Solid Lipid Nanoparticles Enhancing the Leishmanicidal Activity of Delamanid
Abstract
:1. Introduction
2. Materials and Methods
2.1. Identification of Compounds Exhibiting High Activity against Trypanosomatids and Minimal Cytotoxicity
2.1.1. Database Processing
2.1.2. Molecular Docking
2.2. Determination of the Leishmanicidal Activity of the Selected Drugs
2.2.1. Leishmanicidal Activity in Promastigotes
2.2.2. Phase-Contrast Microscopy Imaging
2.3. Delamanid Encapsulation in SLNPs
2.3.1. Design and Synthesis of the SLNPs
2.3.2. Characterization of SLNPs
2.3.3. In Vitro Drug Release
2.4. In Cellulo Activity of SLNPs
2.4.1. Cellular Proof-of-Concept Drug Release
2.4.2. Transdermal PoC Drug Release
2.4.3. Electron Microscopy Imaging of Infected Macrophages
2.4.4. Leishmanicidal Activity in Amastigotes
3. Results
3.1. Identification of Compounds Exhibiting High Activity against Trypanosomatids and Minimal Cytotoxicity
3.1.1. Database Processing
3.1.2. Molecular Docking
3.2. Assessing Leishmanicidal Activity of Selected Drugs against Promastigotes
3.2.1. Leishmanicidal Activity in Promastigotes
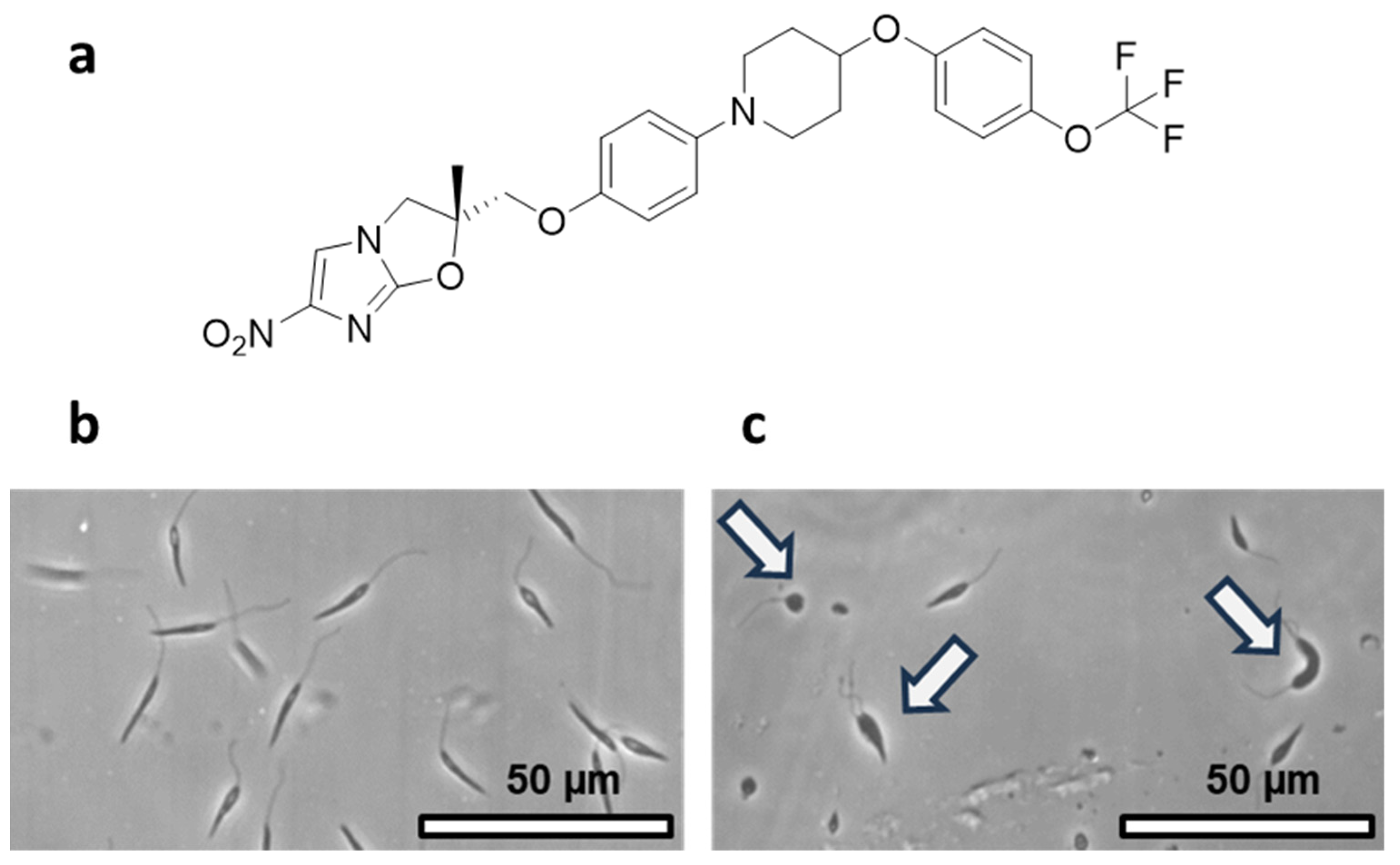
3.2.2. Phase-Contrast Microscopy Evaluation of the Effect of Delamanid on Promastigotes
3.3. Encapsulation of Delamanid in SLNPs
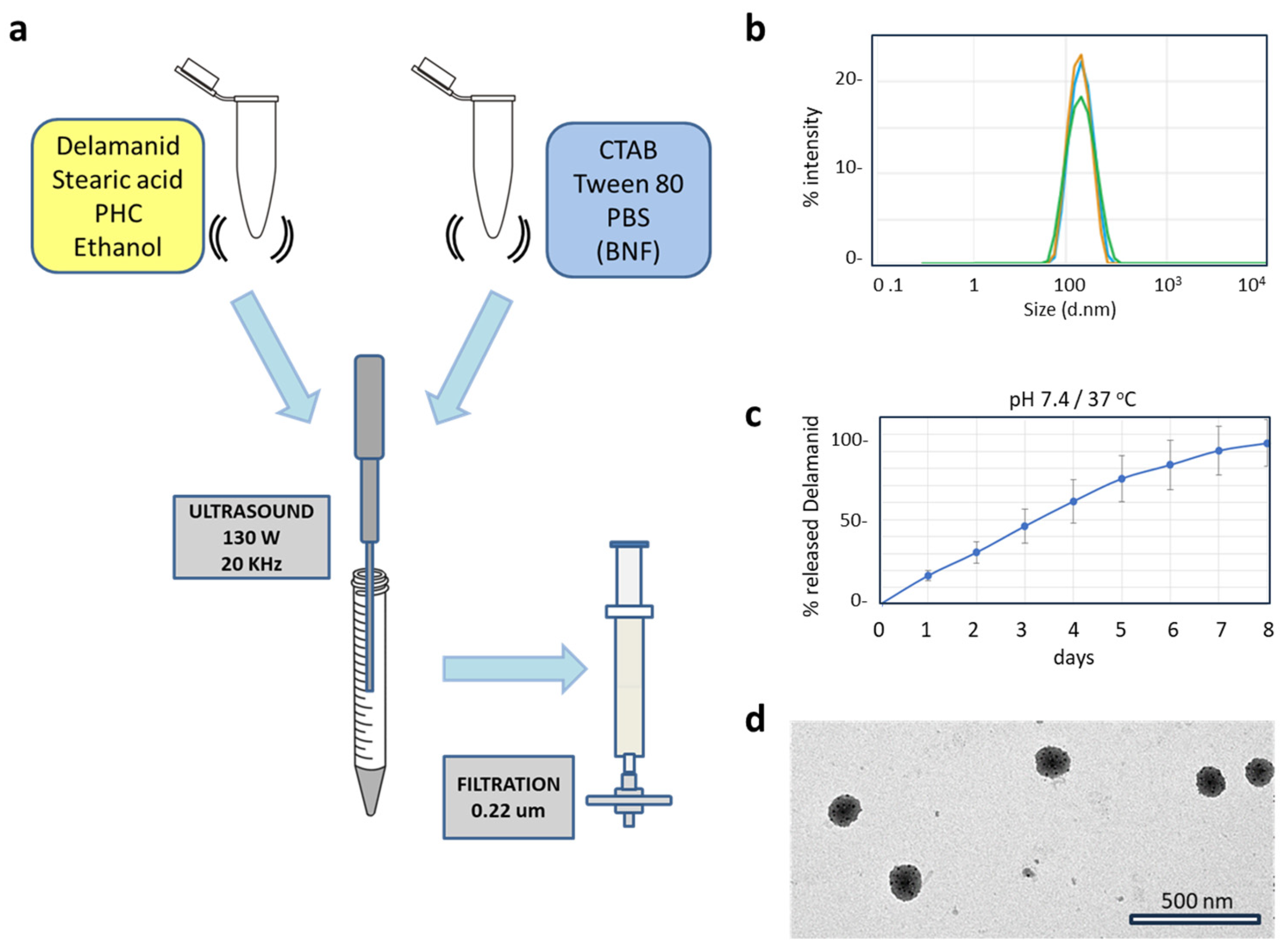
3.3.1. Design and Synthesis of the SLNPs
3.3.2. Characterization of SLNPs
3.4. SLNP Payload Release: Proof-of-Concept
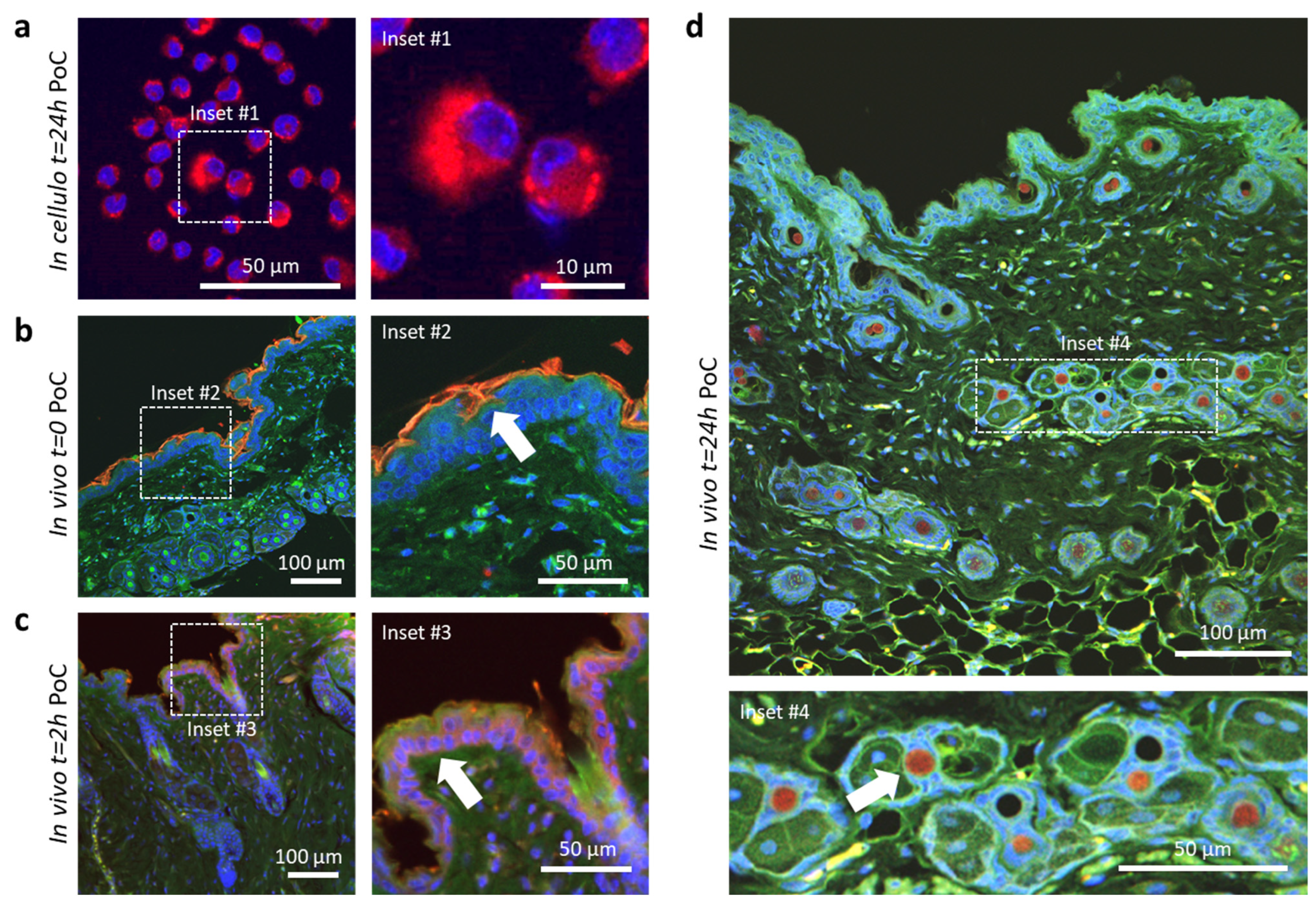
3.4.1. In Cellulo and In Vivo Payload Release
3.4.2. Subcellular Distribution of SLNPs in Infected Macrophages
3.4.3. Comparative Leishmanicidal Efficacy of SLNPs against Intracellular Amastigotes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Neglected Tropical Diseases. Available online: https://www.who.int/health-topics/neglected-tropical-diseases#tab=tab_1 (accessed on 15 November 2023).
- González, C.; Wang, O.; Strutz, S.E.; González-Salazar, C.; Sánchez-Cordero, V.; Sarkar, S. Climate Change and Risk of Leishmaniasis in North America: Predictions from Ecological Niche Models of Vector and Reservoir Species. PLoS Negl. Trop. Dis. 2010, 4, e585. [Google Scholar] [CrossRef] [PubMed]
- Wijerathna, T.; Gunathilaka, N. Time Series Analysis of Leishmaniasis Incidence in Sri Lanka: Evidence for Humidity-Associated Fluctuations. Int. J. Biometeorol. 2023, 67, 275–284. [Google Scholar] [CrossRef] [PubMed]
- Burza, S.; Croft, S.L.; Boelaert, M. Leishmaniasis. Lancet 2018, 392, 951–970. [Google Scholar] [CrossRef] [PubMed]
- Cecílio, P.; Cordeiro-da-Silva, A.; Oliveira, F. Sand Flies: Basic Information on the Vectors of Leishmaniasis and Their Interactions with Leishmania Parasites. Commun. Biol. 2022, 5, 305. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Ending the Neglect to Attain the Sustainable Development Goals: A Road Map for Neglected Diseases 2021–2030; World Health Organization: Geneva, Switzerland, 2020; ISBN 9789240010352.
- Ainsworth, C. Tropical Diseases Move North. Nature 2023. [Google Scholar] [CrossRef] [PubMed]
- WHO Expert Committee on the Control of the Leishmaniases. Control de Las Leishmaniasis: Informe de Una Reunión Del Comité de Expertos de La OMS Sobre El Control de Las Leishmaniasis, Ginebra, 22 a 26 de Marzo de 2010; Organización Mundial de la Salud: Ginebra, Switzerland, 2012.
- Lenk, E.J.; Redekop, W.K.; Luyendijk, M.; Rijnsburger, A.J.; Severens, J.L. Productivity Loss Related to Neglected Tropical Diseases Eligible for Preventive Chemotherapy: A Systematic Literature Review. PLoS Negl. Trop. Dis. 2016, 10, e0004397. [Google Scholar] [CrossRef] [PubMed]
- Sims, K.R.; MacEren, J.P.; Strand, A.I.; He, B.; Overby, C.; Benoit, D.S.W. Rigor and Reproducibility in Polymer Nanoparticle Synthesis and Characterization. RSC Adv. 2020, 10, 2513–2518. [Google Scholar] [CrossRef]
- Makin, S. Mental Health: The Invisible Effects of Neglected Tropical Diseases. Nature 2023. [Google Scholar] [CrossRef]
- Organización Panamericana de la Salud. Manual de Procedimientos Para La Vigilancia y El Control de Las Leishmaniasis En La Región de Las Américas; Organización Panamericana de la Salud: Washington, DC, USA, 2023.
- Pan American Health Organization. Guideline for the Treatment of Leishmaniasis in the Americas, 2nd ed.; Pan American Health Organization: Washington, DC, USA, 2022.
- Field, M.C.; Horn, D.; Fairlamb, A.H.; Ferguson, M.A.J.; Gray, D.W.; Read, K.D.; De Rycker, M.; Torrie, L.S.; Wyatt, P.G.; Wyllie, S.; et al. Anti-Trypanosomatid Drug Discovery: An Ongoing Challenge and a Continuing Need. Nat. Rev. Microbiol. 2017, 15, 217–231. [Google Scholar] [CrossRef]
- Ashburn, T.T.; Thor, K.B. Drug Repositioning: Identifying and Developing New Uses for Existing Drugs. Nat. Rev. Drug Discov. 2004, 3, 673–683. [Google Scholar] [CrossRef]
- Andrews, K.T.; Fisher, G.; Skinner-Adams, T.S. Drug Repurposing and Human Parasitic Protozoan Diseases. Int. J. Parasitol. Drugs Drug Resist. 2014, 4, 95–111. [Google Scholar] [CrossRef]
- Jourdan, J.P.; Bureau, R.; Rochais, C.; Dallemagne, P. Drug Repositioning: A Brief Overview. J. Pharm. Pharmacol. 2020, 72, 1145–1151. [Google Scholar] [CrossRef] [PubMed]
- Gns, H.S.; Saraswathy, G.R.; Murahari, M.; Krishnamurthy, M. An Update on Drug Repurposing: Re-Written Saga of the Drug’s Fate. Biomed. Pharmacother. 2019, 110, 700–716. [Google Scholar] [CrossRef] [PubMed]
- Hua, Y.; Dai, X.; Xu, Y.; Xing, G.; Liu, H.; Lu, T.; Chen, Y.; Zhang, Y. Drug Repositioning: Progress and Challenges in Drug Discovery for Various Diseases. Eur. J. Med. Chem. 2022, 234, 114239. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.; Park, J.; Shim, M.K.; Um, W.; Yoon, H.Y.; Ryu, J.H.; Lim, D.K.; Kim, K. Recent Advances and Challenges of Repurposing Nanoparticle-Based Drug Delivery Systems to Enhance Cancer Immunotherapy. Theranostics 2019, 9, 7906–7923. [Google Scholar] [CrossRef] [PubMed]
- Volpedo, G.; Costa, L.; Ryan, N.; Halsey, G.; Satoskar, A.; Oghumu, S. Nanoparticulate Drug Delivery Systems for the Treatment of Neglected Tropical Protozoan Diseases. J. Venom. Anim. Toxins Incl. Trop. Dis. 2019, 25, e144118. [Google Scholar] [CrossRef]
- Haider, M.; Abdin, S.M.; Kamal, L.; Orive, G. Nanostructured Lipid Carriers for Delivery of Chemotherapeutics: A Review. Pharmaceutics 2020, 12, 288. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, V.H.; Thuy, V.N.; Van, T.V.; Dao, A.H.; Lee, B.J. Nanostructured Lipid Carriers and Their Potential Applications for Versatile Drug Delivery via Oral Administration. OpenNano 2022, 8, 100064. [Google Scholar] [CrossRef]
- Assefi, M.; Ataeinaeini, M.; Nazari, A.; Gholipour, A.; Vertiz-Osores, J.J.; Melody Calla-Vásquez, K.; Zuhair Talib Al-Naqeeb, B.; Hussein Jassim, K.; Kalajahi, H.G.; Yasamineh, S.; et al. A State-of-the-Art Review on Solid Lipid Nanoparticles as a Nanovaccines Delivery System. J. Drug Deliv. Sci. Technol. 2023, 86, 104623. [Google Scholar] [CrossRef]
- Punu, G.F.; Harahap, Y.; Anjani, Q.K.; Hartrianti, P.; Donnelly, R.F.; Ramadon, D. Solid Lipid Nanoparticles (SLN): Formulation and Fabrication. Pharm. Sci. Res. (PSR) 2023, 10, 55–66. [Google Scholar]
- Duan, Y.; Dhar, A.; Patel, C.; Khimani, M.; Neogi, S.; Sharma, P.; Siva Kumar, N.; Vekariya, R.L. A Brief Review on Solid Lipid Nanoparticles: Part and Parcel of Contemporary Drug Delivery Systems. RSC Adv. 2020, 10, 26777–26791. [Google Scholar] [CrossRef]
- Wadekar, A.B.; Manwar, J.V.; Bakal, R.L.; Kumbhar, D.D. Mechanisms and Pharmaceutical Application of Solid Lipid Nanoparticles as Efficient Drug Delivery System. Syst. Rev. Pharm. 2022, 13, 870–881. [Google Scholar]
- Abualfaraa, W.; Salonitis, K.; Al-Ashaab, A.; Ala’raj, M. Lean-Green Manufacturing Practices and Their Link with Sustainability: A Critical Review. Sustainability 2020, 12, 981. [Google Scholar] [CrossRef]
- Anastas, P.; Eghbali, N. Green Chemistry: Principles and Practice. Chem. Soc. Rev. 2010, 39, 301–312. [Google Scholar] [CrossRef] [PubMed]
- Duan, H.; Wang, D.; Li, Y. Green Chemistry for Nanoparticle Synthesis. Chem. Soc. Rev. 2015, 44, 5778–5792. [Google Scholar] [CrossRef]
- Singh, H.; Desimone, M.F.; Pandya, S.; Jasani, S.; George, N.; Adnan, M.; Aldarhami, A.; Bazaid, A.S.; Alderhami, S.A. Revisiting the Green Synthesis of Nanoparticles: Uncovering Influences of Plant Extracts as Reducing Agents for Enhanced Synthesis Efficiency and Its Biomedical Applications. Int. J. Nanomed. 2023, 18, 4727–4750. [Google Scholar] [CrossRef] [PubMed]
- Uzcanga, G.; Lara, E.; Gutiérrez, F.; Beaty, D.; Beske, T.; Teran, R.; Navarro, J.C.; Pasero, P.; Benítez, W.; Poveda, A. Nuclear DNA Replication and Repair in Parasites of the Genus Leishmania: Exploiting Differences to Develop Innovative Therapeutic Approaches. Crit. Rev. Microbiol. 2017, 43, 156–177. [Google Scholar] [CrossRef] [PubMed]
- Espíndola, L. Validación de La ADN Opoisomerasa Tipo II Como Diana Terapéutica En El Tratamiento de Leishmaniasis. Bachelor’s Thesis, Universidad San Francisco de Quito, Quito, Ecuador, 2019. [Google Scholar]
- Jacho, D.; Méndez, M.A.; Santamaría-Aguirre, J. Métodos Computacionales Para El Diseño de Fluoroquinolonas Con Alta Afinidad Por Topoisomerasa II de Leishmania. Bachelor’s Thesis, Universidad Central del Ecuador, Quito, Ecuador, 2021. [Google Scholar]
- Esteves, L. Efecto de Las Fluoroquinolonas Sobre Topoisomerosas Tipo II En Trypanosomatidae. Bachelor’s Thesis, Universidad Central del Ecuador, Quito, Ecuador, 2018. [Google Scholar]
- Shi, Z.; Zhang, J.; Tian, L.; Xin, L.; Liang, C.; Ren, X.; Li, M. A Comprehensive Overview of the Antibiotics Approved in the Last Two Decades: Retrospects and Prospects. Molecules 2023, 28, 1762. [Google Scholar] [CrossRef]
- Matera, M.G. Pharmacologic Characteristics of Prulifloxacin. Pulm. Pharmacol. Ther. 2006, 19, 20–29. [Google Scholar] [CrossRef]
- Hudhomme, P. Four-Membered Rings with One Sulfur and One Nitrogen Atom. In Comprehensive Heterocyclic Chemistry III; Katritzky, A., Ramsden, C., Taylor, R., Eds.; Elsevier Science: Amsterdam, The Netherlands, 2008. [Google Scholar]
- Albarracín, J. Efecto de La Enrofloxacina En La Movilidad de Los Promastigotes de Leishmania Mexicana. Bachelor’s Thesis, Universidad Central del Ecuador, Quito, Ecuador, 2020. [Google Scholar]
- Loachamin, G. Comparación de La Actividad Leishmanicida de Los Transferosomas de Enrofloxacina Frente a Enrofloxacina En Solución Usando Promastigotes de L. Mexicana Como Modelo Biológico. Bachelor’s Thesis, Universidad Central del Ecuador, Quito, Ecuador, 2018. [Google Scholar]
- Morales, N. Desarrollo de Nanopartículas de Enrofloxacina de Liberación Modificada. Bachelor’s Thesis, Universidad Central del Ecuador, Quito, Ecuador, 2018. [Google Scholar]
- Patterson, S.; Wyllie, S.; Norval, S.; Stojanovski, L.; Simeons, F.R.; Auer, J.L.; Osuna-Cabello, M.; Read, K.D.; Fairlamb, A.H. The Anti-Tubercular Drug Delamanid as a Potential Oral Treatment for Visceral Leishmaniasis. eLife 2016, 5, e09744. [Google Scholar] [CrossRef]
- European Chemicals Agency. Substance Infocard Cetrimonium Bromide. Available online: https://echa.europa.eu/substance-information/-/substanceinfo/100.000.283 (accessed on 20 October 2023).
- Dhiman, N.; Awasthi, R.; Sharma, B.; Kharkwal, H.; Kulkarni, G.T. Lipid Nanoparticles as Carriers for Bioactive Delivery. Front. Chem. 2021, 9, 580118. [Google Scholar] [CrossRef]
- García-Hevia, L.; Casafont, I.; Oliveira, J.; Terán, N.; Fanarraga, M.L.; Gallo, J.; Bañobre-López, M. Magnetic lipid nanovehicles synergize the controlled thermal release of chemotherapeutics with magnetic ablation while enabling non-invasive monitoring by MRI for melanoma theranostics. Bioact. Mat. 2021, 17, 153–164. [Google Scholar] [CrossRef]
- Ghasemiyeh, P.; Mohammadi-Samani, S. Solid Lipid Nanoparticles and Nanostructured Lipid Carriers as Novel Drug Delivery Systems: Applications, Advantages and Disadvantages. Res. Pharm. Sci. 2018, 13, 288–303. [Google Scholar] [CrossRef] [PubMed]
- Khoshnood, S.; Taki, E.; Sadeghifard, N.; Kaviar, V.H.; Haddadi, M.H.; Farshadzadeh, Z.; Kouhsari, E.; Goudarzi, M.; Heidary, M. Mechanism of Action, Resistance, Synergism, and Clinical Implications of Delamanid Against Multidrug-Resistant Mycobacterium Tuberculosis. Front. Microbiol. 2021, 12, 717045. [Google Scholar] [CrossRef]
- Marrakchi, H.; Lanéelle, M.A.; Daffé, M. Mycolic Acids: Structures, Biosynthesis, and Beyond. Chem. Biol. 2014, 21, 67–85. [Google Scholar] [CrossRef] [PubMed]
- Fish, W.R.; Holz, G.G.; Beach, D.H.; Owen, E.; Anekwe, G.E. The Cyclopropane Fatty Acid of Trypanosomatids. Mol. Biochem. Parasitol. 1981, 3, 103–115. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-Prada, C.; Vincent, I.M.; Brotherton, M.C.; Roberts, M.; Roy, G.; Rivas, L.; Leprohon, P.; Smith, T.K.; Ouellette, M. Different Mutations in a P-Type ATPase Transporter in Leishmania Parasites Are Associated with Cross-Resistance to Two Leading Drugs by Distinct Mechanisms. PLoS Negl. Trop. Dis. 2016, 10, e0005171. [Google Scholar] [CrossRef]
- Xu, W.; Mukherjee, S.; Ning, Y.; Hsu, F.F.; Zhang, K. Cyclopropane Fatty Acid Synthesis Affects Cell Shape and Acid Resistance in Leishmania Mexicana. Int. J. Parasitol. 2018, 48, 245–256. [Google Scholar] [CrossRef] [PubMed]
- Efstathiou, A.; Smirlis, D. Leishmania Protein Kinases: Important Regulators of the Parasite Life Cycle and Molecular Targets for Treating Leishmaniasis. Microorganisms 2021, 9, 691. [Google Scholar] [CrossRef]
- Chhajer, R.; Bhattacharyya, A.; Didwania, N.; Shadab, M.; Das, N.; Palit, P.; Vaidya, T.; Ali, N. Leishmania Donovani Aurora Kinase: A Promising Therapeutic Target against Visceral Leishmaniasis. Biochim. Biophys. Acta Gen. Subj. 2016, 1860, 1973–1988. [Google Scholar] [CrossRef]

| Species/Cell Line | IC 50 (nM) |
|---|---|
| L. infantum | 17.2 ± 0.9 |
| L. major | 21.9 ± 2.8 |
| L. Mexicana | 13.5 ± 0.9 |
| DH82 macrophages | >1.6 × 105 |
| J774 macrophages | >1.6 × 105 |
| Component | % (w/w) |
|---|---|
| Delamanid | 0.0015 |
| PHC | 0.0025 |
| Stearic acid | 0.0152 |
| Ethanol | 3.240 |
| CTAB | 0.0320 |
| Tween 80 | 0.0800 |
| PBS | 96.6290 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Santamaría-Aguirre, J.; Jacho, D.; Méndez, M.A.; Poveda, A.; Carrión, J.; Fanarraga, M.L. Solid Lipid Nanoparticles Enhancing the Leishmanicidal Activity of Delamanid. Pharmaceutics 2024, 16, 41. https://doi.org/10.3390/pharmaceutics16010041
Santamaría-Aguirre J, Jacho D, Méndez MA, Poveda A, Carrión J, Fanarraga ML. Solid Lipid Nanoparticles Enhancing the Leishmanicidal Activity of Delamanid. Pharmaceutics. 2024; 16(1):41. https://doi.org/10.3390/pharmaceutics16010041
Chicago/Turabian StyleSantamaría-Aguirre, Javier, Daniela Jacho, Miguel A. Méndez, Ana Poveda, Javier Carrión, and Mónica L. Fanarraga. 2024. "Solid Lipid Nanoparticles Enhancing the Leishmanicidal Activity of Delamanid" Pharmaceutics 16, no. 1: 41. https://doi.org/10.3390/pharmaceutics16010041
APA StyleSantamaría-Aguirre, J., Jacho, D., Méndez, M. A., Poveda, A., Carrión, J., & Fanarraga, M. L. (2024). Solid Lipid Nanoparticles Enhancing the Leishmanicidal Activity of Delamanid. Pharmaceutics, 16(1), 41. https://doi.org/10.3390/pharmaceutics16010041








