Chronotherapeutics for Solid Tumors
Abstract
1. Introduction
2. Chrono-Pharmacology in Solid Tumor Treatment
3. Chrono-Chemotherapy for Solid Tumor Treatment
4. Chrono-Radiotherapy for Solid Tumor Treatment
5. Additional Chronotherapies for Solid Tumor Treatment
5.1. Hormone Therapy
5.2. Tyrosine Kinase Inhibitors
5.3. Antiangiogenic Therapy
5.4. Immunotherapy
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Silva, S.; Bicker, J.; Falcão, A.; Fortuna, A. Antidepressants and Circadian Rhythm: Exploring Their Bidirectional Interaction for the Treatment of Depression. Pharmaceutics 2021, 13, 1975. [Google Scholar] [CrossRef]
- Quante, M.; Mariani, S.; Weng, J.; Marinac, C.R.; Kaplan, E.R.; Rueschman, M.; Mitchell, J.A.; James, P.; Hipp, J.A.; Cespedes Feliciano, E.M.; et al. Zeitgebers and their Association with Rest-Activity Patterns. Chronobiol. Int. 2019, 36, 203–213. [Google Scholar] [CrossRef]
- Berson, D.M.; Dunn, F.A.; Takao, M. Phototransduction by Retinal Ganglion Cells that Set the Circadian Clock. Science 2002, 295, 1070–1073. [Google Scholar] [CrossRef]
- Do, M.T.H. Melanopsin and the Intrinsically Photosensitive Retinal Ganglion Cells: Biophysics to Behavior. Neuron 2019, 104, 205–226. [Google Scholar] [CrossRef]
- Hankins, M.W.; Peirson, S.N.; Foster, R.G. Melanopsin: An Exciting Photopigment. Trends Neurosci. 2008, 31, 27–36. [Google Scholar] [CrossRef]
- Miyamoto, Y.; Sancar, A. Vitamin B2-Based Blue-Light Photoreceptors in the Retinohypothalamic Tract as the Photoactive Pigments for Setting the Circadian Clock in Mammals. Proc. Natl. Acad. Sci. USA 1998, 95, 6097–6102. [Google Scholar] [CrossRef]
- Walker, W.H., II; Walton, J.C.; DeVries, A.C.; Nelson, R.J. Circadian Rhythm Disruption and Mental Health. Transl. Psychiatry 2020, 10, 28. [Google Scholar] [CrossRef]
- Becker-Krail, D.D.; Walker, W.H., II; Nelson, R.J. The Ventral Tegmental Area and Nucleus Accumbens as Circadian Oscillators: Implications for Drug Abuse and Substance Use Disorders. Front. Physiol. 2022, 13, 886704. [Google Scholar] [CrossRef]
- Ashton, A.; Foster, R.G.; Jagannath, A. Photic Entrainment of the Circadian System. Int. J. Mol. Sci. 2022, 23, 729. [Google Scholar] [CrossRef]
- Guillaumond, F.; Dardente, H.; Giguère, V.; Cermakian, N. Differential control of Bmal1 Circadian Transcription by REV-ERB and ROR Nuclear Receptors. J. Biol. Rhythm. 2005, 20, 391–403. [Google Scholar] [CrossRef]
- Pulido, R.S.; Munji, R.N.; Chan, T.C.; Quirk, C.R.; Weiner, G.A.; Weger, B.D.; Rossi, M.J.; Elmsaouri, S.; Malfavon, M.; Deng, A.; et al. Neuronal Activity Regulates Blood-Brain Barrier Efflux Transport through Endothelial Circadian Genes. Neuron 2020, 108, 937–952.e7. [Google Scholar] [CrossRef]
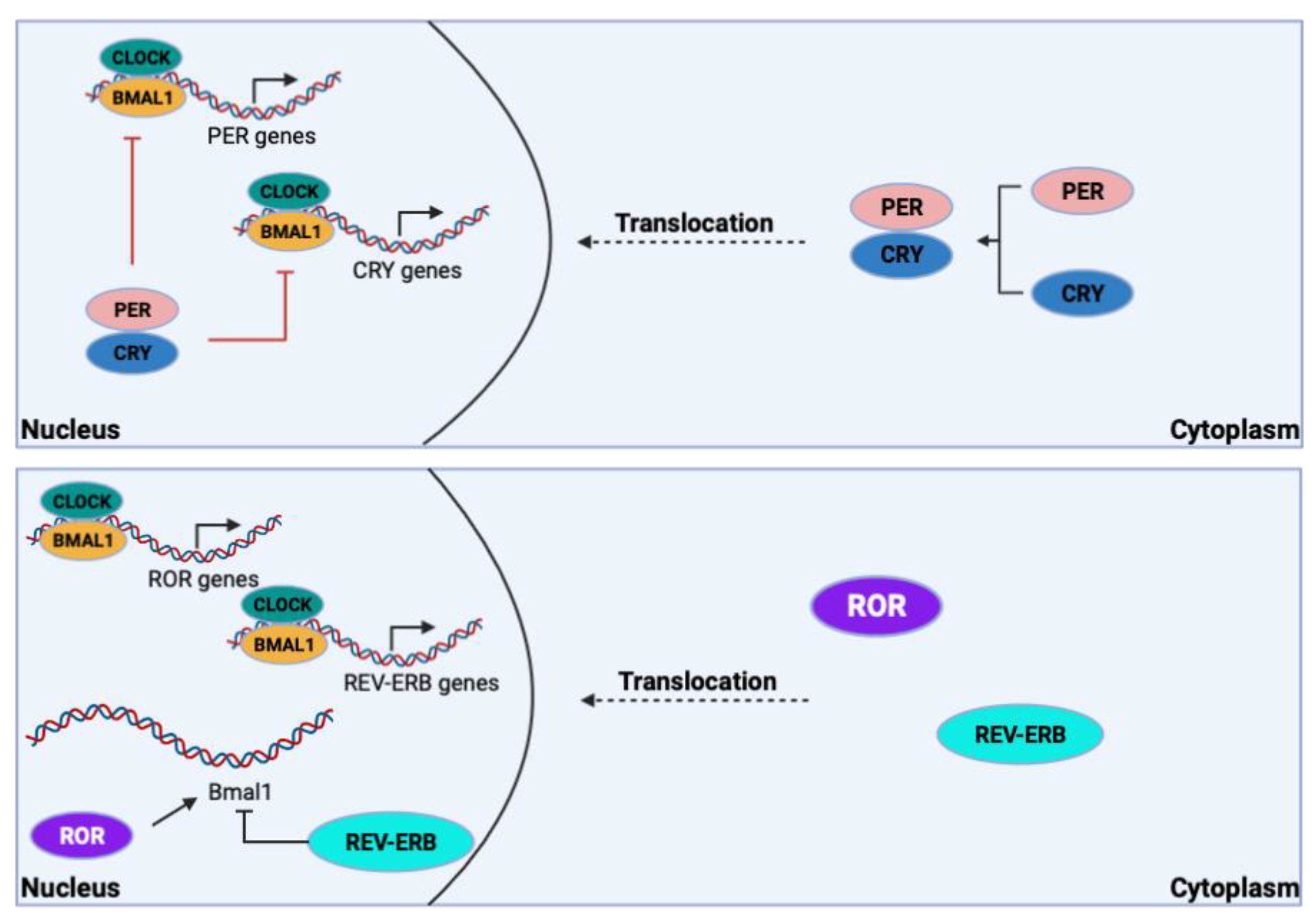
- Partch, C.L.; Green, C.B.; Takahashi, J.S. Molecular Architecture of the Mammalian Circadian Clock. Trends Cell Biol. 2014, 24, 90–99. [Google Scholar] [CrossRef]
- Chen, W.D.; Wen, M.S.; Shie, S.S.; Lo, Y.L.; Wo, H.T.; Wang, C.C.; Hsieh, I.C.; Lee, T.H.; Wang, C.Y. The Circadian Rhythm Controls Telomeres and Telomerase Activity. Biochem. Biophys. Res. Commun. 2014, 451, 408–414. [Google Scholar] [CrossRef]
- Sulli, G.; Lam, M.T.Y.; Panda, S. Interplay between Circadian Clock and Cancer: New Frontiers for Cancer Treatment. Trends Cancer 2019, 5, 475–494. [Google Scholar] [CrossRef]
- Fu, L.; Pelicano, H.; Liu, J.; Huang, P.; Lee, C. The Circadian Gene Period2 Plays an Important Role in Tumor Suppression and DNA Damage Response in vivo. Cell 2002, 111, 41–50. [Google Scholar] [CrossRef]
- Walker, W.H., II; Bumgarner, J.R.; Walton, J.C.; Liu, J.A.; Meléndez-Fernández, O.H.; Nelson, R.J.; DeVries, A.C. Light Pollution and Cancer. Int. J. Mol. Sci. 2020, 21, 9360. [Google Scholar] [CrossRef]
- Kowalska, E.; Ripperger, J.A.; Hoegger, D.C.; Bruegger, P.; Buch, T.; Birchler, T.; Mueller, A.; Albrecht, U.; Contaldo, C.; Brown, S.A. NONO Couples the Circadian Clock to the Cell Cycle. Proc. Natl. Acad. Sci. USA 2013, 110, 1592–1599. [Google Scholar] [CrossRef]
- Gréchez-Cassiau, A.; Rayet, B.; Guillaumond, F.; Teboul, M.; Delaunay, F. The Circadian Clock Component BMAL1 is a Critical Regulator of p21WAF1/CIP1 Expression and Hepatocyte Proliferation. J. Biol. Chem. 2008, 283, 4535–4542. [Google Scholar] [CrossRef]
- Gery, S.; Komatsu, N.; Baldjyan, L.; Yu, A.; Koo, D.; Koeffler, H.P. The Circadian Gene per1 Plays an Important Role in Cell Growth and DNA Damage Control in Human Cancer Cells. Mol. Cell 2006, 22, 375–382. [Google Scholar] [CrossRef]
- Rao, X.; Lin, L. Circadian Clock as a Possible Control Point in Colorectal Cancer Progression (Review). Int. J. Oncol. 2022, 61, 149. [Google Scholar] [CrossRef]
- Vetter, C. Circadian Disruption: What do we Actually Mean? Eur. J. Neurosci. 2020, 51, 531–550. [Google Scholar] [CrossRef]
- Evans, J.A.; Davidson, A.J. Health Consequences of Circadian Disruption in Humans and Animal Models. Prog. Mol. Biol. Transl. Sci. 2013, 119, 283–323. [Google Scholar] [CrossRef]
- Ritonja, J.; Papantoniou, K.; Ebenberger, A.; Wagner, G.; Gartlehner, G.; Klerings, I.; Morgan, R.L.; Herkner, H.; Aronson, K.J.; Schernhammer, E.S. Effects of Exposure to Night Shift Work on Cancer Risk in Workers. Cochrane Database Syst. Rev. 2019, 2019, CD013466. [Google Scholar] [CrossRef]
- Cos, S.; González, A.; Martínez-Campa, C.; Mediavilla, M.D.; Alonso-González, C.; Sánchez-Barceló, E.J. Estrogen-Signaling Pathway: A Link Between Breast Cancer and Melatonin Oncostatic Actions. Cancer Detect. Prev. 2006, 30, 118–128. [Google Scholar] [CrossRef]
- Koritala, B.S.C.; Porter, K.I.; Sarkar, S.; Gaddameedhi, S. Circadian Disruption and Cisplatin Chronotherapy for Mammary Carcinoma. Toxicol. Appl. Pharm. Pharmacol. 2022, 436, 115863. [Google Scholar] [CrossRef]
- Mhatre, M.C.; Shah, P.N.; Juneja, H.S. Effect of Varying Photoperiods on Mammary Morphology, DNA Synthesis, and Hormone Profile in Female Rats. J. Natl. Cancer Inst. 1984, 72, 1411–1416. [Google Scholar]
- Wu, J.; Dauchy, R.T.; Tirrell, P.C.; Wu, S.S.; Lynch, D.T.; Jitawatanarat, P.; Burrington, C.M.; Dauchy, E.M.; Blask, D.E.; Greene, M.W. Light at Night Activates IGF-1R/PDK1 Signaling and Accelerates Tumor Growth in Human Breast Cancer Xenografts. Cancer Res. 2011, 71, 2622–2631. [Google Scholar] [CrossRef]
- Van Dycke, K.C.; Rodenburg, W.; van Oostrom, C.T.; van Kerkhof, L.W.; Pennings, J.L.; Roenneberg, T.; van Steeg, H.; van der Horst, G.T. Chronically Alternating Light Cycles Increase Breast Cancer Risk in Mice. Curr. Biol. 2015, 25, 1932–1937. [Google Scholar] [CrossRef]
- Haus, E.; Halberg, F.; Pauly, J.E.; Cardoso, S.; Kühl, J.F.; Sothern, R.B.; Shiotsuka, R.N.; Hwang, D.S. Increased Tolerance of Leukemic Mice to Arabinosyl Cytosine with Schedule Adjusted to Circadian System. Science 1972, 177, 80–82. [Google Scholar] [CrossRef]
- Amiama-Roig, A.; Verdugo-Sivianes, E.M.; Carnero, A.; Blanco, J.R. Chronotherapy: Circadian Rhythms and Their Influence in Cancer Therapy. Cancers 2022, 14, 5071. [Google Scholar] [CrossRef]
- Beltran-Bless, A.A.; Vandermeer, L.; Ibrahim, M.F.K.; Hutton, B.; Shorr, R.; Savard, M.F.; Clemons, M. Does the Time of Day at Which Endocrine Therapy Is Taken Affect Breast Cancer Patient Outcomes? Curr. Oncol. 2021, 28, 2523–2528. [Google Scholar] [CrossRef] [PubMed]
- Ozturk, N.; Ozturk, D.; Kavakli, I.H.; Okyar, A. Molecular Aspects of Circadian Pharmacology and Relevance for Cancer Chronotherapy. Int. J. Mol. Sci. 2017, 18, 2168. [Google Scholar] [CrossRef] [PubMed]
- Li, X.M.; Tanaka, K.; Sun, J.; Filipski, E.; Kayitalire, L.; Focan, C.; Lévi, F. Preclinical Relevance of Dosing Time for the Therapeutic Index of Gemcitabine-Cisplatin. Br. J. Cancer 2005, 92, 1684–1689. [Google Scholar] [CrossRef] [PubMed]
- Granda, T.G.; Filipski, E.; D’Attino, R.M.; Vrignaud, P.; Anjo, A.; Bissery, M.C.; Lévi, F. Experimental Chronotherapy of Mouse Mammary Adenocarcinoma MA13/C with Docetaxel and Doxorubicin as Single Agents and in Combination. Cancer Res. 2001, 61, 1996–2001. [Google Scholar]
- Gachon, F. Physiological Function of PARbZip Circadian Clock-Controlled Transcription Factors. Ann. Med. 2007, 39, 562–571. [Google Scholar] [CrossRef] [PubMed]
- Gachon, F.; Olela, F.F.; Schaad, O.; Descombes, P.; Schibler, U. The Circadian PAR-Domain Basic Leucine Zipper Transcription Factors DBP, TEF, and HLF Modulate Basal and Inducible Xenobiotic Detoxification. Cell Metab. 2006, 4, 25–36. [Google Scholar] [CrossRef]
- Kriebs, A.; Jordan, S.D.; Soto, E.; Henriksson, E.; Sandate, C.R.; Vaughan, M.E.; Chan, A.B.; Duglan, D.; Papp, S.J.; Huber, A.L.; et al. Circadian Repressors CRY1 and CRY2 Broadly Interact with Nuclear Receptors and Modulate Transcriptional Activity. Proc. Natl. Acad. Sci. USA 2017, 114, 8776–8781. [Google Scholar] [CrossRef]
- Gorbacheva, V.Y.; Kondratov, R.V.; Zhang, R.; Cherukuri, S.; Gudkov, A.V.; Takahashi, J.S.; Antoch, M.P. Circadian Sensitivity to the Chemotherapeutic Agent Cyclophosphamide Depends on the Functional Status of the CLOCK/BMAL1 Transactivation Complex. Proc. Natl. Acad. Sci. USA 2005, 102, 3407–3412. [Google Scholar] [CrossRef]
- Murakami, Y.; Higashi, Y.; Matsunaga, N.; Koyanagi, S.; Ohdo, S. Circadian Clock-Controlled Intestinal Expression of the Multidrug-Resistance Gene mdr1a in Mice. Gastroenterology 2008, 135, 1636–1644.e3. [Google Scholar] [CrossRef]
- Lévi, F.; Okyar, A.; Dulong, S.; Innominato, P.F.; Clairambault, J. Circadian Timing in Cancer Treatments. Annu. Rev. Pharm. Pharmacol. Toxicol. 2010, 50, 377–421. [Google Scholar] [CrossRef]
- Wilson, B.E.; Jacob, S.; Yap, M.L.; Ferlay, J.; Bray, F.; Barton, M.B. Estimates of Global Chemotherapy Demands and Corresponding Physician Workforce Requirements for 2018 and 2040: A Population-Based Study. Lancet Oncol. 2019, 20, 769–780. [Google Scholar] [CrossRef]
- Walton, J.C.; Walker, W.H., II; Bumgarner, J.R.; Meléndez-Fernández, O.H.; Liu, J.A.; Hughes, H.L.; Kaper, A.L.; Nelson, R.J. Circadian Variation in Efficacy of Medications. Clin. Pharm. Pharmacol. Ther. 2021, 109, 1457–1488. [Google Scholar] [CrossRef] [PubMed]
- Amjad, M.T.; Chidharla, A.; Kasi, A. Cancer Chemotherapy. In StatPearls; StatPearls Publishing LLC.: Treasure Island, FL, USA, 2023. [Google Scholar]
- Rosenthal, P.J. Clinical Pharmacology of the Antihelminthic Drugs. In Basic. & Clinical Pharmacology, 12th ed.; Bertram, G., Katzung, M., Eds.; The McGraw-Hill Companies: New York City, NY, USA, 2012; pp. 937–948. [Google Scholar]
- van den Boogaard, W.M.C.; Komninos, D.S.J.; Vermeij, W.P. Chemotherapy Side-Effects: Not All DNA Damage Is Equal. Cancers 2022, 14, 627. [Google Scholar] [CrossRef] [PubMed]
- Petković, M.; Henis, M.; Heese, O.; Relógio, A. Chronotherapy in Glioblastoma: State of the Art and Future Perspectives. EBioMedicine 2023, 89, 104470. [Google Scholar] [CrossRef]
- Kang, T.H.; Sancar, A. Circadian Regulation of DNA Excision Repair: Implications for Chrono-Chemotherapy. Cell Cycle 2009, 8, 1665–1667. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, M.; Wood, P.A.; Hrushesky, W.J. Circadian Chemotherapy for Gynecological and Genitourinary Cancers. Chronobiol. Int. 2002, 19, 237–251. [Google Scholar] [CrossRef]
- Roosendaal, J.; Jacobs, B.A.W.; Pluim, D.; Rosing, H.; de Vries, N.; van Werkhoven, E.; Nuijen, B.; Beijnen, J.H.; Huitema, A.D.R.; Schellens, J.H.M.; et al. Phase I Pharmacological Study of Continuous Chronomodulated Capecitabine Treatment. Pharm. Res. 2020, 37, 89. [Google Scholar] [CrossRef]
- Gou, X.X.; Jin, F.; Wu, W.L.; Long, J.H.; Li, Y.Y.; Gong, X.Y.; Chen, G.Y.; Chen, X.X.; Liu, L.N. Induction Chronomodulated Chemotherapy Plus Radiotherapy for Nasopharyngeal Carcinoma: A Phase II Prospective Randomized Study. J. Cancer Res. Ther. 2018, 14, 1613–1619. [Google Scholar] [CrossRef]
- Lin, H.X.; Hua, Y.J.; Chen, Q.Y.; Luo, D.H.; Sun, R.; Qiu, F.; Mo, H.Y.; Mai, H.Q.; Guo, X.; Xian, L.J.; et al. Randomized Study of Sinusoidal Chronomodulated Versus Flat Intermittent Induction Chemotherapy with Cisplatin and 5-fluorouracil Followed by Traditional Radiotherapy for Locoregionally Advanced Nasopharyngeal Carcinoma. Chin. J. Cancer 2013, 32, 502–511. [Google Scholar] [CrossRef]
- Lévi, F. Circadian Chronotherapy for Human Cancers. Lancet Oncol. 2001, 2, 307–315. [Google Scholar] [CrossRef]
- Hrushesky, W.J. Circadian Timing of Cancer Chemotherapy. Science 1985, 228, 73–75. [Google Scholar] [CrossRef]
- Li, J.; Chen, R.; Ji, M.; Zou, S.L.; Zhu, L.N. Cisplatin-Based Chronotherapy for Advanced Non-Small Cell Lung Cancer Patients: A Randomized Controlled Study and its Pharmacokinetics Analysis. Cancer Chemother. Pharm. Pharmacol. 2015, 76, 651–655. [Google Scholar] [CrossRef] [PubMed]
- von Roemeling, R.; Hrushesky, W.J. Circadian Patterning of Continuous Floxuridine Infusion Reduces Toxicity and Allows Higher Dose Intensity in Patients with Widespread Cancer. J. Clin. Oncol. 1989, 7, 1710–1719. [Google Scholar] [CrossRef] [PubMed]
- Printezi, M.I.; Kilgallen, A.B.; Bond, M.J.G.; Štibler, U.; Putker, M.; Teske, A.J.; Cramer, M.J.; Punt, C.J.A.; Sluijter, J.P.G.; Huitema, A.D.R.; et al. Toxicity and Efficacy of Chronomodulated Chemotherapy: A Systematic Review. Lancet Oncol. 2022, 23, e129–e143. [Google Scholar] [CrossRef]
- Walker, W.H., II; Sprowls, S.A.; Bumgarner, J.R.; Liu, J.A.; Meléndez-Fernández, O.H.; Walton, J.C.; Lockman, P.R.; DeVries, A.C.; Nelson, R.J. Circadian Influences on Chemotherapy Efficacy in a Mouse Model of Brain Metastases of Breast Cancer. Front. Oncol. 2021, 11, 752331. [Google Scholar] [CrossRef]
- Mormont, M.C.; Levi, F. Cancer Chronotherapy: Principles, Applications, and Perspectives. Cancer 2003, 97, 155–169. [Google Scholar] [CrossRef] [PubMed]
- Pence, S.T.; Chesnut, G.T.; Shafi, A.A. Time Matters: Importance of Circadian Rhythms, Disruption, and Chronotherapy in Urologic Malignancies. Urology 2023, 175, 6–12. [Google Scholar] [CrossRef] [PubMed]
- Damato, A.R.; Luo, J.; Katumba, R.G.N.; Talcott, G.R.; Rubin, J.B.; Herzog, E.D.; Campian, J.L. Temozolomide Chronotherapy in Patients with Glioblastoma: A Retrospective Single-Institute Study. Neuro-Oncol. Adv. 2021, 3, vdab041. [Google Scholar] [CrossRef]
- Hu, J.; Fu, S.; Peng, Q.; Han, Y.; Xie, J.; Zan, N.; Chen, Y.; Fan, J. Paclitaxel-Loaded Polymeric Nanoparticles Combined with Chronomodulated Chemotherapy on Lung Cancer: In vitro and in vivo Evaluation. Int. J. Pharm. 2017, 516, 313–322. [Google Scholar] [CrossRef]
- Nong, J.; Glassman, P.M.; Myerson, J.W.; Zuluaga-Ramirez, V.; Rodriguez-Garcia, A.; Mukalel, A.; Omo-Lamai, S.; Walsh, L.R.; Zamora, M.E.; Gong, X.; et al. Targeted Nanocarriers Co-Opting Pulmonary Intravascular Leukocytes for Drug Delivery to the Injured Brain. ACS Nano 2023, 17, 13121–13136. [Google Scholar] [CrossRef]
- Moreira, A.; Bernardo, C.; Ramos, C.; Aguiar, P.; Alves da Costa, F. National Trends in the Use of Oral Chemotherapy Over 13 Years. Front. Pharm. Pharmacol. 2022, 13, 909948. [Google Scholar] [CrossRef]
- Abu-Samak, A.-A.; Abu-Samak, M.; Al-Waeli, H.; Cai, W.; Al-Tamimi, M.; Tamimi, F.; Nicolau, B. Chronotherapy in Head and Neck Cancer (HNC): A Systematic Review. J. Clin. Oncol. 2023, 41, e18016. [Google Scholar] [CrossRef]
- Bermúdez-Guzmán, L.; Blanco-Saborío, A.; Ramírez-Zamora, J.; Lovo, E. The Time for Chronotherapy in Radiation Oncology. Front. Oncol. 2021, 11, 687672. [Google Scholar] [CrossRef] [PubMed]
- Sapienza, L.G.; Nasra, K.; Berry, R.; Danesh, L.; Little, T.; Abu-Isa, E. Clinical Effects of Morning and Afternoon Radiotherapy on High-Grade Gliomas. Chronobiol. Int. 2021, 38, 732–741. [Google Scholar] [CrossRef]
- Squire, T.; Buchanan, G.; Rangiah, D.; Davis, I.; Yip, D.; Chua, Y.J.; Rich, T.; Elsaleh, H. Does Chronomodulated Radiotherapy Improve Pathological Response in Locally Advanced Rectal Cancer? Chronobiol. Int. 2017, 34, 492–503. [Google Scholar] [CrossRef] [PubMed]
- Butti, R.; Das, S.; Gunasekaran, V.P.; Yadav, A.S.; Kumar, D.; Kundu, G.C. Receptor Tyrosine Kinases (RTKs) in Breast Cancer: Signaling, Therapeutic Implications and Challenges. Mol. Cancer 2018, 17, 34. [Google Scholar] [CrossRef] [PubMed]
- Szałek, E.; Karbownik, A.; Sobańska, K.; Połom, W.; Grabowski, T.; Wolc, A.; Matuszewski, M.; Grześkowiak, E. The Influence of the Time-of-Day Administration of the Drug on the Pharmacokinetics of Sunitinib in Rabbits. Eur. Rev. Med. Pharm. Pharmacol. Sci. 2014, 18, 2393–2399. [Google Scholar]
- Escudier, B.; Roigas, J.; Gillessen, S.; Harmenberg, U.; Srinivas, S.; Mulder, S.F.; Fountzilas, G.; Peschel, C.; Flodgren, P.; Maneval, E.C.; et al. Phase II Study of Sunitinib Administered in a Continuous Once-Daily Dosing Regimen in Patients with Cytokine-Refractory Metastatic Renal Cell Carcinoma. J. Clin. Oncol. 2009, 27, 4068–4075. [Google Scholar] [CrossRef]
- George, S.; Blay, J.Y.; Casali, P.G.; Le Cesne, A.; Stephenson, P.; Deprimo, S.E.; Harmon, C.S.; Law, C.N.; Morgan, J.A.; Ray-Coquard, I.; et al. Clinical Evaluation of Continuous Daily Dosing of Sunitinib Malate in Patients with Advanced Gastrointestinal Stromal Tumour after Imatinib Failure. Eur. J. Cancer 2009, 45, 1959–1968. [Google Scholar] [CrossRef]
- Nishida, N.; Yano, H.; Nishida, T.; Kamura, T.; Kojiro, M. Angiogenesis in Cancer. Vasc. Health Risk Manag. 2006, 2, 213–219. [Google Scholar] [CrossRef]
- Koyanagi, S.; Nakagawa, H.; Kuramoto, Y.; Ohdo, S.; Soeda, S.; Shimeno, H. Optimizing the Dosing Schedule of TNP-470 [O-(chloroacetyl-carbamoyl) fumagillol] Enhances its Antitumor and Antiangiogenic Efficacies. J. Pharm. Pharmacol. Exp. Ther. 2003, 304, 669–674. [Google Scholar] [CrossRef] [PubMed]
- Gamaleia, N.F.; Lisnyak, I.A.; Shishko, E.D.; Mamchur, A.A.; Prokopenko, I.V.; Kholin, V.V. Chronobiological Approaches to Antiangiogenic Photodynamic Therapy of Tumors: The First Experimental Evaluation. Exp. Oncol. 2012, 34, 364–366. [Google Scholar] [PubMed]
- Wang, C.; Barnoud, C.; Cenerenti, M.; Sun, M.; Caffa, I.; Kizil, B.; Bill, R.; Liu, Y.; Pick, R.; Garnier, L.; et al. Dendritic Cells Direct Circadian Anti-Tumour Immune Responses. Nature 2023, 614, 136–143. [Google Scholar] [CrossRef]
- Carlino, M.S.; Larkin, J.; Long, G.V. Immune Checkpoint Inhibitors in Melanoma. Lancet 2021, 398, 1002–1014. [Google Scholar] [CrossRef] [PubMed]
- Druzd, D.; Matveeva, O.; Ince, L.; Harrison, U.; He, W.; Schmal, C.; Herzel, H.; Tsang, A.H.; Kawakami, N.; Leliavski, A.; et al. Lymphocyte Circadian Clocks Control Lymph Node Trafficking and Adaptive Immune Responses. Immunity 2017, 46, 120–132. [Google Scholar] [CrossRef] [PubMed]
- Scheiermann, C.; Gibbs, J.; Ince, L.; Loudon, A. Clocking in to Immunity. Nat. Rev. Immunol. 2018, 18, 423–437. [Google Scholar] [CrossRef]
- Rousseau, A.; Tagliamento, M.; Auclin, E.; Aldea, M.; Frelaut, M.; Levy, A.; Benitez, J.C.; Naltet, C.; Lavaud, P.; Botticella, A.; et al. Clinical Outcomes by Infusion Timing of Immune Checkpoint Inhibitors in Patients with Advanced Non-Small Cell Lung Cancer. Eur. J. Cancer 2023, 182, 107–114. [Google Scholar] [CrossRef]
- Qian, D.C.; Kleber, T.; Brammer, B.; Xu, K.M.; Switchenko, J.M.; Janopaul-Naylor, J.R.; Zhong, J.; Yushak, M.L.; Harvey, R.D.; Paulos, C.M.; et al. Effect of Immunotherapy Time-of-Day Infusion on Overall Survival Among Patients with Advanced Melanoma in the USA (MEMOIR): A Propensity Score-Matched Analysis of a Single-Centre, Longitudinal Study. Lancet Oncol. 2021, 22, 1777–1786. [Google Scholar] [CrossRef]
- Zhang, Z.; Zeng, P.; Gao, W.; Zhou, Q.; Feng, T.; Tian, X. Circadian Clock: A Regulator of the Immunity in Cancer. Cell Commun. Signal. 2021, 19, 37. [Google Scholar] [CrossRef]
- Diamantopoulou, Z.; Gvozdenovic, A.; Aceto, N. A New Time Dimension in the Fight Against Metastasis. Trends Cell Biol. 2023. [Google Scholar] [CrossRef]
- Monje, M.; Borniger, J.C.; D’Silva, N.J.; Deneen, B.; Dirks, P.B.; Fattahi, F.; Frenette, P.S.; Garzia, L.; Gutmann, D.H.; Hanahan, D.; et al. Roadmap for the Emerging Field of Cancer Neuroscience. Cell 2020, 181, 219–222. [Google Scholar] [CrossRef]
- Winkler, F.; Venkatesh, H.S.; Amit, M.; Batchelor, T.; Demir, I.E.; Deneen, B.; Gutmann, D.H.; Hervey-Jumper, S.; Kuner, T.; Mabbott, D.; et al. Cancer Neuroscience: State of the Field, Emerging Directions. Cell 2023, 186, 1689–1707. [Google Scholar] [CrossRef] [PubMed]
- Innominato, P.F.; Lévi, F.A.; Bjarnason, G.A. Chronotherapy and the Molecular Clock: Clinical Implications in Oncology. Adv. Drug Deliv. Rev. 2010, 62, 979–1001. [Google Scholar] [CrossRef] [PubMed]
- Nelson, R.J.; Bumgarner, J.R.; Liu, J.A.; Love, J.A.; Meléndez-Fernández, O.H.; Becker-Krail, D.D.; Walker, W.H., II; Walton, J.C.; DeVries, A.C.; Prendergast, B.J. Time of Day as a Critical Variable in Biology. BMC Biol. 2022, 20, 142–157. [Google Scholar] [CrossRef] [PubMed]

| Tumor Type | Species | Treatment | Results | |
|---|---|---|---|---|
| Chrono-Chemotherapy | Brain metastases of breast cancer [57] | Mice | 13 mg/kg of paclitaxel at ZT0 or ZT17 | Mice treated at ZT17 demonstrated a significant delay of neurological symptoms compared to those treated at ZT0 |
| Ovarian Cancer [53] | Human | 60 mg/m2 of Adriamycin from 0600–0630 h and 60 mg/m2 cisplatin from 1800–1830 h (schedule A) or vise versa (schedule B) | Patients on schedule B required more dose reductions and experienced more complications (i.e., infections and bleeding) | |
| Various solid tumors [49] | Human | Capecitabine every day with administration of 750 mg/m2 at 0900 h and 1250 mg/m2 at 2400 h | Maximum tolerated dose was 20% higher than that of the current approved regimen (1250 mg/m2 bi-daily) | |
| Chrono-Radiotherapy | Nasopharyngeal carcinoma [50] | Human | 80 mg/m2 of cisplatin from 1000–2200 h; 1000 mg/m2 of 5-FU and 200 mg/m2 of citrovorum factor from 2200–1000 h for 3 days | Chronomodulation of treatment significantly reduced leukocytopenia, thrombocytopenia, and nausea/vomiting when compared to constant administration |
| Nasopharyngeal carcinoma [51] | Human | DDP administration from 1000–2200 h; 5-FU administration from 2200–1000 h | Significant decrease in stomatitis during radiotherapy compared to constant administration | |
| Leukemia [29] | Mouse | 240 mg/kg of Ara-C with higher doses earlier on that the standard regimen | Increased tolerance and survival | |
| Glasgow osteosarcoma [33] | Mouse | 200 mg/kg of gemcitabine at HALO 11 or 23; 5 mg/kg of cisplatin 1 min or 4 h after gemcitabine | Decreased neutropenia and weight loss when gemcitabine given at HALO 11 regardless of cisplatin administration time | |
| Advanced non-small cell lung cancer [54] | Human | 75 mg/m2 of docetaxel on day 1; 20 mg/m2 of cisplatin on days 1–4 at either 0600 h or 1800 h; 1000 mg/m2 of gemcitabine on days 1 and 8 | Significantly reduced nausea and neutropenia with cisplatin administration at 1800 h | |
| Various metastases [55] | Human | Constant administration of FUDR with maximal flow rate in the late afternoon and minimal flow rate in the early morning | Patients receiving chronomodulated treatment experienced less severe gastrointestinal side effects and higher drug tolerance | |
| Triple negative mammary carcinoma [25] | Mouse | 5 mg/kg of cisplatin at ZT10 or ZT22 | Treatment at ZT22 reduced tumor growth, but this effect was negated by phase shift (jet lag) | |
| Glioblastoma [60] | Human | Temozolomide in the morning or evening | Patients taking Temozolomide in the morning had a higher rate of overall survival at ~5 years post-treatment | |
| Lung cancer [61] | Mouse | Novel nanoparticle-conjugated paclitaxel | Nanoparticle delivery resulted in significantly higher anti-tumor efficacy at HALO 15 than paclitaxel alone | |
| Mixed; 80% glioblastoma [66] | Human | Radiotherapy in the morning or evening | Time of day had no effect on toxicity, progression-free survival, or overall survival | |
| Rectal cancer [67] | Human | Radiotherapy in the morning or evening | Patients receiving treatment after 1200 h the majority of the time were significantly more likely to respond to treatment | |
| Naïve [69] | Rabbit | 25 mg of Sunitinib at 0800 h or 2000 h | Pharmacokinetics of the drug were significantly enhanced at 2000 h | |
| Metastatic renal cell carcinoma [70] | Human | 37.5 mg/day of sunitinib in the morning or evening | Time of day had no significant effect on efficacy, tolerance, or quality of life | |
| Imatinib-resistant/intolerant Gastrointestinal stromal tumor [71] | Human | 37.5 mg/day of sunitinib in the morning or evening | Time of day had no significant effect on efficacy or adverse events | |
| Additional Chronotherapies | Lewis lung carcinoma and sarcoma 180 [74] | Mouse | Photodynamic therapy (laser irradiation) at 0200 h or 1400 h | Tumor growth was significantly inhibited when treated during the day rather than at night |
| Melanoma [75] | Mouse | Anti-tumor vaccine at ZT9 or ZT21 | Tumor volume was significantly smaller following treatment in mice vaccinated at ZT9 rather than ZT21 | |
| Non-small cell lung cancer [79] | Human | Single-agent anti-PD-1 before or after 1630 h | Patients receiving treatment after 1630 h at least 20% of the time had a significantly shorter progression-free survival than those receiving treatment after 1630 h less than 20% of the time | |
| Stage IV melanoma [80] | Human | Ipilimumab, nivolumab, pembrolizumab, or any combo of these before or after 1630 h | Patients receiving treatment after 1630 h at least 20% of the time had a significantly shorter overall survival than those receiving treatment after 1630 h less than 20% of the time |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kisamore, C.O.; Elliott, B.D.; DeVries, A.C.; Nelson, R.J.; Walker, W.H., II. Chronotherapeutics for Solid Tumors. Pharmaceutics 2023, 15, 2023. https://doi.org/10.3390/pharmaceutics15082023
Kisamore CO, Elliott BD, DeVries AC, Nelson RJ, Walker WH II. Chronotherapeutics for Solid Tumors. Pharmaceutics. 2023; 15(8):2023. https://doi.org/10.3390/pharmaceutics15082023
Chicago/Turabian StyleKisamore, Claire O., Brittany D. Elliott, A. Courtney DeVries, Randy J. Nelson, and William H. Walker, II. 2023. "Chronotherapeutics for Solid Tumors" Pharmaceutics 15, no. 8: 2023. https://doi.org/10.3390/pharmaceutics15082023
APA StyleKisamore, C. O., Elliott, B. D., DeVries, A. C., Nelson, R. J., & Walker, W. H., II. (2023). Chronotherapeutics for Solid Tumors. Pharmaceutics, 15(8), 2023. https://doi.org/10.3390/pharmaceutics15082023








