Mesoporous Silica Particles as Drug Delivery Systems—The State of the Art in Loading Methods and the Recent Progress in Analytical Techniques for Monitoring These Processes
Abstract
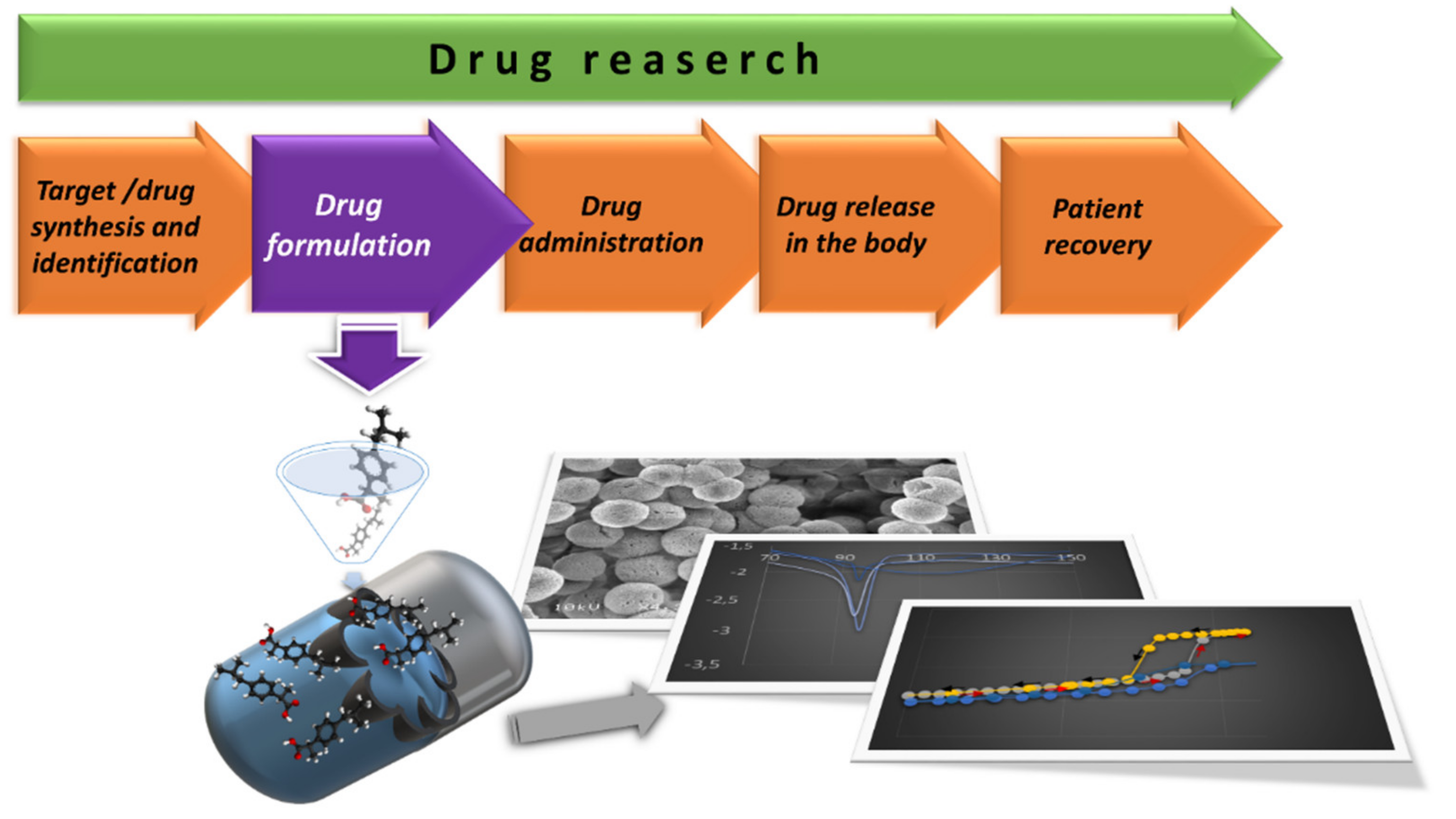
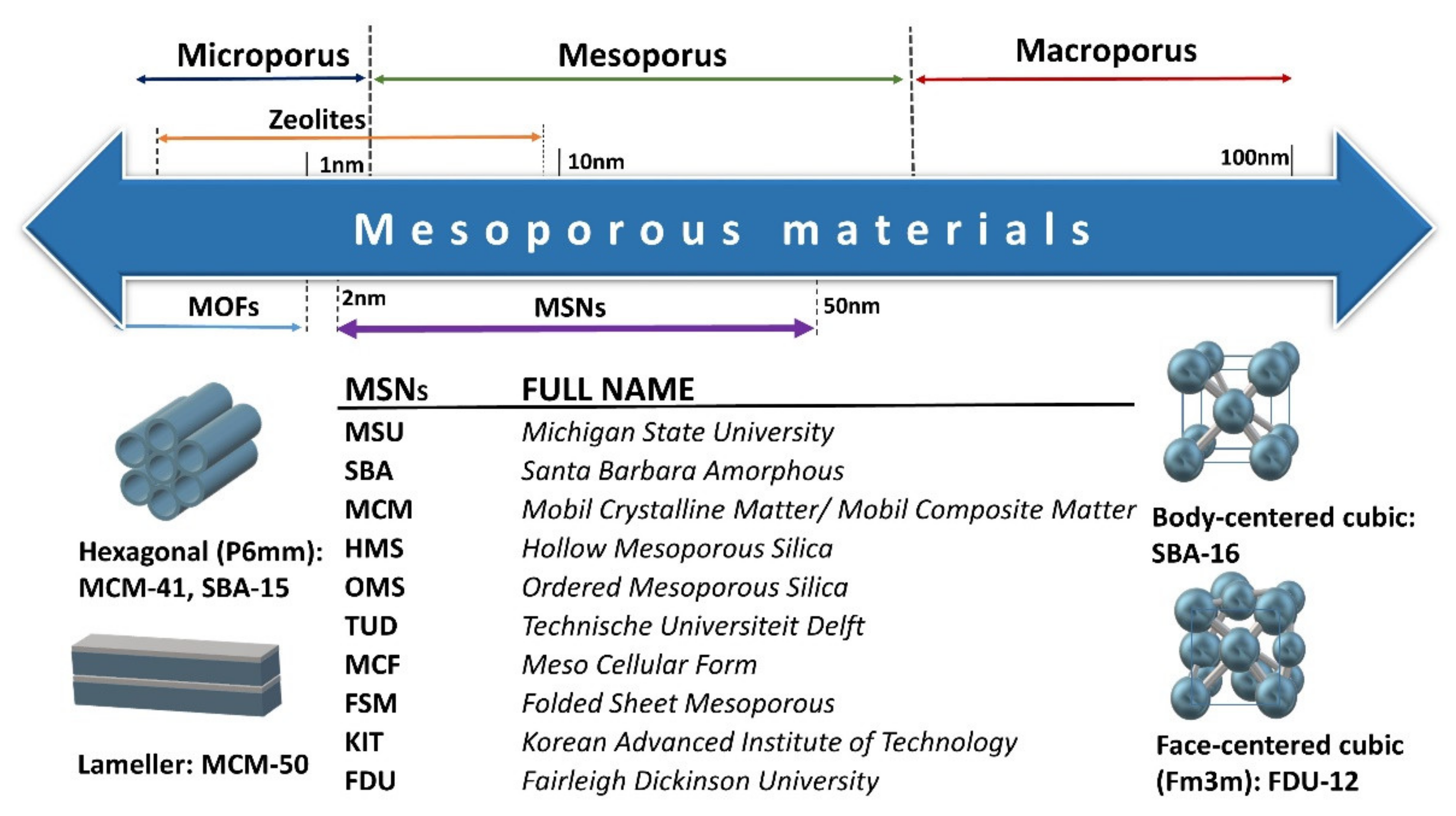
:1. Introduction
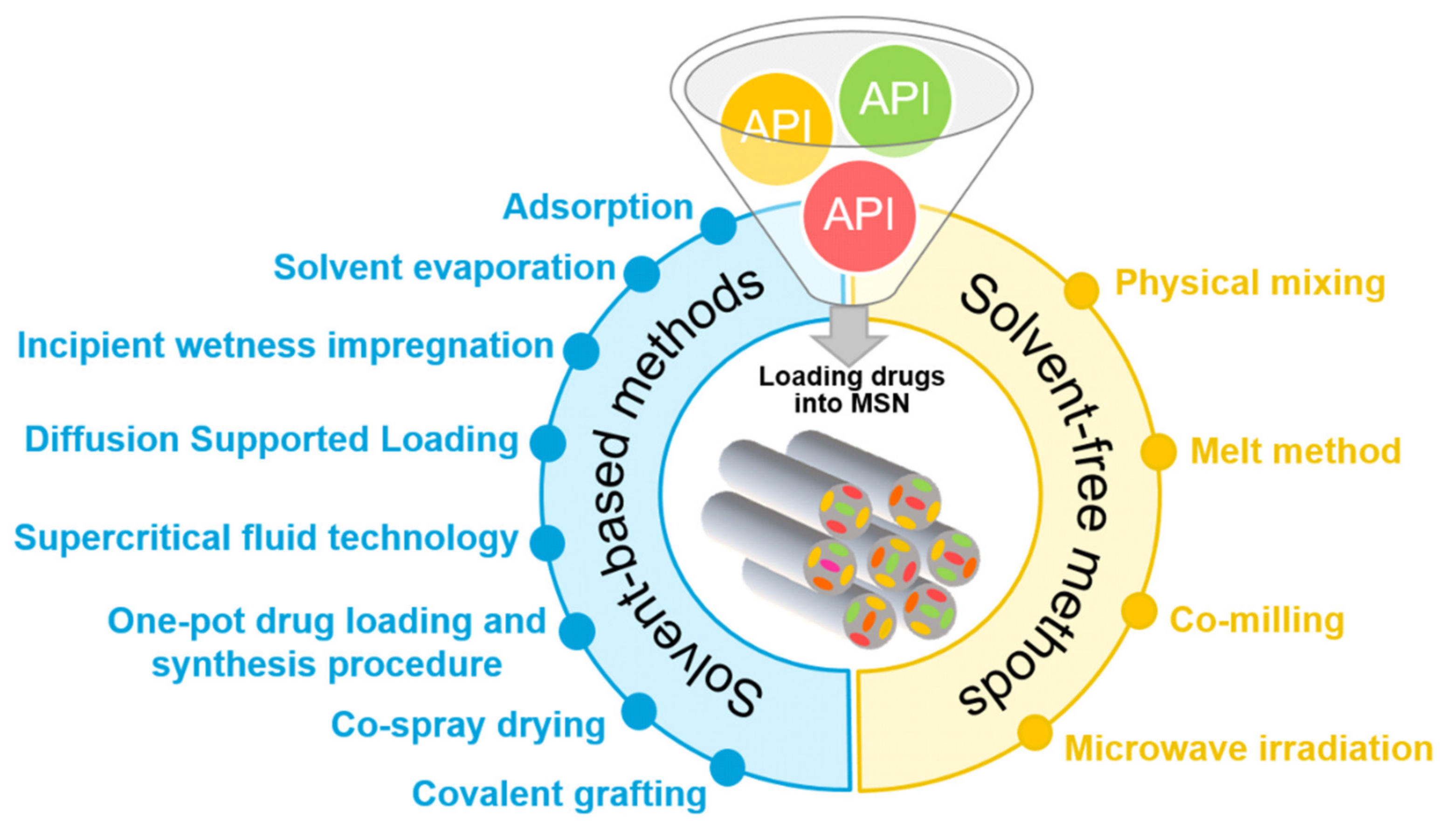
2. Drug Loading Methods
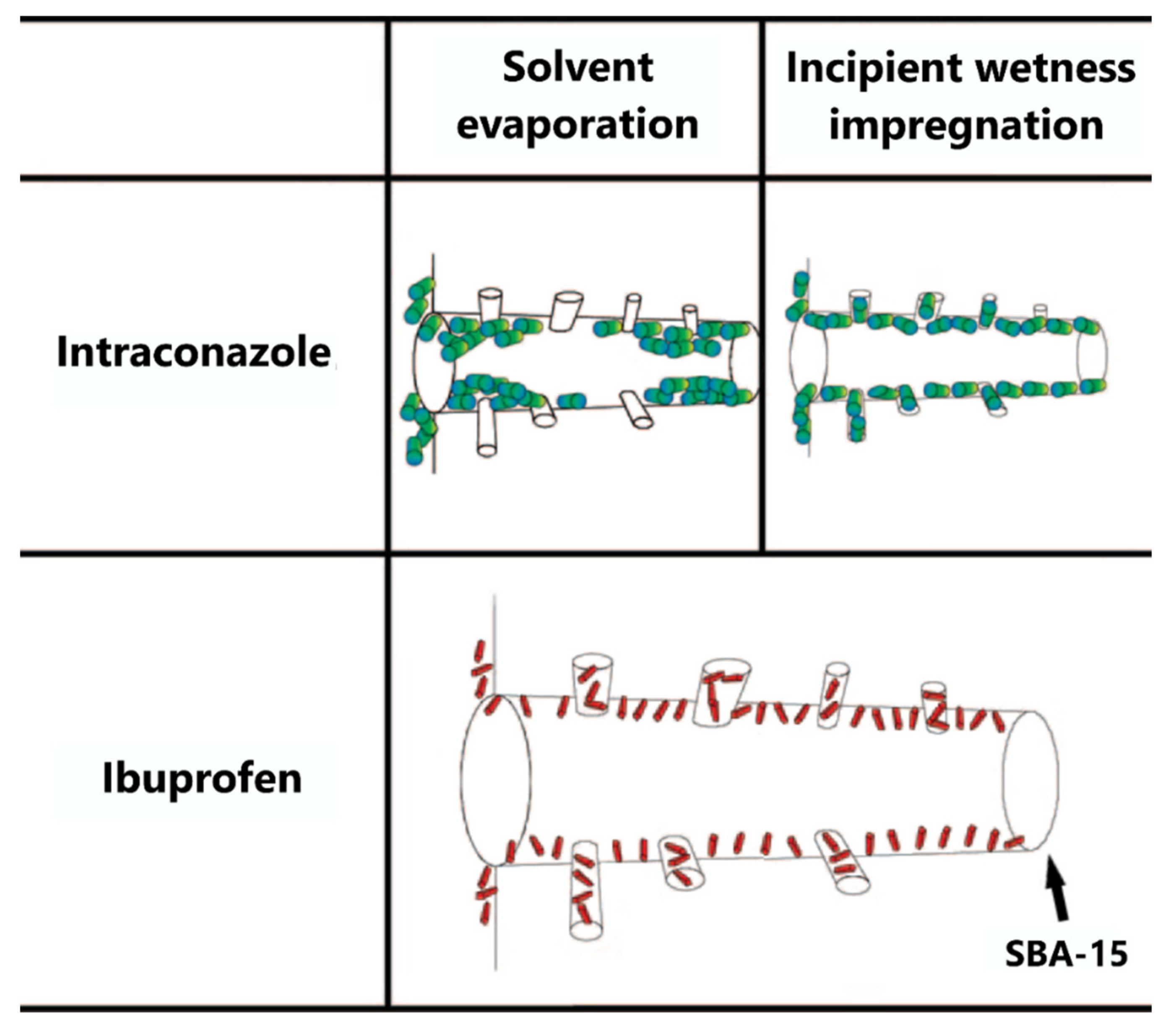
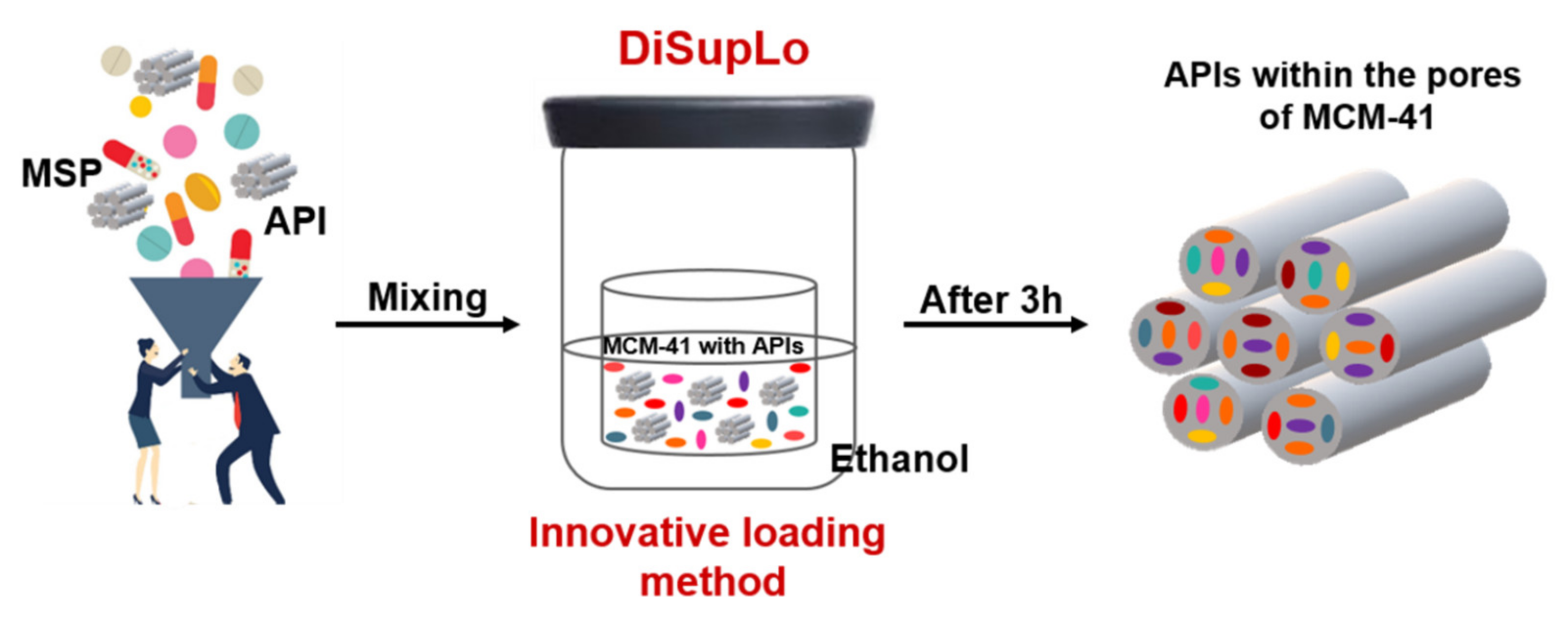
2.1. Solvent-Based Methods
2.2. Solvent-Free Methods
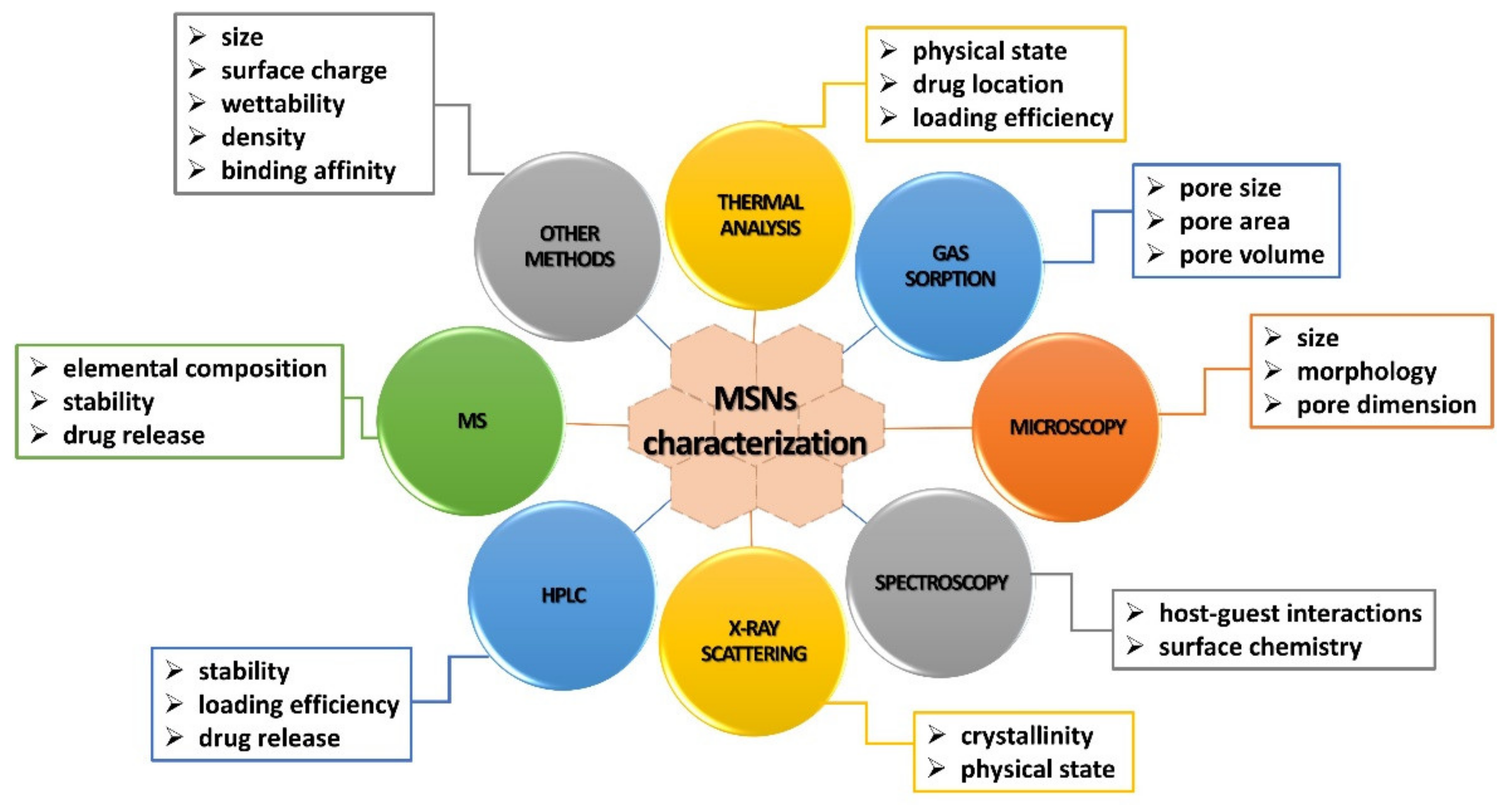
3. Analytical Techniques
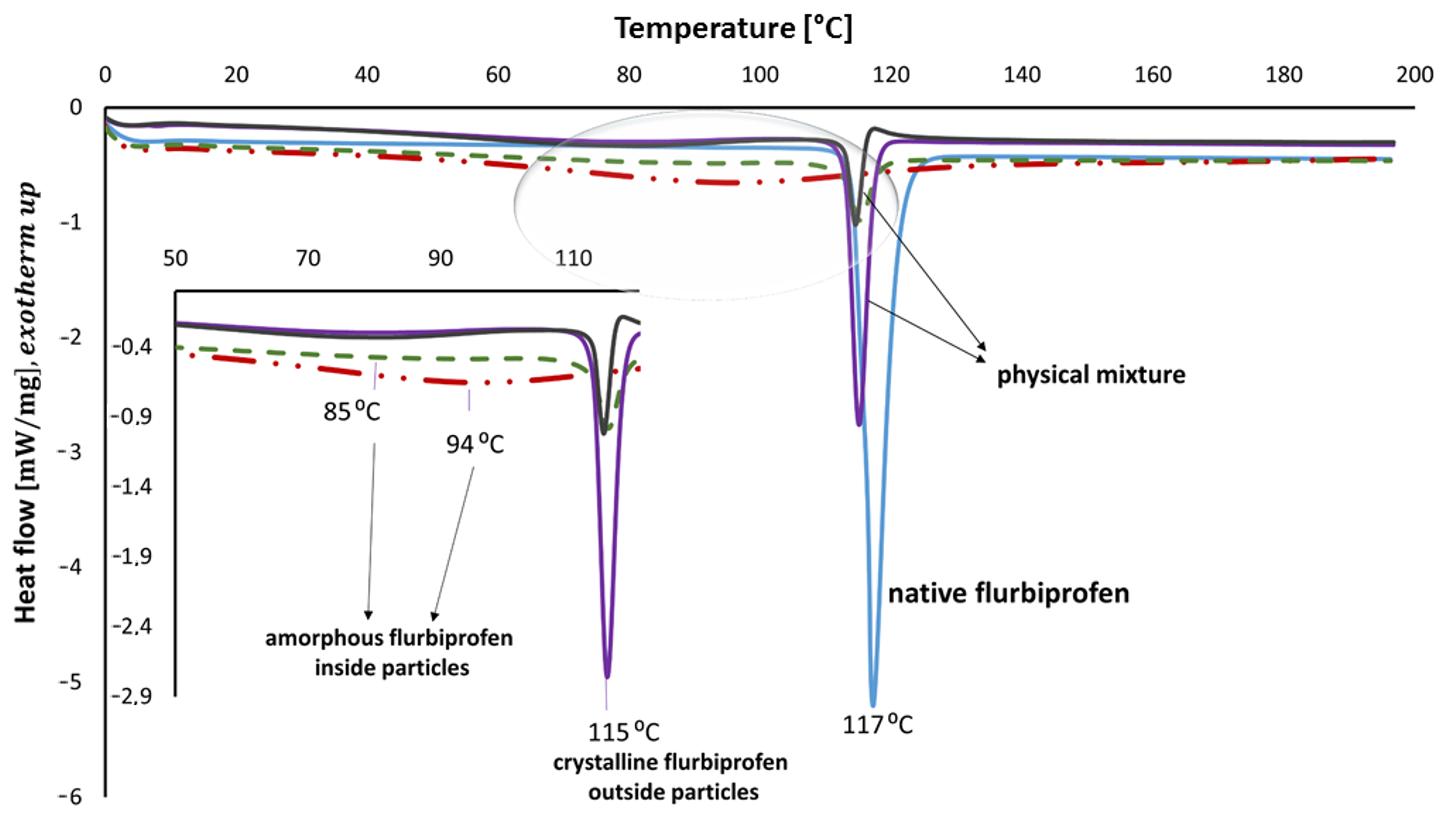
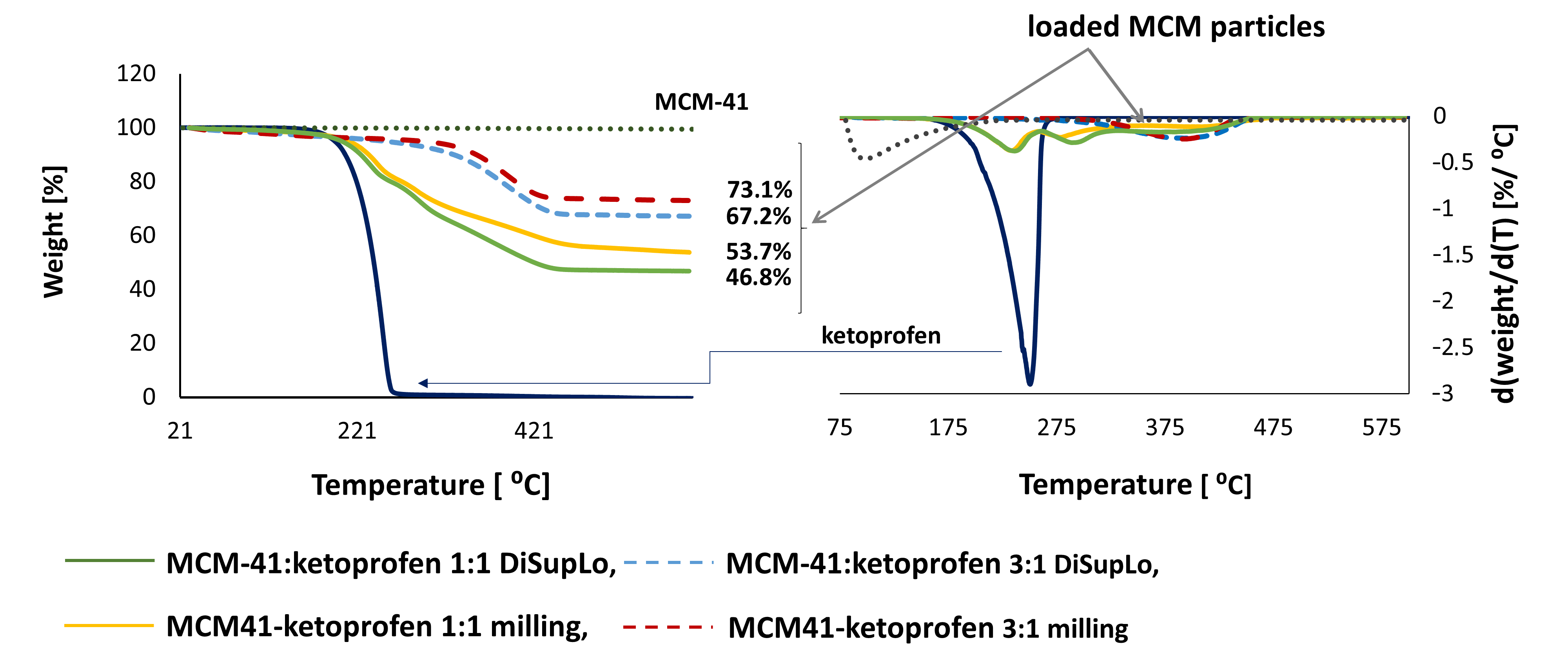
3.1. Thermal Analysis
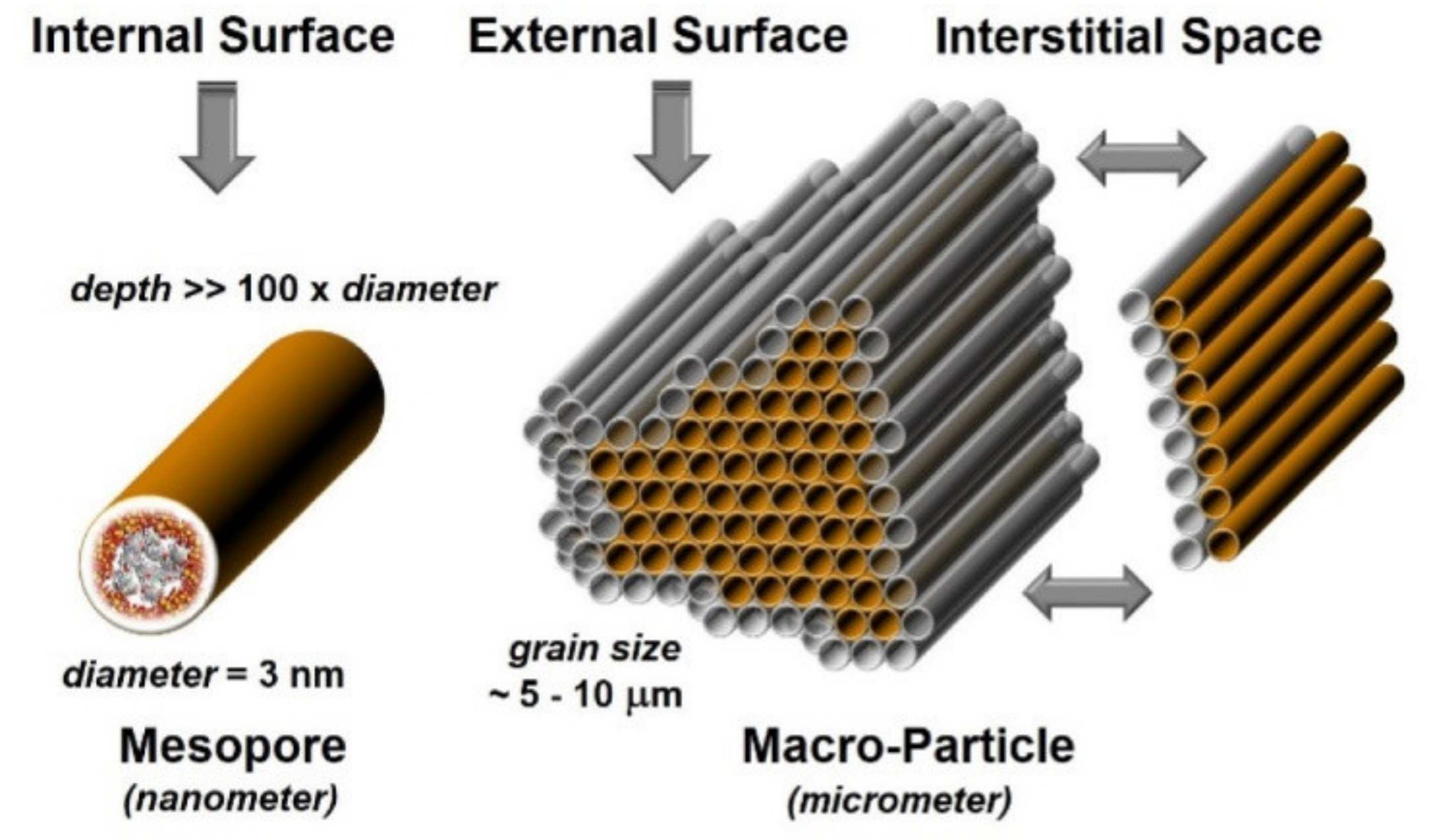
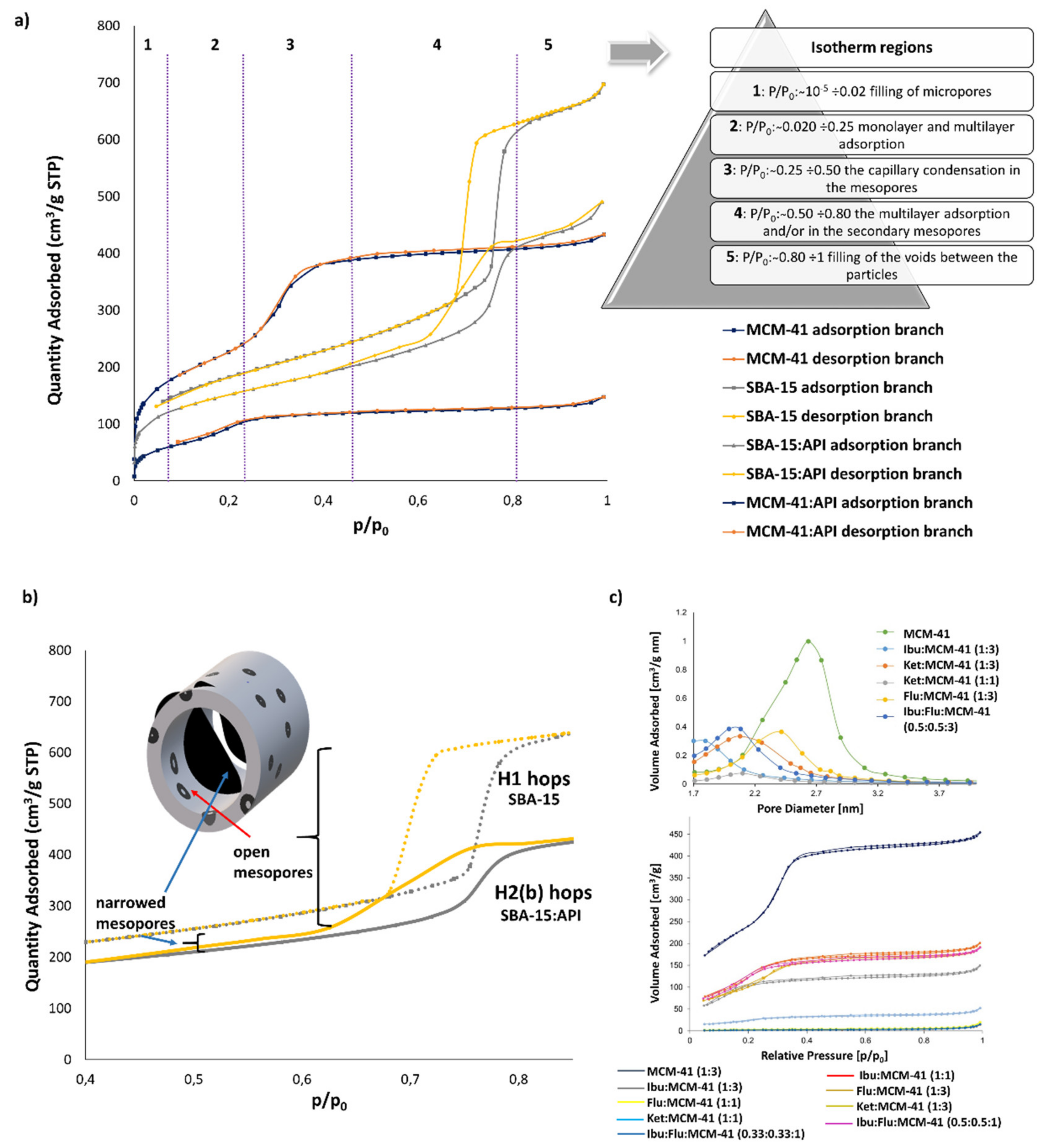
3.2. Gas Sorption
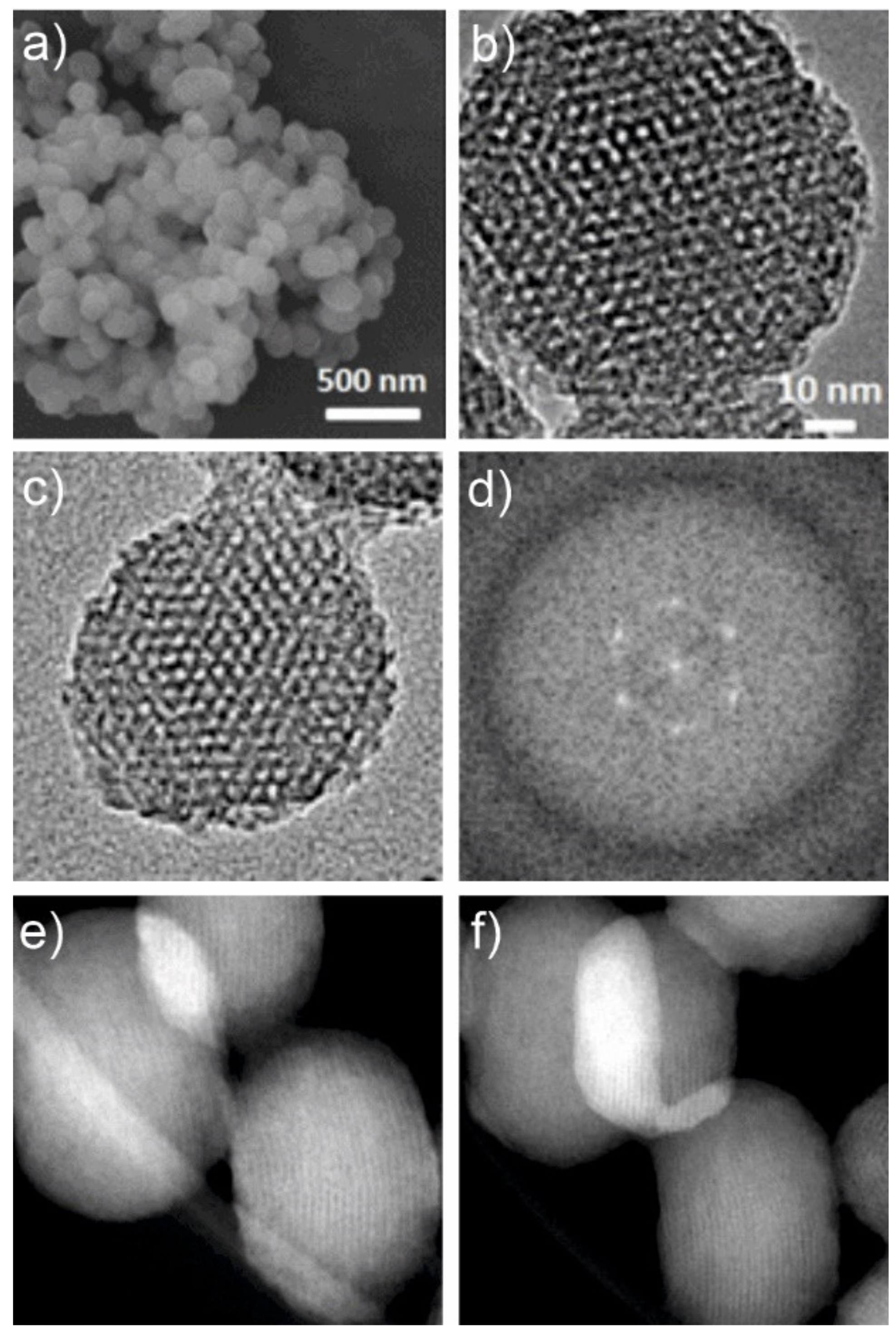
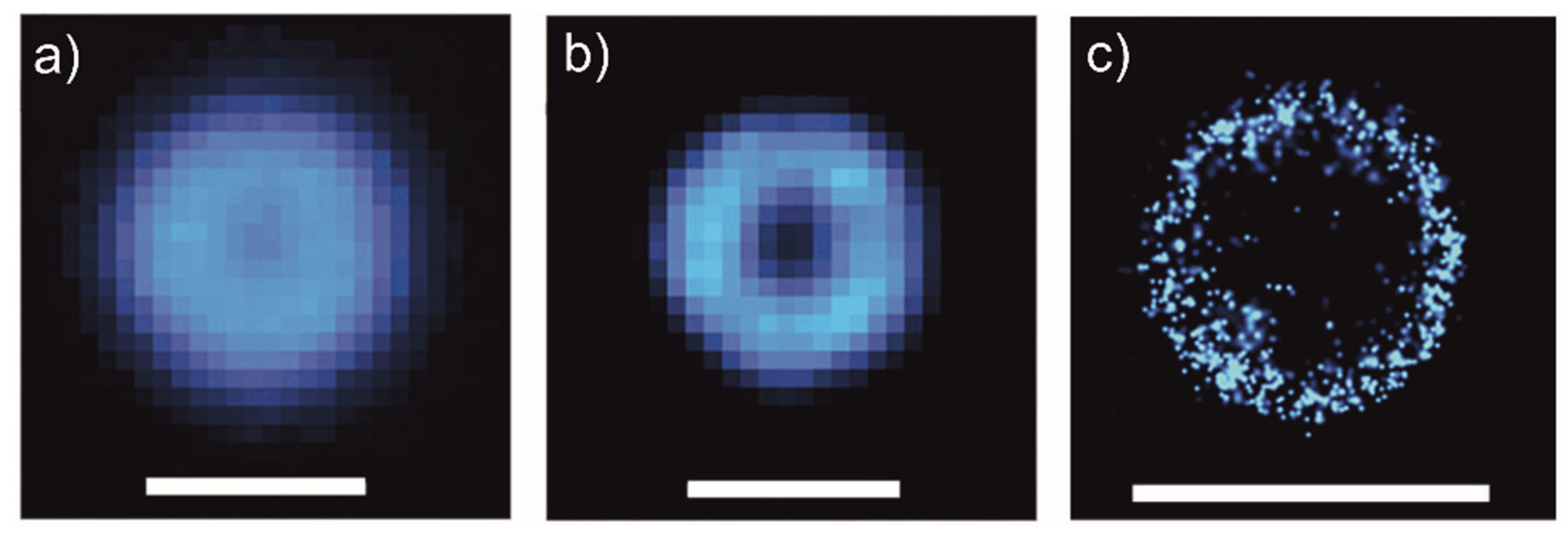
3.3. Microscopy
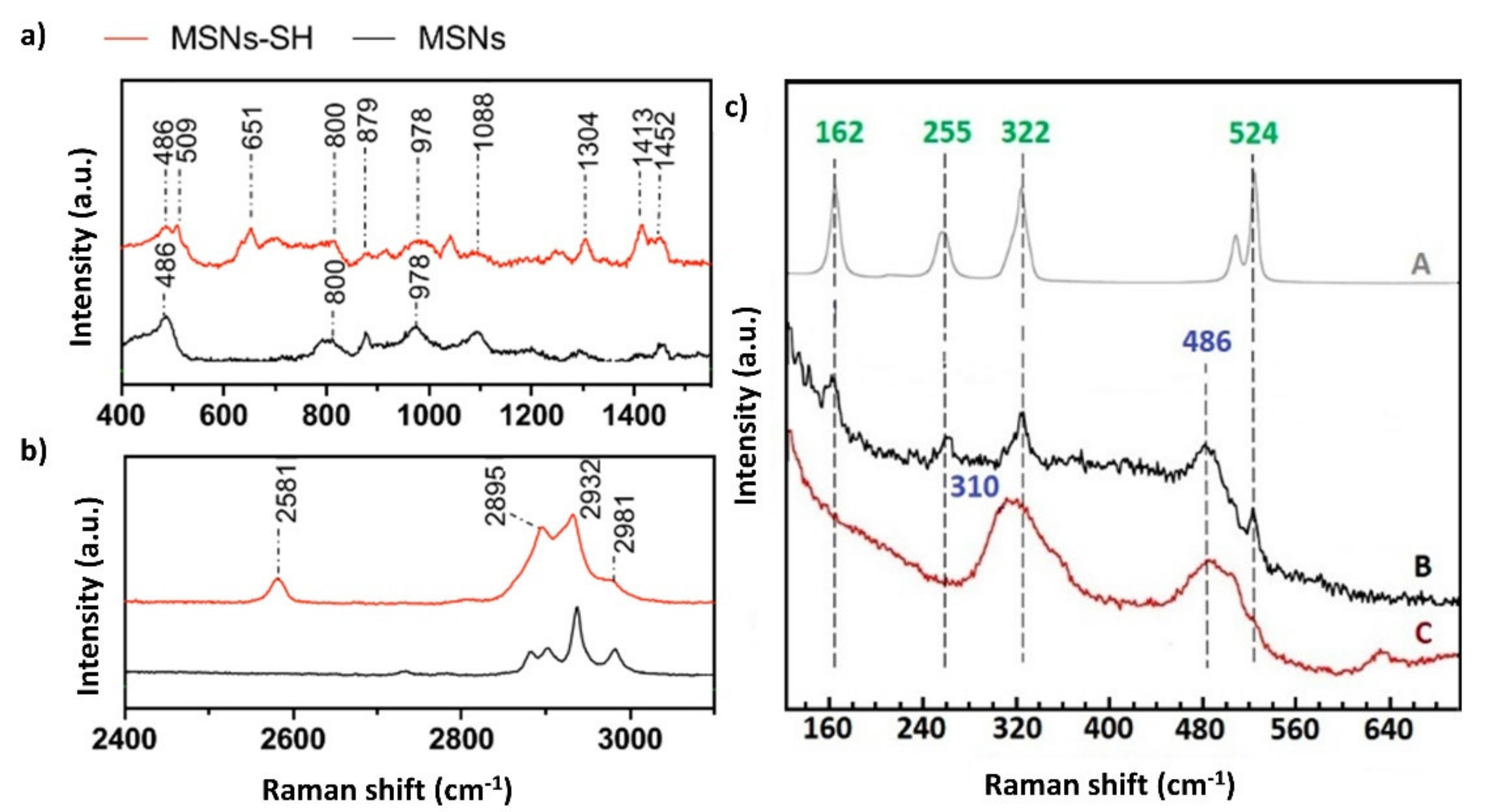
3.4. Spectroscopy
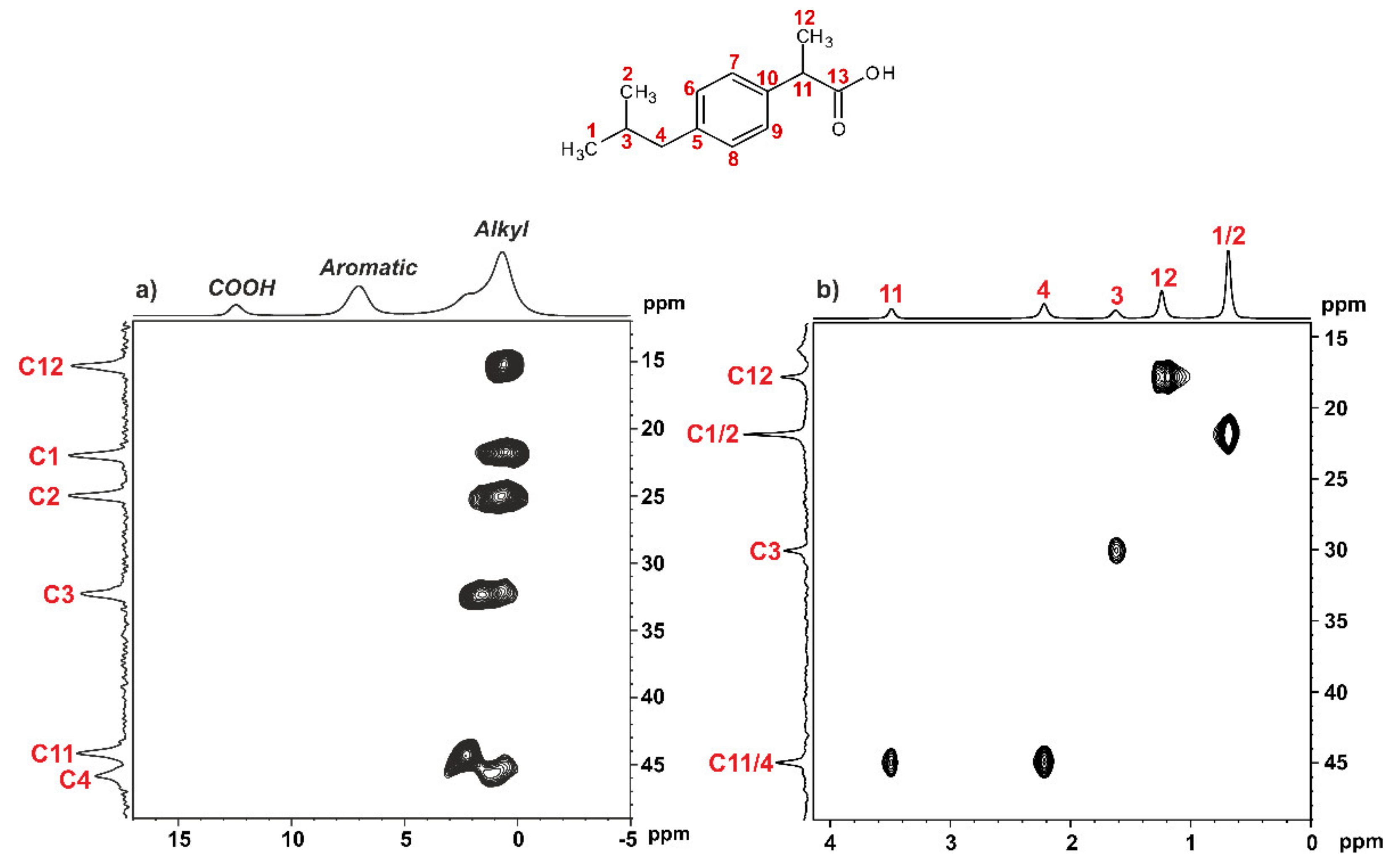
3.4.1. Solid-State NMR
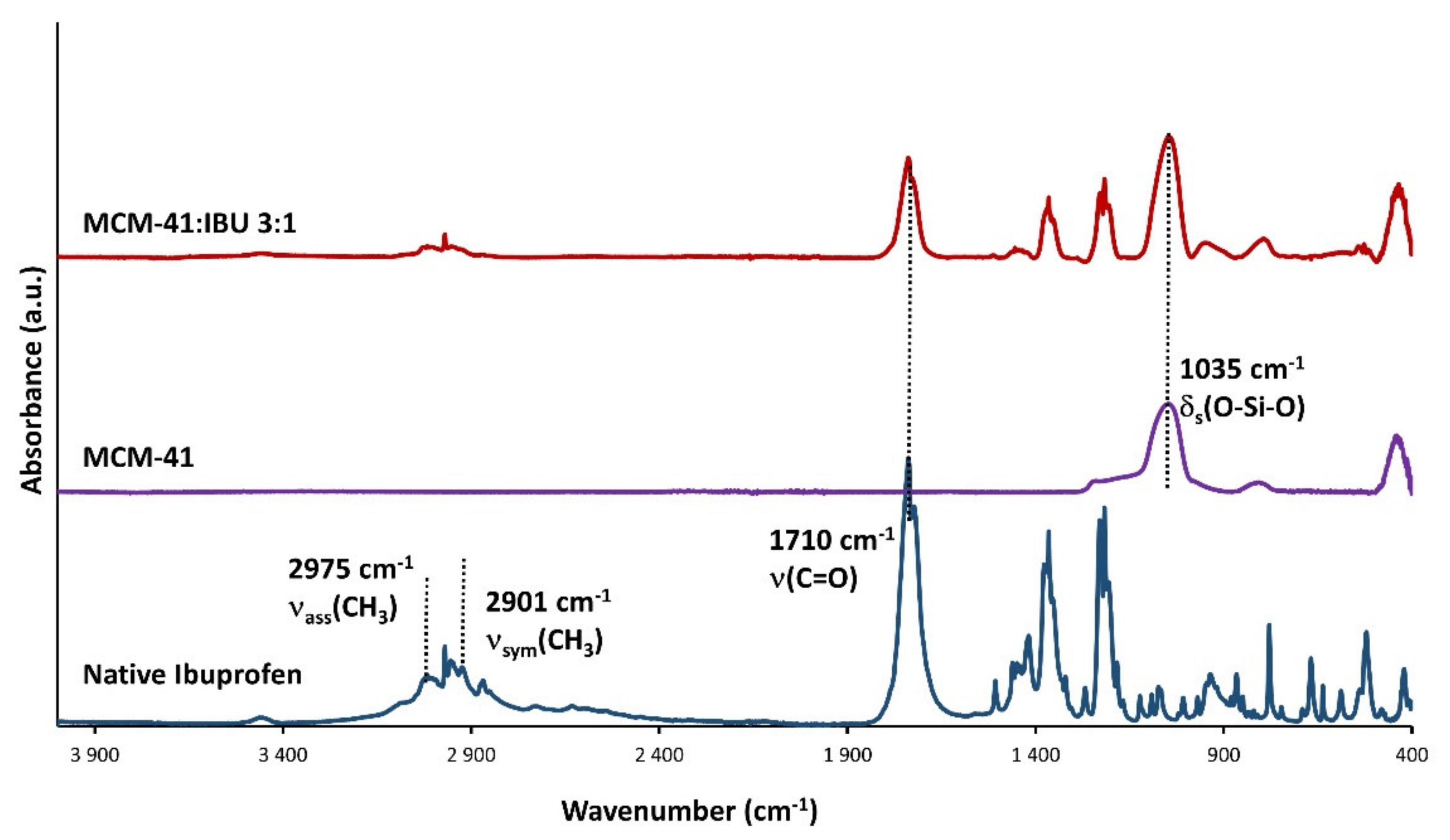
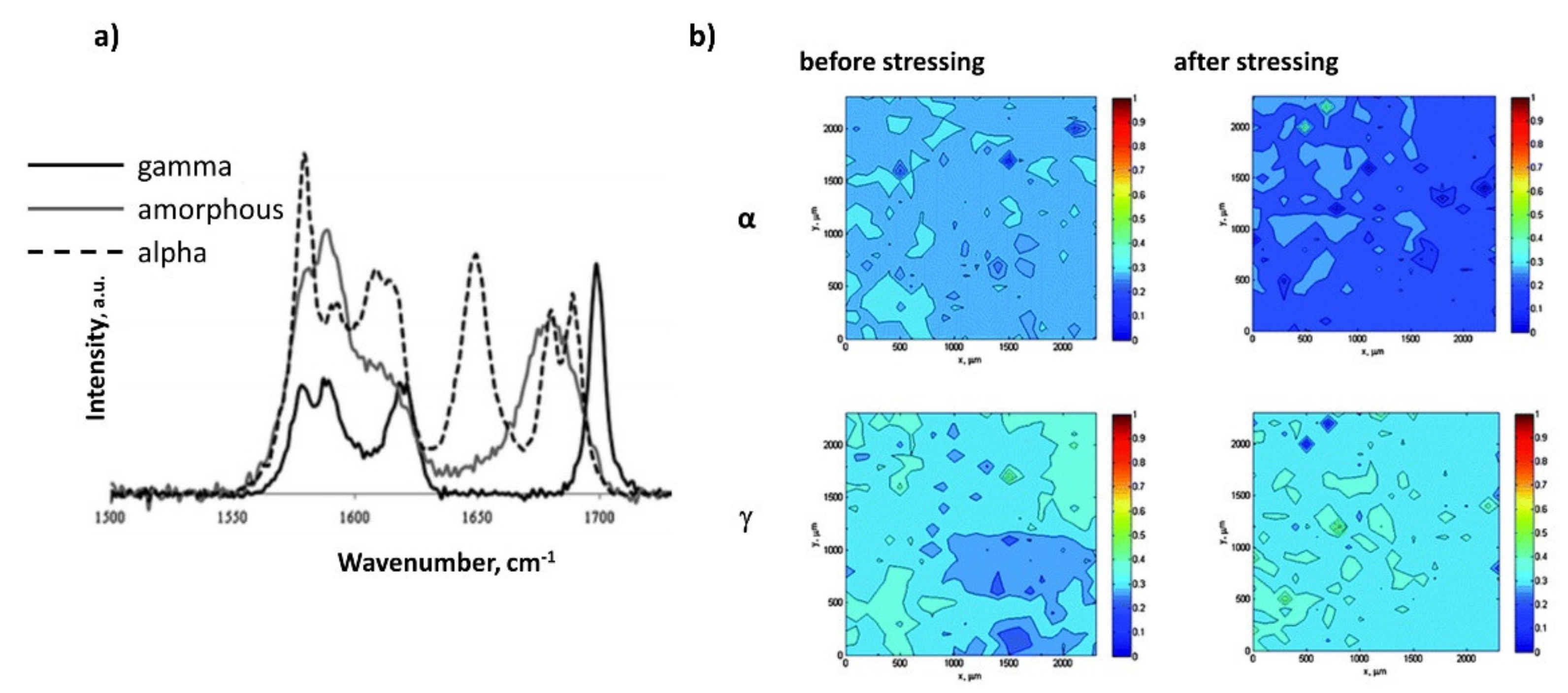
3.4.2. Vibrational Spectroscopy
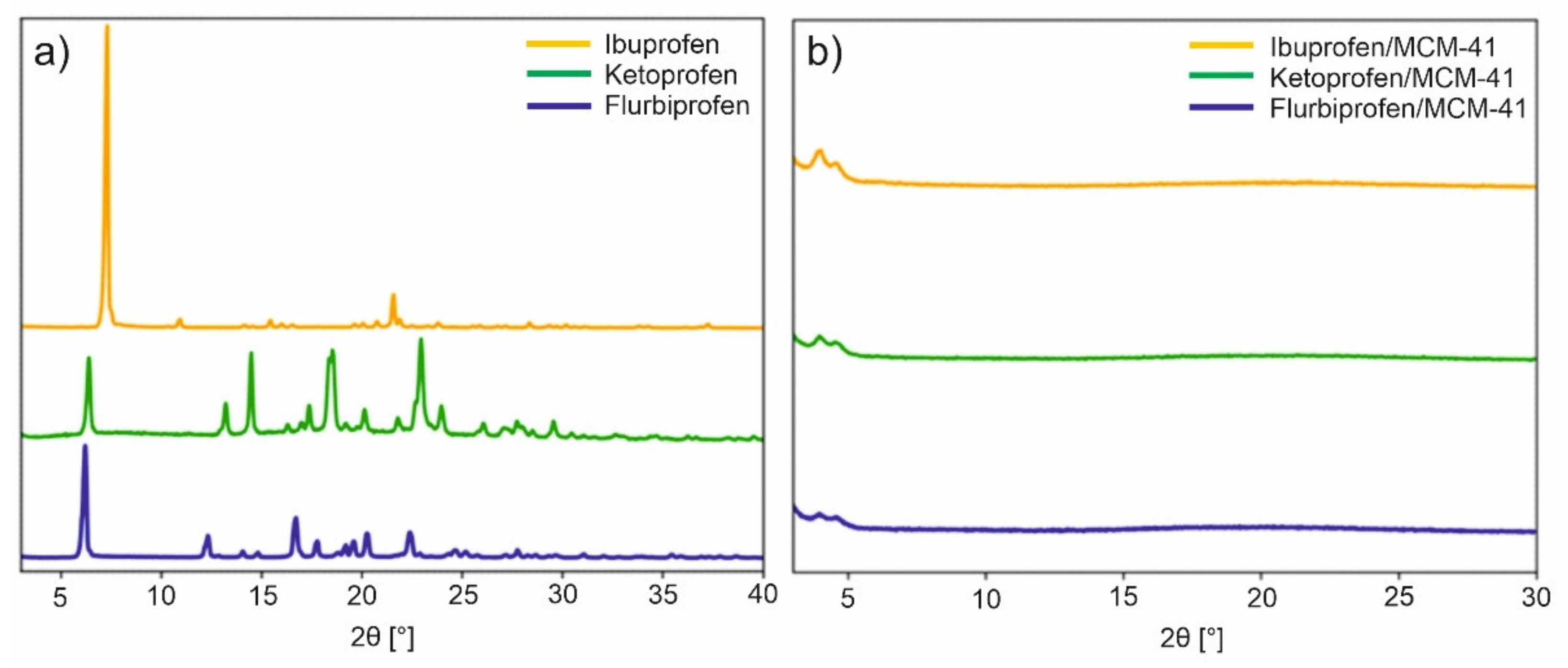
3.5. Powder X-ray Diffraction (PXRD) and Small-Angle X-ray Scattering (SAXS)
3.6. Chromatography
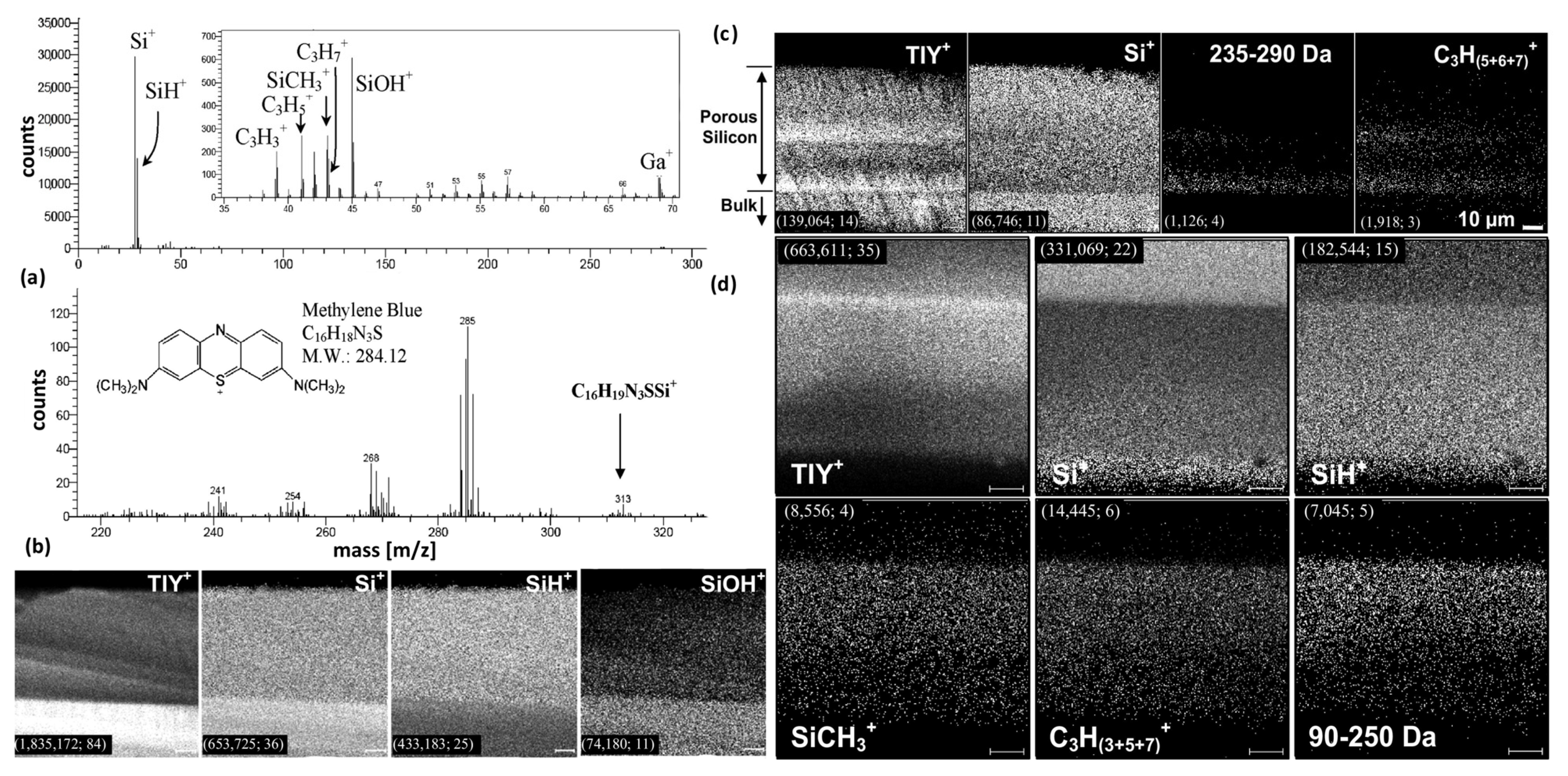
3.7. Mass Spectrometry
3.8. Other Methods
4. Conclusions and Future Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Vallet-Regi, M.; Ramila, A.; del Real, R.P.; Perez-Pariente, J. A new property of MCM-41: Drug delivery system. Chem. Mater. 2001, 13, 308–311. [Google Scholar] [CrossRef]
- Garcia-Bennett, A.E. Synthesis, toxicology and potential of ordered mesoporous materials in nanomedicine. Nanomedicine 2011, 6, 867–877. [Google Scholar] [CrossRef]
- Liu, T.L.; Li, L.L.; Teng, X.; Huang, X.L.; Liu, H.Y.; Chen, D.; Ren, J.; He, J.Q.; Tang, F.Q. Single and repeated dose toxicity of mesoporous hollow silica nanoparticles in intravenously exposed mice. Biomaterials 2011, 32, 1657–1668. [Google Scholar] [CrossRef]
- He, Q.J.; Shi, J.L.; Zhu, M.; Chen, Y.; Chen, F. The three-stage in vitro degradation behavior of mesoporous silica in simulated body fluid. Micropor. Mesopor. Mater. 2010, 131, 314–320. [Google Scholar] [CrossRef]
- Fu, C.H.; Liu, T.L.; Li, L.L.; Liu, H.Y.; Chen, D.; Tang, F.Q. The absorption, distribution, excretion and toxicity of mesoporous silica nanoparticles in mice following different exposure routes. Biomaterials 2013, 34, 2565–2575. [Google Scholar] [CrossRef] [PubMed]
- Tang, F.Q.; Li, L.L.; Chen, D. Mesoporous Silica Nanoparticles: Synthesis, Biocompatibility and Drug Delivery. Adv. Mater. 2012, 24, 1504–1534. [Google Scholar] [CrossRef]
- Kinnari, P.; Makila, E.; Heikkila, T.; Salonen, J.; Hirvonen, J.; Santos, H.A. Comparison of mesoporous silicon and non-ordered mesoporous silica materials as drug carriers for itraconazole. Int. J. Pharm. 2011, 414, 148–156. [Google Scholar] [CrossRef]
- Buyuktimkin, T.; Wurster, D.E. The influence of the adsorption of metoclopramide on the surface ionization of fumed silica. Int. J. Pharm. 2015, 478, 164–171. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, C.A.; Ahern, R.J.; Dontireddy, R.; Ryan, K.B.; Crean, A.M. Mesoporous silica formulation strategies for drug dissolution enhancement: A review. Expert Opin. Drug Deliv. 2016, 13, 93–108. [Google Scholar] [CrossRef]
- Bharti, C.; Nagaich, U.; Pal, A.K.; Gulati, N. Mesoporous silica nanoparticles in target drug delivery system: A review. Int. J. Pharm. Investig. 2015, 5, 124–133. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jeelani, P.G.; Mulay, P.; Venkat, R.; Ramalingam, C. Multifaceted Application of Silica Nanoparticles. A Review. Silicon 2020, 12, 1337–1354. [Google Scholar] [CrossRef]
- Miura, H.; Kanebako, M.; Shirai, H.; Nakao, H.; Inagi, T.; Terada, K. Enhancement of dissolution rate and oral absorption of a poorly water-soluble drug, K-832, by adsorption onto porous silica using supercritical carbon dioxide. Eur. J. Pharm. Biopharm. 2010, 76, 215–221. [Google Scholar] [CrossRef]
- Carvalho, G.C.; Sábio, R.M.; de Cássia Ribeiro, T.; Monteiro, A.S.; Pereira, D.V.; Ribeiro, S.J.L.; Chorilli, M. Highlights in Mesoporous Silica Nanoparticles as a Multifunctional Controlled Drug Delivery Nanoplatform for Infectious Diseases Treatment. Pharm. Res. 2020, 37, 191. [Google Scholar] [CrossRef]
- Chircov, C.; Spoiala, A.; Paun, C.; Craciun, L.; Ficai, D.; Ficai, A.; Andronescu, E.; Turculet, S.C. Mesoporous Silica Platforms with Potential Applications in Release and Adsorption of Active Agents. Molecules 2020, 25, 3814. [Google Scholar] [CrossRef]
- Zid, L.; Zelenak, V.; Almasi, M.; Zelenakova, A.; Szucsova, J.; Bednarcik, J.; Sulekova, M.; Hudak, A.; Vahovska, L. Mesoporous Silica as a Drug Delivery System for Naproxen: Influence of Surface Functionalization. Molecules 2020, 25, 4722. [Google Scholar] [CrossRef]
- Natarajan, S.K.; Selvaraj, S. Mesoporous silica nanoparticles: Importance of surface modifications and its role in drug delivery. RSC Adv. 2014, 4, 14328–14334. [Google Scholar] [CrossRef]
- Le, T.T.; Elyafi, A.K.E.; Mohammed, A.R.; Al-Khattawi, A. Delivery of Poorly Soluble Drugs via Mesoporous Silica: Impact of Drug Overloading on Release and Thermal Profiles. Pharmaceutics 2019, 11, 269. [Google Scholar] [CrossRef] [Green Version]
- Seljak, K.B.; Kocbek, P.; Gašperlin, M. Mesoporous silica nanoparticles as delivery carriers: An overview of drug loading techniques. J. Drug Deliv. Sci. Technol. 2020, 59, 101906. [Google Scholar] [CrossRef]
- Li, Z.; Zhang, Y.T.; Feng, N.P. Mesoporous silica nanoparticles: Synthesis, classification, drug loading, pharmacokinetics, biocompatibility, and application in drug delivery. Expert Opin. Drug Deliv. 2019, 16, 219–237. [Google Scholar] [CrossRef] [PubMed]
- Maleki, A.; Kettiger, H.; Schoubben, A.; Rosenholm, J.M.; Ambrogi, V.; Hamidi, M. Mesoporous silica materials: From physico-chemical properties to enhanced dissolution of poorly water-soluble drugs. J. Control. Release 2017, 262, 329–347. [Google Scholar] [CrossRef]
- Andersson, J.; Rosenholm, J.; Areva, S.; Lindén, M. Influences of Material Characteristics on Ibuprofen Drug Loading and Release Profiles from Ordered Micro- and Mesoporous Silica Matrices. Chem. Mater. 2004, 16, 4160–4167. [Google Scholar] [CrossRef]
- Singh, A.; Worku, Z.A.; Van den Mooter, G. Oral formulation strategies to improve solubility of poorly water-soluble drugs. Expert Opin. Drug Deliv. 2011, 8, 1361–1378. [Google Scholar] [CrossRef]
- Prestidge, C.A.; Barnes, T.J.; Lau, C.-H.; Barnett, C.; Loni, A.; Canham, L. Mesoporous silicon: A platform for the delivery of therapeutics. Expert Opin. Drug Deliv. 2007, 4, 101–110. [Google Scholar] [CrossRef] [PubMed]
- Kumar, D.; Sailaja Chirravuri, S.V.; Shastri, N.R. Impact of surface area of silica particles on dissolution rate and oral bioavailability of poorly water soluble drugs: A case study with aceclofenac. Int. J. Pharm. 2014, 461, 459–468. [Google Scholar] [CrossRef]
- Andrade, G.F.; Soares, D.C.F.; Almeida, R.K.d.S.; Sousa, E.M.B. Mesoporous Silica SBA-16 Functionalized with Alkoxysilane Groups: Preparation, Characterization, and Release Profile Study. J. Nanomater. 2012, 2012, 1687–4110. [Google Scholar] [CrossRef]
- Maleki, A.; Hamidi, M. Dissolution enhancement of a model poorly water-soluble drug, atorvastatin, with ordered mesoporous silica: Comparison of MSF with SBA-15 as drug carriers. Expert Opin. Drug Deliv. 2016, 13, 171–181. [Google Scholar] [CrossRef] [PubMed]
- Thomas, M.J.K.; Slipper, I.; Walunj, A.; Jain, A.; Favretto, M.E.; Kallinteri, P.; Douroumis, D. Inclusion of poorly soluble drugs in highly ordered mesoporous silica nanoparticles. Int. J. Pharm. 2010, 387, 272–277. [Google Scholar] [CrossRef]
- Ambrogi, V.; Perioli, L.; Marmottini, F.; Accorsi, O.; Pagano, C.; Ricci, M.; Rossi, C. Role of mesoporous silicates on carbamazepine dissolution rate enhancement. Micropor. Mesopor. Mater. 2008, 113, 445–452. [Google Scholar] [CrossRef]
- Speybroeck, M.V.; Barillaro, V.; Thi, T.D.; Mellaerts, R.; Martens, J.; Humbeeck, J.V.; Vermant, J.; Annaert, P.; Den Mooter, G.V.; Augustijns, P. Ordered Mesoporous Silica Material SBA-15: A Broad-Spectrum Formulation Platform for Poorly Soluble Drugs. J. Pharm. Sci. 2009, 98, 2648–2658. [Google Scholar] [CrossRef] [PubMed]
- Ambrogi, V.; Marmottini, F.; Pagano, C. Amorphous carbamazepine stabilization by the mesoporous silicate SBA-15. Micropor. Mesopor. Mater. 2013, 177, 1–7. [Google Scholar] [CrossRef]
- Chen, B.; Wang, Z.; Quan, G.; Peng, X.; Pan, X.; Wang, R.; Xu, Y.; Li, G.; Wu, C. In vitro and in vivo evaluation of ordered mesoporous silica as a novel adsorbent in liquisolid formulation. Int. J. Nanomed. 2012, 7, 1176–9114. [Google Scholar] [CrossRef] [Green Version]
- Hu, Y.; Zhi, Z.; Zhao, Q.; Wu, C.; Zhao, P.; Jiang, H.; Jiang, T.; Wang, S. 3D cubic mesoporous silica microsphere as a carrier for poorly soluble drug carvedilol. Micropor. Mesopor. Mater. 2012, 147, 94–101. [Google Scholar] [CrossRef]
- Gunaydin, S.; Yılmaz, A. Improvement of solubility of celecoxib by inclusion in MCM-41 mesoporous silica: Drug loading and release. Turk. J. Chem. 2015, 39, 317–333. [Google Scholar] [CrossRef]
- Eren, Z.S.; Tunçer, S.; Gezer, G.; Yildirim, L.T.; Banerjee, S.; Yilmaz, A. Improved solubility of celecoxib by inclusion in SBA-15 mesoporous silica: Drug loading in different solvents and release. Micropor. Mesopor. Mater. 2016, 235, 211–223. [Google Scholar] [CrossRef]
- Li, J.; Wang, Y.; Zheng, X.; Zhang, Y.; Sun, C.; Gao, Y.; Jiang, T.; Wang, S. The synthesis and application involving regulation of the insoluble drug release from mesoporous silica nanotubes. Appl. Surf. Sci. 2015, 330, 374–382. [Google Scholar] [CrossRef]
- Chen, W.; Cheng, C.-A.; Lee, B.-Y.; Clemens, D.L.; Huang, W.-Y.; Horwitz, M.A.; Zink, J.I. Facile Strategy Enabling Both High Loading and High Release Amounts of the Water-Insoluble Drug Clofazimine Using Mesoporous Silica Nanoparticles. ACS Appl. Mater. Interfaces 2018, 10, 31870–31881. [Google Scholar] [CrossRef] [PubMed]
- Kjellman, T.; Xia, X.; Alfredsson, V.; Garcia-Bennett, A.E. Influence of microporosity in SBA-15 on the release properties of anticancer drug dasatinib. J. Mater. Chem. B 2014, 2, 5265–5271. [Google Scholar] [CrossRef] [PubMed]
- Ambrogi, V.; Perioli, L.; Pagano, C.; Marmottini, F.; Moretti, M.; Mizzi, F.; Rossi, C. Econazole Nitrate-Loaded MCM-41 for an Antifungal Topical Powder Formulation. J. Pharm. Sci. 2010, 99, 4738–4745. [Google Scholar] [CrossRef] [PubMed]
- Kiekens, F.; Eelen, S.; Verheyden, L.; Daems, T.; Martens, J.; Den Mooter, G.V. Use of Ordered Mesoporous Silica to Enhance the Oral Bioavailability of Ezetimibe in Dogs. J. Pharm. Sci. 2012, 101, 1136–1144. [Google Scholar] [CrossRef]
- Wu, C.; Zhao, Z.; Zhao, Y.; Hao, Y.; Liu, Y.; Liu, C. Preparation of a push–pull osmotic pump of felodipine solubilized by mesoporous silica nanoparticles with a core–shell structure. Int. J. Pharm. 2014, 475, 298–305. [Google Scholar] [CrossRef]
- Ahern, R.J.; Crean, A.M.; Ryan, K.B. The influence of supercritical carbon dioxide (SC-CO2) processing conditions on drug loading and physicochemical properties. Int. J. Pharm. 2012, 439, 92–99. [Google Scholar] [CrossRef]
- Van Speybroeck, M.; Mellaerts, R.; Mols, R.; Thi, T.D.; Martens, J.A.; Van Humbeeck, J.; Annaert, P.; Van den Mooter, G.; Augustijns, P. Enhanced absorption of the poorly soluble drug fenofibrate by tuning its release rate from ordered mesoporous silica. Eur. J. Pharm. Sci. 2010, 41, 623–630. [Google Scholar] [CrossRef] [PubMed]
- Ahern, R.J.; Hanrahan, J.P.; Tobin, J.M.; Ryan, K.B.; Crean, A.M. Comparison of fenofibrate–mesoporous silica drug-loading processes for enhanced drug delivery. Eur. J. Pharm. Sci. 2013, 50, 400–409. [Google Scholar] [CrossRef] [PubMed]
- Hong, S.; Shen, S.; Tan, D.C.T.; Ng, W.K.; Liu, X.; Chia, L.S.O.; Irwan, A.W.; Tan, R.; Nowak, S.A.; Marsh, K.; et al. High drug load, stable, manufacturable and bioavailable fenofibrate formulations in mesoporous silica: A comparison of spray drying versus solvent impregnation methods. Drug Deliv. 2016, 23, 316–327. [Google Scholar] [CrossRef]
- Bouledjouidja, A.; Masmoudi, Y.; Van Speybroeck, M.; Schueller, L.; Badens, E. Impregnation of Fenofibrate on mesoporous silica using supercritical carbon dioxide. Int. J. Pharm. 2016, 499, 1–9. [Google Scholar] [CrossRef]
- Kerkhofs, S.; Saïdi, F.; Vandervoort, N.; Van den Mooter, G.; Martineau, C.; Taulelle, F.; Martens, J.A. Silica capsules enclosing P123 triblock copolymer micelles for flurbiprofen storage and release. J. Mater. Chem. B 2015, 3, 3054–3061. [Google Scholar] [CrossRef] [PubMed]
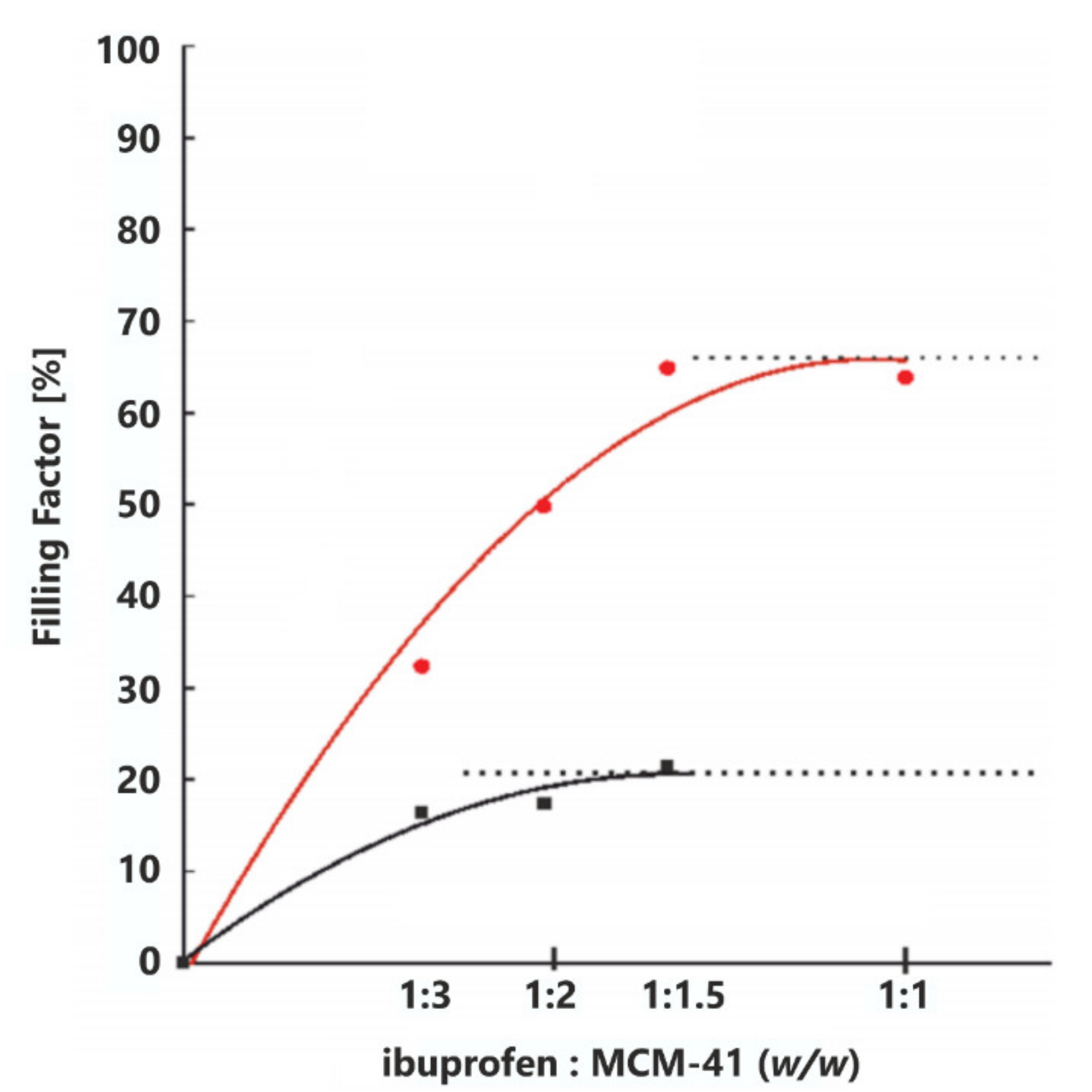
- Trzeciak, K.; Kaźmierski, S.; Wielgus, E.; Potrzebowski, M.J. DiSupLo—New extremely easy and efficient method for loading of active pharmaceutical ingredients into the pores of MCM-41 mesoporous silica particles. Micropor. Mesopor. Mater. 2020, 308, 110506. [Google Scholar] [CrossRef]
- Ambrogi, V.; Perioli, L.; Pagano, C.; Latterini, L.; Marmottini, F.; Ricci, M.; Rossi, C. MCM-41 for furosemide dissolution improvement. Micropor. Mesopor. Mater. 2012, 147, 343–349. [Google Scholar] [CrossRef]
- Ambrogi, V.; Perioli, L.; Pagano, C.; Marmottini, F.; Ricci, M.; Sagnella, A.; Rossi, C. Use of SBA-15 for furosemide oral delivery enhancement. Eur. J. Pharm. Sci. 2012, 46, 43–48. [Google Scholar] [CrossRef]
- Van Speybroeck, M.; Mellaerts, R.; Thi, T.D.; Martens, J.A.; Van Humbeeck, J.; Annaert, P.; Van den Mooter, G.; Augustijns, P. Preventing release in the acidic environment of the stomach via occlusion in ordered mesoporous silica enhances the absorption of poorly soluble weakly acidic drugs. J. Pharm. Sci. 2011, 100, 4864–4876. [Google Scholar] [CrossRef] [PubMed]
- Jambhrunkar, S.; Qu, Z.; Popat, A.; Karmakar, S.; Xu, C.; Yu, C. Modulating in vitro release and solubility of griseofulvin using functionalized mesoporous silica nanoparticles. J. Colloid Interface Sci. 2014, 434, 218–225. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hillerström, A.; van Stam, J.; Andersson, M. Ibuprofen loading into mesostructured silica using liquid carbon dioxide as a solvent. Green Chem. 2009, 11, 662–667. [Google Scholar] [CrossRef]
- Shen, S.-C.; Ng, W.K.; Chia, L.; Hu, J.; Tan, R.B.H. Physical state and dissolution of ibuprofen formulated by co-spray drying with mesoporous silica: Effect of pore and particle size. Int. J. Pharm. 2011, 410, 188–195. [Google Scholar] [CrossRef]
- Charnay, C.; Bégu, S.; Tourné-Péteilh, C.; Nicole, L.; Lerner, D.A.; Devoisselle, J.M. Inclusion of ibuprofen in mesoporous templated silica: Drug loading and release property. Eur. J. Pharm. Biopharm. 2004, 57, 533–540. [Google Scholar] [CrossRef] [PubMed]
- Tourné-Péteilh, C.; Brunel, D.; Bégu, S.; Chiche, B.; Fajula, F.; Lerner, D.A.; Devoisselle, J.-M. Synthesis and characterisation of ibuprofen-anchored MCM-41 silica and silica gel. New J. Chem. 2003, 27, 1415–1418. [Google Scholar] [CrossRef]
- Heikkilä, T.; Salonen, J.; Tuura, J.; Kumar, N.; Salmi, T.; Murzin, D.Y.; Hamdy, M.S.; Mul, G.; Laitinen, L.; Kaukonen, A.M.; et al. Evaluation of mesoporous TCPSi, MCM-41, SBA-15, and TUD-1 materials as API carriers for oral drug delivery. Drug Deliv. 2007, 14, 337–347. [Google Scholar] [CrossRef] [PubMed]
- Mellaerts, R.; Jammaer, J.A.G.; Van Speybroeck, M.; Chen, H.; Humbeeck, J.V.; Augustijns, P.; Van den Mooter, G.; Martens, J.A. Physical State of Poorly Water Soluble Therapeutic Molecules Loaded into SBA-15 Ordered Mesoporous Silica Carriers: A Case Study with Itraconazole and Ibuprofen. Langmuir 2008, 24, 8651–8659. [Google Scholar] [CrossRef]
- Shen, S.C.; Ng, W.K.; Chia, L.; Dong, Y.C.; Tan, R.B.H. Stabilized Amorphous State of Ibuprofen by Co-Spray Drying With Mesoporous SBA-15 to Enhance Dissolution Properties. J. Pharm. Sci. 2010, 99, 1997–2007. [Google Scholar] [CrossRef] [PubMed]
- Malfait, B.; Correia, N.T.; Mussi, A.; Paccou, L.; Guinet, Y.; Hédoux, A. Solid-state loading of organic molecular materials within mesoporous silica matrix: Application to ibuprofen. Micropor. Mesopor. Mater. 2019, 277, 203–207. [Google Scholar] [CrossRef]
- Hu, Y.; Wang, J.; Zhi, Z.; Jiang, T.; Wang, S. Facile synthesis of 3D cubic mesoporous silica microspheres with a controllable pore size and their application for improved delivery of a water-insoluble drug. J. Colloid Interface Sci. 2011, 363, 410–417. [Google Scholar] [CrossRef]
- Wang, Y.; Zhao, Q.; Hu, Y.; Sun, L.; Bai, L.; Jiang, T.; Wang, S. Ordered nanoporous silica as carriers for improved delivery of water insoluble drugs: A comparative study between three dimensional and two dimensional macroporous silica. Int. J. Nanomed. 2013, 8, 4015–4031. [Google Scholar] [CrossRef] [Green Version]
- Limnell, T.; Santos, H.A.; Mäkilä, E.; Heikkilä, T.; Salonen, J.; Murzin, D.Y.; Kumar, N.; Laaksonen, T.; Peltonen, L.; Hirvonen, J. Drug Delivery Formulations of Ordered and Nonordered Mesoporous Silica: Comparison of Three Drug Loading Methods. J. Pharm. Sci. 2011, 100, 3294–3306. [Google Scholar] [CrossRef]
- Liu, X.; Che, S. Enhanced release of the poorly soluble drug itraconazole loaded in ordered mesoporous silica. Sci. China Chem. 2015, 58, 400–410. [Google Scholar] [CrossRef]
- Vialpando, M.; Aerts, A.; Persoons, J.; Martens, J.; Van Den Mooter, G. Evaluation of ordered mesoporous silica as a carrier for poorly soluble drugs: Influence of pressure on the structure and drug release. J. Pharm. Sci. 2011, 100, 3411–3420. [Google Scholar] [CrossRef]
- Abd-elbary, A.; El Nabarawi, M.A.; Hassen, D.H.; Taha, A.A. Inclusion and characterization of ketoprofen into different mesoporous silica nanoparticles using three loading methods. Int. J. Pharm. Pharm. Sci. 2014, 6, 183–191. [Google Scholar]
- Vadia, N.; Rajput, S. Study on formulation variables of methotrexate loaded mesoporous MCM-41 nanoparticles for dissolution enhancement. Eur. J. Pharm. Sci. 2012, 45, 8–18. [Google Scholar] [CrossRef] [PubMed]
- Guo, Z.; Liu, X.-M.; Ma, L.; Li, J.; Zhang, H.; Gao, Y.-P.; Yuan, Y. Effects of particle morphology, pore size and surface coating of mesoporous silica on Naproxen dissolution rate enhancement. Colloids Surf. B 2013, 101, 228–235. [Google Scholar] [CrossRef] [PubMed]
- Jia, L.; Shen, J.; Li, Z.; Zhang, D.; Zhang, Q.; Duan, C.; Liu, G.; Zheng, D.; Liu, Y.; Tian, X. Successfully tailoring the pore size of mesoporous silica nanoparticles: Exploitation of delivery systems for poorly water-soluble drugs. Int. J. Pharm. 2012, 439, 81–91. [Google Scholar] [CrossRef]
- Yuan, L.; Chen, W.; Hu, J.; Zhang, J.Z.; Yang, D. Mechanistic Study of the Covalent Loading of Paclitaxel via Disulfide Linkers for Controlled Drug Release. Langmuir 2013, 29, 734–743. [Google Scholar] [CrossRef]
- Tingming, F.; Liwei, G.; Kang, L.; Tianyao, W.; Jin, L. Template occluded SBA-15: An effective dissolution enhancer for poorly water-soluble drug. Appl. Surf. Sci. 2010, 256, 6963–6968. [Google Scholar] [CrossRef]
- Ambrogi, V.; Perioli, L.; Marmottini, F.; Giovagnoli, S.; Esposito, M.; Rossi, C. Improvement of dissolution rate of piroxicam by inclusion into MCM-41 mesoporous silicate. Eur. J. Pharm. Sci. 2007, 32, 216–222. [Google Scholar] [CrossRef]
- Martín, A.; García, R.A.; Karaman, D.S.; Rosenholm, J.M. Polyethyleneimine-functionalized large pore ordered silica materials for poorly water-soluble drug delivery. J. Mater. Sci. 2014, 49, 1437–1447. [Google Scholar] [CrossRef]
- Bi, Y.; Wu, C.; Xin, M.; Bi, S.; Yan, C.; Hao, J.; Li, F.; Li, S. Facile large-scale preparation of mesoporous silica microspheres with the assistance of sucrose and their drug loading and releasing properties. Int. J. Pharm. 2016, 500, 77–84. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhi, Z.; Jiang, T.; Zhang, J.; Wang, Z.; Wang, S. Spherical mesoporous silica nanoparticles for loading and release of the poorly water-soluble drug telmisartan. J. Controll. Release 2010, 145, 257–263. [Google Scholar] [CrossRef] [PubMed]
- ICH Guideline Q3C (R6). Available online: https://www.ema.europa.eu/en/ich-q3c-r6-residual-solvents (accessed on 27 April 2021).
- Belhadj-Ahmed, F.; Badens, E.; Llewellyn, P.; Denoyel, R.; Charbit, G. Impregnation of vitamin E acetate on silica mesoporous phases using supercritical carbon dioxide. J. Supercrit. Fluids 2009, 51, 278–286. [Google Scholar] [CrossRef]
- Lehto, V.P.; Riikonen, J. Drug loading and characterization of porous silicon materials. In Porous Silicon for Biomedical Applications; Santos, H.A., Ed.; Woodhead Publishing: Cambridge, UK, 2014; pp. 337–355. [Google Scholar]
- Xie, X.; Li, F.; Zhang, H.; Lu, Y.; Lian, S.; Lin, H.; Gao, Y.; Jia, L. EpCAM aptamer-functionalized mesoporous silica nanoparticles for efficient colon cancer cell-targeted drug delivery. Eur. J. Pharm. Sci. 2016, 83, 28–35. [Google Scholar] [CrossRef]
- Sarkar, A.; Ghosh, S.; Chowdhury, S.; Pandey, B.; Sil, P.C. Targeted delivery of quercetin loaded mesoporous silica nanoparticles to the breast cancer cells. Biochim. Biophys. Acta 2016, 1860, 2065–2075. [Google Scholar] [CrossRef]
- Brás, A.R.; Fonseca, I.M.; Dionísio, M.; Schönhals, A.; Affouard, F.; Correia, N.T. Influence of Nanoscale Confinement on the Molecular Mobility of Ibuprofen. J. Phys. Chem. C 2014, 118, 13857–13868. [Google Scholar] [CrossRef]
- Zheng, X.; Feng, S.; Wang, X.; Shi, Z.; Mao, Y.; Zhao, Q.; Wang, S. MSNCs and MgO-MSNCs as drug delivery systems to control the adsorption kinetics and release rate of indometacin. Asian J. Pharm. Sci. 2019, 14, 275–286. [Google Scholar] [CrossRef]
- Šoltys, M.; Kovačík, P.; Dammer, O.; Beránek, J.; Štěpánek, F. Effect of solvent selection on drug loading and amorphisation in mesoporous silica particles. Int. J. Pharm. 2019, 555, 19–27. [Google Scholar] [CrossRef] [PubMed]
- Skorupska, E.; Jeziorna, A.; Paluch, P.; Potrzebowski, M.J. Ibuprofen in Mesopores of Mobil Crystalline Material 41 (MCM-41): A Deeper Understanding. Mol. Pharm. 2014, 11, 1512–1519. [Google Scholar] [CrossRef] [PubMed]
- Deraz, N. The comparative jurisprudence of catalysts preparation methods: I. Precipitation and impregnation methods. J. Ind. Environ. Chem. 2017, 2, 19–21. [Google Scholar]
- Campanati, M.; Fornasari, G.; Vaccari, A. Fundamentals in the preparation of heterogeneous catalysts. Catal. Today 2003, 77, 299–314. [Google Scholar] [CrossRef]
- Wang, Y.; Zhao, Q.; Han, N.; Bai, L.; Li, J.; Liu, J.; Che, E.; Hu, L.; Zhang, Q.; Jiang, T.; et al. Mesoporous silica nanoparticles in drug delivery and biomedical applications. Nanomed. NBM 2015, 11, 313–327. [Google Scholar] [CrossRef]
- He, Y.; Liang, S.; Long, M.; Xu, H. Mesoporous silica nanoparticles as potential carriers for enhanced drug solubility of paclitaxel. Mater. Sci. Eng. C 2017, 78, 12–17. [Google Scholar] [CrossRef]
- Liu, Q.; Zhang, J.; Sun, W.; Xie, Q.R.; Xia, W.; Gu, H. Delivering hydrophilic and hydrophobic chemotherapeutics simultaneously by magnetic mesoporous silica nanoparticles to inhibit cancer cells. Int. J. Nanomed. 2012, 7, 999–1013. [Google Scholar] [CrossRef] [Green Version]
- Rosenholm, J.M.; Peuhu, E.; Eriksson, J.E.; Sahlgren, C.; Lindén, M. Targeted Intracellular Delivery of Hydrophobic Agents using Mesoporous Hybrid Silica Nanoparticles as Carrier Systems. Nano Lett. 2009, 9, 3308–3311. [Google Scholar] [CrossRef] [PubMed]
- Kompella, U.B.; Koushik, K. Preparation of drug delivery systems using supercritical fluid technology. Crit. Rev. Ther. Drug Carr. Syst. 2001, 18, 173–199. [Google Scholar] [CrossRef]
- Pasquali, I.; Bettini, R. Are pharmaceutics really going supercritical? Int. J. Pharm. 2008, 364, 176–187. [Google Scholar] [CrossRef]
- Bush, J.R.; Akgerman, A.; Hall, K.R. Synthesis of controlled release device with supercritical CO2 and co-solvent. J. Supercrit. Fluids 2007, 41, 311–316. [Google Scholar] [CrossRef]
- Li-Hong, W.; Xin, C.; Hui, X.; Li-Li, Z.; Jing, H.; Mei-Juan, Z.; Jie, L.; Yi, L.; Jin-Wen, L.; Wei, Z.; et al. A novel strategy to design sustained-release poorly water-soluble drug mesoporous silica microparticles based on supercritical fluid technique. Int. J. Pharm. 2013, 454, 135–142. [Google Scholar] [CrossRef]
- Hillerström, A.; Andersson, M.; Samuelsson, J.; van Stam, J. Solvent strategies for loading and release in mesoporous silica. Colloid Interface Sci. Commun. 2014, 3, 5–8. [Google Scholar] [CrossRef] [Green Version]
- Gurikov, P.; Smirnova, I. Amorphization of drugs by adsorptive precipitation from supercritical solutions: A review. J. Supercrit. Fluids 2018, 132, 105–125. [Google Scholar] [CrossRef]
- Nuchuchua, O.; Nejadnik, M.R.; Goulooze, S.C.; Lješković, N.J.; Every, H.A.; Jiskoot, W. Characterization of drug delivery particles produced by supercritical carbon dioxide technologies. J. Supercrit. Fluids 2017, 128, 244–262. [Google Scholar] [CrossRef]
- Padrela, L.; Rodrigues, M.A.; Duarte, A.; Dias, A.M.A.; Braga, M.E.M.; de Sousa, H.C. Supercritical carbon dioxide-based technologies for the production of drug nanoparticles/nanocrystals—A comprehensive review. Adv. Drug Deliv. Rev. 2018, 131, 22–78. [Google Scholar] [CrossRef]
- Dohrn, R.; Bertakis, E.; Behrend, O.; Voutsas, E.; Tassios, D. Melting point depression by using supercritical CO2 for a novel melt dispersion micronization process. J. Mol. Liq. 2007, 131–132, 53–59. [Google Scholar] [CrossRef]
- Dementeva, O.V.; Rudoy, V.M.; Zhigletsova, S.K. One-pot synthesis and loading of silica nanocontainers using surface active drugs as templating agents. Int. J. Drug Dev. Res. 2018, 10, C1–C002. [Google Scholar]
- Dementeva, O.V.; Rudoy, V.M. One-pot synthesis and loading of mesoporous SiO2 nanocontainers using micellar drugs as a template. RSC Adv. 2016, 6, 36207–36210. [Google Scholar] [CrossRef]
- Dementeva, O.V.; Roumyantseva, T.B.; Rudoy, V.M. The first example of silica nanoshell synthesis on vesicles of a cationic glycerolipid—Potential antitumor drug. Colloid J. 2016, 78, 281–284. [Google Scholar] [CrossRef]
- Davis, B.; Richens, J.; O’shea, P. Label-free critical micelle concentration determination of bacterial quorum sensing molecules. Biophys. J. 2011, 101, 245–254. [Google Scholar] [CrossRef] [Green Version]
- Zhou, C.; Weir, M.D.; Zhang, K.; Deng, D.; Cheng, L.; Xu, H.H.K. Synthesis of new antibacterial quaternary ammonium monomer for incorporation into CaP nanocomposite. Dent. Mater. 2013, 29, 859–870. [Google Scholar] [CrossRef] [Green Version]
- Wan, M.M.; Li, Y.Y.; Yang, T.; Zhang, T.; Sun, X.D.; Zhu, J.H. In Situ Loading of Drugs into Mesoporous Silica SBA-15. Chem. Eur. J. 2016, 22, 6294–6301. [Google Scholar] [CrossRef]
- Tourne-Peteilh, C.; Begu, S.; Lerner, D.A.; Galarneau, A.; Lafont, U.; Devoisselle, J.-M. Sol–gel one-pot synthesis in soft conditions of mesoporous silica materials ready for drug delivery system. J. Sol. Gel Sci. Technol. 2012, 61, 455–462. [Google Scholar] [CrossRef] [Green Version]
- Wang, N.; Cheng, X.; Li, N.; Wang, H.; Chen, H. Nanocarriers and Their Loading Strategies. Adv. Healthcare Mater. 2019, 8. [Google Scholar] [CrossRef] [PubMed]
- Fasiku, V.; Amuhaya, E.K.; Rajab, K.M.; Omolo, C.A. Nano/Microparticles Encapsulation Via Covalent Drug Conjugation. In Nano- and Micro-Encapsulation—Techniques and Applications; Abu-Thabit, N., Ed.; IntechOpen: London, UK, 2019; Volume 86, pp. 230–251. [Google Scholar]
- Giret, S.; Wong Chi Man, M.; Carcel, C. Mesoporous-Silica-Functionalized Nanoparticles for Drug Delivery. Chem. Eur. J. 2015, 21, 13850–13865. [Google Scholar] [CrossRef] [PubMed]
- Wong, P.T.; Choi, S.K. Mechanisms of Drug Release in Nanotherapeutic Delivery Systems. Chem. Rev. 2015, 115, 3388–3432. [Google Scholar] [CrossRef] [PubMed]
- Ding, C.; Li, Z. A review of drug release mechanisms from nanocarrier systems. Mater. Sci. Eng. C 2017, 76, 1440–1453. [Google Scholar] [CrossRef]
- Manzano, M.; Vallet-Regí, M. New developments in ordered mesoporous materials for drug delivery. J. Mater. Chem. 2010, 20, 5593–5604. [Google Scholar] [CrossRef]
- Mortera, R.; Vivero-Escoto, J.; Slowing, I.I.; Garrone, E.; Onida, B.; Lin, V.S.-Y. Cell-induced intracellular controlled release of membrane impermeable cysteine from a mesoporous silica nanoparticle-based drug delivery system. Chem. Commun. 2009, 3219–3221. [Google Scholar] [CrossRef]
- Popat, A.; Ross, B.P.; Liu, J.; Jambhrunkar, S.; Kleitz, F.; Qiao, S. Enzyme-responsive controlled release of covalently bound prodrug from functional mesoporous silica nanospheres. Angew. Chem. Int. Ed. Engl. 2012, 51, 12486–12489. [Google Scholar] [CrossRef]
- Rosenholm, J.M.; Peuhu, E.; Bate-Eya, L.T.; Eriksson, J.E.; Sahlgren, C.; Lindén, M. Cancer-cell-specific induction of apoptosis using mesoporous silica nanoparticles as drug-delivery vectors. Small 2010, 6, 1234–1241. [Google Scholar] [CrossRef]
- Carino, I.S.; Pasqua, L.; Testa, F.; Aiello, R.; Puoci, F.; Iemma, F.; Picci, N. Silica-Based Mesoporous Materials as Drug Delivery System for Methotrexate Release. Drug Deliv. 2007, 14, 491–495. [Google Scholar] [CrossRef] [Green Version]
- Uejo, F.; Limwikrant, W.; Moribe, K.; Yamamoto, K. Dissolution improvement of fenofibrate by melting inclusion in mesoporous silica. Asian J. Pharm. Sci. 2013, 8, 329–335. [Google Scholar] [CrossRef] [Green Version]
- Niu, X.; Wan, L.; Hou, Z.; Wang, T.; Sun, C.; Sun, J.; Zhao, P.; Jiang, T.; Wang, S. Mesoporous carbon as a novel drug carrier of fenofibrate for enhancement of the dissolution and oral bioavailability. Int. J. Pharm. 2013, 452, 382–389. [Google Scholar] [CrossRef] [PubMed]
- Waters, L.J.; Bedford, S.; Parkes, G.M.B. Controlled Microwave Processing Applied to the Pharmaceutical Formulation of Ibuprofen. AAPS Pharmscitech 2011, 12, 1038–1043. [Google Scholar] [CrossRef] [PubMed]
- Waters, L.J.; Hussain, T.; Parkes, G.; Hanrahan, J.P.; Tobin, J.M. Inclusion of fenofibrate in a series of mesoporous silicas using microwave irradiation. Eur. J. Pharm. Biopharm. 2013, 85, 936–941. [Google Scholar] [CrossRef]
- Hampsey, J.E.; Castro, C.M.; McCaughey, B.; Wang, D.; Mitchell, B.; Lu, Y. Preparation of Micrometer- to Sub-micrometer-Sized Nanostructured Silica Particles Using High-Energy Ball Milling. J. Am. Ceram. Soc. 2004, 87, 1280–1286. [Google Scholar] [CrossRef]
- Willart, J.F.; Descamps, M. Solid State Amorphization of Pharmaceuticals. Mol. Pharm. 2008, 5, 905–920. [Google Scholar] [CrossRef] [PubMed]
- Trzeciak, K.; Kaźmierski, S.; Drużbicki, K.; Potrzebowski, M.J. Mapping of Guest Localization in Mesoporous Silica Particles by Solid-State NMR and Ab Initio Modeling: New Insights into Benzoic Acid and p-Fluorobenzoic Acid Embedded in MCM-41 via Ball Milling. J. Phys. Chem. C 2021, 125, 10096–10109. [Google Scholar] [CrossRef]
- Abu-Zied, B.M.; Schwieger, W.; Asiri, A.M. Effect of ball milling on the structural and textural features of MCM-41 mesoporous material. Micropor. Mesopor. Mater. 2015, 218, 153–159. [Google Scholar] [CrossRef]
- Torres-Barthelemy, V.; Pérez-Hernández, N.; Shenderovich, I.G.; Tolstoy, P.M.; Denisov, G.S.; Limbach, H.-H. NMR-Detected Host–Guest Proton Exchange as a Tool to Explore Surface/Volume Ratios and Fluid Filling of Internal and External Spaces of Porous Solids Containing Surface OH Groups. J. Phys. Chem. C 2020, 124, 22082–22095. [Google Scholar] [CrossRef]
- Höhne, G.W.H.; Hemminger, W.F.; Flammersheim, H.J. Theoretical Fundamentals of Differential Scanning Calorimeters. In Differential Scanning Calorimetry, 2nd ed.; Messerschmidt, C., Ed.; Springer: Berlin/Heidelberg, Germany, 2003; pp. 21–40. [Google Scholar]
- Shilyaeva, Y.; Volovlikova, O.; Poyarkov, K.; Yuditskaya, S.; Gavrilov, S. Characterization of Mesoporous Silicon Using DSC Thermoporometry. Int. J. Nanosci. 2019, 18, 1940073–1940077. [Google Scholar] [CrossRef]
- Hempel, N.J.; Brede, K.; Olesen, N.E.; Genina, N.; Knopp, M.M.; Lobmann, K. A fast and reliable DSC-based method to determine the monomolecular loading capacity of drugs with good glass-forming ability in mesoporous silica. Int. J. Pharm. 2018, 544, 153–157. [Google Scholar] [CrossRef]
- Lehto, V.P.; Vaha-Heikkila, K.; Paski, J.; Salonen, J. Use of thermoanalytical methods in quantification of drug load in mes-oporous silicon microparticles. J. Therm. Anal. Calorim. 2005, 80, 393–397. [Google Scholar] [CrossRef]
- Bavnhoj, C.G.; Knopp, M.M.; Madsen, C.M.; Lobmann, K. The role interplay between mesoporous silica pore volume and surface area and their effect on drug loading capacity. Int. J. Pharm. X 2019, 1, 1000082–1000087. [Google Scholar] [CrossRef]
- Nassimbeni, L.R.; Ba’thori, N.B.; Atwood, J.L. (Eds.) Thermal Analysis. In Comprehensive Supramolecular Chemistry II, Molecular Sciences and Chemical Engineering, 2nd ed.; Elsevier: Burlington, MA, USA, 2017; pp. 3–21. [Google Scholar]
- Sing, K.S.W.; Everett, D.H.; Haul, R.A.W.; Moscou, L.; Pierotti, R.A.; Rouquerol, J.; Siemieniewska, T. Reporting phy-sisorption data for gas solid systems with special reference to the determination of surface-area and porosity (recommendations 1984). Pure Appl. Chem. 1985, 57, 603–619. [Google Scholar] [CrossRef]
- Thommes, M.; Kaneko, K.; Neimark, A.V.; Olivier, J.P.; Rodriguez-Reinoso, F.; Rouquerol, J.; Sing, K.S.W. Physisorp-tion of gases, with special reference to the evaluation of surface area and pore size distribution (IUPAC Technical Report). Pure Appl. Chem. 2015, 87, 1051–1069. [Google Scholar] [CrossRef] [Green Version]
- Rouquerol, J.; Avnir, D.; Everett, D.H.; Fairbridge, C.; Haynes, M.; Pernicone, N.; Ramsay, J.D.F.; Sing, K.S.W.; Unger, K.K. Guidelines for the characterization of porous solids. Characterization of Porous Solids. Stud. Surf. Sci. Catal. 1994, 87, 1–9. [Google Scholar]
- Huang, B.Y.; Bartholomew, C.H.; Woodfield, B.F. Improved calculations of pore size distribution for relatively large, irregular slit-shaped mesopore structure. Micropor. Mesopor. Mater. 2014, 184, 112–121. [Google Scholar] [CrossRef]
- Vallet-Regi, M.; Balas, F.; Colilla, M.; Manzano, M. Bone-regenerative bioceramic implants with drug and protein controlled delivery capability. Prog. Solid. State Chem. 2008, 36, 163–191. [Google Scholar] [CrossRef]
- Izquierdo-Barba, I.; Sousa, E.; Doadrio, J.C.; Doadrio, A.L.; Pariente, J.P.; Martinez, A.; Babonneau, F.; Vallet-Regi, M. Influence of mesoporous structure type on the controlled delivery of drugs: Release of ibuprofen from MCM-48, SBA-15 and functionalized SBA-15. J. Solgel. Sci. Technol. 2009, 50, 421–429. [Google Scholar] [CrossRef]
- Tzankova, V.; Aluani, D.; Yordanov, Y.; Valoti, M.; Frosini, M.; Spassova, I.; Kovacheva, D.; Tzankov, B. In vitro tox-icity evaluation of lomefloxacin-loaded MCM-41 mesoporous silica nanoparticles. Drug Chem. Toxicol. 2021, 44, 238–249. [Google Scholar] [CrossRef]
- Jani, A.T.; Haghighi, N.B.; Pour, M.S.H.; Aminian, M.; Molzemi, S. Hydroxyapatite incorporation into MCM-41 and study of ibuprofen drug release. J. Aust. Ceram. Soc. 2020, 56, 653–661. [Google Scholar] [CrossRef]
- Burguete, P.; Beltran, A.; Guillem, C.; Latorre, J.; Perez-Pla, F.; Beltran, D.; Amoros, P. Pore Length Effect on Drug Uptake and Delivery by Mesoporous Silicas. ChemPlusChem 2012, 77, 817–831. [Google Scholar] [CrossRef]
- Edeler, D.; Kaluderovic, M.R.; Dojcinovic, B.; Schmidt, H.; Kaluderovic, G.N. SBA-15 mesoporous silica particles loaded with cisplatin induce senescence in B16F10 cells. RSC Adv. 2016, 6, 111031–111040. [Google Scholar] [CrossRef] [Green Version]
- Jin, D.; Xi, P.; Wang, B.; Zhang, L.; Enderlein, J.; van Oijen, A.M. Nanoparticles for super-resolution microscopy and single-molecule tracking. Nat. Methods 2018, 15, 415–423. [Google Scholar] [CrossRef]
- Wang, W. Imaging the chemical activity of single nanoparticles with optical microscopy. Chem. Soc. Rev. 2018, 47, 2485–2508. [Google Scholar] [CrossRef] [PubMed]
- Stewart, P.L. Cryo-electron microscopy and cryo-electron tomography of nanoparticles. WIREs Nanomed. Nanobiotechnol. 2017, 9, e1417. [Google Scholar] [CrossRef]
- Huang, X.; Young, N.P.; Townley, H.E. Characterization and Comparison of Mesoporous Silica Particles for Optimized Drug Delivery. Nanomater. Nanotechnol. 2014, 4, 2. [Google Scholar] [CrossRef]
- Fu, L.; Zhao, S.; Chen, Y.; Liu, Z. One-pot synthesis of mesoporous silica hollow spheres with Mn–N–C integrated into the framework for ethylbenzene oxidation. Chem. Commun. 2016, 52, 5577–5580. [Google Scholar] [CrossRef]
- Lin, X.; Fu, L.; Chen, Y.; Zhu, R.; Wang, S.; Liu, Z. Mn–N-C Nanoreactor Prepared through Heating Metalloporphyrin Supported in Mesoporous Hollow Silica Spheres. ACS Appl. Mater. Interfaces 2016, 8, 26809–26816. [Google Scholar] [CrossRef]
- Li, K.; Wei, J.; Yu, H.; Xu, P.; Wang, J.; Yin, H.; Cohen Stuart, M.A.; Wang, J.; Zhou, S. A Generic Method for Preparing Hollow Mesoporous Silica Catalytic Nanoreactors with Metal Oxide Nanoparticles inside Their Cavities. Angew. Chem. Int. Ed. 2018, 57, 16458–16463. [Google Scholar] [CrossRef] [PubMed]
- Girleanu, M.; Lopes Silva, S.; Ihiawakrim, D.; Chaumonnot, A.; Bonduelle-Skrzypczak, A.; Lefebvre, F.; Dufaud, V.; Gay, A.-S.; Ersen, O. HAADF-STEM high-resolution study of nanometric MoS2 inside mesoporous SBA-15. Micropor. Mesopor. Mater. 2015, 217, 190–195. [Google Scholar] [CrossRef]
- Qin, L.; Niu, D.; Jiang, Y.; He, J.; Jia, X.; Zhao, W.; Li, P.; Li, Y. Confined growth of multiple gold nanorices in dual-mesoporous silica nanospheres for improved computed tomography imaging and photothermal therapy. Int. J. Nanomed. 2019, 14, 1519–1532. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Piras, M.; Salis, A.; Piludu, M.; Steri, D.; Monduzzi, M. 3D vision of human lysozyme adsorbed onto a SBA-15 nanostructured matrix. Chem. Commun. 2011, 47, 7338–7340. [Google Scholar] [CrossRef] [PubMed]
- Piludu, M.; Medda, L.; Cugia, F.; Monduzzi, M.; Salis, A. Silver Enhancement for Transmission Electron Microscopy Imaging of Antibody Fragment–Gold Nanoparticles Conjugates Immobilized on Ordered Mesoporous Silica. Langmuir 2015, 31, 9458–9463. [Google Scholar] [CrossRef]
- Piludu, M.; Medda, L.; Monduzzi, M.; Salis, A. Gold Nanoparticles: A Powerful Tool to Visualize Proteins on Ordered Mesoporous Silica and for the Realization of Theranostic Nanobioconjugates. Int. J. Mol. Sci. 2018, 19, 1991. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zezzi do Valle Gomes, M.; Nabavi Zadeh, P.S.; Palmqvist, A.E.C.; Åkerman, B. Spatial Distribution of Enzymes Immobilized in Mesoporous Silicas for Biocatalysis. ACS Appl. Nano Mater. 2019, 2, 7245–7254. [Google Scholar] [CrossRef]
- Clemments, A.M.; Botella, P.; Landry, C.C. Spatial Mapping of Protein Adsorption on Mesoporous Silica Nanoparticles by Stochastic Optical Reconstruction Microscopy. J. Am. Chem. Soc. 2017, 139, 3978–3981. [Google Scholar] [CrossRef]
- Chen, S.; Wang, J.; Xin, B.; Yang, Y.; Ma, Y.; Zhou, Y.; Yuan, L.; Huang, Z.; Yuan, Q. Direct Observation of Nanoparticles within Cells at Subcellular Levels by Super-Resolution Fluorescence Imaging. Anal. Chem. 2019, 91, 5747–5752. [Google Scholar] [CrossRef]
- Weiss, A.C.G.; Krüger, K.; Besford, Q.A.; Schlenk, M.; Kempe, K.; Förster, S.; Caruso, F. In Situ Characterization of Protein Corona Formation on Silica Microparticles Using Confocal Laser Scanning Microscopy Combined with Microfluidics. ACS Appl. Mater. Interfaces 2019, 11, 2459–2469. [Google Scholar] [CrossRef] [PubMed]
- Fijneman, A.J.; Heinrichs, J.M.J.J.; van Leuken, S.H.M.; de With, G.; Friedrich, H. Time-resolved investigation of mesoporous silica microsphere formation using in situ heating optical microscopy. J. Colloid Interface Sci. 2021, 585, 118–125. [Google Scholar] [CrossRef]
- Marrese, M.; Guarino, V.; Ambrosio, L. Atomic Force Microscopy: A Powerful Tool to Address Scaffold Design in Tissue Engineering. J. Funct. Biomater. 2017, 8, 7. [Google Scholar] [CrossRef] [Green Version]
- Ivanov, Y.D.; Pleshakova, T.O.; Shumov, I.D.; Kozlov, A.F.; Ivanova, I.A.; Valueva, A.A.; Tatur, V.Y.; Smelov, M.V.; Ivanova, N.D.; Ziborov, V.S. AFM Imaging of Protein Aggregation in Studying the Impact of Knotted Electromagnetic Field on A Peroxidase. Sci. Rep. 2020, 10, 9022. [Google Scholar] [CrossRef] [PubMed]
- Ariaeenejad, S.; Jokar, F.; Hadian, P.; Ma’mani, L.; Gharaghani, S.; Fereidoonnezhad, M.; Salekdeh, G.H. An efficient nano-biocatalyst for lignocellulosic biomass hydrolysis: Xylanase immobilization on organically modified biogenic mesoporous silica nanoparticles. Int. J. Biol. Macromol. 2020, 164, 3462–3473. [Google Scholar] [CrossRef]
- Ménard, M.; Meyer, F.; Parkhomenko, K.; Leuvrey, C.; Francius, G.; Bégin-Colin, S.; Mertz, D. Mesoporous silica templated-albumin nanoparticles with high doxorubicin payload for drug delivery assessed with a 3-D tumor cell model. Biochim. Biophys. Acta 2019, 1863, 332–341. [Google Scholar] [CrossRef]
- Chaudhary, Z.; Khan, G.M.; Abeer, M.M.; Pujara, N.; Wan-Chi Tse, B.; McGuckin, M.A.; Popat, A.; Kumeria, T. Efficient photoacoustic imaging using indocyanine green (ICG) loaded functionalized mesoporous silica nanoparticles. Biomater. Sci. 2019, 7, 5002–5015. [Google Scholar] [CrossRef] [PubMed]
- Kang, J.; Kim, D.; Wang, J.; Han, Y.; Zuidema, J.M.; Hariri, A.; Park, J.H.; Jokerst, J.V.; Sailor, M.J. Enhanced Performance of a Molecular Photoacoustic Imaging Agent by Encapsulation in Mesoporous Silicon Nanoparticles. Adv. Mater. 2018, 30, e1800512. [Google Scholar] [CrossRef]
- Prokopowicz, M.; Żegliński, J.; Gandhi, A.; Sawicki, W.; Tofail, S.A.M. Bioactive silica-based drug delivery systems containing doxorubicin hydrochloride: In vitro studies. Colloids Surf. B Biointerfaces 2012, 93, 249–259. [Google Scholar] [CrossRef] [PubMed]
- Geppi, M.; Mollica, G.; Borsacchi, S.; Veracini, C.A. Solid-State NMR Studies of Pharmaceutical Systems. Appl. Spectrosc. Rev. 2008, 43, 202–302. [Google Scholar] [CrossRef]
- Merisko-Liversidge, E.M.; Liversidge, G.G. Drug Nanoparticles: Formulating Poorly Water-Soluble Compounds. Toxicol. Pathol. 2008, 36, 43–48. [Google Scholar] [CrossRef] [PubMed]
- Kalepu, S.; Nekkanti, V. Insoluble drug delivery strategies: Review of recent advances and business prospects. Acta Pharm. Sin. B 2015, 5, 442–453. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mirzaei, M.; Zarch, M.B.; Darroudi, M.; Sayyadi, K.; Keshavarz, S.T.; Sayyadi, J.; Fallah, A.; Maleki, H. Silica Mesoporous Structures: Effective Nanocarriers in Drug Delivery and Nanocatalysts. Appl. Sci. 2020, 10, 7533. [Google Scholar] [CrossRef]
- Vallet-Regí, M.; Balas, F.; Arcos, D. Mesoporous Materials for Drug Delivery. Angew. Chem. Int. Ed. 2007, 46, 7548–7558. [Google Scholar] [CrossRef]
- Trébosc, J.; Wiench, J.W.; Huh, S.; Lin, V.S.-Y.; Pruski, M. Solid-State NMR Study of MCM-41-type Mesoporous Silica Nanoparticles. J. Am. Chem. Soc. 2005, 127, 3057–3068. [Google Scholar] [CrossRef] [PubMed]
- Trebosc, J.; Wiench, J.W.; Huh, S.; Lin, V.S.-Y.; Pruski, M. Studies of Organically Functionalized Mesoporous Silicas Using Heteronuclear Solid-State Correlation NMR Spectroscopy under Fast Magic Angle Spinning. J. Am. Chem. Soc. 2005, 127, 7587–7593. [Google Scholar] [CrossRef] [PubMed]
- Mao, K.; Kobayashi, T.; Wiench, J.W.; Chen, H.-T.; Tsai, C.-H.; Lin, V.S.-Y.; Pruski, M. Conformations of Silica-Bound (Pentafluorophenyl)propyl Groups Determined by Solid-State NMR Spectroscopy and Theoretical Calculations. J. Am. Chem. Soc. 2010, 132, 12452–12457. [Google Scholar] [CrossRef]
- Wiench, J.W.; Avadhut, Y.S.; Maity, N.; Bhaduri, S.; Lahiri, G.K.; Pruski, M.; Ganapathy, S. Characterization of Covalent Linkages in Organically Functionalized MCM-41 Mesoporous Materials by Solid-State NMR and Theoretical Calculations. J. Phys. Chem. B 2007, 111, 3877–3885. [Google Scholar] [CrossRef]
- Kobayashi, T.; Pruski, M. Spatial Distribution of Silica-Bound Catalytic Organic Functional Groups Can Now Be Revealed by Conventional and DNP-Enhanced Solid-State NMR Methods. ACS Catal. 2019, 9, 7238–7249. [Google Scholar] [CrossRef] [Green Version]
- Perras, F.A.; Kobayashi, T.; Pruski, M. Natural Abundance 17O DNP Two-Dimensional and Surface-Enhanced NMR Spectroscopy. J. Am. Chem. Soc. 2015, 137, 8336–8339. [Google Scholar] [CrossRef]
- Perras, F.A.; Chaudhary, U.; Slowing, I.I.; Pruski, M. Probing Surface Hydrogen Bonding and Dynamics by Natural Abundance, Multidimensional, 17O DNP-NMR Spectroscopy. J. Phys. Chem. C 2016, 120, 11535–11544. [Google Scholar] [CrossRef] [Green Version]
- Baccile, N. Application of Advanced Solid-State NMR Techniques to the Characterization of Nanomaterials: A Focus on Interfaces and Structure. In Ideas in Chemistry and Molecular Sciences: Advances in Nanotechnology, Part II; Pignataro, B., Ed.; WILEY-VCH Verlag GmbH: Weinheim, Germany, 2010; pp. 139–182. [Google Scholar]
- Shenderovich, I.G.; Limbach, H.-H. Solid State NMR for Nonexperts: An Overview of Simple but General Practical Methods. Solids 2021, 2, 139–154. [Google Scholar] [CrossRef]
- Babonneau, F.; Yeung, L.; Steunou, N.; Gervais, C. Solid State NMR Characterisation of Encapsulated Molecules in Mesoporous Silica. J. Sol. Gel Sci. Technol. 2004, 31, 219–223. [Google Scholar] [CrossRef]
- Azaïs, T.; Tourné-Péteilh, C.; Aussenac, F.; Baccile, N.; Coelho, C.; Devoisselle, J.-M.; Babonneau, F. Solid-State NMR Study of Ibuprofen Confined in MCM-41 Material. Chem. Mater. 2006, 18, 6382–6390. [Google Scholar] [CrossRef]
- Azaïs, T.; Laurent, G.; Panesar, K.; Nossov, A.; Guenneau, F.; Sanfeliu Cano, C.; Tourné-Péteilh, C.; Devoisselle, J.-M.; Babonneau, F. Implication of Water Molecules at the Silica–Ibuprofen Interface in Silica-Based Drug Delivery Systems Obtained through Incipient Wetness Impregnation. J. Phys. Chem. C 2017, 121, 26833–26839. [Google Scholar] [CrossRef]
- Ukmar, T.; Čendak, T.; Mazaj, M.; Kaučič, V.; Mali, G. Structural and Dynamical Properties of Indomethacin Molecules Embedded within the Mesopores of SBA-15: A Solid-State NMR View. J. Phys. Chem. C 2012, 116, 2662–2671. [Google Scholar] [CrossRef]
- Azaïs, T.; Hartmeyer, G.; Quignard, S.; Laurent, G.; Tourné-Péteilh, C.; Devoisselle, J.-M.; Babonneau, F. Solid-state NMR characterization of drug-model molecules encapsulated in MCM-41 silica. Pure Appl. Chem. 2009, 81, 1345–1355. [Google Scholar] [CrossRef]
- Ruffel, L.; Soulié, J.; Coppel, Y.; Roblin, P.; Brouillet, F.; Frances, C.; Tourbin, M. Ibuprofen loading into mesoporous silica nanoparticles using Co-Spray drying: A multi-scale study. Micropor. Mesopor. Mater. 2020, 291, 109689. [Google Scholar] [CrossRef]
- Vogt, F.G.; Roberts-Skilton, K.; Kennedy-Gabb, S.A. A solid-state NMR study of amorphous ezetimibe dispersions in mesoporous silica. Pharm. Res. 2013, 30, 2315–2331. [Google Scholar] [CrossRef]
- Fatnassi, M.; Tourne-Peteilh, C.; Mineva, T.; Devoisselle, J.-M.; Gaveau, P.; Fayon, F.; Alonso, B. Drug nano-domains in spray-dried ibuprofen-silica microspheres. Phys. Chem. Chem. Phys. 2012, 14, 1463–9076. [Google Scholar] [CrossRef] [PubMed]
- Ukmar, T.; Godec, A.; Planinšek, O.; Kaučič, V.; Mali, G.; Gaberšček, M. The phase (trans)formation and physical state of a model drug in mesoscopic confinement. Phys. Chem. Chem. Phys. 2011, 13, 16046–16054. [Google Scholar] [CrossRef]
- Aiello, D.; Folliet, N.; Laurent, G.; Testa, F.; Gervais, C.; Babonneau, F.; Azaïs, T. Solid state NMR characterization of phenylphosphonic acid encapsulated in SBA-15 and aminopropyl-modified SBA-15. Micropor. Mesopor. Mater. 2013, 166, 109–116. [Google Scholar] [CrossRef]
- Datt, A.; El-Maazawi, I.; Larsen, S.C. Aspirin Loading and Release from MCM-41 Functionalized with Aminopropyl Groups via Co-condensation or Postsynthesis Modification Methods. J. Phys. Chem. C 2012, 116, 18358–18366. [Google Scholar] [CrossRef]
- Brodrecht, M.; Kumari, B.; Breitzke, H.; Gutmann, T.; Buntkowsky, G. Chemically Modified Silica Materials as Model Systems for the Characterization of Water-Surface Interactions. Z. Phys. Chem. 2018, 232, 1127–1146. [Google Scholar] [CrossRef]
- Juère, E.; Caillard, R.; Kleitz, F. Pore confinement and surface charge effects in protein-mesoporous silica nanoparticles formulation for oral drug delivery. Micropor. Mesopor. Mater. 2020, 306, 110482. [Google Scholar] [CrossRef]
- Juère, E.; Kleitz, F. On the nanopore confinement of therapeutic drugs into mesoporous silica materials and its implications. Micropor. Mesopor. Mater. 2018, 270, 109–119. [Google Scholar] [CrossRef]
- Riikonen, J.; Mäkilä, E.; Salonen, J.; Lehto, V.-P. Determination of the Physical State of Drug Molecules in Mesoporous Silicon with Different Surface Chemistries. Langmuir 2009, 25, 6137–6142. [Google Scholar] [CrossRef] [PubMed]
- Patrick, W.A.; Kemper, W.A. Melting temperatures of compounds adsorbed on silica gel1. J. Phys. Chem. 1938, 42, 369–380. [Google Scholar] [CrossRef]
- Rennie, G.K.; Clifford, J. Melting of ice in porous solids. J. Chem. Soc. Faraday Trans. 1 1977, 73, 680–689. [Google Scholar] [CrossRef]
- Morineau, D.; Guegan, R.; Xia, Y.; Alba-Simionesco, C. Structure of liquid and glassy methanol confined in cylindrical pores. J. Chem. Phys. 2004, 121, 1466–1473. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morishige, K.; Kawano, K. Freezing and melting of methanol in a single cylindrical pore: Dynamical supercooling and vitrification of methanol. J. Chem. Phys. 2000, 112, 11023–11029. [Google Scholar] [CrossRef]
- Takei, T.; Konishi, T.; Fuji, M.; Watanabe, T.; Chikazawa, M. Phase transition of capillary condensed liquids in porous silica: Effect of surface hydroxyl groups. Thermochimica Acta 1995, 267, 159–167. [Google Scholar] [CrossRef]
- Gedat, E.; Schreiber, A.; Albrecht, J.; Emmler, T.; Shenderovich, I.; Findenegg, G.H.; Limbach, H.-H.; Buntkowsky, G. 2H-Solid-State NMR Study of Benzene-d6 Confined in Mesoporous Silica SBA-15. J. Phys. Chem. B 2002, 106, 1977–1984. [Google Scholar] [CrossRef]
- Aksnes, D.W.; Kimtys, L. 1H and 2H NMR studies of benzene confined in porous solids: Melting point depression and pore size distribution. Solid State Nucl. Magn. Reson. 2004, 25, 146–152. [Google Scholar] [CrossRef]
- Tielens, F.; Folliet, N.; Bondaz, L.; Etemovic, S.; Babonneau, F.; Gervais, C.; Azaïs, T. Molecular Picture of the Adsorption of Ibuprofen and Benzoic Acid on Hydrated Amorphous Silica through DFT-D Calculations Combined with Solid-State NMR Experiments. J. Phys. Chem. C 2017, 121, 17339–17347. [Google Scholar] [CrossRef] [Green Version]
- Skorupska, E.; Jeziorna, A.; Potrzebowski, M.J. Thermal Solvent-Free Method of Loading of Pharmaceutical Cocrystals into the Pores of Silica Particles: A Case of Naproxen/Picolinamide Cocrystal. J. Phys. Chem. C 2016, 120, 13169–13180. [Google Scholar] [CrossRef]
- Skorupska, E.; Kaźmierski, S.; Potrzebowski, M.J. Solid State NMR Characterization of Ibuprofen:Nicotinamide Cocrystals and New Idea for Controlling Release of Drugs Embedded into Mesoporous Silica Particles. Mol. Pharm. 2017, 14, 1800–1810. [Google Scholar] [CrossRef]
- Karagianni, A.; Malamatari, M.; Kachrimanis, K. Pharmaceutical Cocrystals: New Solid Phase Modification Approaches for the Formulation of APIs. Pharmaceutics 2018, 10, 18. [Google Scholar] [CrossRef] [Green Version]
- Douroumis, D.; Ross, S.A.; Nokhodchi, A. Advanced methodologies for cocrystal synthesis. Adv. Drug Deliv. Rev. 2017, 117, 178–195. [Google Scholar] [CrossRef]
- Pindelska, E.; Sokal, A.; Kolodziejski, W. Pharmaceutical cocrystals, salts and polymorphs: Advanced characterization techniques. Adv. Drug Deliv. Rev. 2017, 117, 111–146. [Google Scholar] [CrossRef]
- Skorupska, E.; Jeziorna, A.; Kazmierski, S.; Potrzebowski, M.J. Recent progress in solid-state NMR studies of drugs confined within drug delivery systems. Solid State Nucl. Magn. Reson. 2014, 57–58, 2–16. [Google Scholar] [CrossRef] [PubMed]
- Dudek, M.K.; Kaźmierski, S.; Potrzebowski, M.J. Fast and very fast MAS solid state NMR studies of pharmaceuticals. Annu. Rep. NMR Spectrosc. 2021. [Google Scholar] [CrossRef]
- Li, M.Y.; Xu, W.; Su, Y.C. Solid-state NMR spectroscopy in pharmaceutical sciences. TRAC Trend Anal. Chem. 2021, 135. [Google Scholar] [CrossRef]
- Wu, H.M.; Xiao, Y.; Guo, Y.; Miao, S.J.; Chen, Q.Q.; Chen, Z. Functionalization of SBA-15 mesoporous materials with 2-acetylthiophene for adsorption of Cr(III) ions. Micropor. Mesopor. Mater. 2020, 292, 109754–109765. [Google Scholar] [CrossRef]
- Melnyk, I.V.; Nazarchuk, G.I.; Vaclavikova, M.; Zub, Y.L. IR spectroscopy study of SBA-15 silicas functionalized with the ethylthiocarbamidepropyl groups and their interactions with Ag(I) and Hg(II) ions. Appl. Nanosci. 2019, 9, 683–694. [Google Scholar] [CrossRef]
- Tomozawa, M.; Hong, J.W.; Ryu, S.R. Infrared (IR) investigation of the structural changes of silica glasses with fictive temperature. J. Non. Cryst. Solids 2005, 351, 1054–1060. [Google Scholar] [CrossRef]
- Acharya, M.; Mishra, S.; Sahoo, R.N.; Mallick, S. Infrared Spectroscopy for Analysis of Co-processed Ibuprofen and Magnesium Trisilicate at Milling and Freeze Drying. Acta Chim. Slov. 2017, 64, 45–54. [Google Scholar] [CrossRef] [Green Version]
- Daneluti, A.L.M.; Neto, F.M.; Velasco, M.V.R.; Baby, A.R.; Matos, J.D. Evaluation and characterization of the encapsulation/entrapping process of octyl methoxycinnamate in ordered mesoporous silica type SBA-15. J. Therm. Anal. Calorim. 2018, 131, 789–798. [Google Scholar] [CrossRef]
- Albayati, T.M.; Salih, I.K.; Alazzawi, H.F. Synthesis and characterization of a modified surface of SBA-15 mesoporous silica for a chloramphenicol drug delivery system. Heliyon 2019, 5, e02539–e02547. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, L.K.; Gao, H.W. Molecular structure and vibrational spectra of ibuprofen using density function theory calculations. Spectrochim. Acta A Mol. Biomol. Spectrosc. 2012, 89, 201–209. [Google Scholar] [CrossRef]
- Lai, J.M.; Lin, W.; Scholes, P.; Li, M.Z. Investigating the Effects of Loading Factors on the In Vitro Pharmaceutical Performance of Mesoporous Materials as Drug Carriers for Ibuprofen. Materials 2017, 10, 150. [Google Scholar] [CrossRef] [Green Version]
- Tzankov, B.; Tzankova, V.; Aluani, D.; Yordanov, Y.; Spassova, I.; Kovacheva, D.; Avramova, K.; Valoti, M.; Yoncheva, K. Development of MCM-41 mesoporous silica nanoparticles as a platform for pramipexole delivery. J. Drug Deliv. Sci. Technol. 2019, 51, 26–35. [Google Scholar] [CrossRef]
- Rahman, M.M.; Aznan, M.; Yusof, A.M.; Ansaryr, H.; Siddiqi, M.J.; Yusan, S. Synthesis and Characterization of Functionalized Se-MCM-41 a New Drug Carrier Mesopore Composite. Orient. J. Chem. 2017, 33, 611–621. [Google Scholar] [CrossRef] [Green Version]
- Salam, M.S.A.; Betiha, M.A.; Shaban, S.A.; Elsabagh, A.M.; Abd El-Aal, R.M.; El Kady, F.Y. Synthesis and characterization of MCM-41-supported nano zirconia catalysts. Egypt. J. Pet. 2015, 24, 49–57. [Google Scholar] [CrossRef] [Green Version]
- Liu, Y.M.; Cao, Y.; Yi, N.; Feng, W.L.; Dai, W.L.; Yan, S.R.; He, H.Y.; Fan, K.N. Vanadium oxide supported on mesoporous SBA-15 as highly selective catalysts in the oxidative dehydrogenation of propane. J. Catal. 2004, 224, 417–428. [Google Scholar] [CrossRef]
- Varache, M.; Bezverkhyy, I.; Weber, G.; Saviot, L.; Chassagnon, R.; Baras, F.; Bouyer, F. Loading of Cisplatin into Mesoporous Silica Nanoparticles: Effect of Surface Functionalization. Langmuir 2019, 35, 8984–8995. [Google Scholar] [CrossRef]
- Hellstaen, S.; Qu, H.Y.; Heikkila, T.; Kohonen, J.; Reinikainen, S.P.; Louhi-Kultanen, M. Raman spectroscopic imaging of indomethacin loaded in porous silica. Cryst. Eng. Comm. 2012, 14, 1582–1587. [Google Scholar] [CrossRef]
- Paudel, A.; Raijada, D.; Rantanen, J. Raman spectroscopy in pharmaceutical product design. Adv. Drug Deliv. Rev. 2015, 89, 3–20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fussell, A.L.; Mah, P.T.; Offerhaus, H.; Niemi, S.M.; Salonen, J.; Santos, H.A.; Strachan, C. Coherent anti-Stokes Raman scattering microscopy driving the future of loaded mesoporous silica imaging. Acta Biomater. 2014, 10, 4870–4877. [Google Scholar] [CrossRef]
- Scrivens, G.; Ticehurst, M.; Swanson, J.T. Strategies for improving the reliability of accelerated predictive stability (APS) studies. In Accelerated Predictive Stability; Qiu, F., Scrivens, G., Eds.; Academic Press: Cambridge, MA, USA, 2018; pp. 175–206. [Google Scholar] [CrossRef]
- Biswas, N. Modified mesoporous silica nanoparticles for enhancing oral bioavailability and antihypertensive activity of poorly water soluble valsartan. Eur. J. Pharm. Sci. 2017, 99, 152–160. [Google Scholar] [CrossRef]
- Abedi, M.; Abolmaali, S.S.; Abedanzadeh, M.; Farjadian, F.; Mohammadi Samani, S.; Tamaddon, A.M. Core-Shell Imidazoline-Functionalized Mesoporous Silica Superparamagnetic Hybrid Nanoparticles as a Potential Theranostic Agent for Controlled Delivery of Platinum(II) Compound. Int. J. Nanomed. 2020, 15, 2617–2631. [Google Scholar] [CrossRef] [Green Version]
- Peralta, M.E.; Jadhav, S.A.; Magnacca, G.; Scalarone, D.; Mártire, D.O.; Parolo, M.E.; Carlos, L. Synthesis and in vitro testing of thermoresponsive polymer-grafted core-shell magnetic mesoporous silica nanoparticles for efficient controlled and targeted drug delivery. J. Colloid Interface Sci. 2019, 544, 198–205. [Google Scholar] [CrossRef]
- Zhang, W.; Zheng, N.; Chen, L.; Xie, L.; Cui, M.; Li, S.; Xu, L. Effect of Shape on Mesoporous Silica Nanoparticles for Oral Delivery of Indomethacin. Pharmaceutics 2019, 11, 4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Delpiano, G.R.; Casula, M.F.; Piludu, M.; Corpino, R.; Ricci, P.C.; Vallet-Regí, M.; Sanjust, E.; Monduzzi, M.; Salis, A. Assembly of Multicomponent Nano-Bioconjugates Composed of Mesoporous Silica Nanoparticles, Proteins, and Gold Nanoparticles. ACS Omega 2019, 4, 11044–11052. [Google Scholar] [CrossRef]
- Gounani, Z.; Asadollahi, M.A.; Pedersen, J.N.; Lyngsø, J.; Skov Pedersen, J.; Arpanaei, A.; Meyer, R.L. Mesoporous silica nanoparticles carrying multiple antibiotics provide enhanced synergistic effect and improved biocompatibility. Colloids Surf. B 2019, 175, 498–508. [Google Scholar] [CrossRef] [PubMed]
- Harada, M.; Nakamura, T.; Yano, K. Evaluating the internal structure of monodispersed mesoporous silica spheres by small-angle X-ray scattering. Colloid Interface Sci. Commun. 2019, 33, 100203. [Google Scholar] [CrossRef]
- Yi, Z.; Dumée, L.F.; Garvey, C.J.; Feng, C.; She, F.; Rookes, J.E.; Mudie, S.; Cahill, D.M.; Kong, L. A New Insight into Growth Mechanism and Kinetics of Mesoporous Silica Nanoparticles by in Situ Small Angle X-ray Scattering. Langmuir 2015, 31, 8478–8487. [Google Scholar] [CrossRef] [PubMed]
- Schmitt, J.; Kjellman, T.; Kwaśniewski, P.; Meneau, F.; Pedersen, J.S.; Edler, K.J.; Rennie, A.R.; Alfredsson, V.; Impéror-Clerc, M. Outset of the Morphology of Nanostructured Silica Particles during Nucleation Followed by Ultrasmall-Angle X-ray Scattering. Langmuir 2016, 32, 5162–5172. [Google Scholar] [CrossRef]
- Bhavsar, D.; Gajjar, J.; Sawant, K. Formulation and development of smart pH responsive mesoporous silica nanoparticles for breast cancer targeted delivery of anastrozole: In vitro and in vivo characterizations. Micropor. Mesopor. Mater. 2019, 279, 107–116. [Google Scholar] [CrossRef]
- Limnell, T.; Heikkilä, T.; Santos, H.A.; Sistonen, S.; Hellstén, S.; Laaksonen, T.; Peltonen, L.; Kumar, N.; Murzin, D.Y.; Louhi-Kultanen, M.; et al. Physicochemical stability of high indomethacin payload ordered mesoporous silica MCM-41 and SBA-15 microparticles. Int. J. Pharm. 2011, 416, 242–251. [Google Scholar] [CrossRef] [PubMed]
- Hooshyar, S.; Nafisi, S.; Mohseni, M.; Mehravi, B. Design and synthesis of potential nano-carrier for delivery of diphencyprone to hair follicle. J. Pharm. Investig. 2021, 51, 173–181. [Google Scholar] [CrossRef]
- Christoforidou, T.; Giasafaki, D.; Andriotis, E.G.; Bouropoulos, N.; Theodoroula, N.F.; Vizirianakis, I.S.; Steriotis, T.; Charalambopoulou, G.; Fatouros, D.G. Oral Drug Delivery Systems Based on Ordered Mesoporous Silica Nanoparticles for Modulating the Release of Aprepitant. Int. J. Mol. Sci. 2021, 22, 1896. [Google Scholar] [CrossRef]
- Masood, A.; Maheen, S.; Khan, H.U.; Shafqat, S.S.; Irshad, M.; Aslam, I.; Rasul, A.; Bashir, S.; Zafar, M.N. Pharmaco-Technical Evaluation of Statistically Formulated and Optimized Dual Drug-Loaded Silica Nanoparticles for Improved Antifungal Efficacy and Wound Healing. ACS Omega 2021, 6, 8210–8225. [Google Scholar] [CrossRef] [PubMed]
- Chaudhary, Z.; Subramaniam, S.; Khan, G.M.; Abeer, M.M.; Qu, Z.; Janjua, T.; Kumeria, T.; Batra, J.; Popat, A. Encapsulation and Controlled Release of Resveratrol Within Functionalized Mesoporous Silica Nanoparticles for Prostate Cancer Therapy. Front. Bioeng. Biotechnol. 2019, 7, 225. [Google Scholar] [CrossRef]
- Mohseni, M.; Gilani, K.; Mortazavi, S.A. Preparation and characterization of rifampin loaded mesoporous silica nanoparticles as a potential system for pulmonary drug delivery. Iran. J. Pharm. Res. 2015, 14, 27–34. [Google Scholar] [PubMed]
- Baer, D.R.; Shutthanandan, V. Nano-objects as biomaterials: Immense opportunities, significant challenges and the important use of surface analytical methods. In Comprehensive Biomaterials II; Elsevier: Amsterdam, The Netherlands, 2017; Volume 3.6, pp. 86–107. [Google Scholar]
- Barnes, T.J.; Kempson, I.M.; Prestidge, C.A. Surface analysis for compositional, chemical and structural imaging in pharmaceutics with mass spectrometry: A ToF-SIMS perspective. Int. J. Pharm. 2011, 417, 61–69. [Google Scholar] [CrossRef]
- Kempson, I.M.; Barnes, T.J.; Prestidge, C.A. Use of TOF-SIMS to Study Adsorption and Loading Behavior of Methylene Blue and Papain in a Nano-Porous Silicon Layer. J. Am. Soc. Mass Spectrom. 2010, 21, 254–260. [Google Scholar] [CrossRef] [Green Version]
- Clemens, D.; Lee, B.-Y.; Plamthottam, S.; Tullius, M.V.; Wang, R.; Yu, C.-J.; Li, Z.; Dillon, B.J.; Zink, J.I.; Horwitz, M.A. Nanoparticle Formulation of Moxifloxacin and Intramuscular Route of Delivery Improve Antibiotic Pharmacokinetics and Treatment of Pneumonic Tularemia in a Mouse Model. ACS Infect. Dis. 2019, 5, 281–291. [Google Scholar] [CrossRef]
- Kaasalainen, M.; Aseyev, V.; von Haartman, E.; Karaman, D.Ş.; Mäkilä, E.; Tenhu, H.; Rosenholm, J.; Salonen, J. Size, Stability, and Porosity of Mesoporous Nanoparticles Characterized with Light Scattering. Nanoscale Res. Lett. 2017, 12, 74. [Google Scholar] [CrossRef] [Green Version]
- Patel, V.R.; Agrawal, Y.K. Nanosuspension: An approach to enhance solubility of drugs. J. Adv. Pharm. Technol. Res. 2011, 2, 81–87. [Google Scholar] [CrossRef]
- Bhattacharjee, S. DLS and zeta potential—What they are and what they are not? J. Controll. Release 2016, 235, 337–351. [Google Scholar] [CrossRef]
- You, Y.; He, L.; Ma, B.; Chen, T. High-Drug-Loading Mesoporous Silica Nanorods with Reduced Toxicity for Precise Cancer Therapy against Nasopharyngeal Carcinoma. Adv. Funct. Mat. 2017, 27, 1703313. [Google Scholar] [CrossRef]
- Muster, T.H.; Prestidge, C.A.; Hayes, R.A. Water adsorption kinetics and contact angles of silica particles. Colloids Surf. A 2001, 176, 253–266. [Google Scholar] [CrossRef]
- Rother, G.; Stack, A.G.; Gautam, S.; Liu, T.; Cole, D.R.; Busch, A. Water Uptake by Silica Nanopores: Impacts of Surface Hydrophilicity and Pore Size. J. Phys. Chem. C 2020, 124, 15188–15194. [Google Scholar] [CrossRef]
- Ho, Y.-J.; Wu, C.-H.; Jin, Q.-F.; Lin, C.-Y.; Chiang, P.-H.; Wu, N.; Fan, C.-H.; Yang, C.-M.; Yeh, C.-K. Superhydrophobic drug-loaded mesoporous silica nanoparticles capped with β-cyclodextrin for ultrasound image-guided combined antivascular and chemo-sonodynamic therapy. Biomaterials 2020, 232, 119723. [Google Scholar] [CrossRef]
- Skwira, A.; Szewczyk, A.; Prokopowicz, M. The Effect of Polydimethylsiloxane-Ethylcellulose Coating Blends on the Surface Characterization and Drug Release of Ciprofloxacin-Loaded Mesoporous Silica. Polymers 2019, 11, 1450. [Google Scholar] [CrossRef] [Green Version]
- Mäkilä, E.; Bimbo, L.M.; Kaasalainen, M.; Herranz, B.; Airaksinen, A.J.; Heinonen, M.; Kukk, E.; Hirvonen, J.; Santos, H.A.; Salonen, J. Amine Modification of Thermally Carbonized Porous Silicon with Silane Coupling Chemistry. Langmuir 2012, 28, 14045–14054. [Google Scholar] [CrossRef]
- Chen, W.-Y.; Matulis, D.; Hu, W.-P.; Lai, Y.-F.; Wang, W.-H. Studies of the interactions mechanism between DNA and silica surfaces by Isothermal Titration Calorimetry. J. Taiwan Inst. Chem. Eng. 2020, 116, 62–66. [Google Scholar] [CrossRef]
- Khan, M.A.; Kiser, M.R.; Moradipour, M.; Nadeau, E.A.; Ghanim, R.W.; Webb, B.A.; Rankin, S.E.; Knutson, B.L. Effect of Confinement in Nanopores on RNA Interactions with Functionalized Mesoporous Silica Nanoparticles. J. Phys. Chem. B 2020, 124, 8549–8561. [Google Scholar] [CrossRef]
- Zhang, X.; Cresswell, M. Silica-Based Amorphous Drug Delivery Systems. In Inorganic Controlled Release Technology; Zhang, X., Cresswell, M., Eds.; Butterworth-Heinemann: Oxford, UK, 2016; pp. 93–137. [Google Scholar]
- Waters, L.J.; Hanrahan, J.P.; Tobin, J.M.; Finch, C.V.; Parkes, G.M.B.; Ahmad, S.A.; Mohammad, F.; Saleem, M. Enhancing the dissolution of phenylbutazone using Syloid® based mesoporous silicas for oral equine applications. J. Pharm. Anal. 2018, 8, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Mura, P.; Valleri, M.; Fabianelli, E.; Maestrelli, F.; Cirri, M. Characterization and evaluation of different mesoporous silica kinds as carriers for the development of effective oral dosage forms of glibenclamide. Int. J. Pharm. 2019, 563, 43–52. [Google Scholar] [CrossRef] [PubMed]
- Angelopoulou, A.; Efthimiadou, E.K.; Kordas, G. Dextran modified pH sensitive silica hydro-xerogels as promising drug delivery scaffolds. Mater. Lett. 2012, 74, 50–53. [Google Scholar] [CrossRef]
- Zhang, P.; Jiang, Q.; Zheng, Y.; Li, J. Double-nano silica xerogel contributes to establish nifedipine delivery system with superior delivery effect. Micropor. Mesopor. Mater. 2020, 296, 109996. [Google Scholar] [CrossRef]
- Rajanna, S.K.; Kumar, D.; Vinjamur, M.; Mukhopadhyay, M. Silica Aerogel Microparticles from Rice Husk Ash for Drug Delivery. Ind. Eng. Chem. Res. 2015, 54, 949–956. [Google Scholar] [CrossRef]
- Smirnova, I.; Suttiruengwong, S.; Arlt, W. Feasibility study of hydrophilic and hydrophobic silica aerogels as drug delivery systems. J. Non Cryst. Solids 2004, 350, 54–60. [Google Scholar] [CrossRef]
- Giray, S.; Bal, T.; Kartal, A.M.; Kızılel, S.; Erkey, C. Controlled drug delivery through a novel PEG hydrogel encapsulated silica aerogel system. J. Biomed. Mater. Res. A 2012, 100A, 1307–1315. [Google Scholar] [CrossRef]
- Guenther, U.; Smirnova, I.; Neubert, R.H.H. Hydrophilic silica aerogels as dermal drug delivery systems—Dithranol as a model drug. Eur. J. Pharm. Biopharm. 2008, 69, 935–942. [Google Scholar] [CrossRef]
- Luo, G.; Chen, W.; Jia, H.; Sun, Y.; Cheng, H.; Zhuo, R.; Zhang, X. An indicator-guided photo-controlled drug delivery system based on mesoporous silica/gold nanocomposites. Nano Res. 2015, 8, 1893–1905. [Google Scholar] [CrossRef]
- Zou, H.; Wu, S.; Shen, J. Polymer/Silica Nanocomposites: Preparation, Characterization, Properties, and Applications. Chem. Rev. 2008, 108, 3893–3957. [Google Scholar] [CrossRef]
- Rasouli, S.; Davaran, S.; Rasouli, F.; Mahkam, M.; Salehi, R. Synthesis, characterization and pH-controllable methotrexate release from biocompatible polymer/silica nanocomposite for anticancer drug delivery. Drug Deliv. 2014, 21, 155–163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dementeva, O.V.; Senchikhin, I.N.; Kartseva, M.E.; Ogarev, V.A.; Zaitseva, A.V.; Matushkina, N.N.; Rudoy, V.M. A new method for loading mesoporous silica nanoparticles with drugs: Sol–gel synthesis using drug micelles as a template. Colloid J. 2016, 78, 586–595. [Google Scholar] [CrossRef]
- Hagman, E.; Elimam, A.; Kupferschmidt, N.; Ekbom, K.; Rössner, S.; Iqbal, M.N.; Johnston, E.; Lindgren, M.; Bengtsson, T.; Danielsson, P. Oral intake of mesoporous silica is safe and well tolerated in male humans. PLoS ONE 2020, 15, e0240030. [Google Scholar] [CrossRef] [PubMed]
- Phillips, E.; Penate-Medina, O.; Zanzonico, P.B.; Carvajal, R.D.; Mohan, P.; Ye, Y.; Humm, J.; Gönen, M.; Kalaigian, H.; Schöder, H.; et al. Clinical translation of an ultrasmall inorganic optical-PET imaging nanoparticle probe. Sci. Transl. Med. 2014, 6, 260ra149. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Donaldson, L. ‘Cornell Dots’ receive approval for clinical trials: Nanotechnology. Mater. Today 2011, 14, 131. [Google Scholar] [CrossRef]
- Chen, F.; Ma, K.; Madajewski, B.; Zhuang, L.; Zhang, L.; Rickert, K.; Marelli, M.; Yoo, B.; Turker, M.Z.; Overholtzer, M.; et al. Ultrasmall targeted nanoparticles with engineered antibody fragments for imaging detection of HER2-overexpressing breast cancer. Nat. Commun. 2018, 9, 4141. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Drug | BCS Class | MSP | Loading Method | Reference |
|---|---|---|---|---|
| Aceclofenac | II | MCM-41 | Solvent evaporation | [24] |
| Atenolol | III | SBA-16 | Adsorption | [25] |
| Atorvastatin | II | SBA-15 | Solvent evaporation | [26] |
| Carbamazepine | II | SBA-16 | Adsorption | [27] |
| MCM-41 | Adsorption | [28] | ||
| SBA-15 | Incipient wetness | [29] | ||
| SBA-15 | Solvent evaporation | [30] | ||
| OMS | Liquid solid technique | [31] | ||
| Carvedilol | II | MCM-41 | Solvent evaporation | [32] |
| SBA-16 | ||||
| Celecoxib | II | MCM-41 | Adsorption | [33] |
| SBA-15 | [34] | |||
| Cilostazol | II | SNT | Solvent evaporation | [35] |
| Cinnarizine | II | SBA-15 | Incipient wetness | [29] |
| Clofazimine | II | MSN | Chaperone assistance | [36] |
| Danazol | II | SBA-15 | Incipient wetness | [29] |
| Dasatinib | II | SBA-15 | Solvent evaporation | [37] |
| Diazepam | II | SBA-15 | Incipient wetness | [29] |
| Econazole | II | MCM-41 | Melting | [38] |
| Ezetimibe | II | OMS | Incipient wetness | [39] |
| Felodipine | II | MSN | Solvent evaporation | [40] |
| Fenofibrate | II | SBA-15 | Supercritical CO2 | [41] |
| Incipient wetness | [42] | |||
| Physical mixing | [43] | |||
| MCM-41 | Incipient wetness | [44] | ||
| Co-spray drying | [44] | |||
| OMS | Supercritical CO2 | [45] | ||
| Flurbiprofen | II | COK-12 | The one-pot drug loading and synthesis | [46] |
| MCM-41 | Diffusion Supported Loading | [47] | ||
| Furosemide | IV | MCM-41 | Solvent evaporation | [48] |
| SBA-15 | [49] | |||
| Glibenclamide | II | SBA-15 | Incipient wetness | [50] |
| Griseofulvin | II | MCM-41 | Solvent evaporation | [51] |
| Ibuprofen | II | MCM-41 | Diffusion Supported Loading | [47] |
| Liquid CO2 | [52] | |||
| Co-spray drying | [53] | |||
| Incipient wetness | [54] | |||
| Adsorption | [54] | |||
| Covalent grafting | [55] | |||
| SBA-15 | Adsorption | [56] | ||
| Incipient wetness | [57] | |||
| Solvent evaporation | [57] | |||
| Melting | [57] | |||
| Co-spray drying | [58] | |||
| Co-milling | [59] | |||
| Indomethacin | II | SBA-16 | Solvent evaporation | [60] |
| MCM-41 | Solvent evaporation | [61] | ||
| Adsorption | [62] | |||
| SBA-15 | Incipient wetness | [50] | ||
| Solvent evaporation | [61] | |||
| Itraconazole | II | SBA-15 | Solvent evaporation | [57] |
| Incipient wetness | [57,63] | |||
| Melting | [57] | |||
| MCM-41 | Incipient wetness | [63] | ||
| KIT-6 | [63] | |||
| FDU-12 | [63] | |||
| COK-12 | [64] | |||
| Ketoconazole | II | SBA-15 | Incipient wetness | [29] |
| Ketoprofen | II | MCM-41 | Diffusion Supported Loading | [47] |
| Solvent evaporation | [65] | |||
| Incipient wetness | [65] | |||
| Adsorption | [65] | |||
| Methotrexate | III | MCM-41 | Adsorption | [66] |
| Naproxen | II | MCM-41 | Adsorption | [67] |
| SBA-15 | [67] | |||
| Nifedipine | II | SBA-15 | Incipient wetness | [29] |
| Paclitaxel | IV | MSN | Adsorption | [68] |
| Covalent grafting | [69] | |||
| Phenylbutazone | II | SBA-15 | Incipient wetness | [29] |
| Piroxicam | II | SBA-15 | Adsorption | [70] |
| MCM-41 | [71] | |||
| Prednisolone | I | SBA-15 | Adsorption | [72] |
| SBA-3 | [72] | |||
| FDU-12 | [72] | |||
| Resveratrol | II | MSM | Incipient wetness | [73] |
| Rufinamide | II | SBA-16 | Adsorption | [27] |
| Telmisartan | II | MSN | Solvent evaporation | [74] |
| Material [Reference] | H Type | SBET(m2/g) | Pore Volume (cm3/g) | Pore Diameter (nm) | |||
|---|---|---|---|---|---|---|---|
| MSN | MSN-API | MSN | MSN-API | MSN | MSN-API | ||
| MCM41- lomefloxacin [137] | IV/I | 1020 | 866 | 1.04 | 1.02 | 4.1 | 4.7 |
| MCM41- hydroxyatite [138] | IV | 895 | 649 | 0.7 | 0.64 | 3.1 | 3.95 |
| MCM41- Ibuprofen(25.5%) [139] | IV | 1028 | 536 | 0.86 | 0.25 | 2.71 | 1.89 |
| MCM41- Ibuprofen(31.2%) [47] | IV | 1072 | 361 | 0.69 | 0.22 | 2.6 | 1.8 |
| SBA15-cisplatin [140] | IV | 810 | 561 | 0.83 | 0.59 | 4.88 | 4.41 |
| SBA15-Ibuprofen [136] | IV | 787 | 254 | 1.06 | 0.37 | 8.8 | 7.1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Trzeciak, K.; Chotera-Ouda, A.; Bak-Sypien, I.I.; Potrzebowski, M.J. Mesoporous Silica Particles as Drug Delivery Systems—The State of the Art in Loading Methods and the Recent Progress in Analytical Techniques for Monitoring These Processes. Pharmaceutics 2021, 13, 950. https://doi.org/10.3390/pharmaceutics13070950
Trzeciak K, Chotera-Ouda A, Bak-Sypien II, Potrzebowski MJ. Mesoporous Silica Particles as Drug Delivery Systems—The State of the Art in Loading Methods and the Recent Progress in Analytical Techniques for Monitoring These Processes. Pharmaceutics. 2021; 13(7):950. https://doi.org/10.3390/pharmaceutics13070950
Chicago/Turabian StyleTrzeciak, Katarzyna, Agata Chotera-Ouda, Irena I. Bak-Sypien, and Marek J. Potrzebowski. 2021. "Mesoporous Silica Particles as Drug Delivery Systems—The State of the Art in Loading Methods and the Recent Progress in Analytical Techniques for Monitoring These Processes" Pharmaceutics 13, no. 7: 950. https://doi.org/10.3390/pharmaceutics13070950
APA StyleTrzeciak, K., Chotera-Ouda, A., Bak-Sypien, I. I., & Potrzebowski, M. J. (2021). Mesoporous Silica Particles as Drug Delivery Systems—The State of the Art in Loading Methods and the Recent Progress in Analytical Techniques for Monitoring These Processes. Pharmaceutics, 13(7), 950. https://doi.org/10.3390/pharmaceutics13070950






