Recent Options and Techniques to Assess Improved Bioavailability: In Vitro and Ex Vivo Methods
Abstract
1. Introduction
2. Oral Route
2.1. In Vitro Methods
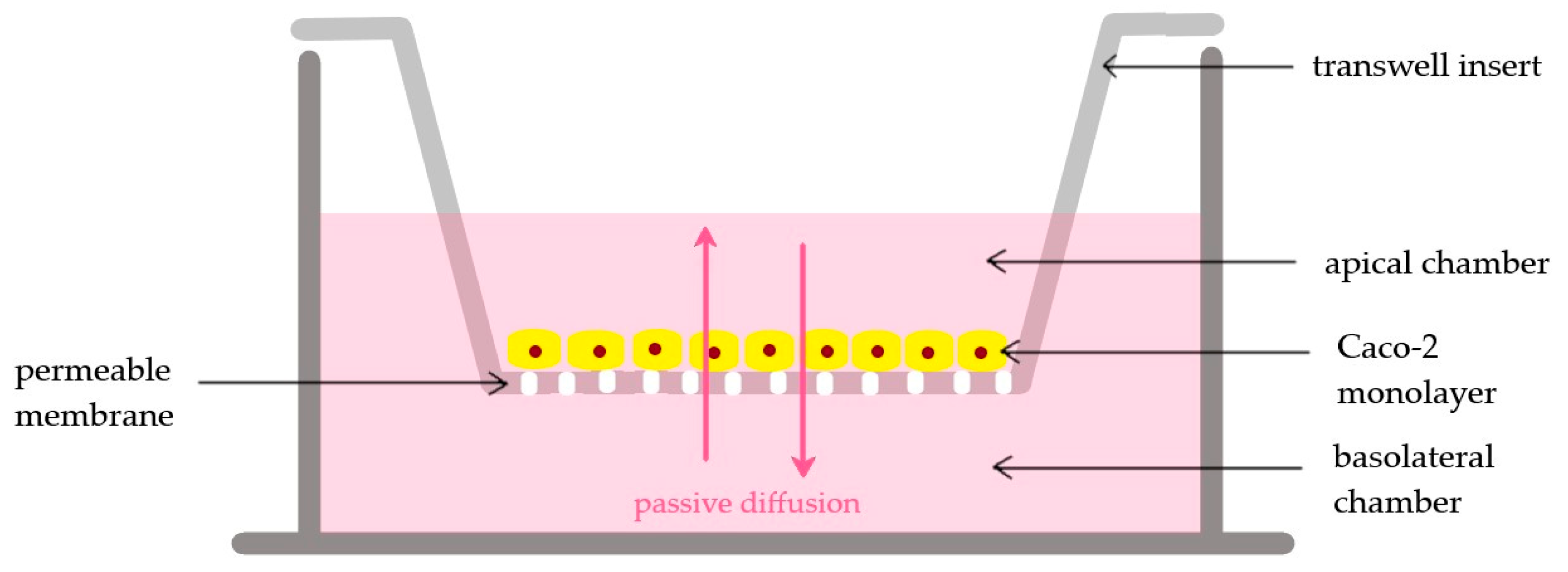
2.2. Cell Culture
2.3. Ex Vivo
3. Nasal or Inhalation
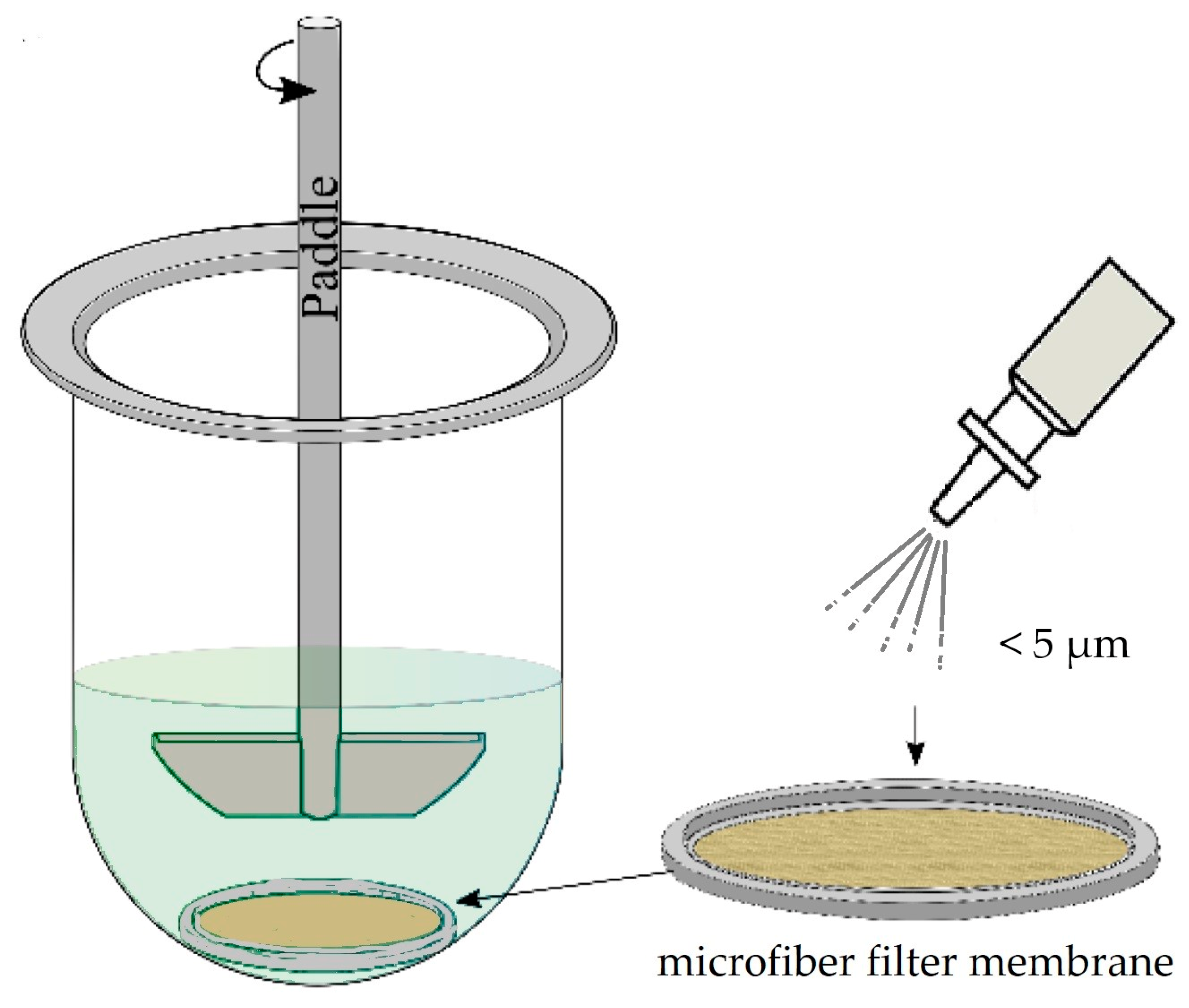
3.1. In Vitro
3.2. Cell Culture
3.3. Ex Vivo
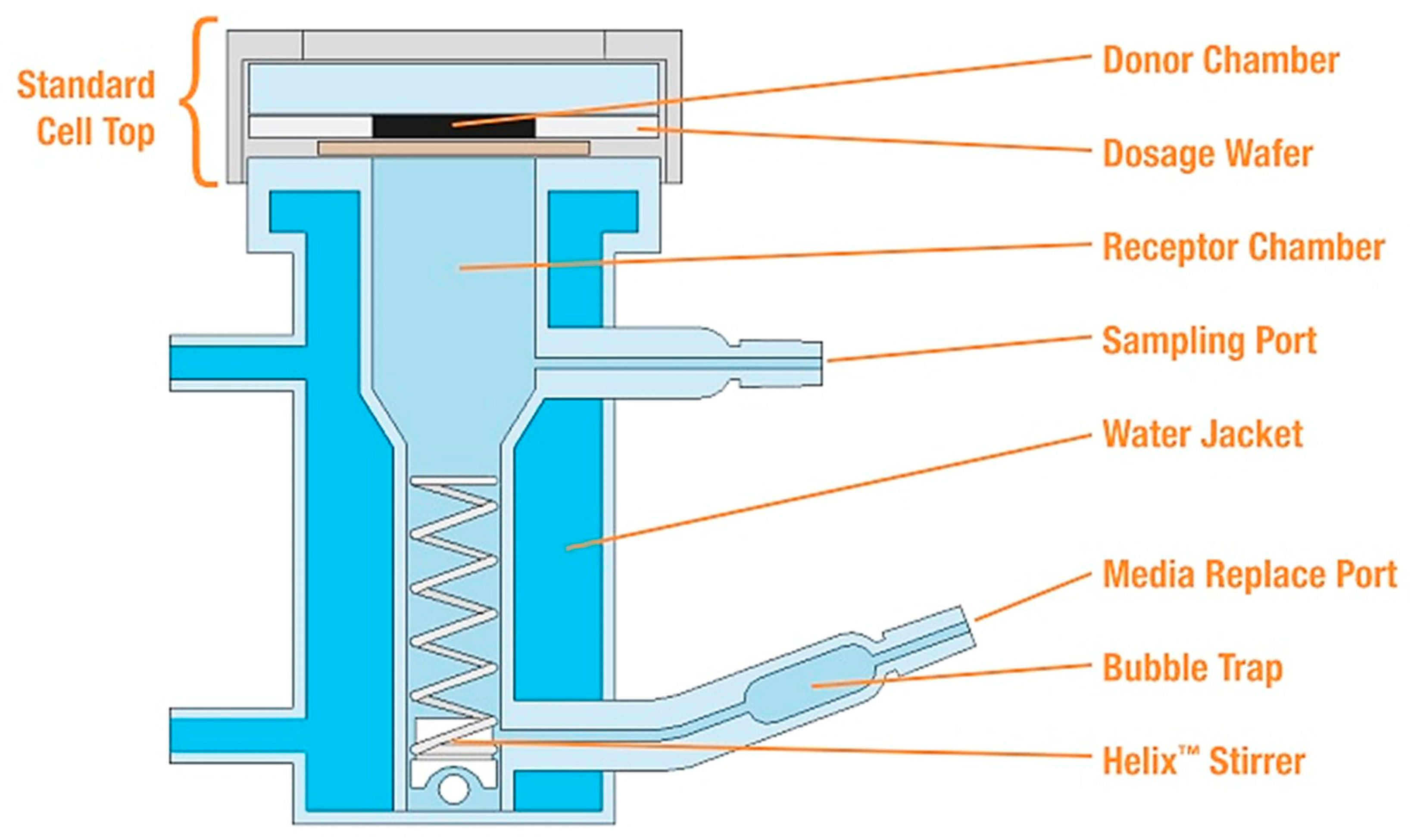
4. Transdermal
4.1. In Vitro
4.2. Cell Culture
4.3. Ex Vivo
5. Ophthalmic
5.1. In Vitro
5.2. Cell Culture
5.3. Ex Vivo
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Avila, A.M.; Bebenek, I.; Bonzo, J.A.; Bourcier, T.; Davis Bruno, K.L.; Carlson, D.B.; Dubinion, J.; Elayan, I.; Harrouk, W.; Lee, S.-L.; et al. An FDA/CDER Perspective on Nonclinical Testing Strategies: Classical Toxicology Approaches and New Approach Methodologies (NAMs). Regul. Toxicol. Pharmacol. 2020, 114, 104662. [Google Scholar] [CrossRef] [PubMed]
- Jaroch, K.; Jaroch, A.; Bojko, B. Cell Cultures in Drug Discovery and Development: The Need of Reliable in vitro-in vivo Extrapolation for Pharmacodynamics and Pharmacokinetics Assessment. J. Pharm. Biomed. Anal. 2018, 147, 297–312. [Google Scholar] [CrossRef] [PubMed]
- Castelo-Branco, D.d.S.C.M.; Amando, B.R.; Ocadaque, C.J.; Aguiar, L.d.; Paiva, D.D.d.Q.; Diógenes, E.M.; Guedes, G.M.d.M.; Costa, C.L.; Santos-Filho, A.S.P.; Andrade, A.R.C.d.; et al. Mini-Review: From in vitro to Ex Vivo Studies: An Overview of Alternative Methods for the Study of Medical Biofilms. Biofouling 2020, 36, 1129–1148. [Google Scholar] [CrossRef]
- Kirk, R.G.W. Recovering the Principles of Humane Experimental Technique. Sci. Technol. Hum. Values 2018, 43, 622–648. [Google Scholar] [CrossRef]
- Xu, Y.; Shrestha, N.; Préat, V.; Beloqui, A. An Overview of in vitro, Ex Vivo and in vivo Models for Studying the Transport of Drugs across Intestinal Barriers. Adv. Drug Deliv. Rev. 2021, 175, 113795. [Google Scholar] [CrossRef] [PubMed]
- Meigs, L. Animal Testing and Its Alternatives—The Most Important Omics Is Economics. ALTEX 2018, 35, 275–305. [Google Scholar] [CrossRef] [PubMed]
- Zsikó, S.; Csányi, E.; Kovács, A.; Budai-Szűcs, M.; Gácsi, A.; Berkó, S. Novel In Vitro Investigational Methods for Modeling Skin Permeation: Skin PAMPA, Raman Mapping. Pharmaceutics 2020, 12, 803. [Google Scholar] [CrossRef]
- Peeters, E.; Nelis, H.J.; Coenye, T. Comparison of Multiple Methods for Quantification of Microbial Biofilms Grown in Microtiter Plates. J. Microbiol. Methods 2008, 72, 157–165. [Google Scholar] [CrossRef]
- Roberts, A.E.L.; Kragh, K.N.; Bjarnsholt, T.; Diggle, S.P. The Limitations of In Vitro Experimentation in Understanding Biofilms and Chronic Infection. J. Mol. Biol. 2015, 427, 3646–3661. [Google Scholar] [CrossRef]
- Pearce, S.C.; Coia, H.G.; Karl, J.P.; Pantoja-Feliciano, I.G.; Zachos, N.C.; Racicot, K. Intestinal in vitro and Ex Vivo Models to Study Host-Microbiome Interactions and Acute Stressors. Front. Physiol. 2018, 9, 1584. [Google Scholar] [CrossRef]
- Štukelj, J.; Svanbäck, S.; Agopov, M.; Löbmann, K.; Strachan, C.J.; Rades, T.; Yliruusi, J. Direct Measurement of Amorphous Solubility. Anal. Chem. 2019, 91, 7411–7417. [Google Scholar] [CrossRef] [PubMed]
- Wilson, V.; Lou, X.; Osterling, D.J.; Stolarik, D.F.; Jenkins, G.; Gao, W.; Zhang, G.G.Z.; Taylor, L.S. Relationship between Amorphous Solid Dispersion in vivo Absorption and in vitro Dissolution: Phase Behavior during Dissolution, Speciation, and Membrane Mass Transport. J. Control. Release 2018, 292, 172–182. [Google Scholar] [CrossRef] [PubMed]
- Elkhabaz, A.; Moseson, D.E.; Brouwers, J.; Augustijns, P.; Taylor, L.S. Interplay of Supersaturation and Solubilization: Lack of Correlation between Concentration-Based Supersaturation Measurements and Membrane Transport Rates in Simulated and Aspirated Human Fluids. Mol. Pharm. 2019, 16, 5042–5053. [Google Scholar] [CrossRef] [PubMed]
- Vertzoni, M.; Dressman, J.; Butler, J.; Hempenstall, J.; Reppas, C. Simulation of Fasting Gastric Conditions and Its Importance for the in vivo Dissolution of Lipophilic Compounds. Eur. J. Pharm. Biopharm. 2005, 60, 413–417. [Google Scholar] [CrossRef]
- Jantratid, E.; Dressman, J. Biorelevant Dissolution Media Simulating the Proximal Human Gastrointestinal Tract: An Update. Dissolution Technol. 2009, 16, 21–25. [Google Scholar] [CrossRef]
- Jantratid, E.; Janssen, N.; Chokshi, H.; Tang, K.; Dressman, J.B. Designing Biorelevant Dissolution Tests for Lipid Formulations: Case Example—Lipid Suspension of RZ-50. Eur. J. Pharm. Biopharm. 2008, 69, 776–785. [Google Scholar] [CrossRef]
- Dressman, J.B.; Amidon, G.L.; Reppas, C.; Shah, V.P. Dissolution Testing as a Prognostic Tool for Oral Drug Absorption: Immediate Release Dosage Forms. Pharm. Res. 1998, 15, 11–22. [Google Scholar] [CrossRef]
- Sorasitthiyanukarn, F.N.; Muangnoi, C.; Rojsitthisak, P.; Rojsitthisak, P. Chitosan Oligosaccharide/Alginate Nanoparticles as an Effective Carrier for Astaxanthin with Improving Stability, in vitro Oral Bioaccessibility, and Bioavailability. Food Hydrocoll. 2022, 124, 107246. [Google Scholar] [CrossRef]
- Dahan, A.; Hoffman, A. Use of a Dynamic in vitro Lipolysis Model to Rationalize Oral Formulation Development for Poor Water Soluble Drugs: Correlation with in vivo Data and the Relationship to Intra-Enterocyte Processes in Rats. Pharm. Res. 2006, 23, 2165–2174. [Google Scholar] [CrossRef]
- Caon, T.; Kratz, J.M.; Kuminek, G.; Heller, M.; Konig, R.A.; Micke, G.A.; Koester, L.S.; Simões, C.M.O. Oral Saquinavir Mesylate Solid Dispersions: In Vitro Dissolution, Caco-2 Cell Model Permeability and in vivo Absorption Studies. Powder Technol. 2015, 269, 200–206. [Google Scholar] [CrossRef]
- Zhao, Q.; Wang, Z.; Wang, X.; Yan, X.; Guo, Q.; Yue, Y.; Yue, T.; Yuan, Y. The Bioaccessibility, Bioavailability, Bioactivity, and Prebiotic Effects of Phenolic Compounds from Raw and Solid-Fermented Mulberry Leaves during in vitro Digestion and Colonic Fermentation. Food Res. Int. 2023, 165, 112493. [Google Scholar] [CrossRef]
- Feeney, O.M.; Crum, M.F.; McEvoy, C.L.; Trevaskis, N.L.; Williams, H.D.; Pouton, C.W.; Charman, W.N.; Bergström, C.A.S.; Porter, C.J.H. 50 Years of Oral Lipid-Based Formulations: Provenance, Progress and Future Perspectives. Adv. Drug Deliv. Rev. 2016, 101, 167–194. [Google Scholar] [CrossRef]
- Murshed, M.; Pham, A.; Vithani, K.; Salim, M.; Boyd, B.J. Controlling Drug Release by Introducing Lipase Inhibitor within a Lipid Formulation. Int. J. Pharm. 2022, 623, 121958. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Yu, Q.; Chen, Z.; Wu, W.; Zhu, Q.; Lu, Y. In vitro and in vivo Correlation for Lipid-Based Formulations: Current Status and Future Perspectives. Acta Pharm. Sin. B 2021, 11, 2469–2487. [Google Scholar] [CrossRef]
- Berlin, M.; Przyklenk, K.-H.; Richtberg, A.; Baumann, W.; Dressman, J.B. Prediction of Oral Absorption of Cinnarizine—A Highly Supersaturating Poorly Soluble Weak Base with Borderline Permeability. Eur. J. Pharm. Biopharm. 2014, 88, 795–806. [Google Scholar] [CrossRef] [PubMed]
- Pettarin, M.; Bolger, M.B.; Chronowska, M.; Kostewicz, E.S. A Combined in vitro In-Silico Approach to Predict the Oral Bioavailability of Borderline BCS Class II/IV Weak Base Albendazole and Its Main Metabolite Albendazole Sulfoxide. Eur. J. Pharm. Sci. 2020, 155, 105552. [Google Scholar] [CrossRef] [PubMed]
- Hate, S.S.; Mosquera-Giraldo, L.I.; Taylor, L.S. A Mechanistic Study of Drug Mass Transport from Supersaturated Solutions Across PAMPA Membranes. J. Pharm. Sci. 2022, 111, 102–115. [Google Scholar] [CrossRef]
- Đanić, M.; Pavlović, N.; Stanimirov, B.; Lazarević, S.; Vukmirović, S.; Al-Salami, H.; Mikov, M. PAMPA Model of Gliclazide Permeability: The Impact of Probiotic Bacteria and Bile Acids. Eur. J. Pharm. Sci. 2021, 158, 105668. [Google Scholar] [CrossRef]
- Borbás, E.; Nagy, Z.K.; Nagy, B.; Balogh, A.; Farkas, B.; Tsinman, O.; Tsinman, K.; Sinkó, B. The Effect of Formulation Additives on in vitro Dissolution-Absorption Profile and in vivo Bioavailability of Telmisartan from Brand and Generic Formulations. Eur. J. Pharm. Sci. 2018, 114, 310–317. [Google Scholar] [CrossRef]
- Li, J.; Tsinman, K.; Tsinman, O.; Wigman, L. Using PH Gradient Dissolution with In-Situ Flux Measurement to Evaluate Bioavailability and DDI for Formulated Poorly Soluble Drug Products. AAPS PharmSciTech 2018, 19, 2898–2907. [Google Scholar] [CrossRef]
- Patel, M.H.; Sawant, K.K. Self Microemulsifying Drug Delivery System of Lurasidone Hydrochloride for Enhanced Oral Bioavailability by Lymphatic Targeting: In vitro, Caco-2 Cell Line and in vivo Evaluation. Eur. J. Pharm. Sci. 2019, 138, 105027. [Google Scholar] [CrossRef] [PubMed]
- Jarc, T.; Novak, M.; Hevir, N.; Rižner, T.L.; Kreft, M.E.; Kristan, K. Demonstrating Suitability of the Caco-2 Cell Model for BCS-Based Biowaiver According to the Recent FDA and ICH Harmonised Guidelines. J. Pharm. Pharmacol. 2019, 71, 1231–1242. [Google Scholar] [CrossRef] [PubMed]
- Faralli, A.; Shekarforoush, E.; Ajalloueian, F.; Mendes, A.C.; Chronakis, I.S. In Vitro Permeability Enhancement of Curcumin across Caco-2 Cells Monolayers Using Electrospun Xanthan-Chitosan Nanofibers. Carbohydr. Polym. 2019, 206, 38–47. [Google Scholar] [CrossRef] [PubMed]
- Ferruzza, S.; Rossi, C.; Scarino, M.L.; Sambuy, Y. A Protocol for Differentiation of Human Intestinal Caco-2 Cells in Asymmetric Serum-Containing Medium. Toxicol. Vitr. 2012, 26, 1252–1255. [Google Scholar] [CrossRef]
- Fenyvesi, F.; Nguyen, T.L.P.; Haimhoffer, Á.; Rusznyák, Á.; Vasvári, G.; Bácskay, I.; Vecsernyés, M.; Ignat, S.-R.; Dinescu, S.; Costache, M.; et al. Cyclodextrin Complexation Improves the Solubility and Caco-2 Permeability of Chrysin. Materials 2020, 13, 3618. [Google Scholar] [CrossRef]
- Haimhoffer, Á.; Dossi, E.; Béresová, M.; Bácskay, I.; Váradi, J.; Afsar, A.; Rusznyák, Á.; Vasvári, G.; Fenyvesi, F. Preformulation Studies and Bioavailability Enhancement of Curcumin with a ‘Two in One’ PEG-β-Cyclodextrin Polymer. Pharmaceutics 2021, 13, 1710. [Google Scholar] [CrossRef]
- Gantzsch, S.P.; Kann, B.; Ofer-Glaessgen, M.; Loos, P.; Berchtold, H.; Balbach, S.; Eichinger, T.; Lehr, C.-M.; Schaefer, U.F.; Windbergs, M. Characterization and Evaluation of a Modified PVPA Barrier in Comparison to Caco-2 Cell Monolayers for Combined Dissolution and Permeation Testing. J. Control. Release 2014, 175, 79–86. [Google Scholar] [CrossRef]
- Remenyik, J.; Biró, A.; Klusóczki, Á.; Juhász, K.Z.; Szendi-Szatmári, T.; Kenesei, Á.; Szőllősi, E.; Vasvári, G.; Stündl, L.; Fenyvesi, F.; et al. Comparison of the Modulating Effect of Anthocyanin-Rich Sour Cherry Extract on Occludin and ZO-1 on Caco-2 and HUVEC Cultures. Int. J. Mol. Sci. 2022, 23, 9036. [Google Scholar] [CrossRef]
- Nguyen, T.L.P.; Fenyvesi, F.; Remenyik, J.; Homoki, J.R.; Gogolák, P.; Bácskay, I.; Fehér, P.; Ujhelyi, Z.; Vasvári, G.; Vecsernyés, M.; et al. Protective Effect of Pure Sour Cherry Anthocyanin Extract on Cytokine-Induced Inflammatory Caco-2 Monolayers. Nutrients 2018, 10, 861. [Google Scholar] [CrossRef]
- Réti-Nagy, K.; Malanga, M.; Fenyvesi, É.; Szente, L.; Vámosi, G.; Váradi, J.; Bácskay, I.; Fehér, P.; Ujhelyi, Z.; Róka, E.; et al. Endocytosis of Fluorescent Cyclodextrins by Intestinal Caco-2 Cells and Its Role in Paclitaxel Drug Delivery. Int. J. Pharm. 2015, 496, 509–517. [Google Scholar] [CrossRef]
- Rusznyák, Á.; Malanga, M.; Fenyvesi, É.; Szente, L.; Váradi, J.; Bácskay, I.; Vecsernyés, M.; Vasvári, G.; Haimhoffer, Á.; Fehér, P.; et al. Investigation of the Cellular Effects of Beta- Cyclodextrin Derivatives on Caco-2 Intestinal Epithelial Cells. Pharmaceutics 2021, 13, 157. [Google Scholar] [CrossRef]
- Józsa, L.; Ujhelyi, Z.; Vasvári, G.; Sinka, D.; Nemes, D.; Fenyvesi, F.; Váradi, J.; Vecsernyés, M.; Szabó, J.; Kalló, G.; et al. Formulation of Creams Containing Spirulina Platensis Powder with Different Nonionic Surfactants for the Treatment of Acne Vulgaris. Molecules 2020, 25, 4856. [Google Scholar] [CrossRef] [PubMed]
- Pamlényi, K.; Regdon, G.; Nemes, D.; Fenyvesi, F.; Bácskay, I.; Kristó, K. Stability, Permeability and Cytotoxicity of Buccal Films in Allergy Treatment. Pharmaceutics 2022, 14, 1633. [Google Scholar] [CrossRef] [PubMed]
- Clarke, L.L. A Guide to Ussing Chamber Studies of Mouse Intestine. Am. J. Physiol. Liver Physiol. 2009, 296, G1151–G1166. [Google Scholar] [CrossRef] [PubMed]
- Arnold, Y.E.; Kalia, Y.N. Using Ex Vivo Porcine Jejunum to Identify Membrane Transporter Substrates: A Screening Tool for Early—Stage Drug Development. Biomedicines 2020, 8, 340. [Google Scholar] [CrossRef]
- Andlauer, W.; Kolb, J.; Fürst, P. Absorption and Metabolism of Genistin in the Isolated Rat Small Intestine. FEBS Lett. 2000, 475, 127–130. [Google Scholar] [CrossRef]
- Luo, Z.; Liu, Y.; Zhao, B.; Tang, M.; Dong, H.; Zhang, L.; Lv, B.; Wei, L. Ex Vivo and in Situ Approaches Used to Study Intestinal Absorption. J. Pharmacol. Toxicol. Methods 2013, 68, 208–216. [Google Scholar] [CrossRef]
- Jung, S.-M.; Kim, S. In Vitro Models of the Small Intestine for Studying Intestinal Diseases. Front. Microbiol. 2022, 12, 4102. [Google Scholar] [CrossRef]
- Sjöberg, Å.; Lutz, M.; Tannergren, C.; Wingolf, C.; Borde, A.; Ungell, A.-L. Comprehensive Study on Regional Human Intestinal Permeability and Prediction of Fraction Absorbed of Drugs Using the Ussing Chamber Technique. Eur. J. Pharm. Sci. 2013, 48, 166–180. [Google Scholar] [CrossRef]
- Miyake, M.; Koga, T.; Kondo, S.; Yoda, N.; Emoto, C.; Mukai, T.; Toguchi, H. Prediction of Drug Intestinal Absorption in Human Using the Ussing Chamber System: A Comparison of Intestinal Tissues from Animals and Humans. Eur. J. Pharm. Sci. 2017, 96, 373–380. [Google Scholar] [CrossRef]
- Nunes, R.; Silva, C.; Chaves, L. Tissue-Based in vitro and Ex Vivo Models for Intestinal Permeability Studies. In Concepts and Models for Drug Permeability Studies; Elsevier: Amsterdam, The Netherlands, 2016; pp. 203–236. ISBN 9780081000946. [Google Scholar]
- Streekstra, E.J.; Kiss, M.; van den Heuvel, J.; Nicolaï, J.; van den Broek, P.; Botden, S.M.B.I.; Stommel, M.W.J.; van Rijssel, L.; Ungell, A.; van de Steeg, E.; et al. A Proof of Concept Using the Ussing Chamber Methodology to Study Pediatric Intestinal Drug Transport and Age-dependent Differences in Absorption. Clin. Transl. Sci. 2022, 15, 2392–2402. [Google Scholar] [CrossRef] [PubMed]
- Luo, L.-Y.; Fan, M.-X.; Zhao, H.-Y.; Li, M.-X.; Wu, X.; Gao, W.-Y. Pharmacokinetics and Bioavailability of the Isoflavones Formononetin and Ononin and Their in vitro Absorption in Ussing Chamber and Caco-2 Cell Models. J. Agric. Food Chem. 2018, 66, 2917–2924. [Google Scholar] [CrossRef]
- Kalungwana, N.; Marshall, L.; Mackie, A.; Boesch, C. An Ex Vivo Intestinal Absorption Model Is More Effective than an in vitro Cell Model to Characterise Absorption of Dietary Carotenoids Following Simulated Gastrointestinal Digestion. Food Res. Int. 2023, 166, 112558. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Park, H.J.; Xiu, H.; Akoh, C.C.; Kong, F. Predicting Intestinal Effective Permeability of Different Transport Mechanisms: Comparing Ex Vivo Porcine and in vitro Dialysis Models. J. Food Eng. 2023, 338, 111256. [Google Scholar] [CrossRef]
- Faiz, S.; Arshad, S.; Kamal, Y.; Imran, S.; Asim, M.H.; Mahmood, A.; Inam, S.; Irfan, H.M.; Riaz, H. Pioglitazone-Loaded Nanostructured Lipid Carriers: In-Vitro and in-Vivo Evaluation for Improved Bioavailability. J. Drug Deliv. Sci. Technol. 2023, 79, 104041. [Google Scholar] [CrossRef]
- Wang, D.; Liu, R.; Zeng, J.; Li, C.; Xiang, W.; Zhong, G.; Xia, Z. Preliminary Screening of the Potential Active Ingredients in Traditional Chinese Medicines Using the Ussing Chamber Model Combined with HPLC-PDA-MS. J. Chromatogr. B 2022, 1189, 123090. [Google Scholar] [CrossRef] [PubMed]
- Lennernas, H. Animal Data: The Contributions of the Ussing Chamber and Perfusion Systems to Predicting Human Oral Drug Delivery in vivo☆. Adv. Drug Deliv. Rev. 2007, 59, 1103–1120. [Google Scholar] [CrossRef]
- Ruela, A.L.M.; Perissinato, A.G.; Lino, M.E.d.S.; Mudrik, P.S.; Pereira, G.R. Evaluation of Skin Absorption of Drugs from Topical and Transdermal Formulations. Brazilian J. Pharm. Sci. 2016, 52, 527–544. [Google Scholar] [CrossRef]
- Castro, P.; Madureira, R.; Sarmento, B.; Pintado, M. Tissue-Based in vitro and Ex Vivo Models for Buccal Permeability Studies. In Concepts and Models for Drug Permeability Studies; Elsevier: Amsterdam, The Netherlands, 2016; pp. 189–202. [Google Scholar]
- Wang, S.; Zuo, A.; Guo, J. Types and Evaluation of in vitro Penetration Models for Buccal Mucosal Delivery. J. Drug Deliv. Sci. Technol. 2021, 61, 102122. [Google Scholar] [CrossRef]
- Sa, G.; Xiong, X.; Wu, T.; Yang, J.; He, S.; Zhao, Y. Histological Features of Oral Epithelium in Seven Animal Species: As a Reference for Selecting Animal Models. Eur. J. Pharm. Sci. 2016, 81, 10–17. [Google Scholar] [CrossRef]
- Obradovic, T.; Hidalgo, I.J. In Vitro Models for Investigations of Buccal Drug Permeation and Metabolism. In Drug Absorption Studies; Springer: Boston, MA, USA; pp. 167–181.
- Meng-Lund, E.; Marxen, E.; Pedersen, A.M.L.; Müllertz, A.; Hyrup, B.; Holm, R.; Jacobsen, J. Ex Vivo Correlation of the Permeability of Metoprolol across Human and Porcine Buccal Mucosa. J. Pharm. Sci. 2014, 103, 2053–2061. [Google Scholar] [CrossRef] [PubMed]
- van Eyk, A.D.; van der Bijl, P. Comparative Permeability of Various Chemical Markers through Human Vaginal and Buccal Mucosa as Well as Porcine Buccal and Mouth Floor Mucosa. Arch. Oral Biol. 2004, 49, 387–392. [Google Scholar] [CrossRef] [PubMed]
- Pinto, S.; Pintado, M.E.; Sarmento, B. In Vivo, Ex Vivo and in vitro Assessment of Buccal Permeation of Drugs from Delivery Systems. Expert Opin. Drug Deliv. 2020, 17, 33–48. [Google Scholar] [CrossRef] [PubMed]
- Wilson, T.H.; Wiseman, G. The Use of Sacs of Everted Small Intestine for the Study of the Transference of Substances from the Mucosal to the Serosal Surface. J. Physiol. 1954, 123, 116–125. [Google Scholar] [CrossRef] [PubMed]
- Cotter, P.; López-Expósito, I.; Kleiveland, C.; Lea, T.; Mackie, A.; Requena, T.; Swiatecka, D.; Harry, W. The Impact of Food Bioactives on Health; Verhoeckx, K., Cotter, P., López-Expósito, I., Kleiveland, C., Lea, T., Mackie, A., Requena, T., Swiatecka, D., Wichers, H., Eds.; Springer International Publishing: Cham, Switzerland, 2015; ISBN 978-3-319-15791-7. [Google Scholar]
- Dixit, P.; Jain, D.K.; Dumbwani, J. Standardization of an Ex Vivo Method for Determination of Intestinal Permeability of Drugs Using Everted Rat Intestine Apparatus. J. Pharmacol. Toxicol. Methods 2012, 65, 13–17. [Google Scholar] [CrossRef]
- Gandia, P.; Lacombe, O.; Woodley, J.; Houin, G. The Perfused Everted Intestinal Segment of Rat. Arzneimittelforschung 2011, 54, 467–473. [Google Scholar] [CrossRef]
- Gagliardi, M.; Clemente, N.; Monzani, R.; Fusaro, L.; Ferrari, E.; Saverio, V.; Grieco, G.; Pańczyszyn, E.; Carton, F.; Santoro, C.; et al. Gut-Ex-Vivo System as a Model to Study Gluten Response in Celiac Disease. Cell Death Discov. 2021, 7, 45. [Google Scholar] [CrossRef]
- Committee for Medicinal Products for Human Use (CHMP). Guideline on the Investigation of Bioequivalence; Committee for Medicinal Products for Human Use (CHMP): London, UK, 2010. [Google Scholar]
- Committee for Medicinal Products for Human Use (CHMP). ICH M9 on Biopharmaceutics Classification System Based Biowaivers—Scientific Guideline; Committee for Medicinal Products for Human Use (CHMP): Amsterdam, The Netherlands, 2020. [Google Scholar]
- United States. Department of Health and Human Services; United States. Food and Drug Administration; Center for Drug Evaluation and Research (U.S.). Waiver of In Vivo Bioavailability and Bioequivalence Studies for Immediate-Release Solid Oral Dosage Forms Based on a Biopharmaceutics Classification System; Guidance for Industry; Center for Drug Evaluation and Research: Silver Spring, MD, USA, 2017. [Google Scholar]
- Committee for Medicinal Products for Human Use (CHMP). Guideline on Quality of Oral Modified Release Products; Committee for Medicinal Products for Human Use (CHMP): London, UK, 2014. [Google Scholar]
- Committee for Medicinal Products for Human Use (CHMP). Guideline on the Pharmacokinetic and Clinical Evaluation of Modified Release Dosage Forms; Committee for Medicinal Products for Human Use (CHMP): London, UK, 2014. [Google Scholar]
- Pu, Y.; Goodey, A.P.; Fang, X.; Jacob, K. A Comparison of the Deposition Patterns of Different Nasal Spray Formulations Using a Nasal Cast. Aerosol Sci. Technol. 2014, 48, 930–938. [Google Scholar] [CrossRef]
- Le Guellec, S.; Ehrmann, S.; Vecellio, L. In Vitro—In Vivo Correlation of Intranasal Drug Deposition. Adv. Drug Deliv. Rev. 2021, 170, 340–352. [Google Scholar] [CrossRef]
- Williams, G.; Suman, J.D. In Vitro Anatomical Models for Nasal Drug Delivery. Pharmaceutics 2022, 14, 1353. [Google Scholar] [CrossRef]
- Hilton, C.; Wiedmann, T.; Martin, M.S.; Humphrey, B.; Schleiffarth, R.; Rimell, F. Differential Deposition of Aerosols in the Maxillary Sinus of Human Cadavers by Particle Size. Am. J. Rhinol. 2008, 22, 395–398. [Google Scholar] [CrossRef] [PubMed]
- Okuda, T.; Tang, P.; Yu, J.; Finlay, W.H.; Chan, H.-K. Powder Aerosol Delivery through Nasal High-Flow System: In Vitro Feasibility and Influence of Process Conditions. Int. J. Pharm. 2017, 533, 187–197. [Google Scholar] [CrossRef] [PubMed]
- Spence, C.J.T.; Buchmann, N.A.; Jermy, M.C.; Moore, S.M. Stereoscopic PIV Measurements of Flow in the Nasal Cavity with High Flow Therapy. Exp. Fluids 2011, 50, 1005–1017. [Google Scholar] [CrossRef]
- Le Guellec, S.; Le Pennec, D.; Gatier, S.; Leclerc, L.; Cabrera, M.; Pourchez, J.; Diot, P.; Reychler, G.; Pitance, L.; Durand, M.; et al. Validation of Anatomical Models to Study Aerosol Deposition in Human Nasal Cavities. Pharm. Res. 2014, 31, 228–237. [Google Scholar] [CrossRef] [PubMed]
- Shah, S.A.; Dickens, C.J.; Ward, D.J.; Banaszek, A.A.; George, C.; Horodnik, W. Design of Experiments to Optimize an In Vitro Cast to Predict Human Nasal Drug Deposition. J. Aerosol Med. Pulm. Drug Deliv. 2014, 27, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Hartigan, D.R.; Adelfio, M.; Shutt, M.E.; Jones, S.M.; Patel, S.; Marchand, J.T.; McGuinness, P.D.; Buchholz, B.O.; Ghezzi, C.E. In Vitro Nasal Tissue Model for the Validation of Nasopharyngeal and Midturbinate Swabs for SARS-CoV-2 Testing. ACS Omega 2022, 7, 12193–12201. [Google Scholar] [CrossRef] [PubMed]
- Salade, L.; Wauthoz, N.; Goole, J.; Amighi, K. How to Characterize a Nasal Product. The State of the Art of in vitro and Ex Vivo Specific Methods. Int. J. Pharm. 2019, 561, 47–65. [Google Scholar] [CrossRef] [PubMed]
- McFadden, E.R.; Pichurko, B.M.; Bowman, H.F.; Ingenito, E.; Burns, S.; Dowling, N.; Solway, J. Thermal Mapping of the Airways in Humans. J. Appl. Physiol. 1985, 58, 564–570. [Google Scholar] [CrossRef]
- Radivojev, S.; Zellnitz, S.; Paudel, A.; Fröhlich, E. Searching for Physiologically Relevant in vitro Dissolution Techniques for Orally Inhaled Drugs. Int. J. Pharm. 2019, 556, 45–56. [Google Scholar] [CrossRef]
- Steimer, A.; Haltner, E.; Lehr, C.-M. Cell Culture Models of the Respiratory Tract Relevant to Pulmonary Drug Delivery. J. Aerosol Med. 2005, 18, 137–182. [Google Scholar] [CrossRef]
- Geraghty, R.J.; Stacey, G.N.; Masters, J.R.W.; Lovell-Badge, R.; Vias, M.; Davis, J.M.; Downward, J.; Thraves, P.; Knezevic, I.; Capes-Davis, A.; et al. Guidelines for the Use of Cell Lines in Biomedical Research. Br. J. Cancer 2015, 111, 1976–1977. [Google Scholar] [CrossRef]
- Fulcher, M.L.; Randell, S.H. Human Nasal and Tracheo-Bronchial Respiratory Epithelial Cell Culture. In Epithelial Cell Culture Protocols: Second Edition; Springer: Berlin/Heidelberg, Germany, 2012; Volume 945, pp. 109–121. ISBN 9781627031257. [Google Scholar]
- Mercier, C.; Perek, N.; Delavenne, X. Is RPMI 2650 a Suitable In Vitro Nasal Model for Drug Transport Studies? Eur. J. Drug Metab. Pharmacokinet. 2018, 43, 13–24. [Google Scholar] [CrossRef] [PubMed]
- Sibinovska, N.; Žakelj, S.; Trontelj, J.; Kristan, K. Applicability of RPMI 2650 and Calu-3 Cell Models for Evaluation of Nasal Formulations. Pharmaceutics 2022, 14, 369. [Google Scholar] [CrossRef] [PubMed]
- Sibinovska, N.; Žakelj, S.; Kristan, K. Suitability of RPMI 2650 Cell Models for Nasal Drug Permeability Prediction. Eur. J. Pharm. Biopharm. 2019, 145, 85–95. [Google Scholar] [CrossRef]
- Callaghan, P.J.; Ferrick, B.; Rybakovsky, E.; Thomas, S.; Mullin, J.M. Epithelial Barrier Function Properties of the 16HBE14o- Human Bronchial Epithelial Cell Culture Model. Biosci. Rep. 2020, 40, BSR20201532. [Google Scholar] [CrossRef]
- Forbes, B.; Shah, A.; Martin, G.P.; Lansley, A.B. The Human Bronchial Epithelial Cell Line 16HBE14o- as a Model System of the Airways for Studying Drug Transport. Int. J. Pharm. 2003, 257, 161–167. [Google Scholar] [CrossRef] [PubMed]
- Lin, H.-L.; Chiu, Y.-W.; Wang, C.-C.; Tung, C.-W. Computational Prediction of Calu-3-Based in vitro Pulmonary Permeability of Chemicals. Regul. Toxicol. Pharmacol. 2022, 135, 105265. [Google Scholar] [CrossRef]
- Ji, X.; Sheng, Y.; Guan, Y.; Li, Y.; Xu, Y.; Tang, L. Evaluation of Calu-3 Cell Lines as an in vitro Model to Study the Inhalation Toxicity of Flavoring Extracts. Toxicol. Mech. Methods 2022, 32, 171–179. [Google Scholar] [CrossRef]
- Selo, M.A.; Sake, J.A.; Kim, K.-J.; Ehrhardt, C. In Vitro and Ex Vivo Models in Inhalation Biopharmaceutical Research—Advances, Challenges and Future Perspectives. Adv. Drug Deliv. Rev. 2021, 177, 113862. [Google Scholar] [CrossRef]
- Andreasson, A.S.I.; Dark, J.H.; Fisher, A.J. Ex Vivo Lung Perfusion in Clinical Lung Transplantation--State of the Art. Eur. J. Cardio-Thoracic Surg. 2014, 46, 779–788. [Google Scholar] [CrossRef]
- Paranjpe, M.; Neuhaus, V.; Finke, J.H.; Richter, C.; Gothsch, T.; Kwade, A.; Büttgenbach, S.; Braun, A.; Müller-Goymann, C.C. In Vitro and Ex Vivo Toxicological Testing of Sildenafil-Loaded Solid Lipid Nanoparticles. Inhal. Toxicol. 2013, 25, 536–543. [Google Scholar] [CrossRef] [PubMed]
- Hansen, N.U.B.; Karsdal, M.A.; Brockbank, S.; Cruwys, S.; Rønnow, S.; Leeming, D.J. Tissue Turnover of Collagen Type I, III and Elastin Is Elevated in the PCLS Model of IPF and Can Be Restored Back to Vehicle Levels Using a Phosphodiesterase Inhibitor. Respir. Res. 2016, 17, 76. [Google Scholar] [CrossRef] [PubMed]
- Liu, G.; Betts, C.; Cunoosamy, D.M.; Åberg, P.M.; Hornberg, J.J.; Sivars, K.B.; Cohen, T.S. Use of Precision Cut Lung Slices as a Translational Model for the Study of Lung Biology. Respir. Res. 2019, 20, 162. [Google Scholar] [CrossRef]
- Cidem, A.; Bradbury, P.; Traini, D.; Ong, H.X. Modifying and Integrating in vitro and Ex Vivo Respiratory Models for Inhalation Drug Screening. Front. Bioeng. Biotechnol. 2020, 8, 1–15. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Health and Human Services Food and Drug Administration. Guidance for Industry Bioavailability and Bioequivalence Studies for Nasal Aerosols and Nasal Sprays for Local Action; U.S. Department of Health and Human Services Food and Drug Administration: Silver Spring, MD, USA, 2003. [Google Scholar]
- Committee for Medicinal Products for Human Use(Chmp). Guideline on the Pharmaceutical Quality of Inhalation and Nasal Products; Committee for Medicinal Products for Human Use(Chmp): London, UK, 2004. [Google Scholar]
- El-Nabarawi, M.A.; Bendas, E.R.; El Rehem, R.T.A.; Abary, M.Y.S. Transdermal Drug Delivery of Paroxetine through Lipid-Vesicular Formulation to Augment Its Bioavailability. Int. J. Pharm. 2013, 443, 307–317. [Google Scholar] [CrossRef]
- Abdel Azim, A.M.; El-Ashmoony, M.; Swealem, A.M.; Shoukry, R.A. Transdermal Films Containing Tizanidine: In Vitro and in vivo Evaluation. J. Drug Deliv. Sci. Technol. 2014, 24, 92–99. [Google Scholar] [CrossRef]
- Akhtar, B.; Muhammad, F.; Aslam, B.; Saleemi, M.K.; Sharif, A. Biodegradable Nanoparticle Based Transdermal Patches for Gentamicin Delivery: Formulation, Characterization and Pharmacokinetics in Rabbits. J. Drug Deliv. Sci. Technol. 2020, 57, 101680. [Google Scholar] [CrossRef]
- Abouhussein, D.M.N. Enhanced Transdermal Permeation of BCS Class IV Aprepitant Using Binary Ethosome: Optimization, Characterization and Ex Vivo Permeation. J. Drug Deliv. Sci. Technol. 2021, 61, 102185. [Google Scholar] [CrossRef]
- Kumar, A.; Singh, S.; Gautam, H. An Official Publication of Association of Pharmacy Professionals Theoretical aspects of transdermal drug. Bull. Pharm. Res. 2013, 1, 18–30. [Google Scholar]
- Selzer, D.; Abdel-Mottaleb, M.M.A.; Hahn, T.; Schaefer, U.F.; Neumann, D. Finite and Infinite Dosing: Difficulties in Measurements, Evaluations and Predictions. Adv. Drug Deliv. Rev. 2013, 65, 278–294. [Google Scholar] [CrossRef]
- Tsai, M.; Lu, I.; Fu, Y.; Fang, Y.; Huang, Y.; Wu, P. Colloids and Surfaces B: Biointerfaces Nanocarriers Enhance the Transdermal Bioavailability of Resveratrol: In-Vitro and in-Vivo Study. Colloids Surf. B Biointerfaces 2016, 148, 650–656. [Google Scholar] [CrossRef] [PubMed]
- Krishnaiah, Y.S.R.; Yang, Y.; Hunt, R.L.; Khan, M.A. Cold Fl Ow of Estradiol Transdermal Systems: In Fl Uence of Drug Loss on the in vitro Fl Ux and Drug Transfer across Human Epidermis. Int. J. Pharm. 2014, 477, 73–80. [Google Scholar] [CrossRef] [PubMed]
- Chien, Y.W.; Liu, J.C. Transdermal Drug Delivery Systems. J. Biomater. Appl. 1986, 1, 183–206. [Google Scholar] [CrossRef] [PubMed]
- Jung, E.; Young, E.; Choi, H.; Ban, S.; Choi, S.; Sun, J.; Yoon, I.; Kim, D. Development of Drug-in-Adhesive Patch Formulations for Transdermal Delivery of Fl Uoxetine: In Vitro and in vivo Evaluations. Int. J. Pharm. 2015, 487, 49–55. [Google Scholar] [CrossRef]
- Mohamed, L.A.; Kamal, N.; Elfakhri, K.H.; Ibrahim, S.; Ashraf, M.; Zidan, A.S. Application of Synthetic Membranes in Establishing Bio-Predictive IVPT for Testosterone Transdermal Gel. Int. J. Pharm. 2020, 586, 119572. [Google Scholar] [CrossRef] [PubMed]
- Kuznetsova, D.A.; Vasileva, L.A.; Gaynanova, G.A.; Vasilieva, E.A.; Lenina, O.A.; Nizameev, I.R.; Kadirov, M.K.; Petrov, K.A.; Zakharova, L.Y.; Sinyashin, O.G. Cationic Liposomes Mediated Transdermal Delivery of Meloxicam and Ketoprofen: Optimization of the Composition, in vitro and in vivo Assessment of Efficiency. Int. J. Pharm. 2021, 605, 120803. [Google Scholar] [CrossRef]
- Yang, Y.; Manda, P.; Pavurala, N.; Khan, M.A.; Krishnaiah, Y.S.R. Development and Validation of in vitro-in vivo Correlation (IVIVC) for Estradiol Transdermal Drug Delivery Systems. J. Control. Release 2015, 210, 58–66. [Google Scholar] [CrossRef]
- Boscariol, R.; Oliveira Junior, J.M.; Baldo, D.A.; Balcão, V.M.; Vila, M.M.D.C. Transdermal Permeation of Curcumin Promoted by Choline Geranate Ionic Liquid: Potential for the Treatment of Skin Diseases. Saudi Pharm. J. 2022, 30, 382–397. [Google Scholar] [CrossRef]
- Patel, N.; Jain, S.; Lin, S. Transdermal Iontophoretic Delivery of Tacrine Hydrochloride: Correlation between in vitro Permeation and in vivo Performance in Rats. Int. J. Pharm. 2016, 513, 393–403. [Google Scholar] [CrossRef]
- Puri, A.; Frempong, D.; Mishra, D.; Dogra, P. Microneedle-Mediated Transdermal Delivery of Naloxone Hydrochloride for Treatment of Opioid Overdose. Int. J. Pharm. 2021, 604, 120739. [Google Scholar] [CrossRef]
- Ottaviani, G.; Martel, S.; Carrupt, P.-A. Parallel Artificial Membrane Permeability Assay: A New Membrane for the Fast Prediction of Passive Human Skin Permeability. J. Med. Chem. 2006, 49, 3948–3954. [Google Scholar] [CrossRef] [PubMed]
- Sinkó, B.; Garrigues, T.M.; Balogh, G.T.; Nagy, Z.K.; Tsinman, O.; Avdeef, A.; Takács-Novák, K. Skin–PAMPA: A New Method for Fast Prediction of Skin Penetration. Eur. J. Pharm. Sci. 2012, 45, 698–707. [Google Scholar] [CrossRef] [PubMed]
- Sinkó, B.; Kökösi, J.; Avdeef, A.; Takács-Novák, K. A PAMPA Study of the Permeability-Enhancing Effect of New Ceramide Analogues. Chem. Biodivers. 2009, 6, 1867–1874. [Google Scholar] [CrossRef] [PubMed]
- Pulsoni, I.; Lubda, M.; Aiello, M.; Fedi, A.; Marzagalli, M.; von Hagen, J.; Scaglione, S. Comparison Between Franz Diffusion Cell and a Novel Micro-Physiological System for In Vitro Penetration Assay Using Different Skin Models. SLAS Technol. 2022, 27, 161–171. [Google Scholar] [CrossRef]
- Van De Sandt, J.J.M.; Van Burgsteden, J.A.; Cage, S.; Carmichael, P.L.; Dick, I.; Kenyon, S.; Korinth, G.; Larese, F.; Limasset, J.C.; Maas, W.J.M.; et al. In Vitro Predictions of Skin Absorption of Caffeine, Testosterone, and Benzoic Acid: A Multi-Centre Comparison Study. Regul. Toxicol. Pharmacol. 2004, 39, 271–281. [Google Scholar] [CrossRef]
- Mohammadi, M.H.; Heidary Araghi, B.; Beydaghi, V.; Geraili, A.; Moradi, F.; Jafari, P.; Janmaleki, M.; Valente, K.P.; Akbari, M.; Sanati-Nezhad, A. Skin Diseases Modeling Using Combined Tissue Engineering and Microfluidic Technologies. Adv. Healthc. Mater. 2016, 5, 2459–2480. [Google Scholar] [CrossRef]
- Hopf, N.B.; Champmartin, C.; Schenk, L.; Berthet, A.; Chedik, L.; Du Plessis, J.L.; Franken, A.; Frasch, F.; Gaskin, S.; Johanson, G.; et al. Reflections on the OECD Guidelines for in vitro Skin Absorption Studies. Regul. Toxicol. Pharmacol. 2020, 117, 104752. [Google Scholar] [CrossRef]
- Yousuf, Y.; Amini-Nik, S.; Jeschke, M.G. Overall Perspective on the Clinical Importance of Skin Models. In Skin Tissue Models for Regenerative Medicine; Elsevier: Amsterdam, The Netherlands, 2018; pp. 39–54. [Google Scholar]
- Edmondson, R.; Broglie, J.J.; Adcock, A.F.; Yang, L. Three-Dimensional Cell Culture Systems and Their Applications in Drug Discovery and Cell-Based Biosensors. Assay Drug Dev. Technol. 2014, 12, 207–218. [Google Scholar] [CrossRef]
- van den Broek, L.J.; Bergers, L.I.J.C.; Reijnders, C.M.A.; Gibbs, S. Progress and Future Prospectives in Skin-on-Chip Development with Emphasis on the Use of Different Cell Types and Technical Challenges. Stem Cell Rev. Reports 2017, 13, 418–429. [Google Scholar] [CrossRef]
- Zhang, Q.; Sito, L.; Mao, M.; He, J.; Zhang, Y.S.; Zhao, X. Current Advances in Skin-on-a-Chip Models for Drug Testing. Microphysiological Syst. 2018, 2, 4. [Google Scholar] [CrossRef]
- Antoni, D.; Burckel, H.; Josset, E.; Noel, G. Three-Dimensional Cell Culture: A Breakthrough in vivo. Int. J. Mol. Sci. 2015, 16, 5517–5527. [Google Scholar] [CrossRef] [PubMed]
- Netzlaff, F.; Lehr, C.-M.; Wertz, P.W.; Schaefer, U.F. The Human Epidermis Models EpiSkin®, SkinEthic® and EpiDerm®: An Evaluation of Morphology and Their Suitability for Testing Phototoxicity, Irritancy, Corrosivity, and Substance Transport. Eur. J. Pharm. Biopharm. 2005, 60, 167–178. [Google Scholar] [CrossRef] [PubMed]
- Neupane, R.; Boddu, S.H.S.; Renukuntla, J.; Babu, R.J.; Tiwari, A.K. Alternatives to Biological Skin in Permeation Studies: Current Trends and Possibilities. Pharmaceutics 2020, 12, 152. [Google Scholar] [CrossRef] [PubMed]
- Alépée, N.; Grandidier, M.-H.; Cotovio, J. Usefulness of the EpiSkinTM Reconstructed Human Epidermis Model within Integrated Approaches on Testing and Assessment (IATA) for Skin Corrosion and Irritation. Toxicol. Vitr. 2019, 54, 147–167. [Google Scholar] [CrossRef]
- Kandárová, H.; Hayden, P.; Klausner, M.; Kubilus, J.; Kearney, P.; Sheasgreen, J. In Vitro Skin Irritation Testing: Improving the Sensitivity of the EpiDerm Skin Irritation Test Protocol. Altern. to Lab. Anim. 2009, 37, 671–689. [Google Scholar] [CrossRef]
- Pellevoisin, C.; Videau, C.; Briotet, D.; Grégoire, C.; Tornier, C.; Alonso, A.; Rigaudeau, A.S.; Bouez, C.; Seyler, N. SkinEthicTM RHE for in vitro Evaluation of Skin Irritation of Medical Device Extracts. Toxicol. Vitr. 2018, 50, 418–425. [Google Scholar] [CrossRef]
- Dreher, F.; Fouchard, F.; Patouillet, C.; Andrian, M.; Simonnet, J.-T.; Benech-Kieffer, F. Comparison of Cutaneous Bioavailability of Cosmetic Preparations Containing Caffeine or α-Tocopherol Applied on Human Skin Models or Human Skin Ex Vivo at Finite Doses. Skin Pharmacol. Physiol. 2002, 15, 40–58. [Google Scholar] [CrossRef]
- Schäfer-Korting, M.; Bock, U.; Diembeck, W.; Düsing, H.-J.; Gamer, A.; Haltner-Ukomadu, E.; Hoffmann, C.; Kaca, M.; Kamp, H.; Kersen, S.; et al. The Use of Reconstructed Human Epidermis for Skin Absorption Testing: Results of the Validation Study. Altern. to Lab. Anim. 2008, 36, 161–187. [Google Scholar] [CrossRef]
- Lotte, C.; Patouillet, C.; Zanini, M.; Messager, A.; Roguet, R. Permeation and Skin Absorption: Reproducibility of Various Industrial Reconstructed Human Skin Models. Skin Pharmacol. Physiol. 2002, 15, 18–30. [Google Scholar] [CrossRef]
- Jírová, D.; Basketter, D.; Liebsch, M.; Bendová, H.; Kejlová, K.; Marriott, M.; Kandárová, H. Comparison of Human Skin Irritation Patch Test Data with in vitro Skin Irritation Assays and Animal Data. Contact Dermat. 2010, 62, 109–116. [Google Scholar] [CrossRef]
- Van Gele, M.; Geusens, B.; Brochez, L.; Speeckaert, R.; Lambert, J. Three-Dimensional Skin Models as Tools for Transdermal Drug Delivery: Challenges and Limitations. Expert Opin. Drug Deliv. 2011, 8, 705–720. [Google Scholar] [CrossRef] [PubMed]
- Bernerd, F.; Asselineau, D. An Organotypic Model of Skin to Study Photodamage and Photoprotection in vitro. J. Am. Acad. Dermatol. 2008, 58, S155–S159. [Google Scholar] [CrossRef] [PubMed]
- Reisinger, K.; Blatz, V.; Brinkmann, J.; Downs, T.R.; Fischer, A.; Henkler, F.; Hoffmann, S.; Krul, C.; Liebsch, M.; Luch, A.; et al. Validation of the 3D Skin Comet Assay Using Full Thickness Skin Models: Transferability and Reproducibility. Mutat. Res. Toxicol. Environ. Mutagen. 2018, 827, 27–41. [Google Scholar] [CrossRef] [PubMed]
- Pageon, H.; Zucchi, H.; Asselineau, D. Distinct and Complementary Roles of Papillary and Reticular Fibroblasts in Skin Morphogenesis and Homeostasis. Eur. J. Dermatology 2012, 22, 324–332. [Google Scholar] [CrossRef] [PubMed]
- Markiewicz, E.; Jerome, J.; Mammone, T.; Idowu, O.C. Anti-Glycation and Anti-Aging Properties of Resveratrol Derivatives in the in-Vitro 3D Models of Human Skin. Clin. Cosmet. Investig. Dermatol. 2022, 15, 911–927. [Google Scholar] [CrossRef] [PubMed]
- Zoio, P.; Ventura, S.; Leite, M.; Oliva, A. Pigmented Full-Thickness Human Skin Model Based on a Fibroblast-Derived Matrix for Long-Term Studies. Tissue Eng. Part C Methods 2021, 27, 433–443. [Google Scholar] [CrossRef] [PubMed]
- Hamada, H.; Shimoda, K.; Horio, Y.; Ono, T.; Hosoda, R.; Nakayama, N.; Urano, K. Pterostilbene and Its Glucoside Induce Type XVII Collagen Expression. Nat. Prod. Commun. 2017, 12, 1934578X1701200. [Google Scholar] [CrossRef]
- Ackermann, K.; Lombardi Borgia, S.; Korting, H.C.; Mewes, K.R.; Schäfer-Korting, M. The Phenion® Full-Thickness Skin Model for Percutaneous Absorption Testing. Skin Pharmacol. Physiol. 2010, 23, 105–112. [Google Scholar] [CrossRef]
- Bataillon, M.; Lelièvre, D.; Chapuis, A.; Thillou, F.; Autourde, J.B.; Durand, S.; Boyera, N.; Rigaudeau, A.-S.; Besné, I.; Pellevoisin, C. Characterization of a New Reconstructed Full Thickness Skin Model, T-SkinTM, and Its Application for Investigations of Anti-Aging Compounds. Int. J. Mol. Sci. 2019, 20, 2240. [Google Scholar] [CrossRef]
- Li, Z.; Hui, J.; Yang, P.; Mao, H. Microfluidic Organ-on-a-Chip System for Disease Modeling and Drug Development. Biosensors 2022, 12, 370. [Google Scholar] [CrossRef]
- Risueño, I.; Valencia, L.; Jorcano, J.L.; Velasco, D. Skin-on-a-Chip Models: General Overview and Future Perspectives. APL Bioeng. 2021, 5, 030901. [Google Scholar] [CrossRef] [PubMed]
- Abaci, H.E.; Gledhill, K.; Guo, Z.; Christiano, A.M.; Shuler, M.L. Pumpless Microfluidic Platform for Drug Testing on Human Skin Equivalents. Lab Chip 2015, 15, 882–888. [Google Scholar] [CrossRef] [PubMed]
- Song, H.J.; Lim, H.Y.; Chun, W.; Choi, K.C.; Sung, J.H.; Sung, G.Y. Fabrication of a Pumpless, Microfluidic Skin Chip from Different Collagen Sources. J. Ind. Eng. Chem. 2017, 56, 375–381. [Google Scholar] [CrossRef]
- Mo, L.; Lu, G.; Ou, X.; Ouyang, D. Saudi Journal of Biological Sciences Formulation and Development of Novel Control Release Transdermal Patches of Carvedilol to Improve Bioavailability for the Treatment of Heart Failure. Saudi J. Biol. Sci. 2022, 29, 266–272. [Google Scholar] [CrossRef] [PubMed]
- Morsi, N.M.; Aboelwafa, A.A.; Dawoud, M.H.S. Improved Bioavailability of Timolol Maleate via Transdermal Transfersomal Gel: Statistical Optimization, Characterization, and Pharmacokinetic Assessment. J. Adv. Res. 2016, 7, 691–701. [Google Scholar] [CrossRef]
- Kalaria, D.R.; Singhal, M.; Patravale, V.; Merino, V. European Journal of Pharmaceutics and Biopharmaceutics Simultaneous Controlled Iontophoretic Delivery of Pramipexole and Rasagiline in vitro and in vivo: Transdermal Polypharmacy to Treat Parkinson ’ s Disease. Eur. J. Pharm. Biopharm. 2018, 127, 204–212. [Google Scholar] [CrossRef]
- Domínguez-robles, J.; Tekko, I.A.; Larra, E.; Ramadon, D.; Donnelly, R.F. Versatility of Hydrogel-Forming Microneedles in in vitro Transdermal Delivery of Tuberculosis Drugs. Eur. J. Pharm. Biopharm. 2021, 158, 294–312. [Google Scholar] [CrossRef]
- Calatayud-pascual, M.A.; Balaguer-fernández, C.; Serna-jiménez, C.E.; Rio-sancho, S. Del Effect of Iontophoresis on in vitro Transdermal Absorption of Almotriptan. Int. J. Pharm. 2011, 416, 189–194. [Google Scholar] [CrossRef]
- Herkenne, C.; Naik, A.; Kalia, Y.N.; Hadgraft, J.; Guy, R.H. Ibuprofen Transport into and through Skin from Topical Formulations: In vitro-in vivo Comparison. J. Invest. Dermatol. 2007, 127, 135–142. [Google Scholar] [CrossRef]
- Godin, B.; Touitou, E. Transdermal Skin Delivery: Predictions for Humans from in vivo, Ex vivo and Animal Models☆. Adv. Drug Deliv. Rev. 2007, 59, 1152–1161. [Google Scholar] [CrossRef]
- Argenziano, M.; Haimhoffer, A.; Bastiancich, C.; Jicsinszky, L.; Caldera, F.; Trotta, F.; Scutera, S.; Alotto, D.; Fumagalli, M.; Musso, T.; et al. In Vitro Enhanced Skin Permeation and Retention of Imiquimod Loaded in β-Cyclodextrin Nanosponge Hydrogel. Pharmaceutics 2019, 11, 138. [Google Scholar] [CrossRef]
- U.S. Department of Health and Human Services Food and DrugAdministration. Transdermal and Topical Delivery Systems—Product Development and Quality Considerations; U.S. Department of Health and Human Services Food and Drug Administration: Silver Spring, MD, USA, 2019. [Google Scholar]
- Committee for Medicinal Products for Human Use (CHMP). Guideline on Quality of Transdermal Patches; Committee for Medicinal Products for Human Use (CHMP): London, UK, 2014. [Google Scholar]
- Committee for Medicinal Products for Human Use (CHMP). Guideline on Quality and Equivalence of Topical Products; Committee for Medicinal Products for Human Use (CHMP): London, UK, 2018. [Google Scholar]
- Alvarez-Trabado, J.; Diebold, Y.; Sanchez, A. Designing Lipid Nanoparticles for Topical Ocular Drug Delivery. Int. J. Pharm. 2017, 532, 204–217. [Google Scholar] [CrossRef] [PubMed]
- Lieto, K.; Skopek, R.; Lewicka, A.; Stelmasiak, M.; Klimaszewska, E.; Zelent, A.; Szymański, Ł.; Lewicki, S. Looking into the Eyes—In Vitro Models for Ocular Research. Int. J. Mol. Sci. 2022, 23, 9158. [Google Scholar] [CrossRef] [PubMed]
- Draize, J.H.; Woodard, G.; Calvery, H.O. Methods for the Study of Irritation and Toxicity of Substances Applied Topically to the Skin and Mucous Membranes. J. Pharmacol. Exp. Ther. 1944, 82, 377–390. [Google Scholar]
- Food and Drug Administration. Draft Guidance on Nepafenac; Food and Drug Administration: Silver Spring, MD, USA, 2016. [Google Scholar]
- Food and Drug Administration. Draft Guidance on Cyclosporine; Food and Drug Administration: Silver Spring, MD, USA, 2022. [Google Scholar]
- Le Merdy, M.; Fan, J.; Bolger, M.B.; Lukacova, V.; Spires, J.; Tsakalozou, E.; Patel, V.; Xu, L.; Stewart, S.; Chockalingam, A.; et al. Application of Mechanistic Ocular Absorption Modeling and Simulation to Understand the Impact of Formulation Properties on Ophthalmic Bioavailability in Rabbits: A Case Study Using Dexamethasone Suspension. AAPS J. 2019, 21, 65. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.H.; Lionberger, R.A. Clinical, Pharmacokinetic, and In Vitro Studies to Support Bioequivalence of Ophthalmic Drug Products. AAPS J. 2016, 18, 1032–1038. [Google Scholar] [CrossRef]
- Rahman, Z.; Xu, X.; Katragadda, U.; Krishnaiah, Y.S.R.; Yu, L.; Khan, M.A. Quality by Design Approach for Understanding the Critical Quality Attributes of Cyclosporine Ophthalmic Emulsion. Mol. Pharm. 2014, 11, 787–799. [Google Scholar] [CrossRef]
- Soliman, O.A.E.-A.; Mohamed, E.A.; Khatera, N.A.A. Enhanced Ocular Bioavailability of Fluconazole from Niosomal Gels and Microemulsions: Formulation, Optimization, and in vitro–in vivo Evaluation. Pharm. Dev. Technol. 2019, 24, 48–62. [Google Scholar] [CrossRef]
- Verma, P.; Gupta, R.N.; Jha, A.K.; Pandey, R. Development, in vitro and in vivo Characterization of Eudragit RL 100 Nanoparticles for Improved Ocular Bioavailability of Acetazolamide. Drug Deliv. 2013, 20, 269–276. [Google Scholar] [CrossRef]
- Luo, Q.; Yang, J.; Xu, H.; Shi, J.; Liang, Z.; Zhang, R.; Lu, P.; Pu, G.; Zhao, N.; Zhang, J. Sorafenib-Loaded Nanostructured Lipid Carriers for Topical Ocular Therapy of Corneal Neovascularization: Development, in-Vitro and in vivo Study. Drug Deliv. 2022, 29, 837–855. [Google Scholar] [CrossRef]
- Ashraf, O.; Nasr, M.; Nebsen, M.; Said, A.M.A.; Sammour, O. In Vitro Stabilization and in vivo Improvement of Ocular Pharmacokinetics of the Multi-Therapeutic Agent Baicalin: Delineating the Most Suitable Vesicular Systems. Int. J. Pharm. 2018, 539, 83–94. [Google Scholar] [CrossRef] [PubMed]
- Kaluzhny, Y.; Klausner, M. In Vitro Reconstructed 3D Corneal Tissue Models for Ocular Toxicology and Ophthalmic Drug Development. Vitr. Cell. Dev. Biol.-Anim. 2021, 57, 207–237. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, P.; Rupenthal, I.D. In Vitro and Ex Vivo Corneal Penetration and Absorption Models. Drug Deliv. Transl. Res. 2016, 6, 634–647. [Google Scholar] [CrossRef]
- Yang, P.; Dong, Y.; Huang, D.; Zhu, C.; Liu, H.; Pan, X.; Wu, C. Silk Fibroin Nanoparticles for Enhanced Bio-Macromolecule Delivery to the Retina. Pharm. Dev. Technol. 2019, 24, 575–583. [Google Scholar] [CrossRef]
- Yadav, M.; Schiavone, N.; Guzman-Aranguez, A.; Giansanti, F.; Papucci, L.; Perez de Lara, M.J.; Singh, M.; Kaur, I.P. Atorvastatin-Loaded Solid Lipid Nanoparticles as Eye Drops: Proposed Treatment Option for Age-Related Macular Degeneration (AMD). Drug Deliv. Transl. Res. 2020, 10, 919–944. [Google Scholar] [CrossRef]
- Jakubiak, P.; Cantrill, C.; Urtti, A.; Alvarez-Sánchez, R. Establishment of an In Vitro–In Vivo Correlation for Melanin Binding and the Extension of the Ocular Half-Life of Small-Molecule Drugs. Mol. Pharm. 2019, 16, 4890–4901. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Zhang, L.; Li, R.; Yan, M. New Resveratrol Micelle Formulation for Ocular Delivery: Characterization and in vitro/in vivo Evaluation. Drug Dev. Ind. Pharm. 2020, 46, 1960–1970. [Google Scholar] [CrossRef] [PubMed]
- Yousry, C.; Zikry, P.M.; Salem, H.M.; Basalious, E.B.; El-Gazayerly, O.N. Integrated Nanovesicular/Self-Nanoemulsifying System (INV/SNES) for Enhanced Dual Ocular Drug Delivery: Statistical Optimization, in vitro and in vivo Evaluation. Drug Deliv. Transl. Res. 2020, 10, 801–814. [Google Scholar] [CrossRef]
- Okur, N.Ü.; Yozgatli, V.; Okur, M.E. In vitro–in vivo Evaluation of Tetrahydrozoline-loaded Ocular in Situ Gels on Rabbits for Allergic Conjunctivitis Management. Drug Dev. Res. 2020, 81, 716–727. [Google Scholar] [CrossRef]
- Mohamed, H.B.; Attia Shafie, M.A.; Mekkawy, A.I. Chitosan Nanoparticles for Meloxicam Ocular Delivery: Development, In Vitro Characterization, and In Vivo Evaluation in a Rabbit Eye Model. Pharmaceutics 2022, 14, 893. [Google Scholar] [CrossRef]
- Liang, Z.; Zhang, Z.; Yang, J.; Lu, P.; Zhou, T.; Li, J.; Zhang, J. Assessment to the Antifungal Effects in vitro and the Ocular Pharmacokinetics of Solid-Lipid Nanoparticle in Rabbits. Int. J. Nanomed. 2021, 16, 7847–7857. [Google Scholar] [CrossRef]
- Li, X.; Nie, S.; Kong, J.; Li, N.; Ju, C.; Pan, W. A Controlled-Release Ocular Delivery System for Ibuprofen Based on Nanostructured Lipid Carriers. Int. J. Pharm. 2008, 363, 177–182. [Google Scholar] [CrossRef] [PubMed]
- Rathod, L.V.; Kapadia, R.; Sawant, K.K. A Novel Nanoparticles Impregnated Ocular Insert for Enhanced Bioavailability to Posterior Segment of Eye: In vitro, in vivo and Stability Studies. Mater. Sci. Eng. C 2017, 71, 529–540. [Google Scholar] [CrossRef] [PubMed]
- Gai, X.; Cheng, L.; Li, T.; Liu, D.; Wang, Y.; Wang, T.; Pan, W.; Yang, X. In Vitro and In Vivo Studies on a Novel Bioadhesive Colloidal System: Cationic Liposomes of Ibuprofen. AAPS PharmSciTech 2018, 19, 700–709. [Google Scholar] [CrossRef] [PubMed]
- Lai, S.; Wei, Y.; Wu, Q.; Zhou, K.; Liu, T.; Zhang, Y.; Jiang, N.; Xiao, W.; Chen, J.; Liu, Q.; et al. Liposomes for Effective Drug Delivery to the Ocular Posterior Chamber. J. Nanobiotechnol. 2019, 17, 64. [Google Scholar] [CrossRef] [PubMed]
| Study Type | Regulatory Acceptance or Opinion |
|---|---|
| Solubility |
|
| Dissolution |
|
| Permeability on artificial membrane |
|
| Cell culture models |
|
| Ex vivo models |
|
| Study Type | Regulatory Acceptance or Opinion |
|---|---|
| Solubility |
|
| Dissolution |
|
| Permeability on artificial membrane |
|
| Cell culture models |
|
| Ex vivo models |
|
| Study Type | Regulatory Acceptance or Opinion |
|---|---|
| Dissolution * |
|
| Permeability on artificial membrane |
|
| Cell culture models |
|
| Ex vivo models |
|
| Study Type | Regulatory Acceptance or Opinion |
|---|---|
| Dissolution |
|
| Permeability on artificial membrane |
|
| Cell culture models |
|
| Ex vivo models |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Józsa, L.; Nemes, D.; Pető, Á.; Kósa, D.; Révész, R.; Bácskay, I.; Haimhoffer, Á.; Vasvári, G. Recent Options and Techniques to Assess Improved Bioavailability: In Vitro and Ex Vivo Methods. Pharmaceutics 2023, 15, 1146. https://doi.org/10.3390/pharmaceutics15041146
Józsa L, Nemes D, Pető Á, Kósa D, Révész R, Bácskay I, Haimhoffer Á, Vasvári G. Recent Options and Techniques to Assess Improved Bioavailability: In Vitro and Ex Vivo Methods. Pharmaceutics. 2023; 15(4):1146. https://doi.org/10.3390/pharmaceutics15041146
Chicago/Turabian StyleJózsa, Liza, Dániel Nemes, Ágota Pető, Dóra Kósa, Réka Révész, Ildikó Bácskay, Ádám Haimhoffer, and Gábor Vasvári. 2023. "Recent Options and Techniques to Assess Improved Bioavailability: In Vitro and Ex Vivo Methods" Pharmaceutics 15, no. 4: 1146. https://doi.org/10.3390/pharmaceutics15041146
APA StyleJózsa, L., Nemes, D., Pető, Á., Kósa, D., Révész, R., Bácskay, I., Haimhoffer, Á., & Vasvári, G. (2023). Recent Options and Techniques to Assess Improved Bioavailability: In Vitro and Ex Vivo Methods. Pharmaceutics, 15(4), 1146. https://doi.org/10.3390/pharmaceutics15041146











