miRNAs in Herpesvirus Infection: Powerful Regulators in Small Packages
Abstract
1. Introduction
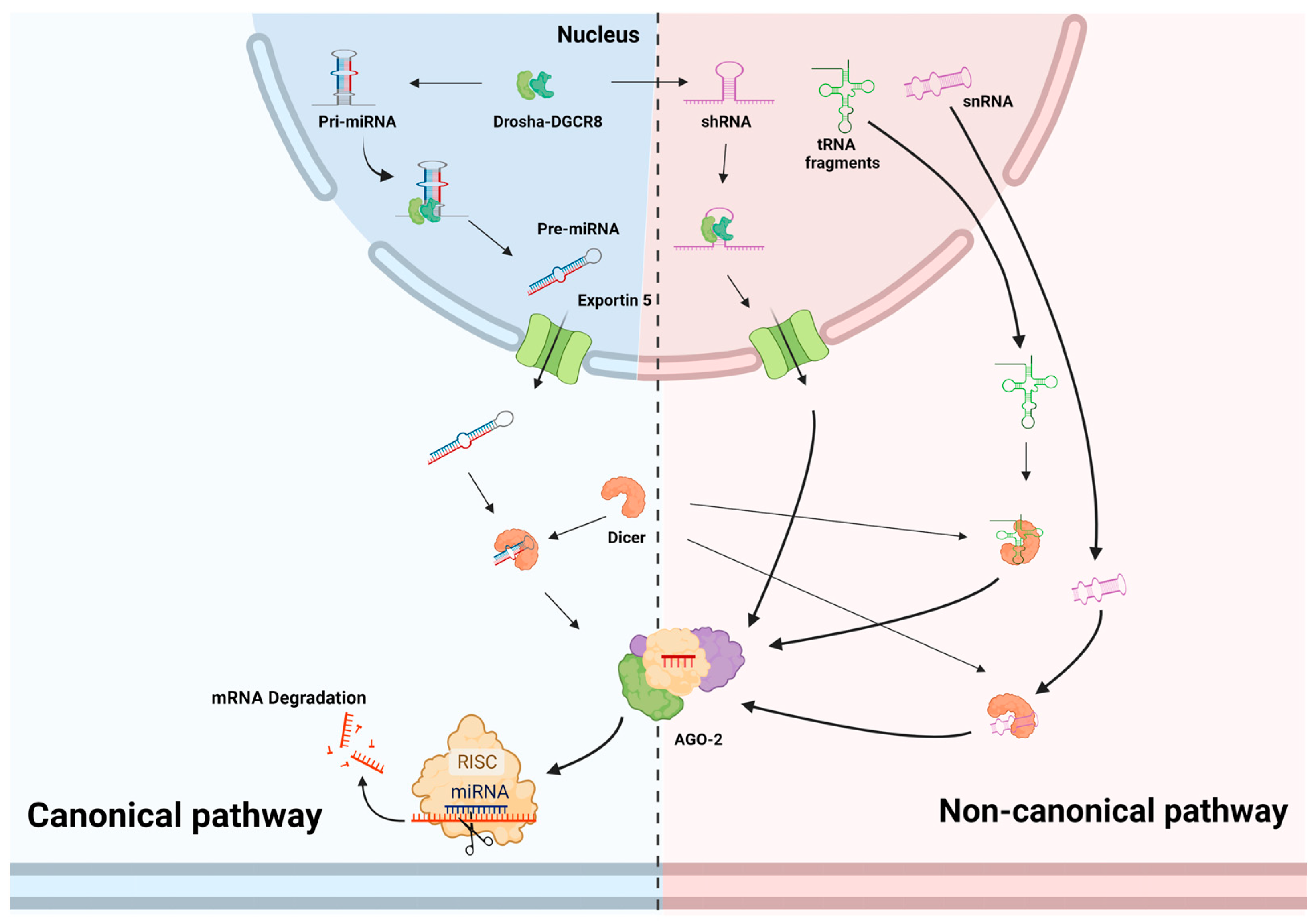
2. General Overview and Synthesis of miRNA
2.1. Canonical Pathway for miRNA Synthesis
2.1.1. Synthesis of Cellular miRNAs
2.1.2. Synthesis of Viral miRNAs
2.2. Noncanonical Pathway for miRNA Synthesis
3. miRNA and Herpes Virus
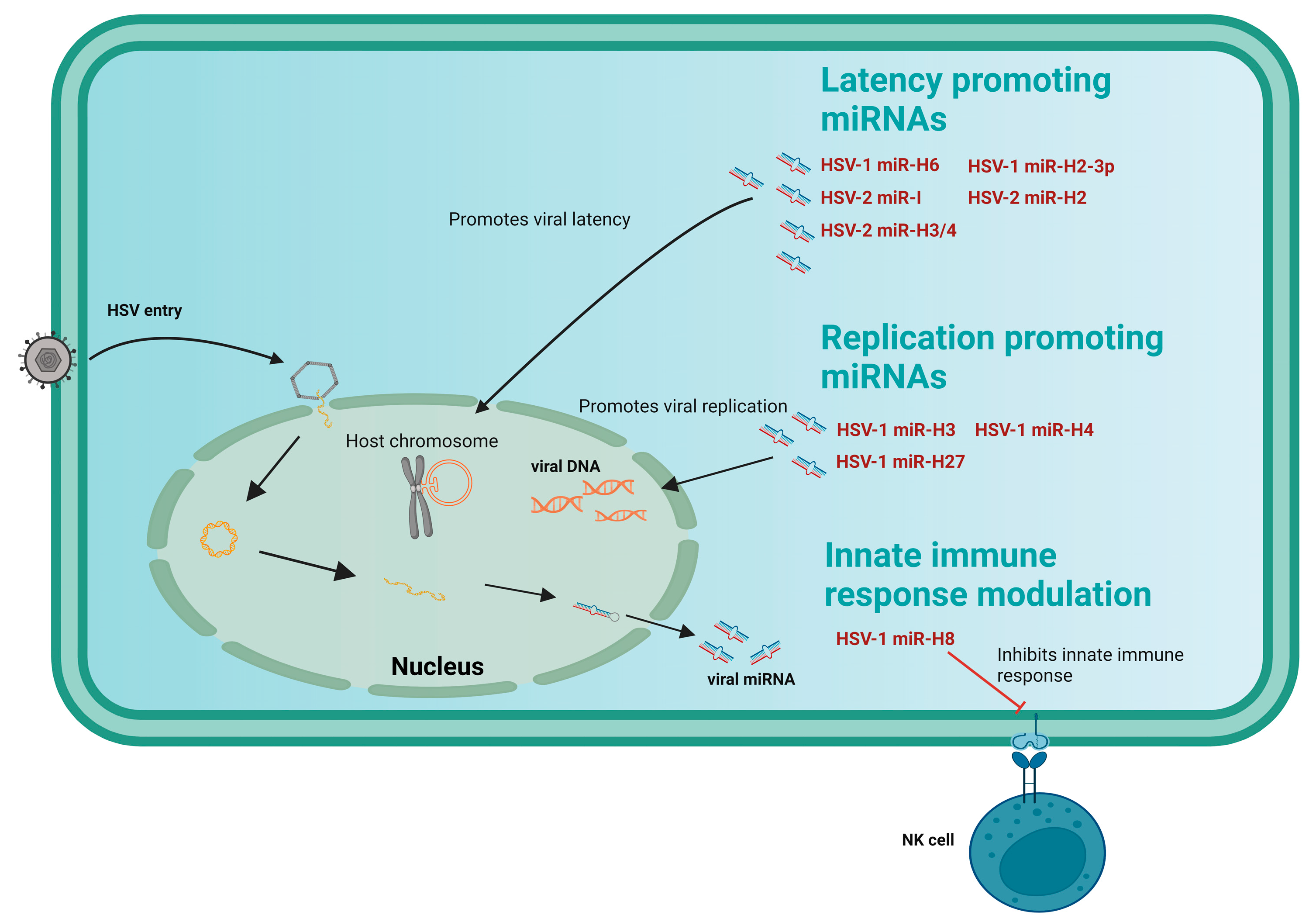
3.1. Role of miRNAs in HSV Infection
3.1.1. Role of Cellular miRNAs in HSV Replication
3.1.2. Role of Viral miRNAs in HSV Replication
3.1.3. Role of miRNAs in HSV Latency
3.1.4. Immunopathological Consequence of HSV Infection
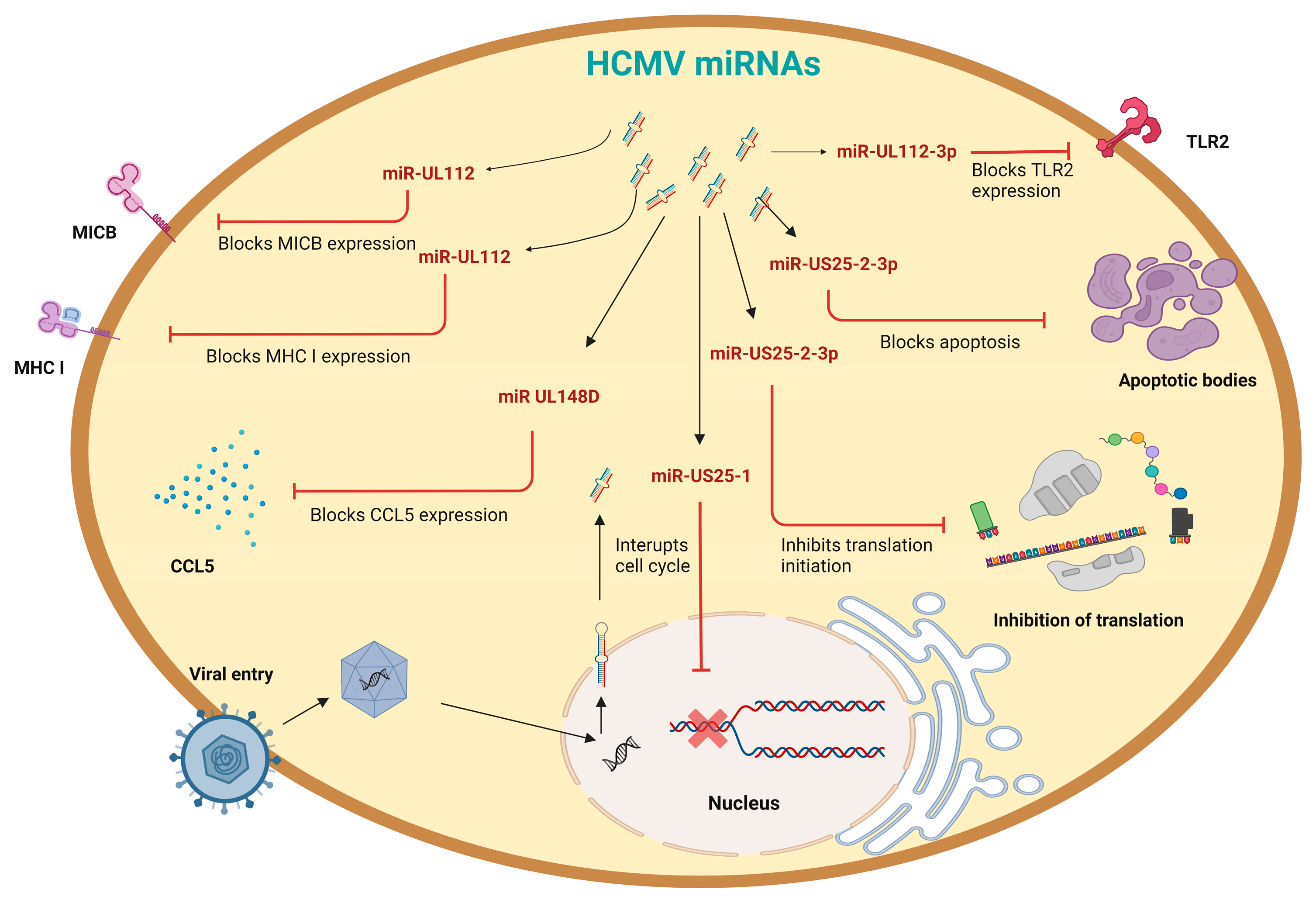
3.2. miRNAs in Human Cytomegalovirus Infection
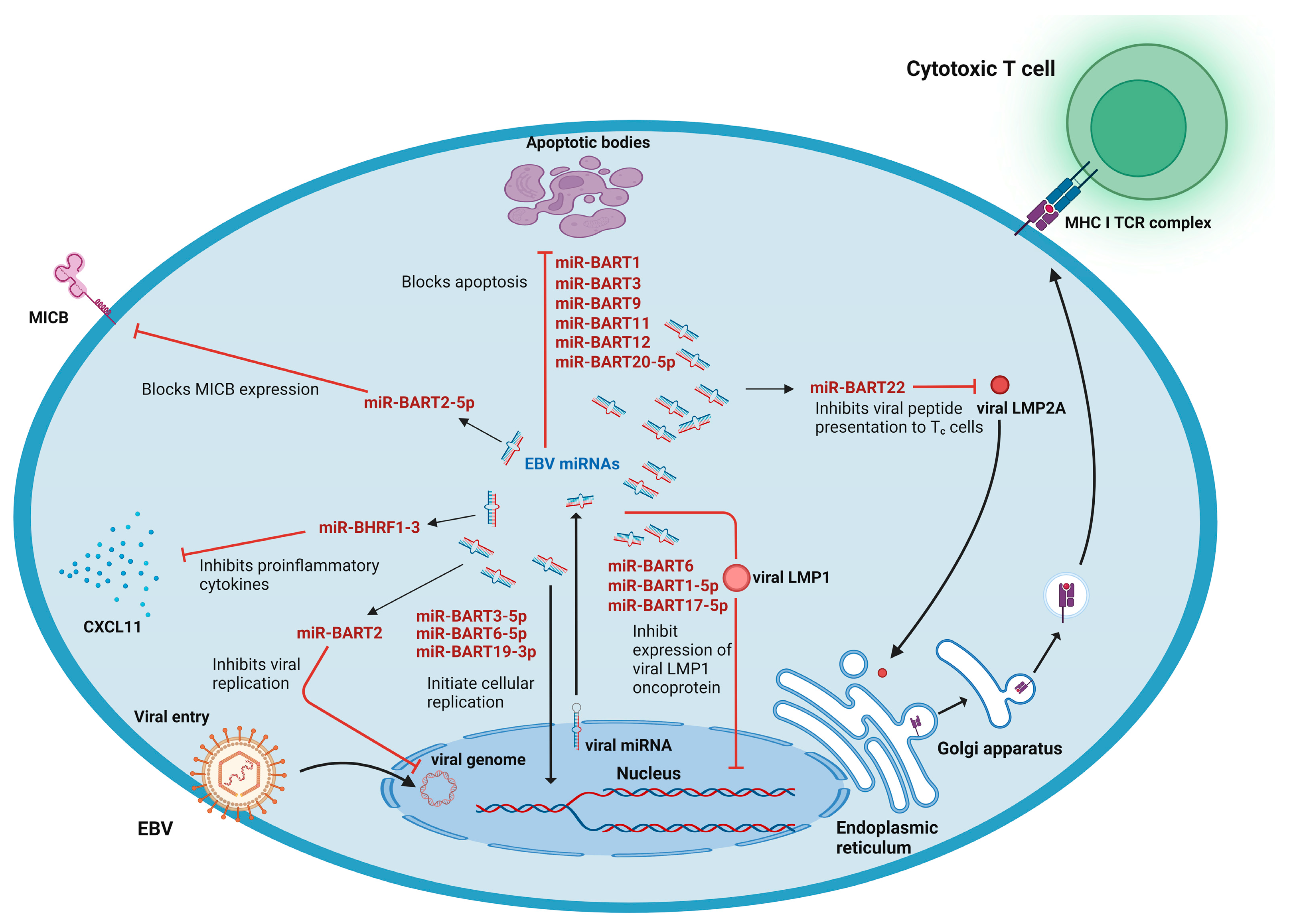
3.3. miRNAs in Epstein–Barr Virus (EBV) Infection
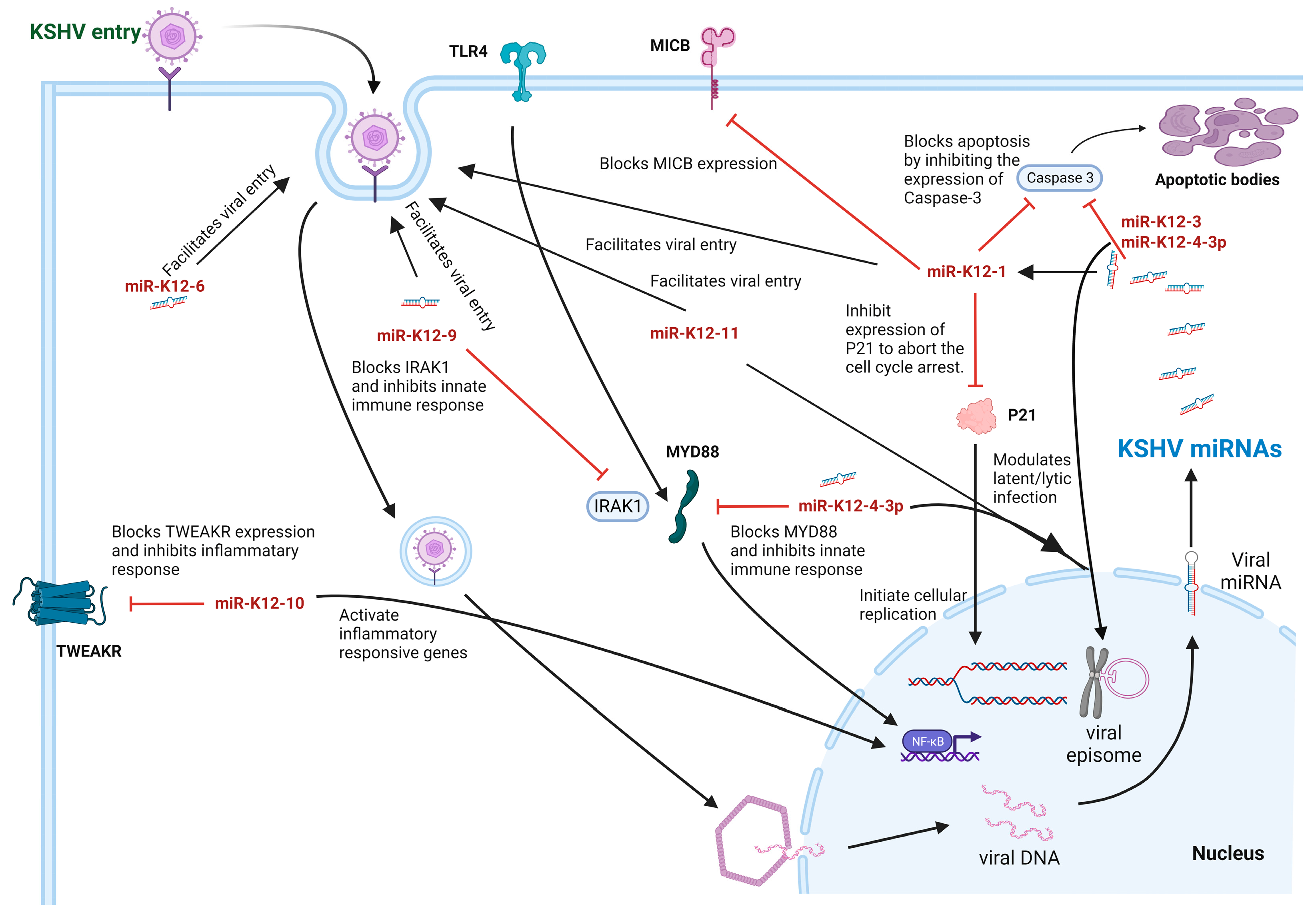
3.4. miRNAs in Kaposi’s Sarcoma-Associated Herpes Virus (HHV-8/KSHV) Infection
4. miRNAs as Potential Biomarkers
4.1. miRNAs as Potential Biomarker during Herpes Virus Infection
4.2. Limitations of miRNAs as Biomarkers
5. Therapeutic Considerations
6. Future Perspectives
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lee, R.C.; Feinbaum, R.L.; Ambros, V. The C. Elegans Heterochronic Gene Lin-4 Encodes Small RNAs with Antisense Complementarity to Lin-14. Cell 1993, 75, 843–854. [Google Scholar] [CrossRef] [PubMed]
- Cai, Z.; Jia, R. Progress on the Function of Herpesvirus-encoded MicroRNAs. Bing Du Xue Bao 2015, 31, 704–711. [Google Scholar]
- Friedman, R.C.; Farh, K.K.-H.; Burge, C.B.; Bartel, D.P. Most Mammalian MRNAs Are Conserved Targets of MicroRNAs. Genome Res. 2009, 19, 92–105. [Google Scholar] [CrossRef] [PubMed]
- Banerjee, A.; Kulkarni, S.; Mukherjee, A. Herpes Simplex Virus: The Hostile Guest That Takes Over Your Home. Front. Microbiol. 2020, 11, 733. [Google Scholar] [CrossRef] [PubMed]
- Cullen, B.R. Herpesvirus MicroRNAs: Phenotypes and Functions. Curr. Opin. Virol. 2011, 1, 211–215. [Google Scholar] [CrossRef]
- Deshmane, S.L.; Fraser, N.W. During Latency, Herpes Simplex Virus Type 1 DNA Is Associated with Nucleosomes in a Chromatin Structure. J. Virol. 1989, 63, 943–947. [Google Scholar] [CrossRef]
- Grey, F. Role of MicroRNAs in Herpesvirus Latency and Persistence. J. Gen. Virol. 2015, 96, 739–751. [Google Scholar] [CrossRef]
- Jochum, S.; Moosmann, A.; Lang, S.; Hammerschmidt, W.; Zeidler, R. The EBV Immunoevasins VIL-10 and BNLF2a Protect Newly Infected B Cells from Immune Recognition and Elimination. PLoS Pathog. 2012, 8, e1002704. [Google Scholar] [CrossRef]
- Grey, F.; Hook, L.; Nelson, J. The Functions of Herpesvirus-Encoded MicroRNAs. Med. Microbiol. Immunol. 2008, 197, 261–267. [Google Scholar] [CrossRef]
- Cui, C.; Griffiths, A.; Li, G.; Silva, L.M.; Kramer, M.F.; Gaasterland, T.; Wang, X.-J.; Coen, D.M. Prediction and Identification of Herpes Simplex Virus 1-Encoded MicroRNAs. J. Virol. 2006, 80, 5499–5508. [Google Scholar] [CrossRef]
- Umbach, J.L.; Kramer, M.F.; Jurak, I.; Karnowski, H.W.; Coen, D.M.; Cullen, B.R. MicroRNAs Expressed by Herpes Simplex Virus 1 during Latent Infection Regulate Viral MRNAs. Nature 2008, 454, 780–783. [Google Scholar] [CrossRef] [PubMed]
- Umbach, J.L.; Wang, K.; Tang, S.; Krause, P.R.; Mont, E.K.; Cohen, J.I.; Cullen, B.R. Identification of Viral MicroRNAs Expressed in Human Sacral Ganglia Latently Infected with Herpes Simplex Virus 2. J. Virol. 2010, 84, 1189–1192. [Google Scholar] [CrossRef] [PubMed]
- Hook, L.; Hancock, M.; Landais, I.; Grabski, R.; Britt, W.; Nelson, J.A. Cytomegalovirus MicroRNAs. Curr. Opin. Virol. 2014, 7, 40–46. [Google Scholar] [CrossRef] [PubMed]
- Pfeffer, S.; Zavolan, M.; Grässer, F.A.; Chien, M.; Russo, J.J.; Ju, J.; John, B.; Enright, A.J.; Marks, D.; Sander, C.; et al. Identification of Virus-Encoded MicroRNAs. Science 2004, 304, 734–736. [Google Scholar] [CrossRef] [PubMed]
- Pfeffer, S.; Sewer, A.; Lagos-Quintana, M.; Sheridan, R.; Sander, C.; Grässer, F.A.; van Dyk, L.F.; Ho, C.K.; Shuman, S.; Chien, M.; et al. Identification of MicroRNAs of the Herpesvirus Family. Nat. Methods 2005, 2, 269–276. [Google Scholar] [CrossRef]
- Piedade, D.; Azevedo-Pereira, J. The Role of MicroRNAs in the Pathogenesis of Herpesvirus Infection. Viruses 2016, 8, 156. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, J.; Hayder, H.; Zayed, Y.; Peng, C. Overview of MicroRNA Biogenesis, Mechanisms of Actions, and Circulation. Front. Endocrinol. 2018, 9, 402. [Google Scholar] [CrossRef]
- Lee, Y.; Ahn, C.; Han, J.; Choi, H.; Kim, J.; Yim, J.; Lee, J.; Provost, P.; Rådmark, O.; Kim, S.; et al. The Nuclear RNase III Drosha Initiates MicroRNA Processing. Nature 2003, 425, 415–419. [Google Scholar] [CrossRef]
- Denli, A.M.; Tops, B.B.J.; Plasterk, R.H.A.; Ketting, R.F.; Hannon, G.J. Processing of Primary MicroRNAs by the Microprocessor Complex. Nature 2004, 432, 231–235. [Google Scholar] [CrossRef]
- Yi, R.; Qin, Y.; Macara, I.G.; Cullen, B.R. Exportin-5 Mediates the Nuclear Export of Pre-MicroRNAs and Short Hairpin RNAs. Genes Dev. 2003, 17, 3011–3016. [Google Scholar] [CrossRef]
- Hutvágner, G.; McLachlan, J.; Pasquinelli, A.E.; Bálint, É.; Tuschl, T.; Zamore, P.D. A Cellular Function for the RNA-Interference Enzyme Dicer in the Maturation of the Let-7 Small Temporal RNA. Science 2001, 293, 834–838. [Google Scholar] [CrossRef] [PubMed]
- Chekulaeva, M.; Filipowicz, W. Mechanisms of MiRNA-Mediated Post-Transcriptional Regulation in Animal Cells. Curr. Opin. Cell Biol. 2009, 21, 452–460. [Google Scholar] [CrossRef] [PubMed]
- Brennecke, J.; Stark, A.; Russell, R.B.; Cohen, S.M. Principles of MicroRNA–Target Recognition. PLoS Biol. 2005, 3, e85. [Google Scholar] [CrossRef] [PubMed]
- Piedade, D.; Azevedo-Pereira, J.M. MicroRNAs, HIV and HCV: A Complex Relation towards Pathology. Rev. Med. Virol. 2016, 26, 197–215. [Google Scholar] [CrossRef]
- Abdelfattah, A.M.; Park, C.; Choi, M.Y. Update on Non-Canonical MicroRNAs. Biomol. Concepts 2014, 5, 275–287. [Google Scholar] [CrossRef]
- Kozomara, A.; Griffiths-Jones, S. MiRBase: Integrating MicroRNA Annotation and Deep-Sequencing Data. Nucleic Acids Res. 2011, 39, D152–D157. [Google Scholar] [CrossRef]
- Zhu, Y.; Haecker, I.; Yang, Y.; Gao, S.-J.; Renne, R. γ-Herpesvirus-Encoded MiRNAs and Their Roles in Viral Biology and Pathogenesis. Curr. Opin. Virol. 2013, 3, 266–275. [Google Scholar] [CrossRef]
- Boss, I.W.; Renne, R. Viral MiRNAs and Immune Evasion. Biochim. Biophys. Acta (BBA)-Gene Regul. Mech. 2011, 1809, 708–714. [Google Scholar] [CrossRef]
- Plaisance-Bonstaff, K.; Renne, R. Viral MiRNAs. Methods Mol. Biol. 2011, 721, 43–66. [Google Scholar] [CrossRef]
- Watson, Z.L.; Washington, S.D.; Phelan, D.M.; Lewin, A.S.; Tuli, S.S.; Schultz, G.S.; Neumann, D.M.; Bloom, D.C. In Vivo Knockdown of the Herpes Simplex Virus 1 Latency-Associated Transcript Reduces Reactivation from Latency. J. Virol. 2018, 92, e00812-18. [Google Scholar] [CrossRef]
- Bauman, Y.; Mandelboim, O. MicroRNA Based Immunoevasion Mechanism of Human Polyomaviruses. RNA Biol. 2011, 8, 591–594. [Google Scholar] [CrossRef] [PubMed]
- Stern-Ginossar, N.; Elefant, N.; Zimmermann, A.; Wolf, D.G.; Saleh, N.; Biton, M.; Horwitz, E.; Prokocimer, Z.; Prichard, M.; Hahn, G.; et al. Host Immune System Gene Targeting by a Viral MiRNA. Science 2007, 317, 376–381. [Google Scholar] [CrossRef] [PubMed]
- Bhela, S.; Rouse, B.T. Are MiRNAs Critical Determinants in Herpes Simplex Virus Pathogenesis? Microbes Infect. 2018, 20, 461–465. [Google Scholar] [CrossRef] [PubMed]
- Santhakumar, D.; Forster, T.; Laqtom, N.N.; Fragkoudis, R.; Dickinson, P.; Abreu-Goodger, C.; Manakov, S.A.; Choudhury, N.R.; Griffiths, S.J.; Vermeulen, A.; et al. Combined Agonist–Antagonist Genome-Wide Functional Screening Identifies Broadly Active Antiviral MicroRNAs. Proc. Natl. Acad. Sci. USA 2010, 107, 13830–13835. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, K.; Suemasa, F.; Sagara, H.; Nakamura, S.; Ino, Y.; Kobayashi, K.; Hiramatsu, H.; Haraguchi, T.; Kurokawa, K.; Todo, T.; et al. MiR-199a Inhibits Secondary Envelopment of Herpes Simplex Virus-1 Through the Downregulation of Cdc42-Specific GTPase Activating Protein Localized in Golgi Apparatus. Sci. Rep. 2017, 7, 6650. [Google Scholar] [CrossRef]
- Zhang, Y.; Dai, J.; Tang, J.; Zhou, L.; Zhou, M. MicroRNA-649 Promotes HSV-1 Replication by Directly Targeting MALT1. J. Med. Virol. 2017, 89, 1069–1079. [Google Scholar] [CrossRef]
- Wang, X.; Diao, C.; Yang, X.; Yang, Z.; Liu, M.; Li, X.; Tang, H. ICP4-Induced MiR-101 Attenuates HSV-1 Replication. Sci. Rep. 2016, 6, 23205. [Google Scholar] [CrossRef]
- Zheng, S.; Li, Y.; Zhang, Y.; Li, X.; Tang, H. MiR-101 Regulates HSV-1 Replication by Targeting ATP5B. Antivir. Res. 2011, 89, 219–226. [Google Scholar] [CrossRef]
- Ru, J.; Sun, H.; Fan, H.; Wang, C.; Li, Y.; Liu, M.; Tang, H. MiR-23a Facilitates the Replication of HSV-1 through the Suppression of Interferon Regulatory Factor 1. PLoS ONE 2014, 9, e114021. [Google Scholar] [CrossRef]
- Xie, Y.; He, S.; Wang, J. MicroRNA-373 Facilitates HSV-1 Replication through Suppression of Type I IFN Response by Targeting IRF1. Biomed. Pharmacother. 2018, 97, 1409–1416. [Google Scholar] [CrossRef]
- Lagos, D.; Pollara, G.; Henderson, S.; Gratrix, F.; Fabani, M.; Milne, R.S.B.; Gotch, F.; Boshoff, C. MiR-132 Regulates Antiviral Innate Immunity through Suppression of the P300 Transcriptional Co-Activator. Nat. Cell Biol. 2010, 12, 513–519. [Google Scholar] [CrossRef] [PubMed]
- Duan, F.; Liao, J.; Huang, Q.; Nie, Y.; Wu, K. HSV-1 MiR-H6 Inhibits HSV-1 Replication and IL-6 Expression in Human Corneal Epithelial Cells In Vitro. Clin. Dev. Immunol. 2012, 2012, 192791. [Google Scholar] [CrossRef] [PubMed]
- Duan, Y.; Zeng, J.; Fan, S.; Liao, Y.; Feng, M.; Wang, L.; Zhang, Y.; Li, Q. Herpes Simplex Virus Type 1–Encoded MiR-H2-3p Manipulates Cytosolic DNA–Stimulated Antiviral Innate Immune Response by Targeting DDX41. Viruses 2019, 11, 756. [Google Scholar] [CrossRef] [PubMed]
- Enk, J.; Levi, A.; Weisblum, Y.; Yamin, R.; Charpak-Amikam, Y.; Wolf, D.G.; Mandelboim, O. HSV1 MicroRNA Modulation of GPI Anchoring and Downstream Immune Evasion. Cell Rep. 2016, 17, 949–956. [Google Scholar] [CrossRef]
- Wu, W.; Guo, Z.; Zhang, X.; Guo, L.; Liu, L.; Liao, Y.; Wang, J.; Wang, L.; Li, Q. A MicroRNA Encoded by HSV-1 Inhibits a Cellular Transcriptional Repressor of Viral Immediate Early and Early Genes. Sci. China Life Sci. 2013, 56, 373–383. [Google Scholar] [CrossRef]
- Everett, R.D. ICP0, a regulator of herpes simplex virus during lytic and latent infection. Bioessays 2000, 22, 761–770. [Google Scholar] [CrossRef]
- Pan, D.; Flores, O.; Umbach, J.L.; Pesola, J.M.; Bentley, P.; Rosato, P.C.; Leib, D.A.; Cullen, B.R.; Coen, D.M. A Neuron-Specific Host MicroRNA Targets Herpes Simplex Virus-1 ICP0 Expression and Promotes Latency. Cell Host Microbe 2014, 15, 446–456. [Google Scholar] [CrossRef]
- Tang, S.; Bertke, A.S.; Patel, A.; Wang, K.; Cohen, J.I.; Krause, P.R. An Acutely and Latently Expressed Herpes Simplex Virus 2 Viral MicroRNA Inhibits Expression of ICP34.5, a Viral Neurovirulence Factor. Proc. Natl. Acad. Sci. USA 2008, 105, 10931–10936. [Google Scholar] [CrossRef]
- Tang, S.; Patel, A.; Krause, P.R. Novel Less-Abundant Viral MicroRNAs Encoded by Herpes Simplex Virus 2 Latency-Associated Transcript and Their Roles in Regulating ICP34.5 and ICP0 MRNAs. J. Virol. 2009, 83, 1433–1442. [Google Scholar] [CrossRef]
- Han, Z.; Liu, X.; Chen, X.; Zhou, X.; Du, T.; Roizman, B.; Zhou, G. MiR-H28 and MiR-H29 Expressed Late in Productive Infection Are Exported and Restrict HSV-1 Replication and Spread in Recipient Cells. Proc. Natl. Acad. Sci. USA 2016, 113, E894–E901. [Google Scholar] [CrossRef]
- Kim, H.; Iizasa, H.; Kanehiro, Y.; Fekadu, S.; Yoshiyama, H. Herpesviral MicroRNAs in Cellular Metabolism and Immune Responses. Front. Microbiol. 2017, 8, 1318. [Google Scholar] [CrossRef] [PubMed]
- Sun, L.; Li, Q. The MiRNAs of Herpes Simplex Virus (HSV). Virol. Sin. 2012, 27, 332–337. [Google Scholar] [CrossRef]
- Jurak, I.; Kramer, M.F.; Mellor, J.C.; van Lint, A.L.; Roth, F.P.; Knipe, D.M.; Coen, D.M. Numerous Conserved and Divergent MicroRNAs Expressed by Herpes Simplex Viruses 1 and 2. J. Virol. 2010, 84, 4659–4672. [Google Scholar] [CrossRef] [PubMed]
- Tang, S.; Bertke, A.S.; Patel, A.; Margolis, T.P.; Krause, P.R. Herpes Simplex Virus 2 MicroRNA MiR-H6 Is a Novel Latency-Associated Transcript-Associated MicroRNA, but Reduction of Its Expression Does Not Influence the Establishment of Viral Latency or the Recurrence Phenotype. J. Virol. 2011, 85, 4501–4509. [Google Scholar] [CrossRef] [PubMed]
- Louten, J.; Beach, M.; Palermino, K.; Weeks, M.; Holenstein, G. MicroRNAs Expressed during Viral Infection: Biomarker Potential and Therapeutic Considerations. Biomark. Insights 2015, 10, 25–52. [Google Scholar] [CrossRef]
- Lei, X.; Bai, Z.; Ye, F.; Huang, Y.; Gao, S.-J. Regulation of Herpesvirus Lifecycle by Viral MicroRNAs. Virulence 2010, 1, 433–435. [Google Scholar] [CrossRef]
- Bhela, S.; Mulik, S.; Reddy, P.B.J.; Richardson, R.L.; Gimenez, F.; Rajasagi, N.K.; Veiga-Parga, T.; Osmand, A.P.; Rouse, B.T. Critical Role of MicroRNA-155 in Herpes Simplex Encephalitis. J. Immunol. 2014, 192, 2734–2743. [Google Scholar] [CrossRef] [PubMed]
- Sun, B.; Yang, X.; Hou, F.; Yu, X.; Wang, Q.; Oh, H.S.; Raja, P.; Pesola, J.M.; Vanni, E.A.H.; McCarron, S.; et al. Regulation of Host and Virus Genes by Neuronal MiR-138 Favours Herpes Simplex Virus 1 Latency. Nat. Microbiol. 2021, 6, 682–696. [Google Scholar] [CrossRef]
- Chen, S.; Deng, Y.; Chen, H.; Lin, Y.; Yang, X.; Sun, B.; Pan, D. Neuronal MiR-138 Represses HSV-2 Lytic Infection by Regulating Viral and Host Genes with Mechanistic Differences from HSV-1. J. Virol. 2022, 96, e00349-22. [Google Scholar] [CrossRef]
- Chentoufi, A.A.; BenMohamed, L. Mucosal Herpes Immunity and Immunopathology to Ocular and Genital Herpes Simplex Virus Infections. Clin. Dev. Immunol. 2012, 2012, 1–22. [Google Scholar] [CrossRef]
- Biswas, P.S.; Rouse, B.T. Early Events in HSV Keratitis--Setting the Stage for a Blinding Disease. Microbes Infect. 2005, 7, 799–810. [Google Scholar] [CrossRef] [PubMed]
- Podshivalova, K.; Salomon, D.R. MicroRNA Regulation of T-Lymphocyte Immunity: Modulation of Molecular Networks Responsible for T-Cell Activation, Differentiation, and Development. Crit. Rev. Immunol. 2013, 33, 435–476. [Google Scholar] [CrossRef] [PubMed]
- Bhela, S.; Mulik, S.; Gimenez, F.; Reddy, P.B.J.; Richardson, R.L.; Varanasi, S.K.; Jaggi, U.; Xu, J.; Lu, P.Y.; Rouse, B.T. Role of MiR-155 in the Pathogenesis of Herpetic Stromal Keratitis. Am. J. Pathol. 2015, 185, 1073–1084. [Google Scholar] [CrossRef] [PubMed]
- Mulik, S.; Xu, J.; Reddy, P.B.J.; Rajasagi, N.K.; Gimenez, F.; Sharma, S.; Lu, P.Y.; Rouse, B.T. Role of MiR-132 in Angiogenesis after Ocular Infection with Herpes Simplex Virus. Am. J. Pathol. 2012, 181, 525–534. [Google Scholar] [CrossRef]
- Zhang, X.; Dervillez, X.; Chentoufi, A.A.; Badakhshan, T.; Bettahi, I.; Benmohamed, L. Targeting the Genital Tract Mucosa with a Lipopeptide/Recombinant Adenovirus Prime/Boost Vaccine Induces Potent and Long-Lasting CD8+ T Cell Immunity against Herpes: Importance of MyD88. J. Immunol. 2012, 189, 4496–4509. [Google Scholar] [CrossRef]
- Alami Chentoufi, A.; Kritzer, E.; Yu, D.M.; Nesburn, A.B.; BenMohamed, L. Towards a Rational Design of an Asymptomatic Clinical Herpes Vaccine: The Old, the New, and the Unknown. Clin. Dev. Immunol. 2012, 2012, 187585. [Google Scholar] [CrossRef]
- Kuang, L.; Deng, Y.; Liu, X.; Zou, Z.; Mi, L. Differential Expression of MRNA and MiRNA in Guinea Pigs Following Infection with HSV2v. Exp. Ther. Med. 2017, 14, 2577–2583. [Google Scholar] [CrossRef]
- Kimberlin, D.W.; Whitley, R.J.; Wan, W.; Powell, D.A.; Storch, G.; Ahmed, A.; Palmer, A.; Sánchez, P.J.; Jacobs, R.F.; Bradley, J.S.; et al. Oral Acyclovir Suppression and Neurodevelopment after Neonatal Herpes. N. Engl. J. Med. 2011, 365, 1284–1292. [Google Scholar] [CrossRef]
- Boss, I.W.; Plaisance, K.B.; Renne, R. Role of Virus-Encoded MicroRNAs in Herpesvirus Biology. Trends Microbiol. 2009, 17, 544–553. [Google Scholar] [CrossRef]
- Esteso, G.; Luzón, E.; Sarmiento, E.; Gómez-Caro, R.; Steinle, A.; Murphy, G.; Carbone, J.; Valés-Gómez, M.; Reyburn, H.T. Altered MicroRNA Expression after Infection with Human Cytomegalovirus Leads to TIMP3 Downregulation and Increased Shedding of Metalloprotease Substrates, Including MICA. J. Immunol. 2014, 193, 1344–1352. [Google Scholar] [CrossRef]
- Kim, S.; Lee, S.; Shin, J.; Kim, Y.; Evnouchidou, I.; Kim, D.; Kim, Y.-K.; Kim, Y.-E.; Ahn, J.-H.; Riddell, S.R.; et al. Human Cytomegalovirus MicroRNA MiR-US4-1 Inhibits CD8+ T Cell Responses by Targeting the Aminopeptidase ERAP1. Nat. Immunol. 2011, 12, 984–991. [Google Scholar] [CrossRef] [PubMed]
- Landais, I.; Pelton, C.; Streblow, D.; DeFilippis, V.; McWeeney, S.; Nelson, J.A. Human Cytomegalovirus MiR-UL112-3p Targets TLR2 and Modulates the TLR2/IRAK1/NFκB Signaling Pathway. PLoS Pathog. 2015, 11, e1004881. [Google Scholar] [CrossRef]
- Kim, Y.; Lee, S.; Kim, S.; Kim, D.; Ahn, J.-H.; Ahn, K. Human Cytomegalovirus Clinical Strain-Specific MicroRNA MiR-UL148D Targets the Human Chemokine RANTES during Infection. PLoS Pathog. 2012, 8, e1002577. [Google Scholar] [CrossRef] [PubMed]
- Qi, M.; Qi, Y.; Ma, Y.; He, R.; Ji, Y.; Sun, Z.; Ruan, Q. Over-Expression of Human Cytomegalovirus MiR-US25-2-3p Downregulates EIF4A1 and Inhibits HCMV Replication. FEBS Lett. 2013, 587, 2266–2271. [Google Scholar] [CrossRef] [PubMed]
- Murphy, E.; Vanícek, J.; Robins, H.; Shenk, T.; Levine, A.J. Suppression of Immediate-Early Viral Gene Expression by Herpesvirus-Coded MicroRNAs: Implications for Latency. Proc. Natl. Acad. Sci. USA 2008, 105, 5453–5458. [Google Scholar] [CrossRef]
- Stern-Ginossar, N.; Saleh, N.; Goldberg, M.D.; Prichard, M.; Wolf, D.G.; Mandelboim, O. Analysis of Human Cytomegalovirus-Encoded MicroRNA Activity during Infection. J. Virol. 2009, 83, 10684–10693. [Google Scholar] [CrossRef]
- Zhang, L.; Yu, J.; Liu, Z. MicroRNAs Expressed by Human Cytomegalovirus. Virol. J. 2020, 17, 34. [Google Scholar] [CrossRef]
- Liang, Q.; Wang, K.; Wang, B.; Cai, Q. HCMV-Encoded MiR-UL112-3p Promotes Glioblastoma Progression via Tumour Suppressor Candidate 3. Sci. Rep. 2017, 7, 44705. [Google Scholar] [CrossRef]
- Ulasov, I.V.; Kaverina, N.V.; Ghosh, D.; Baryshnikova, M.A.; Kadagidze, Z.G.; Karseladze, A.I.; Baryshnikov, A.Y.; Cobbs, C.S. CMV70-3P MiRNA Contributes to the CMV Mediated Glioma Stemness and Represents a Target for Glioma Experimental Therapy. Oncotarget 2017, 8, 25989–25999. [Google Scholar] [CrossRef]
- Fu, Y.-R.; Liu, X.-J.; Li, X.-J.; Shen, Z.; Yang, B.; Wu, C.-C.; Li, J.-F.; Miao, L.-F.; Ye, H.-Q.; Qiao, G.-H.; et al. MicroRNA MiR-21 Attenuates Human Cytomegalovirus Replication in Neural Cells by Targeting Cdc25a. J. Virol. 2015, 89, 1070–1082. [Google Scholar] [CrossRef]
- Delecluse, H.-J.; Feederle, R.; O’Sullivan, B.; Taniere, P. Epstein Barr Virus-Associated Tumours: An Update for the Attention of the Working Pathologist. J. Clin. Pathol. 2006, 60, 1358–1364. [Google Scholar] [CrossRef]
- Barth, S.; Meister, G.; Grässer, F.A. EBV-Encoded MiRNAs. Biochim. Biophys. Acta (BBA)-Gene Regul. Mech. 2011, 1809, 631–640. [Google Scholar] [CrossRef]
- Lo, A.K.F.; To, K.F.; Lo, K.W.; Lung, R.W.M.; Hui, J.W.Y.; Liao, G.; Hayward, S.D. Modulation of LMP1 Protein Expression by EBV-Encoded MicroRNAs. Proc. Natl. Acad. Sci. USA 2007, 104, 16164–16169. [Google Scholar] [CrossRef] [PubMed]
- Lung, R.W.-M.; Tong, J.H.-M.; Sung, Y.-M.; Leung, P.-S.; Ng, D.C.-H.; Chau, S.-L.; Chan, A.W.-H.; Ng, E.K.-O.; Lo, K.-W.; To, K.-F. Modulation of LMP2A Expression by a Newly Identified Epstein-Barr Virus-Encoded MicroRNA MiR-BART22. Neoplasia 2009, 11, 1174-IN17. [Google Scholar] [CrossRef] [PubMed]
- Xia, T.; O’Hara, A.; Araujo, I.; Barreto, J.; Carvalho, E.; Sapucaia, J.B.; Ramos, J.C.; Luz, E.; Pedroso, C.; Manrique, M.; et al. EBV MicroRNAs in Primary Lymphomas and Targeting of CXCL-11 by Ebv-Mir-BHRF1-3. Cancer Res. 2008, 68, 1436–1442. [Google Scholar] [CrossRef] [PubMed]
- Nachmani, D.; Stern-Ginossar, N.; Sarid, R.; Mandelboim, O. Diverse Herpesvirus MicroRNAs Target the Stress-Induced Immune Ligand MICB to Escape Recognition by Natural Killer Cells. Cell Host Microbe 2009, 5, 376–385. [Google Scholar] [CrossRef]
- Haneklaus, M.; Gerlic, M.; Kurowska-Stolarska, M.; Rainey, A.-A.; Pich, D.; McInnes, I.B.; Hammerschmidt, W.; O’Neill, L.A.J.; Masters, S.L. Cutting Edge: MiR-223 and EBV MiR-BART15 Regulate the NLRP3 Inflammasome and IL-1β Production. J. Immunol. 2012, 189, 3795–3799. [Google Scholar] [CrossRef]
- Choy, E.Y.-W.; Siu, K.-L.; Kok, K.-H.; Lung, R.W.-M.; Tsang, C.M.; To, K.-F.; Kwong, D.L.-W.; Tsao, S.W.; Jin, D.-Y. An Epstein-Barr Virus–Encoded MicroRNA Targets PUMA to Promote Host Cell Survival. J. Exp. Med. 2008, 205, 2551–2560. [Google Scholar] [CrossRef]
- Harold, C.; Cox, D.; Riley, K.J. Epstein-Barr Viral MicroRNAs Target Caspase 3. Virol. J. 2016, 13, 145. [Google Scholar] [CrossRef]
- Marquitz, A.R.; Mathur, A.; Nam, C.S.; Raab-Traub, N. The Epstein–Barr Virus BART MicroRNAs Target the pro-Apoptotic Protein Bim. Virology 2011, 412, 392–400. [Google Scholar] [CrossRef]
- Kim, H.; Choi, H.; Lee, S.K. Epstein–Barr Virus MiR-BART20-5p Regulates Cell Proliferation and Apoptosis by Targeting BAD. Cancer Lett. 2015, 356, 733–742. [Google Scholar] [CrossRef] [PubMed]
- Iizasa, H.; Wulff, B.-E.; Alla, N.R.; Maragkakis, M.; Megraw, M.; Hatzigeorgiou, A.; Iwakiri, D.; Takada, K.; Wiedmer, A.; Showe, L.; et al. Editing of Epstein-Barr Virus-Encoded BART6 MicroRNAs Controls Their Dicer Targeting and Consequently Affects Viral Latency. J. Biol. Chem. 2010, 285, 33358–33370. [Google Scholar] [CrossRef]
- Lei, T.; Yuen, K.-S.; Xu, R.; Tsao, S.W.; Chen, H.; Li, M.; Kok, K.-H.; Jin, D.-Y. Targeting of DICE1 Tumor Suppressor by Epstein-Barr Virus-Encoded MiR-BART3* MicroRNA in Nasopharyngeal Carcinoma: DICE1 Targeting by EBV MiR-BART3*. Int. J. Cancer 2013, 133, 79–87. [Google Scholar] [CrossRef] [PubMed]
- Wong, A.M.G.; Kong, K.L.; Tsang, J.W.H.; Kwong, D.L.W.; Guan, X.-Y. Profiling of Epstein-Barr Virus-Encoded MicroRNAs in Nasopharyngeal Carcinoma Reveals Potential Biomarkers and Oncomirs. Cancer 2012, 118, 698–710. [Google Scholar] [CrossRef] [PubMed]
- Marquitz, A.R.; Mathur, A.; Chugh, P.E.; Dittmer, D.P.; Raab-Traub, N. Expression Profile of MicroRNAs in Epstein-Barr Virus-Infected AGS Gastric Carcinoma Cells. J. Virol. 2014, 88, 1389–1393. [Google Scholar] [CrossRef] [PubMed]
- Motsch, N.; Alles, J.; Imig, J.; Zhu, J.; Barth, S.; Reineke, T.; Tinguely, M.; Cogliatti, S.; Dueck, A.; Meister, G.; et al. MicroRNA Profiling of Epstein-Barr Virus-Associated NK/T-Cell Lymphomas by Deep Sequencing. PLoS ONE 2012, 7, e42193. [Google Scholar] [CrossRef]
- Esquela-Kerscher, A.; Slack, F.J. Oncomirs—MicroRNAs with a Role in Cancer. Nat. Rev. Cancer 2006, 6, 259–269. [Google Scholar] [CrossRef]
- Ellis-Connell, A.L.; Iempridee, T.; Xu, I.; Mertz, J.E. Cellular MicroRNAs 200b and 429 Regulate the Epstein-Barr Virus Switch between Latency and Lytic Replication. J. Virol. 2010, 84, 10329–10343. [Google Scholar] [CrossRef]
- Mansouri, S.; Pan, Q.; Blencowe, B.J.; Claycomb, J.M.; Frappier, L. Epstein-Barr Virus EBNA1 Protein Regulates Viral Latency through Effects on Let-7 MicroRNA and Dicer. J. Virol. 2014, 88, 11166–11177. [Google Scholar] [CrossRef]
- Hassan, J.; Dean, J.; De Gascun, C.F.; Riordan, M.; Sweeney, C.; Connell, J.; Awan, A. Plasma EBV MicroRNAs in Paediatric Renal Transplant Recipients. J. Nephrol. 2018, 31, 445–451. [Google Scholar] [CrossRef]
- Kim, H.; Choi, H.; Lee, S.K. Epstein-Barr Virus MicroRNA MiR-BART20-5p Suppresses Lytic Induction by Inhibiting BAD -Mediated Caspase-3 -Dependent Apoptosis. J. Virol. 2016, 90, 1359–1368. [Google Scholar] [CrossRef] [PubMed]
- Barth, S.; Pfuhl, T.; Mamiani, A.; Ehses, C.; Roemer, K.; Kremmer, E.; Jäker, C.; Höck, J.; Meister, G.; Grässer, F.A. Epstein-Barr Virus-Encoded MicroRNA MiR-BART2 down-Regulates the Viral DNA Polymerase BALF5. Nucleic Acids Res. 2008, 36, 666–675. [Google Scholar] [CrossRef] [PubMed]
- Abend, J.R.; Ramalingam, D.; Kieffer-Kwon, P.; Uldrick, T.S.; Yarchoan, R.; Ziegelbauer, J.M. Kaposi’s Sarcoma-Associated Herpesvirus MicroRNAs Target IRAK1 and MYD88, Two Components of the Toll-Like Receptor/Interleukin-1R Signaling Cascade, To Reduce Inflammatory-Cytokine Expression. J. Virol. 2012, 86, 11663–11674. [Google Scholar] [CrossRef] [PubMed]
- Liang, D.; Gao, Y.; Lin, X.; He, Z.; Zhao, Q.; Deng, Q.; Lan, K. A Human Herpesvirus MiRNA Attenuates Interferon Signaling and Contributes to Maintenance of Viral Latency by Targeting IKKε. Cell Res. 2011, 21, 793–806. [Google Scholar] [CrossRef] [PubMed]
- Gottwein, E.; Cullen, B.R. A Human Herpesvirus MicroRNA Inhibits P21 Expression and Attenuates P21-Mediated Cell Cycle Arrest. J. Virol. 2010, 84, 5229–5237. [Google Scholar] [CrossRef]
- Abend, J.R.; Uldrick, T.; Ziegelbauer, J.M. Regulation of Tumor Necrosis Factor-Like Weak Inducer of Apoptosis Receptor Protein (TWEAKR) Expression by Kaposi’s Sarcoma-Associated Herpesvirus MicroRNA Prevents TWEAK-Induced Apoptosis and Inflammatory Cytokine Expression. J. Virol. 2010, 84, 12139–12151. [Google Scholar] [CrossRef]
- Lei, X.; Zhu, Y.; Jones, T.; Bai, Z.; Huang, Y.; Gao, S.-J. A Kaposi’s Sarcoma-Associated Herpesvirus MicroRNA and Its Variants Target the Transforming Growth Factor β Pathway To Promote Cell Survival. J. Virol. 2012, 86, 11698–11711. [Google Scholar] [CrossRef]
- Liu, Y.; Sun, R.; Lin, X.; Liang, D.; Deng, Q.; Lan, K. Kaposi’s Sarcoma-Associated Herpesvirus-Encoded MicroRNA MiR-K12-11 Attenuates Transforming Growth Factor Beta Signaling through Suppression of SMAD5. J. Virol. 2012, 86, 1372–1381. [Google Scholar] [CrossRef]
- Suffert, G.; Malterer, G.; Hausser, J.; Viiliäinen, J.; Fender, A.; Contrant, M.; Ivacevic, T.; Benes, V.; Gros, F.; Voinnet, O.; et al. Kaposi’s Sarcoma Herpesvirus MicroRNAs Target Caspase 3 and Regulate Apoptosis. PLoS Pathog. 2011, 7, e1002405. [Google Scholar] [CrossRef]
- Qin, Z.; Freitas, E.; Sullivan, R.; Mohan, S.; Bacelieri, R.; Branch, D.; Romano, M.; Kearney, P.; Oates, J.; Plaisance, K.; et al. Upregulation of XCT by KSHV-Encoded MicroRNAs Facilitates KSHV Dissemination and Persistence in an Environment of Oxidative Stress. PLoS Pathog. 2010, 6, e1000742. [Google Scholar] [CrossRef]
- Skalsky, R.L.; Samols, M.A.; Plaisance, K.B.; Boss, I.W.; Riva, A.; Lopez, M.C.; Baker, H.V.; Renne, R. Kaposi’s Sarcoma-Associated Herpesvirus Encodes an Ortholog of MiR-155. J. Virol. 2007, 81, 12836–12845. [Google Scholar] [CrossRef] [PubMed]
- Gottwein, E.; Mukherjee, N.; Sachse, C.; Frenzel, C.; Majoros, W.H.; Chi, J.-T.A.; Braich, R.; Manoharan, M.; Soutschek, J.; Ohler, U.; et al. A Viral MicroRNA Functions as an Orthologue of Cellular MiR-155. Nature 2007, 450, 1096–1099. [Google Scholar] [CrossRef] [PubMed]
- Hansen, A.; Henderson, S.; Lagos, D.; Nikitenko, L.; Coulter, E.; Roberts, S.; Gratrix, F.; Plaisance, K.; Renne, R.; Bower, M.; et al. KSHV-Encoded MiRNAs Target MAF to Induce Endothelial Cell Reprogramming. Genes Dev. 2010, 24, 195–205. [Google Scholar] [CrossRef]
- Qin, Z.; Jakymiw, A.; Findlay, V.; Parsons, C. KSHV-Encoded MicroRNAs: Lessons for Viral Cancer Pathogenesis and Emerging Concepts. Int. J. Cell Biol. 2012, 2012, 603961. [Google Scholar] [CrossRef]
- Lin, X.; Liang, D.; He, Z.; Deng, Q.; Robertson, E.S.; Lan, K. MiR-K12-7-5p Encoded by Kaposi’s Sarcoma-Associated Herpesvirus Stabilizes the Latent State by Targeting Viral ORF50/RTA. PLoS ONE 2011, 6, e16224. [Google Scholar] [CrossRef] [PubMed]
- Lu, F.; Stedman, W.; Yousef, M.; Renne, R.; Lieberman, P.M. Epigenetic Regulation of Kaposi’s Sarcoma-Associated Herpesvirus Latency by Virus-Encoded MicroRNAs That Target Rta and the Cellular Rbl2-DNMT Pathway. J. Virol. 2010, 84, 2697–2706. [Google Scholar] [CrossRef]
- Lu, C.; Li, Z.; Chu, C.; Feng, J.; Feng, J.; Sun, R.; Rana, T.M. MicroRNAs Encoded by Kaposi’s Sarcoma-associated Herpesvirus Regulate Viral Life Cycle. EMBO Rep. 2010, 11, 784–790. [Google Scholar] [CrossRef]
- Ziegelbauer, J.M.; Sullivan, C.S.; Ganem, D. Tandem Array–Based Expression Screens Identify Host MRNA Targets of Virus-Encoded MicroRNAs. Nat. Genet. 2009, 41, 130–134. [Google Scholar] [CrossRef]
- Tsai, Y.-H.; Wu, M.-F.; Wu, Y.-H.; Chang, S.-J.; Lin, S.-F.; Sharp, T.V.; Wang, H.-W. The M Type K15 Protein of Kaposi’s Sarcoma-Associated Herpesvirus Regulates MicroRNA Expression via Its SH2-Binding Motif To Induce Cell Migration and Invasion. J. Virol. 2009, 83, 622–632. [Google Scholar] [CrossRef]
- Qin, Z.; Peruzzi, F.; Reiss, K.; Dai, L. Role of Host MicroRNAs in Kaposi’s Sarcoma-Associated Herpesvirus Pathogenesis. Viruses 2014, 6, 4571–4580. [Google Scholar] [CrossRef]
- Lei, X.; Bai, Z.; Ye, F.; Xie, J.; Kim, C.-G.; Huang, Y.; Gao, S.-J. Regulation of NF-ΚB Inhibitor IκBα and Viral Replication by a KSHV MicroRNA. Nat. Cell Biol. 2010, 12, 193–199. [Google Scholar] [CrossRef] [PubMed]
- Lawrie, C.H.; Gal, S.; Dunlop, H.M.; Pushkaran, B.; Liggins, A.P.; Pulford, K.; Banham, A.H.; Pezzella, F.; Boultwood, J.; Wainscoat, J.S.; et al. Detection of Elevated Levels of Tumour-Associated MicroRNAs in Serum of Patients with Diffuse Large B-Cell Lymphoma. Br. J. Haematol. 2008, 141, 672–675. [Google Scholar] [CrossRef] [PubMed]
- Lugli, G.; Cohen, A.M.; Bennett, D.A.; Shah, R.C.; Fields, C.J.; Hernandez, A.G.; Smalheiser, N.R. Plasma Exosomal MiRNAs in Persons with and without Alzheimer Disease: Altered Expression and Prospects for Biomarkers. PLoS ONE 2015, 10, e0139233. [Google Scholar] [CrossRef]
- Farr, R.J.; Joglekar, M.V.; Taylor, C.J.; Hardikar, A.A. Circulating Non-Coding RNAs as Biomarkers of Beta Cell Death in Diabetes. Pediatr. Endocrinol. Rev. 2013, 11, 14–20. [Google Scholar]
- Taylor, C.R. Introduction to Predictive Biomarkers: Definitions and Characteristics. In Predictive Biomarkers in Oncology; Badve, S., Kumar, G.L., Eds.; Springer International Publishing: Cham, Switzerland, 2019; pp. 3–18. ISBN 978-3-319-95227-7. [Google Scholar]
- Hanke, M.; Hoefig, K.; Merz, H.; Feller, A.C.; Kausch, I.; Jocham, D.; Warnecke, J.M.; Sczakiel, G. A Robust Methodology to Study Urine MicroRNA as Tumor Marker: MicroRNA-126 and MicroRNA-182 Are Related to Urinary Bladder Cancer. Urol. Oncol. 2010, 28, 655–661. [Google Scholar] [CrossRef]
- Park, N.J.; Zhou, H.; Elashoff, D.; Henson, B.S.; Kastratovic, D.A.; Abemayor, E.; Wong, D.T. Salivary MicroRNA: Discovery, Characterization, and Clinical Utility for Oral Cancer Detection. Clin. Cancer Res. 2009, 15, 5473–5477. [Google Scholar] [CrossRef] [PubMed]
- Meckes, D.G.; Shair, K.H.Y.; Marquitz, A.R.; Kung, C.-P.; Edwards, R.H.; Raab-Traub, N. Human Tumor Virus Utilizes Exosomes for Intercellular Communication. Proc. Natl. Acad. Sci. USA 2010, 107, 20370–20375. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Ba, Y.; Ma, L.; Cai, X.; Yin, Y.; Wang, K.; Guo, J.; Zhang, Y.; Chen, J.; Guo, X.; et al. Characterization of MicroRNAs in Serum: A Novel Class of Biomarkers for Diagnosis of Cancer and Other Diseases. Cell Res. 2008, 18, 997–1006. [Google Scholar] [CrossRef] [PubMed]
- Kotton, C.N. CMV: Prevention, Diagnosis and Therapy: CMV: Prevention, Diagnosis and Therapy. Am. J. Transplant. 2013, 13, 24–40. [Google Scholar] [CrossRef]
- Kawano, Y.; Iwata, S.; Kawada, J.; Gotoh, K.; Suzuki, M.; Torii, Y.; Kojima, S.; Kimura, H.; Ito, Y. Plasma Viral MicroRNA Profiles Reveal Potential Biomarkers for Chronic Active Epstein-Barr Virus Infection. J. Infect. Dis. 2013, 208, 771–779. [Google Scholar] [CrossRef]
- Ørum, H. Locked Nucleic Acids as MicroRNA Therapeutics. In MicroRNAs in Medicine; Lawrie, C.H., Ed.; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2013; pp. 663–672. ISBN 978-1-118-30031-2. [Google Scholar]
- Crooke, S.T.; Baker, B.F.; Crooke, R.M.; Liang, X.-H. Antisense Technology: An Overview and Prospectus. Nat. Rev. Drug Discov. 2021, 20, 427–453. [Google Scholar] [CrossRef]
- Lanford, R.E.; Hildebrandt-Eriksen, E.S.; Petri, A.; Persson, R.; Lindow, M.; Munk, M.E.; Kauppinen, S.; Ørum, H. Therapeutic Silencing of MicroRNA-122 in Primates with Chronic Hepatitis C Virus Infection. Science 2010, 327, 198–201. [Google Scholar] [CrossRef]
- Peng, S.; Wang, J.; Wei, S.; Li, C.; Zhou, K.; Hu, J.; Ye, X.; Yan, J.; Liu, W.; Gao, G.F.; et al. Endogenous Cellular MicroRNAs Mediate Antiviral Defense against Influenza A Virus. Mol. Ther.-Nucleic Acids 2018, 10, 361–375. [Google Scholar] [CrossRef]
- Xie, Y.; Murray-Stewart, T.; Wang, Y.; Yu, F.; Li, J.; Marton, L.J.; Casero, R.A.; Oupický, D. Self-Immolative Nanoparticles for Simultaneous Delivery of MicroRNA and Targeting of Polyamine Metabolism in Combination Cancer Therapy. J. Control. Release 2017, 246, 110–119. [Google Scholar] [CrossRef]
- Santos-Carballal, B.; Aaldering, L.J.; Ritzefeld, M.; Pereira, S.; Sewald, N.; Moerschbacher, B.M.; Götte, M.; Goycoolea, F.M. Physicochemical and Biological Characterization of Chitosan-MicroRNA Nanocomplexes for Gene Delivery to MCF-7 Breast Cancer Cells. Sci. Rep. 2015, 5, 13567. [Google Scholar] [CrossRef]
- Xu, F.; Liao, J.-Z.; Xiang, G.-Y.; Zhao, P.-X.; Ye, F.; Zhao, Q.; He, X.-X. MiR-101 and Doxorubicin Codelivered by Liposomes Suppressing Malignant Properties of Hepatocellular Carcinoma. Cancer Med. 2017, 6, 651–661. [Google Scholar] [CrossRef]
- Baek, D.; Villén, J.; Shin, C.; Camargo, F.D.; Gygi, S.P.; Bartel, D.P. The Impact of MicroRNAs on Protein Output. Nature 2008, 455, 64–71. [Google Scholar] [CrossRef]
- Doench, J.G.; Sharp, P.A. Specificity of MicroRNA Target Selection in Translational Repression. Genes Dev. 2004, 18, 504–511. [Google Scholar] [CrossRef]
- Zhu, G.; Mei, L.; Vishwasrao, H.D.; Jacobson, O.; Wang, Z.; Liu, Y.; Yung, B.C.; Fu, X.; Jin, A.; Niu, G.; et al. Intertwining DNA-RNA Nanocapsules Loaded with Tumor Neoantigens as Synergistic Nanovaccines for Cancer Immunotherapy. Nat. Commun. 2017, 8, 1482. [Google Scholar] [CrossRef]
- Lee, S.W.L.; Paoletti, C.; Campisi, M.; Osaki, T.; Adriani, G.; Kamm, R.D.; Mattu, C.; Chiono, V. MicroRNA Delivery through Nanoparticles. J. Control. Release 2019, 313, 80–95. [Google Scholar] [CrossRef]
| Virus Family | Virus Species | Number of Known Pre-miRNAs | Number of miRNAs | Citations |
|---|---|---|---|---|
| α herpesviruses | Herpes simplex virus 1 | 16 | 27 | [5,10,11] |
| Herpes simplex virus 2 | 18 | 24 | [5,12] | |
| β herpesviruses | Human cytomegalovirus | 14 | 21 | [13] |
| γ herpesviruses | Epstein–Barr virus | 25 | 44 | [14] |
| Kaposi’s sarcoma-associated herpesvirus | 13 | 25 | [15,16] |
| Herpesvirus | miRNA | Target | Function | References |
|---|---|---|---|---|
| Viral targets | ||||
| HSV-1 | miR-H2-3p | ICP0 | Immune evasion | [11,46,47] |
| miR-H3, miR-H4 | ICP34.5 | Immune evasion | [9] | |
| miR-H6 | ICP4 | Immune evasion | [9] | |
| miR-H8 | GPI | Inhibits viral growth | [44] | |
| HSV-2 | miR-I | ICP34.5 | Immune evasion | [16,48,49] |
| miR-H2 | ICP34.5 | Immune evasion | [48,49] | |
| miR-H3/4 | ICP0 | Immune evasion | [46,48,49] | |
| Cellular targets | ||||
| HSV-1 | miR-H-27 | KLHL24 | Immune evasion, viral replication and proliferation | [45] |
| HCMV | miRNA | Target | Function | Reference |
|---|---|---|---|---|
| Cellular targets | miR-UL112 | MICB | Immune evasion | [32] |
| miR-US25-2-3p | TIMP3 | Immune evasion | [70] | |
| miR-UL112-3p | TLR2 | Immune evasion | [72] | |
| miRNA UL148D | CCL5 | Immune evasion | [73] | |
| miR-US4-1 | ERAP1 | Immune evasion | [71] | |
| miR-US25-1 | CD147, CCNE2, EID1, BRCC3, MAPRE2, H3F3B, ATP6V0CP1 | Interrupts cell cycle | [11] | |
| miR-US25-2-3p | eIF4A1 | Immune evasion | [74] | |
| Viral targets | miR-UL112-1 | IE72, UL114 | Favors latency | [75] |
| Herpesvirus | miRNA | Target | Function | Reference |
|---|---|---|---|---|
| Cellular targets | miR-BHRF1-3 | CXCL11 | Immune evasion | [85] |
| miR-BART1 miR-BART3 | BIM | Inhibits apoptosis | [90] | |
| miR-BART1-3p | CASPASE 3 | Inhibits apoptosis | [89] | |
| miR-BART2-5p | MICB | Immune evasion | [100] | |
| miR-BART3-5p | DICE1 | Cell transformation and proliferation | [93] | |
| miR-BART5-5p | PUMA | Immune evasion | [88] | |
| miR-BART6-5p | DICER | Cell transformation and proliferation | [92] | |
| miR-BART9 miR-BART11 miR-BART12 | BIM | Inhibits apoptosis | [90] | |
| miR-BART15 | NLRP3 | Immune evasion | [87] | |
| miR-BART16 | TOMM2 CASPASE 3 | Immune evasion Inhibits apoptosis | [89,90,101] | |
| miR-BART19-3p | WIF1 | Cell transformation and proliferation | [94] | |
| miR-BART20-5p | BAD | Inhibits apoptosis | [101] | |
| Viral targets | miR-BART16, miR-BART17-5p miR-BART1-5p | LMP1 | Immune evasion | [83] |
| miR-BART22 | LMP2A | Immune evasion | [84] | |
| miR-BART2 | BALF5 | Regulates viral replication | [102] |
| Herpesvirus | miRNA | Target | Function | References |
|---|---|---|---|---|
| Cellular targets | miR-K12-1 | MICB P21 IκBα CASPASE 3 xCT | Immune evasion Oncogenesis Cell survival Modulates latent/lytic infection Facilitates viral entry | [105,107,109,110,111,121] |
| miR-K12-3 | CASPASE 3 NFIB | Cell survival Modulates latent/lytic infection | [109,117] | |
| miR-K12-4-3p | CASPASE 3 RBL | Cell survival Modulates latent/lytic infection | [109,116] | |
| miR-K12-5 | MYD88 BCLAF1 | Immune evasion Modulates latent/lytic infection | [103,118] | |
| miR-K12-6 | xCT | Facilitates viral entry | [110,113] | |
| miR-K12-9 | IRAK1 BCLAF1 xCT | Immune evasion Modulates latent/lytic infection Facilitates viral entry | [103,109,118] | |
| miR-K12-10 | TWEAKR TGFBR2 | Immune evasion Cell survival Cell survival Oncogenesis | [106,107] | |
| miR-K12-11 | xCT IKKε SMAD5 | Facilitates viral entry Modulates latent/lytic infection Immune evasion Cell survival Oncogenesis | [104,108,110,113] | |
| Viral targets | miR-K12-7 miR-K12-9 | KSHV ORF50 | Modulates latent/lytic infection | [115] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dass, D.; Dhotre, K.; Chakraborty, M.; Nath, A.; Banerjee, A.; Bagchi, P.; Mukherjee, A. miRNAs in Herpesvirus Infection: Powerful Regulators in Small Packages. Viruses 2023, 15, 429. https://doi.org/10.3390/v15020429
Dass D, Dhotre K, Chakraborty M, Nath A, Banerjee A, Bagchi P, Mukherjee A. miRNAs in Herpesvirus Infection: Powerful Regulators in Small Packages. Viruses. 2023; 15(2):429. https://doi.org/10.3390/v15020429
Chicago/Turabian StyleDass, Debashree, Kishore Dhotre, Muskan Chakraborty, Anushka Nath, Anwesha Banerjee, Parikshit Bagchi, and Anupam Mukherjee. 2023. "miRNAs in Herpesvirus Infection: Powerful Regulators in Small Packages" Viruses 15, no. 2: 429. https://doi.org/10.3390/v15020429
APA StyleDass, D., Dhotre, K., Chakraborty, M., Nath, A., Banerjee, A., Bagchi, P., & Mukherjee, A. (2023). miRNAs in Herpesvirus Infection: Powerful Regulators in Small Packages. Viruses, 15(2), 429. https://doi.org/10.3390/v15020429






