Abstract
Both temperature and humidity may independently or jointly contribute to the risk of human rhinovirus (HRV) infections, either through altered survival and spread of viruses in the environment or due to changes in host susceptibility. This study examined the relationship between short-term variations in temperature and humidity and the risk of HRV infections in a subarctic climate. We conducted a case-crossover study among conscripts (n = 892) seeking medical attention due to respiratory symptoms during their military training and identified 147 HRV cases by real-time PCR. An average temperature, a decline in daily ambient temperature and absolute humidity (AH) during the three preceding days of the onset (hazard period) and two reference periods (a week prior and after the onset) were obtained. The average daily temperature preceding HRV infections was −9.9 ± 4.9 °C and the average AH was 2.2 ± 0.9 g/m3. An average (odds ratios (OR) 1.07 (95% confidence interval (CI) 1.00–1.15)) and maximal (OR 1.08 (1.01–1.17)) change in temperature increased the risk of HRV infections by 8% per 1 °C decrease. An average (OR 1.20 (CI 1.03–1.40)) and maximal decrease (OR 1.13 (CI 0.96–1.34)) in AH increased the risk of HRV infection by 13% and 20% per 0.5 g/m3 decrease. A higher average temperature during the three preceding days was positively associated with HRV infections (OR 1.07 (CI 1.00–1.15)). A decrease rather than low temperature and humidity per se during the preceding few days increases the risk of HRV infections in a cold climate. The information is applicable to populations residing in cold climates for appropriate personal protection and prevention of adverse health effects.
1. Introduction
Human rhinovirus (HRV) infections have a dominant role as causative agents in upper respiratory tract infections (RTIs) [1,2]. RTIs are the most common infections worldwide, and pose a significant public health burden in terms of absenteeism at schools and at work, increased costs related to lower work productivity, and overload of health care services. HRV infections present various clinical signs such as the common cold, otitis media, sinusitis, bronchiolitis, pneumonia, exacerbation of asthma or chronic obstructive pulmonary disease (COPD), and a HRV epidemic can eventually lead to increased mortality at the population level [2].
Cold weather-related adverse health effects are also related to behavioral, socioeconomic and housing factors which are moderated by vulnerabilities such as age, gender and comorbidities [3]. Substantial evidence exists on the seasonal variation of respiratory morbidity and mortality with the increased use of health services and hospital admissions during the winter season [4,5,6]. Environmental factors, in particular ambient air temperature and humidity, may contribute to the observed seasonal variation of respiratory viruses and the resulting RTIs [6,7,8]. All HRV species have been identified throughout the year, in temperate, tropical, subtropical, and semiarid regions [1], and peaks may occur, during autumn, winter and spring, depending on the climate and the species [2]. However, the reasons for the seasonal variation of HRV infections are not clear and their association with meteorological parameters, if any, has remained largely unknown. Experimental [7,9] and epidemiological [10,11] studies have shown that low temperature and dry air, either separately or combined, increase the risk of viral infections. Although controversial, scientific evidence suggests that inhalation of cold and dry air lowers the upper airways temperature [12,13] and dries the mucosal membrane and may cause pathophysiological responses [14] that contribute to increase the host susceptibility to viral infections. Even body surface cooling may elicit symptoms and a pathophysiological response in the host [15,16]. Also the pathogen itself may be sensitive, so that both low temperature and humidity may improve virus stability and transmission [9].
To our knowledge no previous studies examining the association between meteorological parameters and HRV infections have been conducted in cold climates involving subfreezing temperatures. Overall, only a few studies have examined the association between bio-meteorological assessments and HRV infections [8,17,18,19]. Hence, the objective of this study was to examine the relationship between short-term variations in temperature and humidity and the risk of HRV infections in a subarctic climate. To this purpose, we conducted a case-crossover study among army conscripts during their training period. Military training combines the exposure to cold and heavy physical exercises which may independently or jointly increase host susceptibility to RTIs [20,21,22]. Our hypothesis was that a decrease in daily temperature and humidity increases the risk of HRV infections.
2. Materials and Methods
2.1. Study Subjects
This work is part of a larger CIAS (Cold, Infections and ASthma) study about risk factors for asthma and respiratory infections in Finnish military conscripts [23]. Briefly, 892 men from a total of 3697 men making up two intakes of conscripts to the Kainuu Brigade in Kajaani, Northern Finland (N64°, L27°), in July 2004 and January 2005, were enrolled in this study. The subjects consisted of conscripts of whom a total of 1196 were invited to the study; 937 agreed to participate and 45 were later discharged from service because of health problems, leaving a total of 224 asthmatic and 668 non-asthmatic participants. Their mean (± SD) age was 19.1 ± 0.8 years. The enrolment procedure has been described in detail previously [23]. Each participant was followed until the end of his service lasting six to 12 months.
2.2. Identification of Rhinovirus Infections
Conscripts who sought medical attention for acute respiratory infections at the military primary health care clinic of the Kainuu Brigade were assessed initially by a nurse and then examined by a physician for diagnosis and treatment [23]. The day the physician was consulted for respiratory symptoms was considered the day of onset. Consultations occurring within two weeks were considered as one episode for which information of symptoms, findings and drug prescriptions were collected. The conscripts received a questionnaire inquiring about the circumstances preceding the RTI. A total of 386 sputum samples were collected and the specimens were stored at −70 °C for virological analyses. Overall, broad virus analyses (rhinovirus, influenza, adenovirus, parainfluenza, RSV, human metapneumovirus, enterovirus, Chlamydophila pneumoniae, and Mycoplasma pneumoniae) by sputum PCR and/or serology were conducted. However, the present study focuses on HRV due to scientific interest, and to the abundance of all detected viruses. HRV was identified at the sole pathogen (of those that were tested in the study) in 59 episodes and the remainder of the episodes consisted of HRV together with some other pathogen. Also other pathogens may have been present that were not tested here.
The viral RNA was isolated from 100 μL of sample with MagNA Pure LC Total Nucleic Acid isolation kit using MagNA Pure LC equipment (Roche, Mannheim, Germany) Real-time reverse transcription PCR (RT-PCR) for detection of HRV was performed [24]. The cut-off threshold was set at approximately 8% of the strongest positive control (HRV2 dilution of 10−3) and all plots rising above it were considered positive.
2.3. Exposure Assessment and Measures
Exposure assessment was based on meteorological data obtained from Kajaani Airport Meteorological Station (Paltaniemi, Finland) located at 15 km from the garrison. Average daily temperature and absolute humidity (AH) were calculated based on eight measurements conducted at three-hour intervals. A systematic review suggests that the average incubation period for HRV is 1.9 days [25] and severe symptoms peak 48 h after inoculation of the virus [26]. Therefore, an average of the three days (e.g., a 72 h-period) preceding the visit to the clinic (day 0) was calculated and used in the regression models to capture the potential effect of meteorological variables in the onset of an infection. We separately examined maximal changes, as well as the starting level from where temperature and AH changed. The meteorological conditions at day 0 were not included in the analyses.
2.4. Ethics Statement
The study protocol was approved by the Medical Ethics Committee of the Kainuu Central Hospital (approval No. 20/55/12.05.2003, Kajaani, Finland). The conscripts were informed of the study, possible inconvenience, confidentiality and storing of data both in written and oral form. Participation was voluntary and they could discontinue their participation at any time. The conscripts provided their written informed consent following this information.
2.5. Statistical Analyses
The study employed a case-crossover design which focuses on the point in time when the event occurred and is appropriate for assessing the association between short-term exposure and the risk of an acute event. For environmental temperature and AH the hazard period was defined as three days preceding the visit to the clinic for a respiratory infection. A symmetric bidirectional selection of two reference periods before and after the hazard period was utilized [27]. This means that for temperature and humidity, three-day periods in the seven days before and after the hazard period were used in the models. The statistical model compares the level and change in temperature and humidity during the days preceding the onset (hazard period) to days before and after the onset. This addresses the question of whether the onset of infection precedes unusual levels or a decline in these parameters. As the total number of episodes occurred over 85 days, meteorological information from 765 days was used in our analyses. Conditional logistic regression models were used to calculate the exposure odds ratios (OR) for the hazard compared with the reference periods. The adjusted analyses took into account the initial levels of temperature and humidity. For mean temperature and AH we adjusted for seasonal variation whereas the adjustment of the change in these parameters also considered the fact that the potential for decline in temperature and humidity depends on the starting point. Two-way interactions were tested for temperature, humidity and HRV infections. Statistical analyses were performed by SAS version 9.2 for Windows (SAS Institute, Inc.; Cary, NC, USA).
3. Results
Out of 386 sputum specimens, 147 (37.8%) were analysed by real-time RT-PCR [28] and found positive for HRV. A majority of the episodes were detected during the winter season and occurred as follows: 13 in November 2004, 13 in December 2004, 13 in January 2005, 29 in February 2005, 33 in March 2005, 16 in April 2005, 5 in May 2005, and 7 in June 2005. The remaining episodes were scattered over the rest of the winter season. The temperature ranged from −22.8 °C to 22.0 °C (± 10.1) and AH from 0.8 g/m3 to 14.3 g/m3 (± 3.2) during the follow-up (Figure 1). We observed that 74% of the infection episodes occurred when temperatures were ≤0 °C (109 of 147) and 26% when temperatures were above 0 °C (38 of 147). Of those conscripts infected by HRV who were engaged in outdoor training, 89% (76 of 85) reported being engaged in physical exercise, 73% (62 of 85) felt symptoms of freezing and 36% (31 of 85) reported wetting of socks or gloves during the three days prior to seeking medical consultation.
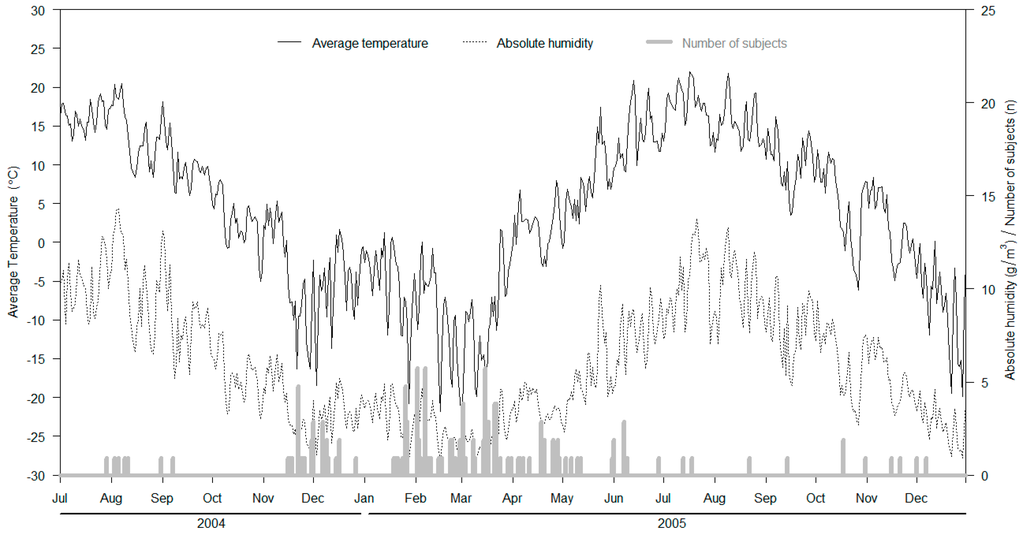
Figure 1.
Incidence of rhinovirus infections, average temperature (°C; black solid line) and absolute humidity (AH) (g/m3; grey dotted line) during the study period.
The average and mean and maximal changes during the hazard and reference periods are presented in Table 1.

Table 1.
Mean and maximal decline in temperature and absolute humidity (AH) during the hazard period (n = 146) prior to the onset of rhinovirus infections and during the reference periods. Values represent mean ± standard deviation (SD).
We observed that the means of the meteorological conditions for the hazard period are not very different from the reference conditions.
According to the adjusted analyses, the effect estimate demonstrates an higher HRV infection risk during the preceding three days for both the mean temperature as well as its change. A reduction in the mean and maximum temperature of 1 °C increases the risk of HRV infection by 8% (Table 2). At the same time, a higher average temperature level increased the risk of HRV infection by 7%. A decrease in the mean and maximal AH during the preceding three days increased the risk by 13% and 20% for each 0.5 g/m3. However, despite the elevated effect estimate, the confidence intervals for mean AH change do not suggest a statistically significant effect. In addition, mean AH during the preceding three days was not significantly associated with HRV infections.

Table 2.
Onset of a human rhinovirus (HRV) infection (n = 146) and its association with mean values and declines in temperature (per 1 °C) and humidity (0.5 g/m3).
4. Discussion
Consistent evidence demonstrates that wintertime cold temperatures increase respiratory morbidity and mortality [4,5,11]. We conducted a case-crossover study to assess the relationship between the daily temperature and humidity and the risk of HRV infections in a subarctic climate. Our results indicate that the risk of HRV infection is associated with a decrease in both temperature and humidity during the three days preceding the infection, but that the risk in general is lower at subfreezing temperatures.
4.1. HRV Infections, Temperature and Humidity
Our novel finding was that a decrease in either temperature or humidity, rather than their levels per se, increases the risk of HRV infections in the three days before seeking medical care. To our knowledge this is the first study assessing relationship between short-term variation in meteorological factors and HRV infections. Our finding is consistent with the observed higher risk of influenza [11] in the same population, assessed in a smaller sample. Support for the importance of variation in temperature as a risk factor for RTIs was also recently obtained from a population study in China where large diurnal differences in temperature increase emergency visits for RTIs [19].
The reason why a decrease in temperature or AH may increase the risk of HRV infections could be related to changes in the host susceptibility. Our hypothesis was that a combination of low temperature and humidity would lead to the cooling and drying of the respiratory tract which may be enhanced during the outdoor physical activity [29] related to military training. This was supported by the cold stress reported by most of the infected individuals during the previous three days. An experimental study showed that breathing cold air during exercise reduces the upper respiratory tract temperature by several degrees and even more because of increased ventilation [13]. A sudden decrease in temperature and humidity could be related to altered airways function, increasing the susceptibility to viral agents. For example, inhaling larger volumes of air with low AH while exercising dries the mucosal membrane [12]. This can even lead to epithelial damage, depress ciliary movement in the respiratory tract [13] and increase the susceptibility to infections. Even cooling of the body surface could elicit a reflex of vasoconstriction in the nose and upper airways, inhibit the respiratory defense and convert an asymptomatic subclinical viral infection into a symptomatic clinical infection [15]. An experimental study on humans showed that acute chilling of the feet elicits symptoms of the common cold [16]. However, another study did not demonstrate altered host resistance to HRV infections as a result of whole-body cold exposure [30]. Finally, both cold exposure and heavy exercise involve stress. Stress itself may predispose the host to acute RTIs [31] and one possible reason is through the suppressed immune processes of the host [21,22]. However, it should be noted that the association between immune function and cold exposure has not been clearly demonstrated [32].
According to our analyses HRV infections were positively related to the mean temperature. This seemingly contradictory finding could be related to the viability and transmission of the pathogen. It is possible that at very low temperatures, the transmission and survival of the virus decrease, as opposed to conditions where temperatures approach zero degrees, and where we observed most of the respiratory tract infections [10]. Previous experimental research on influenza in animal models has suggested that both low temperature and AH increase the viability and transmission of influenza. Low temperature itself could improve viral stability, increase shedding and affect the physical properties of the pathogen [9]. On the other hand, for some viruses, such as respiratory syncytial virus (RSV), elevated temperature may induce conformational changes and increased fusion activity [33]. HRV replication has been shown to improve when the temperature resembles the one in the upper (33 °C) compared to the lower (35 °C) airways [34]. Although we did not observe an association between mean AH and HRV infections, previous experimental studies have shown that both airborne and contact survival of HRV decrease when the relative humidity (RH) ranges from low to moderate (20%–50%) but improves when the RH is high (80%) [35,36]. Even a bimodal pattern for some pathogens has been suggested with altered virus survival and transmission at very low to high humidity [37]. Low humidity could favor viability and transmission of viruses within aerosols [9] which could be an important mode of transmission in cold and dry climates [7,9,37]. The primary route of HRV transmission is controversial and may vary according to environmental conditions either as airborne or contact transmission [1,2]. In addition, our study design does not enable assessment of the specific environmental or host conditions (e.g., role of co-infections) that occurred at the time of the acquisition, or shedding of the virus. It should be noted from our study that in addition to low wintertime outdoor temperature, dry air affects residents both indoors and outdoors.
4.2. Seasonality of HRV Infections
The unique aspect of our study is related to the considerable annual variation in temperature and humidity. We demonstrated that although HRV occurred throughout the year, distinct peaks were observed during the winter season and early spring. The observed HRV infections appeared before, during and after the detected influenza episodes in this study [11] and were not related to the enrolment in military service which occurs twice a year, in July and January. A previous report from the present data showed that all known HRV types were present in the sputum of conscripts: HRV-A strains were discovered steadily throughout the year while HRV-C strains were present in winter and spring specimens and HRV-B strains were found scarcely and mainly during the summer months [28].
There are relatively few studies reporting the association between HRV infections and meteorological parameters. A study investigating hospitalized children from Germany over a five-year period detected that HRV infections occurred more often when the mean (two weeks’) relative humidity was higher. In contrast, low temperature was associated with higher hospitalizations for other acute respiratory illness pathogens [8]. Gardinazzi [18], on the other hand, studied monthly temperature and humidity related with children hospitalized with viral respiratory infections in Brazil, and observed that the infections occurred during the coldest and driest months. Similarly, a recent study from Africa detected that respiratory infection epidemics occurred when mean monthly night-time temperatures and humidity were at their lowest [17]. A comparison between the different studies is difficult or impossible due to variations in climate (mode of transmission), as well as different approaches to study the association between exposure (e.g., seasonal, short-term) and outcomes.
Overall, the reasons for the seasonality of HRV pathogens can be related to the previously mentioned effects of climatic factors on the survival and spread of viruses in the environment; due to changes in the population’s susceptibility to acute RTIs (e.g., seasonal changes in the immune function), and related to the physiological reactions of the host to certain climatic conditions (e.g., breathing cold and dry air) or due to altered transmission of pathogens responsible for acute respiratory illnesses through changing host behavior (e.g., crowding) in certain climatic conditions [6]. The significance of meteorological parameters as determinants of the seasonal variation of respiratory infections is being debated. The concern is timely due to the expected increased variability in winter weather patterns as a result of the climate change.
4.3. Strengths and Limitations of the Study
We used a case-crossover design where time-invariant confounders are controlled by making within-subject comparisons, and time-varying confounders (e.g. seasonal variation in determinants of HRV) by matching referents to the index time [27,38]. Compared to the general population, conscripts are more frequently exposed to cold and physical exercise, which provides additional strength to this study. Military service is mandatory for young men in Finland, and conscripts represent the ordinary and healthy population of this group of age. Despite the case-crossover design, the effect of crowding cannot be excluded. Previous research has shown that that military training is related to a broad spectrum of respiratory pathogens [39] that are effectively spread [21] and can cause mild or severe outbreaks of acute respiratory diseases [20,40]. However, in our study no clear effects related to the onset of military service and the occurrence of HRV infections were observed. In addition, crowding remained constant throughout the follow-up and has not likely affected the main results of our study. One possible limitation is that seeking of medical care may be delayed due to individual differences in incubation times and responses to cold exposure, as well as related to symptoms of HRV infections sometimes being mild. However, on the other hand, we assume that the outdoor training reported frequently in this study, including heavy exercise and chilling and preceding the onset of infections could have worsened the symptoms and favored care-seeking. Another limitation is that the specimens of this study were sputa collected at times of any RTI and it cannot be ruled out that they may have been contaminated with pharyngeal HRV.
5. Conclusions
Our results show that a decrease in temperature and AH is associated with the increased occurrence of HRV infections. In contrast, the risk of HRV infections is reduced at subfreezing temperatures and higher AH. The information is applicable to all populations residing in moderate or cold climates. Individuals and healthcare professionals need to be aware of lowered temperature and humidity as contributing factors in the development of HRV infections. Appropriate whole-body and respiratory protection may reduce potential cold-related adverse respiratory health effects.
Acknowledgments
The CIAS (Cold, Infections and Asthma) Study Group Collaborators (Maija Leinonen, Pekka Saikku, Ari Peitso, Pentti Kuronen, Juhani Hassi, Sylvi Silvennoinen-Kassinen, Thedi Ziegler, Esa Rönkkö, Terttu Harju and Aini Bloigu) are warmly thanked. The Kainuu Central Hospital is acknowledged for the implementation of this study. The Finnish Meteorological Institute is acknowledged for providing the meteorological data.
Author Contributions
T.M.I., R.J., O.V., K.J., J.J., R.J. and A.S. planned the study R.J. collected the data and M.R. performed the HRV analyses. J.J.K.J. was consulted for the statistical approach and T.M.I., J.J., K.J., A.S. and J.J.K.J. contributed to the data analysis. T.M.I., K.J. and A.S. wrote the first draft of the manuscript; all other authors critically reviewed it and approved the final version.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Jacobs, S.E.; Lamson, D.M.; St George, K.; Walsh, T.J. Human rhinoviruses. Clin. Microbiol. Rev. 2013, 26, 135–162. [Google Scholar] [CrossRef] [PubMed]
- Winther, B. Rhinovirus Infections in the upper airway. Proc. Am. Thorac. Soc. 2011, 8, 79–89. [Google Scholar] [CrossRef]
- Tanner, L.M.; Moffatt, S.; Milne, E.M.; Mills, S.D.H.; White, M. Socioeconomic and behavioural risk factors for adverse winter health and social outcomes in economically developed countries: A systematic review of quantitative observational studies. J. Epidemiol. Community Health 2013, 67, 1061–1067. [Google Scholar] [CrossRef] [PubMed]
- Mourtzoukou, E.G.; Falagas, M.E. Exposure to cold and respiratory tract infections. Int. J. Tuberc. Lung Dis. 2007, 11, 938–943. [Google Scholar] [PubMed]
- Conlon, K.C.; Rajkovich, N.B.; White-Newsome, J.L.; Lasen, L.; O’Neill, M.S. Preventing cold-related morbidity and mortality in a changing climate. Maturitas 2011, 69, 197–202. [Google Scholar] [CrossRef] [PubMed]
- Sloan, C.; Moore, M.L.; Hartert, T. Impact of pollution, climate, and sociodemographic factors on spatiotemporal dynamics of seasonal respiratory viruses. Clin. Transl. Sci. 2011, 4, 48–54. [Google Scholar] [CrossRef] [PubMed]
- Shaman, J.; Kohn, M. Absolute humidity modulates influenza survival, transmission, and seasonality. Proc. Natl. Acad. Sci. USA 2009, 106, 3243–3248. [Google Scholar] [CrossRef] [PubMed]
- Du Prel, J.B.; Puppe, W.; Gröndahl, B.; Knuf, M.; Weigl, J.A.I.; Schaaff, F.; Schmitt, H. Are meteorological parameters associated with acute respiratory tract infections? Clin. Infect. Dis. 2009, 49, 861–868. [Google Scholar] [CrossRef] [PubMed]
- Lowen, A.C.; Steel, J. Roles of humidity and temperature in shaping influenza seasonality. J. Virol. 2014, 88, 7692–7695. [Google Scholar] [CrossRef] [PubMed]
- Mäkinen, T.M.; Juvonen, R.; Jokelainen, J.; Harju, T.H.; Peitso, A.; Bloigu, A.; Silvennoinen-Kassinen, S.; Leinonen, M.; Hassi, J. Cold temperature and low humidity are associated with increased occurrence of respiratory tract infections. Respir. Med. 2009, 103, 456–462. [Google Scholar] [CrossRef] [PubMed]
- Jaakkola, K.; Saukkoriipi, A.; Jokelainen, J.; Juvonen, R.; Kauppila, J.; Vainio, O.; Ziegler, T.; Rönkkö, E.; Jaakkola, J.J.; Ikäheimo, T.M.; et al. Decline in temperature and humidity increases the occurrence of influenza in cold climate. Environ. Health 2014, 13, 13–22. [Google Scholar] [CrossRef] [PubMed]
- Liener, K.; Leiacker, R.; Lindemann, J.; Rettinger, G.; Keck, T. Nasal mucosal temperature after exposure to cold, dry air and hot, humid air. Acta Otolaryngol. 2003, 123, 851–856. [Google Scholar] [PubMed]
- Jaeger, J.J.; Deal, E.C., Jr.; Roberts, D.E., Jr.; Mcfadden, E.R., Jr. Cold air inhalation and esophageal temperature in exercising humans. Med. Sci. Sports Exerc. 1980, 12, 365–369. [Google Scholar] [CrossRef] [PubMed]
- Cruz, A.A.; Naclerio, R.M.; Proud, D.; Toqias, A. Epithelial shedding is associated with reactions to cold, dry air. J. Allergy Clin. Immunol. 2006, 117, 1351–1358. [Google Scholar] [CrossRef] [PubMed]
- Eccles, R. Acute cooling of the body surface and the common cold. Rhinology 2002, 40, 109–114. [Google Scholar] [PubMed]
- Johnson, C.; Eccles, R. Acute cooling of the feet and the onset of common cold symptoms. Fam. Pract. 2005, 22, 608–613. [Google Scholar] [CrossRef] [PubMed]
- Ouédraogo, S.; Traoré, B.; Nene Bi, Z.A.; Yonli, F.T.; Kima, D.; Bonané, P.; Congo, L.; Traoré, R.O.; Yé, D.; Marguet, C.; et al. Viral etiology of respiratory tract infections in children at the pediatric hospital in Ouagadougou (Burkina Faso). PLoS ONE 2014, 31, e110435. [Google Scholar] [CrossRef] [PubMed]
- Gardinassi, L.G.; Marques Simas, P.V.; Salomão, J.B.; Durigon, E.L.; Trevisan, D.M.Z.; Cordeiro, J.A.; Lacerda, M.N.; Rahal, P.; de Souza, F.P. Seasonality of viral respiratory infections in southeast of Brazil: The influence of temperature and air humidity. Braz. J. Microbiol. 2012, 43, 98–108. [Google Scholar] [CrossRef] [PubMed]
- Ge, W.Z.; Xu, F.; Zhao, Z.H.; kan, H.D. Association between diurnal temperature range and respiratory tract infections. Biomed. Environ. Sci. 2013, 26, 222–225. [Google Scholar] [PubMed]
- O’Shea, M.K.; Wilson, D. Respiratory infections in the military. J. R. Army Med. Corps 2013, 159, 181–189. [Google Scholar] [CrossRef] [PubMed]
- Korzeniewski, K.; Nitsch-Osuch, A.; Chciałowski, A.; Korsak, J. Environmental factors, immune changes and respiratory diseases in troops during military activities. Respir. Physiol. Neurobiol. 2013, 187, 118–122. [Google Scholar] [CrossRef] [PubMed]
- Shephard, R.J. Immune changes induced by exercise in an adverse environment. Can. J. Physiol. Pharmacol. 1998, 76, 539–546. [Google Scholar] [CrossRef] [PubMed]
- Juvonen, R.; Bloigu, A.; Peitso, A.; Harju, T. Risk factors for acute respiratory tract illness in military conscripts. Respirology 2008, 13, 575–580. [Google Scholar] [CrossRef] [PubMed]
- Lu, X.; Holloway, B.; Dare, R.K.; Kuypers, J.; Yagi, S.; Williams, J.V.; Hall, C.B.; Erdman, D.D. Real-time reverse transcription-PCR assay for comprehensive detection of human rhinoviruses. J. Clin. Microbiol. 2008, 46, 533–539. [Google Scholar] [CrossRef] [PubMed]
- Lessler, J.; Reich, N.G.; Brookmeyer, R.; Perl, T.M.; Nelson, K.E.; Cummings, D.A. Incubation periods of acute respiratory viral infections: A systematic review. Lancet Infect. Dis. 2009, 9, 291–300. [Google Scholar] [CrossRef]
- Gwaltney, J.M., Jr.; Hendley, J.O.; Patrie, J.T. Symptom severity patterns in experimental common colds and their usefulness in timing onset of illness in natural colds. Clin. Infect. Dis. 2003, 36, 714–723. [Google Scholar] [CrossRef] [PubMed]
- Janes, H.; Sheppard, L.; Lumley, T. Reference selection strategies in case-crossover analyses of air pollution exposure data: Implications for bias. Epidemiology 2005, 16, 717–726. [Google Scholar] [CrossRef] [PubMed]
- Savolainen-Kopra, C.; Blomqvist, S.; Kaijalainen, S.; Jounio, U.; Juvonen, R.; Peitso, A.; Saukkoriipi, A.; Vainio, O.; Hovi, T.; Roivainen, M. All known human rhinovirus species are present in sputum specimens of military recruits during respiratory infection. Viruses 2009, 1, 1178–1189. [Google Scholar] [CrossRef] [PubMed]
- Carlsen, K.H. Sports in extreme conditions: The impact of exercise in cold temperatures on asthma and bronchial hyper-responsiveness in athletes. Br. J. Sports Med. 2012, 46, 796–799. [Google Scholar] [CrossRef] [PubMed]
- Douglas, R.G.; Lindgren, K.M.; Couch, R.B. Exposure to cold environment and Rhinovirus common cold-failure to demonstrate the effect. N. Engl. J. Med. 1968, 279, 742–747. [Google Scholar] [CrossRef]
- Graham, N.M.; Douglas, R.M.; Ryan, P. Stress and acute respiratory infection. Am. J. Epidemiol. 1986, 124, 389–401. [Google Scholar] [PubMed]
- Castellani, J.W.; M Brenner, I.K.; Rhind, S.G. Cold exposure: Human immune responses and intracellular cytokine expression. Med. Sci. Sports Exerc. 2002, 34, 2013–2020. [Google Scholar] [CrossRef] [PubMed]
- Yunus, A.S.; Jackson, T.P.; Crisafi, K.; Burimski, I.; Kilgore, N.R.; Zoumplis, D.; Allaway, G.P.; Wild, C.T.; Salzwedel, K. Elevated temperature triggers human respiratory syncytial virus F protein six-helix bundle formation. Virology 2010, 96, 226–237. [Google Scholar] [CrossRef] [PubMed]
- Papadopoulos, N.G.; Sanderson, G.; Hunter, J.; Johnston, S.L. Rhinoviruses replicate effectively at lower airway temperatures. J. Med. Virol. 1999, 58, 100–104. [Google Scholar] [CrossRef]
- Karim, Y.G.; Ijaz, M.K.; Sattar, S.A.; Johnson-Lussenburg, C.M. Effect of relative humidity on the airborne survival of rhinovirus-14. Can. J. Microbiol. 1985, 31, 1058–1061. [Google Scholar] [CrossRef] [PubMed]
- Sattar, S.A.; Karim, Y.G.; Springthorpe, V.S.; Johnson-Lussenburg, C.M. Survival of human rhinovirus type 14 dried onto nonporous inanimate surfaces: Effect of relative humidity and suspending medium. Can. J. Microbiol. 1987, 33, 802–806. [Google Scholar] [CrossRef] [PubMed]
- Tamerius, J.D.; Shaman, J.; Alonso, W.J.; Bloom-Feshbach, K.; Uejio, C.K.; Comrie, A.; Viboudet, C. Environmental predictors of seasonal influenza epidemics across temperate and tropical climates. PLoS Pathog. 2013, 9, e1003194. [Google Scholar] [CrossRef]
- Jackson, M.L. Confounding by season in ecologic studies of seasonal exposures and outcomes: Examples from estimates of mortality due to influenza. Ann. Epidemiol. 2009, 19, 681–691. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Malanoski, A.P.; Lin, B.; Long, N.C.; Leski, T.A.; Blanay, K.M.; Hansen, C.J.; Brown, J.; Broderick, M.; Stenger, D.A.; et al. Broad spectrum respiratory pathogen analysis of throat swabs from military recruits reveals interference between rhinoviruses and adenoviruses. Microb. Ecol. 2010, 59, 623–634. [Google Scholar] [CrossRef] [PubMed]
- Tate, J.E.; Bunning, M.L.; Lott, L.; Li, X.; Su, J.; Metzgar, D.; Brosch, L.; Panozzo, C.A.; Marconi, V.C.; Faix, D.J.; et al. Outbreak of severe respiratory disease associated with emergent human adenovirus serotype 14 at a US Air Force training facility in 2007. J. Infect. Dis. 2009, 199, 1419–1426. [Google Scholar] [CrossRef] [PubMed]
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).