Long-Term Impairment of Working Ability in Subjects under 60 Years of Age Hospitalised for COVID-19 at 2 Years of Follow-Up: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Subjects
2.3. Procedures
2.4. Endpoints
- Impaired working ability compared to pre-COVID-19 period as reported by the participants.
- Predictors or risk factors associated with long-term impairment of working ability in this population, Demographic, clinical, or socio-economic factors that significantly influence the likelihood of long-term working impairment following COVID-19 hospitalization.
- The correlation between comorbidities, the severity of COVID-19 illness during hospitalization, and long-term working ability outcomes.
2.5. Statistical Analysis
2.6. Questionnaires
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Long COVID or Post-COVID Conditions. Cent. Dis. Control Prev. 2022. Available online: https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html (accessed on 4 August 2022).
- Tsuchida, T.; Yoshimura, N.; Ishizuka, K.; Katayama, K.; Inoue, Y.; Hirose, M.; Nakagama, Y.; Kido, Y.; Sugimori, H.; Matsuda, T.; et al. Five cluster classifications of long COVID and their background factors: A cross-sectional study in Japan. Clin. Exp. Med. 2023, 23, 3663–3670. [Google Scholar] [CrossRef]
- International Labour Organization. Available online: https://www.ilo.org/global/publications/books/WCMS_845642/lang--en/index.htm (accessed on 4 August 2022).
- Ladlow, P.; O’Sullivan, O.; Bennett, A.N.; Barker-Davies, R.; Houston, A.; Chamley, R.; May, S.; Mills, D.; Dewson, D.; Rogers-Smith, K.; et al. The effect of medium-term recovery status after COVID-19 illness on cardiopulmonary exercise capacity in a physically active adult population. J. Appl. Physiol. 2022, 132, 1525–1535. [Google Scholar] [CrossRef]
- Lamontagne, S.J.; Winters, M.F.; Pizzagalli, D.A.; Olmstead, M.C. Post-acute sequelae of COVID-19: Evidence of mood & cognitive impairment. Brain Behav. Immun.-Health 2021, 17, 100347. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, G.K.; Khedr, E.M.; Hamad, D.A.; Meshref, T.S.; Hashem, M.M.; Aly, M.M. Long term impact of COVID-19 infection on sleep and mental health: A cross-sectional study. Psychiatry Res. 2021, 305, 114243. [Google Scholar] [CrossRef]
- O’Brien, K.; Townsend, L.; Dowds, J.; Bannan, C.; Nadarajan, P.; Kent, B.; Murphy, N.; Sheill, G.; Martin-Loeches, I.; Guinan, E. 1-year quality of life and health-outcomes in patients hospitalised with COVID-19: A longitudinal cohort study. Respir. Res. 2022, 23, 115. [Google Scholar] [CrossRef]
- Buonsenso, D.; Gualano, M.R.; Rossi, M.F.; Valz Gris, A.; Sisti, L.G.; Borrelli, I.; Santoro, P.E.; Tumminello, A.; Gentili, C.; Malorni, W.; et al. Post-Acute COVID-19 Sequelae in a Working Population at One Year Follow-Up: A Wide Range of Impacts from an Italian Sample. Int. J. Environ. Res. Public Health 2022, 19, 11093. [Google Scholar] [CrossRef] [PubMed]
- Peter, R.S.; Nieters, A.; Kräusslich, H.-G.; Brockmann, S.O.; Göpel, S.; Kindle, G.; Merle, U.; Steinacker, J.M.; Rothenbacher, D.; Kern, W.V. Post-acute sequelae of COVID-19 six to 12 months after infection: Population based study. BMJ 2022, 379, e071050. [Google Scholar] [CrossRef]
- Alkodaymi, M.S.; Omrani, O.A.; Fawzy, N.A.; Shaar, B.A.; Almamlouk, R.; Riaz, M.; Obeidat, M.; Obeidat, Y.; Gerberi, D.; Taha, R.M.; et al. Prevalence of post-acute COVID-19 syndrome symptoms at different follow-up periods: A systematic review and meta-analysis. Clin. Microbiol. Infect. 2022, 28, 657–666. [Google Scholar] [CrossRef]
- Di Gennaro, F.; Belati, A.; Tulone, O.; Diella, L.; Fiore Bavaro, D.; Bonica, R.; Genna, V.; Smith, L.; Trott, M.; Bruyere, O.; et al. Incidence of long COVID-19 in people with previous SARS-CoV-2 infection: A systematic review and meta-analysis of 120,970 patients. Intern. Emerg. Med. 2022, 18, 1573–1581. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing; R Core Team: Vienna, Austria, 2023; Available online: https://www.R-project.org/ (accessed on 4 August 2022).
- Iqbal, F.M.; Lam, K.; Sounderajah, V.; Clarke, J.M.; Ashrafian, H.; Darzi, A. Characteristics and predictors of acute and chronic post-COVID syndrome: A systematic review and meta-analysis. EClinicalMedicine 2021, 36, 100899. [Google Scholar] [CrossRef] [PubMed]
- Maglietta, G.; Diodati, F.; Puntoni, M.; Lazzarelli, S.; Marcomini, B.; Patrizi, L.; Caminiti, C. Prognostic Factors for Post-COVID-19 Syndrome: A Systematic Review and Meta-Analysis. J. Clin. Med. 2022, 11, 1541. [Google Scholar] [CrossRef] [PubMed]
- Lambert, N.; Survivor Corps; El-Azab, S.A.; Ramrakhiani, N.S.; Barisano, A.; Yu, L.; Taylor, K.; Esperança, Á.; Mendiola, C.; Downs, C.A.; et al. The other COVID-19 survivors: Timing, duration, and health impact of post-acute sequelae of SARS-CoV-2 infection. J. Clin. Nurs. 2022, 33, 76–88. [Google Scholar] [CrossRef] [PubMed]
- Fernández-de-las-Peñas, C.; Martín-Guerrero, J.D.; Pellicer-Valero, Ó.J.; Navarro-Pardo, E.; Gómez-Mayordomo, V.; Cuadrado, M.L.; Arias-Navalón, J.A.; Cigarán-Méndez, M.; Hernández-Barrera, V.; Arendt-Nielsen, L. Female Sex Is a Risk Factor Associated with Long-Term Post-COVID Related-Symptoms but Not with COVID-19 Symptoms: The LONG-COVID-EXP-CM Multicenter Study. J. Clin. Med. 2022, 11, 413. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Ramasamy, A.; Verduzco-Gutierrez, M.; Brode, W.M.; Melamed, E. Acute and post-acute sequelae of SARS-CoV-2 infection: A review of risk factors and social determinants. Virol. J. 2023, 20, 124. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Ebinger, J.E.; Mostafa, R.; Budde, P.; Gajewski, J.; Walker, B.; Joung, S.; Wu, M.; Bräutigam, M.; Hesping, F.; et al. Paradoxical sex-specific patterns of autoantibody response to SARS-CoV-2 infection. J. Transl. Med. 2021, 19, 524. [Google Scholar] [CrossRef]
- Guaraldi, G.; Milic, J.; Barbieri, S.; Marchiò, T.; Caselgrandi, A.; Motta, F.; Beghè, B.; Verduri, A.; Belli, M.; Gozzi, L.; et al. Quality of life and intrinsic capacity in patients with post-acute COVID-19 syndrome is in relation to frailty and resilience phenotypes. Sci. Rep. 2023, 13, 8956. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lai, C.-C.; Hsu, C.-K.; Yen, M.-Y.; Lee, P.-I.; Ko, W.-C.; Hsueh, P.-R. Long COVID: An inevitable sequela of SARS-CoV-2 infection. J. Microbiol. Immunol. Infect. 2023, 56, 1–9. [Google Scholar] [CrossRef]
- Davies, N.G.; Klepac, P.; Liu, Y.; Prem, K.; Jit, M.; CMMID COVID-19 Working Group; Pearson, C.A.B.; Quilty, B.J.; Kucharski, A.J.; Gibbs, H.; et al. Age-dependent effects in the transmission and control of COVID-19 epidemics. Nat. Med. 2020, 26, 1205–1211. [Google Scholar] [CrossRef]
- Yoo, S.M.; Liu, T.C.; Motwani, Y.; Sim, M.S.; Viswanathan, N.; Samras, N.; Hsu, F.; Wenger, N.S. Factors Associated with Post-Acute Sequelae of SARS-CoV-2 (PASC) After Diagnosis of Symptomatic COVID-19 in the Inpatient and Outpatient Setting in a Diverse Cohort. J. Gen. Intern. Med. 2022, 37, 1988–1995. [Google Scholar] [CrossRef]
- Tsampasian, V.; Elghazaly, H.; Chattopadhyay, R.; Debski, M.; Naing, T.K.P.; Garg, P.; Clark, A.; Ntatsaki, E.; Vassiliou, V.S. Risk Factors Associated With Post−COVID-19 Condition: A Systematic Review and Meta-analysis. JAMA Intern. Med. 2023, 183, 566. [Google Scholar] [CrossRef]
- Gerganova, A.; Assyov, Y.; Kamenov, Z. Stress Hyperglycemia, Diabetes Mellitus and COVID-19 Infection: Risk Factors, Clinical Outcomes and Post-Discharge Implications. Front. Clin. Diabetes Healthc. 2022, 3, 826006. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.K.; Feng, Y.; Yuan, M.Y.; Yuan, S.Y.; Fu, H.J.; Wu, B.Y.; Sun, G.Z.; Yang, G.R.; Zhang, X.L.; Wang, L.; et al. Plasma glucose levels and diabetes are independent predictors for mortality and morbidity in patients with SARS. Diabet. Med. 2006, 23, 623–628. [Google Scholar] [CrossRef]
- Azhar, A.; Khan, W.H.; Al-hosaini, K.; Zia, Q.; Kamal, M.A. Crosstalk between SARS-CoV-2 Infection and Type II Diabetes. Comb. Chem. High Throughput Screen. 2022, 25, 2429–2442. [Google Scholar] [CrossRef] [PubMed]
- Xie, Y.; Al-Aly, Z. Risks and burdens of incident diabetes in long COVID: A cohort study. Lancet Diabetes Endocrinol. 2022, 10, 311–321. [Google Scholar] [CrossRef] [PubMed]
- Sherif, Z.A.; Gomez, C.R.; Connors, T.J.; Henrich, T.J.; Reeves, W.B.; RECOVER Mechanistic Pathway Task Force. Pathogenic mechanisms of post-acute sequelae of SARS-CoV-2 infection (PASC). eLife 2023, 12, e86002. [Google Scholar] [CrossRef]
- Zsichla, L.; Müller, V. Risk Factors of Severe COVID-19: A Review of Host, Viral and Environmental Factors. Viruses 2023, 15, 175. [Google Scholar] [CrossRef]
- Veronese, N.; Segala, F.V.; Carruba, L.; La Carrubba, A.; Pollicino, F.; Di Franco, G.; Guido, G.; Cormio, M.; Lugli, A.; De Santis, L.; et al. Anemia as a risk factor for disease progression in patients admitted for COVID-19: Data from a large, multicenter cohort study. Sci. Rep. 2023, 13, 9035. [Google Scholar] [CrossRef] [PubMed]
- Sukocheva, O.A.; Maksoud, R.; Beeraka, N.M.; Madhunapantula, S.V.; Sinelnikov, M.; Nikolenko, V.N.; Neganova, M.E.; Klochkov, S.G.; Amjad Kamal, M.; Staines, D.R.; et al. Analysis of post COVID-19 condition and its overlap with myalgic encephalomyelitis/chronic fatigue syndrome. J. Adv. Res. 2022, 40, 179–196. [Google Scholar] [CrossRef]
- Xie, Y.; Choi, T.; Al-Aly, Z. Nirmatrelvir and the Risk of Post-Acute Sequelae of COVID-19; Infectious Diseases (except HIV/AIDS). MedRxiv 2022. [Google Scholar] [CrossRef]
- Veronese, N.; Di Gennaro, F.; Frallonardo, L.; Ciriminna, S.; Papagni, R.; Carruba, L.; Agnello, D.; De Iaco, G.; De Gennaro, N.; Di Franco, G.; et al. Real life experience on the use of Remdesivir in patients admitted to COVID-19 in two referral Italian hospital: A propensity score matched analysis. Sci. Rep. 2024, 14, 9303. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, A.; Iwagami, M.; Yasuhara, J.; Takagi, H.; Kuno, T. Protective effect of COVID-19 vaccination against long COVID syndrome: A systematic review and meta-analysis. Vaccine 2023, 41, 1783–1790. [Google Scholar] [CrossRef] [PubMed]
- Veronese, N.; Bonica, R.; Cotugno, S.; Tulone, O.; Camporeale, M.; Smith, L.; Trott, M.; Bruyere, O.; Mirarchi, L.; Rizzo, G.; et al. Interventions for Improving Long COVID-19 Symptomatology: A Systematic Review. Viruses 2022, 14, 1863. [Google Scholar] [CrossRef] [PubMed]
- Evans, R.A.; McAuley, H.; Harrison, E.M.; Shikotra, A.; Singapuri, A.; Sereno, M.; Elneima, O.; Docherty, A.B.; Lone, N.I.; Leavy, O.C.; et al. Physical, cognitive, and mental health impacts of COVID-19 after hospitalisation (PHOSP-COVID): A UK multicentre, prospective cohort study. Lancet Respir. Med. 2021, 9, 1275–1287. [Google Scholar] [CrossRef] [PubMed]
- Meyer, B.; Zill, A.; Dilba, D.; Gerlach, R.; Schumann, S. Employee psychological well-being during the COVID -19 pandemic in Germany: A longitudinal study of demands, resources, and exhaustion. Int. J. Psychol. 2021, 56, 532–550. [Google Scholar] [CrossRef]
- Zhang, W.; Bansback, N.; Boonen, A.; Young, A.; Singh, A.; Anis, A.H. Validity of the work productivity and activity impairment questionnaire—General health version in patients with rheumatoid arthritis. Arthritis Res. Ther. 2010, 12, R177. [Google Scholar] [CrossRef]
| Reachable Subjects (n = 322) | Unreachable Subjects (n = 172) | p-Value | |
|---|---|---|---|
| Age at hospital admission, years a | 46 (36.54) | 49 (25–55) | 0.42 |
| Males | 188 (58.4) | 112 (65.1) | 0.17 |
| Hypertension | 61 (18.9) | 38 (22.1) | 0.47 |
| Dyslipidemia | 32 (9.9) | 12 (7.0) | 0.34 |
| Diabetes | 28 (8.7) | 15 (8.7) | 0.99 |
| Obesity (BMI > 30 km/m2) | 58 (18.0) | 24 (14.0) | 0.30 |
| Smoking habits: Current smoker Former smoker None | 18 (5.6) 16 (5.0) 288 (89.4) | 19/171 (11.1) 16/171 (9.4) 136/171 (79.5) | 0.01 |
| Any cancer | 30 (9.3) | 19 (11.0) | 0.64 |
| Any immunosuppression condition | 54 (16.8) | 32/170 (18.8) | 0.65 |
| Elevated D-Dimer | 180/308 (58.4) | 92/164 (56.1) | 0.69 |
| Elevated PCR | 267/321 (83.2) | 135/171 (78.9) | 0.30 |
| Elevated LDH | 141/314 (44.9) | 69/168 (41.1) | 0.47 |
| ICU admission | 43 (13.3) | 16 (9.3) | 0.23 |
| Oxygen during hospital stay | 162 (50.3) | 73 (42.4) | 0.11 |
| High flow nasal cannula | 43 (13.3) | 12 (7.0) | 0.04 |
| Non-invasive mechanical ventilation | 42 (13.0) | 23 (13.4) | 0.99 |
| Invasive-mechanical ventilation | 12 (3.7) | 8 (4.7) | 0.79 |
| Length of hospital stay, days a | 25 (19–40) | 11 (7–17) | <0.0001 |
| Comparable Working Ability (n = 184) | Impaired Working Ability (n = 134) | p-Value | |
|---|---|---|---|
| Age at hospital admission, years a | 44 (33–53) | 50 (44–54) | 0.001 |
| Males | 118 (64.1) | 69 (51.5) | 0.03 |
| Hypertension | 26 (14.1) | 34 (25.4) | 0.01 |
| Dyslipidemia | 13 (7.1) | 19 (14.2) | 0.06 |
| Diabetes | 8 (4.3) | 20 (14.9) | 0.002 |
| Obesity (BMI > 30 km/m2) | 28 (15.2) | 30 (22.4) | 0.13 |
| Smoking habits: Current smoker Former smoker None | 12 (6.5) 6 (3.3) 166 (90.2) | 6 (4.5) 10 (7.5) 118 (88.0) | 0.18 |
| Any cancer | 14 (7.6) | 14 (10.4) | 0.49 |
| Any immunosuppression condition | 23 (12.5) | 27 (20.1) | 0.09 |
| Elevated D-Dimer | 99/179 (55.3) | 78/126 (61.9) | 0.30 |
| Elevated PCR | 147/183 (80.3) | 116 (86.6) | 0.19 |
| Elevated LDH | 75/179 (41.9) | 64/131 (48.9) | 0.27 |
| COVID-19 vaccination status at admission: Booster First cycle No vaccination | 18/182 (9.9) 24/182 (13.2) 140/182 (76.9) | 16/133 (12.0) 15/133 (11.3) 102/133 (76.7) | 0.75 |
| Corticosteroids | 73 (39.7) | 58 (43.2) | 0.59 |
| Remdesivir | 35 (19.0) | 31 (23.1) | 0.45 |
| ICU admission | 26 (14.1) | 15 (11.2) | 0.54 |
| Oxygen during hospital stay | 83 (45.1) | 77 (57.5) | 0.04 |
| High-flow nasal cannula | 27 (14.7) | 15 (11.2) | 0.46 |
| Non-invasive mechanical ventilation | 24 (13.0) | 16 (11.9) | 0.90 |
| Invasive-mechanical ventilation | 7 (3.8) | 5 (3.7) | 0.99 |
| Length of hospital stay, days a | 12 (7–18) | 14 (9–23) | 0.04 |
| Odds Ratio (95% Confidence Interval) | p-Value | |
|---|---|---|
| Age at hospital admission, years | 1.02 (0.99 to 1.04) | 0.05 |
| Sex: female vs. male | 1.90 (1.18 to 3.08) | 0.008 |
| Diabetes: yes vs. no | 3.73 (1.57 to 9.65) | 0.004 |
| Oxygen during hospital stay: yes vs. no | 1.76 (1.01 to 3.06) | 0.04 |
| Severe disease: yes vs. no a | 0.51 (0.26 to 1.01) | 0.05 |
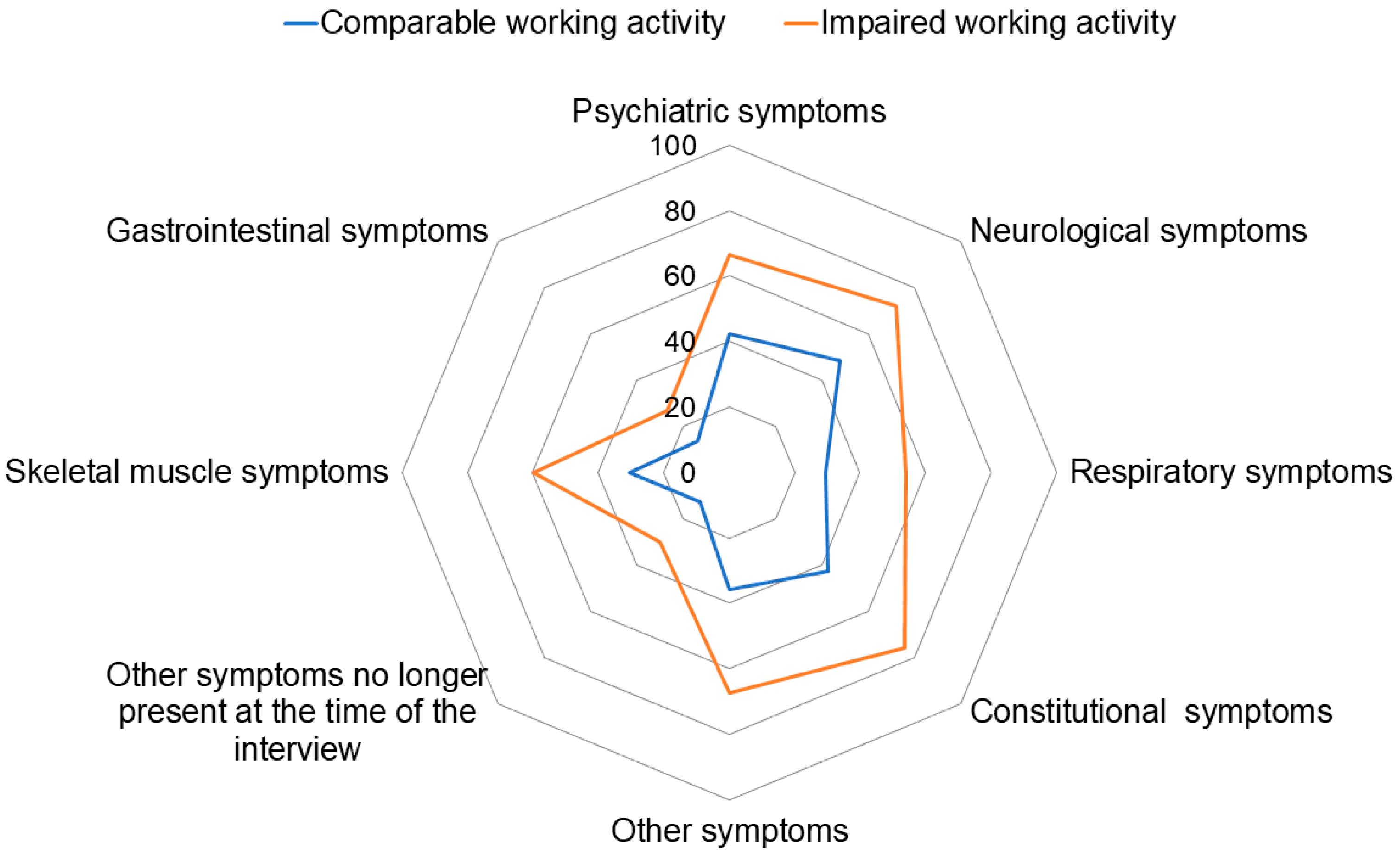
| Category | Comparable Working Ability (n = 184) | Impaired Working Ability (n = 134) | p-Value |
|---|---|---|---|
| Self-perception of the overall status a | 8 (7–9) | 7 (6–8) | <0.0001 |
| Psychiatric symptoms | 77/182 (42.3) | 89 (66.4) | <0.0001 |
| Neurological symptoms | 86/179 (48.0) | 95/132 (72.0) | <0.0001 |
| Respiratory symptoms | 54 (29.3) | 72/133 (54.1) | <0.0001 |
| Constitutional symptoms | 77/181 (42.5) | 100/132 (75.8) | <0.0001 |
| Skeletal muscle symptoms | 56 (30.4) | 80 (59.7) | <0.0001 |
| Gastrointestinal symptoms | 24/181 (13.3) | 36 (26.9) | 0.0004 |
| Other symptoms | 65/181 (35.9) | 87/129 (67.4) | <0.0001 |
| Other symptoms no longer present at the time of the interview | 23 (12.5) | 40 (29.9) | 0.0002 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Frallonardo, L.; Ritacco, A.I.; Amendolara, A.; Cassano, D.; Manco Cesari, G.; Lugli, A.; Cormio, M.; De Filippis, M.; Romita, G.; Guido, G.; et al. Long-Term Impairment of Working Ability in Subjects under 60 Years of Age Hospitalised for COVID-19 at 2 Years of Follow-Up: A Cross-Sectional Study. Viruses 2024, 16, 688. https://doi.org/10.3390/v16050688
Frallonardo L, Ritacco AI, Amendolara A, Cassano D, Manco Cesari G, Lugli A, Cormio M, De Filippis M, Romita G, Guido G, et al. Long-Term Impairment of Working Ability in Subjects under 60 Years of Age Hospitalised for COVID-19 at 2 Years of Follow-Up: A Cross-Sectional Study. Viruses. 2024; 16(5):688. https://doi.org/10.3390/v16050688
Chicago/Turabian StyleFrallonardo, Luisa, Annunziata Ilenia Ritacco, Angela Amendolara, Domenica Cassano, Giorgia Manco Cesari, Alessia Lugli, Mariangela Cormio, Michele De Filippis, Greta Romita, Giacomo Guido, and et al. 2024. "Long-Term Impairment of Working Ability in Subjects under 60 Years of Age Hospitalised for COVID-19 at 2 Years of Follow-Up: A Cross-Sectional Study" Viruses 16, no. 5: 688. https://doi.org/10.3390/v16050688
APA StyleFrallonardo, L., Ritacco, A. I., Amendolara, A., Cassano, D., Manco Cesari, G., Lugli, A., Cormio, M., De Filippis, M., Romita, G., Guido, G., Piccolomo, L., Giliberti, V., Cavallin, F., Segala, F. V., Di Gennaro, F., & Saracino, A. (2024). Long-Term Impairment of Working Ability in Subjects under 60 Years of Age Hospitalised for COVID-19 at 2 Years of Follow-Up: A Cross-Sectional Study. Viruses, 16(5), 688. https://doi.org/10.3390/v16050688








