Impact of B Cell Depletion on COVID-19 in Kidney Transplant Recipients
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Study Items
2.3. Medical Practice for COVID-19
2.4. Treatment for COVID-19
2.5. Immunological Status at Transplantation and Immunosuppressive Protocol
2.6. B Cell Population
2.7. Ethical Considerations
2.8. Statistical Analysis
3. Results
3.1. Comparison by Disease Severity
3.2. Association between B Cell Depletion Therapy and COVID-19
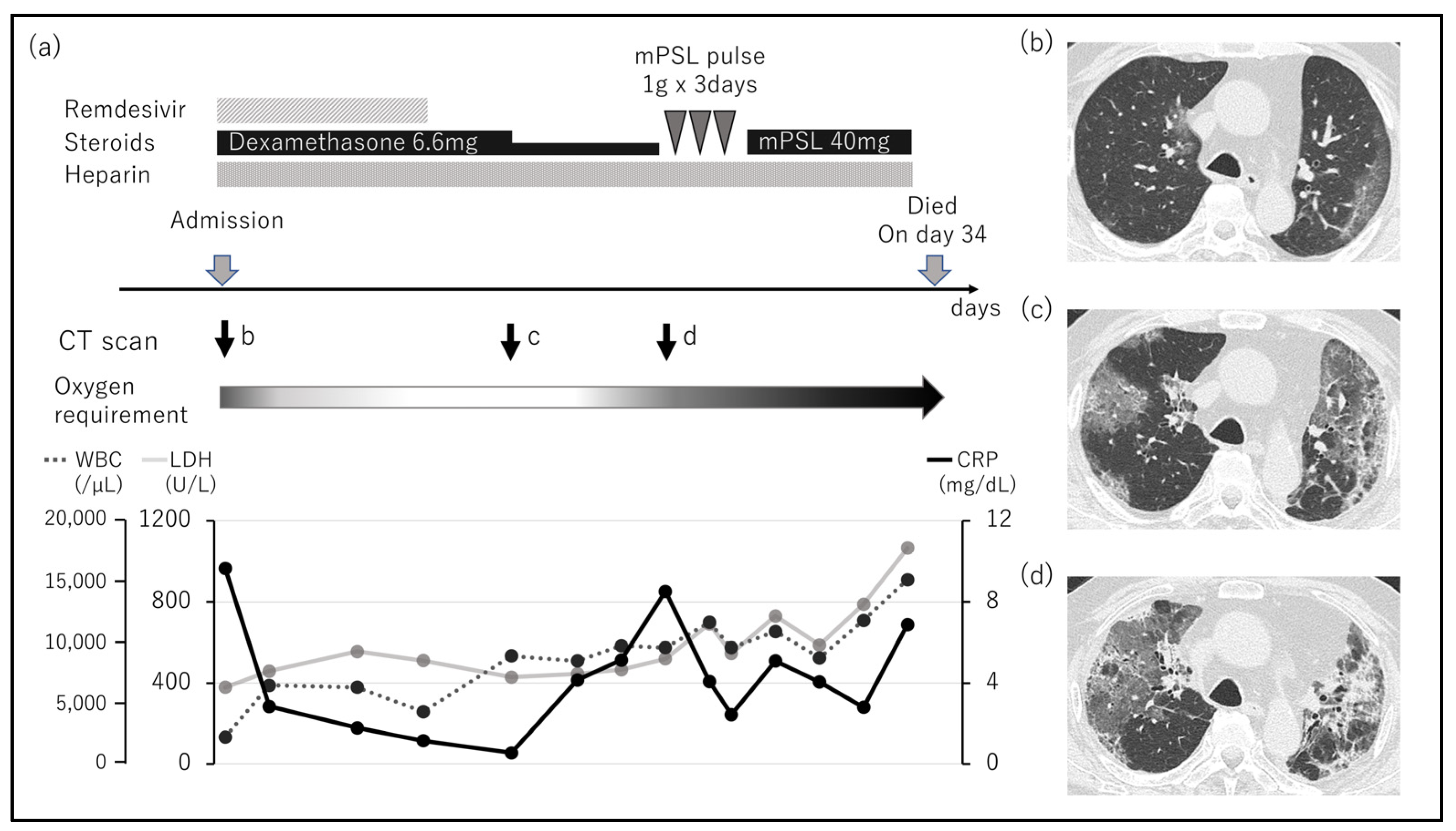
3.3. Association between B Cell Depletion and Clinical Course
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed on 21 January 2023).
- Sandoval, M.; Nguyen, D.T.; Huang, H.J.; Yi, S.G.; Ghobrial, R.M.; Gaber, A.O.; Graviss, E.A. COVID-19 mortality may be reduced among fully vaccinated solid organ transplant recipients. PLoS ONE 2022, 17, e0279222. [Google Scholar] [CrossRef] [PubMed]
- Hardgrave, H.; Wells, A.; Nigh, J.; Klutts, G.; Krinock, D.; Osborn, T.; Bhusal, S.; Rude, M.K.; Burdine, L.; Giorgakis, E. COVID-19 Mortality in Vaccinated vs. unvaccinated Liver & Kidney Transplant Recipients: A Single-Center United States Propensity Score Matching Study on Historical Data. Vaccines 2022, 10, 1921. [Google Scholar] [CrossRef]
- Boyarsky, B.J.; Werbel, W.A.; Avery, R.K.; Tobian, A.A.R.; Massie, A.B.; Segev, D.L.; Garonzik-Wang, J.M. Antibody response to 2-dose SARS-CoV-2 mRNA vaccine series in solid organ transplant recipients. JAMA 2021, 325, 2204–2206. [Google Scholar] [CrossRef] [PubMed]
- Radcliffe, C.; Palacios, C.F.; Azar, M.M.; Cohen, E.; Malinis, M. Real-world experience with available, outpatient COVID-19 therapies in solid organ transplant recipients during the omicron surge. Am. J. Transplant. 2022, 22, 2458–2463. [Google Scholar] [CrossRef]
- Montero, C.; Torres, R.; Benavidez, C.; Garcia, P.; Jimenez, S.; Yomayusa, N.; Gayon, D.; Perez, J.; Rosselli, D.; Restrepo, H.; et al. Impact of immunosuppression regimen on COVID-19 mortality in kidney transplant recipients: Analysis from a Colombian transplantation centers registry. Nefrología 2023. [Google Scholar] [CrossRef]
- Japanese Society for Clinical Renal Transplantation. The Japan Society for transplantation annual progress report from the Japanese Renal Transplant Registry: Number of renal transplantations in 2021 and follow-up survey. Ishoku 2022, 57, 199–219. (In Japanese) [Google Scholar]
- WHO Working Group on the Clinical Characterisation and Management of COVID-19 Infection. A minimal common outcome measure set for COVID-19 clinical research. Lancet Infect. Dis. 2020, 20, e192–e197. [Google Scholar] [CrossRef]
- Kanda, Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transpl. 2013, 48, 452–458. [Google Scholar] [CrossRef]
- Genberg, H.; Hansson, A.; Wernerson, A.; Wennberg, L.; Tydén, G. Pharmacodynamics of rituximab in kidney allotransplantation. Am. J. Transplant. 2006, 6, 2418–2428. [Google Scholar] [CrossRef]
- Matz, M.; Lehnert, M.; Lorkowski, C.; Fabritius, K.; Weber, U.A.; Mashreghi, M.F.; Neumayer, H.H.; Budde, K. Combined standard and novel immunosuppressive substances affect B-lymphocyte function. Int. Immunopharmacol. 2013, 15, 718–725. [Google Scholar] [CrossRef]
- Goel, R.R.; Apostolidis, S.A.; Painter, M.M.; Mathew, D.; Pattekar, A.; Kuthuru, O.; Gouma, S.; Hicks, P.; Meng, W.; Rosenfeld, A.M.; et al. Distinct antibody and memory B cell responses in SARS-CoV-2 naïve and recovered individuals following mRNA vaccination. Sci. Immunol. 2021, 6, eabi6950. [Google Scholar] [CrossRef]
- Sanders, J.F.; Bemelman, F.J.; Messchendorp, A.L.; Baan, C.C.; van Baarle, D.; van Binnendijk, R.; Diavatopoulos, D.A.; Frölke, S.C.; Geers, D.; GeurtsvanKessel, C.H.; et al. The RECOVAC immune-response study: The immunogenicity, tolerability, and safety of COVID-19 vaccination in patients with chronic kidney disease, on dialysis, or living with a kidney transplant. Transplantation 2022, 106, 821–834. [Google Scholar] [CrossRef]
- Kantauskaite, M.; Müller, L.; Hillebrandt, J.; Lamberti, J.; Fischer, S.; Kolb, T.; Ivens, K.; Koch, M.; Andree, M.; Lübke, N.; et al. Immune response to third SARS-CoV-2 vaccination in seronegative kidney transplant recipients: Possible improvement by mycophenolate mofetil reduction. Clin. Transplant. 2022, 36, e14790. [Google Scholar] [CrossRef] [PubMed]
- Frölke, S.C.; Bouwmans, P.; Messchendorp, A.L.; Geerlings, S.E.; Hemmelder, M.H.; Gansevoort, R.T.; Hilbrands, L.B.; Reinders, M.E.J.; Sanders, J.F.; Bemelman, F.J.; et al. Predictors of nonseroconversion to SARS-CoV-2 vaccination in kidney transplant recipients. Transplant. Direct. 2022, 8, e1397. [Google Scholar] [CrossRef] [PubMed]
- Haskin, O.; Ashkenazi-Hoffnung, L.; Ziv, N.; Borovitz, Y.; Dagan, A.; Levi, S.; Koren, G.; Hamdani, G.; Levi-Erez, D.; Landau, D.; et al. Serological response to the BNT162b2 COVID-19 mRNA vaccine in adolescent and young adult kidney transplant recipients. Transplantation 2021, 105, e226–e233. [Google Scholar] [CrossRef]
- Manothummetha, K.; Chuleerarux, N.; Sanguankeo, A.; Kates, O.S.; Hirankarn, N.; Thongkam, A.; Dioverti-Prono, M.V.; Torvorapanit, P.; Langsiri, N.; Worasilchai, N.; et al. Immunogenicity and risk factors associated with poor humoral immune response of SARS-CoV-2 vaccines in recipients of solid organ transplant: A systematic review and meta-analysis. JAMA Netw. Open 2022, 5, e226822. [Google Scholar] [CrossRef] [PubMed]
- Takai, S.; Nishida, H.; Ito, H.; Fukuhara, H.; Nawano, T.; Narisawa, T.; Kanno, H.; Yagi, M.; Yamagishi, A.; Sakurai, T.; et al. Humoral and cellular immune response and the safety of third SARS-CoV-2 mRNA vaccine with longer interval after the second vaccination in kidney transplant recipients. Front. Immunol. 2022, 13, 1050211. [Google Scholar] [CrossRef] [PubMed]
- Singh, N.; Madhira, V.; Hu, C.; Olex, A.L.; Bergquist, T.; Fitzgerald, K.C.; Huling, J.D.; Patel, R.C.; Singh, J.A. Rituximab is associated with worse COVID-19 outcomes in patients with rheumatoid arthritis: A retrospective, nationally sampled cohort study from the U.S. National COVID Cohort Collaborative (N3C). Semin. Arthritis Rheum. 2023, 58, 152149. [Google Scholar] [CrossRef] [PubMed]
- Kintrilis, N.; Gkinos, C.P.; Galinos, I. Prolonged COVID-19 in a multiple sclerosis patient treated with rituximab. Cureus 2022, 14, e32523. [Google Scholar] [CrossRef]
- Mukhina, O.A.; Fomina, D.S.; Parshin, V.V.; Gushchin, V.A.; Dolzhikova, I.V.; Shchetinin, A.M.; Chudakov, D.M.; Alekseeva, E.; Korostin, D.; Bazykin, G.A.; et al. SARS-CoV-2 evolution in a patient with secondary B-cell immunodeficiency: A clinical case. Hum. Vaccines Immunother. 2022, 18, 2101334. [Google Scholar] [CrossRef]
- Primorac, D.; Vrdoljak, K.; Brlek, P.; Pavelić, E.; Molnar, V.; Matišić, V.; Erceg Ivkošić, I.; Parčina, M. Adaptive immune responses and immunity to SARS-CoV-2. Front. Immunol. 2022, 13, 848582. [Google Scholar] [CrossRef] [PubMed]
- Junqueira, C.; Crespo, Â.; Ranjbar, S.; de Lacerda, L.B.; Lewandrowski, M.; Ingber, J.; Parry, B.; Ravid, S.; Clark, S.; Schrimpf, M.R.; et al. FcγR-mediated SARS-CoV-2 infection of monocytes activates inflammation. Nature 2022, 606, 576–584. [Google Scholar] [CrossRef] [PubMed]
- Levin, M.J.; Ustianowski, A.; De Wit, S.; Launay, O.; Avila, M.; Templeton, A.; Yuan, Y.; Seegobin, S.; Ellery, A.; Levinson, D.J.; et al. Intramuscular AZD7442 (Tixagevimab-Cilgavimab) for prevention of COVID-19. N. Engl. J. Med. 2022, 386, 2188–2200. [Google Scholar] [CrossRef] [PubMed]
- Montgomery, H.; Hobbs, F.D.R.; Padilla, F.; Arbetter, D.; Templeton, A.; Seegobin, S.; Kim, K.; Campos, J.A.S.; Arends, R.H.; Brodek, B.H.; et al. Efficacy and safety of intramuscular administration of tixagevimab-cilgavimab for early outpatient treatment of COVID-19 (TACKLE): A phase 3, randomised, double-blind, placebo-controlled trial. Lancet Respir. Med. 2022, 10, 985–996. [Google Scholar] [CrossRef]
- Takashita, E.; Yamayoshi, S.; Simon, V.; van Bakel, H.; Sordillo, E.M.; Pekosz, A.; Fukushi, S.; Suzuki, T.; Maeda, K.; Halfmann, P.; et al. Efficacy of antibodies and antiviral drugs against omicron BA.2.12.1, BA.4, and BA.5 Subvariants. N. Engl. J. Med. 2022, 387, 468–470. [Google Scholar] [CrossRef]
| All (n = 28) | Mild (n = 18) | Moderate (n = 6) | Severe (n = 4) | p- Value | |
|---|---|---|---|---|---|
| Age (year) | 54.5 (34–77) | 54.5 (34–74) | 48 (36–71) | 75.5 (49–77) | 0.075 |
| Sex (male, %) | 16 (57.1) | 11 (61.1) | 2 (33.3) | 3 (75.0) | 0.36 |
| BMI (kg/m2) | 22.2 (15.4–32.5) | 22.2 (15.4–29.9) | 22.1 (19.9–31.6) | 22.6 (20.1–32.5) | 0.90 |
| Tx Procedure (%) | 0.72 | ||||
| ABO-compatible KTx | 14 (50.0) | 8 (47.4) | 4 (66.7) | 2 (50.0) | |
| ABO-incompatible KTx | 8 (28.6) | 5 (15.2) | 1 (16.7) | 2 (50.0) | |
| SPK | 6 (21.4) | 5 (15.2) | 1 (16.7) | 0 (0.0) | |
| Post-transplant Years | 4.3 (1.2–14.9) | 5.1 (1.6–14.9) | 3.2 (1.4–7.1) | 3.9 (1.2–9.2) | 0.56 |
| Days after onset | 1 (0–12) | 1 (0–4) | 1.5 (0–12) | 1.5 (0–6) | 0.59 |
| Immunosuppressants | |||||
| CNI | 1.0 | ||||
| Tacrolimus | 26 (92.9) | 16 (88.9) | 6 (100) | 4 (100) | |
| Cyclosporine | 2 (7.1) | 2 (11.1) | 0 (0.0) | 0 (0.0) | |
| MMF | 23 (80.0) | 16 (88.9) | 4 (66.7) | 3 (75.0) | 0.37 |
| Everolimus | 8 (28.6) | 5 (27.8) | 2 (33.3) | 1 (25.0) | 0.95 |
| Steroid | 28 (100) | 19 (100) | 8 (100) | 4 (100) | 1.0 |
| B cell depletion therapy | 12 (42.9) | 7 (38.9) | 2 (33.3) | 3 (75.0) | 0.50 |
| Blood Examination | |||||
| WBC (×103/µL) | 5.8 (3.0–12.2) | 5.8 (3.0–12.1) | 5.7 (4.1–8.3) | 8.2 (5.6–12.2) | 0.16 |
| LDH (U/L) | 268 (141–623) | 237 (141–623) | 285 (237–397) | 320 (303–403) | 0.059 |
| CRP (mg/dL) | 1.2 (0.1–17.0) | 1.0 (0.1–2.9) | 2.5 (0.5–7.4) | 10.9 (7.2–17.0) | <0.01 |
| Peak CRP (mg/dL) | 3.2 (0.1–25.6) | 1.5 (0.1–7.1) | 5.0 (0.7–25.6) | 17.0 (9.7–23.2) | <0.01 |
| D-dimer (µg/mL) | 0.9 (0.5–3.9) | 0.8 (0.6–3.7) | 1.5 (1.1–3.9) | 1.7 (0.5–3.6) | 0.13 |
| Cre (mg/dL) | 1.2 (0.6–3.4) | 1.3 (0.6–3.4) | 0.9 (0.6–1.8) | 1.2 (1.0–2.5) | 0.39 |
| B cell depletion (%) | 8 (28.6) | 4 (22.2) | 2 (33.3) | 2 (50.0) | 0.52 |
| IgG (mg/dL) | 926.5 (440–1830) | 1129 (440–1830) | 903.5 (757–1098) | 752 (656–869) | 0.12 |
| IgM (mg/dL) | 64.5 (12–198) | 62 (27–198) | 66 (38–156) | 53 (12–125) | 0.67 |
| Outcome | |||||
| Progression (%) | 5 (17.9) | 1 (5.6) | 1 (16.7) | 3 (75.0) | <0.01 |
| ICU stay (%) | 4 (14.3) | 0 (0) | 0 (0) | 4 (100) | <0.01 |
| Hospitalization days | 9 (3–38) | 6 (3–20) | 15 (8–27) | 35.5 (16–38) | <0.01 |
| Survival (%) | 26 (92.9) | 18 (100) | 6 (100) | 2 (50.0) | <0.01 |
| Age/ Sex | Immunosuppress Protocol | Years After Tx | Cre (mg/dL) | CD19(+) Cells (%) | Severity at Visit | Hospitalization Days | Progression | Survival |
|---|---|---|---|---|---|---|---|---|
| 76/M | R + T, M, S | 6.3 | 2.5 | 0.3 | Severe | 16 | Yes | Dead |
| 69/M | R + T, M, E, S | 1.6 | 1.3 | 0.3 | Mild | 7 | No | Alive |
| 77/M | R + T, M, S | 1.6 | 1.0 | 0.6 | Severe | 35 | Yes | Dead |
| 44/F | R + T, E, S | 6.1 | 1.3 | 0.9 | Moderate | 27 | Yes | Alive |
| 71/M | R + T, M, S | 7.1 | 0.8 | 0.9 | Moderate | 16 | No | Alive |
| 41/M | R + T, E, S | 2.9 | 3.4 | 1.0 | Mild | 20 | No | Alive |
| 65/F | SX + T, M, S | 14.9 | 1.6 | 1.4 | Mild | 12 | Yes | Alive |
| 74/F | R + C, M, E, S | 2.1 | 0.7 | 1.6 | Mild | 8 | No | Alive |
| 64/F | R + C, M, E, S | 6.2 | 1.5 | 4.3 | Mild | 5 | No | Alive |
| 52/M | R + T, M, S | 6.9 | 1.2 | 8.2 | Mild | 6 | No | Alive |
| 45/M | R + T, M, S | 8.3 | 1.5 | 11.0 | Mild | 8 | No | Alive |
| 49/F | R + T, M, S | 9.1 | 1.1 | 16.8 | Severe | 38 | Yes | Alive |
| Factor | Normal (n = 20) | Depletion (n = 8) | p-Value |
|---|---|---|---|
| Age (years) | 52 (34–75) | 70 (41–77) | 0.039 |
| Sex (male, %) | 11 (55.0) | 5 (62.5) | 1.0 |
| BMI | 22.4 (17.1–32.5) | 21.2 (15.4–31.6) | 0.48 |
| Tx procedure (%) | 0.032 | ||
| ABO-compatible KTx | 11 (55.0) | 3 (37.5) | |
| ABO-incompatible KTx | 3 (15.0) | 5 (62.5) | |
| SPK | 6 (30.0) | 0 (0) | |
| Tx to onset (years) | 4.3 (1.2–9.2) | 4.5 (1.6–14.9) | 1.0 |
| Vaccination (%) | 19 (95.0) | 9 (100) | |
| Immunosuppressant (%) | |||
| CNI | 0.50 | ||
| Tacrolimus | 19 (95.0) | 7 (87.5) | |
| Cyclosporine | 1 (5.0) | 1 (12.5) | |
| MMF | 17 (85.0) | 6 (75.0) | 0.61 |
| Everolimus | 4 (20.0) | 4 (50.0) | 0.17 |
| Rituximab | 4 (20.0) | 7 (87.5) | <0.01 |
| Splenectomy | 0 (0) | 1 (12.5) | |
| Blood Examination | |||
| WBC (×103/µL) | 5.6 (3.0–12.2) | 6.9 (4.6–12.1) | 0.15 |
| LDH (U/L) | 240 (141–623) | 306.5 (236–403) | 0.038 |
| CRP (mg/dL) | 1.2 (0.1–17.0) | 2.1 (0.4–7.6) | 0.28 |
| PeakCRP (mg/dL) | 2.1 (0.1–17.8) | 7.3 (4.6–12.1) | 0.032 |
| D-dimer (µg/mL) | 0.8 (0.5–3.9) | 1.5 (0.7–3.7) | 0.16 |
| Cre (mg/dL) | 1.2 (0.6–2.6) | 1.3 (0.7–3.4) | 0.49 |
| IgG (mg/dL) | 1032 (653–1830) | 888.5 (440–1098) | 0.33 |
| IgM (mg/dL) | 64.5 (27–198) | 61 (12–126) | 0.56 |
| Outcome | |||
| Severity at visit (%) | 0.50 | ||
| Mild | 14 (70.0) | 4 (50.0) | |
| Moderate | 4 (20.0) | 2 (25.0) | |
| Severe | 2 (10.0) | 2 (25.0) | |
| Progression (%) | 1 (5.0) | 4 (50.0) | 0.015 |
| ICU stay (%) | 2 (10.0) | 2 (25.0) | 0.56 |
| Hospitalization days(days) | 7 (3–38) | 16 (7–35) | 0.034 |
| Survival (%) | 20 (100) | 6 (75.0) | 0.074 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aida, N.; Ito, T.; Kurihara, K.; Hiratsuka, I.; Shibata, M.; Suzuki, A.; Hasegawa, M.; Kenmochi, T. Impact of B Cell Depletion on COVID-19 in Kidney Transplant Recipients. Viruses 2023, 15, 1520. https://doi.org/10.3390/v15071520
Aida N, Ito T, Kurihara K, Hiratsuka I, Shibata M, Suzuki A, Hasegawa M, Kenmochi T. Impact of B Cell Depletion on COVID-19 in Kidney Transplant Recipients. Viruses. 2023; 15(7):1520. https://doi.org/10.3390/v15071520
Chicago/Turabian StyleAida, Naohiro, Taihei Ito, Kei Kurihara, Izumi Hiratsuka, Megumi Shibata, Atsushi Suzuki, Midori Hasegawa, and Takashi Kenmochi. 2023. "Impact of B Cell Depletion on COVID-19 in Kidney Transplant Recipients" Viruses 15, no. 7: 1520. https://doi.org/10.3390/v15071520
APA StyleAida, N., Ito, T., Kurihara, K., Hiratsuka, I., Shibata, M., Suzuki, A., Hasegawa, M., & Kenmochi, T. (2023). Impact of B Cell Depletion on COVID-19 in Kidney Transplant Recipients. Viruses, 15(7), 1520. https://doi.org/10.3390/v15071520






