Synthesis, Characterization, and In Vitro Cytotoxicity Evaluation of Doxorubicin-Loaded Magnetite Nanoparticles on Triple-Negative Breast Cancer Cell Lines
Abstract
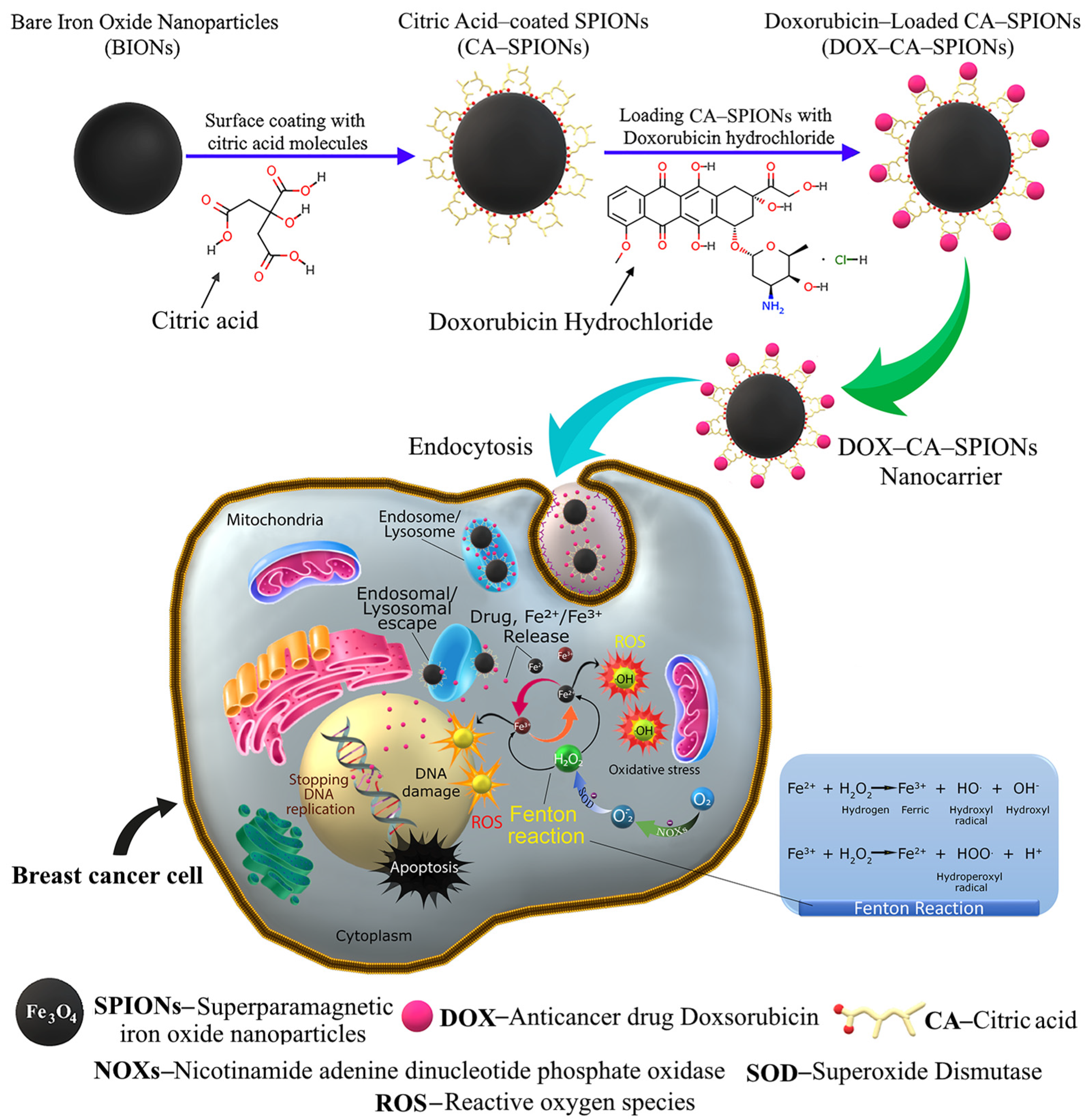
1. Introduction
2. Materials and Methods
2.1. Reagents
2.2. Synthesis of Magnetic Nanoparticles
2.3. Samples’ Preparation for Doxorubicin Loading Study
2.4. Stability of Doxorubicin-Loaded Magnetic Nanocarriers in DW and Sodium Chloride
2.5. Cell Lines
2.6. Cell Cultures
2.7. MTT Assay
2.8. Materials’ Characterization
3. Results and Discussion
3.1. ELS and DLS Results
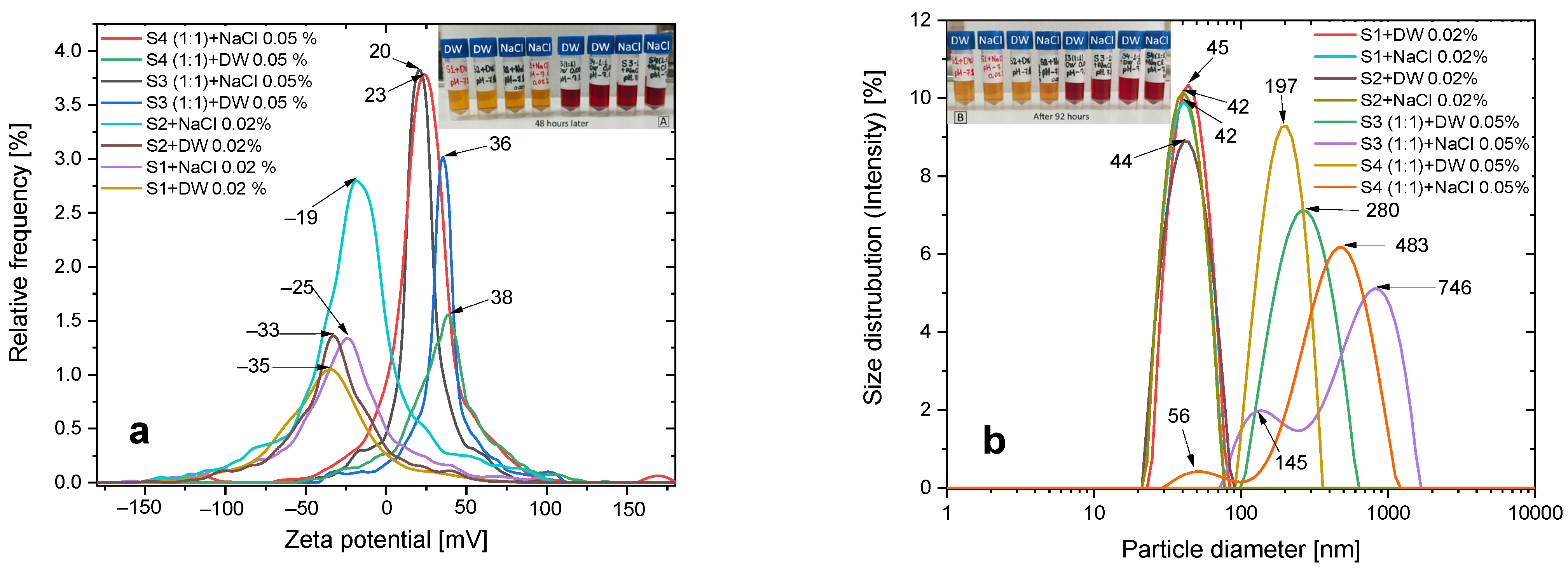
3.2. Colloidal Stability
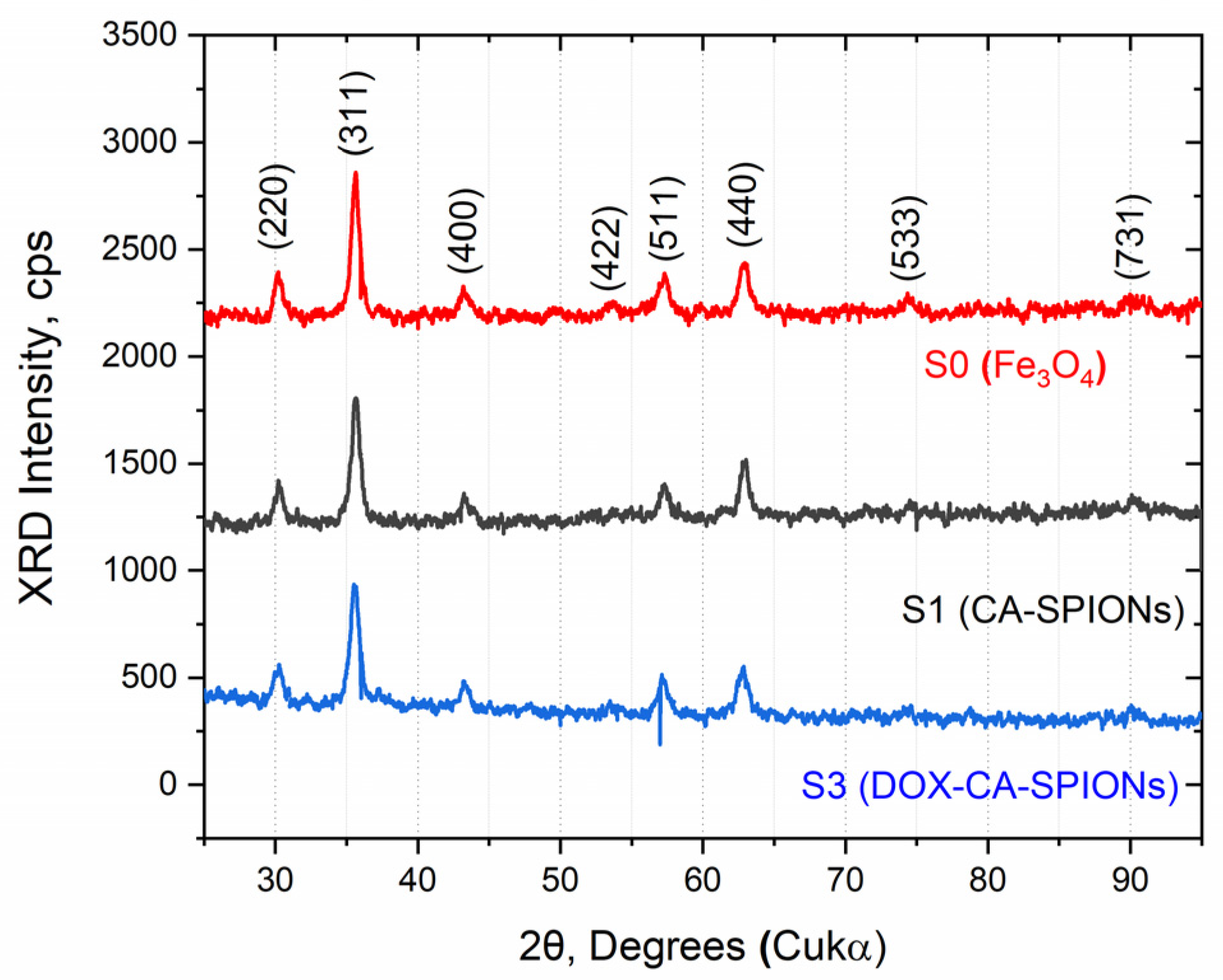
3.3. XRD
3.4. Morphology and Particle Size
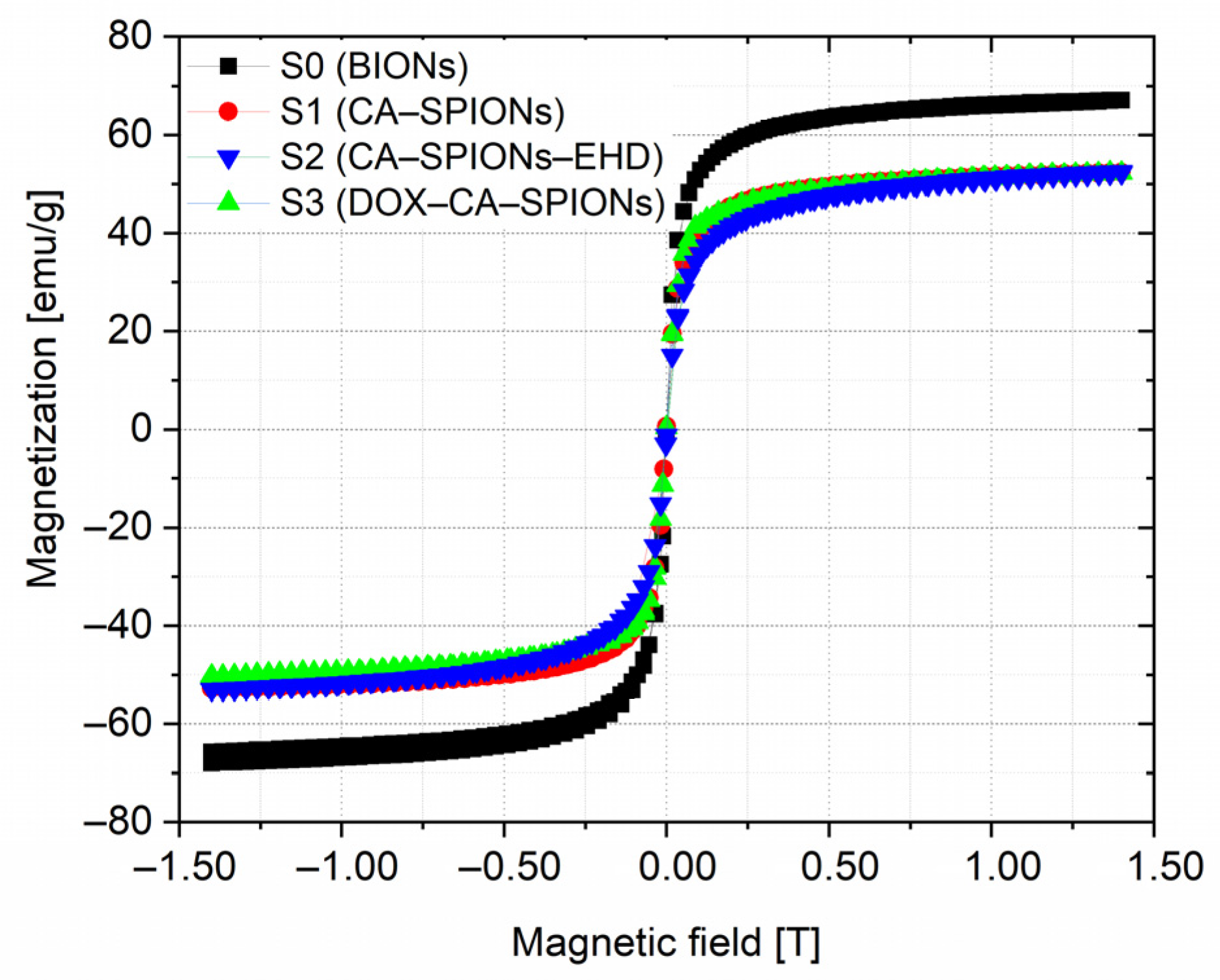
3.5. Magnetization
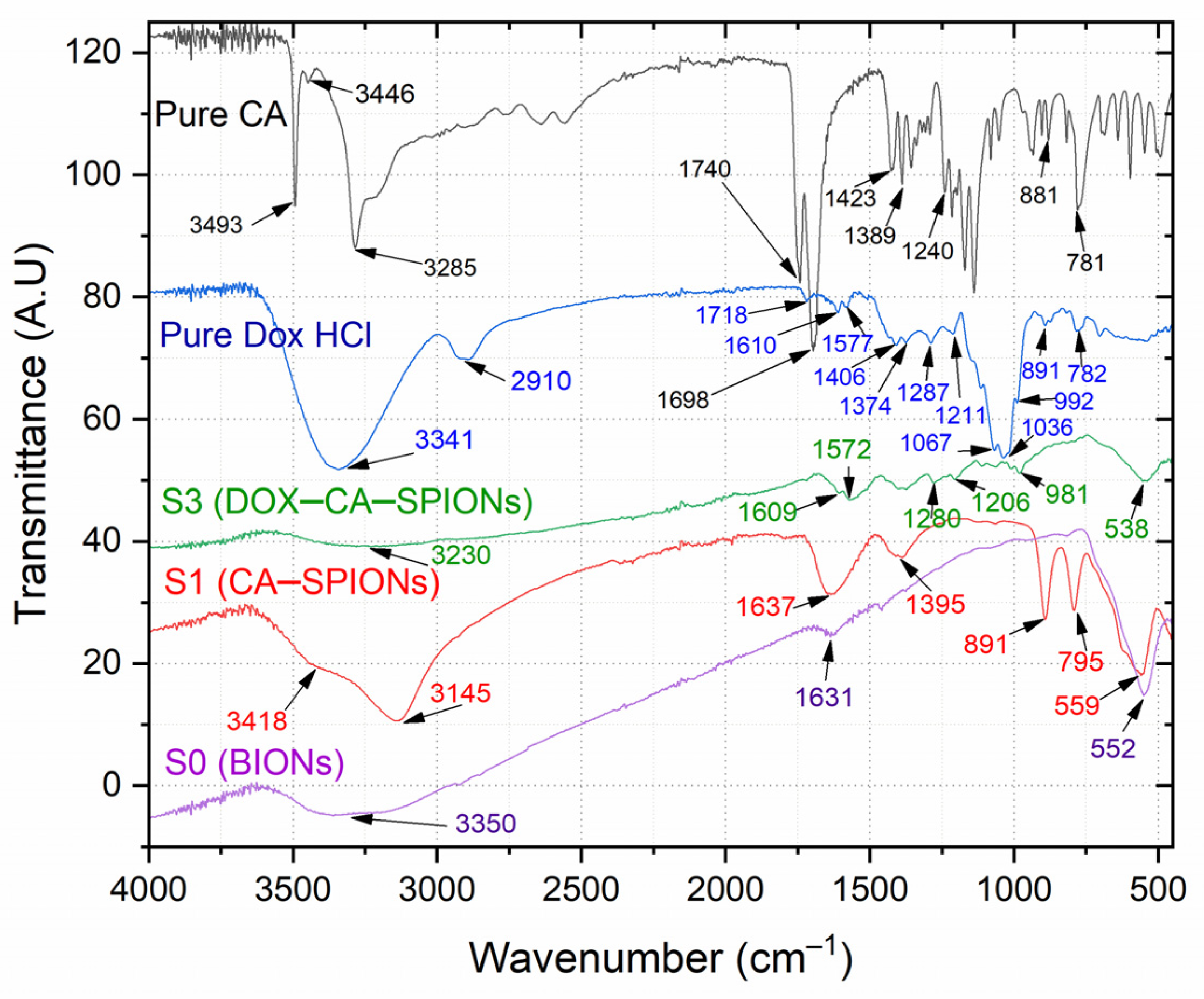
3.6. FTIR Analysis
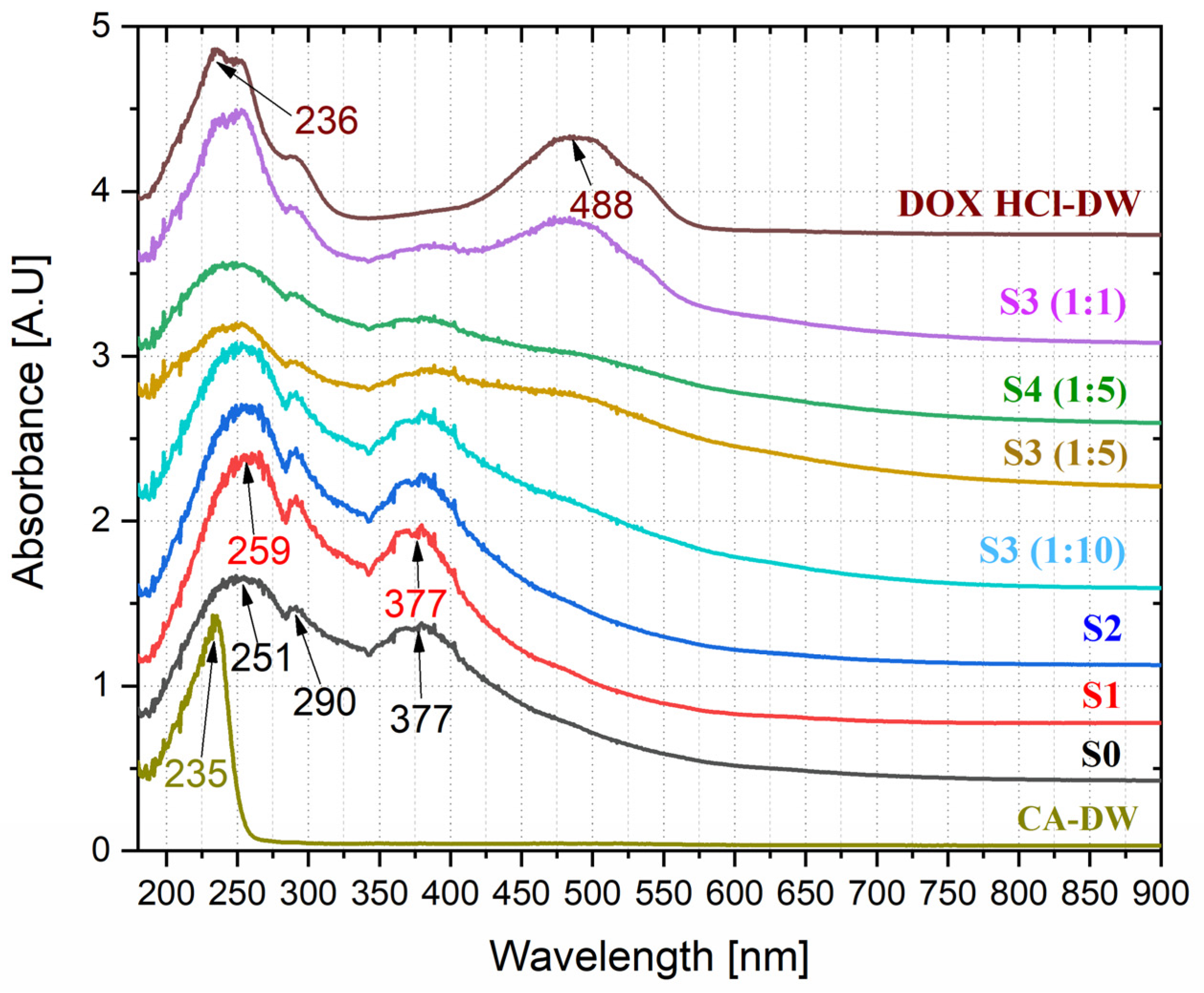
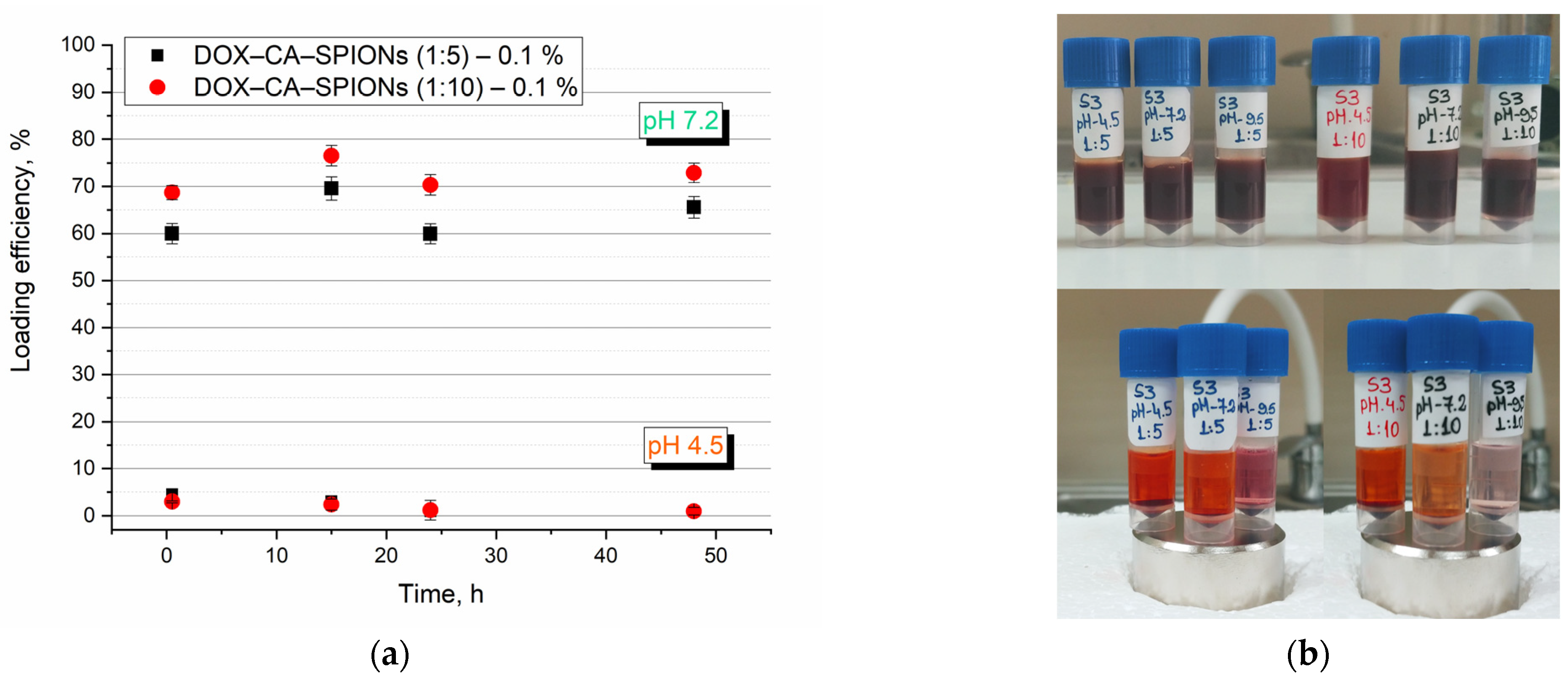
3.7. UV-Vis Optical Studies of Anticancer Drug Loading
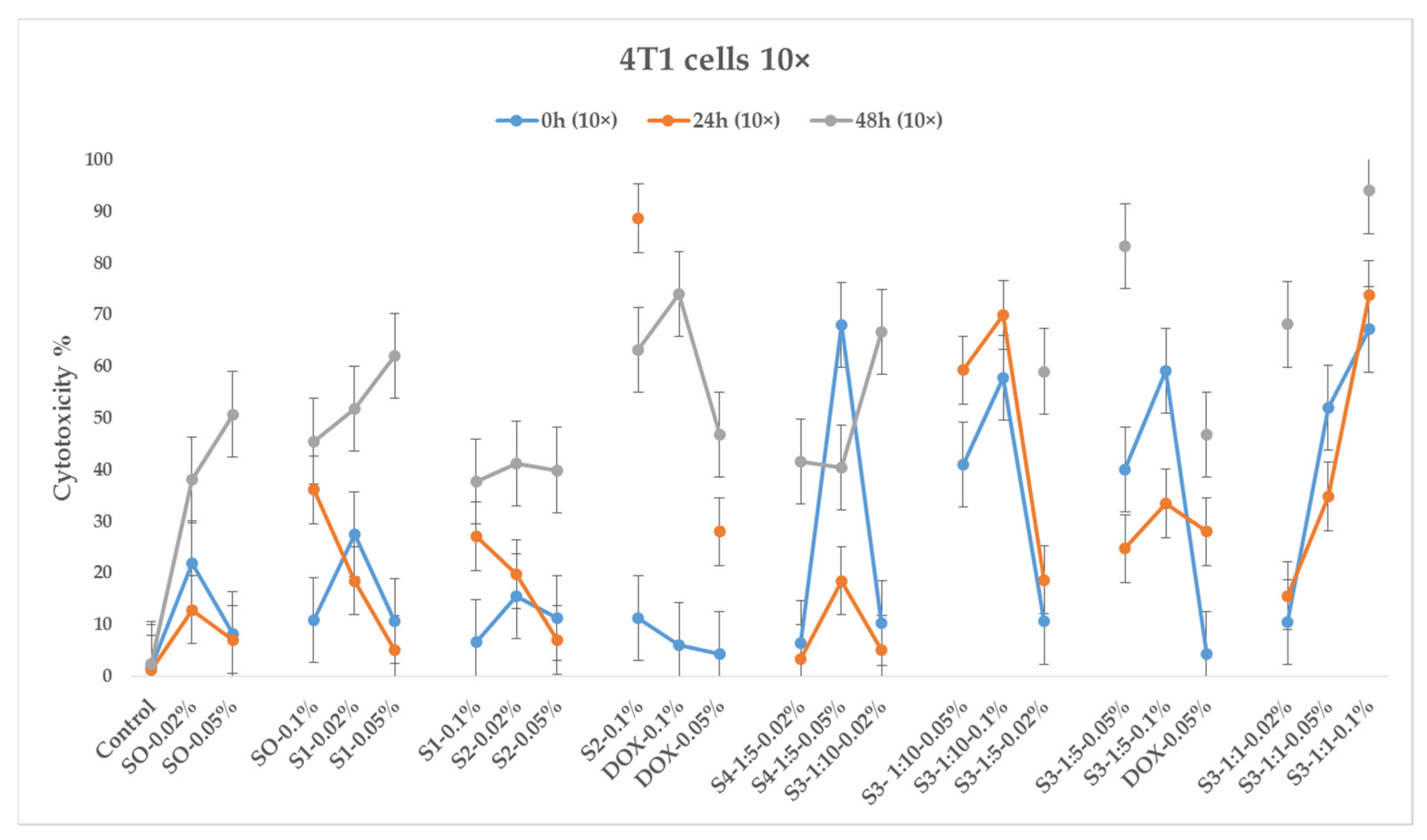
3.8. In Vitro Cytotoxicity
3.8.1. Sample Preparation
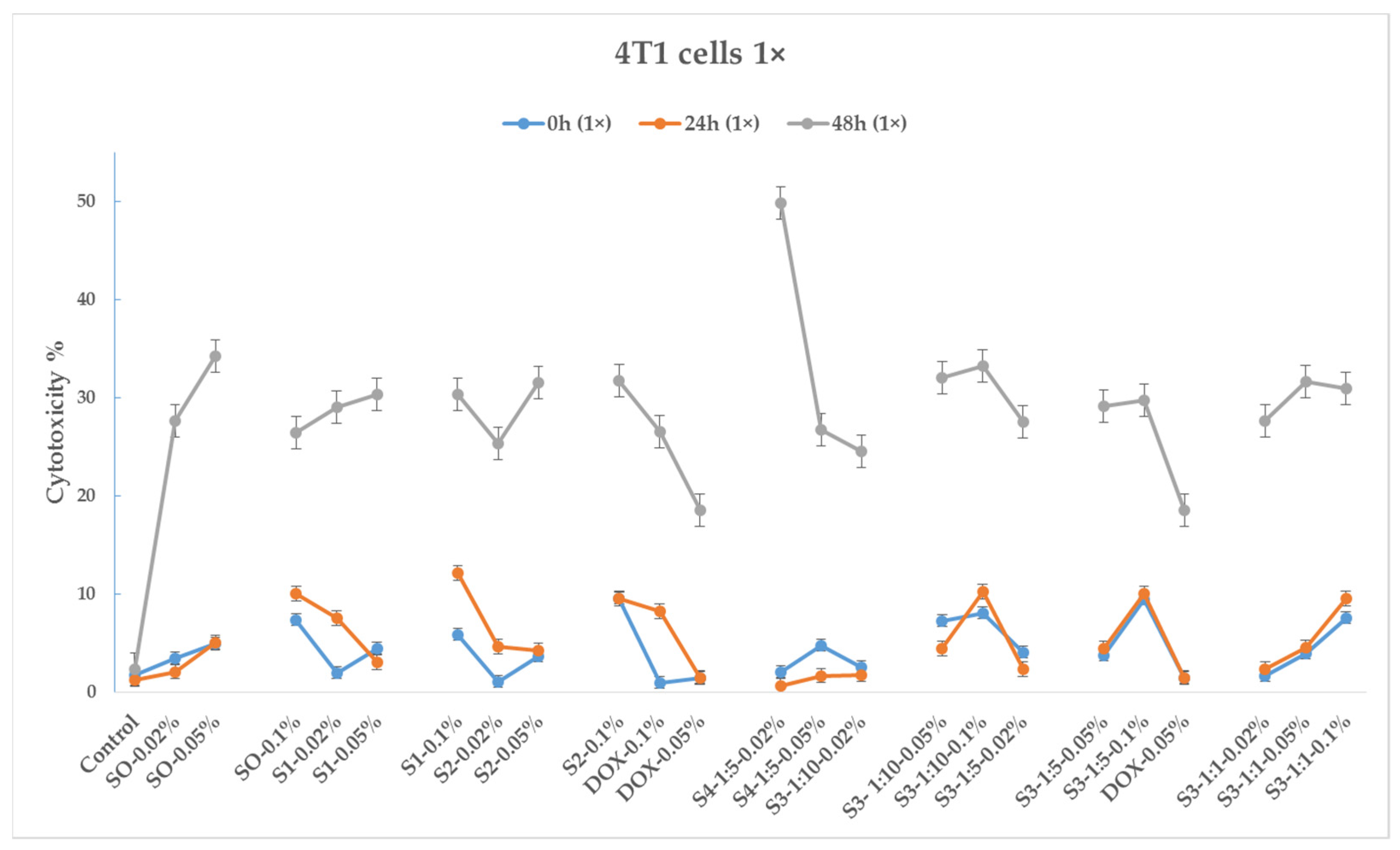
3.8.2. 4T1 Cancer Cell Line
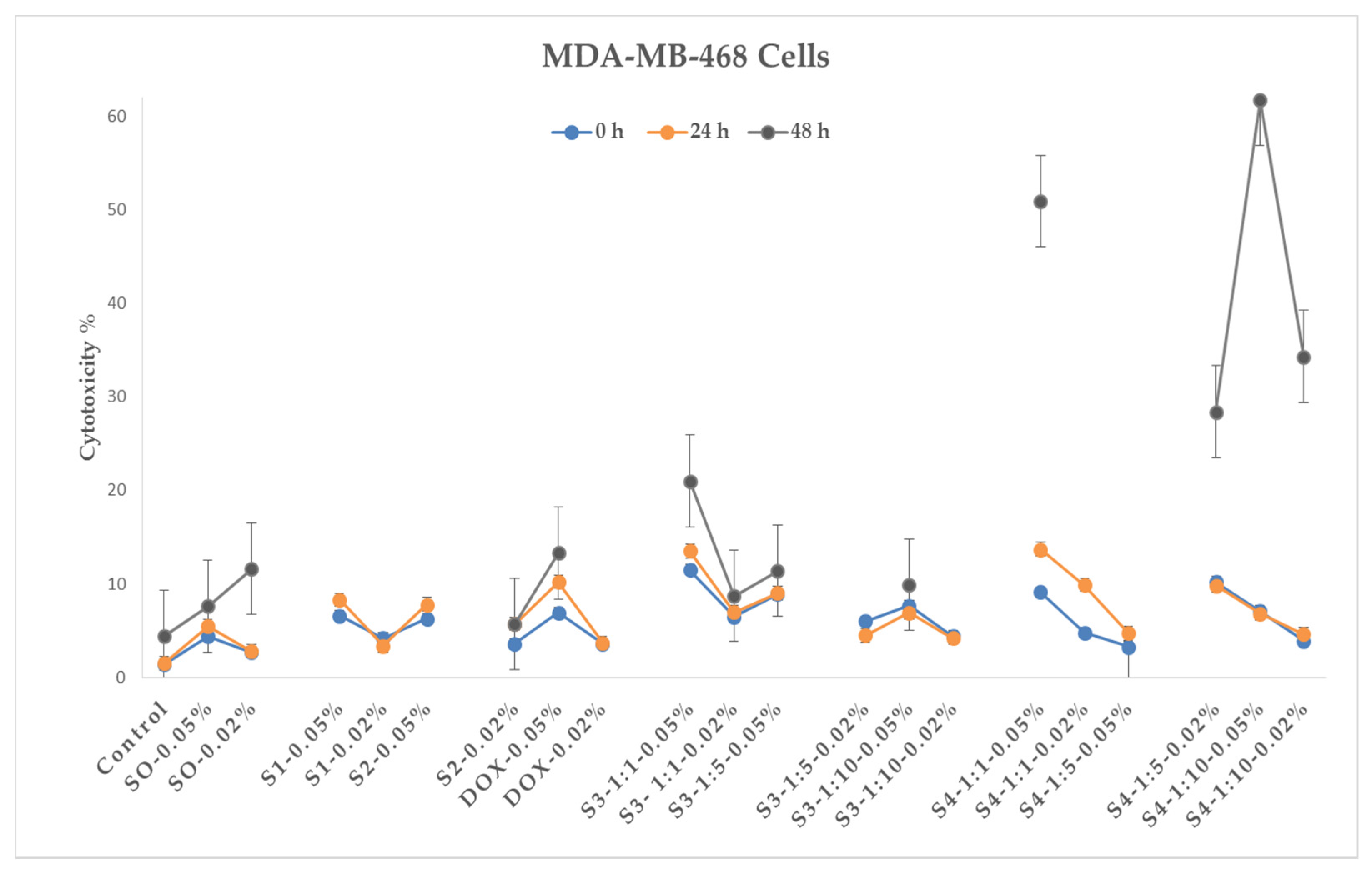
3.8.3. MDA-MB-468 Cancer Cell Line
4. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Juan, A.; Cimas, F.J.; Bravo, I.; Pandiella, A.; Ocaña, A.; Alonso-Moreno, C. Antibody Conjugation of Nanoparticles as Therapeutics for Breast Cancer Treatment. Int. J. Mol. Sci. 2020, 21, 6018. [Google Scholar] [CrossRef]
- Duche, H.; Tsegay, A.T.; Tamirat, K.S. Identifying Risk Factors of Breast Cancer Among Women Attending Selected Hospitals of Addis Ababa City: Hospital-Based Unmatched Case-Control Study. Breast Cancer (Dove Med. Press) 2021, 13, 189–197. [Google Scholar] [CrossRef]
- Assefa, A.A.; Abera, G.; Geta, M. Breast Cancer Screening Practice and Associated Factors Among Women Aged 20–70 Years in Urban Settings of SNNPR, Ethiopia. Breast Cancer (Dove Med. Press) 2021, 13, 9–19. [Google Scholar] [CrossRef]
- Daniyal, A.; Santoso, I.; Gunawan, N.H.P.; Barliana, M.I.; Abdulah, R. Genetic Influences in Breast Cancer Drug Resistance. Breast Cancer (Dove Med. Press) 2021, 13, 59–85. [Google Scholar] [CrossRef]
- Kumar, D.N.; Chaudhuri, A.; Aqil, F.; Dehari, D.; Munagala, R.; Singh, S.; Gupta, R.C.; Agrawal, A.K. Exosomes as Emerging Drug Delivery and Diagnostic Modality for Breast Cancer: Recent Advances in Isolation and Application. Cancers 2022, 14, 1435. [Google Scholar] [CrossRef] [PubMed]
- Arumugam, A.; Subramani, R.; Nandy, S.B.; Terreros, D.; Dwivedi, A.K.; Saltzstein, E.; Lakshmanaswamy, R. Silencing Growth Hormone Receptor Inhibits Estrogen Receptor Negative Breast Cancer through ATP-Binding Cassette Sub-Family G Member 2. Exp. Mol. Med. 2019, 51, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Dai, X.; Xiang, L.; Li, T.; Bai, Z. Cancer Hallmarks, Biomarkers and Breast Cancer Molecular Subtypes. J. Cancer 2016, 7, 1281. [Google Scholar] [CrossRef] [PubMed]
- Abdi, H.; Yekani Motlagh, S.; Soltanipour, H. Study of Magnetic Nanofluid Flow in a Square Cavity under the Magnetic Field of a Wire Carrying the Electric Current in Turbulence Regime. Results Phys. 2020, 18, 103224. [Google Scholar] [CrossRef]
- Wen, S.; Manuel, L.; Doolan, M.; Westhuyzen, J.; Shakespeare, T.P.; Aherne, N.J. Effect of Clinical and Treatment Factors on Survival Outcomes of Triple Negative Breast Cancer Patients. Breast Cancer (Dove Med. Press) 2020, 12, 27–35. [Google Scholar] [CrossRef]
- Dass, S.A.; Tan, K.L.; Rajan, R.S.; Mokhtar, N.F.; Adzmi, E.R.M.; Rahman, W.F.W.A.; Din, T.A.D.A.-A.T.; Balakrishnan, V. Triple Negative Breast Cancer: A Review of Present and Future Diagnostic Modalities. Medicina 2021, 57, 62. [Google Scholar] [CrossRef] [PubMed]
- Qattan, A. Novel MiRNA Targets and Therapies in the Triple-Negative Breast Cancer Microenvironment: An Emerging Hope for a Challenging Disease. Int. J. Mol. Sci. 2020, 21, 8905. [Google Scholar] [CrossRef]
- Cocco, S.; Piezzo, M.; Calabrese, A.; Cianniello, D.; Caputo, R.; Di Lauro, V.; Fusco, G.; di Gioia, G.; Licenziato, M.; de Laurentiis, M. Biomarkers in Triple-Negative Breast Cancer: State-of-the-Art and Future Perspectives. Int. J. Mol. Sci. 2020, 21, 4579. [Google Scholar] [CrossRef]
- Mina, L.A.; Lim, S.; Bahadur, S.W.; Firoz, A.T. Immunotherapy for the Treatment of Breast Cancer: Emerging New Data. Breast Cancer (Dove Med. Press) 2020, 11, 321–328. [Google Scholar] [CrossRef]
- Milioli, H.H.; Tishchenko, I.; Riveros, C.; Berretta, R.; Moscato, P. Basal-like Breast Cancer: Molecular Profiles, Clinical Features and Survival Outcomes. BMC Med. Genom. 2017, 10, 19. [Google Scholar] [CrossRef]
- Calero, M.; Chiappi, M.; Lazaro-Carrillo, A.; Rodríguez, M.J.; Chichón, F.J.; Crosbie-Staunton, K.; Prina-Mello, A.; Volkov, Y.; Villanueva, A.; Carrascosa, J.L. Characterization of Interaction of Magnetic Nanoparticles with Breast Cancer Cells. J. Nanobiotechnol. 2015, 13, 16. [Google Scholar] [CrossRef]
- Sharma, G.N.; Dave, R.; Sanadya, J.; Sharma, P.; Sharma, K.K. Various types and management of breast cancer: An overview. J. Adv. Pharm. Technol. Res. 2010, 1, 109. [Google Scholar] [PubMed]
- Mu, Q.; Wang, H.; Zhang, M. Nanoparticles for Imaging and Treatment of Metastatic Breast Cancer. Expert. Opin. Drug Deliv. 2017, 14, 123–136. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.S.; Yost, S.E.; Yuan, Y. Neoadjuvant Treatment for Triple Negative Breast Cancer: Recent Progresses and Challenges. Cancers 2020, 12, 1404. [Google Scholar] [CrossRef] [PubMed]
- Lv, L.; Shi, Y.; Wu, J.; Li, G. Nanosized Drug Delivery Systems for Breast Cancer Stem Cell Targeting. Int. J. Nanomed. 2021, 16, 1487–1508. [Google Scholar] [CrossRef]
- Wang, X. Explore Genomic Profiles for Triple-Negative Breast Cancer to Discover Drug Targets. In Oncogenomics: From Basic Research to Precision Medicine; Dammacco, F., Silvestris, F., Eds.; Academic Press: Cambridge, MA, USA, 2019; pp. 423–440. [Google Scholar]
- Hematyar, M.; Soleimani, M.; Es-Haghi, A.; Rezaei Mokarram, A. Synergistic Co-Delivery of Doxorubicin and Melittin Using Functionalized Magnetic Nanoparticles for Cancer Treatment: Loading and in Vitro Release Study by LC–MS/MS. Artif. Cells Nanomed. Biotechnol. 2018, 46, 1226–1235. [Google Scholar] [CrossRef]
- Savage, P.; Cooke, R.; O’Nions, J.; Krell, J.; Kwan, A.; Camarata, M.; Dancy, G.; Short, D.; Seckl, M.J.; Swerdlow, A. Effects of Single-Agent and Combination Chemotherapy for Gestational Trophoblastic Tumors on Risks of Second Malignancy and Early Menopause. J. Clin. Oncol. 2015, 33, 472–478. [Google Scholar] [CrossRef]
- Gilad, Y.; Gellerman, G.; Lonard, D.M.; O’Malley, B.W. Drug Combination in Cancer Treatment—From Cocktails to Conjugated Combinations. Cancers 2021, 13, 669. [Google Scholar] [CrossRef]
- Zhu, L.; Zhou, Z.; Mao, H.; Yang, L. Magnetic Nanoparticles for Precision Oncology: Theranostic Magnetic Iron Oxide Nanoparticles for Image-Guided and Targeted Cancer Therapy. Nanomedicine 2017, 12, 73–87. [Google Scholar] [CrossRef] [PubMed]
- Arias, L.S.; Pessan, J.P.; Vieira, A.P.M.; de Lima, T.M.T.; Delbem, A.C.B.; Monteiro, D.R. Iron Oxide Nanoparticles for Biomedical Applications: A Perspective on Synthesis, Drugs, Antimicrobial Activity, and Toxicity. Antibiotics 2018, 7, 46. [Google Scholar] [CrossRef]
- Zhao, S.; Yu, X.; Qian, Y.; Chen, W.; Shen, J. Multifunctional Magnetic Iron Oxide Nanoparticles: An Advanced Platform for Cancer Theranostics. Theranostics 2020, 10, 6278–6309. [Google Scholar] [CrossRef] [PubMed]
- Miller-Kleinhenz, J.M.; Bozeman, E.N.; Yang, L. Targeted Nanoparticles for Image-Guided Treatment of Triple-Negative Breast Cancer: Clinical Significance and Technological Advances. WIREs Nanomed. Nanobiotechnol. 2015, 7, 797–816. [Google Scholar] [CrossRef] [PubMed]
- Garcia Rubia, G.; Peigneux, A.; Jabalera, Y.; Puerma, J.; Oltolina, F.; Elert, K.; Colangelo, D.; Gomez Morales, J.; Prat, M.; Jimenez-Lopez, C. pH-Dependent Adsorption Release of Doxorubicin on MamC-Biomimetic Magnetite Nanoparticles. Langmuir 2018, 34, 13713–13724. [Google Scholar] [CrossRef]
- Nafar, S.; Nouri, N.; Alipour, M.; Fallahi, J.; Zare, F.; Tabei, S.M.B. Exosome as a target for cancer treatment. J. Investig. Nanomed. 2022, 70, 2194. [Google Scholar] [CrossRef]
- Norouzi, M.; Yathindranath, V.; Thliveris, J.A.; Kopec, B.M.; Siahaan, T.J.; Miller, D.W. Doxorubicin-Loaded Iron Oxide Nanoparticles for Glioblastoma Therapy: A Combinational Approach for Enhanced Delivery of Nanoparticles. Sci. Rep. 2020, 10, 11292. [Google Scholar] [CrossRef]
- Malik, A.; Butt, T.T.; Zahid, S.; Zahid, F.; Waquar, S.; Rasool, M.; Qazi, M.H.; Qazi, A.M. Use of Magnetic Nanoparticles as Targeted Therapy: Theranostic Approach to Treat and Diagnose Cancer. J. Nanotechnol. 2017, 2017, 1098765. [Google Scholar] [CrossRef]
- Markhulia, J.; Kekutia, S.; Mitskevich, N.; Mikelashvili, V.; Saneblidze, L.; Leladze, N.; Jabua, Z.; Sacarescu, L.; Kriechbaum, M.; Almásy, L. Synthesis and in vivo Investigation of Therapeutic Effect of Magnetite Nanofluids in Mouse Prostate Cancer Model. Dig. J. Nanomater. Biostruct. 2018, 13, 1081–1090. [Google Scholar]
- Elgqvist, J. Nanoparticles as Theranostic Vehicles in Experimental and Clinical Applications—Focus on Prostate and Breast Cancer. Int. J. Mol. Sci. 2017, 18, 1102. [Google Scholar] [CrossRef] [PubMed]
- Shin, H.Y.; Park, T.J.; Kim, M.I. Recent Research Trends and Future Prospects in Nanozymes. J. Nanomater. 2015, 2015, 756278. [Google Scholar] [CrossRef]
- Wang, P.; Wang, T.; Hong, J.; Yan, X.; Liang, M. Nanozymes: A New Disease Imaging Strategy. Front. Bioeng. Biotechnol. 2020, 8, 15. [Google Scholar] [CrossRef]
- Wydra, R.J.; Oliver, C.E.; Anderson, K.W.; Dziubla, T.D.; Hilt, J.Z. Accelerated generation of free radicals by iron oxide nanoparticles in the presence of an alternating magnetic field. RSC Adv. 2015, 5, 18888–18893. [Google Scholar] [CrossRef]
- Mai, T.; Hilt, J.Z. Magnetic Nanoparticles: Reactive Oxygen Species Generation and Potential Therapeutic Applications. J. Nanoparticle Res. 2017, 19, 253. [Google Scholar] [CrossRef]
- Kicheeva, A.G.; Sushko, E.S.; Bondarenko, L.S.; Kydralieva, K.A.; Pankratov, D.A.; Tropskaya, N.S.; Dzeranov, A.A.; Dzhardimalieva, G.I.; Zarrelli, M.; Kudryasheva, N.S. Functionalized Magnetite Nanoparticles: Characterization, Bioeffects, and Role of Reactive Oxygen Species in Unicellular and Enzymatic Systems. Int. J. Mol. Sci. 2023, 24, 1133. [Google Scholar] [CrossRef]
- Hernandes, E.P.; Lazarin-Bidóia, D.; Bini, R.D.; Nakamura, C.V.; Cótica, L.F.; de Oliveira Silva Lautenschlager, S. Doxorubicin-Loaded Iron Oxide Nanoparticles Induce Oxidative Stress and Cell Cycle Arrest in Breast Cancer Cells. Antioxidants 2023, 12, 237. [Google Scholar] [CrossRef]
- Hernandes, E.P.; Bini, R.D.; Endo, K.M.; de Oliveira Junior, V.A.; de Almeida, I.V.; Dias, G.S.; dos Santos, I.A.; de Oliveira, P.N.; Vicentini, V.E.P.; Cotica, L.F. Doxorubicin-Loaded Magnetic Nanoparticles: Enhancement of Doxorubicin’s Effect on Breast Cancer Cells (MCF-7). Magnetochemistry 2022, 8, 114. [Google Scholar] [CrossRef]
- Liang, M.; Yan, X. Nanozymes: From New Concepts, Mechanisms, and Standards to Applications. Acc. Chem. Res. 2019, 52, 2190–2200. [Google Scholar] [CrossRef]
- Zhu, X.; Liu, Y.; Yuan, G.; Guo, X.; Cen, J.; Gong, Y.; Liu, J.; Gang, Y. In Situ Fabrication of MS@MnO2 Hybrid as Nanozymes for Enhancing ROS-Mediated Breast Cancer Therapy. Nanoscale 2020, 12, 22317–22329. [Google Scholar] [CrossRef]
- Thangudu, S.; Su, C.-H. Peroxidase Mimetic Nanozymes in Cancer Phototherapy: Progress and Perspectives. Biomolecules 2021, 11, 1015. [Google Scholar] [CrossRef]
- Wang, J.; Sun, D.; Huang, L.; Wang, S.; Jin, Y. Targeting Reactive Oxygen Species Capacity of Tumor Cells with Repurposed Drug as an Anticancer Therapy. Oxid. Med. Cell. Longev. 2021, 2021, 8532940. [Google Scholar] [CrossRef]
- Khan, A.Q.; Rashid, K.; AlAmodi, A.A.; Agha, M.V.; Akhtar, S.; Hakeem, I.; Raza, S.S.; Uddin, S. Reactive oxygen species (ROS) in cancer pathogenesis and therapy: An update on the role of ROS in anticancer action of benzophenanthridine alkaloids. Biomed. Pharmacother. 2021, 143, 112142. [Google Scholar] [CrossRef]
- Markhulia, J.; Kekutia, S.; Mikelashvili, V.; Almásy, L.; Saneblidze, L.; Tsertsvadze, T.; Maisuradze, N.; Leladze, N.; Kriechbaum, M. Stable Aqueous Dispersions of Bare and Double Layer Functionalized Superparamagnetic Iron Oxide Nanoparticles for Biomedical Applications. Mater. Sci. Poland 2021, 39, 331–345. [Google Scholar] [CrossRef]
- Socoliuc, V.; Peddis, D.; Petrenko, V.I.; Avdeev, M.V.; Susan-Resiga, D.; Szabó, T.; Turcu, R.; Tombácz, E.; Vékás, L. Magnetic Nanoparticle Systems for Nanomedicine—A Materials Science Perspective. Magnetochemistry 2020, 6, 2. [Google Scholar] [CrossRef]
- Herranz, F.; Salinas, B.; Groult, H.; Pellico, J.; Lechuga-Vieco, A.V.; Bhavesh, R.; Ruiz-Cabello, J. Superparamagnetic Nanoparticles for Atherosclerosis Imaging. Nanomaterials 2014, 4, 408–438. [Google Scholar] [CrossRef]
- Mikelashvili, V.; Kekutia, S.; Markhulia, J.; Saneblidze, L.; Maisuradze, N.; Kriechbaum, M.; Almásy, L. Synthesis and Characterization of Citric Acid-Modified Iron Oxide Nanoparticles Prepared with Electrohydraulic Discharge Treatment. Materials 2023, 16, 746. [Google Scholar] [CrossRef] [PubMed]
- Kovrigina, E.; Chubarov, A.; Dmitrienko, E. High Drug Capacity Doxorubicin-Loaded Iron Oxide Nanocomposites for Cancer Therapy. Magnetochemistry 2022, 8, 54. [Google Scholar] [CrossRef]
- Kumar, P.; Agnihotri, S.; Roy, I. Synthesis of Dox Drug Conjugation and Citric Acid Stabilized Superparamagnetic Iron-Oxide Nanoparticles for Drug Delivery. Biochem. Physiol. 2016, 5, 2. [Google Scholar] [CrossRef]
- Nawara, K.; Romiszewski, J.; Kijewska, K.; Szczytko, J.; Twardowski, A.; Mazur, M.; Krysinski, P. Adsorption of doxorubicin onto citrate-stabilized magnetic nanoparticles. J. Phys. Chem. C 2012, 116, 5598–5609. [Google Scholar] [CrossRef]
- Bajpai, S.; Tiwari, S.K.; Sonker, M.; Joshi, A.; Gupta, V.; Kumar, Y.; Shreyash, N.; Biswas, S. Recent Advances in Nanoparticle-Based Cancer Treatment: A Review. ACS Appl. Nano Mater. 2021, 4, 6441–6470. [Google Scholar] [CrossRef]
- Nayak, J.; Prajapati, K.S.; Kumar, S.; Vashistha, V.K.; Sahoo, S.K.; Kumar, R. Thiolated β-cyclodextrin modified iron oxide nanoparticles for effective targeted cancer therapy. Mater. Today Commun. 2022, 33, 104644. [Google Scholar] [CrossRef]
- Mosmann, T. Rapid Colorimetric Assay for Cellular Growth and Survival: Application to Proliferation and Cytotoxicity Assays. J. Immunol. Methods 1983, 65, 55–63. [Google Scholar] [CrossRef] [PubMed]
- van Rensburg, C.E.J.; Anderson, R.; Jooné, G.; Myer, M.S.; O’Sullivan, J.F. Novel Tetramethylpiperidine-Substituted Phenazines Are Potent Inhibitors of P-Glycoprotein Activity in a Multidrug Resistant Cancer Cell Line. Anticancer Drugs 1997, 8, 708–713. [Google Scholar] [CrossRef]
- Cheraghipour, E.; Javadpour, S.; Mehdizadeh, A.R. Citrate Capped Superparamagnetic Iron Oxide Nanoparticles Used for Hyperthermia Therapy. J. Biomed. Sci. Eng. 2012, 5, 715–719. [Google Scholar] [CrossRef]
- Nigam, S.; Barick, K.C.; Bahadur, D. Development of Citrate-Stabilized Fe3O4 Nanoparticles: Conjugation and Release of Doxorubicin for Therapeutic Applications. J. Magn. Magn. Mater. 2010, 323, 237–243. [Google Scholar] [CrossRef]
- Nalbandian, L.; Patrikiadou, E.; Zaspalis, V.; Patrikidou, A.; Hatzidaki, E.; Papandreou, C.N. Magnetic Nanoparticles in Medical Diagnostic Applications: Synthesis, Characterization and Proteins Conjugation. Curr. Nanosci. 2015, 12, 455–468. [Google Scholar] [CrossRef]
- Ghanbari, M.; Asadi, A.; Rostamzadeh, S. Study of the Cytotoxicity Effect of Doxorubicin-Loaded/Folic Acid-Targeted Super Paramagnetic Iron Oxide Nanoparticles on AGS Cancer Cell Line. J. Nanomed. Nanotechnol. 2016, 7, 368. [Google Scholar] [CrossRef]
- Dahri, M.; Akbarialiabad, H.; Jahromi, A.M.; Maleki, R. Loading and release of cancer chemotherapy drugs utilizing simultaneous temperature and pH-responsive nanohybrid. BMC Pharmacol. Toxicol. 2021, 22, 41. [Google Scholar] [CrossRef]
- Awashra, M.; Młynarz, P. The toxicity of nanoparticles and their interaction with cells: An in vitro metabolomic perspective. Nanoscale Adv. 2023, 5, 2674–2723. [Google Scholar] [CrossRef] [PubMed]
- Bryce, N.S.; Pham, B.T.T.; Fong, N.W.S.; Jain, N.; Pan, E.H.; Whan, R.M.; Hambley, T.W.; Hawkett, B.S. The composition and end-group functionality of sterically stabilized nanoparticles enhances the effectiveness of co-administered cytotoxins. Biomater. Sci. 2013, 1, 1260–1272. [Google Scholar] [CrossRef] [PubMed]
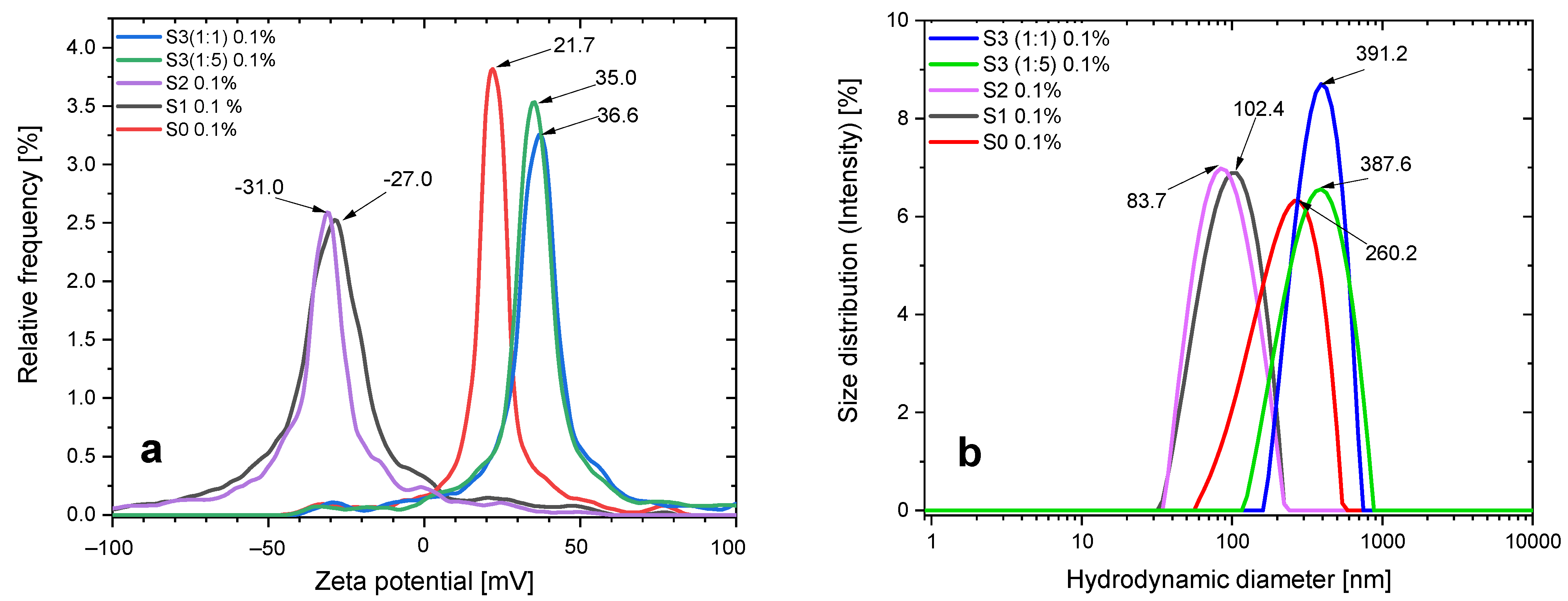

| Samples | Mean Zeta Potential (mV) | Electrophoretic Mobility (µm cm/Vs) | Conductivity (mS/cm) | Hydrodynamic Diameter (nm) | Peak Analysis Intensity (nm) | Polydispersity Index (%) |
|---|---|---|---|---|---|---|
| S0 | 21.0 | 1.63 | 0.007 | 226.4 | 260.2 | 26.2 |
| S1 | −27.7 | −1.96 | 0.003 | 93.6 | 102.4 | 20.5 |
| S2 | −31.5 | −2.45 | 0.01 | 93.8 | 86.9 | 22.4 |
| S3 (1:1) | 36.8 | 2.60 | 0.24 | 380.9 | 391.3 | 18.6 |
| S3 (1:5) | 34.7 | 2.46 | 0.90 | 375.6 | 386.2 | 24.2 |
| Samples | Mean Zeta Potential (mV) | Electrophoretic Mobility (µm cm/Vs) | Conductivity (mS/cm) | Hydrodynamic Diameter (nm) | Standard Dev. (nm) | Polydispersity Index (%) |
|---|---|---|---|---|---|---|
| S1 + DW 0.02% | −29.92 | −2.12 | 0.54 | 46.6 | 11.8 | 12.4 |
| S1 + NaCl 0.02% | −23.29 | −1.64 | 6.92 | 42.2 | 11.3 | 11.7 |
| S2 + DW 0.02% | −33.88 | −2,40 | 0.43 | 43.2 | 13.7 | 10.2 |
| S2 + NaCl 0.02% | −23.82 | −1.68 | 7.70 | 42.6 | 11.0 | 12.6 |
| S3 (1:1) + DW 0.05% | 36.56 | 2.59 | 0.11 | 271.0 | 104.1 | 15.8 |
| S3 (1:1) + NaCl 0.05% | 20.51 | 1.45 | 6.57 | 550.4 | 387.9 | 25.0 |
| S4 (1:1) + DW 0.05% | 38.36 | 2.72 | 0.04 | 198.1 | 61.6 | 17.9 |
| S4 (1:1) + NaCl 0.05% | 23.28 | 1.64 | 5.73 | 455.7 | 223.2 | 26.3 |
| Sample’s Designations | Solid Component | Designations Corresponding to Different Concentrations (w/v) | DOX Concentration (mM) | Concentration, (mg/mL) |
|---|---|---|---|---|
| DOX | Doxorubicin | DOX–0.1% | 1.84 | |
| DOX–0.05% | 0.92 | |||
| DOX–0.02% | 0.37 | |||
| S0 | BIONs – Bare iron oxide nanoparticles | S0–0.1% | 1.00 | |
| S0–0.05% | 0.50 | |||
| S0–0.02% | 0.20 | |||
| S1 | CA-SPIONs – Citric acid-coated iron oxide nanoparticles | S1–0.1% | 1.00 | |
| S1–0.05% | 0.50 | |||
| S1–0.02% | 0.20 | |||
| S2 | CA-SPIONs-EHD – Electrohydraulic discharge-processed CA-SPIONs | S2–0.1% | 1.00 | |
| S2–0.05% | 0.50 | |||
| S2–0.02% | 0.20 | |||
| S3 | DOX-CA-SPIONs – Doxorubicin-loaded CA-SPIONs | S3–1:1–0.1% | 0.92 | 0.50 |
| S3–1:1–0.05% | 0.46 | 0.25 | ||
| S3–1:1–0.02% | 0.18 | 0.10 | ||
| S3–1:5–0.10% | 0.31 | 0.83 | ||
| S3–1:5–0.05% | 0.15 | 0.42 | ||
| S3–1:5–0.02% | 0.06 | 0.17 | ||
| S3–1:10–0.10% | 0.17 | 0.91 | ||
| S3–1:10–0.05% | 0.08 | 0.45 | ||
| S3–1:10–0.02% | 0.03 | 0.18 | ||
| S4 | DOX-CA-SPIONs-EHD – Electrohydraulic discharge-processed DOX-CA-SPIONs | S4–1:1–0.1% | 0.92 | 0.50 |
| S4–1:1–0.05% | 0.46 | 0.25 | ||
| S4–1:1–0.02% | 0.18 | 0.10 | ||
| S4–1:5–0.1% | 0.31 | 0.83 | ||
| S4–1:5–0.05% | 0.15 | 0.42 | ||
| S4–1:5–0.02% | 0.06 | 0.17 | ||
| S4–1:10–0.1% | 0.17 | 0.91 | ||
| S4–1:10–0.05% | 0.08 | 0.45 | ||
| S4–1:10–0.02% | 0.03 | 0.18 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Markhulia, J.; Kekutia, S.; Mikelashvili, V.; Saneblidze, L.; Tsertsvadze, T.; Maisuradze, N.; Leladze, N.; Czigány, Z.; Almásy, L. Synthesis, Characterization, and In Vitro Cytotoxicity Evaluation of Doxorubicin-Loaded Magnetite Nanoparticles on Triple-Negative Breast Cancer Cell Lines. Pharmaceutics 2023, 15, 1758. https://doi.org/10.3390/pharmaceutics15061758
Markhulia J, Kekutia S, Mikelashvili V, Saneblidze L, Tsertsvadze T, Maisuradze N, Leladze N, Czigány Z, Almásy L. Synthesis, Characterization, and In Vitro Cytotoxicity Evaluation of Doxorubicin-Loaded Magnetite Nanoparticles on Triple-Negative Breast Cancer Cell Lines. Pharmaceutics. 2023; 15(6):1758. https://doi.org/10.3390/pharmaceutics15061758
Chicago/Turabian StyleMarkhulia, Jano, Shalva Kekutia, Vladimer Mikelashvili, Liana Saneblidze, Tamar Tsertsvadze, Nino Maisuradze, Nino Leladze, Zsolt Czigány, and László Almásy. 2023. "Synthesis, Characterization, and In Vitro Cytotoxicity Evaluation of Doxorubicin-Loaded Magnetite Nanoparticles on Triple-Negative Breast Cancer Cell Lines" Pharmaceutics 15, no. 6: 1758. https://doi.org/10.3390/pharmaceutics15061758
APA StyleMarkhulia, J., Kekutia, S., Mikelashvili, V., Saneblidze, L., Tsertsvadze, T., Maisuradze, N., Leladze, N., Czigány, Z., & Almásy, L. (2023). Synthesis, Characterization, and In Vitro Cytotoxicity Evaluation of Doxorubicin-Loaded Magnetite Nanoparticles on Triple-Negative Breast Cancer Cell Lines. Pharmaceutics, 15(6), 1758. https://doi.org/10.3390/pharmaceutics15061758









