Potential Use of Biological Proteins for Liver Failure Therapy
Abstract
:1. Introduction
2. Albumin-Based Products
| Product | Features | Product | Features |
|---|---|---|---|
| Albumin | Erythropoietin (EPO) | ||
| Recombination | Marketed approval | Unmodification | Animal study |
| Mannosylation | Animal study | EPO with G-CSF | Clinical study |
| M6P-modification | Animal study | ||
| Nanoparticle | Animal study | α1-Acid glycoprotein (AGP) | |
| Fusion with Trx | Animal study | Unmodification | Animal study |
| Fusion with IFN-α | Clinical study | ||
| PEG modification | Animal study | Gelatin | |
| MARS® | Clinical study | Nanoparticle | Animal study |
| Lactferrin (Lf) | Hemoglobin (Hb) | ||
| Unmodification | In vitro study | CO-bound liposomal Hb | Animal study |
| Animal study | |||
| PEG modification | Animal study | Hb-ribavirin | Animal study |
2.1. Mannosylation
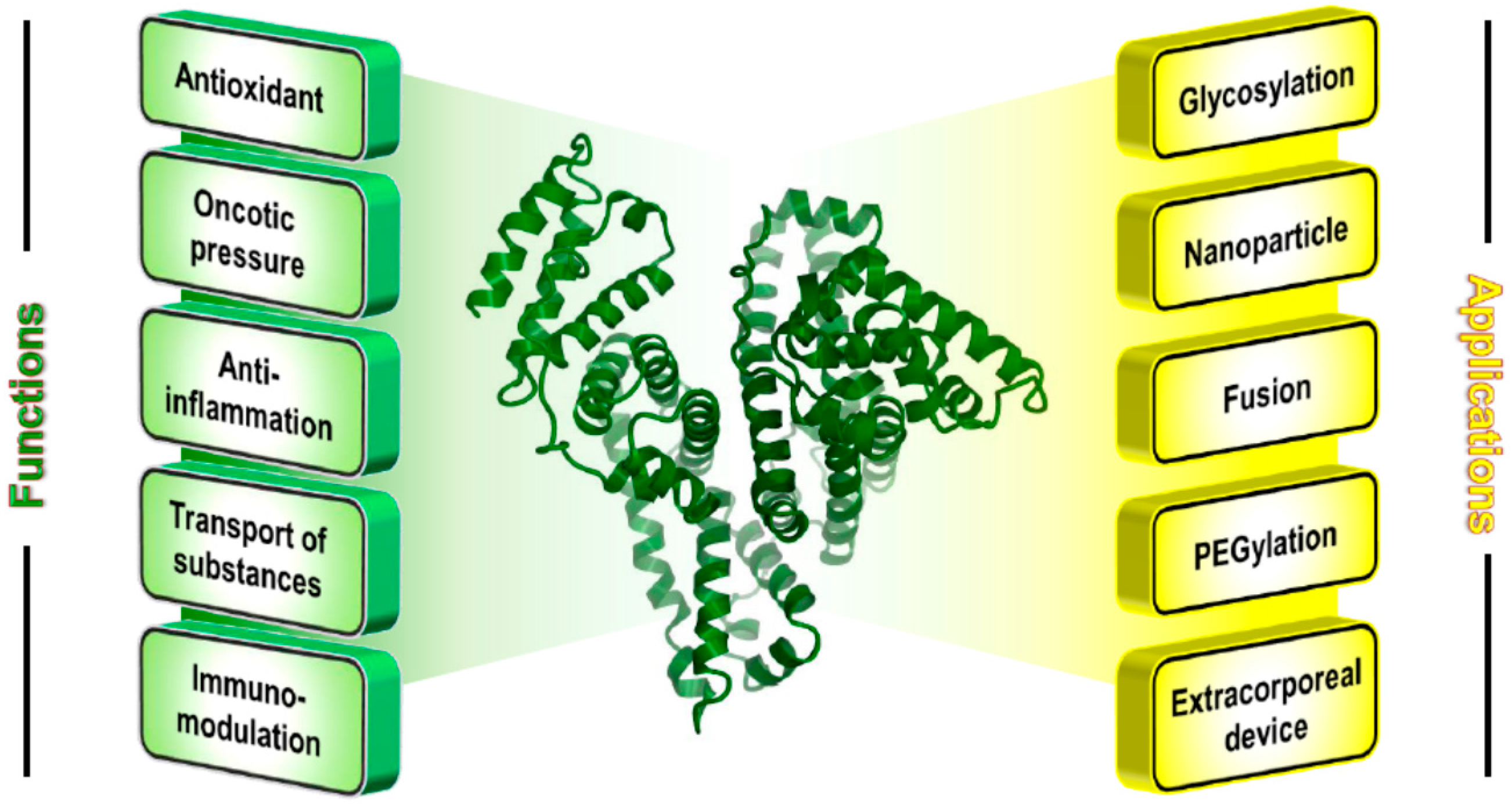
2.2. Nanoparticles
2.3. Fusion
2.4. PEGylated Albumin
2.5. Albumin Dialysis
3. Lactoferrin
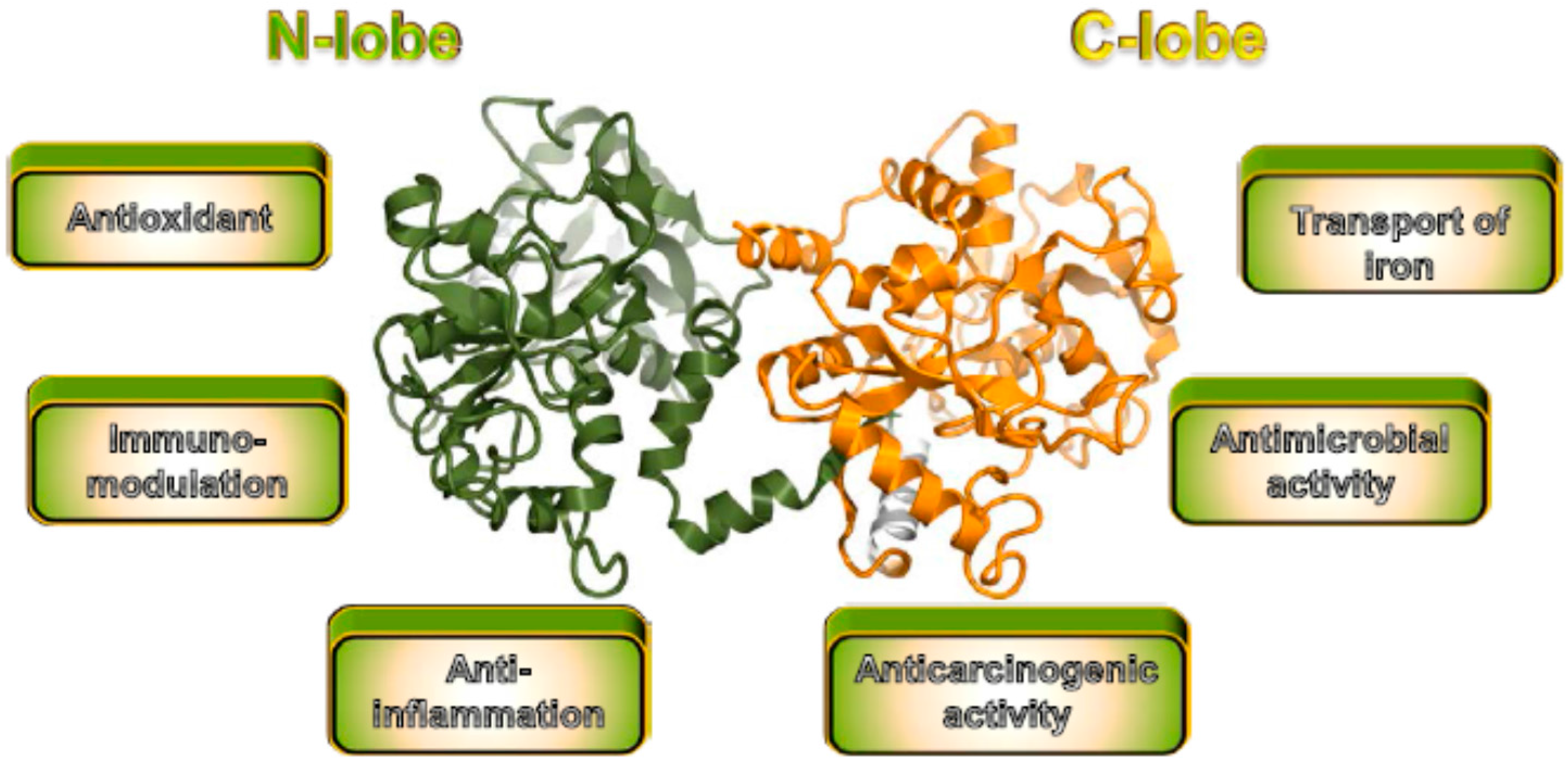
3.1. Unmodified Lactoferrin
3.2. PEGylated Lactoferrin
3.3. Others
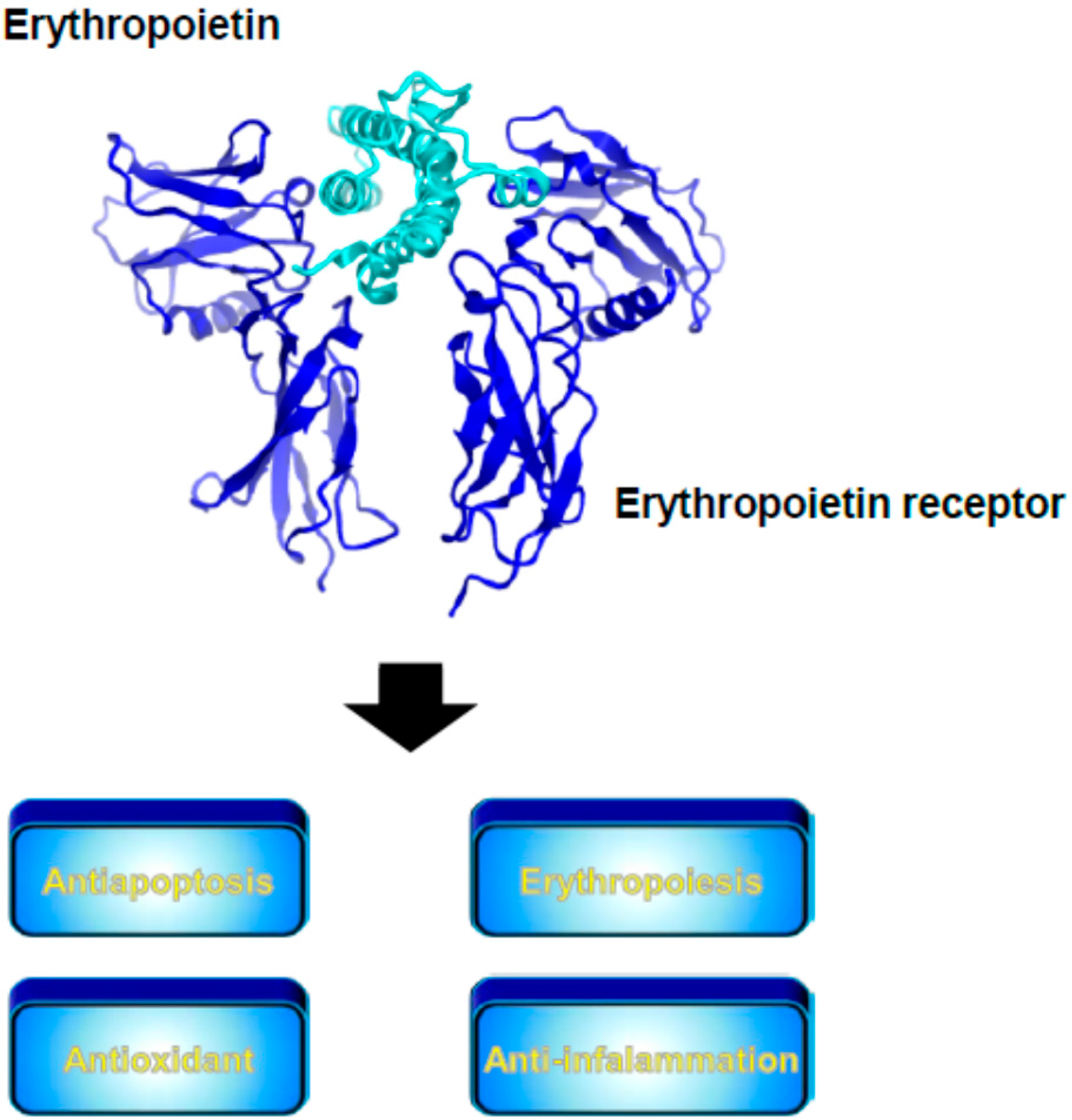
3.4. Erythropoietin
3.5. α1-Acid Glycoprotein
3.6. Gelatin
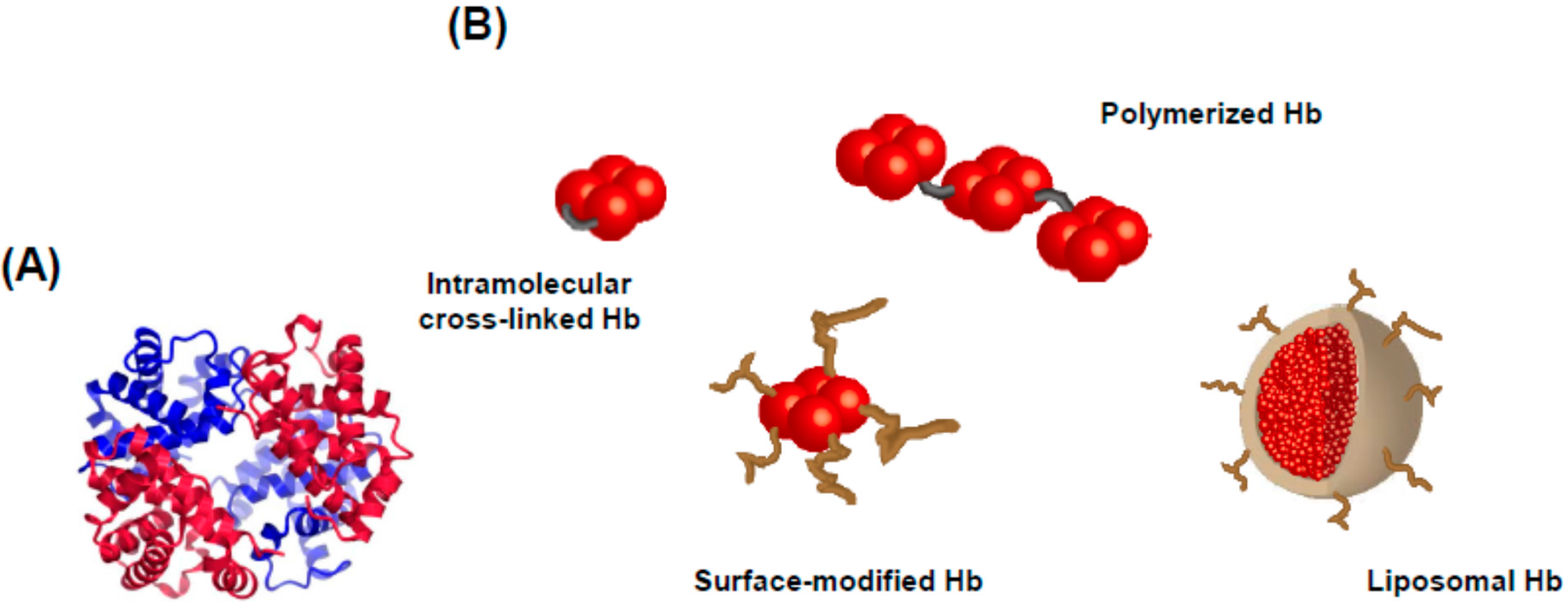
3.7. Hemoglobin
4. Conclusions
Author Contributions
Conflicts of Interest
References
- Dawidczyk, C.M.; Kim, C.; Park, J.H.; Russell, L.M.; Lee, K.H.; Pomper, M.G.; Searson, P.C. State-of-the-art in design rules for drug delivery platforms: Lessons learned from FDA-approved nanomedicines. J. Control. Release 2014, 187, 133–144. [Google Scholar] [CrossRef] [PubMed]
- Miele, E.; Spinelli, G.P.; Miele, E.; Tomao, F.; Tomao, S. Albumin-bound formulation of paclitaxel (Abraxane® ABI-007) in the treatment of breast cancer. Int. J. Nanomed. 2009, 4, 99–105. [Google Scholar]
- Bilzer, M.; Roggel, F.; Gerbes, A.L. Role of Kupffer cells in host defense and liver disease. Liver Int. 2006, 26, 1175–1186. [Google Scholar] [CrossRef] [PubMed]
- Taguchi, K.; Miyasato, M.; Watanabe, H.; Sakai, H.; Tsuchida, E.; Horinouchi, H.; Kobayashi, K.; Maruyama, T.; Otagiri, M. Alteration in the pharmacokinetics of hemoglobin-vesicles in a rat model of chronic liver cirrhosis is associated with Kupffer cell phagocyte activity. J. Pharm. Sci. 2011, 100, 775–783. [Google Scholar] [CrossRef] [PubMed]
- Mederacke, I.; Hsu, C.C.; Troeger, J.S.; Huebener, P.; Mu, X.; Dapito, D.H.; Pradere, J.P.; Schwabe, R.F. Fate tracing reveals hepatic stellate cells as dominant contributors to liver fibrosis independent of its aetiology. Nat. Commun. 2013, 4, 2823. [Google Scholar] [CrossRef] [PubMed]
- Poelstra, K.; Prakash, J.; Beljaars, L. Drug targeting to the diseased liver. J. Control. Release 2012, 161, 188–197. [Google Scholar] [CrossRef] [PubMed]
- Mishra, N.; Yadav, N.P.; Rai, V.K.; Sinha, P.; Yadav, K.S.; Jain, S.; Arora, S. Efficient hepatic delivery of drugs: Novel strategies and their significance. Biomed. Res. Int. 2013, 2013, 382184. [Google Scholar] [CrossRef] [PubMed]
- Caraceni, P.; Domenicali, M.; Tovoli, A.; Napoli, L.; Ricci, C.S.; Tufoni, M.; Bernardi, M. Clinical indications for the albumin use: Still a controversial issue. Eur. J. Int. Med. 2013, 24, 721–728. [Google Scholar] [CrossRef] [PubMed]
- Otagiri, M.; Chuang, V.T.; Maruyama, T.; Kragh-Hansen, U. Human Serum Albumin; Sojo University Publishing Center: Kumamoto, Japan, 2013. [Google Scholar]
- Hirata, K.; Maruyama, T.; Watanabe, H.; Maeda, H.; Nakajou, K.; Iwao, Y.; Ishima, Y.; Katsumi, H.; Hashida, M.; Otagiri, M. Genetically engineered mannosylated-human serum albumin as a versatile carrier for liver-selective therapeutics. J. Control. Release 2010, 145, 9–16. [Google Scholar] [CrossRef] [PubMed]
- Maeda, H.; Hirata, K.; Watanabe, H.; Ishima, Y.; Chuang, V.T.; Taguchi, K.; Inatsu, A.; Kinoshita, M.; Tanaka, M.; Sasaki, Y.; et al. Polythiol-containing, recombinant mannosylated-albumin is a superior CD68+/CD206+ Kupffer cell-targeted nano-antioxidant for treatment of two acute hepatitis models. J. Pharmacol. Exp. Ther. 2015, 352, 244–257. [Google Scholar] [CrossRef] [PubMed]
- Kinoshita, M.; Uchida, T.; Sato, A.; Nakashima, M.; Nakashima, H.; Shono, S.; Habu, Y.; Miyazaki, H.; Hiroi, S.; Seki, S. Characterization of two F4/80-positive Kupffer cell subsets by their function and phenotype in mice. J. Hepatol. 2010, 53, 903–910. [Google Scholar] [CrossRef] [PubMed]
- Tacke, F.; Weiskirchen, R. Update on hepatic stellate cells: Pathogenic role in liver fibrosis and novel isolation techniques. Expert. Rev. Gastroenterol. Hepatol. 2012, 6, 67–80. [Google Scholar] [CrossRef] [PubMed]
- de Bleser, P.J.; Jannes, P.; van Buul-Offers, S.C.; Hoogerbrugge, C.M.; van Schravendijk, C.F.; Niki, T.; Rogiers, V.; van den Brande, J.L.; Wisse, E.; Geerts, A. Insulinlike growth factor-II/mannose 6-phosphate receptor is expressed on CCl4-exposed rat fat-storing cells and facilitates activation of latent transforming growth factor-beta in cocultures with sinusoidal endothelial cells. Hepatology 1995, 21, 1429–1437. [Google Scholar] [PubMed]
- van Beuge, M.M.; Prakash, J.; Lacombe, M.; Post, E.; Reker-Smit, C.; Beljaars, L.; Poelstra, K. Enhanced effectivity of an ALK5-inhibitor after cell-specific delivery to hepatic stellate cells in mice with liver injury. PLoS ONE 2013, 8, e56442. [Google Scholar] [CrossRef] [PubMed]
- Klein, S.; Van Beuge, M.M.; Granzow, M.; Beljaars, L.; Schierwagen, R.; Kilic, S.; Heidari, I.; Huss, S.; Sauerbruch, T.; Poelstra, K.; et al. HSC-specific inhibition of Rho-kinase reduces portal pressure in cirrhotic rats without major systemic effects. J. Hepatol. 2012, 57, 1220–1227. [Google Scholar] [CrossRef] [PubMed]
- Luk, J.M.; Zhang, Q.S.; Lee, N.P.; Wo, J.Y.; Leung, P.P.; Liu, L.X.; Hu, M.Y.; Cheung, K.F.; Hui, C.K.; Lau, G.K.; et al. Hepatic stellate cell-targeted delivery of M6P-HSA-glycyrrhetinic acid attenuates hepatic fibrogenesis in a bile duct ligation rat model. Liver Int. 2007, 27, 548–557. [Google Scholar] [CrossRef] [PubMed]
- Greupink, R.; Reker-Smit, C.; Proost, J.H.; van Loenen Weemaes, A.M.; de Hooge, M.; Poelstra, K.; Beljaars, L. Pharmacokinetics of a hepatic stellate cell-targeted doxorubicin construct in bile duct-ligated rats. Biochem. Pharmacol. 2007, 73, 1455–1462. [Google Scholar] [CrossRef] [PubMed]
- Groult, H.; Ruiz-Cabello, J.; Pellico, J.; Lechuga-Vieco, A.V.; Bhavesh, R.; Zamai, M.; Almarza, E.; Martin-Padura, I.; Cantelar, E.; Martinez-Alcazar, M.P.; et al. Parallel multifunctionalization of nanoparticles: A one-step modular approach for in vivo imaging. Bioconjug. Chem. 2015, 26, 153–160. [Google Scholar] [CrossRef] [PubMed]
- Elzoghby, A.O.; Samy, W.M.; Elgindy, N.A. Albumin-based nanoparticles as potential controlled release drug delivery systems. J. Control. Release 2012, 157, 168–182. [Google Scholar] [CrossRef] [PubMed]
- Li, F.Q.; Su, H.; Wang, J.; Liu, J.Y.; Zhu, Q.G.; Fei, Y.B.; Pan, Y.H.; Hu, J.H. Preparation and characterization of sodium ferulate entrapped bovine serum albumin nanoparticles for liver targeting. Int. J. Pharm. 2008, 349, 274–282. [Google Scholar] [CrossRef] [PubMed]
- Li, F.Q.; Su, H.; Chen, X.; Qin, X.J.; Liu, J.Y.; Zhu, Q.G.; Hu, J.H. Mannose 6-phosphate-modified bovine serum albumin nanoparticles for controlled and targeted delivery of sodium ferulate for treatment of hepatic fibrosis. J. Pharm. Pharmacol. 2009, 61, 1155–1161. [Google Scholar] [CrossRef] [PubMed]
- Kapoor, D.N.; Manvi, F.V.; Doijad, R.C.; Dhawan, S. Prednisolone-loaded albumin nanospheres: In vitro and in vivo evaluation studies. PDA J. Pharm. Sci. Technol. 2008, 62, 111–124. [Google Scholar] [PubMed]
- Santhi, K.; Dhanaraj, S.A.; Koshy, M.; Ponnusankar, S.; Suresh, B. Study of biodistribution of methotrexate-loaded bovine serum albumin nanospheres in mice. Drug Dev. Ind. Pharm. 2000, 26, 1293–1296. [Google Scholar] [CrossRef] [PubMed]
- Maeda, H.; Wu, J.; Sawa, T.; Matsumura, Y.; Hori, K. Tumor vascular permeability and the EPR effect in macromolecular therapeutics: A review. J. Control. Release 2000, 65, 271–284. [Google Scholar] [CrossRef]
- Qi, W.W.; Yu, H.Y.; Guo, H.; Lou, J.; Wang, Z.M.; Liu, P.; Sapin-Minet, A.; Maincent, P.; Hong, X.C.; Hu, X.M.; et al. Doxorubicin-loaded glycyrrhetinic Acid modified recombinant human serum albumin nanoparticles for targeting liver tumor chemotherapy. Mol. Pharm. 2015, 12, 675–683. [Google Scholar] [CrossRef] [PubMed]
- Zu, Y.; Meng, L.; Zhao, X.; Ge, Y.; Yu, X.; Zhang, Y.; Deng, Y. Preparation of 10-hydroxy-camptothecin-loaded glycyrrhizic acid-conjugated bovine serum albumin nanoparticles for hepatocellular carcinoma-targeted drug delivery. Int. J. Nanomed. 2013, 8, 1207–1222. [Google Scholar]
- Chang, J.E.; Shim, W.S.; Yang, S.G.; Kwak, E.Y.; Chong, S.; Kim, D.D.; Chung, S.J.; Shim, C.K. Liver cancer targeting of Doxorubicin with reduced distribution to the heart using hemato-porphyrin-modified albumin nanoparticles in rats. Pharm. Res. 2012, 29, 795–805. [Google Scholar] [CrossRef] [PubMed]
- Shen, Z.; Wei, W.; Tanaka, H.; Kohama, K.; Ma, G.; Dobashi, T.; Maki, Y.; Wang, H.; Bi, J.; Dai, S. A galactosamine-mediated drug delivery carrier for targeted liver cancer therapy. Pharmacol. Res. 2011, 64, 410–419. [Google Scholar] [CrossRef] [PubMed]
- Watcharin, W.; Schmithals, C.; Pleli, T.; Koberle, V.; Korkusuz, H.; Huebner, F.; Zeuzem, S.; Korf, H.W.; Vogl, T.J.; Rittmeyer, C.; et al. Biodegradable human serum albumin nanoparticles as contrast agents for the detection of hepatocellular carcinoma by magnetic resonance imaging. Eur. J. Pharm. Biopharm. 2014, 87, 132–141. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, K. Summary of recombinant human serum albumin development. Biologicals 2006, 34, 55–59. [Google Scholar] [CrossRef] [PubMed]
- Chuang, V.T.; Otagiri, M. Recombinant human serum albumin. Drugs Today 2007, 43, 547–561. [Google Scholar] [CrossRef] [PubMed]
- Beeken, W.L.; Volwiler, W.; Goldsworthy, P.D.; Garby, L.E.; Reynolds, W.E.; Stogsdill, R.; Stemler, R.S. Studies of I-131-albumin catabolism and distribution in normal young male adults. J. Clin. Investig. 1962, 41, 1312–1333. [Google Scholar] [CrossRef] [PubMed]
- Takeda, Y.; Reeve, E.B. Studies of the metabolism and distribution of albumin with autologous I131-albumin in healthy men. J. Lab. Clin. Med. 1963, 61, 183–202. [Google Scholar] [PubMed]
- Ikuta, S.; Chuang, V.T.; Ishima, Y.; Nakajou, K.; Furukawa, M.; Watanabe, H.; Maruyama, T.; Otagiri, M. Albumin fusion of thioredoxin—The production and evaluation of its biological activity for potential therapeutic applications. J. Control. Release 2010, 147, 17–23. [Google Scholar] [CrossRef] [PubMed]
- Yoshihara, E.; Masaki, S.; Matsuo, Y.; Chen, Z.; Tian, H.; Yodoi, J. Thioredoxin/Txnip: Redoxisome, as a redox switch for the pathogenesis of diseases. Front. Immunol. 2014, 4, 514. [Google Scholar] [CrossRef] [PubMed]
- Okuyama, H.; Nakamura, H.; Shimahara, Y.; Araya, S.; Kawada, N.; Yamaoka, Y.; Yodoi, J. Overexpression of thioredoxin prevents acute hepatitis caused by thioacetamide or lipopoly-saccharide in mice. Hepatology 2003, 37, 1015–1025. [Google Scholar] [CrossRef] [PubMed]
- Okuyama, H.; Nakamura, H.; Shimahara, Y.; Uyama, N.; Kwon, Y.W.; Kawada, N.; Yamaoka, Y.; Yodoi, J. Overexpression of thioredoxin prevents thioacetamide-induced hepatic fibrosis in mice. J. Hepatol. 2005, 42, 117–123. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, H.; Herzenberg, L.A.; Bai, J.; Araya, S.; Kondo, N.; Nishinaka, Y.; Herzenberg, L.A.; Yodoi, J. Circulating thioredoxin suppresses lipopolysaccharide-induced neutrophil chemotaxis. Proc. Natl. Acad. Sci. USA 2001, 98, 15143–15148. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, R.; Ishima, Y.; Maeda, H.; Kodama, A.; Nagao, S.; Watanabe, H.; Chuang, V.T.; Otagiri, M.; Maruyama, T. Albumin fusion prolongs the antioxidant and anti-inflammatory activities of thioredoxin in mice with acetaminophen-induced hepatitis. Mol. Pharm. 2014, 11, 1228–1238. [Google Scholar] [CrossRef] [PubMed]
- Ashfaq, U.A.; Idrees, S. Medicinal plants against hepatitis C virus. World J. Gastroenterol. 2014, 20, 2941–2947. [Google Scholar] [CrossRef] [PubMed]
- Subramanian, G.M.; Fiscella, M.; Lamouse-Smith, A.; Zeuzem, S.; McHutchison, J.G. Albinterferon alpha-2b: A genetic fusion protein for the treatment of chronic hepatitis C. Nat. Biotechnol. 2007, 25, 1411–1419. [Google Scholar] [CrossRef] [PubMed]
- Nelson, D.R.; Benhamou, Y.; Chuang, W.L.; Lawitz, E.J.; Rodriguez-Torres, M.; Flisiak, R.; Rasenack, J.W.; Kryczka, W.; Lee, C.M.; Bain, V.G.; et al. Albinterferon Alfa-2b was not inferior to pegylated interferon-alpha in a randomized trial of patients with chronic hepatitis C virus genotype 2 or 3. Gastroenterology 2010, 139, 1267–1276. [Google Scholar] [CrossRef] [PubMed]
- Zeuzem, S.; Sulkowski, M.S.; Lawitz, E.J.; Rustgi, V.K.; Rodriguez-Torres, M.; Bacon, B.R.; Grigorescu, M.; Tice, A.D.; Lurie, Y.; Cianciara, J.; et al. Albinterferon Alfa-2b was not inferior to pegylated interferon-alpha in a randomized trial of patients with chronic hepatitis C virus genotype 1. Gastroenterology 2010, 139, 1257–1266. [Google Scholar] [CrossRef] [PubMed]
- Pianko, S.; Zeuzem, S.; Chuang, W.L.; Foster, G.R.; Sarin, S.K.; Flisiak, R.; Lee, C.M.; Andreone, P.; Piratvisuth, T.; Shah, S.; et al. Randomized trial of albinterferon alfa-2b every 4 weeks for chronic hepatitis C virus genotype 2/3. J. Viral Hepat. 2012, 19, 623–634. [Google Scholar] [CrossRef] [PubMed]
- Colvin, R.A.; Tanwandee, T.; Piratvisuth, T.; Thongsawat, S.; Hui, A.J.; Zhang, H.; Ren, H.; Chen, P.J.; Chuang, W.L.; Sobhonslidsuk, A.; et al. Randomized, controlled pharmacokinetic and pharmacodynamic evaluation of albinterferon in patients with chronic hepatitis B infection. J. Gastroenterol. Hepatol. 2015, 30, 184–191. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.; Sun, H.; Pang, M.; Chuang, W.L.; Sarin, S.K.; Flisiak, R.; Stein, D.S. Population pharmacokinetics and pharmacodynamics of albinterferon alfa-2b in patients treated for hepatitis C virus genotype 2/3. Anti-Infect. Agents 2014, 12, 58–67. [Google Scholar] [CrossRef]
- Milla, P.; Dosio, F.; Cattel, L. PEGylation of proteins and liposomes: A powerful and flexible strategy to improve the drug delivery. Curr. Drug Metab. 2012, 13, 105–119. [Google Scholar] [CrossRef] [PubMed]
- Hightower, C.M.; Salazar Vazquez, B.Y.; Acharya, S.A.; Subramaniam, S.; Intaglietta, M. PEG-albumin plasma expansion increases expression of MCP-1 evidencing increased circulatory wall shear stress: An experimental study. PLoS ONE 2012, 7, e39111. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Komatsu, T.; Yamamoto, H.; Horinouchi, H.; Kobayashi, K.; Tsuchida, E. PEGylated albumin-heme as an oxygen-carrying plasma expander: Exchange transfusion into acute anemia rat model. Biomaterials 2006, 27, 4477–4483. [Google Scholar] [CrossRef] [PubMed]
- Li, X.Y.; Li, T.H.; Guo, J.S.; Wei, Y.; Jing, X.B.; Chen, X.S.; Huang, Y.B. PEGylation of bovine serum albumin using click chemistry for the application as drug carriers. Biotechnol. Prog. 2012, 28, 856–861. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.; David, A.E.; Choi, Y.S.; Wu, Y.; Buschle-Diller, G. Scaffold materials from glycosylated and PEGylated bovine serum albumin. J. Biomed. Mater. Res. A. 2015, 103, 2839–2846. [Google Scholar] [CrossRef] [PubMed]
- Plesner, B.; Fee, C.J.; Westh, P.; Nielsen, A.D. Effects of PEG size on structure, function and stability of PEGylated BSA. Eur. J. Pharm. Biopharm. 2011, 79, 399–405. [Google Scholar] [CrossRef] [PubMed]
- Kumar, V.; Sharma, V.K.; Kalonia, D.S. Effect of polyols on polyethylene glycol (PEG)-induced precipitation of proteins: Impact on solubility, stability and conformation. Int. J. Pharm. 2009, 366, 38–43. [Google Scholar] [CrossRef] [PubMed]
- Katsumi, H.; Nishikawa, M.; Yamashita, F.; Hashida, M. Development of polyethylene glycol-conjugated poly-S-nitrosated serum albumin, a novel S-Nitrosothiol for prolonged delivery of nitric oxide in the blood circulation in vivo. J. Pharmacol. Exp. Ther. 2005, 314, 1117–1124. [Google Scholar] [CrossRef] [PubMed]
- Katsumi, H.; Nishikawa, M.; Yamashita, F.; Hashida, M. Prevention of hepatic ischemia/reperfusion injury by prolonged delivery of nitric oxide to the circulating blood in mice. Transplantation 2008, 85, 264–269. [Google Scholar] [CrossRef] [PubMed]
- Katsumi, H.; Nishikawa, M.; Nishiyama, K.; Hirosaki, R.; Nagamine, N.; Okamoto, H.; Mizuguchi, H.; Kusamori, K.; Yasui, H.; Yamashita, F.; et al. Development of PEGylated serum albumin with multiple reduced thiols as a long-circulating scavenger of reactive oxygen species for the treatment of fulminant hepatic failure in mice. Free Radic. Biol. Med. 2014, 69, 318–323. [Google Scholar] [CrossRef] [PubMed]
- Mitzner, S.R.; Stange, J.; Klammt, S.; Peszynski, P.; Schmidt, R. Albumin dialysis using the molecular adsorbent recirculating system. Curr. Opin. Nephrol. Hypertens. 2001, 10, 777–783. [Google Scholar] [CrossRef] [PubMed]
- Banares, R.; Catalina, M.V.; Vaquero, J. Molecular adsorbent recirculating system and bioartificial devices for liver failure. Clin. Liver Dis. 2014, 18, 945–956. [Google Scholar] [CrossRef] [PubMed]
- Donati, G.; La Manna, G.; Cianciolo, G.; Grandinetti, V.; Carretta, E.; Cappuccilli, M.; Panicali, L.; Iorio, M.; Piscaglia, F.; Bolondi, L.; et al. Extracorporeal detoxification for hepatic failure using molecular adsorbent recirculating system: Depurative efficiency and clinical results in a long-term follow-up. Artif. Organs 2014, 38, 125–134. [Google Scholar] [CrossRef] [PubMed]
- Banares, R.; Nevens, F.; Larsen, F.S.; Jalan, R.; Albillos, A.; Dollinger, M.; Saliba, F.; Sauerbruch, T.; Klammt, S.; Ockenga, J.; et al. Extracorporeal albumin dialysis with the molecular adsorbent recirculating system in acute-on-chronic liver failure: The RELIEF trial. Hepatology 2013, 57, 1153–1162. [Google Scholar] [CrossRef] [PubMed]
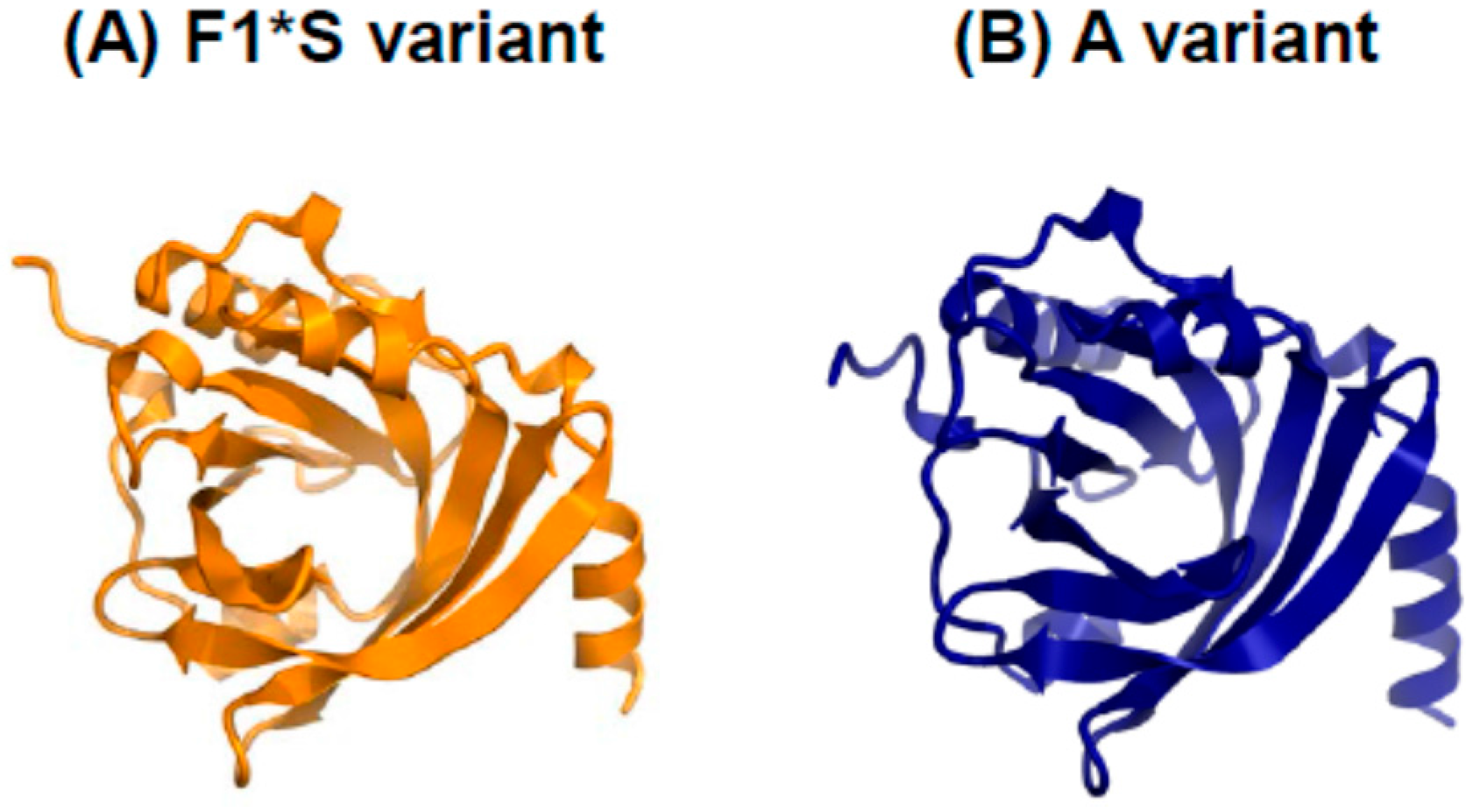
- Minomo, A.; Ishima, Y.; Chuang, V.T.; Suwa, Y.; Kragh-Hansen, U.; Narisoko, T.; Morioka, H.; Maruyama, T.; Otagiri, M. Albumin domain II mutant with high bilirubin binding affinity has a great potential as serum bilirubin excretion enhancer for hyperbilirubinemia treatment. Biochim. Biophys. Acta 2013, 1830, 2917–2923. [Google Scholar] [CrossRef] [PubMed]
- Minomo, A.; Ishima, Y.; Kragh-Hansen, U.; Chuang, V.T.; Uchida, M.; Taguchi, K.; Watanabe, H.; Maruyama, T.; Morioka, H.; Otagiri, M. Biological characteristics of two lysines on human serum albumin in the high-affinity binding of 4Z,15Z-bilirubin-IXalpha revealed by phage display. FEBS J. 2011, 278, 4100–4111. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Montoya, I.A.; Cendon, T.S.; Arevalo-Gallegos, S.; Rascon-Cruz, Q. Lactoferrin a multiple bioactive protein: An overview. Biochim. Biophys. Acta 2012, 1820, 226–236. [Google Scholar] [CrossRef] [PubMed]
- Yin, H.; Cheng, L.; Holt, M.; Hail, N.; Maclaren, R.; Ju, C. Lactoferrin protects against acetaminophen-induced liver injury in mice. Hepatology 2010, 51, 1007–1016. [Google Scholar] [CrossRef] [PubMed]
- Yin, H.; Cheng, L.; Agarwal, C.; Agarwal, R.; Ju, C. Lactoferrin protects against concanavalin A-induced liver injury in mice. Liver Int. 2010, 30, 623–632. [Google Scholar] [CrossRef] [PubMed]
- Zimecki, M.; Dawiskiba, J.; Zawirska, B.; Krawczyk, Z.; Kruzel, M. Bovine lactoferrin decreases histopathological changes in the liver and regulates cytokine production by splenocytes of obstructive jaundiced rats. Inflamm. Res. 2003, 52, 305–310. [Google Scholar] [PubMed]
- Ordaz-Pichardo, C.; Leon-Sicairos, N.; Hernandez-Ramirez, V.I.; Talamas-Rohana, P.; de la Garza, M. Effect of bovine lactoferrin in a therapeutic hamster model of hepatic amoebiasis. Biochem. Cell Biol. 2012, 90, 425–434. [Google Scholar] [CrossRef] [PubMed]
- Kuhara, T.; Tanaka, A.; Yamauchi, K.; Iwatsuki, K. Bovine lactoferrin ingestion protects against inflammation via IL-11 induction in the small intestine of mice with hepatitis. Br. J. Nutr. 2014, 111, 1801–1810. [Google Scholar] [CrossRef] [PubMed]
- Tung, Y.T.; Tang, T.Y.; Chen, H.L.; Yang, S.H.; Chong, K.Y.; Cheng, W.T.; Chen, C.M. Lactoferrin protects against chemical-induced rat liver fibrosis by inhibiting stellate cell activation. J. Dairy Sci. 2014, 97, 3281–3291. [Google Scholar] [CrossRef] [PubMed]
- Ikeda, M.; Nozaki, A.; Sugiyama, K.; Tanaka, T.; Naganuma, A.; Tanaka, K.; Sekihara, H.; Shimotohno, K.; Saito, M.; Kato, N. Characterization of antiviral activity of lactoferrin against hepatitis C virus infection in human cultured cells. Virus Res. 2000, 66, 51–63. [Google Scholar] [CrossRef]
- Ikeda, M.; Sugiyama, K.; Tanaka, T.; Tanaka, K.; Sekihara, H.; Shimotohno, K.; Kato, N. Lactoferrin markedly inhibits hepatitis C virus infection in cultured human hepatocytes. Biochem. Biophys. Res. Commun. 1998, 245, 549–553. [Google Scholar] [CrossRef] [PubMed]
- Nojima, Y.; Suzuki, Y.; Yoshida, K.; Abe, F.; Shiga, T.; Takeuchi, T.; Sugiyama, A.; Shimizu, H.; Sato, A. Lactoferrin conjugated with 40-kDa branched poly(ethylene glycol) has an improved circulating half-life. Pharm. Res. 2009, 26, 2125–2132. [Google Scholar] [CrossRef] [PubMed]
- Sugiyama, A.; Sato, A.; Shimizu, H.; Ando, K.; Takeuchi, T. PEGylated lactoferrin enhances its hepatoprotective effects on acute liver injury induced by d-galactosamine and lipopolysaccharide in rats. J. Vet. Med. Sci. 2010, 72, 173–180. [Google Scholar] [CrossRef] [PubMed]
- Sugiyama, A.; Sato, A.; Takeuchi, T. PEGylated lactoferrin enhanced its hepatoprotective effects on acute liver injury induced by carbon tetrachloride in rats. Food Chem. Toxicol. 2009, 47, 1453–1458. [Google Scholar] [CrossRef] [PubMed]
- Shiga, Y.; Oshima, Y.; Kojima, Y.; Sugimoto, A.; Tamaki, N.; Murata, D.; Takeuchi, T.; Sato, A. Recombinant human lactoferrin-Fc fusion with an improved plasma half-life. Eur. J. Pharm. Sci. 2015, 67, 136–143. [Google Scholar] [CrossRef] [PubMed]
- McAbee, D.D.; Bennatt, D.J.; Ling, Y.Y. Identification and analysis of a CA(2+)-dependent lactoferrin receptor in rat liver. Lactoferrin binds to the asialoglycoprotein receptor in a galactose-independent manner. Adv. Exp. Med. Biol. 1998, 443, 113–121. [Google Scholar] [PubMed]
- Weeke-Klimp, A.H.; Bartsch, M.; Morselt, H.W.; Van Veen-Hof, I.; Meijer, D.K.; Scherphof, G.L.; Kamps, J.A. Targeting of stabilized plasmid lipid particles to hepatocytes in vivo by means of coupled lactoferrin. J. Drug Target. 2007, 15, 585–594. [Google Scholar] [CrossRef] [PubMed]
- Wei, M.; Xu, Y.; Zou, Q.; Tu, L.; Tang, C.; Xu, T.; Deng, L.; Wu, C. Hepatocellular carcinoma targeting effect of PEGylated liposomes modified with lactoferrin. Eur. J. Pharm. Sci. 2012, 46, 131–141. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, F.; Ali, M.J.; Kondapi, A.K. Carboplatin loaded protein nanoparticles exhibit improve anti-proliferative activity in retinoblastoma cells. Int. J. Biol. Macromol. 2014, 70, 572–582. [Google Scholar] [CrossRef] [PubMed]
- Golla, K.; Bhaskar, C.; Ahmed, F.; Kondapi, A.K. A target-specific oral formulation of Doxorubicin-protein nanoparticles: Efficacy and safety in hepatocellular cancer. J. Cancer 2013, 4, 644–652. [Google Scholar] [CrossRef] [PubMed]
- Golla, K.; Cherukuvada, B.; Ahmed, F.; Kondapi, A.K. Efficacy, safety and anticancer activity of protein nanoparticle-based delivery of doxorubicin through intravenous administration in rats. PLoS ONE 2012, 7, e51960. [Google Scholar] [CrossRef] [PubMed]
- Lai, P.H.; Everett, R.; Wang, F.F.; Arakawa, T.; Goldwasser, E. Structural characterization of human erythropoietin. J. Biol. Chem. 1986, 261, 3116–3121. [Google Scholar] [PubMed]
- Fu, W.; Liao, X.; Ruan, J.; Li, X.; Chen, L.; Wang, B.; Wang, K.; Zhou, J. Recombinant human erythropoietin preconditioning attenuates liver ischemia reperfusion injury through the phosphatidylinositol-3 kinase/AKT/endothelial nitric oxide synthase pathway. J. Surg. Res. 2013, 183, 876–884. [Google Scholar] [CrossRef] [PubMed]
- Riehle, K.J.; Hoagland, V.; Benz, W.; Campbell, J.S.; Liggitt, D.H.; Langdale, L.A. Hepatocellular heme oxygenase-1: A potential mechanism of erythropoietin-mediated protection after liver ischemia-reperfusion injury. Shock 2014, 42, 424–431. [Google Scholar] [CrossRef] [PubMed]
- Shawky, H.M.; Younan, S.M.; Rashed, L.A.; Shoukry, H. Effect of recombinant erythropoietin on ischemia-reperfusion-induced apoptosis in rat liver. J. Physiol. Biochem. 2012, 68, 19–28. [Google Scholar] [CrossRef] [PubMed]
- Wu, W.T.; Lin, N.T.; Subeq, Y.M.; Lee, R.P.; Chen, I.H.; Hsu, B.G. Erythropoietin protects severe haemorrhagic shock-induced organ damage in conscious rats. Injury 2010, 41, 724–730. [Google Scholar] [CrossRef] [PubMed]
- Algin, M.C.; Hacioglu, A.; Yaylak, F.; Gulcan, E.; Aydin, T.; Hacioglu, B.A.; Ilhan, D.; Cevik, A.A.; Ates, E. The role of erythropoietin in hemorrhagic shock-induced liver and renal injury in rats. Adv. Ther. 2008, 25, 1353–1374. [Google Scholar] [CrossRef] [PubMed]
- Ben-Ari, Z.; Zilbermints, V.; Pappo, O.; Avlas, O.; Sharon, E.; Greif, F.; Cheporko, Y.; Ravid, A.; Shapiro, R.; Hochhauser, E. Erythropoietin increases survival and attenuates fulminant hepatic failure injury induced by d-galactosamine/lipopolysaccharide in mice. Transplantation 2011, 92, 18–24. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.F.; He, Y.; Li, H.Y.; Liu, X.; Chen, H.; Liu, J.B.; Ji, W.J.; Wang, B.; Chen, L.N. Hepatoprotective effects of erythropoietin on d-galactosamine/lipopolysaccharide-induced fulminant hepatic failure in mice. Mol. Med. Rep. 2014, 10, 555–559. [Google Scholar] [CrossRef] [PubMed]
- Schmeding, M.; Boas-Knoop, S.; Lippert, S.; Ruehl, M.; Somasundaram, R.; Dagdelen, T.; Neuhaus, P.; Neumann, U.P. Erythropoietin promotes hepatic regeneration after extended liver resection in rats. J. Gastroenterol. Hepatol. 2008, 23, 1125–1131. [Google Scholar] [CrossRef] [PubMed]
- Greif, F.; Ben-Ari, Z.; Taya, R.; Pappo, O.; Kurtzwald, E.; Cheporko, Y.; Ravid, A.; Hochhauser, E. Dual effect of erythropoietin on liver protection and regeneration after subtotal hepatectomy in rats. Liver Transpl. 2010, 16, 631–638. [Google Scholar] [CrossRef] [PubMed]
- Gul, M.; Comert, M.; Cakmak, G.K.; Kertis, G.; Ugurbas, E.; Oner, M.O. Effect of erythropoietin on liver regeneration in an experimental model of partial hepatectomy. Int. J. Surg. 2013, 11, 59–63. [Google Scholar] [CrossRef] [PubMed]
- Duan, X.Z.; Liu, F.F.; Tong, J.J.; Yang, H.Z.; Chen, J.; Liu, X.Y.; Mao, Y.L.; Xin, S.J.; Hu, J.H. Granulocyte-colony stimulating factor therapy improves survival in patients with hepatitis B virus-associated acute-on-chronic liver failure. World J. Gastroenterol. 2013, 19, 1104–1110. [Google Scholar] [CrossRef] [PubMed]
- Garg, V.; Garg, H.; Khan, A.; Trehanpati, N.; Kumar, A.; Sharma, B.C.; Sakhuja, P.; Sarin, S.K. Granulocyte colony-stimulating factor mobilizes CD34(+) cells and improves survival of patients with acute-on-chronic liver failure. Gastroenterology 2012, 142, 505–512.e1. [Google Scholar] [CrossRef] [PubMed]
- Vassiliou, I.; Lolis, E.; Nastos, C.; Tympa, A.; Theodosopoulos, T.; Dafnios, N.; Fragulidis, G.; Frangou, M.; Kondi-Pafiti, A.; Smyrniotis, V. The combined effect of erythropoietin and granulocyte macrophage colony stimulating factor on liver regeneration after major hepatectomy in rats. World J. Surg. Oncol. 2010, 8, 57. [Google Scholar] [CrossRef] [PubMed]
- Kedarisetty, C.K.; Anand, L.; Bhardwaj, A.; Bhadoria, A.S.; Kumar, G.; Vyas, A.K.; David, P.; Trehanpati, N.; Rastogi, A.; Bihari, C.; et al. Combination of Granulocyte Colony-Stimulating Factor and Erythropoietin Improves Outcomes of Patients with Decompensated Cirrhosis. Gastroenterology 2015, 148, 1362–1370. [Google Scholar] [CrossRef] [PubMed]
- Fournier, T.; Medjoubi, N.N.; Porquet, D. Alpha-1-acid glycoprotein. Biochim. Biophys. Acta 2000, 1482, 157–171. [Google Scholar] [CrossRef]
- Kagaya, N.; Kamiyoshi, A.; Tagawa, Y.; Akamatsu, S.; Isoda, K.; Kawase, M.; Yagi, K. Suppression of cell death in primary rat hepatocytes by alpha1-acid glycoprotein. J. Biosci. Bioeng. 2005, 99, 81–83. [Google Scholar] [CrossRef] [PubMed]
- Van Molle, W.; Denecker, G.; Rodriguez, I.; Brouckaert, P.; Vandenabeele, P.; Libert, C. Activation of caspases in lethal experimental hepatitis and prevention by acute phase proteins. J. Immunol. 1999, 163, 5235–5241. [Google Scholar] [PubMed]
- Van Molle, W.; Libert, C.; Fiers, W.; Brouckaert, P. Alpha 1-acid glycoprotein and alpha 1-antitrypsin inhibit TNF-induced but not anti-Fas-induced apoptosis of hepatocytes in mice. J. Immunol. 1997, 159, 3555–3564. [Google Scholar] [PubMed]
- Kuzuhara, H.; Nakano, Y.; Yamashita, N.; Imai, M.; Kawamura, Y.; Kurosawa, T.; Nishiyama, S. Protective effects of alpha1-acid glycoprotein and serum amyloid A on concanavalin A-induced liver failure via interleukin-6 induction by ME3738. Eur. J. Pharmacol. 2006, 541, 205–210. [Google Scholar] [CrossRef] [PubMed]
- Elzoghby, A.O. Gelatin-based nanoparticles as drug and gene delivery systems: Reviewing three decades of research. J. Control. Release 2013, 172, 1075–1091. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, F.; Sass, G.; Zillies, J.; Zahler, S.; Tiegs, G.; Hartkorn, A.; Fuchs, S.; Wagner, J.; Winter, G.; Coester, C.; et al. A novel technique for selective NF-kappaB inhibition in Kupffer cells: Contrary effects in fulminant hepatitis and ischaemia-reperfusion. Gut 2009, 58, 1670–1678. [Google Scholar] [CrossRef] [PubMed]
- Dwivedi, P.; Kansal, S.; Sharma, M.; Shukla, R.; Verma, A.; Shukla, P.; Tripathi, P.; Gupta, P.; Saini, D.; Khandelwal, K.; et al. Exploiting 4-sulphate N-acetyl galactosamine decorated gelatin nanoparticles for effective targeting to professional phagocytes in vitro and in vivo. J. Drug Target. 2012, 20, 883–896. [Google Scholar] [CrossRef] [PubMed]
- Jain, S.K.; Gupta, Y.; Jain, A.; Saxena, A.R.; Khare, P.; Jain, A. Mannosylated gelatin nanoparticles bearing an anti-HIV drug didanosine for site-specific delivery. Nanomedicine 2008, 4, 41–48. [Google Scholar] [CrossRef] [PubMed]
- Garg, M.; Madan, J.; Pandey, R.S.; Sardana, S.; Katyal, A.; Chandra, R. Galactosylated gelatin nanovectors of doxorubicin inhibit cell proliferation and induce apoptosis in hepatocarcinoma cells. Anticancer Drugs 2012, 23, 836–845. [Google Scholar] [CrossRef] [PubMed]
- Smani, Y. Hemospan: A hemoglobin-based oxygen carrier for potential use as a blood substitute and for the potential treatment of critical limb ischemia. Curr. Opin. Investig. Drugs 2008, 9, 1009–1019. [Google Scholar] [PubMed]
- Chen, J.Y.; Scerbo, M.; Kramer, G. A review of blood substitutes: Examining the history, clinical trial results, and ethics of hemoglobin-based oxygen carriers. Clinics 2009, 64, 803–813. [Google Scholar] [CrossRef] [PubMed]
- Jahr, J.S.; Moallempour, M.; Lim, J.C. HBOC-201, hemoglobin glutamer-250 (bovine), Hemopure (Biopure Corporation). Expert. Opin. Biol. Ther. 2008, 8, 1425–1433. [Google Scholar] [CrossRef] [PubMed]
- Sakai, H. Present situation of the development of cellular-type hemoglobin-based oxygen carrier (hemoglobin-vesicles). Curr. Drug Discov. Technol. 2012, 9, 188–193. [Google Scholar] [CrossRef] [PubMed]
- Ananthakrishnan, R.; Li, Q.; O’Shea, K.M.; Quadri, N.; Wang, L.; Abuchowski, A.; Schmidt, A.M.; Ramasamy, R. Carbon monoxide form of PEGylated hemoglobin protects myocardium against ischemia/reperfusion injury in diabetic and normal mice. Artif. Cells Nanomed. Biotechnol. 2013, 41, 428–436. [Google Scholar] [CrossRef] [PubMed]
- Nagao, S.; Taguchi, K.; Sakai, H.; Tanaka, R.; Horinouchi, H.; Watanabe, H.; Kobayashi, K.; Otagiri, M.; Maruyama, T. Carbon monoxide-bound hemoglobin-vesicles for the treatment of bleomycin-induced pulmonary fibrosis. Biomaterials 2014, 35, 6553–6562. [Google Scholar] [CrossRef] [PubMed]
- Sakai, H.; Horinouchi, H.; Tsuchida, E.; Kobayashi, K. Hemoglobin vesicles and red blood cells as carriers of carbon monoxide prior to oxygen for resuscitation after hemorrhagic shock in a rat model. Shock 2009, 31, 507–514. [Google Scholar] [CrossRef] [PubMed]
- Ogaki, S.; Taguchi, K.; Watanabe, H.; Ishima, Y.; Otagiri, M.; Maruyama, T. Carbon monoxide-bound red blood cell resuscitation ameliorates hepatic injury induced by massive hemorrhage and red blood cell resuscitation via hepatic cytochrome P450 protection in hemorrhagic shock rats. J. Pharm. Sci. 2014, 103, 2199–2206. [Google Scholar] [CrossRef] [PubMed]
- Ogaki, S.; Taguchi, K.; Watanabe, H.; Otagiri, M.; Maruyama, T. Carbon monoxide-bound red blood cells protect red blood cell transfusion-induced hepatic cytochrome P450 impairment in hemorrhagic-shock rats. Drug Metab. Dispos. 2013, 41, 141–148. [Google Scholar] [CrossRef] [PubMed]
- Kristiansen, M.; Graversen, J.H.; Jacobsen, C.; Sonne, O.; Hoffman, H.J.; Law, S.K.; Moestrup, S.K. Identification of the haemoglobin scavenger receptor. Nature 2001, 409, 198–201. [Google Scholar] [CrossRef] [PubMed]
- Schaer, D.J.; Schaer, C.A.; Buehler, P.W.; Boykins, R.A.; Schoedon, G.; Alayash, A.I.; Schaffner, A. CD163 is the macrophage scavenger receptor for native and chemically modified hemoglobins in the absence of haptoglobin. Blood 2006, 107, 373–380. [Google Scholar] [CrossRef] [PubMed]
- Zhang, N.; Palmer, A.F. Liposomes surface conjugated with human hemoglobin target delivery to macrophages. Biotechnol. Bioeng. 2012, 109, 823–829. [Google Scholar] [CrossRef] [PubMed]
- Brookes, S.; Biessels, P.; Ng, N.F.; Woods, C.; Bell, D.N.; Adamson, G. Synthesis and characterization of a hemoglobin-ribavirin conjugate for targeted drug delivery. Bioconjug. Chem. 2006, 17, 530–537. [Google Scholar] [CrossRef] [PubMed]
- Levy, G.A.; Adamson, G.; Phillips, M.J.; Scrocchi, L.A.; Fung, L.; Biessels, P.; Ng, N.F.; Ghanekar, A.; Rowe, A.; Ma, M.X.; et al. Targeted delivery of ribavirin improves outcome of murine viral fulminant hepatitis via enhanced anti-viral activity. Hepatology 2006, 43, 581–591. [Google Scholar] [CrossRef] [PubMed]
- Etzerodt, A.; Moestrup, S.K. CD163 and inflammation: Biological, diagnostic, and therapeutic aspects. Antioxid. Redox Signal. 2013, 18, 2352–2363. [Google Scholar] [CrossRef] [PubMed]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Taguchi, K.; Yamasaki, K.; Seo, H.; Otagiri, M. Potential Use of Biological Proteins for Liver Failure Therapy. Pharmaceutics 2015, 7, 255-274. https://doi.org/10.3390/pharmaceutics7030255
Taguchi K, Yamasaki K, Seo H, Otagiri M. Potential Use of Biological Proteins for Liver Failure Therapy. Pharmaceutics. 2015; 7(3):255-274. https://doi.org/10.3390/pharmaceutics7030255
Chicago/Turabian StyleTaguchi, Kazuaki, Keishi Yamasaki, Hakaru Seo, and Masaki Otagiri. 2015. "Potential Use of Biological Proteins for Liver Failure Therapy" Pharmaceutics 7, no. 3: 255-274. https://doi.org/10.3390/pharmaceutics7030255
APA StyleTaguchi, K., Yamasaki, K., Seo, H., & Otagiri, M. (2015). Potential Use of Biological Proteins for Liver Failure Therapy. Pharmaceutics, 7(3), 255-274. https://doi.org/10.3390/pharmaceutics7030255