Recent Advances in Biocompatible Ionic Liquids in Drug Formulation and Delivery
Abstract
1. Introduction
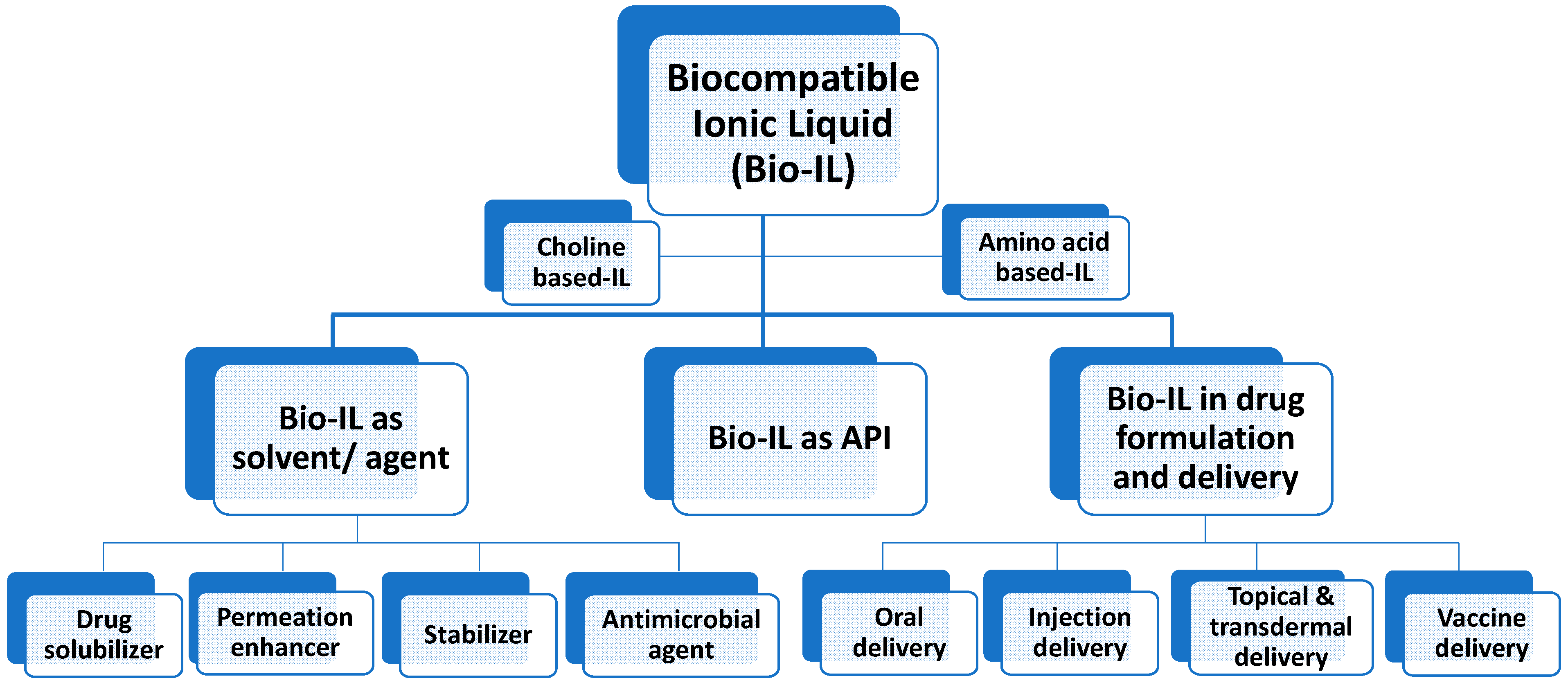
2. Biocompatible Ionic Liquids (Bio-ILs) in Drug Formulation
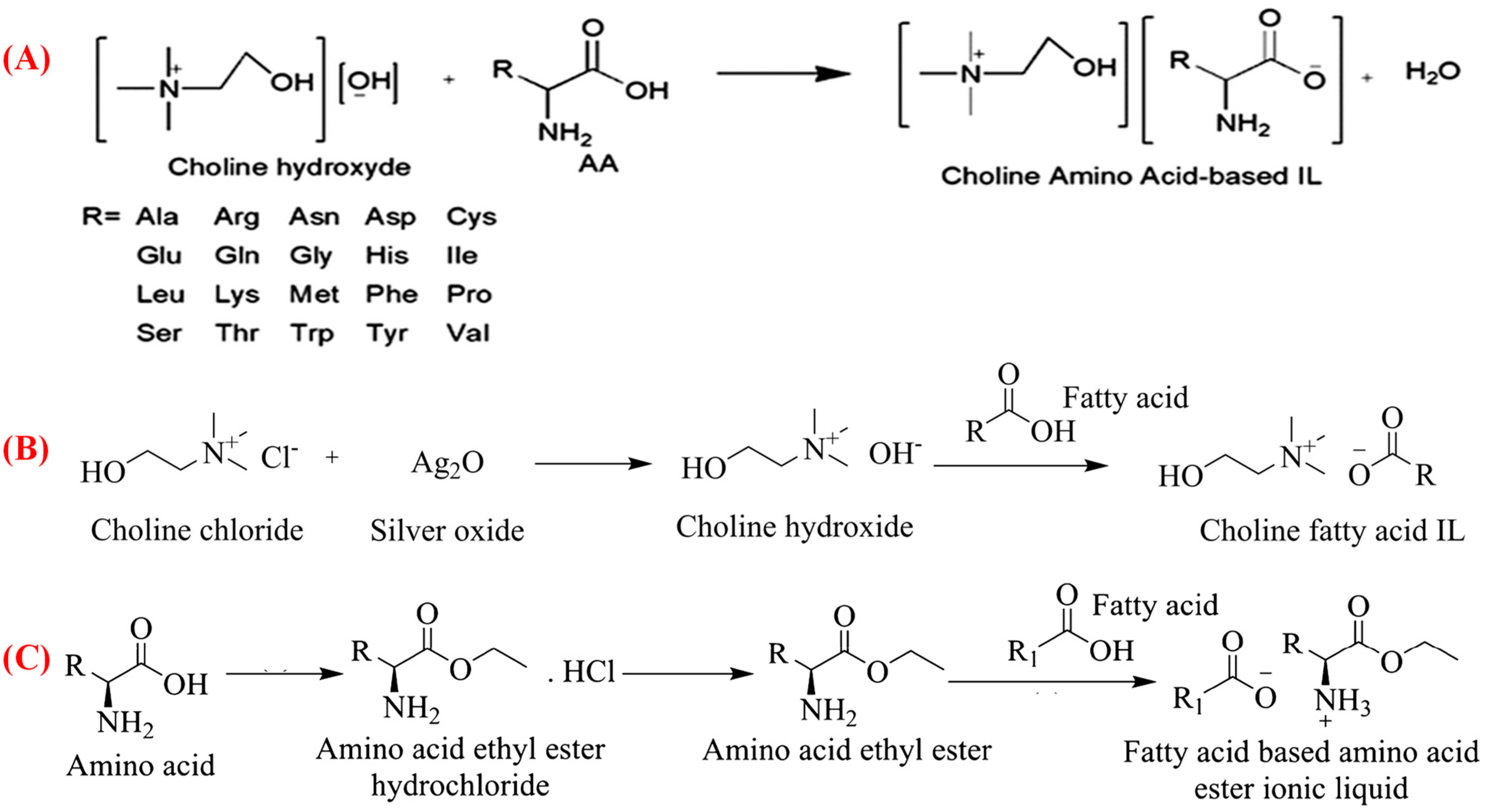
2.1. Choline-Based Bio-ILs
2.2. Amino Acid-Based Bio-ILs
3. Bio-ILs as Solvents/Agents
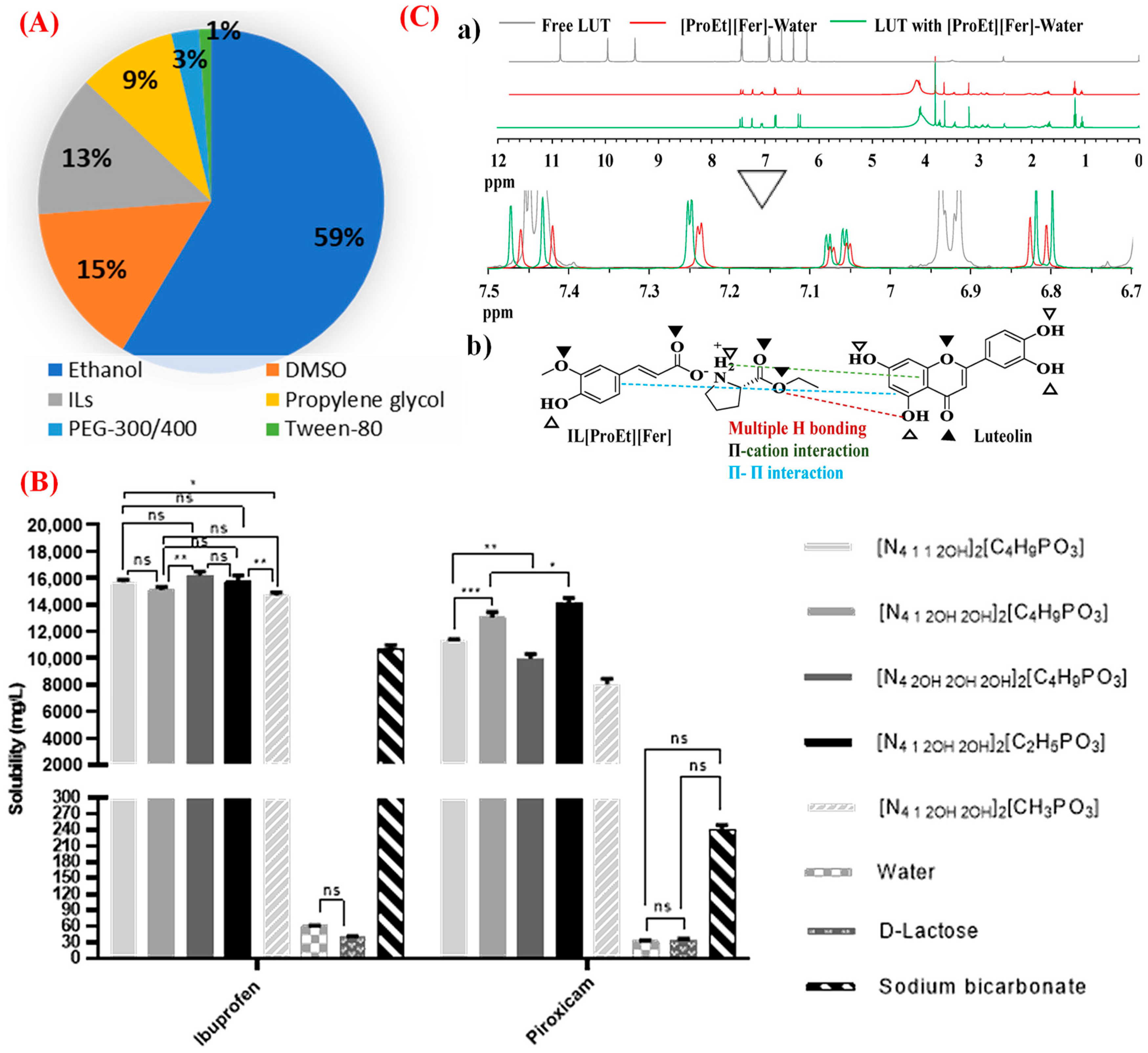
3.1. Drug Solubilizers
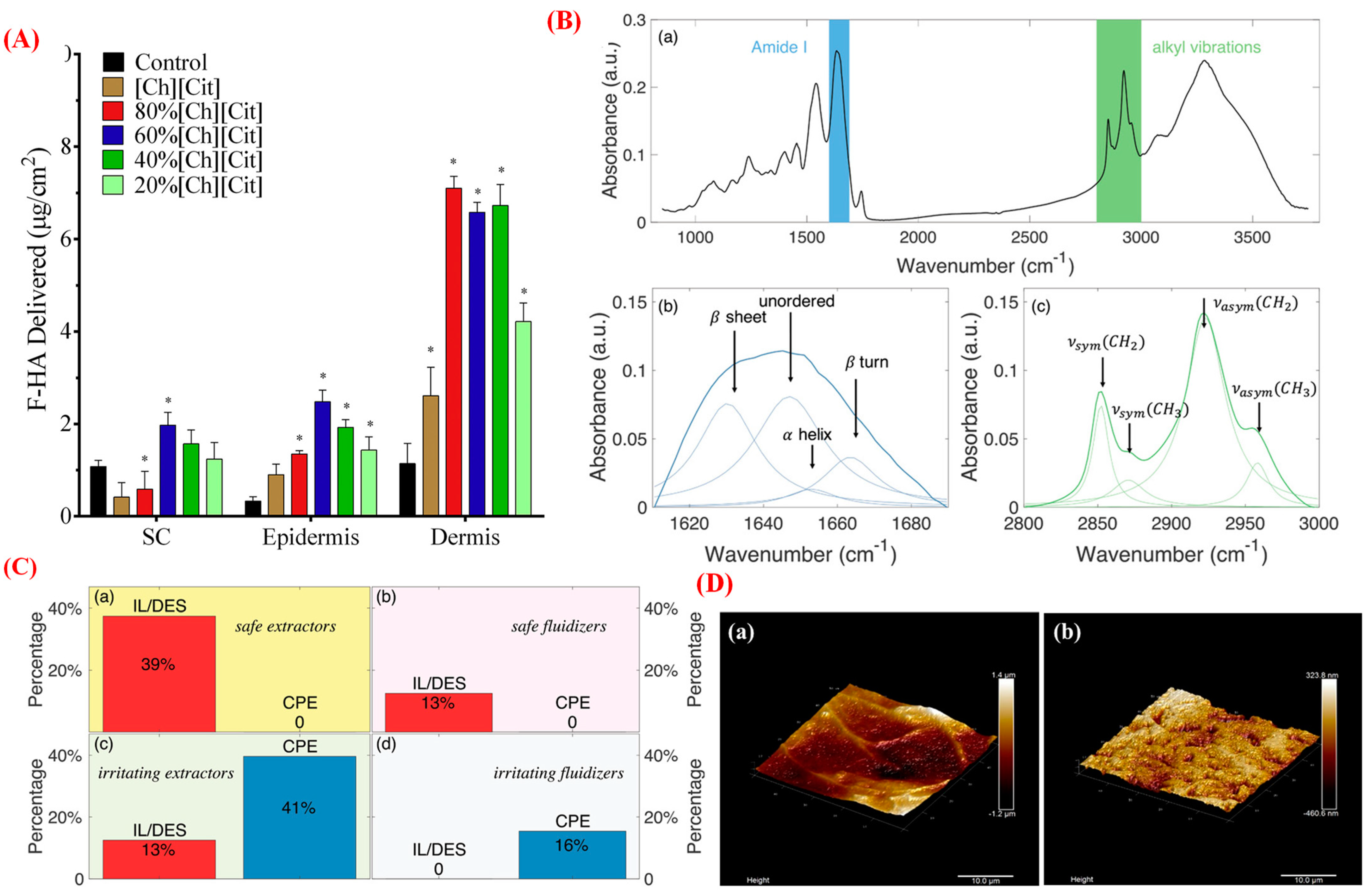
3.2. Permeation Enhancers
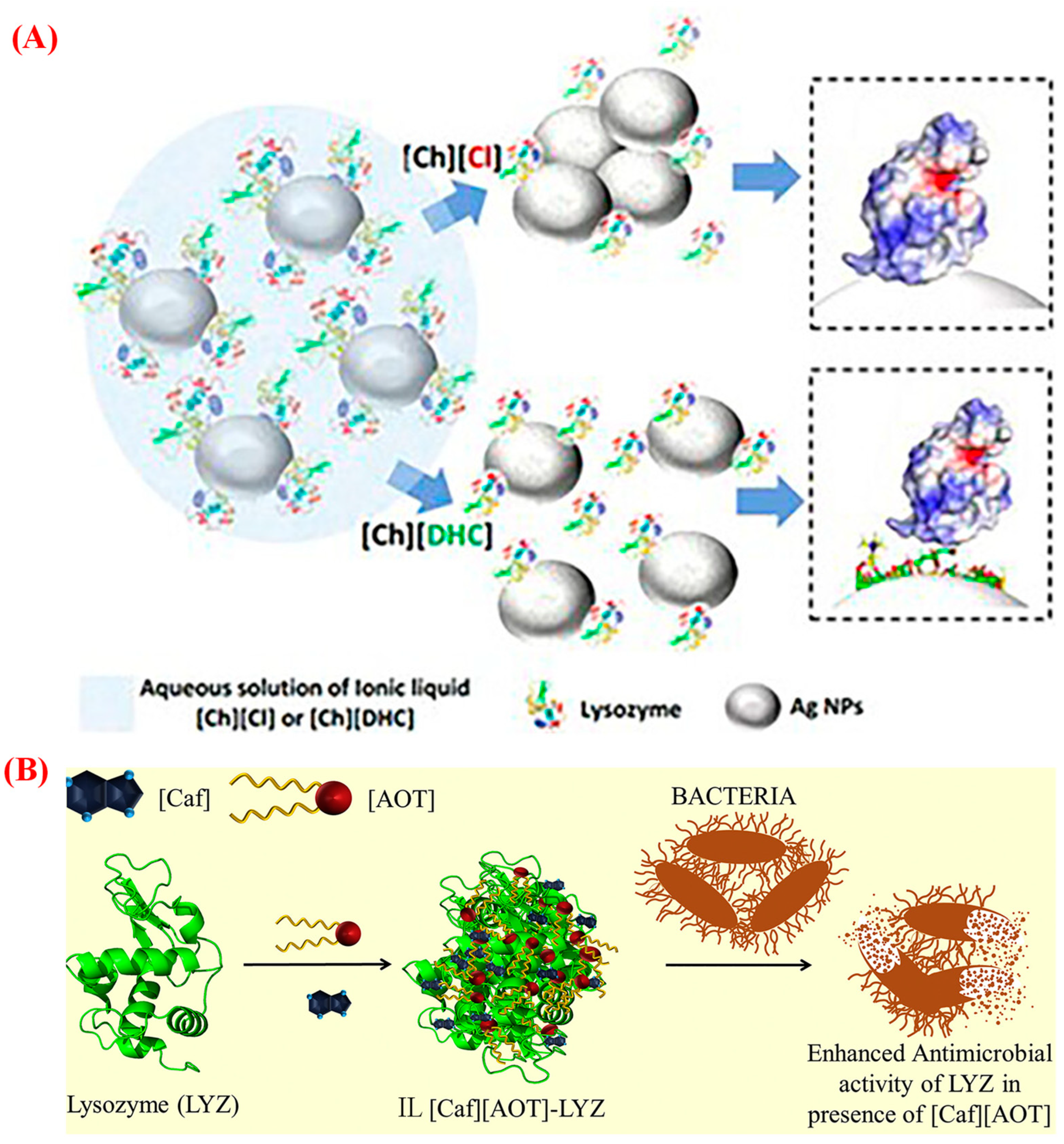
3.3. Macromolecular Therapeutic Stabilizers
3.4. Antimicrobial Agents
| No. | Drug | ILs | Role of ILs | Main Findings | Ref. |
|---|---|---|---|---|---|
| 1. | Hypoxia-inducible factor (HIF) as cancer drug | Pyridinium-based-ILs | Solvents | a. ILs inhibited the cancer cells viability compared to the normal cells. b. ILs suppressed the mitochondria and HIF-1α- dependent glucose metabolic pathway in hypoxic cancer cells. | [59] |
| 2. | Diacerein | Betaine- and carnitine-based ILs | Solubilizing and stabilizing agent | a. Enhanced the solubility and stability of drug. b. Exhibited strong bactericidal activity against pathogens. c. IL-mediated formulation increased the ocular residence time through mucoadhesion. | [60] |
| 3. | Lysozyme Bovine serum albumin | [Cho][H2PO4] [Cho][C4F9SO3] [C2MIN][C4F9SO3] | Solubilizing and encapsulating agent | a. Maintained the globular folded structure and hydrolytic activity of the proteins in the presence of ILs. b. Encapsulated LYZ by the ILs. | [61] |
| 4. | Luteolin | [ProEt][Fer] [ProEt][Van] [ProEt][Cou] [ProEt][Ben] | Solubilizing agent | a. LUT’s solubility in ILs showed 880-fold higher than in water. b. ILs revealed as green solvents. c. Exhibited superior organoleptic properties on red apple slices. | [31] |
| 5. | Luteolin | [Cho][Ole] | Encapsulating agent | a. Formed spherical micelles with a mean particle size of 73 nm. b. Exhibited enhanced aqueous solubility with excellent encapsulation efficiency (94.3%). c. Showed higher antibacterial activity with excellent food preservation activity than toxic chemical preservatives. | [62] |
| 6. | Ibuprofen | [Cho]:[Van], [Gal], [Sal] | Solubilizing agent | Significantly increased the drug solubility compared with conventional hydrotropes. | [63] |
| 7. | Piroxicam Ibuprofen | [N4,1,2OH,2OH]2 [C2H5PO3] | Solubilizing agent | a. Significantly increased the solubility up to 300-fold compared with water. b. Decreased lipophilicity of drugs in the presence of the ILs. c. No significant toxicity observed against fibroblast cells. | [34] |
| 8. | Ibuprofen | Dianionic ILs | Solubilizing agent | a. Solubility increased up to 40-fold compared with water. b. Lipophilicity decreased in the presence of ILs. | [64] |
| 9. | Diclofenac sodium | [Cho][Ace] | Hydrophilic agent in drug carrier | Exhibited excellent biodegradability, stimuli-responsive properties, and biocompatibility. | [65] |
| 10. | Chlorambucil | [C4MIM][Tf2N] | Hydrophilic inner phase | a. Showed a burst release at first 4 h with excellent antitumor activity against breast cancer cells. b. Exhibited a reduced the toxicity in the zebrafish animal model. | [66] |
| 11. | Photosensitizer | [C12MIM][Br] | Surfactant and drug encapsulating agent | a. High drug-loading and encapsulation efficiency compared with conventional surfactant-containing nanocarriers. b. Higher ability to produce cytotoxic singlet oxygen with a sustained release profile. | [67] |
| 12. | Epirubicin | [P6,6,6,14][Cl] | Drug carrier | a. Exhibited good capability in delivering therapeutic to the sickness sites. b. Significantly decreased the adverse effects. | [68] |
| 13. | DNA | lipid-like ILs | Drug carrier | a. Exhibited efficient gene transfection vectors with excellent biocompatibility. b. Formed cationic bilayers to deliver DNA into the targeted cell. | [69] |
| 14. | Curcumin | [Cho][Ole] | Drug carrier | Significantly enhanced solubility and half-life of drug compared with free drug in water. | [70] |
| 15. | Immunoglobin G4 (IgG4) | [Cho][Cl] | Protein stabilizer | a. Predicted the thermodynamic stability with aggregation propensity of protein IgG4. b. Aggregation propensity reduced with increasing IL concentration. | [53] |
| 16. | Lysozyme (LYZ) | [Cho][Cl], [Cho][DHC] | Protein stabilizer | a. The aggregation behavior varied with ILs. b. ILs enhanced the stabilization of LYZ in the interfacial surface. | [54] |
| 17. | Lysozyme | [C2MIM][Tf2N] | Nonpolar phase of the microemulsion | a. Enhanced the thermal stability of LYZ up to 120 °C. b. Enhanced the enzyme activity with the presence of IL. | [71] |
| 18. | TCN Hydrogel sensor | Polyvinyl-imidazole | Polymeric network of the hydrogel | a. Exhibited excellent strain sensing sensitivity, short response time, high durability, and impressive temperature sensing sensitivity. b. Achieved rapid wound closure and condition monitoring. | [72] |
| 19. | - | Choline-based bio-IL | Tissue scaffold | a. Formed in situ 3D printable bio-ionic ink hydrogel with ILs. b. Improved cellular adhesion and reduced potential fouling with excellent biocompatibility and cell proliferation. | [73] |
| 20. | 5-fluorouracil (5-FLU) Indomethacin (IND) | Sulfonate-ILs | crosslinking agents | a. Exhibited controlled and sustained drug release profiles. b. Stronger interactions of 5-FLU with beads, resulting a slower release than IND after 24h. | [74] |
| 21. | calf thymus DNA | Noscapine-IL | Binding agent | Exhibited a strong and stable binding with the target DNA. | [75] |
| 22. | Etodolac (ETO) | [ProEt][ETO] | Pharmaceuticals | a. Enhanced the solubility in the simulated nasal fluid owing to the ionization of drug. b. Improved the drug retention on the nasal mucosa with enhanced the nose-to-brain delivery. c. Suppressed the production of PGE2 in the intranasal administration. | [76] |
| 23. | Ibuprofen | [AAOR][Ibu] | Pharmaceuticals | a. IBU-ILs does not affect the binding affinity of drug to BSA. b. ILs are practically not toxic. c. ILs effectively bound with BSA. | [77] |
| 24. | Donepezil | dicarboxylic acid-based DPZ | Pharmaceuticals | Exhibited improved aqueous solubility and skin permeability compared to the free drug. | [78] |
| 25. | Ketoprofen | Piperine-based IL | Pharmaceuticals | a. Exhibited enhanced aqueous solubility with excellent permeability across the rat skin. b. IL resulted in a 68% less paw swelling than mixture of free drug. | [79] |
| 26. | Pilocarpine (Pilo) | Pilo- oligo-polyethylene glycol ILs | Pharmaceuticals | a. Exhibited a higher corneal permeability coefficient than the free drug. b. ILs does not show apparent toxicity to human corneal epithelial cells. | [80] |
| 27. | lidocaine (Lid) procaine (Pro) | [Lid], [Pro]:[Sal] | Pharmaceuticals | Exhibited a higher aqueous solubility up to 10-fold compared to the free drug, indicating a potential drug delivery carrier for topical drug delivery. | [81] |
| 28. | Salicylic acid | Betaine-, N-hexyl-nicotinamide-, benzalkonium-Sal | Pharmaceuticals | Exhibited higher antimicrobial activity with a lower cytotoxicity than free salicylic acid | [82] |
| 29. | Salicylic acid | [AAOR][Sal] | Pharmaceuticals | a. Decreased the cytotoxicity toward various type of cells. b. Inhibited the production of the proinflammatory cytokine IL-6 in keratinocytes. | [83] |
| 30. | Metformin (Met) | [Met]:[Ibu] | Pharmaceuticals | Exhibited excellent anti-diabetic and anti-inflammatory activities compared to the parent drugs. | [84] |
| 31. | Lidocaine (Lid) imipramine (Imp) levamisole (Lev) | [Lid]:[Lau], [Ole], [Lin], [Ste] [Imp]:[Lau], [Ole], [Lin], [Ste] [Lev]:[Lau], [Ole], [Lin], [Ste] | Pharmaceuticals | a. Freely miscible in ethanol, N-methyl pyrrolidone, Tween 20, and isopropyl myristate. b. Oleate-based Lev formulation showed 2.6-and 5.4-fold higher in vitro and in vivo skin permeation capability, respectively, than the Lev salts. | [85] |
| 32. | Methotrexate | [MTX]:[Cho], [ProEt], [AspEt], [TMA], [TBP] | Pharmaceuticals | a. Enhanced the aqueous solubility up to 5000-fold more than the free drug. b. ProEt-MTX exhibited 4.6-fold higher oral bioavailability compared to free MTX. c. Significantly reduced systemic toxicity compared to free MTX. | [86,87] |
| 33. | Procaine (Pro) | [Pro]:[Sal], [Ibu], [Doc] | Pharmaceuticals | Significantly increased the aqueous solubility of Sal- and Ibu-based drugs but reduced with Doc anion. | [88] |
| 34. | Favipiravir (Fav) | [Fav]:[Cho], [ProEt], [AlaEt] | Pharmaceuticals | a. Improved aqueous solubility by 78 to 125-fold compared to the free drug. b. Significantly increased the oral bioavailability compared to the free drug. | [89] |
| 35. | Cinnarizine | cinnarizine decanoate | Pharmaceuticals | Significantly enhanced the apparent solubility in lipid solution compared to the free drug. | [90] |
4. Bio-ILs as Active Pharmaceutical Ingredients
5. Drug Delivery Applications of Bio-ILs
5.1. Bio-ILs in Oral Formulation and Delivery
5.2. Bio-ILs in Injection Formulation and Delivery
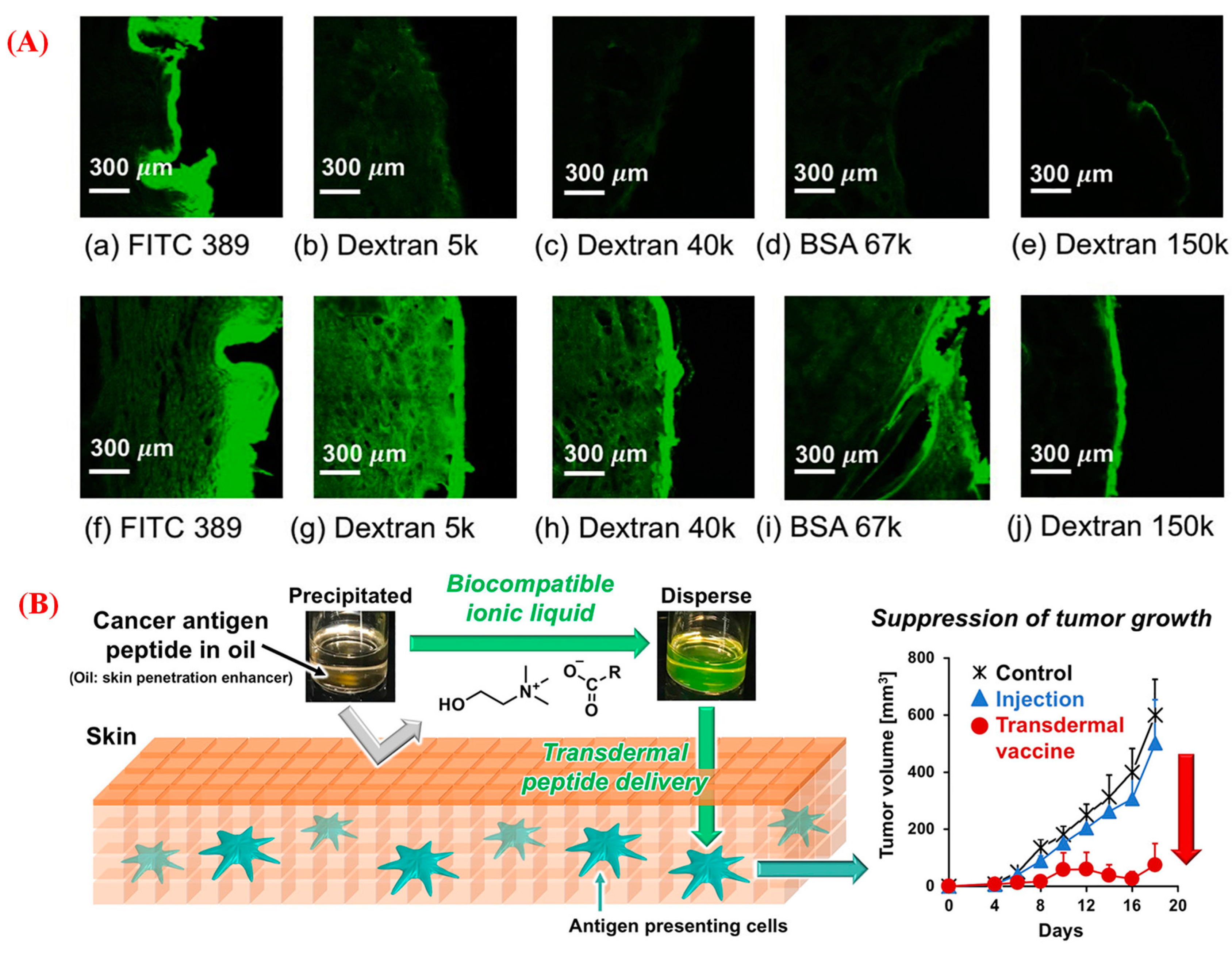
5.3. Bio-ILs in Topical and Transdermal Delivery
5.4. Bio-ILs in Vaccine Formulation and Delivery
| No. | Drug | Role of ILs | Formulation | Main Findings | Ref. |
|---|---|---|---|---|---|
| 1. | Favipiravir (Fav) | [Fav]:[Cho], [ProEt], [AlaEt] as pharmaceuticals | Oral | Significantly increased the oral bioavailability up to 1.9-fold compared to the free drug. | [89] |
| 2. | Paclitaxel (PTX) | Choline oleate as an encapsulating agent | Oral | a. Exhibited higher oral bioavailability of PTX than cremophor EL micelles. b. Showed better stability in the intestinal tract. | [102] |
| 3. | Monoclonal antibodies | choline glycolate as a solubilizing agent | Oral | a. Maintained the stability and structure of TNFα antibody with excellent systemic circulation. b. Significantly improved paracellular antibody transport and reduce the viscosity of the intestinal mucus. | [100] |
| 4. | Insulin Immunoglobulin | CAGE as the solubilizing agents | Oral | a. Significantly enhanced the intestinal absorption of macromolecules. b. Improved the diffusion rates in mucin solution by 4-fold compared with control. | [99] |
| 5. | Methotrexate | [MTX]:[ProEt], [TMA], [Cho], [TBP] as pharmaceuticals | Oral | a. ProEt-MTX exhibited 4.6-fold higher oral bioavailability than MTX sodium. b. Reduced systemic toxicity and suppressed tumor growth better than free MTX. | [86] |
| 6. | Sorafenib | CAGE as a solubilizing agent | Oral | a. Enhanced aqueous solubility by 100 times more than the free drug. b. Improved PK profiles in comparison to parent drug suspension. c. Improved drug accumulation in various organs compared to the control. | [97] |
| 7. | Lumefantrine | lumefantrine docusate as pharmaceutical | Oral | a. Enhanced the solubility in lipid-based vehicles up to 80-fold more than the free drug. b. Exhibited improved plasma exposure up to 35-fold compared to control formulations. | [103] |
| 8. | Insulin | CAGE as a solubilizing agent | Oral | a. Improved paracellular transport up to 10-fold more than native insulin. b. Significantly decreased in blood glucose levels (up to 45%) for longer periods (12 h) compared to injection. | [101] |
| 9. | Protein | CAGE as a solubilizing agent | Injection | a. Considered as a safe, non-toxic formulation b. Enhanced insulin absorption by 200% after subcutaneous injections. b. Reduced the interactions of proteins with the subcutaneous collagen. | [107] |
| 10. | Doxorubicin | CAGE as a solubilizing agent | Injection | a. Led to a consistent tumor ablation in a rabbit liver tumor model for a prolong periods. b. Exhibited in a synergistic cytotoxicity with uniform drug distribution in the ablation zone. | [104] |
| 11. | Paclitaxel | [Cho][Gly] as a solubilizing agent | Injection | a. Exhibited improved antitumor activity with a smaller hypersensitivity effect compared to commercial Taxol formulation. b. Exhibited a similar systemic circulation time, slower elimination rate, and antitumor activity to Taxol. | [106] |
| 12. | Doxorubicin | [C4MIN][PF6] as an agent of the carrier | Injection | a. Exhibited excellent microwave sensitization effects under lower microwave power. b. High inhibition effects in the microwave irradiation. | [105] |
| 13. | Navitoclax (NAVI) | choline octanoate as solubilizing and skin enhancing agent | Topical | a. Exhibited an enhanced skin penetration for an extended period. C. Higher cancer-cell killing efficacy in the topical delivery than oral delivery. | [111] |
| 14. | Thrombin-sensitive nanosensors | CAGE as solubilizing and skin enhancing agent | Topical | a. Provided significant diffusion into the dermis with sustained release into the blood throughout 72 h. b. Released the reporter molecules into the urine by the activation of the clotting cascade. | [44] |
| 15. | Ibuprofen | [Ibu]:[NMP], [Cho] as pharmaceicals | Topical | Exhibited improved skin penetration, and enriched drug accumulation in the target tissue by 2.6 times more than the choline-based drug. | [96] |
| 16. | Framework nucleic acids | [Cho]: carboxylic acid ILs as solubilizing and skin enhancing agents | Topical | a. Exhibited superior structural stability in ILs for a longer period. b. Enhanced FNAs transportation to the lower dermis region in intact, ex vivo porcine skin. | [112] |
| 17. | siRNA | CAGE as solubilizing and skin enhancing agent | Topical | a. Enhanced epidermal and dermal penetration compared with native siRNA. b. Exhibited suppressed GAPDH expression in mice model without toxicity. | [114] |
| 18. | Conotoxins | Matrine oleate | TD | a. High biocompatibility and good fluidity with excellent encapsulation of drug (76%). b. Assisted to penetrate drug across SC barrier and enter the dermis, with a 5.7-fold higher permeability. c. Excellent biocompatibility with improved skin elasticity. | [124] |
| 19. | Levofloxacin | Choline-based poly-IL as drug carrier | TD | a. Exhibited excellent adhesive ability, desirable mechanical properties, and biocompatibility. b. Showed strong antibacterial effect with enhanced transdermal delivery. | [125] |
| 20. | Ovalbumin (OVA) | [EDMPC][Lin] as surfactant and skin enhancing agent | TD | a. Significantly enhanced the transdermal distribution and transdermal flux by 25 and 28-folds, respectively. b. Drastically suppressed tumor growth, and significantly stimulated the OVA-specific tumor immune response in mice model. | [126] |
| 21. | Curcumin | CAGE as solubilizing and skin enhancing agent | TD | a. Significantly enhanced transdermal permeation of curcumin. b. A low percentage of IL was effective in disrupting the skin structure. | [127] |
| 22. | Paclitaxel (PTX) | [Cho][Ole] as surfactant and skin enhancing agent | TD | a. Exhibited a spherical micelles and well-distributed particle size in the range 8.7–25.3 nm. b. Showed 4- and 6-fold higher skin permeation of PTX compared with Tween 80- and ethanol-based formulation, respectively. | [128] |
| 23. | Ovalbumin (OVA) | [Cho][Ole] as surfactant and skin enhancing agent | TD | a. Significantly enhanced the OVA permeation across the skin. b. High level of OVA-specific IgG antibody production with improved tumor growth inhibition compared to the control group. | [129] |
| 24. | Donepezil (DPZ) | dicarboxylic acid-based DPZ as pharmaceutical | TD | Exhibited improved aqueous solubility with excellent skin permeability compared to the free drug. | [78] |
| 25. | Levamisole (Lev) | API-ILs as pharmaceuticals | TD | Oleate-based Lev formulation showed 2.6- and 5.4-fold higher in vitro and in vivo skin permeation capability, respectively, than the Lev salts. | [85] |
| 26. | Gliclazide (Gli) | [Gli][P6,6,6,14] as pharmaceutical | TD | a. Exhibited a sustained release profile with a favorable PK profile in the rat compared to oral suspension. | [130] |
| 27. | Ketoprofen, Flurbiprofen Loxoprofen | Triethylamine-APIs as pharmaceuticals | TD | Exhibited enhanced solubility up to 4.50-fold with high skin penetration compared to control patches. | [131] |
| 28. | Insulin | Choline propionate IL as an internal polar phase and [Cho][Ole] as surfactant and drug encapsulating agent | TD | a. Significantly reduced blood glucose levels compared with a commercial surfactant-based formulation. c. Increased the transdermal bioavailability and sustained the insulin level for a much longer period. | [118] |
| 29. | Peptide | [EDMPC]:[Ole], [Lin], [Ste] as surfactants and skin enhancing agents | TD | a. Significantly increased the formulation stability, drug-loading capacity, and encapsulation efficiency. b. Exhibited increased the transdermal delivery flux by 65-fold compared to the control solution. | [132] |
| 30. | Protein | [EDMPC]:[Lin] as surfactants and skin enhancing agents | Vaccine | a. Significantly increased transdermal drug delivery and anticancer immune responses. b. Stimulated a stronger immune response compared with conventional aqueous formulations. | [133] |
| 31. | Influenza split-virus antigen | Choline niacinate as outer phase of the nano emulsion | Vaccine | a. Exhibited improved stability with a reduced and more uniform particle size. b. Showed induced strong mucosal immune responses by 25- and 5.8-fold higher IgA titers 25- than naked and commercial MF59-adjuvanted antigens, respectively. | [121] |
| 32. | Inactivated foot-and-mouth disease virus antigen | Choline niacinate as outer phase of the nano emulsion | Vaccine | a. IL enhanced the thermostability and long-term stability of the antigen. b. Exhibited improved humoral immune responses in mouse models compared to Montanide ISA 206 adjuvant. | [120] |
| 33. | Ovalbumin | Choline lactate as adjuvant | Vaccine | Maintained the stability and structural integrity of the OVA with enhanced the immune response against the antigen. | [122] |
| 34. | Ovalbumin Imiquimod | [Cho][Ole] as surfactant and imiquimod as adjuvant | Vaccine | a. Significantly enhanced the permeation of the antigenic protein and adjuvant across the skin. b. Exhibited high level of OVA-specific IgG antibody production with excellent tumor growth inhibition compared with the control group. | [129] |
| 35. | Peptide | [Cho]: laurate, oleate as surfactants and skin enhancing agents | Vaccine | a. Exhibited enhanced skin permeation by 28-fold compared with aqueous vehicle. b. Suppressed tumor growth in vivo compared to injection. | [116] |
| 36. | Inactivated foot-and- mouth disease virus (iFMDV) | [Cho]: Phosphate, sulfate, and chloride as stabilizing agents | Vaccine | a. Significantly improved the thermo- and long-term storage stability of iFMDV. b. Not affected the immunogenicity of inactivated iFMDV or immune response in vivo. | [134] |
6. Conclusions and Future Outlooks
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Egorova, K.S.; Gordeev, E.G.; Ananikov, V.P.; Zelinsky, N.D. Biological Activity of Ionic Liquids and Their Application in Pharmaceutics and Medicine. Chem. Rev. 2017, 117, 7132–7189. [Google Scholar] [CrossRef]
- Huang, W.; Wu, X.; Qi, J.; Zhu, Q.; Wu, W.; Lu, Y.; Chen, Z. Ionic Liquids: Green and Tailor-Made Solvents in Drug Delivery. Drug Discov. Today 2020, 25, 901–908. [Google Scholar] [CrossRef] [PubMed]
- Cue, B.W.; Zhang, J. Green Process Chemistry in the Pharmaceutical Industry. Green Chem. Lett. Rev. 2009, 2, 193–211. [Google Scholar] [CrossRef]
- Welton, T. Ionic Liquids: A Brief History. Biophys. Rev. 2018, 10, 691–706. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.K.; Savoy, A.W. Ionic Liquids Synthesis and Applications: An Overview. J. Mol. Liq. 2020, 297, 112038. [Google Scholar] [CrossRef]
- Sanches, M.V.; Freitas, R.; Oliva, M.; Cuccaro, A.; Monni, G.; Mezzetta, A.; Guazzelli, L.; Pretti, C. Toxicity of Ionic Liquids in Marine and Freshwater Microorganisms and Invertebrates: State of the Art. Environ. Sci. Pollut Res. 2023, 30, 39288–39318. [Google Scholar] [CrossRef]
- Dias, A.R.; Costa-Rodrigues, J.; Fernandes, M.H.; Ferraz, R.; Prudêncio, C. The Anticancer Potential of Ionic Liquids. ChemMedChem 2017, 12, 11–18. [Google Scholar] [CrossRef]
- Jaitely, V.; Florence, A.T. Water-Immiscible Room Temperature Ionic Liquids (RTILs) as Drug Reservoirs for Controlled Release. Int. J. Pharm. 2008, 354, 168–173. [Google Scholar] [CrossRef]
- Sheldon, R.A. Biocatalysis and Biomass Conversion in Alternative Reaction Media. Chem. Eur. J. 2016, 22, 12984–12999. [Google Scholar] [CrossRef]
- Hough, W.L.; Smiglak, M.; Rodríguez, H.; Swatloski, R.P.; Spear, S.K.; Daly, D.T.; Pernak, J.; Grisel, J.E.; Carliss, R.D.; Soutullo, M.D.; et al. The Third Evolution of Ionic Liquids: Active Pharmaceutical Ingredients. New J. Chem. 2007, 31, 1429–1436. [Google Scholar] [CrossRef]
- Dias, A.R.; Costa-Rodrigues, J.; Teixeira, C.; Prudêncio, C.; Gomes, P.; Ferraz, R. Ionic Liquids for Topical Delivery in Cancer. Curr. Med. Chem. 2018, 26, 7520–7532. [Google Scholar] [CrossRef]
- El Achkar, T.; Greige-Gerges, H.; Fourmentin, S. Basics and Properties of Deep Eutectic Solvents: A Review. Environ. Chem. Lett. 2021, 19, 3397–3408. [Google Scholar] [CrossRef]
- Płotka-Wasylka, J.; de la Guardia, M.; Andruch, V.; Vilková, M. Deep Eutectic Solvents vs. Ionic Liquids: Similarities and Differences. Microchem. J. 2020, 159, 105539. [Google Scholar] [CrossRef]
- Gomes, J.M.; Silva, S.S.; Reis, R.L. Biocompatible Ionic Liquids: Fundamental Behaviours and Applications. Chem. Soc. Rev. 2019, 48, 4317–4335. [Google Scholar] [CrossRef]
- Flieger, J.; Feder-Kubis, J.; Tatarczak-Michalewska, M. Chiral Ionic Liquids: Structural Diversity, Properties and Applications in Selected Separation Techniques. Int. J. Mol. Sci. 2020, 21, 4253. [Google Scholar] [CrossRef] [PubMed]
- Feder-Kubis, J.; Flieger, J.; Tatarczak-Michalewska, M.; Płazińska, A.; Madejska, A.; Swatko-Ossor, M. Renewable Sources from Plants as the Starting Material for Designing New Terpene Chiral Ionic Liquids Used for the Chromatographic Separation of Acidic Enantiomers. RSC Adv. 2017, 7, 32344–32356. [Google Scholar] [CrossRef]
- Flieger, J.; Feder-Kubis, J.; Tatarczak-Michalewska, M.; Płazińska, A.; Madejska, A.; Swatko-Ossor, M. Natural Terpene Derivatives as New Structural Task-Specific Ionic Liquids to Enhance the Enantiorecognition of Acidic Enantiomers on Teicoplanin-Based Stationary Phase by High-Performance Liquid Chromatography. J. Sep. Sci. 2017, 40, 2374–2381. [Google Scholar] [CrossRef]
- Li, X.; Ma, N.; Zhang, L.; Ling, G.; Zhang, P. Applications of Choline-Based Ionic Liquids in Drug Delivery. Int. J. Pharm. 2022, 612, 121366. [Google Scholar] [CrossRef] [PubMed]
- Zeisel, S.H.; Da Costa, K.A. Choline: An Essential Nutrient for Public Health. Nutr. Rev. 2009, 67, 615–623. [Google Scholar] [CrossRef]
- Moriel, P.; García-Suárez, E.J.; Martínez, M.; García, A.B.; Montes-Morán, M.A.; Calvino-Casilda, V.; Bañares, M.A. Synthesis, Characterization, and Catalytic Activity of Ionic Liquids Based on Biosources. Tetrahedron Lett. 2010, 51, 4877–4881. [Google Scholar] [CrossRef]
- Foulet, A.; Ghanem, O.B.; El-Harbawi, M.; Lévêque, J.M.; Mutalib, M.I.A.; Yin, C.Y. Understanding the Physical Properties, Toxicities and Anti-Microbial Activities of Choline-Amino Acid-Based Salts: Low-Toxic Variants of Ionic Liquids. J. Mol. Liq. 2016, 221, 133–138. [Google Scholar] [CrossRef]
- Chowdhury, M.R.; Moshikur, R.M.; Wakabayashi, R.; Tahara, Y.; Kamiya, N.; Moniruzzaman, M.; Goto, M. Ionic-Liquid-Based Paclitaxel Preparation: A New Potential Formulation for Cancer Treatment. Mol. Pharm. 2018, 15, 2484–2488. [Google Scholar] [CrossRef]
- Tanner, E.E.L.; Curreri, A.M.; Balkaran, J.P.R.; Selig-Wober, N.C.; Yang, A.B.; Kendig, C.; Fluhr, M.P.; Kim, N.; Mitragotri, S. Design Principles of Ionic Liquids for Transdermal Drug Delivery. Adv. Mater. 2019, 31, 1901103. [Google Scholar] [CrossRef]
- Moshikur, R.M.; Ali, M.K.; Wakabayashi, R.; Moniruzzaman, M.; Goto, M. Formation and Potential Application of Micelles Composed of Biocompatible N-Lauroyl-Amino Acid Ionic Liquids Surfactant. J. Mol. Liq. 2020, 320, 114424. [Google Scholar] [CrossRef]
- Pedro, A.Q.; Pereira, P.; Quental, M.J.; Carvalho, A.P.; Santos, S.M.; Queiroz, J.A.; Sousa, F.; Freire, M.G. Cholinium-Based Good’s Buffers Ionic Liquids as Remarkable Stabilizers and Recyclable Preservation Media for Recombinant Small RNAs. ACS Sustain. Chem. Eng. 2018, 6, 16645–16656. [Google Scholar] [CrossRef] [PubMed]
- Ali, M.K.; Moshikur, R.M.; Wakabayashi, R.; Tahara, Y.; Moniruzzaman, M.; Kamiya, N.; Goto, M. Synthesis and Characterization of Choline–Fatty-Acid-Based Ionic Liquids: A New Biocompatible Surfactant. J. Colloid Interface Sci. 2019, 551, 72–80. [Google Scholar] [CrossRef] [PubMed]
- Md Moshikur, R.; Chowdhury, M.R.; Fujisawa, H.; Wakabayashi, R.; Moniruzzaman, M.; Goto, M. Design and Characterization of Fatty Acid-Based Amino Acid Ester as a New “Green” Hydrophobic Ionic Liquid for Drug Delivery. ACS Sustain. Chem. Eng. 2020, 8, 13660–13671. [Google Scholar] [CrossRef]
- Zhang, L.; He, L.; Hong, C.B.; Qin, S.; Tao, G.H. Brønsted Acidity of Bio-Protic Ionic Liquids: The Acidic Scale of [AA]X Amino Acid Ionic Liquids. Green Chem. 2015, 17, 5154–5163. [Google Scholar] [CrossRef]
- Furukawa, S.; Hattori, G.; Sakai, S.; Kamiya, N. Highly Efficient and Low Toxic Skin Penetrants Composed of Amino Acid Ionic Liquids. RSC Adv. 2016, 6, 87753–87755. [Google Scholar] [CrossRef]
- Moshikur, R.M.; Chowdhury, M.R.; Wakabayashi, R.; Tahara, Y.; Moniruzzaman, M.; Goto, M. Characterization and Cytotoxicity Evaluation of Biocompatible Amino Acid Esters Used to Convert Salicylic Acid into Ionic Liquids. Int. J. Pharm. 2018, 546, 31–38. [Google Scholar] [CrossRef] [PubMed]
- Shimul, I.M.; Moshikur, R.M.; Minamihata, K.; Moniruzzaman, M.; Kamiya, N.; Goto, M. Amino Acid Ester Based Phenolic Ionic Liquids as a Potential Solvent for the Bioactive Compound Luteolin: Synthesis, Characterization, and Food Preservation Activity. J. Mol. Liq. 2022, 349, 118103. [Google Scholar] [CrossRef]
- Pereira, M.M.; Almeida, M.R.; Gomes, J.; Rufino, A.F.C.S.; Rosa, M.E.; Coutinho, J.A.P.; Mohamadou, A.; Freire, M.G. Glycine-Betaine Ionic Liquid Analogues as Novel Phase-Forming Components of Aqueous Biphasic Systems. Biotechnol. Prog. 2018, 34, 1205–1212. [Google Scholar] [CrossRef] [PubMed]
- Moshikur, R.; Ali, K.; Goto, M. Ionic Liquids for Increasing the Solubility of Sparingly Soluble Drug Molecules. In Application of Ionic Liquids in Drug Delivery; Goto, M., Moniruzzaman, M., Eds.; Springer: Singapore, 2021; pp. 51–70. [Google Scholar] [CrossRef]
- Agostinho, D.A.S.; Jesus, A.R.; Silva, A.B.P.; Esperança, J.M.S.S.; Paiva, A.; Duarte, A.R.C.; Reis, P.M. Improvement of New Dianionic Ionic Liquids vs. Monoanionic in Solubility of Poorly Water-Soluble Drugs. J. Pharm. Sci. 2021, 110, 2489–2500. [Google Scholar] [CrossRef]
- Hattori, T.; Tagawa, H.; Inai, M.; Kan, T.; Kimura, S.I.; Itai, S.; Mitragotri, S.; Iwao, Y. Transdermal Delivery of Nobiletin Using Ionic Liquids. Sci. Rep. 2019, 9, 20191. [Google Scholar] [CrossRef]
- Islam, M.R.; Chowdhury, M.R.; Wakabayashi, R.; Tahara, Y.; Kamiya, N.; Moniruzzaman, M.; Goto, M. Choline and Amino Acid Based Biocompatible Ionic Liquid Mediated Transdermal Delivery of the Sparingly Soluble Drug Acyclovir. Int. J. Pharm. 2020, 582, 119335. [Google Scholar] [CrossRef]
- Lotfi, M.; Moniruzzaman, M.; Sivapragasam, M.; Kandasamy, S.; Abdul Mutalib, M.I.; Alitheen, N.B.; Goto, M. Solubility of Acyclovir in Nontoxic and Biodegradable Ionic Liquids: COSMO-RS Prediction and Experimental Verification. J. Mol. Liq. 2017, 243, 124–131. [Google Scholar] [CrossRef]
- Cláudio, A.F.M.; Neves, M.C.; Shimizu, K.; Canongia Lopes, J.N.; Freire, M.G.; Coutinho, J.A.P. The Magic of Aqueous Solutions of Ionic Liquids: Ionic Liquids as a Powerful Class of Catanionic Hydrotropes. Green Chem. 2015, 17, 3948–3963. [Google Scholar] [CrossRef] [PubMed]
- Md Moshikur, R.; Chowdhury, M.R.; Moniruzzaman, M.; Goto, M. Biocompatible Ionic Liquids and Their Applications in Pharmaceutics. Green Chem. 2020, 22, 8116–8139. [Google Scholar] [CrossRef]
- Ali, M.K.; Moshikur, R.M.; Goto, M.; Moniruzzaman, M. Recent Developments in Ionic Liquid-Assisted Topical and Transdermal Drug Delivery. Pharm. Res. 2022, 39, 2335–2351. [Google Scholar] [CrossRef]
- Gupta, R.; Dwadasi, B.S.; Rai, B.; Mitragotri, S. Effect of Chemical Permeation Enhancers on Skin Permeability: In Silico Screening Using Molecular Dynamics Simulations. Sci. Rep. 2019, 9, 1456. [Google Scholar] [CrossRef]
- Monti, D.; Egiziano, E.; Burgalassi, S.; Chetoni, P.; Chiappe, C.; Sanzone, A.; Tampucci, S. Ionic Liquids as Potential Enhancers for Transdermal Drug Delivery. Int. J. Pharm. 2017, 516, 45–51. [Google Scholar] [CrossRef]
- Zakrewsky, M.; Lovejoy, K.S.; Kern, T.L.; Miller, T.E.; Le, V.; Nagy, A.; Goumas, A.M.; Iyer, R.S.; Del Sesto, R.E.; Koppisch, A.T.; et al. Ionic Liquids as a Class of Materials for Transdermal Delivery and Pathogen Neutralization. Proc. Natl. Acad. Sci. USA 2014, 111, 13313–13318. [Google Scholar] [CrossRef] [PubMed]
- Bekdemir, A.; Tanner, E.E.L.; Kirkpatrick, J.; Soleimany, A.P.; Mitragotri, S.; Bhatia, S.N. Ionic Liquid-Mediated Transdermal Delivery of Thrombosis-Detecting Nanosensors. Adv. Healthc. Mater. 2022, 11, 2102685. [Google Scholar] [CrossRef]
- Wu, X.; Zhang, H.; He, S.; Yu, Q.; Lu, Y.; Wu, W.; Ding, N.; Zhu, Q.; Chen, Z.; Ma, Y.; et al. Improving Dermal Delivery of Hyaluronic Acid by Ionic Liquids for Attenuating Skin Dehydration. Int. J. Biol. Macromol. 2020, 150, 528–535. [Google Scholar] [CrossRef] [PubMed]
- Qi, Q.M.; Duffy, M.; Curreri, A.M.; Balkaran, J.P.R.; Tanner, E.E.L.; Mitragotri, S. Comparison of Ionic Liquids and Chemical Permeation Enhancers for Transdermal Drug Delivery. Adv. Funct. Mater. 2020, 30, 2004257. [Google Scholar] [CrossRef]
- Yang, D.; Liu, C.; Ding, D.; Quan, P.; Fang, L. The Molecular Design of Drug-Ionic Liquids for Transdermal Drug Delivery: Mechanistic Study of Counterions Structure on Complex Formation and Skin Permeation. Int. J. Pharm. 2021, 602, 120560. [Google Scholar] [CrossRef]
- Zhang, Y.; Cao, Y.; Meng, X.; Li, C.; Wang, H.; Zhang, S. Enhancement of Transdermal Delivery of Artemisinin Using Microemulsion Vehicle Based on Ionic Liquid and Lidocaine Ibuprofen. Colloids Surf. B Biointerfaces 2020, 189, 110886. [Google Scholar] [CrossRef] [PubMed]
- Mandal, A.; Kumbhojkar, N.; Reilly, C.; Dharamdasani, V.; Ukidve, A.; Ingber, D.E.; Mitragotri, S. Treatment of Psoriasis with NFKBIZ SiRNA Using Topical Ionic Liquid Formulations. Sci. Adv. 2020, 6, eabb6049. [Google Scholar] [CrossRef]
- Veríssimo, N.V.; Vicente, F.A.; de Oliveira, R.C.; Likozar, B.; de Souza Oliveira, R.P.; Pereira, J.F.B. Ionic Liquids as Protein Stabilizers for Biological and Biomedical Applications: A Review. Biotechnol. Adv. 2022, 61, 108055. [Google Scholar] [CrossRef]
- Elgharbawy, A.A.M.; Moniruzzaman, M.; Goto, M. Recent Advances of Enzymatic Reactions in Ionic Liquids: Part II. Biochem. Eng. J. 2020, 154, 107426. [Google Scholar] [CrossRef]
- Ali, K.; Moshikur, R.; Goto, M. Surface-Active Ionic Liquids for Medical and Pharmaceutical Applications. In Appplication of Ionic Liquids in Drug Delivery; Goto, M., Moniruzzaman, M., Eds.; Springer: Singapore, 2021; pp. 165–186. [Google Scholar] [CrossRef]
- Shmool, T.A.; Martin, L.K.; Matthews, R.P.; Hallett, J.P. Ionic Liquid-Based Strategy for Predicting Protein Aggregation Propensity and Thermodynamic Stability. J. Am. Chem. Soc. 2022, 2, 2068–2080. [Google Scholar] [CrossRef]
- Sharma, A.; Mondal, S.; Ahuja, T.; Karmakar, T.; Siddhanta, S. Ion-Mediated Protein Stabilization on Nanoscopic Surfaces. Langmuir 2022, 39, 1227–1237. [Google Scholar] [CrossRef]
- Bisht, M.; Venkatesu, P. Influence of Cholinium-Based Ionic Liquids on the Structural Stability and Activity of α-Chymotrypsin. New J. Chem. 2017, 41, 13902–13911. [Google Scholar] [CrossRef]
- Singh, G.; Kaur, M.; Kaur, H.; Kang, T.S. Synthesis and Complexation of a New Caffeine Based Surface Active Ionic Liquid with Lysozyme in Aqueous Medium: Physicochemical, Computational and Antimicrobial Studies. J. Mol. Liq. 2021, 325, 115156. [Google Scholar] [CrossRef]
- Nikfarjam, N.; Ghomi, M.; Agarwal, T.; Hassanpour, M.; Sharifi, E.; Khorsandi, D.; Ali Khan, M.; Rossi, F.; Rossetti, A.; Nazarzadeh Zare, E.; et al. Antimicrobial Ionic Liquid-Based Materials for Biomedical Applications. Adv. Funct. Mater. 2021, 31, 2104148. [Google Scholar] [CrossRef]
- Benedetto, A.; Heinrich, F.; Gonzalez, M.A.; Fragneto, G.; Watkins, E.; Ballone, P. Structure and Stability of Phospholipid Bilayers Hydrated by a Room-Temperature Ionic Liquid/Water Solution: A Neutron Reflectometry Study. J. Phys. Chem. B 2014, 118, 12192–12206. [Google Scholar] [CrossRef]
- Han, T.H.; Lee, J.D.; Seo, B.C.; Jeon, W.H.; Yang, H.A.; Kim, S.; Haam, K.; Park, M.K.; Park, J.; Han, T.S.; et al. Cancer-Specific Cytotoxicity of Pyridinium-Based Ionic Liquids by Regulating Hypoxia-Inducible Factor-1α-Centric Cancer Metabolism. Ecotoxicol. Environ. Saf. 2022, 248, 114334. [Google Scholar] [CrossRef] [PubMed]
- Grassiri, B.; Mezzetta, A.; Maisetta, G.; Migone, C.; Fabiano, A.; Esin, S.; Guazzelli, L.; Zambito, Y.; Batoni, G.; Piras, A.M. Betaine- and L-Carnitine-Based Ionic Liquids as Solubilising and Stabilising Agents for the Formulation of Antimicrobial Eye Drops Containing Diacerein. Int. J. Mol. Sci. 2023, 24, 2714. [Google Scholar] [CrossRef] [PubMed]
- Alves, M.M.S.; Melo, M.N.; Mertens, H.D.T.; Pereiro, A.B.; Archer, M. Studies on the Interaction between Model Proteins and Fluorinated Ionic Liquids. Pharmaceutics 2023, 15, 157. [Google Scholar] [CrossRef]
- Shimul, I.M.; Moshikur, R.M.; Minamihata, K.; Moniruzzaman, M.; Kamiya, N.; Goto, M. Choline Oleate Based Micellar System as a New Approach for Luteolin Formulation: Antioxidant, Antimicrobial, and Food Preservation Properties Evaluation. J. Mol. Liq. 2022, 365, 120151. [Google Scholar] [CrossRef]
- Sintra, T.E.; Abranches, D.O.; Benfica, J.; Soares, B.P.; Ventura, S.P.M.; Coutinho, J.A.P. Cholinium-Based Ionic Liquids as Bioinspired Hydrotropes to Tackle Solubility Challenges in Drug Formulation. Eur. J. Pharm. Biopharm. 2021, 164, 86–92. [Google Scholar] [CrossRef]
- Agostinho, D.A.S.; Santos, F.; Esperança, J.M.S.S.; Duarte, A.R.C.; Reis, P.M. New Non-Toxic Biocompatible Dianionic Ionic Liquids That Enhance the Solubility of Oral Drugs from BCS Class II. J. Ion. Liq. 2021, 1, 100003. [Google Scholar] [CrossRef]
- Pandey, D.K.; Kuddushi, M.; Kumar, A.; Singh, D.K. Iron Oxide Nanoparticles Loaded Smart Hybrid Hydrogel for Anti-Inflammatory Drug Delivery: Preparation and Characterizations. Colloids Surf. A Physicochem. Eng. Asp. 2022, 650, 129631. [Google Scholar] [CrossRef]
- Akdogan, Y.; Cigdem Sozer, S.; Akyol, C.; Basol, M.; Karakoyun, C.; Cakan-Akdogan, G. Synthesis of Albumin Nanoparticles in a Water-Miscible Ionic Liquid System, and Their Applications for Chlorambucil Delivery to Cancer Cells. J. Mol. Liq. 2022, 367, 120575. [Google Scholar] [CrossRef]
- Regina Ebani, P.; Stefanello, L.; Luiza Kuhn, B.; Piccinin Frizzo, C.; Augusto Lima Burgo, T.; Luisa Kloster, C.; Antonio Villetti, M. Carboxymethyl Chitosan/Ionic Liquid Imidazolium-Based Nanoparticles as Nanocarriers for Zinc Phthalocyanine and Its Photodynamic Activity. J. Mol. Liq. 2021, 336, 116874. [Google Scholar] [CrossRef]
- Dalvand, K.; Ghiasvand, A.; Gupta, V.; Paull, B. Chemotaxis-Based Smart Drug Delivery of Epirubicin Using a 3D Printed Microfluidic Chip. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2021, 1162, 122456. [Google Scholar] [CrossRef]
- Siegel, D.J.; Anderson, G.I.; Paul, L.M.; Seibert, P.J.; Hillesheim, P.C.; Sheng, Y.; Zeller, M.; Taubert, A.; Werner, P.; Balischewski, C.; et al. Design Principles of Lipid-like Ionic Liquids for Gene Delivery. ACS Appl. Bio Mater. 2021, 6, 4737–4743. [Google Scholar] [CrossRef]
- Chowdhury, M.R.; Moshikur, R.M.; Wakabayashi, R.; Tahara, Y.; Kamiya, N.; Moniruzzaman, M.; Goto, M. Development of a Novel Ionic Liquid-Curcumin Complex to Enhance Its Solubility, Stability, and Activity. Chem. Commun. 2019, 55, 7737–7740. [Google Scholar] [CrossRef]
- Kaur, M.; Singh, G.; Kaur, A.; Sharma, P.K.; Kang, T.S. Thermally Stable Ionic Liquid-Based Microemulsions for High-Temperature Stabilization of Lysozyme at Nanointerfaces. Langmuir 2019, 35, 4085–4093. [Google Scholar] [CrossRef]
- Qu, X.; Liu, J.; Wang, S.; Shao, J.; Wang, Q.; Wang, W.; Gan, L.; Zhong, L.; Dong, X.; Zhao, Y. Photothermal Regulated Multi-Perceptive Poly(Ionic Liquids) Hydrogel Sensor for Bioelectronics. Chem. Eng. J. 2023, 453, 139785. [Google Scholar] [CrossRef]
- Krishnadoss, V.; Kanjilal, B.; Masoumi, A.; Banerjee, A. Programmable Bio-Ionic Liquid Functionalized Hydrogels for in Situ 3D Bioprinting of Electronics at the Tissue Interface. Mater. Today Adv. 2023, 17, 100352. [Google Scholar] [CrossRef]
- Silva, B.E.M.; Jesus, L.T.; Freire, R.O.; Cassol, T.M.; Júnior, S.A. Sulfonate-Functionalized Ionic Liquids for PH-Sensitive Alginate Beads Preparation: Macromolecular Structure Study and Drug Release Evaluation. Mater. Chem. Phys. 2023, 293, 126957. [Google Scholar] [CrossRef]
- Sehrawat, H.; Kumar, N.; Panchal, S.; Kumar, L.; Chandra, R. Imperative Persistent Interaction Analysis of Anticancer Noscapine-Ionic Liquid with Calf Thymus DNA. Int. J. Biol. Macromol. 2022, 220, 415–425. [Google Scholar] [CrossRef] [PubMed]
- Tanigawa, H.; Suzuki, N.; Suzuki, T. Application of Ionic Liquid to Enhance the Nose-to-Brain Delivery of Etodolac. Eur. J. Pharm. Sci. 2022, 178, 106290. [Google Scholar] [CrossRef] [PubMed]
- Ossowicz-Rupniewska, P.; Klebeko, J.; Świątek, E.; Szachnowska, J.; Janus, E.; Rangelov, M.; Todorova, N.; Taneva, S.G.; Krachmarova, E.; Guncheva, M. Binding Behavior of Ibuprofen-Based Ionic Liquids with Bovine Serum Albumin: Thermodynamic and Molecular Modeling Studies. J. Mol. Liq. 2022, 360, 119367. [Google Scholar] [CrossRef]
- Dinh, L.; Lee, S.; Abuzar, S.M.; Park, H.; Hwang, S.J. Formulation, Preparation, Characterization, and Evaluation of Dicarboxylic Ionic Liquid Donepezil Transdermal Patches. Pharmaceutics 2022, 14, 205. [Google Scholar] [CrossRef] [PubMed]
- Hassan, S.A.; Gad, S.F.; Abdu-Allah, H.H.M.; Qayed, W.S.; AbouElmagd, S.A.; Ibrahim, E.A. Ionic Liquid of Ketoprofen-Piperine Modulates the Pharmaceutical and Therapeutic Characters of Ketoprofen. Int. J. Pharm. 2022, 620, 121724. [Google Scholar] [CrossRef]
- Wang, J.; Li, B.; Tang, J.; Qiu, L.; Qiao, X.; Xu, N.; Yang, H. Ionic Liquid Pilocarpine Analog as an Antiglaucoma Drug Candidate. ACS Pharmacol. Transl. Sci. 2022, 5, 752–760. [Google Scholar] [CrossRef]
- Panić, J.; Vraneš, M.; Mirtič, J.; Cerc Korošec, R.; Zupančič, Š.; Gadžurić, S.; Kristl, J.; Bešter-Rogač, M. Preparation and Characterization of Innovative Electrospun Nanofibers Loaded with Pharmaceutically Applicable Ionic Liquids. Int. J. Pharm. 2022, 615, 121510. [Google Scholar] [CrossRef]
- Dobler, D.; Schmidts, T.; Merzhäuser, M.; Schlupp, P.; Runkel, F. Salicylate-Based Ionic Liquids as Innovative Ingredients in Dermal Formulations. J. Pharm. Sci. 2022, 111, 1414–1420. [Google Scholar] [CrossRef]
- Klebeko, J.; Ossowicz-Rupniewska, P.; Świątek, E.; Szachnowska, J.; Janus, E.; Taneva, S.G.; Krachmarova, E.; Guncheva, M. Salicylic Acid as Ionic Liquid Formulation May Have Enhanced Potency to Treat Some Chronic Skin Diseases. Molecules 2022, 27, 216. [Google Scholar] [CrossRef] [PubMed]
- Safna Hussan, K.P.; Pareeth, C.M.; Muraleedharan, K.; Shahin Thayyil, M.; Babu, T.D. Synthesis, Spectroscopic, Chemical Reactivity, Molecular Docking, DFT Calculations and in-Vitro Anticancer Activity Studies of a Novel Ionic Liquid; Metforminium Ibuprofenate. J. Mol. Liq. 2022, 364, 120046. [Google Scholar] [CrossRef]
- Md Moshikur, R.; Shimul, I.M.; Uddin, S.; Wakabayashi, R.; Moniruzzaman, M.; Goto, M. Transformation of Hydrophilic Drug into Oil-Miscible Ionic Liquids for Transdermal Drug Delivery. ACS Appl. Mater. Interfaces 2022, 14, 55332–55341. [Google Scholar] [CrossRef] [PubMed]
- Moshikur, R.M.; Ali, M.K.; Wakabayashi, R.; Moniruzzaman, M.; Goto, M. Methotrexate-Based Ionic Liquid as a Potent Anticancer Drug for Oral Delivery: In Vivo Pharmacokinetics, Biodistribution, and Antitumor Efficacy. Int. J. Pharm. 2021, 608, 121129. [Google Scholar] [CrossRef] [PubMed]
- Moshikur, R.M.; Chowdhury, M.R.; Wakabayashi, R.; Tahara, Y.; Moniruzzaman, M.; Goto, M. Ionic Liquids with Methotrexate Moieties as a Potential Anticancer Prodrug: Synthesis, Characterization and Solubility Evaluation. J. Mol. Liq. 2019, 278, 226–233. [Google Scholar] [CrossRef]
- Bonkovoski, L.C.; Vilsinski, B.H.; Panice, M.R.; Nunes, C.S.; Braga, G.; Lazarin-Bidóia, D.; Nakamura, C.V.; Martins, A.F.; Muniz, E.C. Cytocompatible Drug Delivery Devices Based on Poly[(2-Dimethylamino) Ethyl Methacrylate]/Chondroitin Sulfate Polyelectrolyte Complexes Prepared in Ionic Liquids. J. Drug Deliv. Sci. Technol. 2021, 63, 102520. [Google Scholar] [CrossRef]
- Moshikur, R.M.; Ali, M.K.; Wakabayashi, R.; Moniruzzaman, M.; Goto, M. Favipiravir-Based Ionic Liquids as Potent Antiviral Drugs for Oral Delivery: Synthesis, Solubility, and Pharmacokinetic Evaluation. Mol. Pharm. 2021, 18, 3108–3115. [Google Scholar] [CrossRef]
- Lai, A.; Sahbaz, Y.; Ford, L.; Nguyen, T.H.; Haque, S.; Williams, H.D.; Benameur, H.; Scammells, P.J.; Porter, C.J.H. Stabilising Disproportionation of Lipophilic Ionic Liquid Salts in Lipid-Based Formulations. Int. J. Pharm. 2021, 597, 120292. [Google Scholar] [CrossRef]
- Moshikur, R.; Goto, M. Ionic Liquids as Active Pharmaceutical Ingredients (APIs). In Application of Ionic Liquids in Drug Delivery; Goto, M., Moniruzzaman, M., Eds.; Springer: Singapore, 2021; pp. 13–33. [Google Scholar] [CrossRef]
- Yoshizawa, M.; Xu, W.; Angell, C.A. Ionic Liquids by Proton Transfer: Vapor Pressure, Conductivity, and the Relevance of ΔpKa from Aqueous Solutions. J. Am. Chem. Soc. 2003, 125, 15411–15419. [Google Scholar] [CrossRef]
- Wu, X.; Zhu, Q.; Chen, Z.; Wu, W.; Lu, Y.; Qi, J. Ionic Liquids as a Useful Tool for Tailoring Active Pharmaceutical Ingredients. J. Control. Release 2021, 338, 268–283. [Google Scholar] [CrossRef]
- Stocker, M.W.; Tsolaki, E.; Harding, M.J.; Healy, A.M.; Ferguson, S.; Healy, A.M.; Ferguson, S.; Isolation-free, C. Combining Isolation-Free and Co-processing Manufacturing Approaches to Access Room Temperature Ionic Liquid Forms of APIs. J. Pharm. Sci. 2023. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Q.H.; Zhang, G.H.; He, L.; Qin, S.; Tian, J.H.; Ma, L.; Tao, G.H. Enhanced Solubility and Antitumor Activity of Curcumin via Breaking and Rebuilding of the Hydrogen Bond. ACS Appl. Bio Mater. 2021, 4, 918–927. [Google Scholar] [CrossRef]
- Moshikur, R.M.; Chowdhury, M.R.; Wakabayashi, R.; Tahara, Y.; Kamiya, N.; Moniruzzaman, M.; Goto, M. Ionic Liquids with N-Methyl-2-Pyrrolidonium Cation as an Enhancer for Topical Drug Delivery: Synthesis, Characterization, and Skin-Penetration Evaluation. J. Mol. Liq. 2020, 299, 112166. [Google Scholar] [CrossRef]
- Shi, Y.; Zhao, Z.; Gao, Y.; Pan, D.C.; Salinas, A.K.; Tanner, E.E.L.; Guo, J.; Mitragotri, S. Oral Delivery of Sorafenib through Spontaneous Formation of Ionic Liquid Nanocomplexes. J. Control. Release 2020, 322, 602–609. [Google Scholar] [CrossRef]
- Zhang, W.X.; Gao, Y.R.; Xue, R.; Nguyen, W.; Chen, W.; Wang, J.H.; Shu, Y. Liquid Formulations Based on Ionic Liquids in Biomedicine. Mater. Today Phys. 2023, 30, 100925. [Google Scholar] [CrossRef]
- Peng, K.; Gao, Y.; Angsantikul, P.; LaBarbiera, A.; Goetz, M.; Curreri, A.M.; Rodrigues, D.; Tanner, E.E.L.; Mitragotri, S. Modulation of Gastrointestinal Mucus Properties with Ionic Liquids for Drug Delivery. Adv. Healthc. Mater. 2021, 10, 2002192. [Google Scholar] [CrossRef]
- Angsantikul, P.; Peng, K.; Curreri, A.M.; Chua, Y.; Chen, K.Z.; Ehondor, J.; Mitragotri, S. Ionic Liquids and Deep Eutectic Solvents for Enhanced Delivery of Antibodies in the Gastrointestinal Tract. Adv. Funct. Mater. 2021, 31, 2002912. [Google Scholar] [CrossRef]
- Banerjee, A.; Ibsen, K.; Brown, T.; Chen, R.; Agatemor, C.; Mitragotri, S. Ionic Liquids for Oral Insulin Delivery. Proc. Natl. Acad. Sci. USA 2018, 115, 7296–7301. [Google Scholar] [CrossRef]
- Zheng, X.; Fang, Z.; Huang, W.; Qi, J.; Dong, X.; Zhao, W.; Wu, W.; Lu, Y. Ionic Co-Aggregates (ICAs) Based Oral Drug Delivery: Solubilization and Permeability Improvement. Acta Pharm. Sin. B 2022, 12, 3972–3985. [Google Scholar] [CrossRef]
- Tay, E.; Nguyen, T.H.; Ford, L.; Williams, H.D.; Benameur, H.; Scammells, P.J.; Porter, C.J.H. Ionic Liquid Forms of the Antimalarial Lumefantrine in Combination with LFCS Type IIIB Lipid-Based Formulations Preferentially Increase Lipid Solubility, in Vitro Solubilization Behavior and in Vivo Exposure. Pharmaceutics 2020, 12, 17. [Google Scholar] [CrossRef]
- Albadawi, H.; Zhang, Z.; Altun, I.; Hu, J.; Jamal, L.; Ibsen, K.N.; Tanner, E.E.L.; Mitragotri, S.; Oklu, R. Percutaneous Liquid Ablation Agent Fortumor Treatment and Drug Delivery. Sci. Transl. Med. 2021, 13, eabe3889. [Google Scholar] [CrossRef] [PubMed]
- Tang, W.; Liu, B.; Wang, S.; Liu, T.; Fu, C.; Ren, X.; Tan, L.; Duan, W.; Meng, X. Doxorubicin-Loaded Ionic Liquid-Polydopamine Nanoparticles for Combined Chemotherapy and Microwave Thermal Therapy of Cancer. RSC Adv. 2016, 6, 32434–32440. [Google Scholar] [CrossRef]
- Chowdhury, M.R.; Moshikur, R.M.; Wakabayashi, R.; Tahara, Y.; Kamiya, N.; Moniruzzaman, M.; Goto, M. In Vivo Biocompatibility, Pharmacokinetics, Antitumor Efficacy, and Hypersensitivity Evaluation of Ionic Liquid-Mediated Paclitaxel Formulations. Int. J. Pharm. 2019, 565, 219–226. [Google Scholar] [CrossRef] [PubMed]
- Curreri, A.M.; Kim, J.; Dunne, M.; Angsantikul, P.; Goetz, M.; Gao, Y.; Mitragotri, S. Deep Eutectic Solvents for Subcutaneous Delivery of Protein Therapeutics. Adv. Sci. 2023, 2205389, 2205389. [Google Scholar] [CrossRef]
- Moshikur, R.M.; Ali, M.K.; Moniruzzaman, M.; Goto, M. Recent Advances in Surface-Active Ionic Liquid-Assisted Self-Assembly Systems for Drug Delivery. Curr. Opin. Colloid Interface Sci. 2021, 56, 101515. [Google Scholar] [CrossRef]
- Herman, A.; Herman, A.P. Essential Oils and Their Constituents as Skin Penetration Enhancer for Transdermal Drug Delivery: A Review. J. Pharm. Pharmacol. 2015, 67, 473–485. [Google Scholar] [CrossRef]
- Kim, B.; Cho, H.-E.; Moon, S.H.; Ahn, H.-J.; Bae, S.; Cho, H.-D.; An, S. Transdermal Delivery Systems in Cosmetics. Biomed. Dermatol. 2020, 4, 10. [Google Scholar] [CrossRef]
- Huda, M.N.; Deaguro, I.G.; Borrego, E.A.; Kumar, R.; Islam, T.; Afrin, H.; Varela-Ramirez, A.; Aguilera, R.J.; Tanner, E.E.L.; Nurunnabi, M. Ionic Liquid-Mediated Delivery of a BCL-2 Inhibitor for Topical Treatment of Skin Melanoma. J. Control. Release 2022, 349, 783–795. [Google Scholar] [CrossRef]
- Tanner, E.E.L.; Wiraja, C.; Curreri, C.A.; Xu, C. Stabilization and Topical Skin Delivery of Framework Nucleic Acids Using Ionic Liquids. Adv. Therap. 2020, 3, 2000041. [Google Scholar] [CrossRef]
- Qi, Q.M.; Mitragotri, S. Mechanistic Study of Transdermal Delivery of Macromolecules Assisted by Ionic Liquids. J. Control. Release 2019, 311–312, 162–169. [Google Scholar] [CrossRef]
- Dharamdasani, V.; Mandal, A.; Qi, Q.M.; Suzuki, I.; Bentley, M.V.L.B.; Mitragotri, S. Topical Delivery of SiRNA into Skin Using Ionic Liquids. J. Control. Release 2020, 323, 475–482. [Google Scholar] [CrossRef]
- Vaidya, A.; Mitragotri, S. Ionic Liquid-Mediated Delivery of Insulin to Buccal Mucosa. J. Control. Release 2020, 327, 26–34. [Google Scholar] [CrossRef] [PubMed]
- Goto, M.; Tahara, Y.; Morita, K.; Wakabayashi, R.; Kamiya, N. Biocompatible Ionic Liquid Enhances Transdermal Antigen Peptide Delivery and Preventive Vaccination Effect. Mol. Pharm. 2020, 17, 3845–3856. [Google Scholar] [CrossRef]
- Ali, M.K.; Moshikur, R.M.; Wakabayashi, R.; Moniruzzaman, M.; Kamiya, N.; Goto, M. Biocompatible Ionic Liquid Surfactant-Based Microemulsion as a Potential Carrier for Sparingly Soluble Drugs. ACS Sustain. Chem. Eng. 2020, 8, 6263–6272. [Google Scholar] [CrossRef]
- Islam, M.R.; Uddin, S.; Chowdhury, M.R.; Wakabayashi, R.; Moniruzzaman, M.; Goto, M. Insulin Transdermal Delivery System for Diabetes Treatment Using a Biocompatible Ionic Liquid-Based Microemulsion. ACS Appl. Mater. Interfaces 2021, 13, 42461–42472. [Google Scholar] [CrossRef]
- Tekko, I.A.; Chen, G.; Domínguez-Robles, J.; Thakur, R.R.S.; Hamdan, I.M.N.; Vora, L.; Larrañeta, E.; McElnay, J.C.; McCarthy, H.O.; Rooney, M.; et al. Development and Characterisation of Novel Poly (Vinyl Alcohol)/Poly (Vinyl Pyrrolidone)-Based Hydrogel-Forming Microneedle Arrays for Enhanced and Sustained Transdermal Delivery of Methotrexate. Int. J. Pharm. 2020, 586, 119580. [Google Scholar] [CrossRef]
- Lin, X.; Yang, Y.; Li, S.; Li, Z.; Sheng, Y.; Su, Z.; Zhang, S. Oil-in-Ionic Liquid Nanoemulsion-Based Adjuvant Simultaneously Enhances the Stability and Immune Responses of Inactivated Foot-and-Mouth Disease Virus. Int. J. Pharm. 2022, 625, 122083. [Google Scholar] [CrossRef] [PubMed]
- Lin, X.; Sheng, Y.; Zhang, X.; Li, Z.; Yang, Y.; Wu, J.; Su, Z.; Ma, G.; Zhang, S. Oil-in-Ionic Liquid Nanoemulsion-Based Intranasal Delivery System for Influenza Split-Virus Vaccine. J. Control. Release 2022, 346, 380–391. [Google Scholar] [CrossRef]
- Ukidve, A.; Cu, K.; Goetz, M.; Angsantikul, P.; Curreri, A.; Tanner, E.E.L.; Lahann, J.; Mitragotri, S. Ionic-Liquid-Based Safe Adjuvants. Adv. Mater. 2020, 32, 2002990. [Google Scholar] [CrossRef]
- Araki, S.; Wakabayashi, R.; Moniruzzaman, M.; Kamiya, N.; Goto, M. Ionic Liquid-Mediated Transcutaneous Protein Delivery with Solid-in-Oil Nanodispersions. Medchemcomm 2015, 6, 2124–2128. [Google Scholar] [CrossRef]
- Liu, T.; Zhang, J.; Lu, B.; Wang, H.; Zhan, J.; Tan, X.; Wu, C.; Liu, S.; Wang, Z.; Zhang, J.; et al. Highly Efficient Conotoxin Delivery Enabled by a Bio-Derived Ionic Liquid. J. Mol. Liq. 2022, 367, 120529. [Google Scholar] [CrossRef]
- Rajendran, S.; Hong Loh, S.; Mohd Ariffin, M.; Mohd Afiq Wan Mohd Khalik, W. Magnetic Effervescent Tablet-Assisted Ionic Liquid Dispersive Liquid–Liquid Microextraction Employing the Response Surface Method for the Preconcentration of Basic Pharmaceutical Drugs: Characterization, Method Development, and Green Profile Assessment. J. Mol. Liq. 2022, 367, 120411. [Google Scholar] [CrossRef]
- Babamale, H.F.; Khor, B.K.; Chear, N.J.Y.; Haque, R.A.; Yam, W.S. The First Tetrafluorinated Azobenzene-Imidazolium Ionic Conjugates as Potential Thermotropic Liquid Crystalline Drugs: Self-Assembly Properties and Cytotoxic Effects. J. Mol. Struct. 2022, 1255, 132470. [Google Scholar] [CrossRef]
- Boscariol, R.; Oliveira Junior, J.M.; Baldo, D.A.; Balcão, V.M.; Vila, M.M.D.C. Transdermal Permeation of Curcumin Promoted by Choline Geranate Ionic Liquid: Potential for the Treatment of Skin Diseases. Saudi Pharm. J. 2022, 30, 382–397. [Google Scholar] [CrossRef] [PubMed]
- Ali, M.K.; Moshikur, R.M.; Wakabayashi, R.; Moniruzzaman, M.; Goto, M. Biocompatible Ionic Liquid-Mediated Micelles for Enhanced Transdermal Delivery of Paclitaxel. ACS Appl. Mater. Interfaces 2021, 13, 19745–19755. [Google Scholar] [CrossRef] [PubMed]
- Chowdhury, M.R.; Moshikur, R.M.; Wakabayashi, R.; Moniruzzaman, M.; Goto, M. Biocompatible Ionic Liquids Assisted Transdermal Co-Delivery of Antigenic Protein and Adjuvant for Cancer Immunotherapy. Int. J. Pharm. 2021, 601, 120582. [Google Scholar] [CrossRef]
- Zhou, B.; Liu, S.; Yin, H.; Qi, M.; Hong, M.; Ren, G. Bin Development of Gliclazide Ionic Liquid and the Transdermal Patches: An Effective and Noninvasive Sustained Release Formulation to Achieve Hypoglycemic Effects. Eur. J. Pharm. Sci. 2021, 164, 105915. [Google Scholar] [CrossRef]
- Yang, D.; Fang, L.; Yang, C. Roles of Molecular Interaction and Mobility on Loading Capacity and Release Rate of Drug-Ionic Liquid in Long-Acting Controlled Release Transdermal Patch. J. Mol. Liq. 2022, 352, 118752. [Google Scholar] [CrossRef]
- Uddin, S.; Islam, M.R.; Chowdhury, M.R.; Wakabayashi, R.; Kamiya, N.; Moniruzzaman, M.; Goto, M. Lipid-Based Ionic-Liquid-Mediated Nanodispersions as Biocompatible Carriers for the Enhanced Transdermal Delivery of a Peptide Drug. ACS Appl. Bio Mater. 2021, 4, 6256–6267. [Google Scholar] [CrossRef]
- Uddin, S.; Islam, M.R.; Moshikur, R.M.; Wakabayashi, R.; Moniruzzaman, M.; Goto, M. Modification with Conventional Surfactants to Improve a Lipid-Based Ionic-Liquid-Associated Transcutaneous Anticancer Vaccine. Molecules 2023, 28, 2969. [Google Scholar] [CrossRef]
- Lin, X.; Yang, Y.; Li, S.; Song, Y.; Ma, G.; Su, Z.; Zhang, S. Unique Stabilizing Mechanism Provided by Biocompatible Choline-Based Ionic Liquids for Inhibiting Dissociation of Inactivated Foot-and-Mouth Disease Virus Particles. RSC Adv. 2019, 9, 13933–13939. [Google Scholar] [CrossRef] [PubMed]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moshikur, R.M.; Carrier, R.L.; Moniruzzaman, M.; Goto, M. Recent Advances in Biocompatible Ionic Liquids in Drug Formulation and Delivery. Pharmaceutics 2023, 15, 1179. https://doi.org/10.3390/pharmaceutics15041179
Moshikur RM, Carrier RL, Moniruzzaman M, Goto M. Recent Advances in Biocompatible Ionic Liquids in Drug Formulation and Delivery. Pharmaceutics. 2023; 15(4):1179. https://doi.org/10.3390/pharmaceutics15041179
Chicago/Turabian StyleMoshikur, Rahman Md, Rebecca L. Carrier, Muhammad Moniruzzaman, and Masahiro Goto. 2023. "Recent Advances in Biocompatible Ionic Liquids in Drug Formulation and Delivery" Pharmaceutics 15, no. 4: 1179. https://doi.org/10.3390/pharmaceutics15041179
APA StyleMoshikur, R. M., Carrier, R. L., Moniruzzaman, M., & Goto, M. (2023). Recent Advances in Biocompatible Ionic Liquids in Drug Formulation and Delivery. Pharmaceutics, 15(4), 1179. https://doi.org/10.3390/pharmaceutics15041179








