Development of a Mass Antiviral Screening System Using Viral Hemorrhagic Septicemia Virus as an RNA Surrogate and Activity Confirmation with a Fish Rhabdovirus
Abstract
1. Introduction
2. Materials and Methods
2.1. Cells and Virus
2.2. Measurement of Virus Titer
2.3. Exploration of eGFP Fluorescence Wavelength
2.4. Optimal MOI and Culture Conditions for Screening
2.5. Screening
2.5.1. Substances for Screening
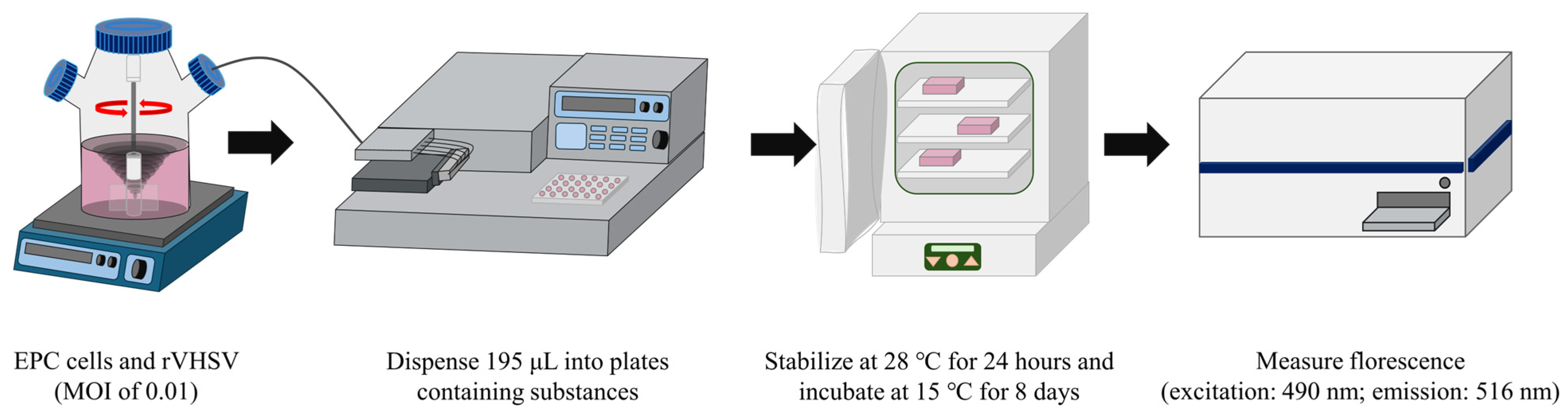
2.5.2. Screening Procedures
2.6. Second-Round Screening of Selected Substances
2.7. CC50 of the Final Candidate
2.8. Determination of the IC50 of the Final Candidate Against rVHSV
2.9. Evaluation of Snakehead Virus
3. Results
3.1. Optimization of Fluorescence Wavelengths for rVHSV-eGFP
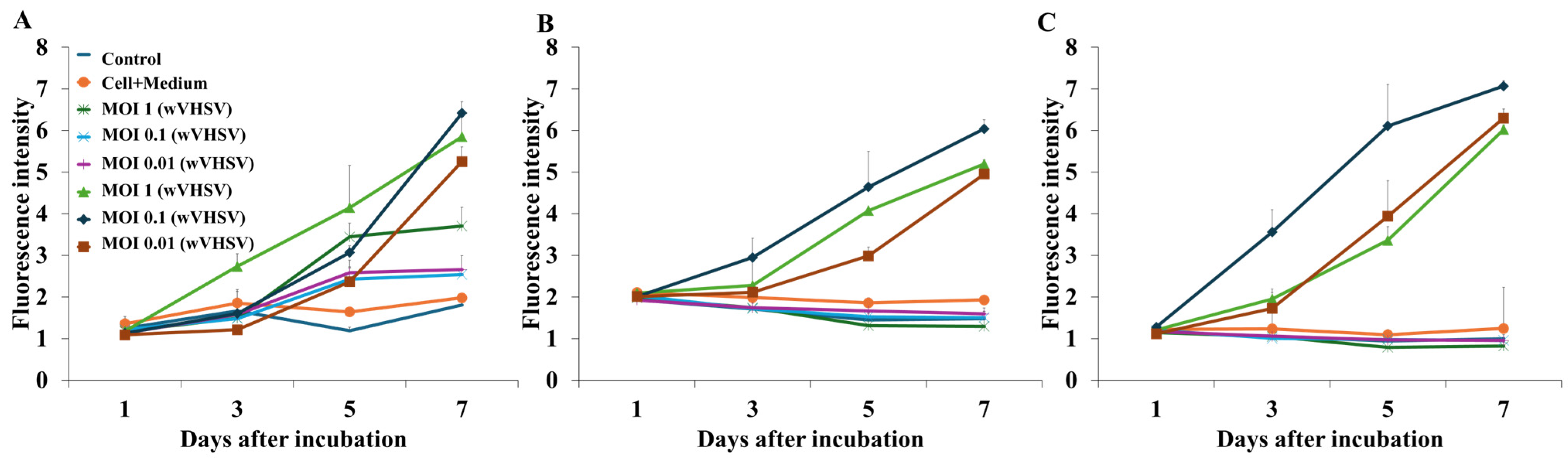
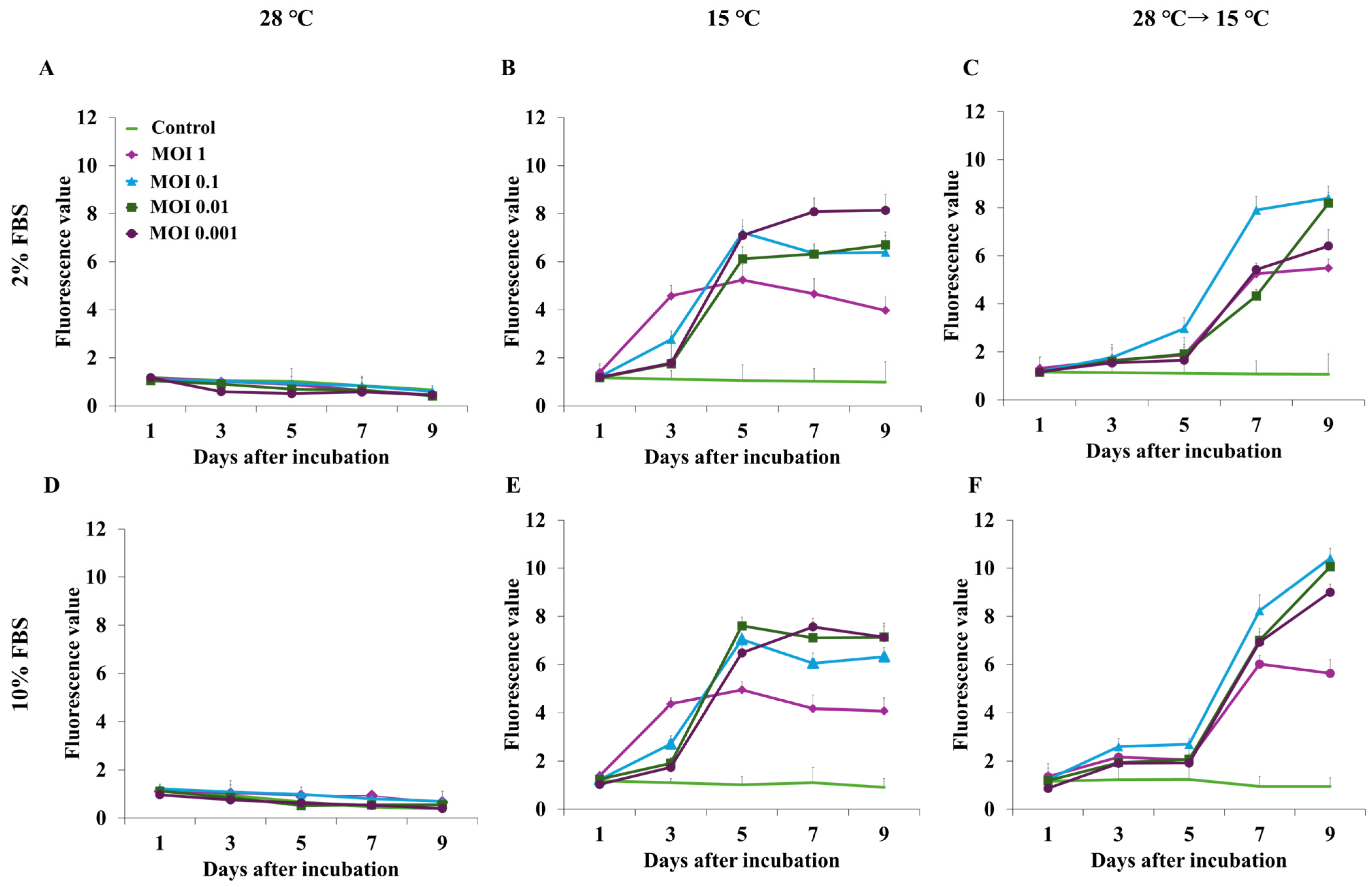
3.2. Optimization of MOI, Temperature, and FBS Concentration for Screening
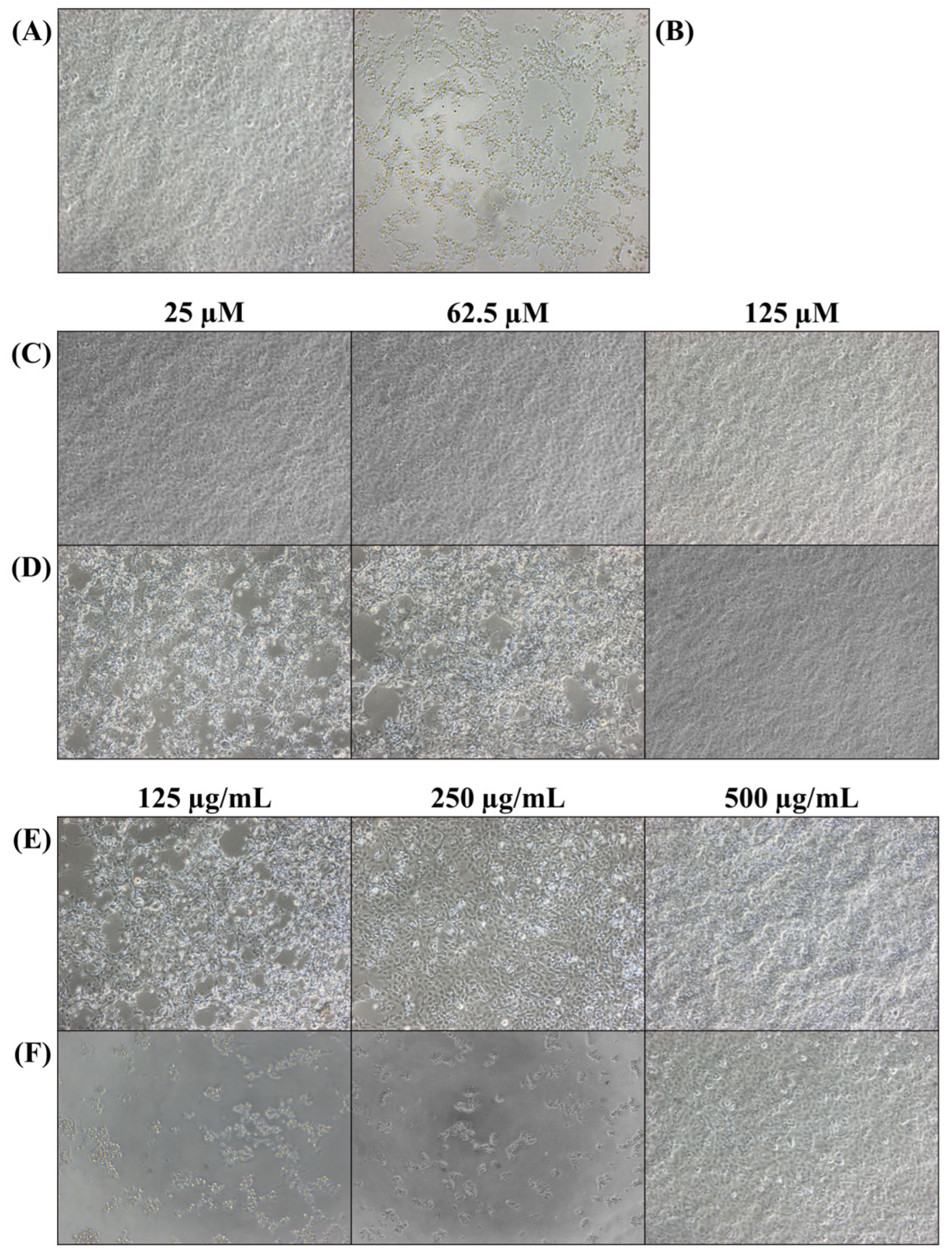
3.3. Screening of Antiviral Substances
3.4. Second-Round Screening
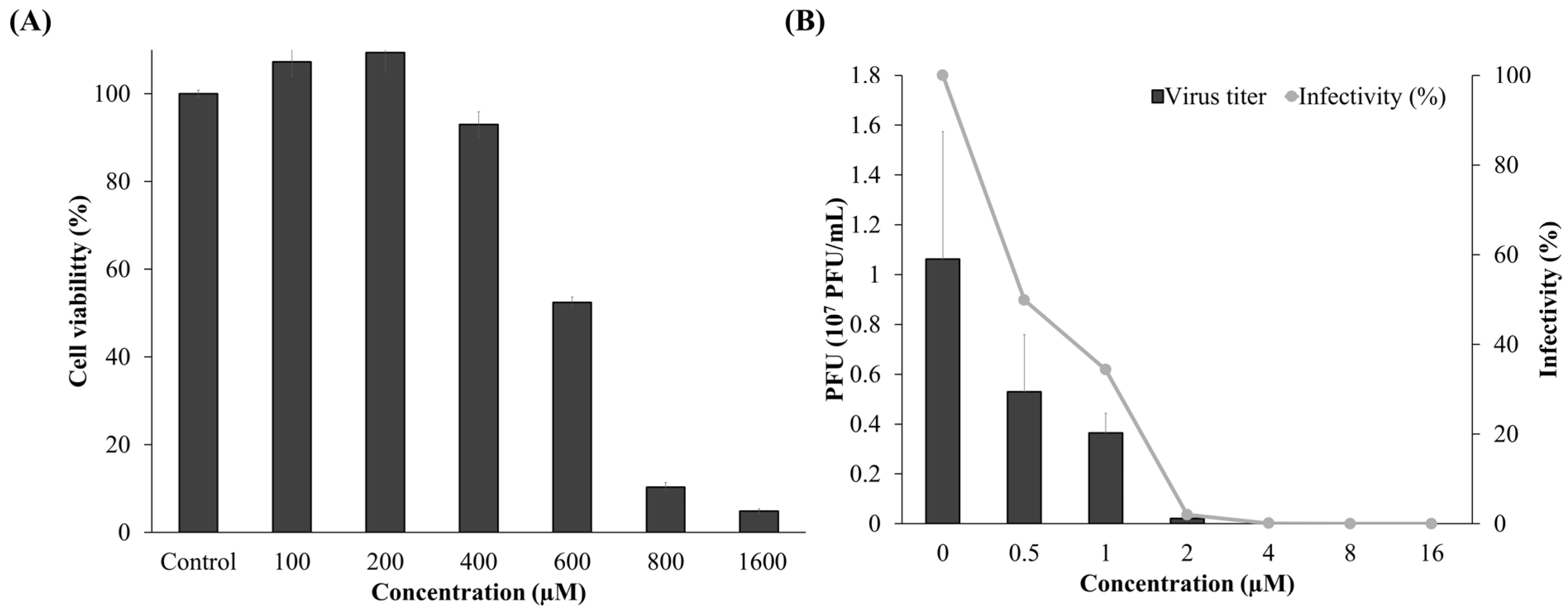
3.5. Cytotoxicity and Antiviral Activity of Compound 3
3.6. Antiviral Activity Against SHRV
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mehle, A.; Dugan, V.G.; Taubenberger, J.K.; Doudna, J.A. Reassortment and Mutation of the Avian Influenza Virus Polymerase PA Subunit Overcome Species Barriers. J. Virol. 2012, 86, 1750–1757. [Google Scholar] [CrossRef]
- Duffy, S. Why are RNA virus mutation rates so damn high? PLoS Biol. 2018, 16, e3000003. [Google Scholar] [CrossRef] [PubMed]
- Jones, B.A.; Grace, D.; Kock, R.; Alonso, S.; Rushton, J.; Said, M.Y.; McKeever, D.; Mutua, F.; Young, J.; McDermott, J.; et al. Zoonosis emergence linked to agricultural intensification and environmental change. Proc. Natl. Acad. Sci. USA 2013, 110, 8399–8404. [Google Scholar] [CrossRef]
- Han, B.A.; Kramer, A.M.; Drake, J.M. Global Patterns of Zoonotic Disease in Mammals. Trends Parasitol. 2016, 32, 565–577. [Google Scholar] [CrossRef]
- Takeuchi, O.; Akira, S. Innate immunity to virus infection. Immunol. Rev. 2009, 227, 75–86. [Google Scholar] [CrossRef] [PubMed]
- Adamson, C.S.; Chibale, K.; Goss, R.J.; Jaspars, M.; Newman, D.J.; Dorrington, R.A. Antiviral drug discovery: Preparing for the next pandemic. Chem. Soc. Rev. 2021, 50, 3647–3655. [Google Scholar] [CrossRef]
- Andrei, G. Vaccines and Antivirals: Grand Challenges and Great Opportunities. Front. Virol. 2021, 1, 666548. [Google Scholar] [CrossRef]
- Kausar, S.; Said Khan, F.; Ishaq Mujeeb Ur Rehman, M.; Akram, M.; Riaz, M.; Rasool, G.; Hamid Khan, A.; Saleem, I.; Shamim, S.; Malik, A. A review: Mechanism of action of antiviral drugs. Int. J. Immunopathol. Pharmacol. 2021, 35, 20587384211002621. [Google Scholar] [CrossRef]
- Clercq, E.D.; Li, G. Approved Antiviral Drugs over the Past 50 Years. Clin. Microbiol. Rev. 2016, 29, 695–747. [Google Scholar] [CrossRef] [PubMed]
- Du, R.; Achi, J.G.; Cui, Q.; Rong, L. Paving new roads toward the advancement of broad-spectrum antiviral agents. J. Med. Virol. 2024, 96, e29369. [Google Scholar] [CrossRef]
- Karim, M.; Lo, C.-W.; Einav, S. Preparing for the next viral threat with broad-spectrum antivirals. J. Clin. Investig. 2023, 133, e170236. [Google Scholar] [CrossRef]
- Haniff, H.S.; Tong, Y.; Liu, X.; Chen, J.L.; Suresh, B.M.; Andrews, R.J.; Peterson, J.M.; O’Leary, C.A.; Benhamou, R.I.; Moss, W.N.; et al. Targeting the SARS-CoV-2 RNA Genome with Small Molecule Binders and Ribonuclease Targeting Chimera (RIBOTAC) Degraders. ACS Cent. Sci. 2020, 6, 1713–1721. [Google Scholar] [CrossRef]
- Jeon, S.; Ko, M.; Lee, J.; Choi, I.; Byun, S.Y.; Park, S.; Shum, D.; Kim, S. Identification of Antiviral Drug Candidates against SARS-CoV-2 from FDA-Approved Drugs. Antimicrob. Agents Chemother. 2020, 64, e00819–e00820. [Google Scholar] [CrossRef]
- Ramirez, D.M.B.; Lara, S.J.P. Technological platforms used for the screening of new antiviral drugs. Int. J. Biosen. Bioelectron. 2018, 4, 42–43. [Google Scholar] [CrossRef]
- Yin, Y.; Xu, Y.; Ou, Z.; Yang, X.; Liu, H. An antiviral drug screening system for enterovirus 71 based on an improved plaque assay: A potential high-throughput method. J. Med. Virol. 2019, 91, 1440–1447. [Google Scholar] [CrossRef]
- Zhang, Z.-R.; Zhang, H.-Q.; Li, X.-D.; Deng, C.-L.; Wang, Z.; Li, J.-Q.; Li, N.; Zhang, Q.-Y.; Zhang, H.-L.; Zhang, B.; et al. Generation and characterization of Japanese encephalitis virus expressing GFP reporter gene for high throughput drug screening. Antivir. Res. 2020, 182, 104884. [Google Scholar] [CrossRef] [PubMed]
- Rothan, H.A.; Teoh, T.C. Cell-Based High-Throughput Screening Protocol for Discovering Antiviral Inhibitors Against SARS-COV-2 Main Protease (3CLpro). Mol. Biotechnol. 2021, 63, 240–248. [Google Scholar] [CrossRef] [PubMed]
- Kaufer, A.M.; Theis, T.; Lau, K.A.; Gray, J.L.; Rawlinson, W.D. Laboratory biosafety measures involving SARS-CoV-2 and the classification as a Risk Group 3 biological agent. Pathology 2020, 52, 790–795. [Google Scholar] [CrossRef]
- Aquino de Carvalho, N.; Stachler, E.N.; Cimabue, N.; Bibby, K. Evaluation of Phi6 Persistence and Suitability as an Enveloped Virus Surrogate. Environ. Sci. Technol. 2017, 51, 8692–8700. [Google Scholar] [CrossRef] [PubMed]
- Feroz, H.; Cetnar, D.; Hewlett, R.; Sharma, S.; Holstein, M.; Ghose, S.; Li, Z.J. Surrogate model to screen for inactivation-based clearance of enveloped viruses during biotherapeutics process development. Biotechnol. J. 2021, 16, 2100176. [Google Scholar] [CrossRef] [PubMed]
- Buckwold, V.E.; Beer, B.E.; Donis, R.O. Bovine viral diarrhea virus as a surrogate model of hepatitis C virus for the evaluation of antiviral agents. Antivir. Res. 2003, 60, 1–15. [Google Scholar] [CrossRef]
- Debing, Y.; Winton, J.; Neyts, J.; Dallmeier, K. Cutthroat trout virus as a surrogate in vitro infection model for testing inhibitors of hepatitis E virus replication. Antivir. Res. 2013, 100, 98–101. [Google Scholar] [CrossRef]
- Jensen, M.H. Research on the virus of Egtved disease. Ann. N. Y. Acad. Sci. 1965, 126, 422–426. [Google Scholar] [CrossRef]
- Mortensen, H.F.; Heuer, O.E.; Lorenzen, N.; Otte, L.; Olesen, N.J. Isolation of viral haemorrhagic septicaemia virus (VHSV) from wild marine fish species in the Baltic Sea, Kattegat, Skagerrak and the North Sea. Virus Res. 1999, 63, 95–106. [Google Scholar] [CrossRef]
- Takano, R.; Nishizawa, T.; Arimoto, M.; Muroga, K. Isolation of viral haemorrhagic septicaemia virus (VHSV) from wild Japanese flounder, Paralichthys olivaceus. Bull.-Eur. Assoc. Fish Pathol. 2000, 20, 186–192. [Google Scholar]
- Hedrick, R.P.; Batts, W.N.; Yun, S.; Traxler, G.S.; Kaufman, J.; Winton, J.R. Host and geographic range extensions of the North American strain of viral hemorrhagic septicemia virus. Dis. Aquat. Org. 2003, 55, 211–220. [Google Scholar] [CrossRef]
- Skall, H.F.; Olesen, N.J.; Mellergaard, S. Viral haemorrhagic septicaemia virus in marine fish and its implications for fish farming—A review. J. Fish Dis. 2005, 28, 509–529. [Google Scholar] [CrossRef]
- Dietzgen, R.G.; Kondo, H.; Goodin, M.M.; Kurath, G.; Vasilakis, N. The family Rhabdoviridae: Mono- and bipartite negative-sense RNA viruses with diverse genome organization and common evolutionary origins. Virus Res. 2017, 227, 158–170. [Google Scholar] [CrossRef] [PubMed]
- Abdellaoui, N.; Kim, S.Y.; Kim, K.H.; Kim, M.S. Effects of Non-Virion Gene Expression Level and Viral Genome Length on the Replication and Pathogenicity of Viral Hemorrhagic Septicemia Virus. Viruses 2022, 14, 1886. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.S.; Choi, S.H.; Kim, K.H. Over-passage of epithelioma papulosum cyprini (EPC) cells increased viral hemorrhagic septicemia virus (VHSV) replication. Fish Shellfish Immunol. 2016, 58, 318–322. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.M.; Kim, D.H.; Kim, K.H. Development of rapid neutralization assay of viral hemorrhagic septicemia virus (VHSV) based on chimeric rhabdovirus expressing heterologous glycoprotein. J. Virol. Methods 2023, 311, 114639. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Gerard, A.L.V.; Huang, B.C.B.; Anderson, D.C.; Payan, D.G.; Luo, Y. Detection of programmed cell death using fluorescence energy transfer. Nucleic Acids Res. 1998, 26, 2034–2035. [Google Scholar] [CrossRef]
- Arpino, J.A.J.; Rizkallah, P.J.; Jones, D.D. Crystal Structure of Enhanced Green Fluorescent Protein to 1.35 Å Resolution Reveals Alternative Conformations for Glu222. PLoS ONE 2012, 7, e47132. [Google Scholar] [CrossRef]
- Kim, S.Y.; Kim, J.Y.; Kim, H.J.; Kim, M.S.; Kim, K.H. Protection of rainbow trout (Oncorhynchus mykiss) against VHSV genotype Ia and IHNV by immunization with VHSV genotype IVa backbone-based single-cycle viruses. Fish Shellfish Immunol. 2023, 132, 108476. [Google Scholar] [CrossRef]
- Kim, M.S.; Kim, D.S.; Kim, K.H. Generation and characterization of NV gene-knockout recombinant viral hemorrhagic septicemia virus (VHSV) genotype IVa. Dis. Aquat. Org. 2011, 97, 25–35. [Google Scholar] [CrossRef][Green Version]
- Choi, M.G.; Kim, K.H. In vitro and in vivo infection of snakehead rhabdovirus (SHRV) and recombinant chimeric SHRVs in Penaeus vannamei to evaluate availability as a vector for heterologous protein expression. Fish Shellfish Immunol. 2025, 161, 110280. [Google Scholar] [CrossRef] [PubMed]
- Sebaugh, J.L. Guidelines for accurate EC50/IC50 estimation. Pharm. Stat. 2011, 10, 128–134. [Google Scholar] [CrossRef]
- Kustin, T.; Stern, A. Biased Mutation and Selection in RNA Viruses. Mol. Biol. Evol. 2020, 38, 575–588. [Google Scholar] [CrossRef]
- Grubaugh, N.D.; Ladner, J.T.; Lemey, P.; Pybus, O.G.; Rambaut, A.; Holmes, E.C.; Andersen, K.G. Tracking virus outbreaks in the twenty-first century. Nat. Microbiol. 2019, 4, 10–19. [Google Scholar] [CrossRef]
- Lü, Z.; Dai, X.; Xu, J.; Liu, Z.; Guo, Y.; Gao, Z.; Meng, F. Medicinal chemistry strategies toward broad-spectrum antiviral agents to prevent next pandemics. Eur. J. Med. Chem. 2024, 271, 116442. [Google Scholar] [CrossRef] [PubMed]
- Martis, E.A.; Radhakrishnan, R.; Badve, R.R. High-Throughput Screening: The Hits and Leads of Drug Discovery—An Overview. J. Appl. Pharm. Sci. 2011, 1, 2–10. [Google Scholar]
- Zang, R.; Li, D.; Tang, I.-C.; Wang, J.; Yang, S.-T. Cell-based assays in high-throughput screening for drug discovery. Int. J. Biotechnol. Wellness Ind. 2012, 1, 31. [Google Scholar]
- Li, X.; Zhang, H.; Zhang, Y.; Li, J.; Wang, Z.; Deng, C.; Jardim, A.C.G.; Terzian, A.C.B.; Nogueira, M.L.; Zhang, B. Development of a rapid antiviral screening assay based on eGFP reporter virus of Mayaro virus. Antivir. Res. 2019, 168, 82–90. [Google Scholar] [CrossRef]
- Li, W.; Zhang, M.; Zheng, H.; Zhou, P.; Liu, Z.; Jongkaewwattana, A.; Luo, R.; He, Q. Construction of a Recombinant Porcine Epidemic Diarrhea Virus Encoding Nanoluciferase for High-Throughput Screening of Natural Antiviral Products. Viruses 2021, 13, 1866. [Google Scholar] [CrossRef]
- Shi, Y.-J.; Li, J.-Q.; Zhang, H.-Q.; Deng, C.-L.; Zhu, Q.-X.; Zhang, B.; Li, X.-D. A high throughput antiviral screening platform for alphaviruses based on Semliki Forest virus expressing eGFP reporter gene. Virol. Sin. 2023, 38, 585–594. [Google Scholar] [CrossRef]
- Vandemaele, L.; Francken, T.; Schepers, J.; Chiu, W.; Cremers, N.; Klaassen, H.; Marcadet, C.; Felipe, L.S.; Marchand, A.; Chaltin, P.; et al. High-throughput split-GFP antiviral screening assay against fusogenic paramyxoviruses. Antivir. Res. 2025, 241, 106242. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.-C.; Sood, C.; Francis, A.C.; Melikyan, G.B.; Dickson, R.M. Facile autofluorescence suppression enabling tracking of single viruses in live cells. J. Biol. Chem. 2019, 294, 19111–19118. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.-Z.; Xu, L.-M.; Liu, M.; Zhang, Z.-y.; Yin, J.-S.; Liu, H.-B.; Lu, T.-Y. Autophagy induced by infectious hematopoietic necrosis virus inhibits intracellular viral replication and extracellular viral yields in epithelioma papulosum cyprini cell line. Dev. Comp. Immunol. 2017, 77, 88–94. [Google Scholar] [CrossRef]
- Kim, M.S.; Kim, K.H. Effect of CRISPR/Cas9-mediated knockout of either Mx1 or ISG15 gene in EPC cells on resistance against VHSV infection. Fish Shellfish Immunol. 2019, 93, 1041–1046. [Google Scholar] [CrossRef] [PubMed]
- Rüdiger, D.; Kupke, S.Y.; Laske, T.; Zmora, P.; Reichl, U. Multiscale modeling of influenza A virus replication in cell cultures predicts infection dynamics for highly different infection conditions. PLOS Comput. Biol. 2019, 15, e1006819. [Google Scholar] [CrossRef]
- Rahpeyma, M.; Bashar, R. Evaluation of Multiplicity of Infection (MOI) and Harvesting Time on the Production of CVS-11 Strain of Rabies Virus in BSR Cell Line. J. Med. Microbiol. Infect. Dis. 2021, 9, 25–31. [Google Scholar] [CrossRef]
- Fijan, N.; Sulimanović, D.; Bearzotti, M.; Muzinić, D.; Zwillenberg, L.O.; Chilmonczyk, S.; Vautherot, J.F.; de Kinkelin, P. Some properties of the Epithelioma papulosum cyprini (EPC) cell line from carp cyprinus carpio. Ann. De L’institut Pasteur Virol. 1983, 134, 207–220. [Google Scholar] [CrossRef]
- Eckhardt, D.; Mueller, J.; Friedrich, J.; Klee, J.-P.; Sardlishvili, I.; Walter, L.E.; Fey, S.; Czermak, P.; Salzig, D. Production of Oncolytic Measles Virus in Vero Cells: Impact of Culture Medium and Multiplicity of Infection. Viruses 2024, 16, 1740. [Google Scholar] [CrossRef] [PubMed]
- Zhang, N.; Liu, Z.; Han, Q.; Chen, J.; Lv, Y. Xanthohumol enhances antiviral effect of interferon α-2b against bovine viral diarrhea virus, a surrogate of hepatitis C virus. Phytomedicine 2010, 17, 310–316. [Google Scholar] [CrossRef] [PubMed]
- Aboubakr, H.A.; Nauertz, A.; Luong, N.T.; Agrawal, S.; El-Sohaimy, S.A.A.; Youssef, M.M.; Goyal, S.M. In Vitro Antiviral Activity of Clove and Ginger Aqueous Extracts against Feline Calicivirus, a Surrogate for Human Norovirus. J. Food Prot. 2016, 79, 1001–1012. [Google Scholar] [CrossRef]
- Basyouni, W.M.; Abbas, S.Y.; El-Bayouki, K.A.M.; Daawod, R.M.; Elawady, M.K. Synthesis and antiviral evaluation of 5-(arylazo)salicylaldehyde thiosemicarbazone derivatives as potent anti-bovine viral diarrhea virus agents. Synth. Commun. 2021, 51, 2168–2174. [Google Scholar] [CrossRef]
- Wang, J.; Ji, J.; Zhong, Y.; Meng, W.; Wan, S.; Ding, X.; Chen, Z.; Wu, W.; Jia, K.; Li, S. Construction of recombinant fluorescent LSDV for high-throughput screening of antiviral drugs. Vet. Res. 2024, 55, 33. [Google Scholar] [CrossRef]
- Sacramento, C.Q.; Bott, R.; Huang, Q.; Eaton, B.; Postnikova, E.; Sabir, A.J.; Argade, M.D.; Ratia, K.; Anantpadma, M.; Carlier, P.R.; et al. Recombinant Pichinde reporter virus as a safe and suitable surrogate for high-throughput antiviral screening against highly pathogenic arenaviruses. Antivir. Res. 2025, 236, 106117. [Google Scholar] [CrossRef]
- Peng, C.; Zhou, Y.; Cao, S.; Pant, A.; Campos Guerrero, M.L.; McDonald, P.; Roy, A.; Yang, Z. Identification of Vaccinia Virus Inhibitors and Cellular Functions Necessary for Efficient Viral Replication by Screening Bioactives and FDA-Approved Drugs. Vaccines 2020, 8, 401. [Google Scholar] [CrossRef]
- Kumar Verma, S.; Verma, R.; Xue, F.; Kumar Thakur, P.; Girish, Y.R.; Rakesh, K.P. Antibacterial activities of sulfonyl or sulfonamide containing heterocyclic derivatives and its structure-activity relationships (SAR) studies: A critical review. Bioorg. Chem. 2020, 105, 104400. [Google Scholar] [CrossRef]
- Negi, M.; Chawla, P.A.; Faruk, A.; Chawla, V. Role of heterocyclic compounds in SARS and SARS CoV-2 pandemic. Bioorg. Chem. 2020, 104, 104315. [Google Scholar] [CrossRef]
- dos Santos, G.C.; Martins, L.M.; Bregadiolli, B.A.; Moreno, V.F.; da Silva-Filho, L.C.; da Silva, B.H.S.T. Heterocyclic compounds as antiviral drugs: Synthesis, structure–activity relationship and traditional applications. J. Heterocycl. Chem. 2021, 58, 2226–2260. [Google Scholar] [CrossRef]
- Sharma, S.; Utreja, D. Synthesis and antiviral activity of diverse heterocyclic scaffolds. Chem. Biol. Drug Des. 2022, 100, 870–920. [Google Scholar] [CrossRef]
- Kim, H.J.; Kwon, S.R.; Olesen, N.J.; Cuenca, A. Development of a novel real-time RT-PCR method using peptide nucleic acid (PNA) probes for detecting and genotyping of viral haemorrhagic septicaemia virus (VHSV). Aquaculture 2023, 570, 739408. [Google Scholar] [CrossRef]
- Bilal, A. Rabies is a zoonotic disease: A literature review. Occup. Med. Health Aff. 2021, 9, 334. [Google Scholar]
- Mohammadisefat, P.; Zorriehzahra, M.J.; Adel, M.; Chamjangali, Z.A.; Jabbari, M.; Eftekhari, A.; Farzipour, H.; Jazi, S.Y. Viral hemorrhagic septicemia virus (VHSV), past, present and future: A review. Int. Aquat. Res. 2023, 15, 191–203. [Google Scholar] [CrossRef]
- Jeong, E.-H.; Vaidya, B.; Cho, S.-Y.; Park, M.-A.; Kaewintajuk, K.; Kim, S.R.; Oh, M.-J.; Choi, J.-S.; Kwon, J.; Kim, D. Identification of regulators of the early stage of viral hemorrhagic septicemia virus infection during curcumin treatment. Fish Shellfish Immunol. 2015, 45, 184–193. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.J.; Moon, C.; Kang, J.-H.; Choi, T.-J. Antiviral effects of extracts from Celosia cristata and Raphanus sativus roots against viral hemorrhagic septicemia virus. Arch. Virol. 2017, 162, 1711–1716. [Google Scholar] [CrossRef]
- Baek, E.J.; Kim, M.J.; Kim, K.I. In vitro and in vivo evaluation of the antiviral activity of arctigenin, ribavirin, and ivermectin against viral hemorrhagic septicemia virus infection. Fish Shellfish Immunol. 2023, 132, 108456. [Google Scholar] [CrossRef] [PubMed]
- Mendis, W.R.H.; Lim, J.-W.; Kim, G.-W.; Kang, S.Y. Antiviral activity of the coumarin derivative scoparone against viral hemorrhagic septicemia virus in vitro and in the olive flounder Paralichthys olivaceus. Aquaculture 2024, 585, 740703. [Google Scholar] [CrossRef]
- Choi, H.-J.; Hong, S.-C.; Kim, J.-H.; Kang, Y.J. Antiviral effects of remdesivir on fish viruses from the Rhabdoviridae family. Aquaculture 2025, 609, 742770. [Google Scholar] [CrossRef]
- Kang, S.Y.; Kang, J.-Y.; Oh, M.-J. Antiviral activities of flavonoids isolated from the bark of Rhus verniciflua stokes against fish pathogenic viruses In Vitro. J. Microbiol. 2012, 50, 293–300. [Google Scholar] [CrossRef] [PubMed]
- Micol, V.; Caturla, N.; Pérez-Fons, L.; Más, V.; Pérez, L.; Estepa, A. The olive leaf extract exhibits antiviral activity against viral haemorrhagic septicaemia rhabdovirus (VHSV). Antivir. Res. 2005, 66, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.Y.; Bessaid, M.; Lee, K.M.; Kim, K.H. Chimeric snakehead rhabdoviruses and zebrafish as a model system for investigating the role of fish rhabdoviral glycoproteins in in vivo virulence. J. Virol. Methods 2025, 338, 115232. [Google Scholar] [CrossRef] [PubMed]
- Bisht, K.; Velthuis, A.J.W.t. Decoding the Role of Temperature in RNA Virus Infections. mBio 2022, 13, e02021–e02022. [Google Scholar] [CrossRef]
- Office International des Épizooties. Manual of Diagnostic Tests for Aquatic Animals, 4th ed.; Paris Office International des Épizooties: Paris, France, 2003; pp. 259–272. ISBN 92-9044-563-7. [Google Scholar]

| No. | Excitation Wavelength (nm) | Emission Wavelength (nm) |
|---|---|---|
| 1 | 488 | 511 |
| 2 | 480 | 520 |
| 3 | 490 | 516 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shin, J.W.; Kim, S.Y.; Kim, M.J.; Lee, T.-K.; Choi, T.-J. Development of a Mass Antiviral Screening System Using Viral Hemorrhagic Septicemia Virus as an RNA Surrogate and Activity Confirmation with a Fish Rhabdovirus. Viruses 2025, 17, 1522. https://doi.org/10.3390/v17111522
Shin JW, Kim SY, Kim MJ, Lee T-K, Choi T-J. Development of a Mass Antiviral Screening System Using Viral Hemorrhagic Septicemia Virus as an RNA Surrogate and Activity Confirmation with a Fish Rhabdovirus. Viruses. 2025; 17(11):1522. https://doi.org/10.3390/v17111522
Chicago/Turabian StyleShin, Ji Woo, Su Yeon Kim, Min Jeong Kim, Taek-Kyun Lee, and Tae-Jin Choi. 2025. "Development of a Mass Antiviral Screening System Using Viral Hemorrhagic Septicemia Virus as an RNA Surrogate and Activity Confirmation with a Fish Rhabdovirus" Viruses 17, no. 11: 1522. https://doi.org/10.3390/v17111522
APA StyleShin, J. W., Kim, S. Y., Kim, M. J., Lee, T.-K., & Choi, T.-J. (2025). Development of a Mass Antiviral Screening System Using Viral Hemorrhagic Septicemia Virus as an RNA Surrogate and Activity Confirmation with a Fish Rhabdovirus. Viruses, 17(11), 1522. https://doi.org/10.3390/v17111522








