Characterization of a STAT-1 Knockout Mouse Model for Machupo Virus Infection and Pathogenesis
Abstract
1. Introduction
2. Materials and Methods
2.1. Cell Lines
2.2. Animal Models
2.3. In Vivo Challenges
2.4. Serial Sampling Studies
2.5. Generation of Mouse-Adapted MACV
2.6. Plaque Assay
2.7. ELISA
2.8. Neutralization Assay
2.9. Cytokine and Chemokine Analysis
2.10. PCR
2.11. Sequencing
2.12. Histopathology
2.13. In Situ Hybridization
2.14. Statistical Analysis
3. Results
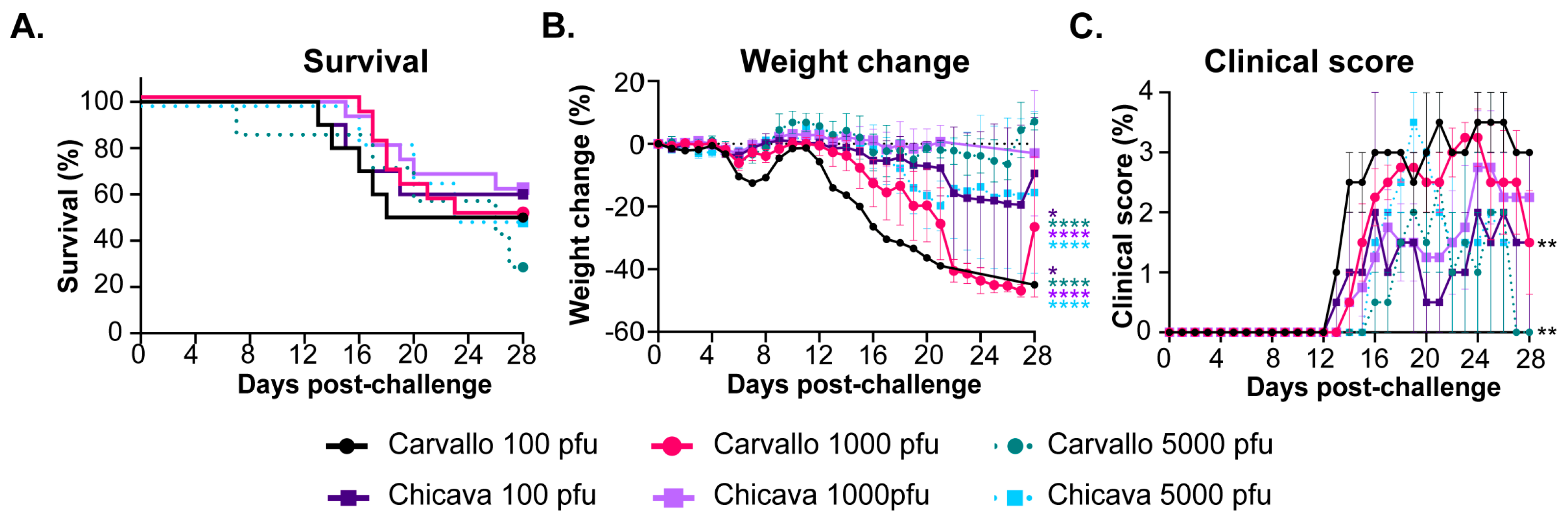
3.1. MACV Is Partially Lethal in STAT-1−/− Mice
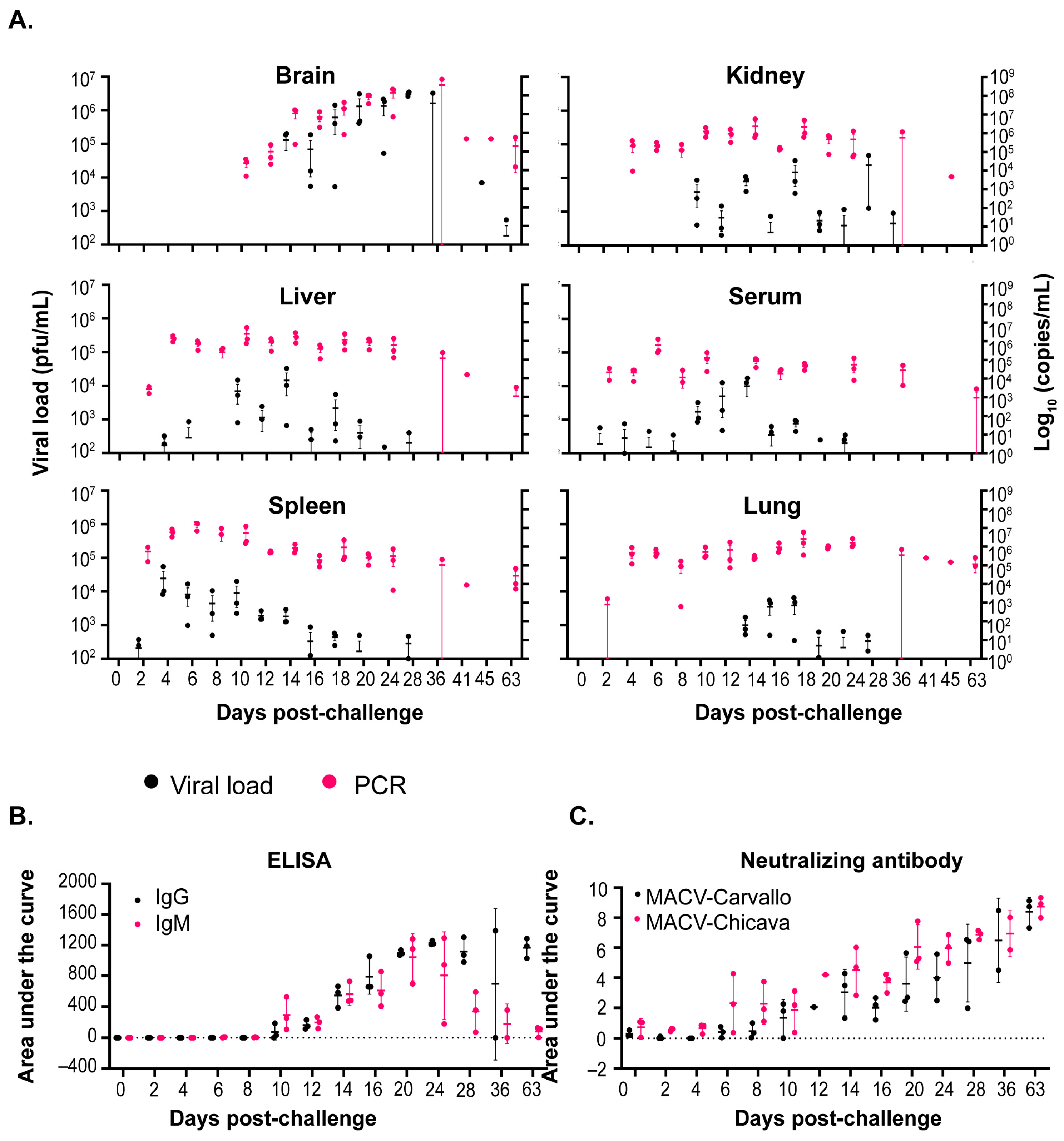
3.2. Analysis of the Progression of MACV Disease in STAT-1−/− Mice
3.2.1. Infectious Virus Load
3.2.2. Antibody Titers and Neutralizing Response
3.2.3. Correlation of Viral Load with Weight Change and Clinical Score
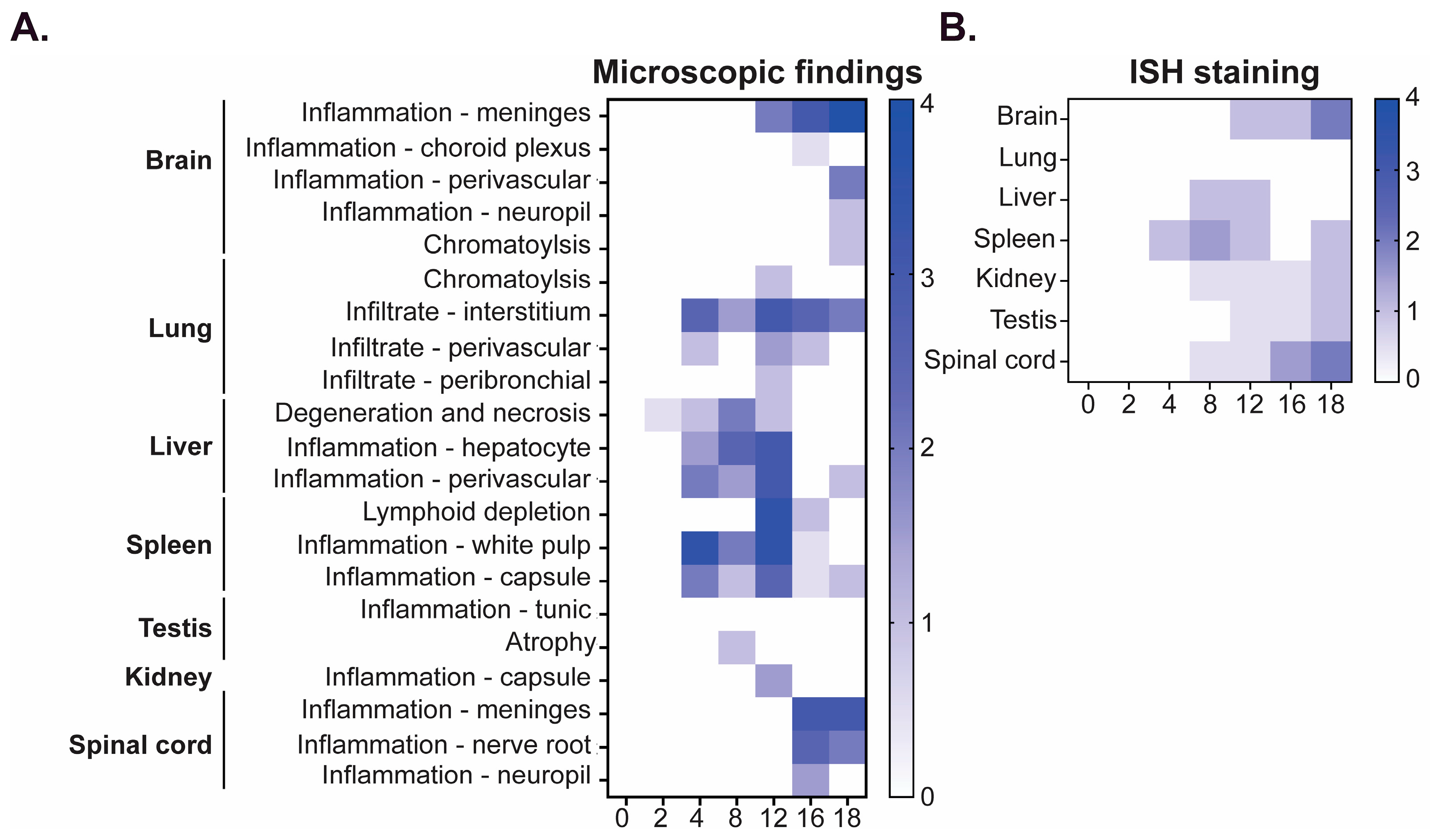
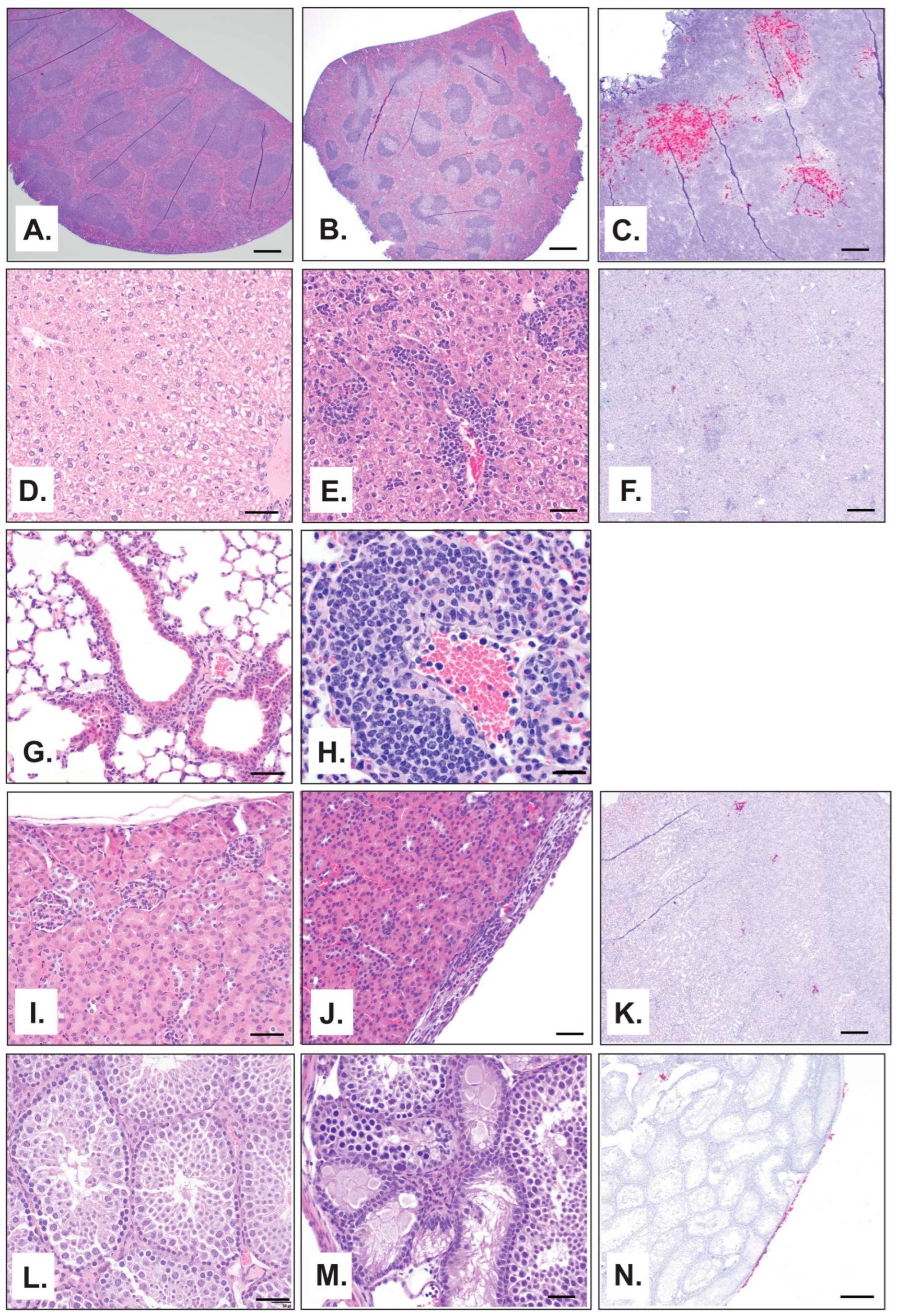
3.2.4. Anatomic Pathology
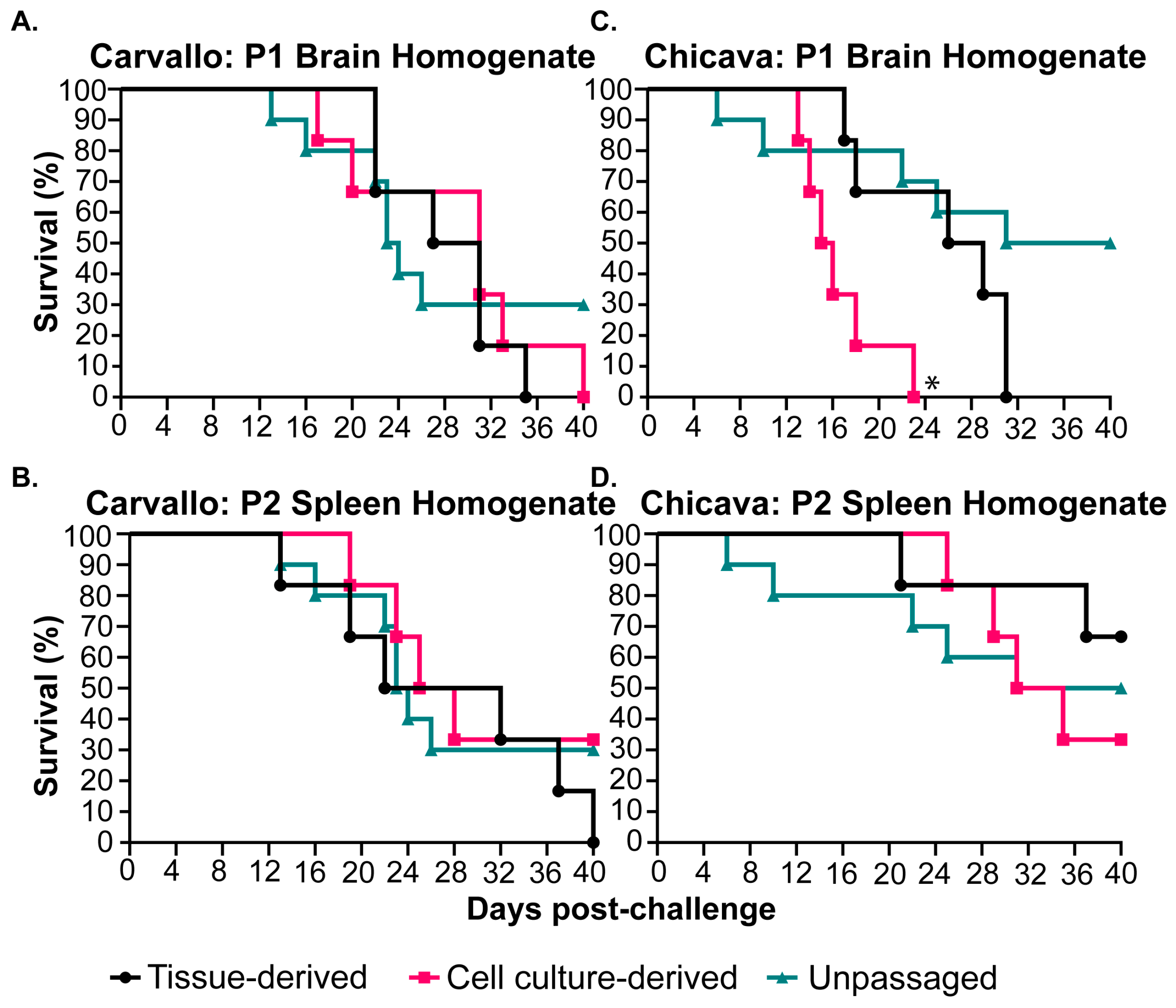
3.3. Adaptation of MACV in STAT-1−/− Mice
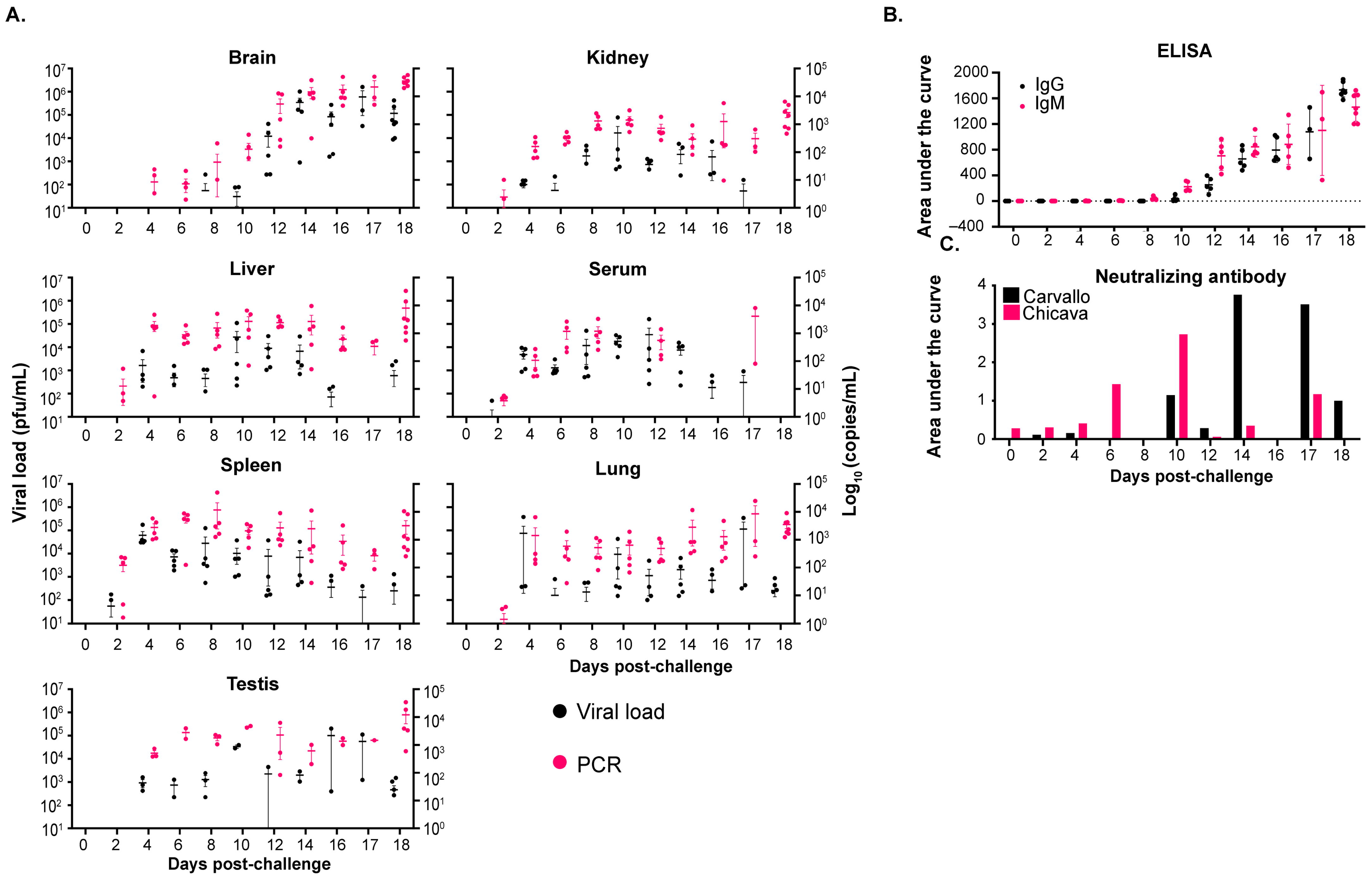
3.4. Analysis of the Progression of maMACV Disease in STAT-1−/− Mice
3.4.1. Infectious Virus Load
3.4.2. Antibody Titers and Neutralizing Response
3.4.3. Correlation of Viral Load with Weight Change and Clinical Score
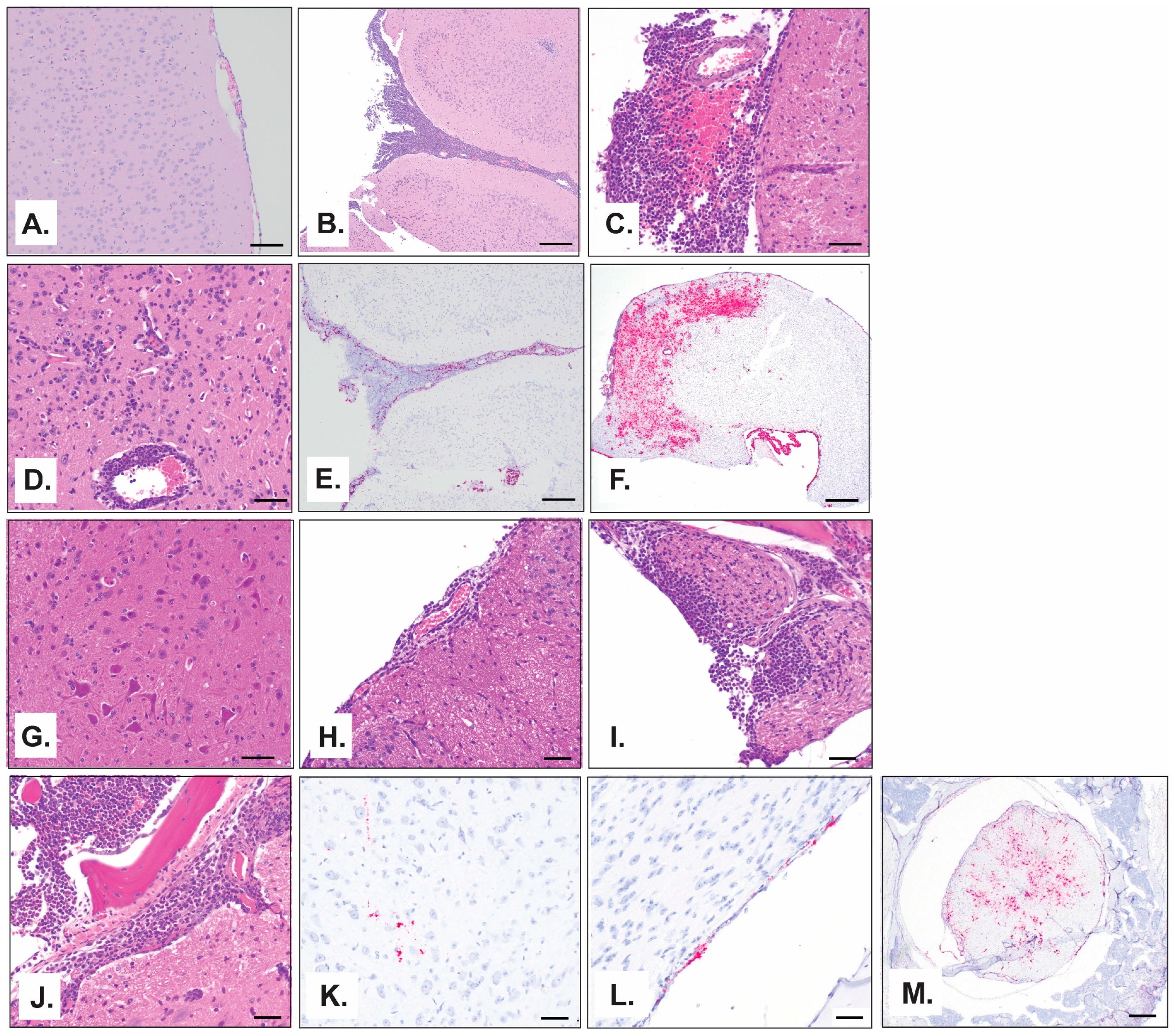
3.4.4. Anatomic Pathology
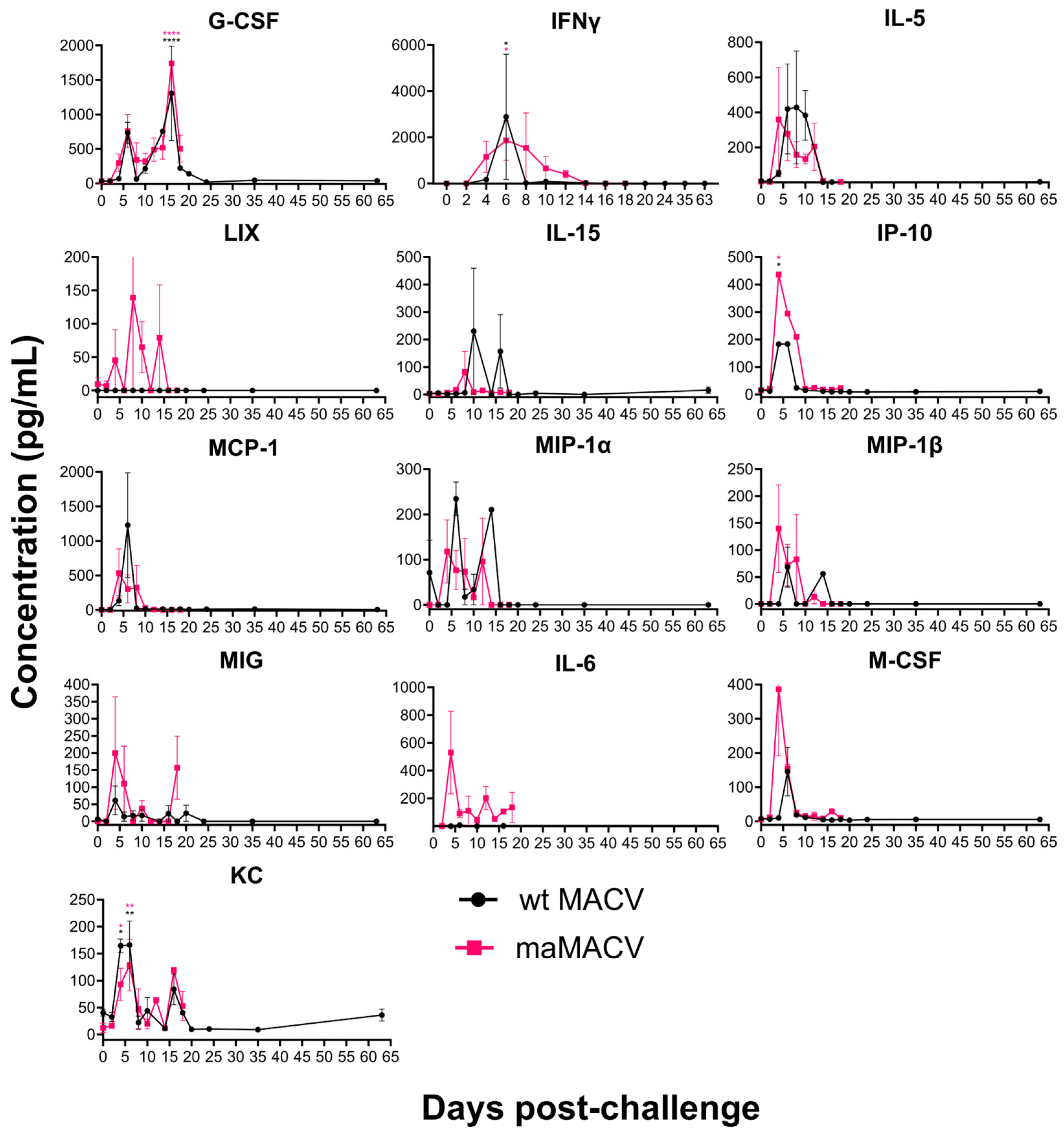
3.4.5. Cytokine and Chemokine Analysis
3.4.6. Sequencing of MACV and maMACV
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Johnson, K.; Kuns, M.; Mackenzie, R.; Webb, P.; Yunker, C. Isolation of Machupo virus from wild rodent Calomys callosus. Am. J. Trop. Med. Hyg. 1966, 15, 103–106. [Google Scholar] [CrossRef] [PubMed]
- Mackenzie, R.B.; Beye, H.K.; Valverde, C.L.; Garrón, H. Epidemic Hemorrhagic Fever in Bolivia. I. A Preliminary Report of the Epide-miologic and Clinical Findings in a New Epidemic Area in South America. Am. J. Trop. Med. Hyg. 1964, 13, 620–625. [Google Scholar] [CrossRef] [PubMed]
- Fields, B.N. Fields’ Virology; Lippincott Williams & Wilkins: Philadelpha, PA, USA, 2007; Volume 1. [Google Scholar]
- Aguilar, P.V.; Camargo, W.; Vargas, J.; Guevara, C.; Roca, Y.; Felices, V.; Laguna-Torres, V.A.; Tesh, R.; Ksiazek, T.G.; Kochel, T.J. Reemergence of Bolivian hemorrhagic fever, 2007–2008. Emerg. Infect. Dis. 2009, 15, 1526–1528. [Google Scholar] [CrossRef] [PubMed]
- Patterson, M.; Grant, A.; Paessler, S. Epidemiology and pathogenesis of Bolivian hemorrhagic fever. Curr. Opin. Virol. 2014, 5, 82–90. [Google Scholar] [CrossRef] [PubMed]
- Silva-Ramos, C.R.; Faccini-Martínez, Á.A.; Calixto, O.-J.; Hidalgo, M. Bolivian hemorrhagic fever: A narrative review. Travel Med. Infect. Dis. 2021, 40, 102001. [Google Scholar] [CrossRef] [PubMed]
- Johnson, K.M. Epidemiology of Machupo virus infection. III. Significance of virological observations in man and animals. Am. J. Trop. Med. Hyg. 1965, 14, 816–818. [Google Scholar] [CrossRef] [PubMed]
- Johnson, K.M.; Wiebenga, N.H.; Mackenzie, R.B.; Kuns, M.L.; Tauraso, N.M.; Shelokov, A.; Webb, P.A.; Justines, G.; Beye, H.K. Virus Isolations from Human Cases of Hemorrhagic Fever in Bolivia. Proc. Soc. Exp. Biol. Med. 1965, 118, 113–118. [Google Scholar] [CrossRef] [PubMed]
- Kuns, M.L. Epidemiology of Machupo virus infection. II. Ecological and control studies of hemorrhagic fever. Am. J. Trop. Med. Hyg. 1965, 14, 813–816. [Google Scholar] [CrossRef] [PubMed]
- Douglas, R.G., Jr.; Wiebenga, N.; Couch, R.B. Bolivian Hemorrhagic Fever probably transmitted by Personal Contact. Am. J. Epidemiol. 1965, 82, 85–91. [Google Scholar] [CrossRef]
- Stinebaugh, B.J.; Schloeder, F.X.; Johnson, K.M.; Mackenzie, R.B.; Entwisle, G.; De Alba, E. Bolivian hemorrhagic fever: A report of four cases. Am. J. Med. 1966, 40, 217–230. [Google Scholar] [CrossRef] [PubMed]
- Book, R. Hemorrhagic Fevers Caused by Arenaviruses; Pickering, L.K., Ed.; American Academy of Pediatrics: Elk Grove Village, IL, USA, 2009; pp. 325–326. [Google Scholar]
- Tesh, R.B. Viral hemorrhagic fevers of South America. Biomédica 2002, 22, 287–295. [Google Scholar] [CrossRef] [PubMed]
- Cajimat, M.N.; Milazzo, M.L.; Rollin, P.E.; Nichol, S.T.; Bowen, M.D.; Ksiazek, T.G.; Fulhorst, C.F. Genetic diversity among Bolivian arenaviruses. Virus Res. 2009, 140, 24–31. [Google Scholar] [CrossRef] [PubMed]
- Charrel, R.N.; de Lamballerie, X. Arenaviruses other than Lassa virus. Antivir. Res. 2003, 57, 89–100. [Google Scholar] [CrossRef] [PubMed]
- Stephen, E.; Scott, S.; Eddy, G.; Levy, H. Effect of interferon on togavirus and arenavirus infections of animals. Tex. Rep. Biol. Med. 1977, 35, 449–454. [Google Scholar] [PubMed]
- Golden, J.W.; Kwilas, S.A.; Hooper, J.W. Glycoprotein-Specific Polyclonal Antibodies Targeting Machupo Virus Protect Guinea Pigs against Lethal Infection. Vaccines 2024, 12, 674. [Google Scholar] [CrossRef] [PubMed]
- Kilgore, P.E.; Peters, C.J.; Mills, J.N.; Rollin, P.E.; Armstrong, L.; Khan, A.S.; Ksiazek, T.G. Prospects for the control of Bolivian hemorrhagic fever. Emerg. Infect. Dis. 1995, 1, 97. [Google Scholar] [CrossRef] [PubMed]
- Kilgore, P.E.; Ksiazek, T.G.; Rollin, P.E.; Mills, J.N.; Villagra, M.R.; Montenegro, M.J.; Costales, M.A.; Paredes, L.C.; Peters, C. Treatment of Bolivian hemorrhagic fever with intravenous ribavirin. Clin. Infect. Dis. 1997, 24, 718–722. [Google Scholar] [CrossRef] [PubMed]
- Eddy, G.; Wagner, F.; Scott, S.; Mahlandt, B. Protection of monkeys against Machupo virus by the passive administration of Bolivian haemorrhagic fever immunoglobulin (human origin). Bull. World Health Organ. 1975, 52, 723. [Google Scholar] [PubMed]
- Webb, P.; Justines, G.; Johnson, K. Infection of wild and laboratory animals with Machupo and Latino viruses. Bull. World Health Organ. 1975, 52, 493. [Google Scholar] [PubMed]
- Terrell, T.G.; Stookey, J.L.; Eddy, G.A.; Kastello, M.D. Pathology of Bolivian hemorrhagic fever in the rhesus monkey. Am. J. Pathol. 1973, 73, 477. [Google Scholar] [PubMed]
- McLeod Jr, C.G.; Stookey, J.L.; White, J.D.; Eddy, G.A.; Fry, G.A. Pathology of Bolivian Hemorrhagic fever in the African green monkey. Am. J. Trop. Med. Hyg. 1978, 27, 822–826. [Google Scholar] [CrossRef] [PubMed]
- Kastello, M.D.; Eddy, G.A.; Kuehne, R.W. A rhesus monkey model for the study of Bolivian hemorrhagic fever. J. Infect. Dis. 1976, 133, 57–62. [Google Scholar] [CrossRef] [PubMed]
- Bell, T.M.; Bunton, T.E.; Shaia, C.I.; Raymond, J.W.; Honnold, S.P.; Donnelly, G.C.; Shamblin, J.D.; Wilkinson, E.R.; Cashman, K.A. Pathogenesis of Bolivian Hemorrhagic Fever in Guinea Pigs. Vet. Pathol. 2016, 53, 190–199. [Google Scholar] [CrossRef] [PubMed]
- Patterson, M.; Seregin, A.; Huang, C.; Kolokoltsova, O.; Smith, J.; Miller, M.; Smith, J.; Yun, N.; Poussard, A.; Grant, A.; et al. Rescue of a recombinant Machupo virus from cloned cDNAs and in vivo characterization in interferon (αβ/γ) receptor double knockout mice. J. Virol. 2014, 88, 1914–1923. [Google Scholar] [CrossRef] [PubMed]
- Bradfute, S.B.; Stuthman, K.S.; Shurtleff, A.C.; Bavari, S. A STAT-1 knockout mouse model for Machupo virus pathogenesis. Virol. J. 2011, 8, 300. [Google Scholar] [CrossRef] [PubMed]
- Kugelman, J.R.; Wiley, M.R.; Nagle, E.R.; Reyes, D.; Pfeffer, B.P.; Kuhn, J.H.; Sanchez-Lockhart, M.; Palacios, G.F. Error baseline rates of five sample preparation methods used to characterize RNA virus populations. PLoS ONE 2017, 12, e0171333. [Google Scholar] [CrossRef] [PubMed]
- Bolger, A.M.; Lohse, M.; Usadel, B. Trimmomatic: A flexible trimmer for Illumina sequence data. Bioinformatics 2014, 30, 2114–2120. [Google Scholar] [CrossRef] [PubMed]
- Bell, T.M.; Shaia, C.I.; Bunton, T.E.; Robinson, C.G.; Wilkinson, E.R.; Hensley, L.E.; Cashman, K.A. Pathology of experimental Machupo virus infection, Chicava strain, in cynomolgus macaques (Macaca fascicularis) by intramuscular and aerosol exposure. Vet. Pathol. 2015, 52, 26–37. [Google Scholar] [CrossRef] [PubMed]
- Yaghoobizad, S.; Norouzbabaei, Z.; Shafiei Jandaghi, N.Z.; Rahimi Foroushani, A.; Sadeghi, K.; Izadi, S.; Fatemi-Nasab, G.S.; Heidari, E.; Salimi, V.; Mokhtari-Azad, T. Evaluation of the focus reduction neutralization and ELISA tests compared to the plaque reduction neutralization test for the detection of antibodies against measles virus. Biologicals 2024, 88, 101795. [Google Scholar] [CrossRef] [PubMed]
- Peters, C.J.; Kuehne, R.; Mercado, R.; Le Bow, R.; Spertzel, R.; Webb, P. Hemorrhagic fever in cochabamba, bolivia, 1971. Am. J. Epidemiol. 1974, 99, 425–433. [Google Scholar] [CrossRef] [PubMed]
- Villagra, M.; Suarez, L.; Arce, R.; Moreira, M. Bolivian hemorrhagic fever-El Beni Department, Bolivia, 1994. Morb. Mortal. Wkly. Rep. 1994, 43, 943–946. [Google Scholar]
- Banerjee, C.; Allen, L.J.; Salazar-Bravo, J. Models for an arenavirus infection in a rodent population: Consequences of horizontal, vertical and sexual transmission. Math. Biosci. Eng. 2008, 5, 617–645. [Google Scholar] [CrossRef]
- Durbin, J.E.; Hackenmiller, R.; Simon, M.C.; Levy, D.E. Targeted disruption of the mouse Stat1 gene results in compromised innate immunity to viral disease. Cell 1996, 84, 443–450. [Google Scholar] [CrossRef] [PubMed]
- Meraz, M.A.; White, J.M.; Sheehan, K.C.; Bach, E.A.; Rodig, S.J.; Dighe, A.S.; Kaplan, D.H.; Riley, J.K.; Greenlund, A.C.; Campbell, D.; et al. Targeted disruption of the Stat1 gene in mice reveals unexpected physiologic specificity in the JAK-STAT signaling pathway. Cell 1996, 84, 431–442. [Google Scholar] [CrossRef] [PubMed]
- Katzenell, S.; Chen, Y.; Parker, Z.M.; Leib, D.A. The differential interferon responses of two strains of Stat1-deficient mice do not alter susceptibility to HSV-1 and VSV in vivo. Virology 2014, 450–451, 350–354. [Google Scholar] [CrossRef] [PubMed]
- Pasieka, T.J.; Collins, L.; O’Connor, M.A.; Chen, Y.; Parker, Z.M.; Berwin, B.L.; Piwnica-Worms, D.R.; Leib, D.A. Bioluminescent imaging reveals divergent viral pathogenesis in two strains of Stat1-deficient mice, and in αβγ interferon receptor-deficient mice. PLoS ONE 2011, 6, e24018. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Koma, T.; Huang, C.; Aronson, J.F.; Walker, A.G.; Miller, M.; Smith, J.N.; Patterson, M.; Paessler, S. The Ectodomain of Glycoprotein from the Candid#1 Vaccine Strain of Junin Virus Rendered Machupo Virus Partially Attenuated in Mice Lacking IFN-αβ/γ Receptor. PLoS Negl. Trop. Dis. 2016, 10, e0004969. [Google Scholar] [CrossRef]
- Martínez-Sobrido, L.; Zúñiga, E.I.; Rosario, D.; García-Sastre, A.; de la Torre, J.C. Inhibition of the type I interferon response by the nucleoprotein of the prototypic arenavirus lymphocytic choriomeningitis virus. J. Virol. 2006, 80, 9192–9199. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Sobrido, L.; Giannakas, P.; Cubitt, B.; García-Sastre, A.; de la Torre, J.C. Differential inhibition of type I interferon induction by arenavirus nucleoproteins. J. Virol. 2007, 81, 12696–12703. [Google Scholar] [CrossRef] [PubMed]
- Papageorgiou, N.; Spiliopoulou, M.; Nguyen, T.-H.V.; Vaitsopoulou, A.; Laban, E.Y.; Alvarez, K.; Margiolaki, I.; Canard, B.; Ferron, F. Brothers in arms: Structure, assembly and function of Arenaviridae nucleoprotein. Viruses 2020, 12, 772. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.J.; Novella, I.S.; Teng, M.N.; Oldstone, M.B.; de la Torre, J.C. NP and L proteins of lymphocytic choriomeningitis virus (LCMV) are sufficient for efficient transcription and replication of LCMV genomic RNA analogs. J. Virol. 2000, 74, 3470–3477. [Google Scholar] [CrossRef] [PubMed]
- López, N.; Jácamo, R.; Franze-Fernández, M.T. Transcription and RNA replication of tacaribe virus genome and antigenome analogs require N and L proteins: Z protein is an inhibitor of these processes. J. Virol. 2001, 75, 12241–12251. [Google Scholar] [CrossRef] [PubMed]
- Casabona, J.C.; Levingston Macleod, J.M.; Loureiro, M.E.; Gomez, G.A.; Lopez, N. The RING domain and the L79 residue of Z protein are involved in both the rescue of nucleocapsids and the incorporation of glycoproteins into infectious chimeric arenavirus-like particles. J. Virol. 2009, 83, 7029–7039. [Google Scholar] [CrossRef] [PubMed]
- Eichler, R.; Strecker, T.; Kolesnikova, L.; ter Meulen, J.; Weissenhorn, W.; Becker, S.; Klenk, H.D.; Garten, W.; Lenz, O. Characterization of the Lassa virus matrix protein Z: Electron microscopic study of virus-like particles and interaction with the nucleoprotein (NP). Virus Res. 2004, 100, 249–255. [Google Scholar] [CrossRef] [PubMed]
- Shtanko, O.; Imai, M.; Goto, H.; Lukashevich, I.S.; Neumann, G.; Watanabe, T.; Kawaoka, Y. A role for the C terminus of Mopeia virus nucleoprotein in its incorporation into Z protein-induced virus-like particles. J. Virol. 2010, 84, 5415–5422. [Google Scholar] [CrossRef] [PubMed]
- Pythoud, C.; Rodrigo, W.S.I.; Pasqual, G.; Rothenberger, S.; Martínez-Sobrido, L.; de la Torre, J.C.; Kunz, S. Arenavirus nucleoprotein targets interferon regulatory factor-activating kinase IKKε. J. Virol. 2012, 86, 7728–7738. [Google Scholar] [CrossRef] [PubMed]
- Rodrigo, W.S.I.; Ortiz-Riaño, E.; Pythoud, C.; Kunz, S.; de la Torre, J.C.; Martínez-Sobrido, L. Arenavirus nucleoproteins prevent activation of nuclear factor kappa B. J. Virol. 2012, 86, 8185–8197. [Google Scholar] [CrossRef] [PubMed]
- Shao, J.; Huang, Q.; Liu, X.; Di, D.; Liang, Y.; Ly, H. Arenaviral nucleoproteins suppress PACT-induced augmentation of RIG-I function to inhibit type I interferon production. J. Virol. 2018, 92, 10–1108. [Google Scholar] [CrossRef] [PubMed]
- Wei, H.; Audet, J.; Wong, G.; He, S.; Huang, X.; Cutts, T.; Theriault, S.; Xu, B.; Kobinger, G.; Qiu, X. Deep-sequencing of Marburg virus genome during sequential mouse passaging and cell-culture adaptation reveals extensive changes over time. Sci. Rep. 2017, 7, 3390. [Google Scholar] [CrossRef] [PubMed]
- Ni, M.; Chen, C.; Qian, J.; Xiao, H.-X.; Shi, W.-F.; Luo, Y.; Wang, H.-Y.; Li, Z.; Wu, J.; Xu, P.-S. Intra-host dynamics of Ebola virus during 2014. Nat. Microbiol. 2016, 1, 16151. [Google Scholar] [CrossRef] [PubMed]
- Fischer, N. Infection-induced epigenetic changes and their impact on the pathogenesis of diseases. Semin. Immunopathol. 2020, 42, 127–130. [Google Scholar] [CrossRef] [PubMed]
- Rehman, U.U.; Ghafoor, D.; Ullah, A.; Ahmad, R.; Hanif, S. Epigenetics regulation during virus-host interaction and their effects on the virus and host cell. Microb. Pathog. 2023, 182, 106271. [Google Scholar] [CrossRef] [PubMed]
- Puthenparampil, M.; Marin, A.; Zanotelli, G.; Mauceri, V.A.; De Napoli, F.; Gaggiola, M.; Miscioscia, A.; Ponzano, M.; Bovis, F.; Perini, P.; et al. Blood-brain barrier damage associates with glia-related cytokines in the cerebrospinal fluid of patients with Multiple Sclerosis. Mult. Scler. Relat. Disord. 2024, 82, 105403. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.-Y.; Tu, Y.-F.; Lin, Y.-C.; Huang, C.-C. CXCL5 signaling is a shared pathway of neuroinflammation and blood–brain barrier injury contributing to white matter injury in the immature brain. J. Neuroinflamm. 2016, 13, 6. [Google Scholar] [CrossRef] [PubMed]
- Ramesh, G.; MacLean, A.G.; Philipp, M.T. Cytokines and chemokines at the crossroads of neuroinflammation, neurodegeneration, and neuropathic pain. Mediat. Inflamm. 2013, 2013, 480739. [Google Scholar] [CrossRef] [PubMed]
- Erta, M.; Quintana, A.; Hidalgo, J. Interleukin-6, a major cytokine in the central nervous system. Int. J. Biol. Sci. 2012, 8, 1254–1266. [Google Scholar] [CrossRef] [PubMed]
- Masood, K.I.; Jamil, B.; Rahim, M.; Islam, M.; Farhan, M.; Hasan, Z. Role of TNF α, IL-6 and CXCL10 in Dengue disease severity. Iran. J. Microbiol. 2018, 10, 202–207. [Google Scholar] [PubMed]
- Mehta, V.K.; Verma, R.; Garg, R.K.; Malhotra, H.S.; Sharma, P.K.; Jain, A. Study of interleukin-6 and interleukin-8 levels in patients with neurological manifestations of dengue. J. Postgrad. Med. 2017, 63, 11–15. [Google Scholar] [CrossRef] [PubMed]
- Guha, D.; Klamar, C.R.; Reinhart, T.; Ayyavoo, V. Transcriptional Regulation of CXCL5 in HIV-1-Infected Macrophages and Its Functional Consequences on CNS Pathology. J. Interferon Cytokine Res. 2015, 35, 373–384. [Google Scholar] [CrossRef] [PubMed]
- Levis, S.; Saavedra, M.; Ceccoli, C.; Falcoff, E.; Feuillade, M.; Enria, D.; Maiztegui, J.; Falcoff, R. Endogenous interferon in Argentine hemorrhagic fever. J. Infect. Dis. 1984, 149, 428–433. [Google Scholar] [CrossRef] [PubMed]
- Levis, S.C.; Saavedra, M.C.; Ceccoli, C.; Feuillade, M.R.; Enría, D.A.; Maiztegui, J.I.; Falcoff, R. Correlation between endogenous interferon and the clinical evolution of patients with Argentine hemorrhagic fever. J. Interferon Res. 1985, 5, 383–389. [Google Scholar] [CrossRef] [PubMed]
- Pozner, R.G.; Ure, A.E.; Jaquenod de Giusti, C.; D’Atri, L.P.; Italiano, J.E.; Torres, O.; Romanowski, V.; Schattner, M.; Gómez, R.M. Junin virus infection of human hematopoietic progenitors impairs in vitro proplatelet formation and platelet release via a bystander effect involving type I IFN signaling. PLoS Pathog. 2010, 6, e1000847. [Google Scholar] [CrossRef] [PubMed]

| Genbank Number | Virus | Segment |
|---|---|---|
| PV861671 | maMACV-Chicava P1 brain | S segment |
| PV861672 | maMACV-Chicava P1 brain | L segment |
| PV861674 | maMACV-Chicava P2 spleen | L segment |
| PV861675 | maMACV-Chicava P2 spleen | S segment |
| PV861684 | maMACV-Carvallo P1 brain | L segment |
| PV861685 | maMACV-Carvallo P1 brain | S segment |
| PV861680 | maMACV-Carvallo P2 spleen | L segment |
| PV861681 | maMACV-Carvallo P2 spleen | S segment |
| Tissue | R2 vs. Weight Loss | p-Value vs. Weight Loss |
|---|---|---|
| Brain | 0.4169 | <0.0001 (****) |
| Liver | 0.00239 | 0.7498 (ns) |
| Spleen | 0.01828 | 0.3759 (ns) |
| Lung | 0.1105 | 0.0257 (*) |
| Kidney | 0.03836 | 0.1973 (ns) |
| Serum | 0.002975 | 0.7219 (ns) |
| Tissue | R2 vs. Clinical Score | p-Value vs. Clinical Score |
|---|---|---|
| Brain | 0.3427 | <0.0001 (****) |
| Liver | 0.003746 | 0.6896 (ns) |
| Spleen | 0.06711 | 0.0857 (ns) |
| Lung | 0.1962 | 0.0023 (**) |
| Kidney | 0.125 | 0.0172 (*) |
| Serum | 0.01172 | 0.4789 (ns) |
| Tissue | R2 vs. Weight Loss | p-Value vs. Weight Loss |
|---|---|---|
| Brain | 0.1152 | 0.0138 (*) |
| Liver | 0.0064 | 0.5714 (ns) |
| Spleen | 0.0842 | 0.0370 (*) |
| Lung | 0.0077 | 0.5374 (ns) |
| Kidney | 0.0076 | 0.5376 (ns) |
| Testis | 0.0871 | 0.1432 (ns) |
| Serum | 0.03588 | 0.1786 (ns) |
| Tissue | R2 vs. Clinical Score | p-Value vs. Clinical Score |
|---|---|---|
| Brain | 0.1069 | 0.0180 (*) |
| Liver | 0.0175 | 0.3504 (ns) |
| Spleen | 0.0584 | 0.0843 (ns) |
| Lung | 0.00001 | 0.9788 (ns) |
| Kidney | 0.0002 | 0.9188 (ns) |
| Testis | 0.1207 | 0.0821 (ns) |
| Serum | 0.0371 | 0.1712 (ns) |
| Virus | Type | Base | SNP | Codon | Feature | Frequency |
|---|---|---|---|---|---|---|
| Carvallo Brain P1 | Mutation | C | A | Q (CAA) @247 K (AAA) | Nucleocapsid protein | 65.88 |
| Mutation | G | A | W (TGG) @250 Stop (TGA) | Nucleocapsid protein | 61.51 | |
| Chicava Brain P1 | Mutation | G | A | N/A | Intergenic | 52.89 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Monticelli, S.R.; Kuehne, A.I.; Bakken, R.R.; Coyne, S.R.; Lewis, K.D.; Raymond, J.L.W.; Zeng, X.; Richardson, J.B.; Lapoint, Z.; Williams, J.L.; et al. Characterization of a STAT-1 Knockout Mouse Model for Machupo Virus Infection and Pathogenesis. Viruses 2025, 17, 996. https://doi.org/10.3390/v17070996
Monticelli SR, Kuehne AI, Bakken RR, Coyne SR, Lewis KD, Raymond JLW, Zeng X, Richardson JB, Lapoint Z, Williams JL, et al. Characterization of a STAT-1 Knockout Mouse Model for Machupo Virus Infection and Pathogenesis. Viruses. 2025; 17(7):996. https://doi.org/10.3390/v17070996
Chicago/Turabian StyleMonticelli, Stephanie R., Ana I. Kuehne, Russell R. Bakken, Susan R. Coyne, Kenise D. Lewis, Jo Lynne W. Raymond, Xiankun Zeng, Joshua B. Richardson, Zebulon Lapoint, Jennifer L. Williams, and et al. 2025. "Characterization of a STAT-1 Knockout Mouse Model for Machupo Virus Infection and Pathogenesis" Viruses 17, no. 7: 996. https://doi.org/10.3390/v17070996
APA StyleMonticelli, S. R., Kuehne, A. I., Bakken, R. R., Coyne, S. R., Lewis, K. D., Raymond, J. L. W., Zeng, X., Richardson, J. B., Lapoint, Z., Williams, J. L., Stefan, C. P., Kugelman, J. R., Koehler, J. W., & Herbert, A. S. (2025). Characterization of a STAT-1 Knockout Mouse Model for Machupo Virus Infection and Pathogenesis. Viruses, 17(7), 996. https://doi.org/10.3390/v17070996







