SARS-CoV-2 Infection and Clinical Signs in Cats and Dogs from Confirmed Positive Households in Germany
Abstract
1. Introduction
2. Materials and Methods
3. Results
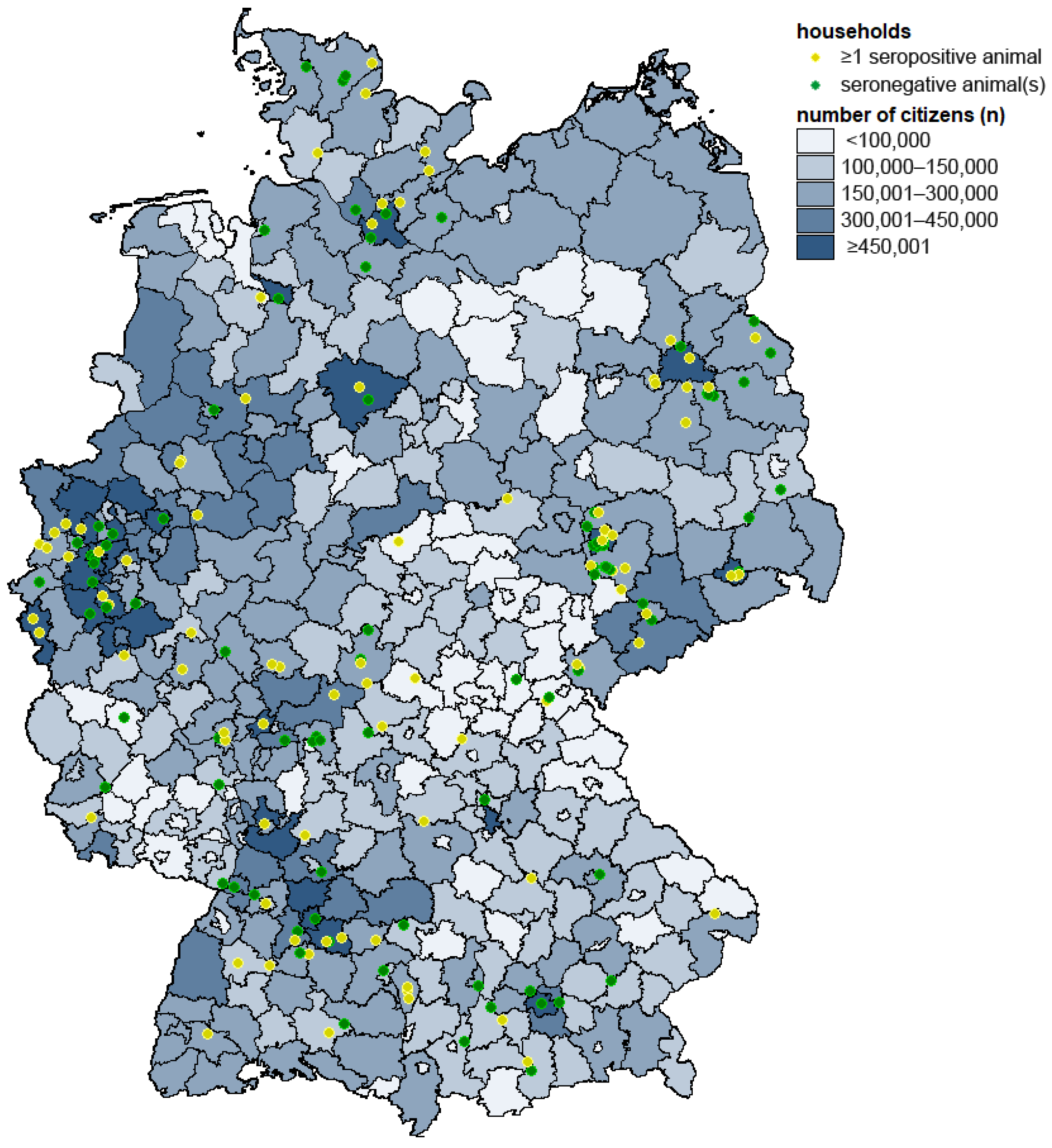
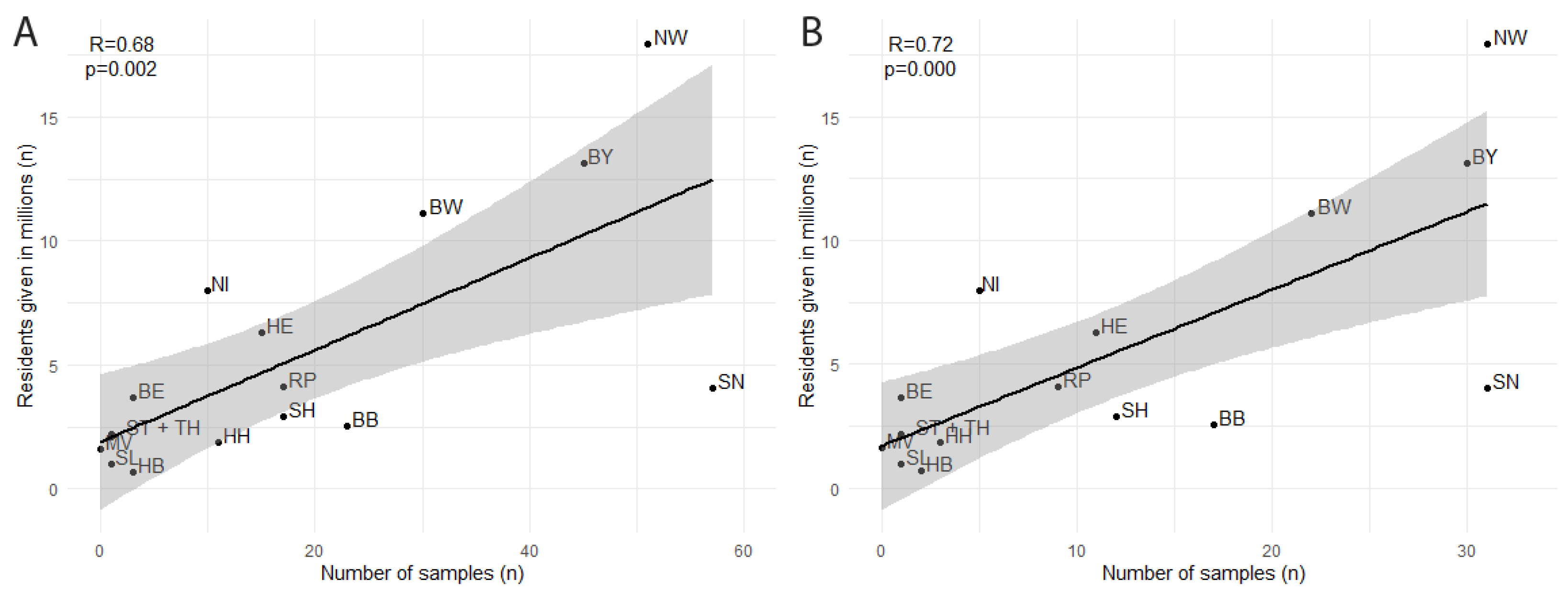
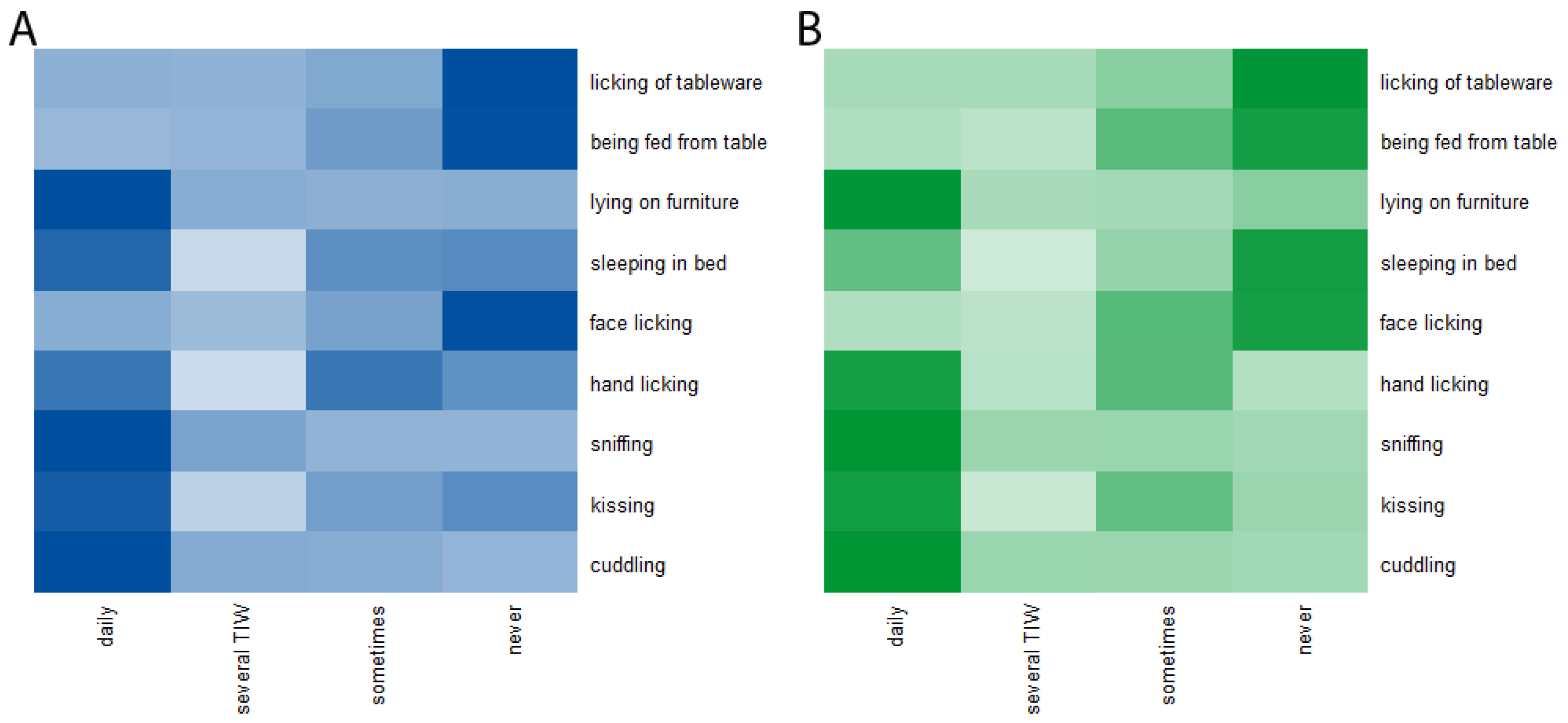
3.1. Properties of Participating Households and Respective Human and Companion Animal Members
3.2. Seroprevalence in Dogs and Cats
3.3. Risk Factors for Infection and Clinical Signs
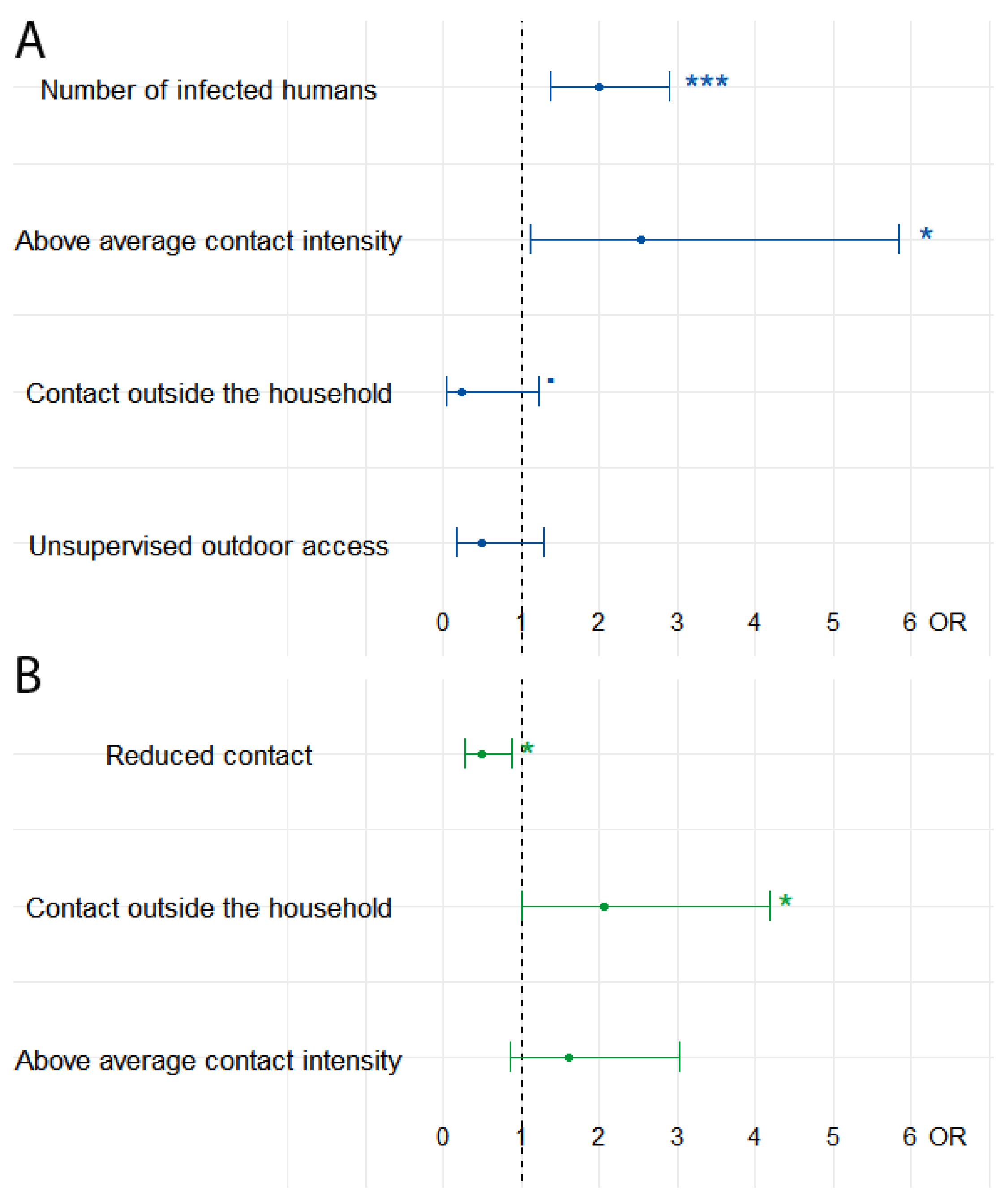
3.3.1. Univariable Statistical Analysis
3.3.2. Multivariable Statistical Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Novel Coronavirus (2019-nCoV) Situation Report—11; WHO: Geneva, Switzerland, 2019. Available online: https://apps.who.int/iris/handle/10665/330776 (accessed on 29 July 2022).
- WHO. Coronavirus Disease 2019 (COVID-19) Situation Report—51; WHO: Geneva, Switzerland, 2019. Available online: https://apps.who.int/iris/handle/10665/331475 (accessed on 29 July 2022).
- Michelitsch, A.; Wernike, K.; Ulrich, L.; Mettenleiter, T.C.; Beer, M. SARS-CoV-2 in animals: From potential hosts to animal models. Adv. Virus Res. 2021, 110, 59–102. [Google Scholar] [CrossRef] [PubMed]
- Meehan, M.; Massavelli, B.; Pachana, N. Using attachment theory and social support theory to examine and measure pets as sources of social support and attachment figures. Anthrozoös 2017, 30, 273–289. [Google Scholar] [CrossRef]
- Gfk. Pet Ownership, Global GfK Survey. Available online: https://cdn2.hubspot.net/hubfs/2405078/cms-pdfs/fileadmin/user_upload/country_one_pager/nl/documents/global-gfk-survey_pet-ownership_2016.pdf (accessed on 27 April 2022).
- Shi, J.; Wen, Z.; Zhong, G.; Yang, H.; Wang, C.; Huang, B.; Liu, R.; He, X.; Shuai, L.; Sun, Z.; et al. Susceptibility of ferrets, cats, dogs, and other domesticated animals to SARS-coronavirus 2. Science 2020, 368, 1016–1020. [Google Scholar] [CrossRef] [PubMed]
- Gaudreault, N.N.; Trujillo, J.D.; Carossino, M.; Meekins, D.A.; Morozov, I.; Madden, D.W.; Indran, S.V.; Bold, D.; Balaraman, V.; Kwon, T.; et al. SARS-CoV-2 infection, disease and transmission in domestic cats. Emerg. Microbes Infect. 2020, 9, 2322–2332. [Google Scholar] [CrossRef] [PubMed]
- Bosco-Lauth, A.M.; Hartwig, A.E.; Porter, S.M.; Gordy, P.W.; Nehring, M.; Byas, A.D.; VandeWoude, S.; Ragan, I.K.; Maison, R.M.; Bowen, R.A. Experimental infection of domestic dogs and cats with SARS-CoV-2: Pathogenesis, transmission, and response to reexposure in cats. Proc. Natl. Acad. Sci. USA 2020, 117, 26382–26388. [Google Scholar] [CrossRef] [PubMed]
- Halfmann, P.J.; Hatta, M.; Chiba, S.; Maemura, T.; Fan, S.; Takeda, M.; Kinoshita, N.; Hattori, S.-i.; Sakai-Tagawa, Y.; Iwatsuki-Horimoto, K.; et al. Transmission of SARS-CoV-2 in domestic cats. N. Engl. J. Med. 2020, 383, 592–594. [Google Scholar] [CrossRef]
- Zhang, Q.; Zhang, H.; Gao, J.; Huang, K.; Yang, Y.; Hui, X.; He, X.; Li, C.; Gong, W.; Zhang, Y.; et al. A serological survey of SARS-CoV-2 in cat in Wuhan. Emerg. Microbes Infect. 2020, 9, 2013–2019. [Google Scholar] [CrossRef]
- Patterson, E.I.; Elia, G.; Grassi, A.; Giordano, A.; Desario, C.; Medardo, M.; Smith, S.L.; Anderson, E.R.; Prince, T.; Patterson, G.T.; et al. Evidence of exposure to SARS-CoV-2 in cats and dogs from households in Italy. Nat. Commun. 2020, 11, 6231. [Google Scholar] [CrossRef]
- Michelitsch, A.; Schön, J.; Hoffmann, D.; Beer, M.; Wernike, K. The second wave of SARS-CoV-2 circulation-Antibody detection in the domestic cat population in Germany. Viruses 2021, 13, 9. [Google Scholar] [CrossRef]
- Michelitsch, A.; Hoffmann, D.; Wernike, K.; Beer, M. Occurrence of antibodies against SARS-CoV-2 in the domestic cat population of Germany. Vaccines 2020, 8, 772. [Google Scholar] [CrossRef]
- Fritz, M.; Rosolen, B.; Krafft, E.; Becquart, P.; Elguero, E.; Vratskikh, O.; Denolly, S.; Boson, B.; Vanhomwegen, J.; Gouilh, M.A.; et al. High prevalence of SARS-CoV-2 antibodies in pets from COVID-19+ households. One Health 2021, 11, 100192. [Google Scholar] [CrossRef] [PubMed]
- Barroso, R.; Vieira-Pires, A.; Antunes, A.; Fidalgo-Carvalho, I. Susceptibility of pets to SARS-CoV-2 infection: Lessons from a seroepidemiologic survey of cats and dogs in Portugal. Microorganisms 2022, 10, 345. [Google Scholar] [CrossRef] [PubMed]
- Smith, S.L.; Anderson, E.R.; Cansado-Utrilla, C.; Prince, T.; Farrell, S.; Brant, B.; Smyth, S.; Noble, P.-J.M.; Pinchbeck, G.L.; Marshall, N.; et al. SARS-CoV-2 neutralising antibodies in dogs and cats in the United Kingdom. CRVIRO 2021, 2, 100011. [Google Scholar] [CrossRef] [PubMed]
- Goryoka, G.W.; Cossaboom, C.M.; Gharpure, R.; Dawson, P.; Tansey, C.; Rossow, J.; Mrotz, V.; Rooney, J.; Torchetti, M.; Loiacono, C.M.; et al. One health investigation of SARS-CoV-2 infection and seropositivity among pets in households with confirmed human COVID-19 cases-Utah and Wisconsin, 2020. Viruses 2021, 13, 1813. [Google Scholar] [CrossRef] [PubMed]
- Klaus, J.; Zini, E.; Hartmann, K.; Egberink, H.; Kipar, A.; Bergmann, M.; Palizzotto, C.; Zhao, S.; Rossi, F.; Franco, V.; et al. SARS-CoV-2 infection in dogs and cats from southern Germany and northern Italy during the first wave of the COVID-19 pandemic. Viruses 2021, 13, 1453. [Google Scholar] [CrossRef] [PubMed]
- Dileepan, M.; Di, D.; Huang, Q.; Ahmed, S.; Heinrich, D.; Ly, H.; Liang, Y. Seroprevalence of SARS-CoV-2 (COVID-19) exposure in pet cats and dogs in Minnesota, USA. Virulence 2021, 12, 1597–1609. [Google Scholar] [CrossRef]
- Stevanovic, V.; Vilibic-Cavlek, T.; Tabain, I.; Benvin, I.; Kovac, S.; Hruskar, Z.; Mauric, M.; Milasincic, L.; Antolasic, L.; Skrinjaric, A.; et al. Seroprevalence of SARS-CoV-2 infection among pet animals in Croatia and potential public health impact. Transbound. Emerg. Dis. 2021, 68, 1767–1773. [Google Scholar] [CrossRef]
- Go, Y.Y.; Carrai, M.; Choi, Y.R.; Brackman, C.J.; Tam, K.W.S.; Law, P.Y.T.; Woodhouse, F.; Gray, J.; Kim, J.H.; Park, J.; et al. Low Prevalence of SARS-CoV-2 Antibodies in Canine and Feline Serum Samples Collected during the COVID-19 Pandemic in Hong Kong and Korea. Viruses 2023, 15, 582. [Google Scholar] [CrossRef]
- El-Tholoth, M.; Hussein, M.; Mohammed, D.; Al-Rasheedi, M.; Al-Qubaisi, H.; Al-Blooshi, A.; Al-Ahbabi, M.; Al-Dhaheri, Z.; Al-Blooshi, K.; Al-Herbawi, M.; et al. Serological investigation on the presence of feline coronavirus (FCoV) and severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in domestic cats living with COVID-19 positive owners in the UAE, 2022. Animals 2023, 13, 493. [Google Scholar] [CrossRef]
- Sirakov, I.; Rusenova, N.; Rusenov, A.; Gergova, R.; Strateva, T. Human ELISA Detects anti-SARS-CoV-2 Antibodies in Cats: Seroprevalence and Risk Factors for Virus Spread in Domestic and Stray Cats in Bulgaria. Vet. Sci. 2023, 10, 42. [Google Scholar] [CrossRef]
- Nielsen, S.S.; Alvarez, J.; Bicout, D.J.; Calistri, P.; Canali, E.; Drewe, J.A.; Garin-Bastuji, B.; Gonzales Rojas, J.L.; Gortázar, C.; Herskin, M.; et al. SARS-CoV-2 in animals: Susceptibility of animal species, risk for animal and public health, monitoring, prevention and control. Efsa J. 2023, 21, e07822. [Google Scholar] [CrossRef] [PubMed]
- Sila, T.; Sunghan, J.; Laochareonsuk, W.; Surasombatpattana, S.; Kongkamol, C.; Ingviya, T.; Siripaitoon, P.; Kositpantawong, N.; Kanchanasuwan, S.; Hortiwakul, T.; et al. Suspected cat-to-human transmission of SARS-CoV-2, Thailand, July–September 2021. Emerg. Infect. Dis. 2022, 28, 1485. [Google Scholar] [CrossRef] [PubMed]
- Oude Munnink, B.B.; Sikkema, R.S.; Nieuwenhuijse, D.F.; Molenaar, R.J.; Munger, E.; Molenkamp, R.; van der Spek, A.; Tolsma, P.; Rietveld, A.; Brouwer, M.; et al. Transmission of SARS-CoV-2 on mink farms between humans and mink and back to humans. Science 2021, 371, 172–177. [Google Scholar] [CrossRef] [PubMed]
- Larsen, H.D.; Fonager, J.; Lomholt, F.K.; Dalby, T.; Benedetti, G.; Kristensen, B.; Urth, T.R.; Rasmussen, M.; Lassaunière, R.; Rasmussen, T.B.; et al. Preliminary report of an outbreak of SARS-CoV-2 in mink and mink farmers associated with community spread, Denmark, June to November 2020. Euro Surveill. 2021, 26, 2100009. [Google Scholar] [CrossRef] [PubMed]
- Hammer, A.S.; Quaade, M.L.; Rasmussen, T.B.; Fonager, J.; Rasmussen, M.; Mundbjerg, K.; Lohse, L.; Strandbygaard, B.; Jørgensen, C.S.; Alfaro-Núñez, A.; et al. SARS-CoV-2 transmission between mink (Neovison vison) and humans, Denmark. Emerg. Infect. Dis. 2021, 27, 547–551. [Google Scholar] [CrossRef]
- Koopmans, M. SARS-CoV-2 and the human-animal interface: Outbreaks on mink farms. Lancet Infect. Dis. 2021, 21, 18–19. [Google Scholar] [CrossRef]
- Haagmans, B.L.; Koopmans, M.P.G. Spreading of SARS-CoV-2 from hamsters to humans. Lancet 2022, 399, 1027–1028. [Google Scholar] [CrossRef]
- Yen, H.L.; Sit, T.H.C.; Brackman, C.J.; Chuk, S.S.Y.; Gu, H.; Tam, K.W.S.; Law, P.Y.T.; Leung, G.M.; Peiris, M.; Poon, L.L.M. Transmission of SARS-CoV-2 delta variant (AY.127) from pet hamsters to humans, leading to onward human-to-human transmission: A case study. Lancet 2022, 399, 1070–1078. [Google Scholar] [CrossRef]
- Zhou, J.; Peacock, T.P.; Brown, J.C.; Goldhill, D.H.; Elrefaey, A.M.E.; Penrice-Randal, R.; Cowton, V.M.; De Lorenzo, G.; Furnon, W.; Harvey, W.T.; et al. Mutations that adapt SARS-CoV-2 to mink or ferret do not increase fitness in the human airway. Cell Rep. 2022, 38, 110344. [Google Scholar] [CrossRef]
- Goldhill, D.H.; Barclay, W.S. 2020 Hindsight: Should evolutionary virologists have expected the unexpected during a pandemic? Evolution 2021, 75, 2311–2316. [Google Scholar] [CrossRef]
- Goodman, L.A. Snowball sampling. AMS 1961, 32, 148–170. [Google Scholar] [CrossRef]
- Baltar, F.; Brunet, I. Social research 2.0: Virtual snowball sampling method using Facebook. Internet Res. 2012, 22, 57–74. [Google Scholar] [CrossRef]
- Schulz, C.; Wylezich, C.; Wernike, K.; Gründl, M.; Dangel, A.; Baechlein, C.; Hoffmann, D.; Röhrs, S.; Hepner, S.; Ackermann, N.; et al. Prolonged SARS-CoV-2 RNA shedding from therapy cat after cluster outbreak in retirement home. Emerg. Infect. Dis. 2021, 27, 1974–1976. [Google Scholar] [CrossRef] [PubMed]
- Wernike, K.; Aebischer, A.; Michelitsch, A.; Hoffmann, D.; Freuling, C.; Balkema-Buschmann, A.; Graaf, A.; Müller, T.; Osterrieder, N.; Rissmann, M.; et al. Multi-species ELISA for the detection of antibodies against SARS-CoV-2 in animals. Transbound. Emerg. Dis. 2021, 68, 1779–1785. [Google Scholar] [CrossRef]
- Fowler, F.J.J. How unclear terms affect survey data. Public Opin. Q. 1992, 56, 218–231. [Google Scholar] [CrossRef]
- Robinson, M.A. Using multi-item psychometric scales for research and practice in human resource management. Hum. Resour. Manag. 2018, 57, 739–750. [Google Scholar] [CrossRef]
- Akaike, H. A new look at the statistical model identification. IEEE Trans. Autom. Control. 1974, 19, 716–723. [Google Scholar] [CrossRef]
- Akaike, H. Information theory and an extension of the maximum likelihood principle. In Selected Papers of Hirotugu Akaike; Springer: Berlin/Heidelberg, Germany, 1998; pp. 199–213. [Google Scholar]
- Croux, C.; Dhaene, G.; Hoorelbeke, D. Robust standard errors for robust estimators. CES-Discuss. Pap. Ser. (DPS) 2004, 3, 1–20. [Google Scholar]
- Kulldorff, M.; Nagarwalla, N. Spatial disease clusters: Detection and inference. Stat. Med. 1995, 14, 799–810. [Google Scholar] [CrossRef]
- Kulldorff, M.; Athas, W.F.; Feurer, E.J.; Miller, B.A.; Key, C.R. Evaluating cluster alarms: A space-time scan statistic and brain cancer in Los Alamos, New Mexico. Am. J. Public Health 1998, 88, 1377–1380. [Google Scholar] [CrossRef]
- Brown, L.D.; Cai, T.T.; DasGupta, A. Interval estimation for a binomial proportion. Stat. Sci. 2001, 16, 101–133. [Google Scholar] [CrossRef]
- Rogan, W.J.; Gladen, B. Estimating prevalence from the results of a screening test. Am. J. Epidemiol. 1978, 107, 71–76. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2017. [Google Scholar]
- Zeileis, A.; Köll, S.; Graham, N. Various versatile variances: An object-oriented implementation of clustered covariances in R. J. Stat. Softw. 2020, 95, 1–36. [Google Scholar] [CrossRef]
- Zeileis, A. Econometric computing with HC and HAC covariance matrix estimators. J. Stat. Softw. 2004, 11, 1–17. [Google Scholar] [CrossRef]
- Zeileis, A.; Hothorn, T. Diagnostic checking in regression relationships. R News 2002, 28, 7–10. [Google Scholar]
- Wickham, R. ggplot2: Elegant Graphics for Data Analysis; Springer-Verlag: New York, NY, USA, 2009. [Google Scholar]
- Lex, A.; Gehlenborg, N.; Strobelt, H.; Vuillemot, R.; Pfister, H. UpSet: Visualization of intersecting sets. IEEE Trans. Vis. Comput. Graph. 2014, 20, 1983–1992. [Google Scholar] [CrossRef]
- Conway, J.R.; Lex, A.; Gehlenborg, N. UpSetR: An R package for the visualization of intersecting sets and their properties. Bioinformatics 2017, 33, 2938–2940. [Google Scholar] [CrossRef]
- DeStatis. Kreisfreie Städte und Landkreise nach Fläche, Bevölkerung und Bevölkerungsdichte am 31.12.2020. Available online: https://www.destatis.de/DE/Themen/Laender-Regionen/Regionales/Gemeindeverzeichnis/Administrativ/04-kreise.html (accessed on 7 July 2022).
- Adler, J.M.; Weber, C.; Wernike, K.; Michelitsch, A.; Friedrich, K.; Trimpert, J.; Beer, M.; Kohn, B.; Osterrieder, K.; Müller, E. Prevalence of anti-severe acute respiratory syndrome coronavirus 2 antibodies in cats in Germany and other European countries in the early phase of the coronavirus disease-19 pandemic. Zoonoses Public Health 2022, 69, 439–450. [Google Scholar] [CrossRef]
- Schulz, C.; Martina, B.; Mirolo, M.; Müller, E.; Klein, R.; Volk, H.; Egberink, H.; Gonzalez-Hernandez, M.; Kaiser, F.; von Köckritz-Blickwede, M.; et al. SARS-CoV-2–specific antibodies in domestic cats during first COVID-19 wave, Europe. Emerg. Infect. Dis. J. 2021, 27, 3115. [Google Scholar] [CrossRef]
- Barua, S.; Hoque, M.; Adekanmbi, F.; Kelly, P.; Jenkins-Moore, M.; Torchetti, M.K.; Chenoweth, K.; Wood, T.; Wang, C. Antibodies to SARS-CoV-2 in dogs and cats, USA. Emerg. Microbes Infect. 2021, 10, 1669–1674. [Google Scholar] [CrossRef]
- Oliveira, A.; Pereira, M.A.; Mateus, T.L.; Mesquita, J.R.; Vala, H. Seroprevalence of SARS-CoV-2 in Client-Owned Cats from Portugal. Vet. Sci. 2022, 9, 363. [Google Scholar] [CrossRef] [PubMed]
- Guo, R.; Wolff, C.; Prada, J.M.; Mughini-Gras, L. When COVID-19 sits on people’s laps: A systematic review of SARS-CoV-2 infection prevalence in household dogs and cats. One Health 2023, 16, 100497. [Google Scholar] [CrossRef]
- Meisner, J.; Baszler, T.V.; Kuehl, K.H.; Ramirez, V.; Baines, A.; Frisbie, L.A.; Lofgren, E.T.; DeAvila, D.M.; Wolking, R.M.; Bradway, D.S.; et al. Household transmission of SARS-CoV-2 from humans to pets in Washington and Idaho: Burden and risk factors. bioRxiv 2022, arXiv:24.440952. [Google Scholar] [CrossRef]
- Kannekens-Jager, M.M.; de Rooij, M.M.T.; de Groot, Y.; Biesbroeck, E.; de Jong, M.K.; Pijnacker, T.; Smit, L.A.M.; Schuurman, N.; Broekhuizen-Stins, M.J.; Zhao, S.; et al. SARS-CoV-2 infection in dogs and cats is associated with contact to COVID-19-positive household members. Transbound. Emerg. Dis. 2022, 69, 4034–4040. [Google Scholar] [CrossRef] [PubMed]
- Byambasuren, O.; Cardona, M.; Bell, K.; Clark, J.; McLaws, M.-L.; Glasziou, P. Estimating the extent of asymptomatic COVID-19 and its potential for community transmission: Systematic review and meta-analysis. J. Assoc. Med. Microbiol. 2020, 5, 223–234. [Google Scholar] [CrossRef]
- Oran, D.P.; Topol, E.J. Prevalence of asymptomatic SARS-CoV-2 infection: A narrative review. Ann. Intern. Med. 2020, 173, 362–367. [Google Scholar] [CrossRef]
- Buitrago-Garcia, D.; Egli-Gany, D.; Counotte, M.J.; Hossmann, S.; Imeri, H.; Ipekci, A.M.; Salanti, G.; Low, N. Occurrence and transmission potential of asymptomatic and presymptomatic SARS-CoV-2 infections: A living systematic review and meta-analysis. PLoS Med. 2020, 17, e1003346. [Google Scholar] [CrossRef]
- Schilling, J.; Lehfeld, A.-S.; Schumacher, D.; Ullrich, A.; Diercke, M.; Buda, S.; Haas, W.; Group, R.C.-S. Krankheitsschwere der ersten COVID-19-Welle in Deutschland basierend auf den Meldungen gemäß Infektionsschutzgesetz. J. Health Monit. 2020, 5, 2–20. [Google Scholar] [CrossRef]
- Buonanno, G.; Robotto, A.; Brizio, E.; Morawska, L.; Civra, A.; Corino, F.; Lembo, D.; Ficco, G.; Stabile, L. Link between SARS-CoV-2 emissions and airborne concentrations: Closing the gap in understanding. J. Hazard. Mater. 2022, 428, 128279. [Google Scholar] [CrossRef]
- Rutter, H.; Parker, S.; Stahl-Timmins, W.; Noakes, C.; Smyth, A.; Macbeth, R.; Fitzgerald, S.; Freeman, A.L.J. Visualising SARS-CoV-2 transmission routes and mitigations. BMJ 2021, 375, e065312. [Google Scholar] [CrossRef]
- Jones, B.; Sharpe, P.; Iddon, C.; Hathway, E.A.; Noakes, C.J.; Fitzgerald, S. Modelling uncertainty in the relative risk of exposure to the SARS-CoV-2 virus by airborne aerosol transmission in well mixed indoor air. Build. Environ. 2021, 191, 107617. [Google Scholar] [CrossRef] [PubMed]
- Buonanno, G.; Morawska, L.; Stabile, L. Quantitative assessment of the risk of airborne transmission of SARS-CoV-2 infection: Prospective and retrospective applications. Environ. Int. 2020, 145, 106112. [Google Scholar] [CrossRef] [PubMed]
- Koler-Matznick, J. The origin of the dog revisited. Anthrozoös 2022, 15, 98–118. [Google Scholar] [CrossRef]
- Crowley, S.L.; Cecchetti, M.; McDonald, R.A. Our wild companions: Domestic cats in the anthropocene. Trends Ecol. Evol. 2020, 35, 477–483. [Google Scholar] [CrossRef] [PubMed]
- Alberto-Orlando, S.; Calderon, J.L.; Leon-Sosa, A.; Patiño, L.; Zambrano-Alvarado, M.N.; Pasquel-Villa, L.D.; Rugel-Gonzalez, D.O.; Flores, D.; Mera, M.D.; Valencia, P.; et al. SARS-CoV-2 transmission from infected owner to household dogs and cats is associated to food sharing. Int. J. Infect. Dis. 2022, 122, 295–299. [Google Scholar] [CrossRef]
- Riggio, G.; Borrelli, C.; Piotti, P.; Grondona, A.; Gazzano, A.; Di Iacovo, F.P.; Fatjó, J.; Bowen, J.E.; Mota-Rojas, D.; Pirrone, F.; et al. Cat owner relationship and cat behaviour: Effects of the COVID-19 confinement and implications for feline management. Vet. Sci. 2022, 9, 369. [Google Scholar] [CrossRef]
- Hosie, M.J.; Hofmann-Lehmann, R.; Hartmann, K.; Egberink, H.; Truyen, U.; Addie, D.D.; Belák, S.; Boucraut-Baralon, C.; Frymus, T.; Lloret, A.; et al. Anthropogenic infection of cats during the 2020 COVID-19 pandemic. Viruses 2021, 13, 185. [Google Scholar] [CrossRef]
- WSAVA. The New Coronavirus and Companion Animals—Advice for WSAVA Members. Available online: https://wsava.org/wp-content/uploads/2020/03/COVID-19_WSAVA-Advisory-Document-Mar-19-2020.pdf (accessed on 22 July 2020).
- CDC. What You Need to Know about COVID-19 and Pets. Available online: https://www.cdc.gov/coronavirus/2019-ncov/downloads/covid-19-pets-prevention.pdf (accessed on 22 July 2022).
- Bradshaw, J.; Rooney, N.; Serpell, J. Dog social behavior and communication. In The Domestic Dog: Its Evolution, Behavior and Interactions with People, 2nd ed.; Serpell, J., Ed.; Cambridge University Press: Cambridge, UK, 2017; pp. 133–159. [Google Scholar]
- Westgarth, C.; Christley, R.M.; Pinchbeck, G.L.; Gaskell, R.M.; Dawson, S.; Bradshaw, J.W.S. Dog behaviour on walks and the effect of use of the leash. Appl. Anim. Behav. Sci. 2010, 125, 38–46. [Google Scholar] [CrossRef]
- Bao, L.; Song, Z.; Xue, J.; Gao, H.; Liu, J.; Wang, J.; Guo, Q.; Zhao, B.; Qu, Y.; Qi, F.; et al. Susceptibility and attenuated transmissibility of SARS-CoV-2 in domestic cats. J. Infect. Dis. 2021, 223, 1313–1321. [Google Scholar] [CrossRef]
- Yaglom, H.D.; Hecht, G.; Goedderz, A.; Jasso-Selles, D.; Ely, J.L.; Ruberto, I.; Bowers, J.R.; Engelthaler, D.M.; Venkat, H. Genomic investigation of a household SARS-CoV-2 disease cluster in Arizona involving a cat, dog, and pet owner. One Health 2021, 13, 100333. [Google Scholar] [CrossRef]
- Sit, T.H.C.; Brackman, C.J.; Ip, S.M.; Tam, K.W.S.; Law, P.Y.T.; To, E.M.W.; Yu, V.Y.T.; Sims, L.D.; Tsang, D.N.C.; Chu, D.K.W.; et al. Infection of dogs with SARS-CoV-2. Nature 2020, 586, 776–778. [Google Scholar] [CrossRef]
- Segalés, J.; Puig, M.; Rodon, J.; Avila-Nieto, C.; Carrillo, J.; Cantero, G.; Terrón, M.T.; Cruz, S.; Parera, M.; Noguera-Julián, M.; et al. Detection of SARS-CoV-2 in a cat owned by a COVID-19-affected patient in Spain. Proc. Natl. Acad. Sci. USA 2020, 117, 24790–24793. [Google Scholar] [CrossRef]
- Newman, A.; Smith, D.; Ghai, R.R.; Wallace, R.M.; Torchetti, M.K.; Loiacono, C.; Murrell, L.S.; Carpenter, A.; Moroff, S.; Rooney, J.A.; et al. First reported cases of SARS-CoV-2 infection in companion animals—New York, March-April 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 710–713. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Bastit, L.; Rodon, J.; Pradenas, E.; Marfil, S.; Trinité, B.; Parera, M.; Roca, N.; Pou, A.; Cantero, G.; Lorca-Oró, C.; et al. First detection of SARS-CoV-2 delta (B.1.617.2) variant of concern in a dog with clinical signs in Spain. Viruses 2021, 13, 2526. [Google Scholar] [CrossRef] [PubMed]
- Pascucci, I.; Paniccià, M.; Giammarioli, M.; Biagetti, M.; Duranti, A.; Campomori, P.; Smilari, V.; Ancora, M.; Scialabba, S.; Secondini, B.; et al. SARS-CoV-2 delta VOC in a paucisymptomatic dog, Italy. Pathogens 2022, 11, 514. [Google Scholar] [CrossRef] [PubMed]
- Giraldo-Ramirez, S.; Rendon-Marin, S.; Jaimes, J.A.; Martinez-Gutierrez, M.; Ruiz-Saenz, J. SARS-CoV-2 clinical outcome in domestic and wild cats: A systematic review. Animals 2021, 11, 2056. [Google Scholar] [CrossRef]
- Keller, M.; Hagag, I.T.; Balzer, J.; Beyer, K.; Kersebohm, J.C.; Sadeghi, B.; Wernike, K.; Höper, D.; Wylezich, C.; Beer, M.; et al. Detection of SARS-CoV-2 variant B.1.1.7 in a cat in Germany. Res. Vet. Sci. 2021, 140, 229–232. [Google Scholar] [CrossRef]
- Carpenter, A.; Ghai, R.R.; Gary, J.; Ritter, J.M.; Carvallo, F.R.; Diel, D.G.; Martins, M.; Murphy, J.; Schroeder, B.; Brightbill, K.; et al. Determining the role of natural SARS-CoV-2 infection in the death of domestic pets: 10 cases (2020-2021). J. Am. Vet. Med. Assoc. 2021, 259, 1032–1039. [Google Scholar] [CrossRef]
- RKI. Anzahl und Anteile von VOC und VOI in Deutschland. Available online: https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Daten/VOC_VOI_Tabelle.html (accessed on 12 May 2022).

| Cats | Dogs | |||||||
|---|---|---|---|---|---|---|---|---|
| Positive | Negative | Positive | Negative | |||||
| Number of participants | 48 | 67 | 95 | 75 | ||||
| Mean | sd * | Mean | sd | Mean | sd | Mean | sd | |
| Age (years) | 6.2 | 5.5 | 6.3 | 5.4 | 6.8 | 3.9 | 5.2 | 4.1 |
| Infected humans (n) | 2.4 | 1.2 | 1.8 | 0.9 | 2.1 | 1.1 | 1.8 | 1.0 |
| n | prop. ** | n | prop. | n | prop. | n | prop. | |
| Male | 30 | 62.5 | 39 | 58.2 | 45 | 47.4 | 30 | 40.0 |
| One or more chronic diseases | 10 | 20.8 | 16 | 23.9 | 29 | 30.5 | 18 | 24.0 |
| Unsupervised outdoor access | 14 | 29.2 | 32 | 47.8 | 21 | 22.1 | 12 | 16.0 |
| Contact outside the household | 3 | 6.3 | 12 | 17.9 | 35 | 36.8 | 17 | 22.7 |
| Above-average contact intensity | 32 | 66.7 | 31 | 46.3 | 57 | 60.0 | 35 | 46.7 |
| Reduced contact | 12 | 25.0 | 22 | 32.8 | 20 | 21.1 | 28 | 37.3 |
| Cats | Dogs | |||||||
|---|---|---|---|---|---|---|---|---|
| Positive | Negative | Positive | Negative | |||||
| Number of participants | 48 | 67 | 95 | 75 | ||||
| n | prop. * | n | prop. | n | prop. | n | prop. | |
| Overall symptoms | 22 | 45.8 | 30 | 44.8 | 32 | 33.7 | 35 | 46.7 |
| Respiratory symptoms | 15 | 31.3 | 19 | 28.6 | 17 | 17.9 | 11 | 14.7 |
| Reduced general health | 15 | 31.3 | 19 | 28.6 | 22 | 23.2 | 18 | 24.0 |
| Diarrhea | 5 | 10.4 | 11 | 16.4 | 12 | 12.6 | 21 | 28.0 |
| Cats | Dogs | ||||||
|---|---|---|---|---|---|---|---|
| Variable xi | Coding of xi | OR * | 95% CI ** | p-Value | OR | 95% CI | p-Value |
| Age (years) | ≤ 6 = 0, > 6 = 1 | 1.13 | 0.48–2.66 | 0.79 | 1.35 | 0.66–2.74 | 0.41 |
| Infected humans (n) | One = 0, > one = 1 | 3.08 | 1.11–8.54 | 0.03 | 2.15 | 0.95–4.84 | 0.07 |
| Sex | Female = 0, male = 1 | 1.20 | 0.56–2.57 | 0.64 | 1.35 | 0.76–2.40 | 0.31 |
| One or more chronic diseases | No = 0, yes = 1 | 0.84 | 0.34–2.04 | 0.70 | 1.39 | 0.66–2.92 | 0.38 |
| Unsupervised outdoor access | No = 0, yes = 1 | 0.45 | 0.18–1.13 | 0.09 | 1.49 | 0.60–3.70 | 0.39 |
| Contact outside the household | No = 0, yes = 1 | 0.31 | 0.06–1.45 | 0.14 | 1.99 | 0.89–4.45 | 0.09 |
| Above-average contact intensity | No = 0, yes = 1 | 2.32 | 0.96–5.62 | 0.06 | 1.71 | 0.75–3.91 | 0.20 |
| Reduced contact | No = 0, yes *** = 1 | 0.68 | 0.24–1.9 | 0.46 | 0.45 | 0.17–1.18 | 0.10 |
| Cats | Dogs | ||||||
|---|---|---|---|---|---|---|---|
| Variable xi | Coding of xi | OR * | 95% CI ** | p-Value | OR | 95% CI | p-Value |
| Overall symptoms | No = 0, yes = 1 | 1.04 | 0.45–2.40 | 0.92 | 0.58 | 0.25–1.32 | 0.20 |
| Respiratory symptoms | No = 0, yes = 1 | 1.15 | 0.49–2.71 | 0.75 | 1.27 | 0.51–3.17 | 0.61 |
| Reduced general health | No = 0, yes = 1 | 1.15 | 0.49–2.71 | 0.75 | 0.95 | 0.41–2.21 | 0.91 |
| Diarrhea | No = 0, yes = 1 | 0.59 | 0.16–2.18 | 0.43 | 0.37 | 0.11–1.21 | 0.10 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Michelitsch, A.; Allendorf, V.; Conraths, F.J.; Gethmann, J.; Schulz, J.; Wernike, K.; Denzin, N. SARS-CoV-2 Infection and Clinical Signs in Cats and Dogs from Confirmed Positive Households in Germany. Viruses 2023, 15, 837. https://doi.org/10.3390/v15040837
Michelitsch A, Allendorf V, Conraths FJ, Gethmann J, Schulz J, Wernike K, Denzin N. SARS-CoV-2 Infection and Clinical Signs in Cats and Dogs from Confirmed Positive Households in Germany. Viruses. 2023; 15(4):837. https://doi.org/10.3390/v15040837
Chicago/Turabian StyleMichelitsch, Anna, Valerie Allendorf, Franz Josef Conraths, Jörn Gethmann, Jana Schulz, Kerstin Wernike, and Nicolai Denzin. 2023. "SARS-CoV-2 Infection and Clinical Signs in Cats and Dogs from Confirmed Positive Households in Germany" Viruses 15, no. 4: 837. https://doi.org/10.3390/v15040837
APA StyleMichelitsch, A., Allendorf, V., Conraths, F. J., Gethmann, J., Schulz, J., Wernike, K., & Denzin, N. (2023). SARS-CoV-2 Infection and Clinical Signs in Cats and Dogs from Confirmed Positive Households in Germany. Viruses, 15(4), 837. https://doi.org/10.3390/v15040837







