Clinical Characteristics and Outcomes of Pediatric COVID-19 Pneumonia Treated with Favipiravir in a Tertiary Care Center
Abstract
1. Introduction
2. Materials and Methods
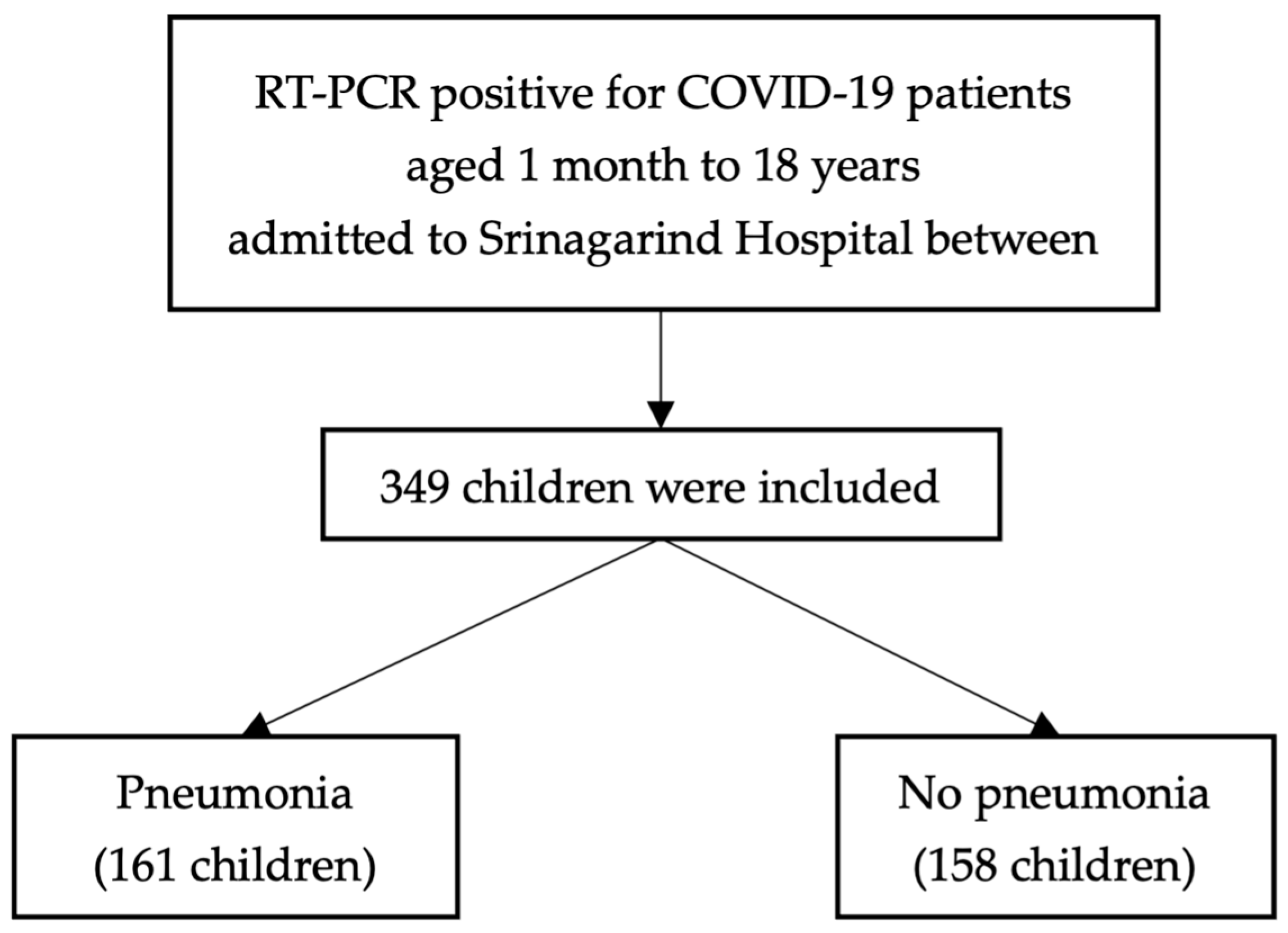
2.1. Study Design and Participants
2.2. Data Collections
2.3. Ethical Consideration
2.4. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wong, J.J.M.; Abbas, Q.; Chuah, S.L.; Malisie, R.F.; Pon, K.M.; Katsuta, T.; Dang, H.; Lee, P.C.; Jayashree, M.; Sultana, R.; et al. Comparative Analysis of Pediatric COVID-19 Infection in Southeast Asia, South Asia, Japan, and China. Am. J. Trop. Med. Hyg. 2021, 105, 413–420. [Google Scholar] [CrossRef] [PubMed]
- Satdhabudha, A.; Chaiyakulsil, C.; Uppala, R.; Niyomkarn, W.; Tovichien, P.; Norasettekul, V.; Ruangnapa, K.; Smathakanee, C.; Choursamran, B.; Kulbun, A.; et al. Development and Validation of the Predictive Score for Pediatric COVID-19 Pneumonia: A Nationwide, Multicenter Study. PLoS ONE 2022, 17, e0273842. [Google Scholar] [CrossRef] [PubMed]
- Uppala, R.; Sitthikarnkha, P.; Niamsanit, S.; Sutra, S.; Thepsuthammarat, K.; Techasatian, L.; Anantasit, N.; Teeratakulpisarn, J. Effect of the COVID-19 Pandemic on Lower Respiratory Tract Infection Determinants in Thai Hospitalized Children: National Data Analysis 2015–2020. Trop. Med. Infect. Dis. 2022, 7, 151. [Google Scholar] [CrossRef] [PubMed]
- Anugulruengkitt, S.; Teeraananchai, S.; Chantasrisawad, N.; Promsena, P.; Jantarabenjakul, W.; Puthanakit, T. Clinical Outcomes of Pediatric COVID-19 in a Tertiary Care Center in Bangkok, Thailand. IJID Reg. 2021, 1, 159–162. [Google Scholar] [CrossRef] [PubMed]
- Bolaños-Almeida, C.E.; Espitia Segura, O.M. Clinical and Epidemiologic Analysis of COVID-19 Children Cases in Colombia PEDIACOVID. Pediatr. Infect. Dis. J. 2021, 40, e7. [Google Scholar] [CrossRef] [PubMed]
- Böncüoğlu, E.; Coşkun, M.; Kıymet, E.; Öztürk Atasoy, T.; Şahinkaya, Ş.; Cem, E.; Düzgöl, M.; Yılmaz Çelebi, M.; Akaslan Kara, A.; Arıkan, K.Ö.; et al. Can Laboratory Findings Predict Pulmonary Involvement in Children with COVID-19 Infection? Pediatr. Pulmonol. 2021, 56, 2489–2494. [Google Scholar] [CrossRef] [PubMed]
- Department of Medical Services, Ministry of Public Health. COVID-19 CPG for Healthcare Workers. Available online: https://ddc.moph.go.th/viralpneumonia/eng/file/guidelines/g_CPG_22Mar22.pdf. (accessed on 24 April 2024).
- Lisson, Y.; Marmor, A.; Gomez, A.; Hall, R.; Parry, A.E.; Wright, R.; Lal, A. Cohorting Children in a Childcare Setting: A Strategy to Reduce SARS-CoV-2 Delta Transmission, August–September 2021. Commun. Dis. Intell. 2023, 47, 1–17. [Google Scholar] [CrossRef]
- Badal, S.; Thapa Bajgain, K.; Badal, S.; Thapa, R.; Bajgain, B.B.; Santana, M.J. Prevalence, Clinical Characteristics, and Outcomes of Pediatric COVID-19: A Systematic Review and Meta-Analysis. J. Clin. Virol. 2021, 135, 104715. [Google Scholar] [CrossRef] [PubMed]
- Özger, H.S.; Aysert Yıldız, P.; Gaygısız, Ü.; Uğraş Dikmen, A.; Demirbaş Gülmez, Z.; Yıldız, M.; Şenol, E.; Hizel, K.; Güzel Tunçcan, Ö.; Çağlar, K.; et al. The Factors Predicting Pneumonia in COVID-19 Patients: Preliminary Results from a University Hospital in Turkey. Turk. J. Med. Sci. 2020, 50, 1810–1816. [Google Scholar] [CrossRef]
- Porto, L.C.; Costa, C.H.; Nunes, A.S.; Bouzas, I.; Ferreira, T.F.; Porto, V.M.; Secco, D.A.; Vilas Boas, S.; Faria, A.C.; Rufino, R.; et al. Clinical and Laboratory Characteristics in Outpatient Diagnosis of COVID-19 in Healthcare Professionals in Rio de Janeiro, Brazil. J. Clin. Pathol. 2022, 75, 185–192. [Google Scholar] [CrossRef] [PubMed]
- McGonagle, D.; Sharif, K.; O’Regan, A.; Bridgewood, C. The Role of Cytokines Including Interleukin-6 in COVID-19 Induced Pneumonia and Macrophage Activation Syndrome-Like Disease. Autoimmun. Rev. 2020, 19, 102537. [Google Scholar] [CrossRef]
- Zhang, Y.; Wang, S.; Xia, H.; Guo, J.; He, K.; Huang, C.; Luo, R.; Chen, Y.; Xu, K.; Gao, H.; et al. Identification of Monocytes Associated with Severe COVID-19 in the PBMCs of Severely Infected Patients Through Single-Cell Transcriptome Sequencing. Engineering 2022, 17, 161–169. [Google Scholar] [CrossRef] [PubMed]
- Xie, Y.; Yu, Y.; Zhao, L.; Ning, P.; Luo, Q.; Zhang, Y.; Yin, L.; Zheng, Y.; Gao, Z. Specific Cytokine Profiles Predict the Severity of Influenza A Pneumonia: A Prospectively Multicenter Pilot Study. Biomed. Res. Int. 2021, 2021, 9533044. [Google Scholar] [CrossRef] [PubMed]
- Vangeti, S.; Falck-Jones, S.; Yu, M.; Österberg, B.; Liu, S.; Asghar, M.; Sondén, K.; Paterson, C.; Whitley, P.; Albert, J.; et al. Human Influenza Virus Infection Elicits Distinct Patterns of Monocyte and Dendritic Cell Mobilization in Blood and the Nasopharynx. eLife 2023, 12, e77345. [Google Scholar] [CrossRef] [PubMed]
- Hensel, M.; Grädel, L.; Kutz, A.; Haubitz, S.; Huber, A.; Mueller, B.; Schuetz, P.; Hügle, T. Peripheral Monocytosis as a Predictive Factor for Adverse Outcome in the Emergency Department: Survey Based on a Register Study. Medicine 2017, 96, e7404. [Google Scholar] [CrossRef] [PubMed]
- Rajamanickam, A.; Kumar, N.P.; Pandiarajan, A.N.; Selvaraj, N.; Munisankar, S.; Renji, R.M.; Venkatramani, V.; Murhekar, M.; Thangaraj, J.W.V.; Kumar, M.S.; et al. Dynamic Alterations in Monocyte Numbers, Subset Frequencies and Activation Markers in Acute and Convalescent COVID-19 Individuals. Sci. Rep. 2021, 11, 20254. [Google Scholar] [CrossRef] [PubMed]
- Jiravisitkul, P.; Thonginnetra, S.; Wongvisavavit, R. Case Report: Favipiravir-Induced Bluish Corneal Discoloration in Infant with COVID-19. Front. Pediatr. 2023, 11, 1154814. [Google Scholar] [CrossRef]
- Rafiei Tabatabaei, S.; Moradi, O.; Karimi, A.; Armin, S.; Fahimzad, A.; Mansour Ghanaie, R.; Jamee, M.; Mousavizadeh, A.; Amini, H.; Mirrahimi, B. A Single-Centered Cohort Study on Favipiravir Safety and Efficacy in Pediatric Patients with COVID-19. Iran. J. Pharm. Res. 2022, 21, e127034. [Google Scholar] [CrossRef] [PubMed]
- Getsuwan, S.; Boonsathorn, S.; Chaisavaneeyakorn, S.; Butsriphum, N.; Tanpowpong, P.; Lertudomphonwanit, C.; Treepongkaruna, S. Clinical Manifestations and Outcomes of Coronavirus Disease 2019 among Pediatric Liver Transplant Recipients in the Delta and Omicron Variant Pandemic: A Retrospective Study. Medicine 2023, 102, e35537. [Google Scholar] [CrossRef]
| Variable | Total N = 349 |
|---|---|
| Gender, n (%) | |
| Male | 181 (51.9) |
| Female | 168 (48.1) |
| Age (year), median (IQR) | 8 (3–14) |
| Underlying diseases, n (%) | |
| Chronic lung disease | 30 (11.5) |
| Asthma | 6 (1.7) |
| Allergic rhinitis | 4 (1.1) |
| Congenital cyanotic heart disease | 1 (0.3) |
| Symptoms, n (%) | |
| Fever | 349 (100) |
| Cough | 259 (74.2) |
| Rash | 87 (24.9) |
| Diarrhea | 18 (5.2) |
| Invasive mechanical ventilation, n (%) | 4 (1.6) |
| HHHFNC, n (%) | 7 (2) |
| PICU admission, n (%) | 10 (2.9) |
| Death, n (%) | 1 (0.3) |
| Length of stay (days); median (IQR) | 12 (10–13) |
| Variables | Results |
|---|---|
| CRP-QT (mg/L), median (IQR) | 1 (0.49–4.59) |
| CBC | |
| Hemoglobin (g/dL), median (IQR) | 12.60 (11.60–13.30) |
| Hematocrit | 37.50 (34.90–44.30) |
| White blood cell (cells/µL) | 7940 (5630–9900) |
| Neutrophil %, median (IQR) | 44.50 (28.00–54.20) |
| Lymphocyte %, median (IQR) | 44.00 (35.30–62.00) |
| Monocyte %, median (IQR) | 8.00 (5.80–9.60) |
| Eosinophil %, median (IQR) | 1.20 (0.60–2.70) |
| Basophil %, median (IQR) | 0.20 (0–0.40) |
| Platelet count (cells/µL), median (IQR) | 291,000 (247,000–363,000) |
| Variables | Pneumonia (n = 161) | No Pneumonia (n = 158) | Crude Odds Ratio | 95% CI | p-Value |
|---|---|---|---|---|---|
| Gender | 0.087 | ||||
| male | 107 (56.02) | 74 (46.84) | 1 | ||
| female | 84 (43.98) | 84 (53.16) | 0.69 | 0.45–1.06 | |
| Age (year), median (IQR) | 8 (3–14) | 9 (3–14) | 0.99 | 0.95–1.03 | 0.502 |
| Underlying diseases, n (%) | 27 (14.14) | 14 (8.86) | 1.69 | 0.86–3.35 | 0.124 |
| CRP (mg/L), (IQR) | 1.45 (0.48–6.47) | 1 (0.50–1.85) | 1.24 | 1.10–1.40 | <0.001 |
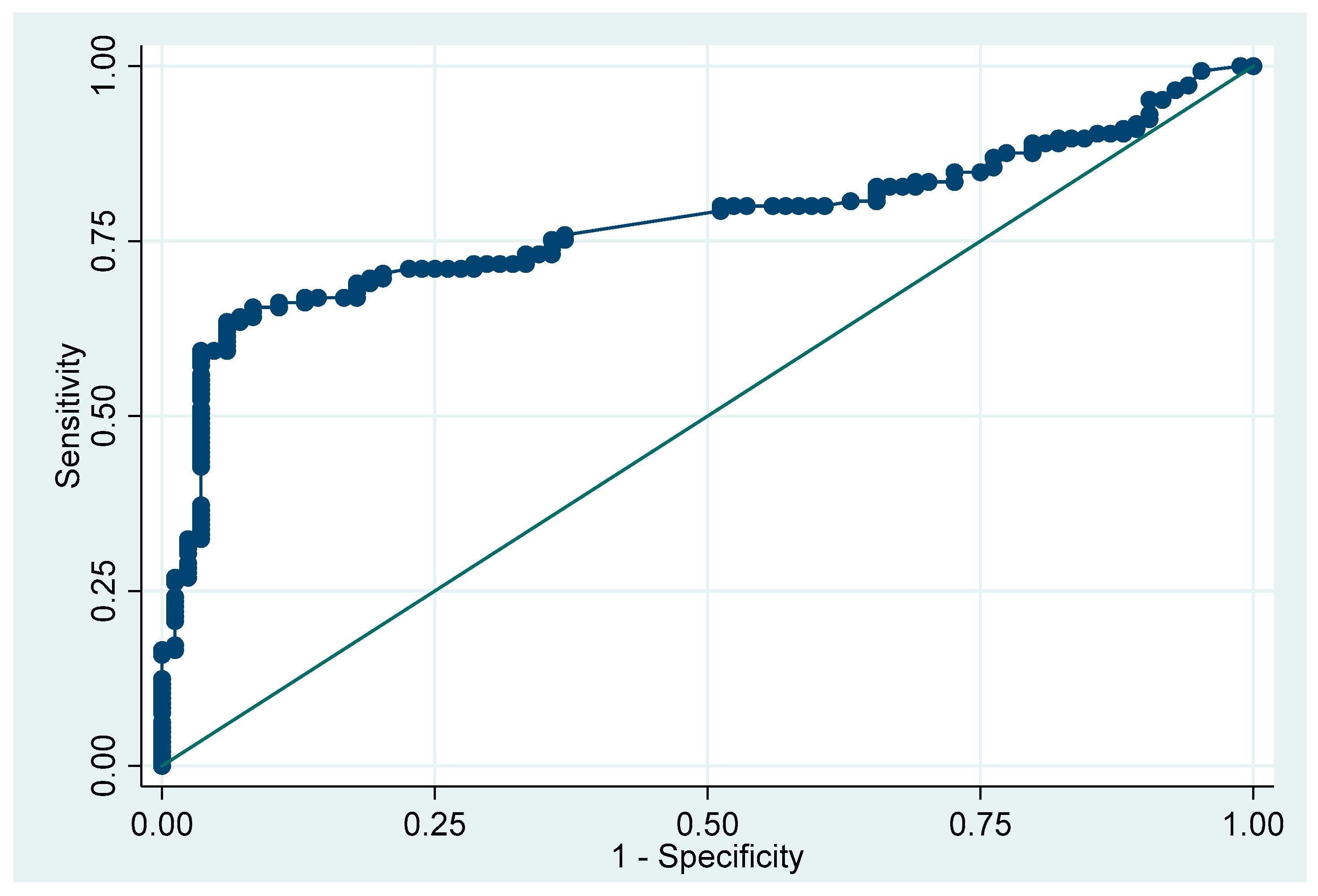
| Monocytosis, n (%) | 85 (58.62) | 3 (3.57) | 38.25 | 11.53–126.84 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sitthikarnkha, P.; Phunyaissaraporn, R.; Niamsanit, S.; Techasatian, L.; Saengnipanthkul, S.; Uppala, R. Clinical Characteristics and Outcomes of Pediatric COVID-19 Pneumonia Treated with Favipiravir in a Tertiary Care Center. Viruses 2024, 16, 946. https://doi.org/10.3390/v16060946
Sitthikarnkha P, Phunyaissaraporn R, Niamsanit S, Techasatian L, Saengnipanthkul S, Uppala R. Clinical Characteristics and Outcomes of Pediatric COVID-19 Pneumonia Treated with Favipiravir in a Tertiary Care Center. Viruses. 2024; 16(6):946. https://doi.org/10.3390/v16060946
Chicago/Turabian StyleSitthikarnkha, Phanthila, Rawisara Phunyaissaraporn, Sirapoom Niamsanit, Leelawadee Techasatian, Suchaorn Saengnipanthkul, and Rattapon Uppala. 2024. "Clinical Characteristics and Outcomes of Pediatric COVID-19 Pneumonia Treated with Favipiravir in a Tertiary Care Center" Viruses 16, no. 6: 946. https://doi.org/10.3390/v16060946
APA StyleSitthikarnkha, P., Phunyaissaraporn, R., Niamsanit, S., Techasatian, L., Saengnipanthkul, S., & Uppala, R. (2024). Clinical Characteristics and Outcomes of Pediatric COVID-19 Pneumonia Treated with Favipiravir in a Tertiary Care Center. Viruses, 16(6), 946. https://doi.org/10.3390/v16060946







