The Association of Oleic Acid and Dexamethasone Acetate into Nanocapsules Enables a Reduction in the Effective Corticosteroid Dose in a UVB Radiation-Induced Sunburn Model in Mice
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Methods
2.2.1. Preparation of Nanostructured Dispersions
2.2.2. Physicochemical Characterization of Nanostructured Dispersions
pH
Assessment of Particle/Droplet Size, Polydispersity Index, and Zeta Potential of Nanostructured Dispersions
Dexamethasone Acetate Content and Encapsulation Efficiency
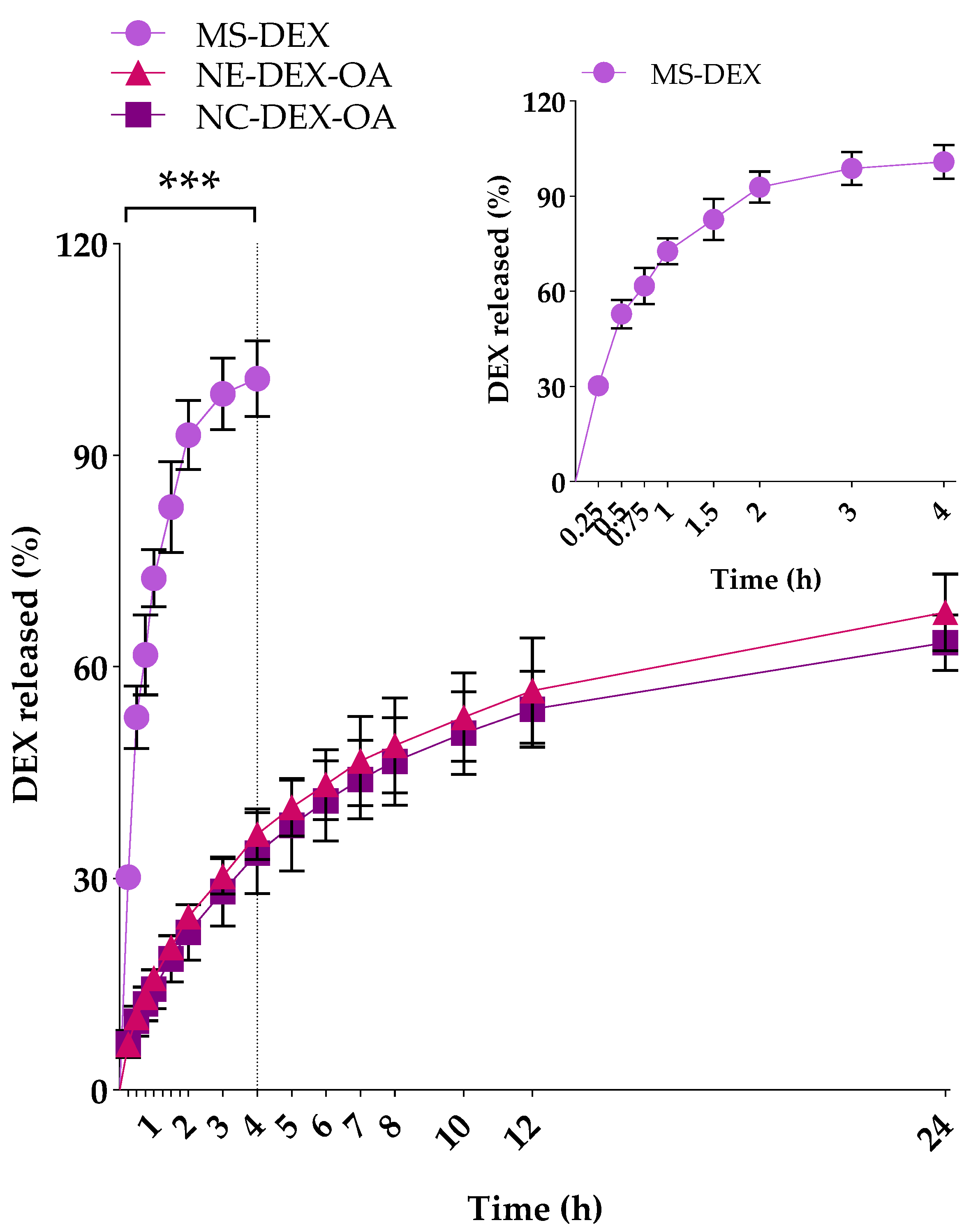
2.2.3. In Vitro Drug Release Study
2.2.4. Preparation of Nanostructure-Based Hydrogels
2.2.5. Hydrogels Characterization
pH
Particle/Droplet Size and PdI
Dexamethasone Acetate Content
Determination of Spreadability
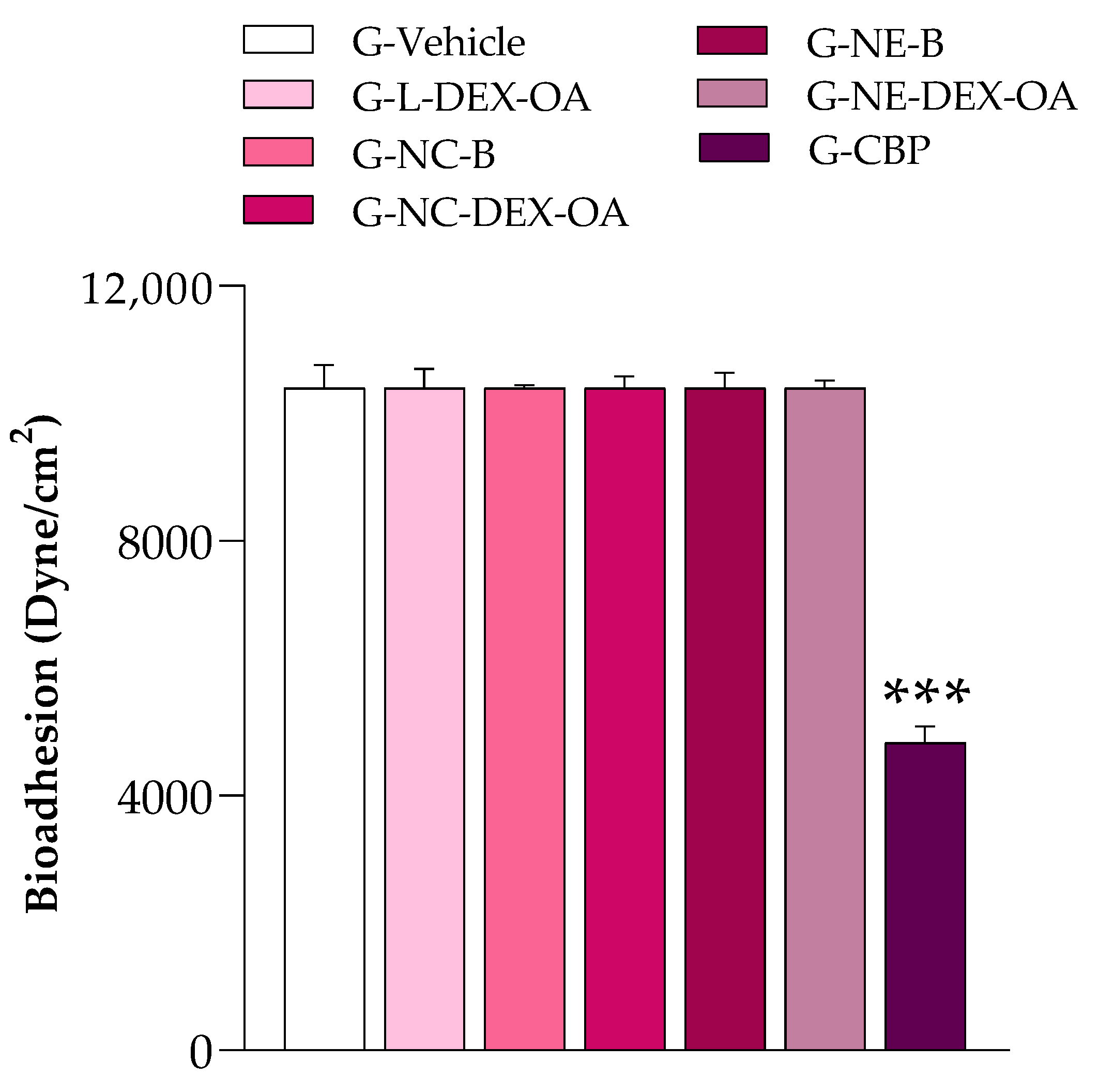
Evaluation of Bioadhesive Properties
2.2.6. Skin Permeation Study
2.2.7. In Vivo Evaluation
Animals
Antiedematogenic Efficacy
Assessment of Myeloperoxidase (MPO) Activity
Evaluation of Hydrogels’ Antiedematogenic Efficacy over 72 h
Histological Analysis
Biochemical Markers of Toxicity
2.2.8. Statistical Analysis
3. Results
3.1. Characterization of Nanostructured Dispersions
3.2. In Vitro DEX Release from Nanostructures
3.3. Hydrogels Characterization
3.4. Evaluation of Hydrogels Bioadhesive Properties
3.5. DEX Skin Permeation Study
3.6. In Vivo Anti-Inflammatory Efficacy
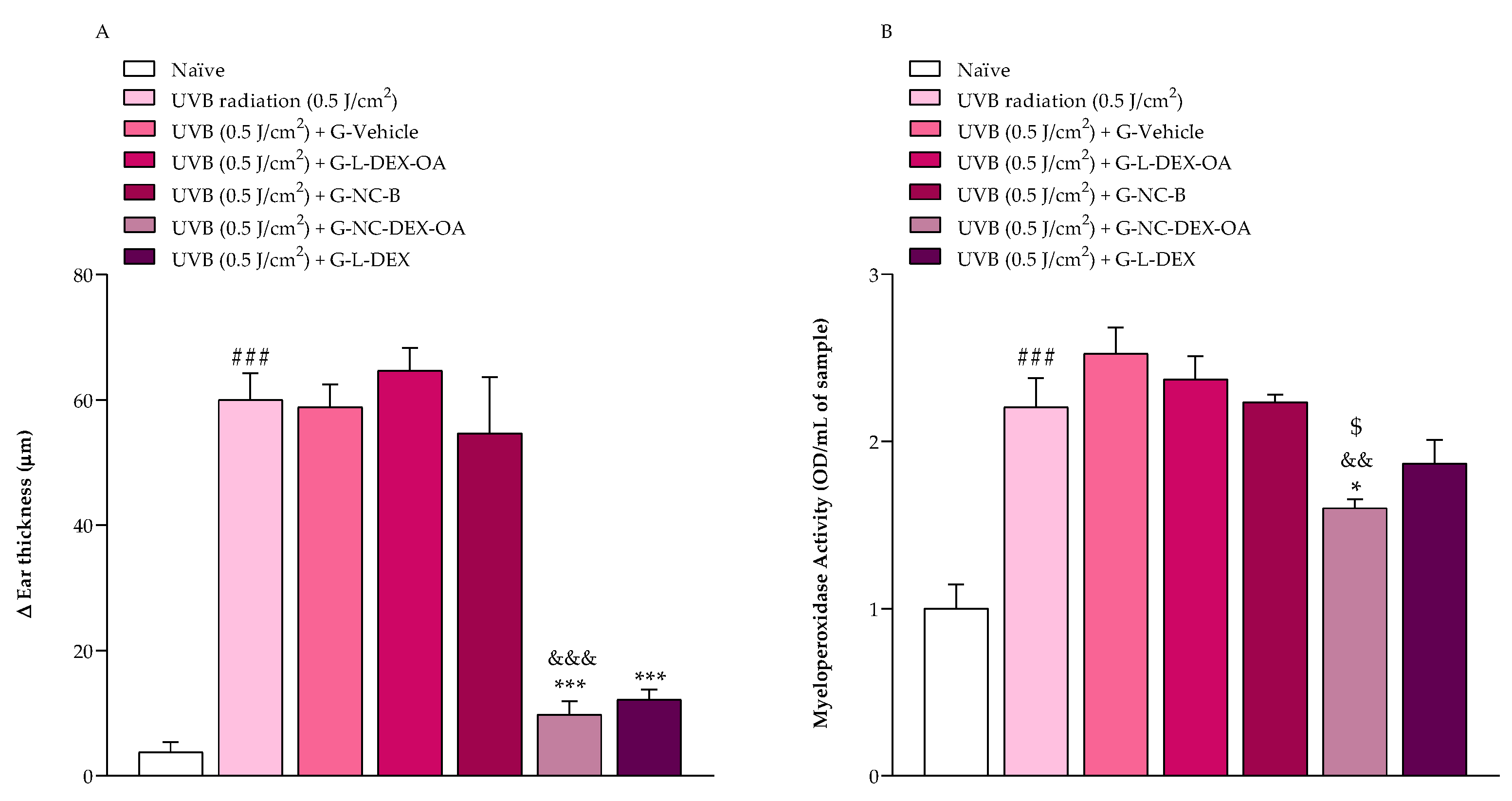
3.6.1. Assessment of Antiedematogenic Effect and Enzyme MPO Activity
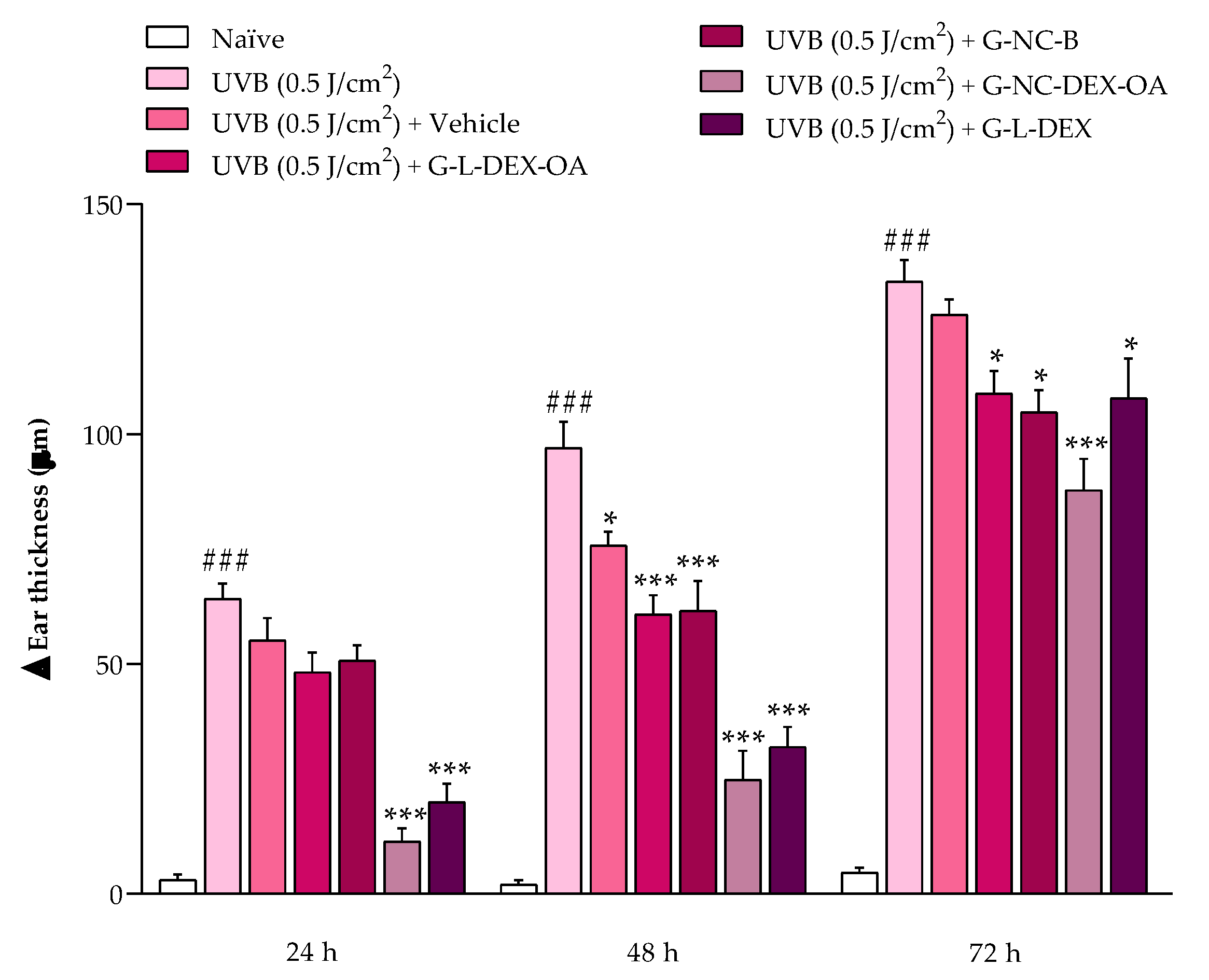
3.6.2. Evaluation of Hydrogels’ Antiedematogenic Efficacy through 72 h
3.6.3. UVB-Radiation-Induced Inflammatory Cell Infiltration
3.6.4. Preliminary Adverse Effects Assessment
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Fathallah, N.; Slim, R.; Larif, S.; Hmouda, H.; Ben Salem, C. Drug-Induced Hyperglycaemia and Diabetes. Drug Saf. 2015, 38, 1153–1168. [Google Scholar] [CrossRef] [PubMed]
- Johns, E.C.; Reynolds, R.M. Topical Glucocorticoids and Risk of Type 2 Diabetes Mellitus. Nat. Rev. Endocrinol. 2019, 15, 379–380. [Google Scholar] [CrossRef] [PubMed]
- Coondoo, A.; Phiske, M.; Verma, S.; Lahiri, K. Side-Effects of Topical Steroids: A Long Overdue Revisit. Indian Dermatol. Online J. 2014, 5, 416. [Google Scholar] [CrossRef] [PubMed]
- Frank, L.A.; Contri, R.V.; Beck, R.C.R.; Pohlmann, A.R.; Guterres, S.S. Improving Drug Biological Effects by Encapsulation into Polymeric Nanocapsules. WIREs Nanomed. Nanobiotechnol. 2015, 7, 623–639. [Google Scholar] [CrossRef] [PubMed]
- Friedrich, R.B.; Fontana, M.C.; Beck, R.C.R.; Pohlmann, A.R.; Guterres, S.S. Development and Physicochemical Characterization of Dexamethasone-Loaded Polymeric Nanocapsule Suspensions. Quim. Nova 2008, 31, 1131–1136. [Google Scholar] [CrossRef][Green Version]
- Siddique, M.I.; Katas, H.; Amin, M.C.I.M.; Ng, S.-F.; Zulfakar, M.H.; Buang, F.; Jamil, A. Minimization of Local and Systemic Adverse Effects of Topical Glucocorticoids by Nanoencapsulation: In Vivo Safety of Hydrocortisone–Hydroxytyrosol Loaded Chitosan Nanoparticles. J. Pharm. Sci. 2015, 104, 4276–4286. [Google Scholar] [CrossRef] [PubMed]
- Md, S.; Kuldeep Singh, J.K.A.; Waqas, M.; Pandey, M.; Choudhury, H.; Habib, H.; Hussain, F.; Hussain, Z. Nanoencapsulation of Betamethasone Valerate Using High Pressure Homogenization–Solvent Evaporation Technique: Optimization of Formulation and Process Parameters for Efficient Dermal Targeting. Drug Dev. Ind. Pharm. 2019, 45, 323–332. [Google Scholar] [CrossRef] [PubMed]
- Ramos Campos, E.V.; Proença, P.L.D.F.; Doretto-Silva, L.; Andrade-Oliveira, V.; Fraceto, L.F.; de Araujo, D.R. Trends in Nanoformulations for Atopic Dermatitis Treatment. Expert. Opin. Drug Deliv. 2020, 17, 1615–1630. [Google Scholar] [CrossRef]
- Sutradhar, K.B.; Amin, M.L. Nanoemulsions: Increasing Possibilities in Drug Delivery. Eur. J. Nanomed. 2013, 5, 97–110. [Google Scholar] [CrossRef]
- Deng, S.; Gigliobianco, M.R.; Censi, R.; Di Martino, P. Polymeric Nanocapsules as Nanotechnological Alternative for Drug Delivery System: Current Status, Challenges and Opportunities. Nanomaterials 2020, 10, 847. [Google Scholar] [CrossRef]
- Altammar, K.A. A Review on Nanoparticles: Characteristics, Synthesis, Applications, and Challenges. Front. Microbiol. 2023, 14, 1155622. [Google Scholar] [CrossRef] [PubMed]
- Yusuf, A.; Almotairy, A.R.Z.; Henidi, H.; Alshehri, O.Y.; Aldughaim, M.S. Nanoparticles as Drug Delivery Systems: A Review of the Implication of Nanoparticles’ Physicochemical Properties on Responses in Biological Systems. Polymers 2023, 15, 1596. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Zhou, Y.; Sun, Q.; Zhou, C.; Hu, S.; Lenahan, C.; Xu, W.; Deng, Y.; Li, G.; Tao, S. Update on Nanoparticle-Based Drug Delivery System for Anti-Inflammatory Treatment. Front. Bioeng. Biotechnol. 2021, 9, 630352. [Google Scholar] [CrossRef]
- Rigon, C.; Marchiori, M.C.L.; da Silva Jardim, F.; Pegoraro, N.S.; Chaves, P.d.S.; Velho, M.C.; Beck, R.C.R.; Ourique, A.F.; Sari, M.H.M.; de Oliveira, S.M.; et al. Hydrogel Containing Silibinin Nanocapsules Presents Effective Anti-Inflammatory Action in a Model of Irritant Contact Dermatitis in Mice. Eur. J. Pharm. Sci. 2019, 137, 104969. [Google Scholar] [CrossRef] [PubMed]
- Giuliani, L.M.; Osmari, B.F.; Camponogara, C.; Pegoraro, N.S.; Rechia, G.C.; Sari, M.H.M.; Oliveira, S.M.; Cruz, L. Locust Bean Gum Hydrogel Containing Indole-3-Carbinol Nanocapsules Has Prolonged Cutaneous Anti-Inflammatory Action. J. Drug Deliv. Sci. Technol. 2023, 87, 104866. [Google Scholar] [CrossRef]
- Tan, Q.; He, L.; Meng, X.; Wang, W.; Pan, H.; Yin, W.; Zhu, T.; Huang, X.; Shan, H. Macrophage Biomimetic Nanocarriers for Anti-Inflammation and Targeted Antiviral Treatment in COVID-19. J. Nanobiotechnol. 2021, 19, 173. [Google Scholar] [CrossRef] [PubMed]
- Jebbawi, R.; Fruchon, S.; Turrin, C.-O.; Blanzat, M.; Poupot, R. Supramolecular and Macromolecular Matrix Nanocarriers for Drug Delivery in Inflammation-Associated Skin Diseases. Pharmaceutics 2020, 12, 1224. [Google Scholar] [CrossRef]
- Mao, L.; Wu, W.; Wang, M.; Guo, J.; Li, H.; Zhang, S.; Xu, J.; Zou, J. Targeted Treatment for Osteoarthritis: Drugs and Delivery System. Drug Deliv. 2021, 28, 1861–1876. [Google Scholar] [CrossRef]
- Zhang, Z.; Yu, Y.; Zhu, G.; Zeng, L.; Xu, S.; Cheng, H.; Ouyang, Z.; Chen, J.; Pathak, J.L.; Wu, L.; et al. The Emerging Role of Plant-Derived Exosomes-Like Nanoparticles in Immune Regulation and Periodontitis Treatment. Front. Immunol. 2022, 13, 896745. [Google Scholar] [CrossRef]
- Luo, W.; Bai, L.; Zhang, J.; Li, Z.; Liu, Y.; Tang, X.; Xia, P.; Xu, M.; Shi, A.; Liu, X.; et al. Polysaccharides-Based Nanocarriers Enhance the Anti-Inflammatory Effect of Curcumin. Carbohydr. Polym. 2023, 311, 120718. [Google Scholar] [CrossRef]
- Pegoraro, N.S.; Barbieri, A.V.; Camponogara, C.; Mattiazzi, J.; Brum, E.S.; Marchiori, M.C.L.; Oliveira, S.M.; Cruz, L. Nanoencapsulation of Coenzyme Q10 and Vitamin E Acetate Protects against UVB Radiation-Induced Skin Injury in Mice. Colloids Surf. B Biointerfaces 2017, 150, 32–40. [Google Scholar] [CrossRef]
- Camponogara, C.; Brum, E.S.; Pegoraro, N.S.; Brusco, I.; Brucker, N.; Oliveira, S.M. Diosmetin, a Novel Transient Receptor Potential Vanilloid 1 Antagonist, Alleviates the UVB Radiation-Induced Skin Inflammation in Mice. Inflammopharmacology 2021, 29, 879–895. [Google Scholar] [CrossRef]
- Yu, C.-H.; Suh, B.; Shin, I.; Kim, E.-H.; Kim, D.; Shin, Y.-J.; Chang, S.-Y.; Baek, S.-H.; Kim, H.; Bae, O.-N. Inhibitory Effects of a Novel Chrysin-Derivative, CPD 6, on Acute and Chronic Skin Inflammation. Int. J. Mol. Sci. 2019, 20, 2607. [Google Scholar] [CrossRef]
- Wittmann, M.; McGonagle, D.; Werfel, T. Cytokines as Therapeutic Targets in Skin Inflammation. Cytokine Growth Factor. Rev. 2014, 25, 443–451. [Google Scholar] [CrossRef]
- Yao, Y.; Ravn Jørgensen, A.-H.; Thomsen, S.F. Biologics for Chronic Inflammatory Skin Diseases: An Update for the Clinician. J. Dermatol. Treat. 2020, 31, 108–130. [Google Scholar] [CrossRef]
- Moayedi, A.; Rezaei, K.; Moini, S.; Keshavarz, B. Chemical Compositions of Oils from Several Wild Almond Species. J. Am. Oil Chem. Soc. 2011, 88, 503–508. [Google Scholar] [CrossRef]
- Garavaglia, J.; Markoski, M.M.; Oliveira, A.; Marcadenti, A. Grape Seed Oil Compounds: Biological and Chemical Actions for Health. Nutr. Metab. Insights 2016, 9, NMI.S32910. [Google Scholar] [CrossRef]
- Akkaya, M.R. Prediction of Fatty Acid Composition of Sunflower Seeds by Near-Infrared Reflectance Spectroscopy. J. Food Sci. Technol. 2018, 55, 2318–2325. [Google Scholar] [CrossRef] [PubMed]
- El Riachy, M.; Hamade, A.; Ayoub, R.; Dandachi, F.; Chalak, L. Oil Content, Fatty Acid and Phenolic Profiles of Some Olive Varieties Growing in Lebanon. Front. Nutr. 2019, 6, 94. [Google Scholar] [CrossRef] [PubMed]
- Pegoraro, N.S.; Camponogara, C.; Gehrcke, M.; Giuliani, L.M.; da Silva, D.T.; Maurer, L.H.; Dias, P.; Emanuelli, T.; Cruz, L.; Oliveira, S.M. Oleic Acid-Containing Semisolid Dosage Forms Exhibit In Vivo Anti-Inflammatory Effect via Glucocorticoid Receptor in a UVB Radiation-Induced Skin Inflammation Model. Inflammopharmacology 2020, 28, 773–786. [Google Scholar] [CrossRef] [PubMed]
- Pegoraro, N.S.; Camponogara, C.; Cruz, L.; Oliveira, S.M. Oleic Acid Exhibits an Expressive Anti-Inflammatory Effect in Croton Oil-Induced Irritant Contact Dermatitis without the Occurrence of Toxicological Effects in Mice. J. Ethnopharmacol. 2021, 267, 113486. [Google Scholar] [CrossRef]
- Fessi, H.; Puisieux, F.; Devissaguet, J.P.; Ammoury, N.; Benita, S. Nanocapsule Formation by Interfacial Polymer Deposition Following Solvent Displacement. Int. J. Pharm. 1989, 55, R1–R4. [Google Scholar] [CrossRef]
- Urban, M.C.C.; Mainardes, R.M.; Gremião, M.P.D. Development and Validation of HPLC Method for Analysis of Dexamethasone Acetate in Microemulsions. Braz. J. Pharm. Sci. 2009, 45, 87–92. [Google Scholar] [CrossRef]
- Borghetti, G.S.; Knorst, M.T. Desenvolvimento e Avaliação Da Estabilidade Física de Loções O/A Contendo Filtros Solares. Rev. Bras. Ciências Farm. 2006, 42, 531–537. [Google Scholar] [CrossRef]
- Rigo, L.A.; Weber, J.; de Silva, C.B.; Beck, R.C.R. Evaluation of the Spreadability of Pharmaceutical or Cosmetic Semisolid Formulations Using Scanned Images. Lat. Am. J. Pharm. 2012, 31, 1387–1391. [Google Scholar]
- Osmari, B.F.; Giuliani, L.M.; Reolon, J.B.; Rigo, G.V.; Tasca, T.; Cruz, L. Gellan Gum-Based Hydrogel Containing Nanocapsules for Vaginal Indole-3-Carbinol Delivery in Trichomoniasis Treatment. Eur. J. Pharm. Sci. 2020, 151, 105379. [Google Scholar] [CrossRef] [PubMed]
- Hobson, D.W. Dermal and Ocular Toxicology: Fundamentals and Methods; Hobson, D.W., Ed.; CRC Press: Boca Raton, FL, USA, 1991. [Google Scholar]
- Laneri, S.; Sacchi, A.; Fratter, A.; Bertin, W.; Bino, A.; Vertuani, S.; Manfredini, S. Self-Nanoemulsifying System in the Accumulation of Resveratrol and N- Acetylcysteine in the Epidermis and Dermis. Nat. Prod. Commun. 2017, 12, 1934578X1701201. [Google Scholar] [CrossRef]
- McGrath, J.C.; Lilley, E. Implementing guidelines on reporting research using animals (ARRIVE etc.): New requirements for publication in BJP. Br. J. Pharmacol. 2015, 172, 3189–3193. [Google Scholar] [CrossRef]
- University of Iowa. Vertebrate Animal Research—Anesthesia Guideline; University of Iowa: Iowa City, IA, USA, 2020. [Google Scholar]
- Oliveira, S.M.; Silva, C.R.; Wentz, A.P.; Paim, G.R.; Correa, M.S.; Bonacorso, H.G.; Prudente, A.S.; Otuki, M.F.; Ferreira, J. Antinociceptive Effect of 3-(4-Fluorophenyl)-5-Trifluoromethyl-1H-1-Tosylpyrazole. A Celecoxib Structural Analog in Models of Pathological Pain. Pharmacol. Biochem. Behav. 2014, 124, 396–404. [Google Scholar] [CrossRef]
- Camponogara, C.; Silva, C.R.; Brusco, I.; Piana, M.; Faccin, H.; de Carvalho, L.M.; Schuch, A.; Trevisan, G.; Oliveira, S.M. Nasturtium Officinale R. Br. Effectively Reduces the Skin Inflammation Induced by Croton Oil via Glucocorticoid Receptor-Dependent and NF-ΚB Pathways without Causing Toxicological Effects in Mice. J. Ethnopharmacol. 2019, 229, 190–204. [Google Scholar] [CrossRef]
- Vaughn, A.R.; Clark, A.K.; Sivamani, R.K.; Shi, V.Y. Natural Oils for Skin-Barrier Repair: Ancient Compounds Now Backed by Modern Science. Am. J. Clin. Dermatol. 2018, 19, 103–117. [Google Scholar] [CrossRef] [PubMed]
- Flores, M.; Saravia, C.; Vergara, C.; Avila, F.; Valdés, H.; Ortiz-Viedma, J. Avocado Oil: Characteristics, Properties, and Applications. Molecules 2019, 24, 2172. [Google Scholar] [CrossRef]
- Sales-Campos, H.; Reis de Souza, P.; Crema Peghini, B.; Santana da Silva, J.; Ribeiro Cardoso, C. An Overview of the Modulatory Effects of Oleic Acid in Health and Disease. Mini Rev. Med. Chem. 2013, 13, 201–210. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.-Y.; Lee, Y.-H.; Chang, S.-H.; Tsai, Y.-F.; Fang, J.-Y.; Hwang, T.-L. Oleic Acid-Loaded Nanostructured Lipid Carrier Inhibits Neutrophil Activities in the Presence of Albumin and Alleviates Skin Inflammation. Int. J. Nanomed. 2019, 14, 6539–6553. [Google Scholar] [CrossRef] [PubMed]
- Lio, P.A.; Lee, M.; LeBovidge, J.; Timmons, K.G.; Schneider, L. Clinical Management of Atopic Dermatitis: Practical Highlights and Updates from the Atopic Dermatitis Practice Parameter 2012. J. Allergy Clin. Immunol. Pract. 2014, 2, 361–369. [Google Scholar] [CrossRef]
- Sabat, R.; Wolk, K.; Loyal, L.; Döcke, W.-D.; Ghoreschi, K. T Cell Pathology in Skin Inflammation. Semin. Immunopathol. 2019, 41, 359–377. [Google Scholar] [CrossRef]
- Patra, J.K.; Das, G.; Fraceto, L.F.; Campos, E.V.R.; del Rodriguez-Torres, M.P.; Acosta-Torres, L.S.; Diaz-Torres, L.A.; Grillo, R.; Swamy, M.K.; Sharma, S.; et al. Nano Based Drug Delivery Systems: Recent Developments and Future Prospects. J. Nanobiotechnol. 2018, 16, 71. [Google Scholar] [CrossRef]
- Lee, J.H.; Yeo, Y. Controlled Drug Release from Pharmaceutical Nanocarriers. Chem. Eng. Sci. 2015, 125, 75–84. [Google Scholar] [CrossRef]
- Baryakova, T.H.; Pogostin, B.H.; Langer, R.; McHugh, K.J. Overcoming Barriers to Patient Adherence: The Case for Developing Innovative Drug Delivery Systems. Nat. Rev. Drug Discov. 2023, 22, 387–409. [Google Scholar] [CrossRef]
- Maqbool, M.A.; Mishra, M.K.; Pathak, S.; Kesharwani, A.; Kesharwani, A. Semi Solid Dosage Forms Manufacturing: Tools, Critical Process Parameters, Strategies, Optimization and Recent Advances. Indo Am. J. Pharm. Res. 2017, 7, 882–893. [Google Scholar]
- Pahri, R. Recent Advances in the Development of Semisolid Dosage Forms. In Pharmaceutical Drug Product Development and Process Optimization; Apple Academic Press: Palm Bay, FL, USA, 2020. [Google Scholar]
- Garg, A.; Aggarwal, D.; Garg, S.; Singla, A.K. Spreading of Semisolid Formulations: An Update. Pharm. Technol. 2002, 26, 84–105. [Google Scholar]
- Marto, J.; Ruivo, E.; Lucas, S.D.; Gonçalves, L.M.; Simões, S.; Gouveia, L.F.; Felix, R.; Moreira, R.; Ribeiro, H.M.; Almeida, A.J. Starch Nanocapsules Containing a Novel Neutrophil Elastase Inhibitor with Improved Pharmaceutical Performance. Eur. J. Pharm. Biopharm. 2018, 127, 1–11. [Google Scholar] [CrossRef]
- Kaur, A.; Katiyar, S.S.; Kushwah, V.; Jain, S. Nanoemulsion Loaded Gel for Topical Co-Delivery of Clobitasol Propionate and Calcipotriol in Psoriasis. Nanomedicine 2017, 13, 1473–1482. [Google Scholar] [CrossRef] [PubMed]
- de Lima, C.S.A.; Varca, J.P.R.O.; Alves, V.M.; Nogueira, K.M.; Cruz, C.P.C.; Rial-Hermida, M.I.; Kadłubowski, S.S.; Varca, G.H.C.; Lugão, A.B. Mucoadhesive Polymers and Their Applications in Drug Delivery Systems for the Treatment of Bladder Cancer. Gels 2022, 8, 587. [Google Scholar] [CrossRef] [PubMed]
- Hamdi, N.A.M.; Sabari, N.H.M.; Ismail, A.F.H.; Azmi, N.A. An Insight into the Use and Advantages of Carbopol in Topical Mucoadhesive Drug Delivery System: A Systematic Review. J. Pharm. 2023, 3, 53–65. [Google Scholar]
- Carvalho, F.C.; Bruschi, M.L.; Evangelista, R.C.; Gremião, M.P.D. Mucoadhesive Drug Delivery Systems. Braz. J. Pharm. Sci. 2010, 46, 1–17. [Google Scholar] [CrossRef]
- Kumar, A.; Naik, P.K.; Pradhan, D.; Ghosh, G.; Rath, G. Mucoadhesive Formulations: Innovations, Merits, Drawbacks, and Future Outlook. Pharm. Dev. Technol. 2020, 25, 797–814. [Google Scholar] [CrossRef] [PubMed]
- Saghazadeh, S.; Rinoldi, C.; Schot, M.; Kashaf, S.S.; Sharifi, F.; Jalilian, E.; Nuutila, K.; Giatsidis, G.; Mostafalu, P.; Derakhshandeh, H.; et al. Drug Delivery Systems and Materials for Wound Healing Applications. Adv. Drug Deliv. Rev. 2018, 127, 138–166. [Google Scholar] [CrossRef] [PubMed]
- Jacob, S.; Nair, A.B.; Shah, J.; Sreeharsha, N.; Gupta, S.; Shinu, P. Emerging Role of Hydrogels in Drug Delivery Systems, Tissue Engineering and Wound Management. Pharmaceutics 2021, 13, 357. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Leobandung, W.; Foss, A.; Peppas, N.A. Molecular Aspects of Muco- and Bioadhesion. J. Control. Release 2000, 65, 63–71. [Google Scholar] [CrossRef]
- Guerra, K.C.; Crane, J.S. Sunburn 2023. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Dhar, S.; Seth, J.; Parikh, D. Systemic Side-Effects of Topical Corticosteroids. Indian J. Dermatol. 2014, 59, 460. [Google Scholar] [CrossRef]
- Lan, C.-C.E.; Wu, C.-S.; Huang, S.-M.; Wu, C.-H.; Lai, H.-C.; Peng, Y.-T.; Hou, P.-S.; Yang, H.-J.; Chen, G.-S. Irradiance-Dependent UVB Photocarcinogenesis. Sci. Rep. 2016, 6, 37403. [Google Scholar] [CrossRef] [PubMed]
- Peng, Z.; Chen, B.; Zheng, Q.; Zhu, G.; Cao, W.; Qin, X.; Zhang, C. Ameliorative Effects of Peptides from the Oyster (Crassostrea Hongkongensis) Protein Hydrolysates against UVB-Induced Skin Photodamage in Mice. Mar. Drugs 2020, 18, 288. [Google Scholar] [CrossRef] [PubMed]
- Kalyan Kumar, G.; Dhamotharan, R.; Kulkarni, N.M.; Mahat, M.Y.A.; Gunasekaran, J.; Ashfaque, M. Embelin Reduces Cutaneous TNF-α Level and Ameliorates Skin Edema in Acute and Chronic Model of Skin Inflammation in Mice. Eur. J. Pharmacol. 2011, 662, 63–69. [Google Scholar] [CrossRef] [PubMed]
- Cho, B.O.; Che, D.N.; Shin, J.Y.; Kang, H.J.; Kim, J.H.; Kim, H.Y.; Cho, W.G.; Jang, S. Il Ameliorative Effects of Diospyros Lotus Leaf Extract against UVB-Induced Skin Damage in BALB/c Mice. Biomed. Pharmacother. 2017, 95, 264–274. [Google Scholar] [CrossRef] [PubMed]
- Németh, T.; Mócsai, A. The Role of Neutrophils in Autoimmune Diseases. Immunol. Lett. 2012, 143, 9–19. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.; Zhang, Z.; Xiong, X.; Wang, X.; Li, J.; Shi, G.; Yang, J.; Zhang, X.; Zhang, H.; Hong, J.; et al. Glucocorticoids Promote Hepatic Cholestasis in Mice by Inhibiting the Transcriptional Activity of the Farnesoid X Receptor. Gastroenterology 2012, 143, 1630–1640.e8. [Google Scholar] [CrossRef]
- Lisakovska, O.; Shymanskyy, I.; Mazanova, A.; Khomenko, A.; Veliky, M. Vitamin D3 Protects against Prednisolone-Induced Liver Injury Associated with the Impairment of the Hepatic NF-ΚB/INOS/NO Pathway. Biochem. Cell Biol. 2017, 95, 213–222. [Google Scholar] [CrossRef]
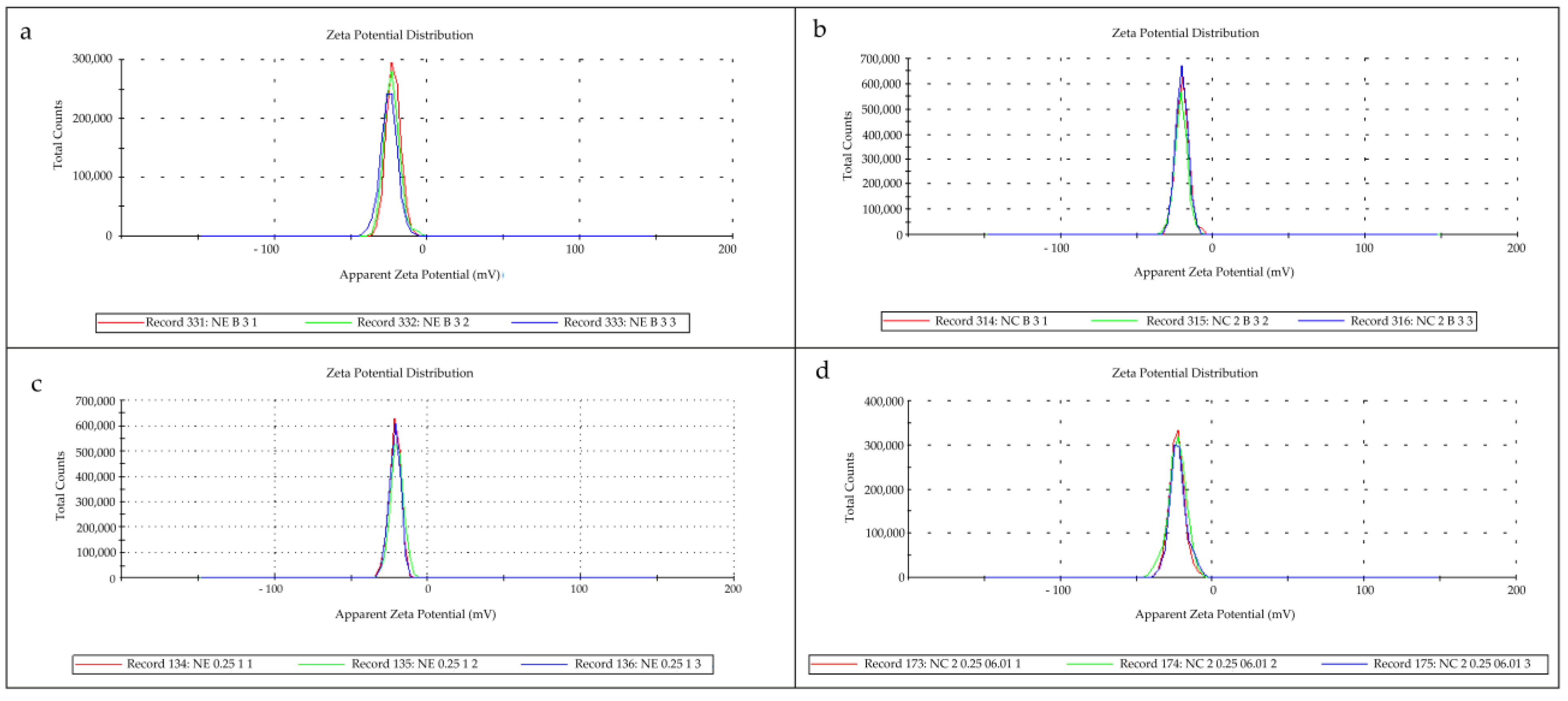


| Formulation | pH | Mean Diameter (nm) | PdI | Zeta Potential (mV) | DEX Content (%) |
|---|---|---|---|---|---|
| NC-B | 5.0 ± 0.1 | 176 ± 10 | 0.09 ± 0.06 | −20.0 ± 0.5 | - |
| NC-DEX-OA | 5.2 ± 0.1 | 175 ± 14 | 0.09 ± 0.03 | −19.8 ± 3.9 | 100.29 ± 2.44 |
| NE-B | 4.6 ± 0.2 | 208 ± 19 | 0.14 ± 0.06 | −20.8 ± 2.2 | - |
| NE-DEX-OA | 4.7 ± 0.3 | 226 ± 46 | 0.19 ± 0.08 | −22.2 ± 3.4 | 98.59 ± 3.95 |
| Formulation | pH | Mean Diameter (nm) | PdI | DEX Content (%) | SF (mm2/g) |
|---|---|---|---|---|---|
| G-Vehicle | 5.0 ± 0.2 | 1345 ± 436 *** | 0.93 ± 0.06 *** | - | 0.68 ± 0.08 |
| G-L-DEX-OA | 5.2 ± 0.1 | - | - | 100.61 ± 3.19 | 0.48 ± 0.09 |
| G-NC-B | 5.4 ± 0.2 | 195 ± 06 | 0.20 ± 0.01 | - | 0.59 ± 0.05 |
| G-NC-DEX-OA | 5.4 ± 0.1 | 181 ± 20 | 0.17 ± 0.08 | 97.23 ± 2.73 | 0.46 ± 0.05 & |
| G-NE-B | 5.1 ± 0.1 | 218 ± 28 | 0.24 ± 0.03 | - | 0.57 ± 0.09 |
| G-NE-DEX-OA | 5.3 ± 0.1 | 280 ± 38 | 0.29 ± 0.10 | 96.72 ± 1.57 | 0.51 ± 0.07 |
| Formulation | AST (U/L) | ALT (U/L) | Glucose (mg/dL) |
|---|---|---|---|
| G-NC-B | 63 ± 37 | 31 ± 18 | 163 ± 94 |
| G-NC-DEX-OA | 57 ± 25 | 28 ± 12 | 145 ± 65 |
| G-L-DEX | 59 ± 26 | 34 ± 15 | 183 ± 82 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pegoraro, N.S.; Gehrcke, M.; Camponogara, C.; Fialho, M.F.P.; Cruz, L.; Oliveira, S.M. The Association of Oleic Acid and Dexamethasone Acetate into Nanocapsules Enables a Reduction in the Effective Corticosteroid Dose in a UVB Radiation-Induced Sunburn Model in Mice. Pharmaceutics 2024, 16, 176. https://doi.org/10.3390/pharmaceutics16020176
Pegoraro NS, Gehrcke M, Camponogara C, Fialho MFP, Cruz L, Oliveira SM. The Association of Oleic Acid and Dexamethasone Acetate into Nanocapsules Enables a Reduction in the Effective Corticosteroid Dose in a UVB Radiation-Induced Sunburn Model in Mice. Pharmaceutics. 2024; 16(2):176. https://doi.org/10.3390/pharmaceutics16020176
Chicago/Turabian StylePegoraro, Natháli Schopf, Mailine Gehrcke, Camila Camponogara, Maria Fernanda Pessano Fialho, Letícia Cruz, and Sara Marchesan Oliveira. 2024. "The Association of Oleic Acid and Dexamethasone Acetate into Nanocapsules Enables a Reduction in the Effective Corticosteroid Dose in a UVB Radiation-Induced Sunburn Model in Mice" Pharmaceutics 16, no. 2: 176. https://doi.org/10.3390/pharmaceutics16020176
APA StylePegoraro, N. S., Gehrcke, M., Camponogara, C., Fialho, M. F. P., Cruz, L., & Oliveira, S. M. (2024). The Association of Oleic Acid and Dexamethasone Acetate into Nanocapsules Enables a Reduction in the Effective Corticosteroid Dose in a UVB Radiation-Induced Sunburn Model in Mice. Pharmaceutics, 16(2), 176. https://doi.org/10.3390/pharmaceutics16020176






