Tackling Immune Pathogenesis of COVID-19 through Molecular Pharmaceutics
Abstract
1. Introduction
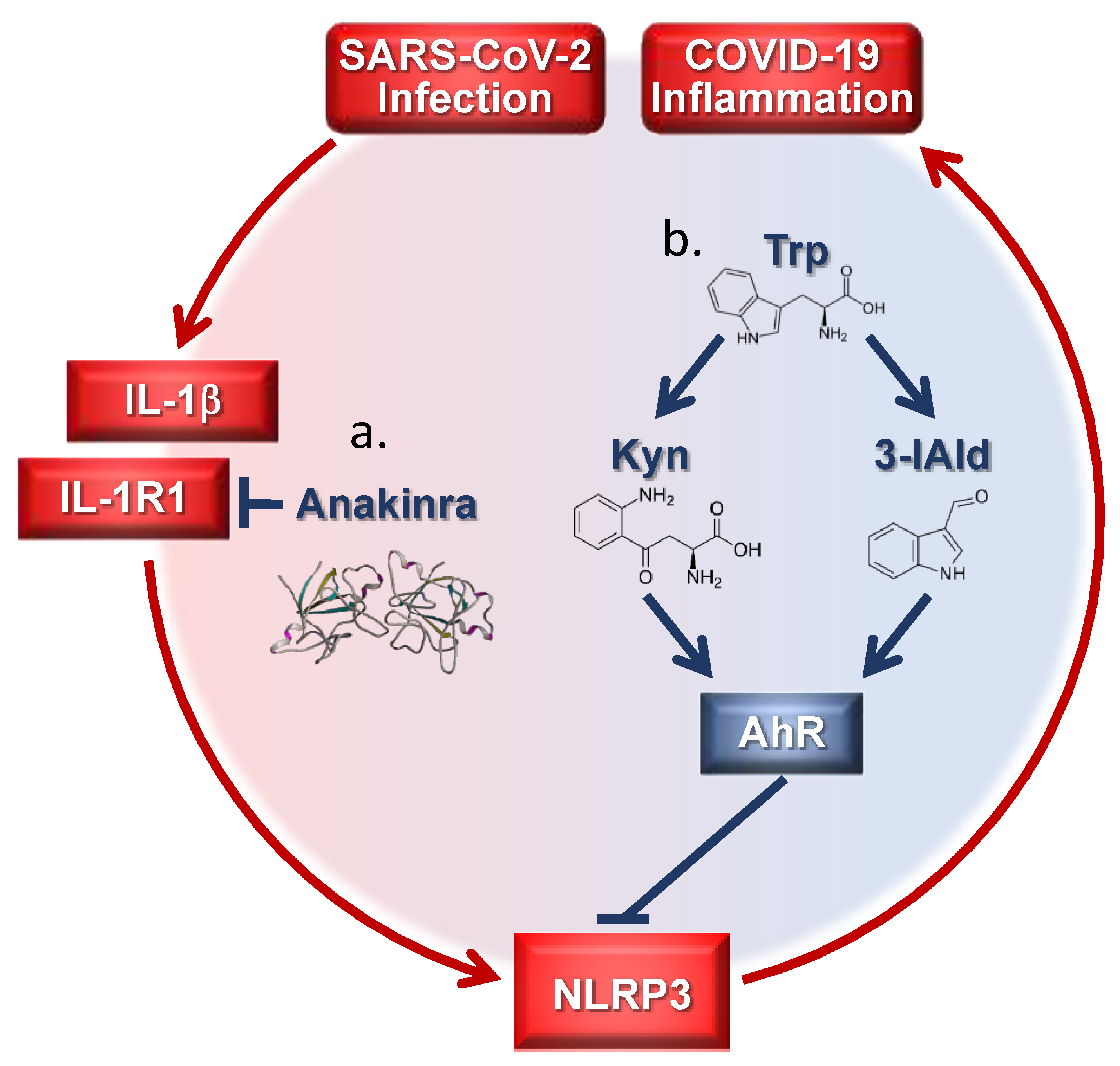
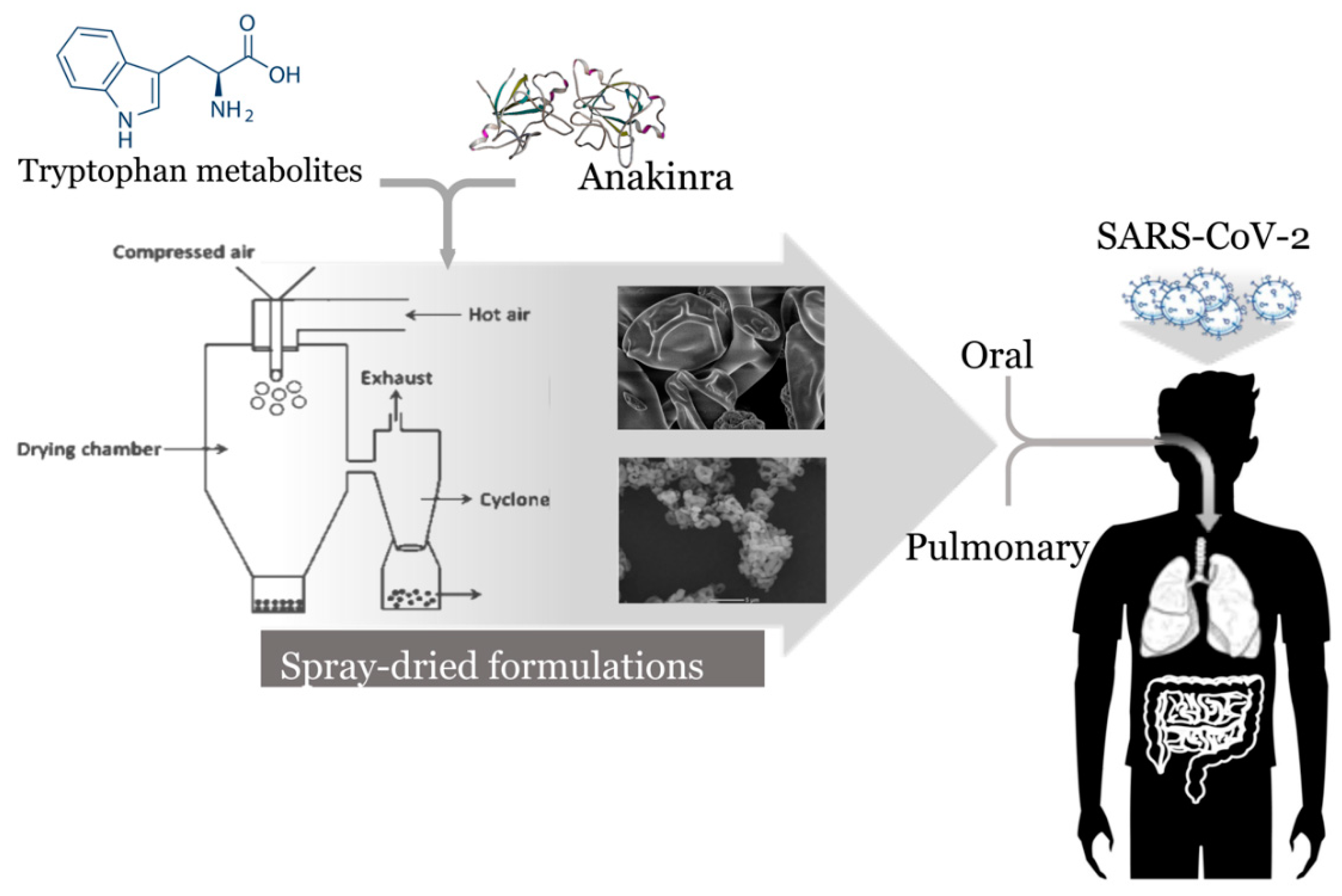
2. Current Anti-Inflammatory Approaches
3. The Inflammasome Pathway
4. The Xenobiotic Pathway
5. Concluding Remarks
Author Contributions
Funding
Conflicts of Interest
References
- Guan, W.J.; Ni, Z.Y.; Hu, Y.; Liang, W.H.; Ou, C.Q.; He, J.X.; Liu, L.; Shan, H.; Lei, C.L.; Hui, D.S.C.; et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef] [PubMed]
- Sohag, A.A.M.; Hannan, M.A.; Rahman, S.; Hossain, M.; Hasan, M.; Khan, M.K.; Khatun, A.; Dash, R.; Uddin, M.J. Revisiting potential druggable targets against SARS-CoV-2 and repurposing therapeutics under preclinical study and clinical trials: A comprehensive review. Drug Dev. Res. 2020. [Google Scholar] [CrossRef]
- Ojha, P.K.; Kar, S.; Krishna, J.G.; Roy, K.; Leszczynski, J. Therapeutics for COVID-19: From computation to practices-where we are, where we are heading to. Mol. Divers 2021, 25, 625–659. [Google Scholar] [CrossRef] [PubMed]
- Tejera, E.; Munteanu, C.R.; Lopez-Cortes, A.; Cabrera-Andrade, A.; Perez-Castillo, Y. Drugs Repurposing Using QSAR, Docking and Molecular Dynamics for Possible Inhibitors of the SARS-CoV-2 M(pro) Protease. Molecules 2020, 25, 5172. [Google Scholar] [CrossRef]
- Egieyeh, S.; Egieyeh, E.; Malan, S.; Christofells, A.; Fielding, B. Computational drug repurposing strategy predicted peptide-based drugs that can potentially inhibit the interaction of SARS-CoV-2 spike protein with its target (humanACE2). PLoS ONE 2021, 16, e0245258. [Google Scholar] [CrossRef] [PubMed]
- Wang, J. Fast Identification of Possible Drug Treatment of Coronavirus Disease-19 (COVID-19) through Computational Drug Repurposing Study. J. Chem. Inf. Model 2020, 60, 3277–3286. [Google Scholar] [CrossRef] [PubMed]
- Singh, T.U.; Parida, S.; Lingaraju, M.C.; Kesavan, M.; Kumar, D.; Singh, R.K. Drug repurposing approach to fight COVID-19. Pharmacol. Rep. 2020, 72, 1479–1508. [Google Scholar] [CrossRef]
- Chen, G.; Wu, D.; Guo, W.; Cao, Y.; Huang, D.; Wang, H.; Wang, T.; Zhang, X.; Chen, H.; Yu, H.; et al. Clinical and immunological features of severe and moderate coronavirus disease 2019. J. Clin. Invest. 2020, 130, 2620–2629. [Google Scholar] [CrossRef]
- Zhang, W.; Zhao, Y.; Zhang, F.; Wang, Q.; Li, T.; Liu, Z.; Wang, J.; Qin, Y.; Zhang, X.; Yan, X.; et al. The use of anti-inflammatory drugs in the treatment of people with severe coronavirus disease 2019 (COVID-19): The Perspectives of clinical immunologists from China. Clin. Immunol. 2020, 214, 108–393. [Google Scholar] [CrossRef]
- Felsenstein, S.; Herbert, J.A.; McNamara, P.S.; Hedrich, C.M. COVID-19: Immunology and treatment options. Clin. Immunol. 2020, 215, 108–448. [Google Scholar] [CrossRef]
- Ucciferri, C.; Vecchiet, J.; Falasca, K. Role of monoclonal antibody drugs in the treatment of COVID-19. World J. Clin. Cases 2020, 8, 4280–4285. [Google Scholar] [CrossRef] [PubMed]
- Romani, L.; Tomino, C.; Puccetti, P.; Garaci, E. Off-label therapy targeting pathogenic inflammation in COVID-19. Cell Death Discov. 2020, 6, 49. [Google Scholar] [CrossRef] [PubMed]
- Prescott, H.C.; Rice, T.W. Corticosteroids in COVID-19 ARDS: Evidence and Hope During the Pandemic. JAMA 2020, 324, 1292–1295. [Google Scholar] [CrossRef] [PubMed]
- Pascual Pareja, J.F.; Garcia-Caballero, R.; Soler Rangel, L.; Vazquez-Ronda, M.A.; Roa Franco, S.; Navarro Jimenez, G.; Moreno Palanco, M.A.; Gonzalez-Ruano, P.; Lopez-Menchaca, R.; Ruiz-Seco, P.; et al. Effectiveness of glucocorticoids in patients hospitalized for severe SARS-CoV-2 pneumonia. Med. Clin. 2021, 156, 221–228. [Google Scholar] [CrossRef]
- Andersen, K.M.; Mehta, H.B.; Palamuttam, N.; Ford, D.; Garibaldi, B.T.; Auwaerter, P.G.; Segal, J.; Alexander, G.C. Association Between Chronic Use of Immunosuppresive Drugs and Clinical Outcomes from Coronavirus Disease 2019 (COVID-19) Hospitalization: A Retrospective Cohort Study in a Large US Health System. Clin. Infect. Dis. 2021, ciaa1488, Online ahead of print. [Google Scholar] [CrossRef]
- D’Ardes, D.; Pontolillo, M.; Esposito, L.; Masciarelli, M.; Boccatonda, A.; Rossi, I.; Bucci, M.; Guagnano, M.T.; Ucciferri, C.; Santilli, F.; et al. Duration of COVID-19: Data from an Italian Cohort and Potential Role for Steroids. Microorganisms 2020, 8, 1327. [Google Scholar] [CrossRef]
- The WHO Rapid Evidence Appraisal for COVID-19 Therapies (REACT) Working Group; Sterne, J.A.C.; Murthy, S.; Diaz, J.V.; Slutsky, A.S.; Villar, J.; Angus, D.C.; Annane, D.; Azevedo, L.C.P.; Berwanger, O.; et al. Association Between Administration of Systemic Corticosteroids and Mortality Among Critically Ill Patients With COVID-19: A Meta-analysis. JAMA 2020, 324, 1330–1341. [Google Scholar] [CrossRef]
- Fang, L.; Karakiulakis, G.; Roth, M. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? Lancet Respir. Med. 2020, 8, e21. [Google Scholar] [CrossRef]
- Park, J.; Lee, S.H.; You, S.C.; Kim, J.; Yang, K. Non-steroidal anti-inflammatory agent use may not be associated with mortality of coronavirus disease 19. Sci. Rep. 2021, 11, 50–87. [Google Scholar] [CrossRef]
- Wong, A.Y.; MacKenna, B.; Morton, C.E.; Schultze, A.; Walker, A.J.; Bhaskaran, K.; Brown, J.P.; Rentsch, C.T.; Williamson, E.; Drysdale, H.; et al. Use of non-steroidal anti-inflammatory drugs and risk of death from COVID-19: An OpenSAFELY cohort analysis based on two cohorts. Ann. Rheum. Dis. 2021, 0, 1–9, Epub ahead of print: 21 January 2021. [Google Scholar] [CrossRef]
- Abu Esba, L.C.; Alqahtani, R.A.; Thomas, A.; Shamas, N.; Alswaidan, L.; Mardawi, G. Ibuprofen and NSAID Use in COVID-19 Infected Patients Is Not Associated with Worse Outcomes: A Prospective Cohort Study. Infect. Dis. Ther. 2021, 10, 253–268. [Google Scholar] [CrossRef]
- Kragholm, K.; Gerds, T.A.; Fosbol, E.; Andersen, M.P.; Phelps, M.; Butt, J.H.; Ostergaard, L.; Bang, C.N.; Pallisgaard, J.; Gislason, G.; et al. Association Between Prescribed Ibuprofen and Severe COVID-19 Infection: A Nationwide Register-Based Cohort Study. Clin. Transl. Sci. 2020, 13, 1103–1107. [Google Scholar] [CrossRef]
- Chandan, J.S.; Zemedikun, D.T.; Thayakaran, R.; Byne, N.; Dhalla, S.; Acosta-Mena, D.; Gokhale, K.M.; Thomas, T.; Sainsbury, C.; Subramanian, A.; et al. Non-steroidal anti-inflammatory drugs and susceptibility to COVID-19. Arthritis Rheumatol. 2020. Online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Rinott, E.; Kozer, E.; Shapira, Y.; Bar-Haim, A.; Youngster, I. Ibuprofen use and clinical outcomes in COVID-19 patients. Clin. Microbiol. Infect. 2020, 26, 1259.e5–1259.e7. [Google Scholar] [CrossRef] [PubMed]
- Kelleni, M.T. Early use of non-steroidal anti-inflammatory drugs in COVID-19 might reverse pathogenesis, prevent complications and improve clinical outcomes. Biomed. Pharmacother. 2021, 133, 110–982. [Google Scholar] [CrossRef] [PubMed]
- Prasher, P.; Sharma, M.; Gunupuru, R. Targeting cyclooxygenase enzyme for the adjuvant COVID-19 therapy. Drug Dev. Res. 2021. Epub ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Bejan, C.A.; Cahill, K.N.; Staso, P.J.; Choi, L.; Peterson, J.F.; Phillips, E.J. DrugWAS: Leveraging drug-wide association studies to facilitate drug repurposing for COVID-19. Med. Rxiv. 2021. 02.04.21251169. [Google Scholar] [CrossRef]
- Castro, V.M.; Ross, R.A.; McBride, S.M.; Perlis, R.H. Identifying common pharmacotherapies associated with reduced COVID-19 morbidity using electronic health records. Med. Rxiv. 2020. 04.11.20061994. [Google Scholar] [CrossRef]
- Horby, P.W.; Pessoa-Amorim, G.; Peto, L.; Brightling, C.E.; Sarkar, R.; Thomas, K.; Jeebun, V.; Ashish, A.; Tully, R.; Chadwick, D.; et al. Tocilizumab in patients admitted to hospital with COVID-19 (RECOVERY): Preliminary results of a randomised, controlled, open-label, platform trial. Med. Rxiv. 2021. 02.11.21249258. [Google Scholar] [CrossRef]
- Investigators, R.-C.; Gordon, A.C.; Mouncey, P.R.; Al-Beidh, F.; Rowan, K.M.; Nichol, A.D.; Arabi, Y.M.; Annane, D.; Beane, A.; van Bentum-Puijk, W.; et al. Interleukin-6 Receptor Antagonists in Critically Ill Patients with Covid-19. N. Engl. J. Med. 2021. Epub ahead of print. [Google Scholar] [CrossRef]
- Chiu, L.; Chow, R.; Chiu, N.; Lo, C.-H.; Aggarwal, R.; Lee, J.; Choi, Y.-G.; Lam, H.; Prsic, E.H.; Shin, H.J. Colchicine use in patients with COVID-19: A systematic review and meta-analysis. Med. Rxiv. 2021. 02.02.21250960. [Google Scholar] [CrossRef]
- Luo, W.; Li, Y.X.; Jiang, L.J.; Chen, Q.; Wang, T.; Ye, D.W. Targeting JAK-STAT Signaling to Control Cytokine Release Syndrome in COVID-19. Trends Pharmacol. Sci. 2020, 41, 531–543. [Google Scholar] [CrossRef]
- Kalil, A.C.; Patterson, T.F.; Mehta, A.K.; Tomashek, K.M.; Wolfe, C.R.; Ghazaryan, V.; Marconi, V.C.; Ruiz-Palacios, G.M.; Hsieh, L.; Kline, S.; et al. Baricitinib plus Remdesivir for Hospitalized Adults with Covid-19. N. Engl. J. Med. 2021, 384, 795–807. [Google Scholar] [CrossRef]
- Gordon, D.E.; Jang, G.M.; Bouhaddou, M.; Xu, J.; Obernier, K.; White, K.M.; O’Meara, M.J.; Rezelj, V.V.; Guo, J.Z.; Swaney, D.L.; et al. A SARS-CoV-2 protein interaction map reveals targets for drug repurposing. Nature 2020, 583, 459–468. [Google Scholar] [CrossRef]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef]
- Qin, C.; Zhou, L.; Hu, Z.; Zhang, S.; Yang, S.; Tao, Y.; Xie, C.; Ma, K.; Shang, K.; Wang, W.; et al. Dysregulation of Immune Response in Patients with Coronavirus 2019 (COVID-19) in Wuhan, China. Clin. Infect. Dis. 2020, 71, 762–768. [Google Scholar] [CrossRef]
- Song, P.; Li, W.; Xie, J.; Hou, Y.; You, C. Cytokine storm induced by SARS-CoV-2. Clin. Chim. Acta 2020, 509, 280–287. [Google Scholar] [CrossRef]
- Jamilloux, Y.; Henry, T.; Belot, A.; Viel, S.; Fauter, M.; El Jammal, T.; Walzer, T.; Francois, B.; Seve, P. Should we stimulate or suppress immune responses in COVID-19? Cytokine and anti-cytokine interventions. Autoimmun. Rev. 2020, 19, 102–567. [Google Scholar] [CrossRef]
- Cavalli, G.; de Luca, G.; Campochiaro, C.; Della-Torre, E.; Ripa, M.; Canetti, D.; Oltolini, C.; Castiglioni, B.; Tassan Din, C.; Boffini, N.; et al. Interleukin-1 blockade with high-dose anakinra in patients with COVID-19, acute respiratory distress syndrome, and hyperinflammation: A retrospective cohort study. Lancet Rheumatol. 2020, 2, 325–331. [Google Scholar] [CrossRef]
- Cauchois, R.; Koubi, M.; Delarbre, D.; Manet, C.; Carvelli, J.; Blasco, V.B.; Jean, R.; Fouche, L.; Bornet, C.; Pauly, V.; et al. Early IL-1 receptor blockade in severe inflammatory respiratory failure complicating COVID-19. Proc. Natl. Acad. Sci. USA 2020, 117, 18951–18953. [Google Scholar] [CrossRef] [PubMed]
- Mehta, P.; Cron, R.Q.; Hartwell, J.; Manson, J.J.; Tattersall, R. Intravenous anakinra for cytokine storm syndromes—Authors’ reply. Lancet Rheumatol. 2020, 2, 522–523. [Google Scholar] [CrossRef]
- Iglesias-Julian, E.; Lopez-Veloso, M.; de-la-Torre-Ferrera, N.; Barraza-Vengoechea, J.C.; Delgado-Lopez, P.D.; Colazo-Burlato, M.; Ubeira-Iglesias, M.; Montero-Baladia, M.; Lorenzo-Martin, A.; Minguito-de-la-Iglesia, J.; et al. High dose subcutaneous Anakinra to treat acute respiratory distress syndrome secondary to cytokine storm syndrome among severely ill COVID-19 patients. J. Autoimmun. 2020, 115, 102–537. [Google Scholar] [CrossRef]
- Huet, T.; Beaussier, H.; Voisin, O.; Jouveshomme, S.; Dauriat, G.; Lazareth, I.; Sacco, E.; Naccache, J.M.; Bezie, Y.; Laplanche, S.; et al. Anakinra for severe forms of COVID-19: A cohort study. Lancet Rheumatol. 2020, 2, 393–400. [Google Scholar] [CrossRef]
- Dimopoulos, G.; de Mast, Q.; Markou, N.; Theodorakopoulou, M.; Komnos, A.; Mouktaroudi, M.; Netea, M.G.; Spyridopoulos, T.; Verheggen, R.J.; Hoogerwerf, J.; et al. Favorable Anakinra Responses in Severe Covid-19 Patients with Secondary Hemophagocytic Lymphohistiocytosis. Cell Host Microbe 2020, 28, 117–123. [Google Scholar] [CrossRef]
- Scambler, T.; Holbrook, J.; Savic, S.; McDermott, M.F.; Peckham, D. Autoinflammatory disease in the lung. Immunology 2018, 154, 563–573. [Google Scholar] [CrossRef] [PubMed]
- Schmitz, N.; Kurrer, M.; Bachmann, M.F.; Kopf, M. Interleukin-1 is responsible for acute lung immunopathology but increases survival of respiratory influenza virus infection. J. Virol. 2005, 79, 6441–6448. [Google Scholar] [CrossRef] [PubMed]
- Van den Berg, D.F.; Te Velde, A.A. Severe COVID-19: NLRP3 Inflammasome Dysregulated. Front Immunol. 2020, 11, 1580. [Google Scholar] [CrossRef] [PubMed]
- Freeman, T.L.; Swartz, T.H. Targeting the NLRP3 Inflammasome in Severe COVID-19. Front Immunol. 2020, 11, 1518. [Google Scholar] [CrossRef]
- Yap, J.K.Y.; Moriyama, M.; Iwasaki, A. Inflammasomes and Pyroptosis as Therapeutic Targets for COVID-19. J. Immunol. 2020, 205, 307–312. [Google Scholar] [CrossRef] [PubMed]
- Ahn, M.; Anderson, D.E.; Zhang, Q.; Tan, C.W.; Lim, B.L.; Luko, K.; Wen, M.; Chia, W.N.; Mani, S.; Wang, L.C.; et al. Dampened NLRP3-mediated inflammation in bats and implications for a special viral reservoir host. Nat. Microbiol. 2019, 4, 789–799. [Google Scholar] [CrossRef] [PubMed]
- Cavalli, G.; Dinarello, C.A. Corrigendum: Anakinra Therapy for Non-cancer Inflammatory Diseases. Front Pharmacol. 2019, 10, 148. [Google Scholar] [CrossRef]
- Dinarello, C.A. The IL-1 family of cytokines and receptors in rheumatic diseases. Nat. Rev. Rheumatol. 2019, 15, 612–632. [Google Scholar] [CrossRef]
- Iannitti, R.G.; Napolioni, V.; Oikonomou, V.; de Luca, A.; Galosi, C.; Pariano, M.; Massi-Benedetti, C.; Borghi, M.; Puccetti, M.; Lucidi, V.; et al. IL-1 receptor antagonist ameliorates inflammasome-dependent inflammation in murine and human cystic fibrosis. Nat. Commun. 2016, 7, 10791. [Google Scholar] [CrossRef] [PubMed]
- Ucciferri, C.; Auricchio, A.; di Nicola, M.; Potere, N.; Abbate, A.; Cipollone, F.; Vecchiet, J.; Falasca, K. Canakinumab in a subgroup of patients with COVID-19. Lancet Rheumatol. 2020, 2, 457–458. [Google Scholar] [CrossRef]
- Katia, F.; Myriam, D.P.; Ucciferri, C.; Auricchio, A.; di Nicola, M.; Marchioni, M.; Eleonora, C.; Emanuela, S.; Cipollone, F.; Vecchiet, J. Efficacy of canakinumab in mild or severe COVID-19 pneumonia. Immun. Inflamm. Dis. 2021. Online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Generali, D.; Bosio, G.; Malberti, F.; Cuzzoli, A.; Testa, S.; Romanini, L.; Fioravanti, A.; Morandini, A.; Pianta, L.; Giannotti, G.; et al. Canakinumab as treatment for COVID-19-related pneumonia: A prospective case-control study. Internation. J. Infect. Dis. IJID Off. Publ. Internation. Soc. Infect. Dis. 2020, 104, 433–440. [Google Scholar] [CrossRef]
- Wichers, M.C.; Koek, G.H.; Robaeys, G.; Verkerk, R.; Scharpe, S.; Maes, M. IDO and interferon-alpha-induced depressive symptoms: A shift in hypothesis from tryptophan depletion to neurotoxicity. Mol. Psychiatry 2005, 10, 538–544. [Google Scholar] [CrossRef] [PubMed]
- Badawy, A.A. Kynurenine Pathway of Tryptophan Metabolism: Regulatory and Functional Aspects. Int. J. Tryptophan Res. 2017, 10, 1178646917691938. [Google Scholar] [CrossRef] [PubMed]
- Comai, S.; Bertazzo, A.; Brughera, M.; Crotti, S. Tryptophan in health and disease. Adv. Clin. Chem. 2020, 95, 165–218. [Google Scholar] [CrossRef] [PubMed]
- Taleb, S. Tryptophan Dietary Impacts Gut Barrier and Metabolic Diseases. Front Immunol. 2019, 10, 2113. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.M.; Park, H.Y.; Suh, Y.S.; Yoon, E.H.; Kim, J.; Jang, W.H.; Lee, W.S.; Park, S.G.; Choi, I.W.; Choi, I.; et al. Inhibition of acute lethal pulmonary inflammation by the IDO-AhR pathway. Proc. Natl. Acad. Sci. USA 2017, 114, 5881–5890. [Google Scholar] [CrossRef] [PubMed]
- Puccetti, P.; Grohmann, U. IDO and regulatory T cells: A role for reverse signalling and non-canonical NF-kappaB activation. Nat. Rev. Immunol. 2007, 7, 817–823. [Google Scholar] [CrossRef] [PubMed]
- Thomas, T.; Stefanoni, D.; Reisz, J.A.; Nemkov, T.; Bertolone, L.; Francis, R.O.; Hudson, K.E.; Zimring, J.C.; Hansen, K.C.; Hod, E.A.; et al. COVID-19 infection alters kynurenine and fatty acid metabolism, correlating with IL-6 levels and renal status. JCI Insight 2020, 5, e140327. [Google Scholar] [CrossRef] [PubMed]
- Rothhammer, V.; Quintana, F.J. The aryl hydrocarbon receptor: An environmental sensor integrating immune responses in health and disease. Nat. Rev. Immunol. 2019, 19, 184–197. [Google Scholar] [CrossRef] [PubMed]
- Stockinger, B.; di Meglio, P.; Gialitakis, M.; Duarte, J.H. The aryl hydrocarbon receptor: Multitasking in the immune system. Annu. Rev. Immunol. 2014, 32, 403–432. [Google Scholar] [CrossRef]
- Puccetti, M.; Paolicelli, G.; Oikonomou, V.; de Luca, A.; Renga, G.; Borghi, M.; Pariano, M.; Stincardini, C.; Scaringi, L.; Giovagnoli, S.; et al. Towards Targeting the Aryl Hydrocarbon Receptor in Cystic Fibrosis. Mediators Inflamm. 2018, 2018, 1601486. [Google Scholar] [CrossRef]
- Moura-Alves, P.; Fae, K.; Houthuys, E.; Dorhoi, A.; Kreuchwig, A.; Furkert, J.; Barison, N.; Diehl, A.; Munder, A.; Constant, P.; et al. AhR sensing of bacterial pigments regulates antibacterial defence. Nature 2014, 512, 387–392. [Google Scholar] [CrossRef]
- Grunewald, M.E.; Shaban, M.G.; Mackin, S.R.; Fehr, A.R.; Perlman, S. Murine Coronavirus Infection Activates the Aryl Hydrocarbon Receptor in an Indoleamine 2,3-Dioxygenase-Independent Manner, Contributing to Cytokine Modulation and Proviral TCDD-Inducible-PARP Expression. J. Virol. 2020, 94, e01743-19. [Google Scholar] [CrossRef]
- Huai, W.; Zhao, R.; Song, H.; Zhao, J.; Zhang, L.; Zhang, L.; Gao, C.; Han, L.; Zhao, W. Aryl hydrocarbon receptor negatively regulates NLRP3 inflammasome activity by inhibiting NLRP3 transcription. Nat. Commun. 2014, 5, 4738. [Google Scholar] [CrossRef]
- Agus, A.; Planchais, J.; Sokol, H. Gut Microbiota Regulation of Tryptophan Metabolism in Health and Disease. Cell Host Microbe 2018, 23, 716–724. [Google Scholar] [CrossRef]
- Emami, F.; Vatanara, A.; Park, E.J.; Na, D.H. Drying Technologies for the Stability and Bioavailability of Biopharmaceuticals. Pharmaceutics 2018, 10, 131. [Google Scholar] [CrossRef] [PubMed]
- Rosiere, R.; Berghmans, T.; de Vuyst, P.; Amighi, K.; Wauthoz, N. The Position of Inhaled Chemotherapy in the Care of Patients with Lung Tumors: Clinical Feasibility and Indications According to Recent Pharmaceutical Progresses. Cancers 2019, 11, 329. [Google Scholar] [CrossRef] [PubMed]
- Fellner, R.C.; Terryah, S.T.; Tarran, R. Inhaled protein/peptide-based therapies for respiratory disease. Mol. Cell Pediatr. 2016, 3, 16. [Google Scholar] [CrossRef] [PubMed]
- Horava, S.D.; Moy, K.J.; Peppas, N.A. Biodegradable hydrophilic carriers for the oral delivery of hematological factor IX for hemophilia B treatment. Int. J. Pharm. 2016, 514, 220–228. [Google Scholar] [CrossRef] [PubMed]
- European Medicines Agency. Assessment Report: Kineret; Procedure No. EMEA/H/C/000363/X/0042; European Medicines Agency: Amsterdam, The Netherlands, 2013. [Google Scholar]
- Kowalewski, J.; Ray, A. Predicting novel drugs for SARS-CoV-2 using machine learning from a >10 million chemical space. Heliyon 2020, 6, e04639. [Google Scholar] [CrossRef]
- Hathout, R.M.; Abdelhamid, S.G.; Metwally, A.A. Chloroquine and hydroxychloroquine for combating COVID-19: Investigating efficacy and hypothesizing new formulations using Bio/chemoinformatics tools. Inform. Med. Unlocked 2020, 21, 100–446. [Google Scholar] [CrossRef]
- Puccetti, M.; Giovagnoli, S.; Zelante, T.; Romani, L.; Ricci, M. Development of Novel Indole-3-Aldehyde-Loaded Gastro-Resistant Spray-Dried Microparticles for Postbiotic Small Intestine Local Delivery. J. Pharm. Sci. 2018, 107, 2341–2353. [Google Scholar] [CrossRef]
- Tabas, I.; Glass, C.K. Anti-inflammatory therapy in chronic disease: Challenges and opportunities. Science 2013, 339, 166–172. [Google Scholar] [CrossRef]
- Sahakijpijarn, S.; Moon, C.; Koleng, J.J.; Christensen, D.J.; Williams Iii, R.O. Development of Remdesivir as a Dry Powder for Inhalation by Thin Film Freezing. Pharmaceutics 2020, 12, 1002. [Google Scholar] [CrossRef]
| Location | Study Title | Development Stage |
|---|---|---|
| U.S. | Safety, tolerability and pharmacokinetics of inhaled nanoparticle formulation of remdesivir (GS-5734) and NA-831 (NEUROSIVIR) | Phase I |
| Switzerland | Inhaled aviptadil for the prevention of COVID-19 related ARDS | Phase I |
| U.S. | An experiment to evaluate the safety of agenT-797 in COVID-19 patients with severe difficulty breathing. | Phase I |
| U.S. | A study to evaluate the safety, tolerability and pharmacokinetics of orally inhaled aerosolized hydroxychloroquine sulfate in healthy adult volunteers | Phase I |
| U.S. | Study in participants with early stage coronavirus disease 2019 (COVID-19) to evaluate the safety, efficacy, and pharmacokinetics of remdesivir administered by inhalation | Phase I/II |
| France | Efficacy of captopril in COVID-19 patients with severe acute respiratory syndrome (SARS) cov-2 pneumonia (CAPTOCOVID) | Phase II |
| Egypt | Efficacy of aerosol combination therapy of 13 cis retinoic acid and captopril for treating COVID-19 patients via indirect inhibition of transmembrane protease, serine 2 (TMPRSS2) | Phase II |
| U.K. | Steroids in COVID-19 study (STOIC) | Phase II |
| U.K. | Inhaled anti-viral (SNG001) for SARS-cov-2 (COVID-19) infection | Phase II |
| Korea | A trial of ciclesonide in adults with mild-to-moderate COVID-19 | Phase II |
| Egypt | Efficacy and safety of drug combination therapy of isotretinoin and some antifungal drugs as a potential aerosol therapy for COVID-19: an innovative therapeutic approach COVID-19. | Phase II |
| Qatar | Inhaled iloprost for suspected COVID-19 respiratory failure (ILOCOVID) | Phase II |
| U.K., Romania, Ukraine, Moldova | TD-0903 for ALI associated with COVID-19 | Phase II |
| Egypt | Aerosol combination therapy of all-trans retinoic acid and isotretinoin as a novel treatment for inducing neutralizing antibodies in COVID -19 infected patients better than vaccine: an innovative treatment (Antibodies) | Phase II |
| Canada | Inhaled ciclesonide for outpatients with COVID-19 (CONTAIN) | Phase II/III |
| Iran | Evaluation of efficacy of levamisole and formoterol+budesonide in treatment of COVID-19 | Phase II/III |
| Russia | An open randomized study of dalargin effectiveness in patients with severe and critical manifestations of SARS-COVID-19 | Phase III |
| U.S. | A study of the safety and efficacy of ciclesonide in the treatment of non-hospitalized COVID-19 patients | Phase III |
| U.S. | Dornase alfa for ARDS in patients with SARS-cov-2 (DORNASESARS2) | Phase III |
| Spain | Inhaled corticosteroid treatment of COVID19 patients with pneumonia | Phase IV |
| Argentina | Nebulized heparin in severe acute respiratory syndrome COVID-19 (NEBUHEPA) | Phase IV |
| China | Evaluation of Ganovo (danoprevir) combined with ritonavir in the treatment of SARS-cov-2 infection | Phase IV |
| U.S. | Valproate alone or in combination with quetiapine for severe COVID-19 pneumonia with agitated delirium | Phase IV |
| Belgium | Sargramostim in patients with acute hypoxic respiratory failure due to COVID-19 (SARPAC) | Phase IV |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Puccetti, M.; Costantini, C.; Ricci, M.; Giovagnoli, S. Tackling Immune Pathogenesis of COVID-19 through Molecular Pharmaceutics. Pharmaceutics 2021, 13, 494. https://doi.org/10.3390/pharmaceutics13040494
Puccetti M, Costantini C, Ricci M, Giovagnoli S. Tackling Immune Pathogenesis of COVID-19 through Molecular Pharmaceutics. Pharmaceutics. 2021; 13(4):494. https://doi.org/10.3390/pharmaceutics13040494
Chicago/Turabian StylePuccetti, Matteo, Claudio Costantini, Maurizio Ricci, and Stefano Giovagnoli. 2021. "Tackling Immune Pathogenesis of COVID-19 through Molecular Pharmaceutics" Pharmaceutics 13, no. 4: 494. https://doi.org/10.3390/pharmaceutics13040494
APA StylePuccetti, M., Costantini, C., Ricci, M., & Giovagnoli, S. (2021). Tackling Immune Pathogenesis of COVID-19 through Molecular Pharmaceutics. Pharmaceutics, 13(4), 494. https://doi.org/10.3390/pharmaceutics13040494







