motor Symptoms Using a Wearable Device: Wearability and Performance Evaluation of PDMonitor®. Front. Neurol. 2023, 14, 1080752. [Google Scholar] [CrossRef]
- Bakirtzis, C.; Ioannidis, P.; Messinis, L.; Nasios, G.; Konstantinopoulou, E.; Papathanasopoulos, P.; Grigoriadis, N. The Rationale for Monitoring Cognitive Function in Multiple Sclerosis: Practical Issues for Clinicians. Open Neurol. J. 2018, 12, 31–40. [Google Scholar] [CrossRef]
- Tea, F.; Groh, A.M.R.; Lacey, C.; Fakolade, A. A scoping review assessing the usability of digital health technologies targeting people with multiple sclerosis. npj Digit. Med. 2024, 7, 168. [Google Scholar] [CrossRef]
- Gallo, G.D.; Micucci, D. Internet of Medical Things Systems Review: Insights into Non-Functional Factors. Sensors 2025, 25, 2795. [Google Scholar] [CrossRef] [PubMed]
- Al Khatib, I.; Shamayleh, A.; Ndiaye, M. Healthcare and the Internet of Medical Things: Applications, Trends, Key Challenges, and Proposed Resolutions. Informatics 2024, 11, 47. [Google Scholar] [CrossRef]
- DE Zambotti, M.; Cellini, N.; Goldstone, A.; Colrain, I.M.; Baker, F.C. Wearable Sleep Technology in Clinical and Research Settings. Med. Sci. Sports Exerc. 2019, 51, 1538–1557. [Google Scholar] [CrossRef] [PubMed]
- Fay-Karmon, T.; Galor, N.; Heimler, B.; Zilka, A.; Bartsch, R.P.; Plotnik, M.; Hassin-Baer, S. Home-Based Monitoring of Persons with Advanced Parkinson’s Disease Using Smartwatch-Smartphone Technology. Sci. Rep. 2024, 14, 9. [Google Scholar] [CrossRef]
- Kourtis, L.C.; Regele, O.B.; Wright, J.M.; Jones, G.B. Digital Biomarkers for Alzheimer’s Disease: The Mobile/Wearable Devices Opportunity. npj Digit. Med. 2019, 2, 9. [Google Scholar] [CrossRef]
- Xia, Z.; Chikersal, P.; Venkatesh, S.; Walker, E.; Dey, A.K.; Goel, M. Longitudinal Digital Phenotyping of Multiple Sclerosis Severity Using Passively Sensed Behaviors and Ecological Momentary Assessments: Real-World Evaluation. J. Med. Internet Res. 2025, 27, e70871. [Google Scholar] [CrossRef]
- Huang, C.; Wang, J.; Wang, S.; Zhang, Y. Internet of Medical Things: A Systematic Review. Neurocomputing 2023, 557, 126719. [Google Scholar] [CrossRef]
- Rehman, A.U.; Lu, S.; Bin Heyat, M.B.; Iqbal, M.S.; Parveen, S.; Bin Hayat, M.A.; Akhtar, F.; Ashraf, M.A.; Khan, O.; Pomary, D.; et al. Internet of Things in Healthcare Research: Trends, Innovations, Security Considerations, Challenges and Future Strategy. Int. J. Intell. Syst. 2025, 2025, 8546245. [Google Scholar] [CrossRef]
- Kim, Y.; Oh, S.; Kim, G. Convergence of Integrated Sensing and Communication (ISAC) and Digital-Twin Technologies in Healthcare Systems: A Comprehensive Review. Signals 2025, 6, 51. [Google Scholar] [CrossRef]
- Giansanti, D. The Future of Healthcare Is Digital: Unlocking the Potential of Mobile Health and E-Health Solutions. Healthcare 2025, 13, 802. [Google Scholar] [CrossRef]
- Matthew, P.; Mchale, S.; Deng, X.; Nakhla, G.; Trovati, M.; Nnamoko, N.; Pereira, E.; Zhang, H.; Raza, M. A Review of the State of the Art for the Internet of Medical Things. Science 2025, 7, 36. [Google Scholar] [CrossRef]
- Kalodanis, K.; Feretzakis, G.; Anastasiou, A.; Rizomiliotis, P.; Anagnostopoulos, D.; Koumpouros, Y. A Privacy-Preserving and Attack-Aware AI Approach for High-Risk Healthcare Systems Under the EU AI Act. Electronics 2025, 14, 1385. [Google Scholar] [CrossRef]
- Mannhart, D.; Lischer, M.; Knecht, S.; du Fay de Lavallaz, J.; Strebel, I.; Serban, T.; Vögeli, D.; Schaer, B.; Osswald, S.; Mueller, C.; et al. Clinical Validation of 5 Direct-to-Consumer Wearable Smart Devices to Detect Atrial Fibrillation. JACC Clin. Electrophysiol. 2023, 9, 232–242. [Google Scholar] [CrossRef] [PubMed]
- Schyvens, A.-M.; Peters, B.; Van Oost, N.C.; Aerts, J.-M.; Masci, F.; Neven, A.; Dirix, H.; Wets, G.; Ross, V.; Verbraecken, J. A Performance Validation of Six Commercial Wrist-Worn Wearable Sleep-Tracking Devices for Sleep Stage Scoring Compared to Polysomnography. SLEEP Adv. 2025, 6, zpaf021. [Google Scholar] [CrossRef]
- Hakobyan, Z.; Zelveian, P.; Topouchian, J.; Hazarapetyan, L.; Asmar, R. Validation of the Withings BPM Core Device for Self-Blood Pressure Measurements in General Population According to the Association for the Advancement of Medical Instrumentation/European Society of Hypertension/International Organization for Standardization Universal Standard. Vasc. Health Risk Manag. 2023, 19, 391–398. [Google Scholar] [CrossRef]
- Withings. Withings ScanWatch, ScanWatch 2. Clinical Studies (EU & ROW). Withings: Paris, France, 2023.
- Ernstsson, J.; Svensson, B.; Liuba, P.; Weismann, C.G. Validation of Smartwatch Electrocardiogram Intervals in Children Compared to Standard 12 Lead Electrocardiograms. Eur. J. Pediatr. 2024, 183, 3915–3923. [Google Scholar] [CrossRef]
- Matos, J.; Ramos, B.; Fernandes, J.; Hansen, C.; Maetzler, W.; Vila-Chã, N.; Maia, L.F. Wearable Sensors for Sleep Monitoring in Free-Living Environments: A Scoping Review on Parkinson’s Disease. Biosensors 2025, 15, 212. [Google Scholar] [CrossRef]
- Withings. Withings Body+ Scale; Withings: Paris, France, 2023; Available online: https://www.withings.com/body-plus (accessed on 20 October 2025).
- Svensson, T.; Madhawa, K.; NT, H.; Chung, U.; Svensson, A.K. Validity and Reliability of the Oura Ring Generation 3 (Gen3) with Oura Sleep Staging Algorithm 2.0 (OSSA 2.0) When Compared to Multi-Night Ambulatory Polysomnography: A Validation Study of 96 Participants and 421,045 Epochs. Sleep. Med. 2024, 115, 251–263. [Google Scholar] [CrossRef]
- Withings. Withings Developer, Advanced Research API; Withings: Paris, France, 2023; Available online: https://developer.withings.com/api-reference (accessed on 20 October 2025).
- Băjenaru, O.L.; Băjenaru, L.; Ianculescu, M.; Constantin, V.-Ș.; Gușatu, A.-M.; Nuță, C.R. Geriatric Healthcare Supported by Decision-Making Tools Integrated into Digital Health Solutions. Electronics 2024, 13, 3440. [Google Scholar] [CrossRef]
- Ianculescu, M.; Constantin, V.-Ș.; Gușatu, A.-M.; Petrache, M.-C.; Mihăescu, A.-G.; Bica, O.; Alexandru, A. Enhancing Connected Health Ecosystems Through IoT-Enabled Monitoring Technologies: A Case Study of the Monit4Healthy System. Sensors 2025, 25, 2292. [Google Scholar] [CrossRef]
- De Pasquale, P.; Bonanno, M.; De Marchis, C.; Pergolizzi, L.; Lombardo Facciale, A.; Paladina, G.; Maggio, M.G.; Impellizzeri, F.; Ciancarelli, I.; Quartarone, A.; et al. Beyond Clinical Scales: An Observational Study on Instrumental Gait Analysis and Biomechanical Patterns in Patients with Parkinson’s Disease. Front. Bioeng. Biotechnol. 2025, 13, 1541240. [Google Scholar] [CrossRef] [PubMed]
- Villarón-Casales, C.; de Bernardo, N.; Alarcón-Jiménez, J.; López-Malo, D.; Proaño, B.; Martín-Ruiz, J.; de la Rubia Ortí, J.E. Amplitude of Lower Limb Muscle Activation in Different Phases of the Illinois Test in Parkinson’s Disease Patients: A Pilot Study. J. Clin. Med. 2024, 13, 5792. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.-H.; Sun, S.-Y.; Li, G.; Gao, X.; Luo, W.; Tian, H.; Zhang, X.; Yin, X.; Liu, Z.; Chen, G.-C.; et al. Physical Activity and Sleep Pattern in Relation to Incident Parkinson’s Disease: A Cohort Study. Int. J. Behav. Nutr. Phys. Act. 2024, 21, 17. [Google Scholar] [CrossRef] [PubMed]
- Withings. Withings Health Data API—Developer Documentation; Withings: Paris, France, 2023; Available online: https://developer.withings.com/api-reference#tag/health-data (accessed on 20 October 2025).
- Nicolau, D.; Bica, O.; Băjenaru, L. Data Security Approach in Remote Healthcare Monitoring. Rom. Cyber Secur. J. 2023, 5, 45–55. [Google Scholar] [CrossRef]
- Saif, S.; Das, P.; Biswas, S.; Khan, S.; Haq, M.A.; Kovtun, V. A Secure Data Transmission Framework for IoT Enabled Healthcare. Heliyon 2024, 10, e36269. [Google Scholar] [CrossRef]
- Singh, A.K.; Krishnan, S. ECG Signal Feature Extraction Trends in Methods and Applications. Biomed. Eng. Online 2023, 22, 22. [Google Scholar] [CrossRef]
- Sergi, G.; Yekutieli, Z.; Meloni, M.; Bianchini, E.; Vivacqua, G.; Di Lazzaro, V.; Marano, M. Sympathetic Burden Measured Through a Chest-Worn Sensor Correlates with Spatiotemporal Gait Performances and Global Cognition in Parkinson’s Disease. Sensors 2025, 25, 5756. [Google Scholar] [CrossRef]
- Shammar, E.; Cui, X.; Zahary, A.; Alsamhi, S.H.; Al-qaness, M.A.A. Threat to Trust: A Systematic Review on Internet of Medical Things Security. J. Parallel Distrib. Comput. 2025, 206, 105172. [Google Scholar] [CrossRef]
- Alasmary, H. ScalableDigitalHealth (SDH): An IoT-Based Scalable Framework for Remote Patient Monitoring. Sensors 2024, 24, 1346. [Google Scholar] [CrossRef]
- Quiroga Gutierrez, A.C.; Lindegger, D.J.; Taji Heravi, A.; Stojanov, T.; Sykora, M.; Elayan, S.; Mooney, S.J.; Naslund, J.A.; Fadda, M.; Gruebner, O. Reproducibility and Scientific Integrity of Big Data Research in Urban Public Health and Digital Epidemiology: A Call to Action. Int. J. Environ. Res. Public Health 2023, 20, 1473. [Google Scholar] [CrossRef]
- Helminski, D.; Sussman, J.B.; Pfeiffer, P.N.; Kokaly, A.N.; Ranusch, A.; Renji, A.D.; Damschroder, L.J.; Landis-Lewis, Z.; Kurlander, J.E. Development, Implementation, and Evaluation Methods for Dashboards in Health Care: Scoping Review. JMIR Med. Inform. 2024, 12, e59828. [Google Scholar] [CrossRef]
- Zhu, P.; Chen, X.; Zhang, Z.; Li, P.; Cheng, X.; Dai, Y. AI-Driven Hypergraph Neural Network for Predicting Gasoline Price Trends. Energy Econ. 2025, 151, 108895. [Google Scholar] [CrossRef]
- Dabnichki, P.; Pang, T.Y. Wearable Sensors and Motion Analysis for Neurological Patient Support. Biosensors 2024, 14, 628. [Google Scholar] [CrossRef] [PubMed]
- Islam, U.; Alatawi, M.N.; Alqazzaz, A.; Alamro, S.; Shah, B.; Moreira, F. A Hybrid Fog-Edge Computing Architecture for Real-Time Health Monitoring in IoMT Systems with Optimized Latency and Threat Resilience. Sci. Rep. 2025, 15, 25655. [Google Scholar] [CrossRef] [PubMed]
- Rancea, A.; Anghel, I.; Cioara, T. Edge Computing in Healthcare: Innovations, Opportunities, and Challenges. Future Internet 2024, 16, 329. [Google Scholar] [CrossRef]
- U.S. Food and Drug Administration. Digital Health Technologies for Remote Data Acquisition in Clinical Investigations; U.S. Food and Drug Administration: Silver Spring, MD, USA, 2023.
- European Commission. MDCG 2025-4 Guidance on the Safe Making Available of Medical Device Software (MDSW) Apps on Online Platforms; European Commission: Brussels, Belgium, 2025. [Google Scholar]
- Rosenbacke, R.; Melhus, Å.; McKee, M.; Stuckler, D. How Explainable Artificial Intelligence Can Increase or Decrease Clinicians’ Trust in AI Applications in Health Care: Systematic Review. JMIR AI 2024, 3, e53207. [Google Scholar] [CrossRef]
- Abdelaal, Y.; Aupetit, M.; Baggag, A.; Al-Thani, D. Exploring the Applications of Explainability in Wearable Data Analytics: Systematic Literature Review. J. Med. Internet Res. 2024, 26, e53863. [Google Scholar] [CrossRef]
- Rodríguez-Martín, D.; Pérez-López, C. Commercial Symptom Monitoring Devices in Parkinson’s Disease: Benefits, Limitations, and Trends. Front. Neurol. 2024, 15, 1470928. [Google Scholar] [CrossRef]
- Lim, W.-S.; Fan, S.-P.; Chiu, S.-I.; Wu, M.-C.; Wang, P.-H.; Lin, K.-P.; Chen, Y.-M.; Peng, P.-L.; Jang, J.-S.R.; Lin, C.-H. Smartphone-Derived Multidomain Features Including Voice, Finger-Tapping Movement and Gait Aid Early Identification of Parkinson’s Disease. npj Park. Dis. 2025, 11, 111. [Google Scholar] [CrossRef]
| Medical Domain | Device(s) | Key Measured Parameters | Relevance for AD/PD/MS Monitoring | Clinical Validation/Access Features |
|---|---|---|---|---|
| Cardiovascular health | Withings BPM Core, Withings ScanWatch | Blood pressure, ECG, HR, SpO2 | Cardiovascular comorbidities and autonomic dysfunction are frequent in PD and MS | BPM Core-validated, according to the Association for the Advancement of Medical Instrumentation/International Organization for Standardization (AAMI/ISO) Universal Standard [27]; ScanWatch validated for AF detection and ECG in multicentric studies [28,29]. |
| Sleep and circadian rhythms | Withings Sleep Analyzer, Withings ScanWatch, Oura Ring | Sleep duration, sleep phases, nocturnal HR, SpO2 | Sleep disturbances and nocturnal desaturation are early markers in AD and PD | Validation of six wrist-worn devices for sleep scoring vs. polysomnography [26]; recent review on sleep monitoring in PD [30]. |
| Anthropometry and metabolism | Withings Body+ scale | Weight, body mass index (BMI), body composition | Monitoring metabolic decline, sarcopenia, or weight loss relevant to neurodegenerative progression | CE-marked; reproducible anthropometric measures (manufacturer reports) [31]. |
| Physical activity and mobility | Fitbit trackers, Withings ScanWatch | Step count, accelerometry, energy expenditure | Reduced mobility and activity fluctuations are key features in PD and MS | BASEL Wearable Study demonstrated accuracy and acceptability of consumer wearables for AF detection, including step/heart rate monitoring [25]; Fitbit/Oura validated in sleep–activity comparison [32]. |
| Lifestyle monitoring | Oura Ring, Fitbit | Daily activity, energy balance | Lifestyle patterns influence vulnerability and symptom exacerbation in AD, PD, MS | Oura and Fitbit validated in recent multi-device sleep/activity studies [26,30]. |
| Application Programming Interface (API) and research access | Withings ecosystem | Secure API for physiological and activity data | Supports reproducibility, integration, and sustainable deployment in research | Withings Advanced Research API enables direct, subscription-free access to physiological and activity data [33]. |
| Medical Domain | Device | Sensors/Modules | Key Measured Parameters | Relevance for AD/PD/MS Monitoring | Validation Stage |
|---|---|---|---|---|---|
| Cardiovascular health | Medical Blackbox | AD8232 ECG, SFM3300-D flow, SpO2, temperature | ECG, respiratory flow, peripheral signals | Autonomic function, respiratory anomalies relevant in AD, PD, MS | Laboratory validation |
| Environmental context | Ambiental Blackbox | CO2, VOC, temperature, humidity, light, motion sensors | Air quality, ambient temperature, humidity | Environmental influence on sleep, fatigue, symptom fluctuation in AD and PD | Laboratory validation |
| Motor function and mobility | Gaitband | Accelerometer, gyroscope, Global System for Mobile Communications (GSM) | Stride length, variability, asymmetry, gait speed | Early gait impairments, fall risk, mobility decline in PD and MS | Laboratory validation |
| Muscle activity | EMG Blackbox | MyoWare 2.0, wireless shield, ESP32 | EMG signals, muscle activation patterns | Complementary high-resolution EMG data to support motor analysis in PD and MS | Laboratory validation |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vevera, A.-V.; Ianculescu, M.; Alexandru, A. A Digital Health Platform for Remote and Multimodal Monitoring in Neurodegenerative Diseases. Future Internet 2025, 17, 571. https://doi.org/10.3390/fi17120571
Vevera A-V, Ianculescu M, Alexandru A. A Digital Health Platform for Remote and Multimodal Monitoring in Neurodegenerative Diseases. Future Internet. 2025; 17(12):571. https://doi.org/10.3390/fi17120571
Chicago/Turabian StyleVevera, Adrian-Victor, Marilena Ianculescu, and Adriana Alexandru. 2025. "A Digital Health Platform for Remote and Multimodal Monitoring in Neurodegenerative Diseases" Future Internet 17, no. 12: 571. https://doi.org/10.3390/fi17120571
APA StyleVevera, A.-V., Ianculescu, M., & Alexandru, A. (2025). A Digital Health Platform for Remote and Multimodal Monitoring in Neurodegenerative Diseases. Future Internet, 17(12), 571. https://doi.org/10.3390/fi17120571







