Population Pharmacokinetics of Levetiracetam and Dosing Evaluation in Critically Ill Patients with Normal or Augmented Renal Function
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Patient Population
2.2. Drug Administration, Sampling Procedure and Analytical Method
2.3. Noncompartmental Analysis
2.4. Pharmacometric Modelling
2.5. Final Model Evaluation
2.6. Dosing Simulations
3. Results
3.1. Patient Demographics
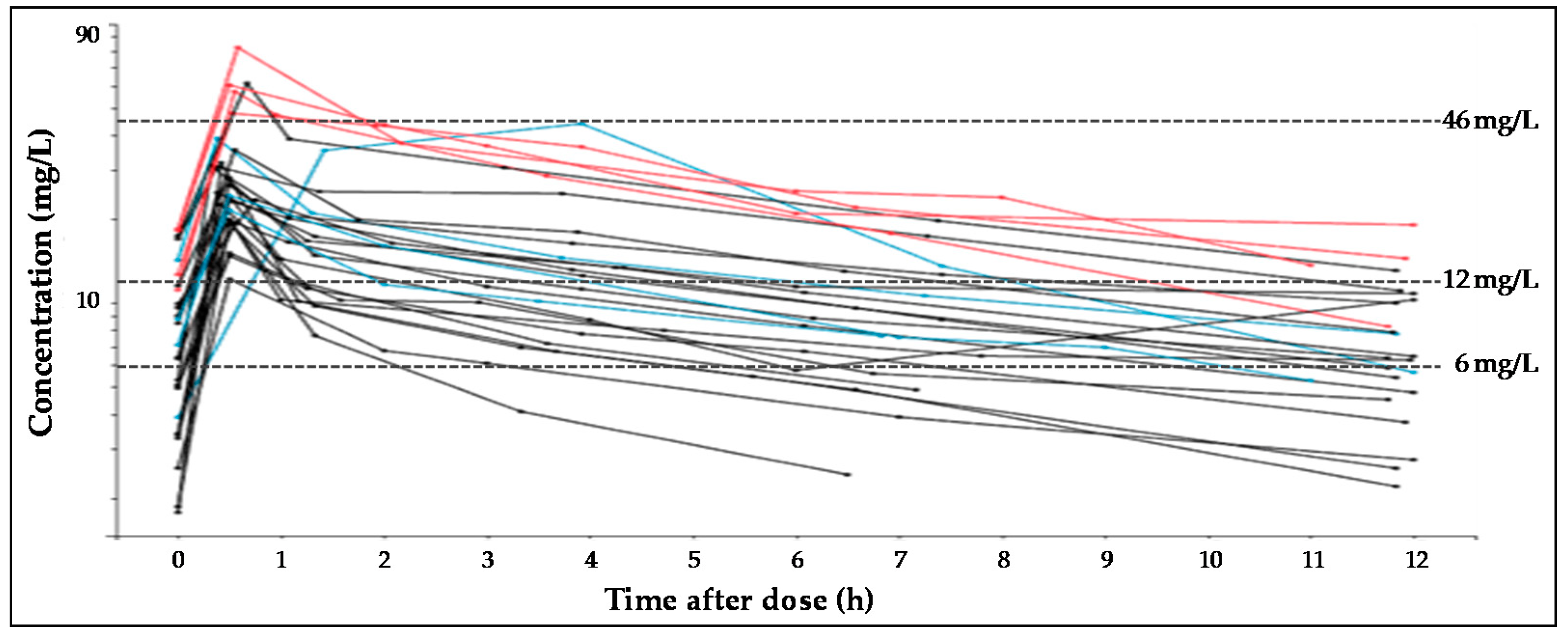
3.2. Noncompartmental Analysis
3.3. Population Pharmacokinetic Modelling
3.4. Dosing Simulations
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- European Medicines Agency. Keppra 100 mg/mL Concentrate for Solution for Infusion-Summary of Product Characteristics (SPC). 2021. Available online: https://www.ema.europa.eu/en/documents/product-information/keppra-epar-product-information_en.pdf (accessed on 7 April 2021).
- Glauser, T.; Shinnar, S.; Gloss, D.; Alldredge, B.; Arya, R.; Bainbridge, J.; Bare, M.; Bleck, T.; Dodson, W.E.; Garrity, L.; et al. Evidence-based guideline: Treatment of convulsive status epilepticus in children and adults: Report of the Guideline Committee of the American Epilepsy Society. Epilepsy Curr. 2016, 16, 48–61. [Google Scholar] [CrossRef]
- Szaflarski, J.P.; Sangha, K.S.; Lindsell, C.J.; Shutter, L.A. Prospective, randomized, single-blinded comparative trial of intravenous levetiracetam versus phenytoin for seizure prophylaxis. Neurocrit. Care 2010, 12, 165–172. [Google Scholar] [CrossRef] [PubMed]
- Patsalos, P.N.; Spencer, E.P.; Berry, D.J. Therapeutic drug monitoring of antiepileptic drugs in epilepsy: A 2018 update. Drug Monit. 2018, 40, 526–548. [Google Scholar] [CrossRef]
- Patsalos, P.N. Clinical pharmacokinetics of levetiracetam. Clin. Pharmacokinet. 2004, 43, 707–724. [Google Scholar] [CrossRef] [PubMed]
- Patsalos, P.N.; Berry, D.J.; Bourgeois, B.F.D.; Cloyd, J.C.; Glauser, T.A.; Johannessen, S.I.; Leppik, I.E.; Tomson, T.; Perucca, E. Antiepileptic drug-best practice guidelines for therapeutic drug monitoring, ILAE commission on therapeutic strategies. Epilepsia 2008, 49, 1239–1276. [Google Scholar] [CrossRef] [PubMed]
- Johannessen, S.I.; Battino, D.; Berry, D.J.; Bialer, M.; Krämer, G.; Tomson, T.; Patsalos, P.N. Therapeutic drug monitoring of the newer antiepileptic drugs. Ther. Drug Monit. 2003, 25, 347–363. [Google Scholar] [CrossRef]
- Sourbron, J.; Chan, H.; van der Heijdenb, E.A.M.; Klarenbeek, P.; Wijnen, B.F.M.; de Haan, G.-J.; van der Kuy, H.; Evers, S.; Majoie, M. Review on the relevance of therapeutic drug monitoring of levetiracetam. Seizure 2018, 62, 131–135. [Google Scholar] [CrossRef]
- Jarvie, D.; Mahmoud, S.H. Therapeutic Drug Monitoring of Levetiracetam in Select Populations. J. Pharm. Pharm. Sci. 2018, 21, 149–176. [Google Scholar] [CrossRef]
- Bilbao-Meseguer, I.; Rodríguez-Gascón, A.; Barrasa, H.; Isla, A.; Solinis, M.A. Augmented Renal Clearance in Critically Ill Patients: A Systematic Review. Clin. Pharmacokinet. 2018, 57, 1107–1121. [Google Scholar] [CrossRef]
- Cook, A.M.; Hatton-Kolpek, J. Augmented Renal Clearance. Pharmacotherapy 2019, 39, 346–354. [Google Scholar] [CrossRef]
- Atkinson, A.J., Jr. Augmented renal clearance. Transl. Clin. Pharmacol. 2018, 26, 111–114. [Google Scholar] [CrossRef][Green Version]
- Mahmoud, S.H.; Shen, C. Augmented Renal Clearance in Critical Illness: An Important Consideration in Drug Dosing. Pharmaceutics 2017, 9, 36. [Google Scholar] [CrossRef]
- Jamal, J.A.; Roger, C.; Roberts, J.A. Understanding the impact of pathophysiological alterations during critical illness on drug pharmacokinetics. Anaesth. Crit. Care Pain Med. 2018, 37, 515–517. [Google Scholar] [CrossRef]
- Campassi, M.L.; Gonzalez, M.C.; Masevicius, F.D.; Vazquez, A.R.; Moseinco, M.; Navarro, N.C.; Previgliano, L.; Rubatto, N.P.; Benites, M.H.; Estenssoro, E.; et al. Augmented renal clearance in critically ill patients: Incidence, associated factors and effects on vancomycin treatment. Rev. Bras. Ter. Intensiva 2014, 26, 13–20. [Google Scholar] [CrossRef]
- Carlier, M.; Carrette, S.; Roberts, J.A.; Stove, V.; Verstraete, A.; Hoste, E.; Depuydt, P.; Decruyenaere, J.; Lipman, J.; Wallis, S.C. Meropenem and piperacillin/tazobactam prescribing in critically ill patients: Does augmented renal clearance affect pharmacokinetic/pharmacodynamic target attainment when extended infusions are used? Crit. Care 2013, 17, R84. [Google Scholar] [CrossRef]
- Udy, A.A.; Varghese, J.M.; Altukroni, M.; Briscoe, S.; McWhinney, B.C.; Ungerer, J.P.; Lipman, J.; Roberts, J.A. Subtherapeutic initial beta-lactam concentrations in select critically Ill patients: Association between augmented renal clearance and low trough drug concentrations. Chest 2012, 142, 30–39. [Google Scholar] [CrossRef] [PubMed]
- Baptista, J.P.; Sousa, E.; Martins, P.J.; Pimentel, J.M. Augmented renal clearance in septic patients and implications for vancomycin optimisation. Int. J. Antimicrob. Agents 2012, 39, 420–423. [Google Scholar] [CrossRef] [PubMed]
- Barrasa, H.; Soraluce, A.; Usón, E.; Sainz, J.; Martín, A.; Sánchez-Izquierdo, J.Á.; Maynar, J.; Rodríguez-Gascón, A.; Isla, A. Impact of augmented renal clearance on the pharmacokinetics of linezolid: Advantages of continuous infusion from a pharmacokinetic/pharmacodynamic perspective. Int. J. Infect. Dis. 2020, 93, 329–338. [Google Scholar] [CrossRef] [PubMed]
- Cook, A.M.; Arora, S.; Davis, J.; Pittman, T. Augmented Renal Clearance of Vancomycin and Levetiracetam in a Traumatic Brain Injury Patient. Neurocrit. Care 2013, 19, 210–214. [Google Scholar] [CrossRef] [PubMed]
- Spencer, D.D.; Jacobi, J.; Juenke, J.M.; Fleck, J.D.; Kays, M.B. Steady-state pharmacokinetics of intravenous levetiracetam in neurocritical care patients. Pharmacotherapy 2011, 31, 934–941. [Google Scholar] [CrossRef]
- Sime, F.B.; Roberts, J.A.; Jeffree, R.L.; Pandey, S.; Adiraju, S.; Livermore, A. Population Pharmacokinetics of Levetiracetam in Patients with Traumatic Brain Injury and Subarachnoid Hemorrhage Exhibiting Augmented Renal Clearance. Clin. Pharmacokinet. 2021. [Google Scholar] [CrossRef] [PubMed]
- Ong, C.L.J.; Goh, P.S.J.; Teo, M.M.; Lim, T.P.; Goh, K.K.K.; Ang, X.Y.; Lim, L.J.K.; Jamaludin, N.H.B.; Ang, B.T.; Kwa, L.H.A. Pharmacokinetics of levetiracetam in neurosurgical ICU patients. J. Crit. Care 2021, 64, 255–261. [Google Scholar] [CrossRef] [PubMed]
- Hernandez-Mitre, M.P.; Medellín-Garibay, S.E.; Rodriguez-Leyva, I.; Rodriguez-Pinal, C.J.; Zarazúa, S.; Jung-Cook, H.H.; Roberts, J.A.; Romano-Moreno, S.; Milán-Segovia, R.D.C. Population pharmacokinetics and dosing recommendations of levetiracetam in adult and elderly patients with epilepsy. J. Pharm. Sci. 2020, 109, 2070–2078. [Google Scholar] [CrossRef] [PubMed]
- Methaneethorn, J.; Leelakanok, N. Population Pharmacokinetics of Levetiracetam: A Systematic Review. Curr. Clin. Pharmacol. 2021. Epub Ahead of Print. [Google Scholar] [CrossRef] [PubMed]
- Reimers, A.; Berg, J.A.; Burns, M.L.; Brodtkorb, E.; Johannessen, S.I.; Landmark, C.J. Reference ranges for antiepileptic drugs revisited: A practical approach to establish national guidelines. Drug Des. Dev. Ther. 2018, 12, 271–280. [Google Scholar] [CrossRef] [PubMed]
- Roberts, J.A.; Lipman, J. Optimal doripenem dosing simulations in critically ill nosocomial pneumonia patients with obesity, augmented renal clearance, and decreased bacterial susceptibility. Crit. Care Med. 2013, 41, 489–495. [Google Scholar] [CrossRef]
- Food and Drug Administration. KEPPRA® (Levetiracetam) Injection, for Intravenous Use-Summary of Product Characteristics. 2020. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/021872s029lbl.pdf (accessed on 7 May 2021).




| Covariate | N (%) | Median (Range) |
|---|---|---|
| Sex: | ||
| ● Male | 18 (67) | - |
| ● Female | 9 (33) | - |
| ARC (CrCl > 130 mL/min): | ||
| ● Yes | 10 (37) | |
| ● No | 17 (63) | |
| Diagnostic: | ||
| ● Haemorrhagic strokes | 10 (37) | - |
| ● Trauma | 8 (30) | - |
| ● Others | 9 (33) | - |
| Age (years) | - | 60 (23–81) |
| Weight (kg) | - | 80 (58–115) |
| Height (cm) | - | 168 (148–189) |
| BSA (m2) 1 | - | 1.9 (1.59–2.33) |
| APACHE II | - | 18 (5–35) |
| CrCl (mL/min) 2 | - | 117 (54–239) |
| Glucose (mg/dL) | - | 142 (91–337) |
| Albumin (g/dL) | - | 3.4 (2.1–3.9) |
| Total bilirubin (mg/dL) | - | 0.6 (0.2–2.1) |
| Hemoglobin (g/dL) | - | 11.6 (6.7–14.5) |
| Leukocytes (109/L) | - | 10.4 (3–24.6) |
| Cmax (mg/L) | Cmax/D (L−1) | AUC12 (mg·h/L) | AUC12/D (h/L) | t1/2(h) | CL (L/h) | Vz (L) | |
|---|---|---|---|---|---|---|---|
| No ARC | 36.36 (17.93) | 0.053 (0.032) | 186.49 (97.79) | 0.267 (0.118) | 8.86 (6.13) | 4.28 (1.40) | 54.41 (42.79) |
| ARC | 24.25 (12.41) | 0.036 (0.011) * | 121.05 (66.08) | 0.182 (0.081) | 7.25 (4.11) | 6.51 (2.65) * | 61.09 (25.07) |
| Parameter | Base Model Estimate (RSE (%)) | Final Model Estimate (RSE (%)) | Bootstrap Median (95% CI) |
|---|---|---|---|
| CL (L/h) = θnr + (CrCl/120)θr | 4.6 (8) | - | |
| θnr | - | 3.5 (9) | 3.5 (2.8–4.1) |
| θr | 2.5 (17) | 2.5 (0.9–3.9) | |
| V1 (L) | 20.8 (18) | 20.7 (18) | 20.8 (13.4–27.7) |
| Q (L/h) | 31.4 (21) | 31.9 (22) | 30.9 (22.5–47.8) |
| V2 (L) | 34.1 (14) | 33.5 (13) | 34.2 (19.9–45.4) |
| IIV_CL (%) | 38.3 (19) | 32.7 (21) | 30.7 (20.2–48.3) |
| IIV_V1 (%) | 54.4 (29) | 56.1 (29) | 58.0 (22.6–114.0) |
| RE_proportional (%) | 22.3 (15) | 22.3 (15) | 21.5 (15.7–27.7) |
| CrCl (mL/min) | Dose (mg) | Perfusion Duration (min) | Daily Dose (mg) | Probability of Cmin (%) | ||
|---|---|---|---|---|---|---|
| >6 mg/L | >12 mg/L | >46 mg/L | ||||
| Twice Daily (Tau = 12 h) | ||||||
| 80 | 500 | 30 | 1000 | 62 | 12 | 0 |
| 1000 | 30 | 2000 | 93 | 60 | 0 | |
| 1500 | 30 | 3000 | 99 | 85 | 3 | |
| 2000 | 30 | 4000 | 100 | 94 | 14 | |
| 120 | 500 | 30 | 1000 | 43 | 6 | 0 |
| 1000 | 30 | 2000 | 86 | 43 | 0 | |
| 1500 | 30 | 3000 | 95 | 72 | 2 | |
| 2000 | 30 | 4000 | 98 | 85 | 6 | |
| 160 | 500 | 30 | 1000 | 22 | 1 | 0 |
| 1000 | 30 | 2000 | 67 | 22 | 0 | |
| 1500 | 30 | 3000 | 87 | 51 | 0 | |
| 2000 | 30 | 4000 | 94 | 69 | 2 | |
| 200 | 1000 | 30 | 2000 | 39 | 6 | 0 |
| 1500 | 30 | 3000 | 68 | 25 | 0 | |
| 2000 | 30 | 4000 | 80 | 42 | 0 | |
| 240 | 1500 | 30 | 3000 | 37 | 7 | 0 |
| 2000 | 30 | 4000 | 55 | 15 | 0 | |
| CrCl (mL/min) | Dose (mg) | Perfusion Duration (min) | Daily Dose (mg) | Probability of Cmin (%) | ||
|---|---|---|---|---|---|---|
| >6 mg/L | >12 mg/L | >46 mg/L | ||||
| Three Times Daily (Tau = 8 h) | ||||||
| 80 | 500 | 30 | 1500 | 94 | 51 | 0 |
| 1000 | 30 | 3000 | 100 | 93 | 5 | |
| 1500 | 30 | 4500 | 100 | 99 | 31 | |
| 120 | 500 | 30 | 1500 | 84 | 33 | 0 |
| 1000 | 30 | 3000 | 99 | 84 | 2 | |
| 1500 | 30 | 4500 | 100 | 96 | 17 | |
| 160 | 500 | 30 | 1500 | 65 | 12 | 0 |
| 1000 | 30 | 3000 | 94 | 65 | 0 | |
| 1500 | 30 | 4500 | 99 | 89 | 5 | |
| 2000 | 30 | 6000 | 100 | 97 | 17 | |
| 200 | 500 | 30 | 1500 | 38 | 4 | 0 |
| 1000 | 30 | 3000 | 83 | 39 | 0 | |
| 1500 | 30 | 4500 | 95 | 69 | 1 | |
| 2000 | 30 | 6000 | 98 | 84 | 5 | |
| 240 | 1000 | 30 | 3000 | 61 | 15 | 0 |
| 1500 | 30 | 4500 | 80 | 38 | 0 | |
| 2000 | 30 | 6000 | 89 | 59 | 1 | |
| 2000 | 120 | 6000 | 94 | 67 | 1 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bilbao-Meseguer, I.; Barrasa, H.; Asín-Prieto, E.; Alarcia-Lacalle, A.; Rodríguez-Gascón, A.; Maynar, J.; Sánchez-Izquierdo, J.Á.; Balziskueta, G.; Griffith, M.S.-B.; Quilez Trasobares, N.; et al. Population Pharmacokinetics of Levetiracetam and Dosing Evaluation in Critically Ill Patients with Normal or Augmented Renal Function. Pharmaceutics 2021, 13, 1690. https://doi.org/10.3390/pharmaceutics13101690
Bilbao-Meseguer I, Barrasa H, Asín-Prieto E, Alarcia-Lacalle A, Rodríguez-Gascón A, Maynar J, Sánchez-Izquierdo JÁ, Balziskueta G, Griffith MS-B, Quilez Trasobares N, et al. Population Pharmacokinetics of Levetiracetam and Dosing Evaluation in Critically Ill Patients with Normal or Augmented Renal Function. Pharmaceutics. 2021; 13(10):1690. https://doi.org/10.3390/pharmaceutics13101690
Chicago/Turabian StyleBilbao-Meseguer, Idoia, Helena Barrasa, Eduardo Asín-Prieto, Ana Alarcia-Lacalle, Alicia Rodríguez-Gascón, Javier Maynar, José Ángel Sánchez-Izquierdo, Goiatz Balziskueta, María Sánchez-Bayton Griffith, Nerea Quilez Trasobares, and et al. 2021. "Population Pharmacokinetics of Levetiracetam and Dosing Evaluation in Critically Ill Patients with Normal or Augmented Renal Function" Pharmaceutics 13, no. 10: 1690. https://doi.org/10.3390/pharmaceutics13101690
APA StyleBilbao-Meseguer, I., Barrasa, H., Asín-Prieto, E., Alarcia-Lacalle, A., Rodríguez-Gascón, A., Maynar, J., Sánchez-Izquierdo, J. Á., Balziskueta, G., Griffith, M. S.-B., Quilez Trasobares, N., Solinís, M. Á., & Isla, A. (2021). Population Pharmacokinetics of Levetiracetam and Dosing Evaluation in Critically Ill Patients with Normal or Augmented Renal Function. Pharmaceutics, 13(10), 1690. https://doi.org/10.3390/pharmaceutics13101690







