A Cross-Sectional Comparative Characterization of Hematological Changes in Patients with COVID-19 Infection, Non-COVID Influenza-like Illnesses and Healthy Controls
Abstract
1. Introduction
2. Material and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hosseini, A.; Hashemi, V.; Shomali, N.; Asghari, F.; Gharibi, T.; Akbari, M.; Gholizadeh, S.; Jafari, A. Innate and adaptive immune responses against coronavirus. Biomed. Pharmacother. 2020, 132, 110859. [Google Scholar] [CrossRef] [PubMed]
- Lamers, M.M.; Haagmans, B.L. SARS-CoV-2 pathogenesis. Nat. Rev. Microbiol. 2022, 20, 270–284. [Google Scholar] [CrossRef] [PubMed]
- Liew, P.X.; Kubes, P. The Neutrophil’s Role During Health and Disease. Physiol. Rev. 2019, 99, 1223–1248. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Liu, S.; Goraya, M.U.; Maarouf, M.; Huang, S.; Chen, J.L. Host Immune Response to Influenza A Virus Infection. Front. Immunol. 2018, 9, 320. [Google Scholar] [CrossRef] [PubMed]
- Yang, A.P.; Liu, J.P.; Tao, W.Q.; Li, H.M. The diagnostic and predictive role of NLR, d-NLR and PLR in COVID-19 patients. Int. Immunopharmacol. 2020, 84, 106504. [Google Scholar] [CrossRef] [PubMed]
- Cui, S.N.; Tan, H.Y.; Fan, G.C. Immunopathological Roles of Neutrophils in Virus Infection and COVID-19. Shock 2021, 56, 345–351. [Google Scholar] [CrossRef]
- Payen, D.; Cravat, M.; Maadadi, H.; Didelot, C.; Prosic, L.; Dupuis, C.; Losser, M.-R.; Bittencourt, M.D.C. A Longitudinal Study of Immune Cells in Severe COVID-19 Patients. Front. Immunol. 2020, 11, 580250. [Google Scholar] [CrossRef]
- Knoll, R.; Schultze, J.L.; Schulte-Schrepping, J. Monocytes and Macrophages in COVID-19. Front. Immunol. 2021, 12, 720109. [Google Scholar] [CrossRef]
- Chen, G.; Wu, D.; Guo, W.; Cao, Y.; Huang, D.; Wang, H.; Wang, T.; Zhang, X.; Chen, H.; Yu, H.; et al. Clinical and immunological features of severe and moderate coronavirus disease 2019. J. Clin. Invest. 2020, 130, 2620–2629. [Google Scholar] [CrossRef]
- Tan, L.; Wang, Q.; Zhang, D.; Ding, J.; Huang, Q.; Tang, Y.-Q.; Wang, Q.; Miao, H. Lymphopenia predicts disease severity of COVID-19: A descriptive and predictive study. Signal Transduct. Target. Ther. 2020, 5, 33. [Google Scholar] [CrossRef]
- Delshad, M.; Tavakolinia, N.; Pourbagheri-Sigaroodi, A.; Safaroghli-Azar, A.; Bagheri, N.; Bashash, D. The contributory role of lymphocyte subsets, pathophysiology of lymphopenia and its implication as prognostic and therapeutic opportunity in COVID-19. Int. Immunopharmacol. 2021, 95, 107586. [Google Scholar] [CrossRef] [PubMed]
- Jayaram, A.; Mathews, N.S.; Nair, S.C.; Geevar, T.; Rose, W.; Verghese, V.P.; Mathuram, A.J.; Gunasekaran, K.; Abraham, A.M.; Mammen, J.J. High fluorescent lymphocyte cell count and scattergram patterns on the Sysmex XN series cell counters-Novel parameters in early and reliable diagnosis of dengue on a background of acute febrile illness. Int. J. Lab. Hematol. 2021, 43, O156–O160. [Google Scholar] [CrossRef] [PubMed]
- Jung, Y.-J.; Kim, J.-H.; Park, Y.-J.; Kahng, J.; Lee, H.; Lee, K.-Y.; Kim, M.Y.; Han, K.; Lee, W. Evaluation of cell population data on the UniCel DxH 800 Coulter Cellular Analysis system as a screening for viral infection in children. Int. J. Lab. Hematol. 2012, 34, 283–289. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Director-General’s Remarks at the Media Briefing on 2019-nCoV on 11 February 2020. Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-remarks-at-the-media-briefing-on-2019-ncov-on-11-february-2020 (accessed on 21 July 2022).
- Brihn, A.; Chang, J.; OYong, K.; Balter, S.; Terashita, D.; Rubin, Z.; Yeganeh, N. Diagnostic Performance of an Antigen Test with RT-PCR for the Detection of SARS-CoV-2 in a Hospital Setting—Los Angeles County, California, June–August 2020. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 702–706. [Google Scholar] [CrossRef]
- Di Mitri, C.; Arcoleo, G.; Mazzuca, E.; Camarda, G.; Farinella, E.M.; Soresi, M.; Carroccio, A.; IMUSG. COVID-19 and non-COVID-19 pneumonia: A comparison. Ann. Med. 2021, 53, 2321–2331. [Google Scholar] [CrossRef]
- Richardson, S.; Hirsch, J.S.; Narasimhan, M.; Crawford, J.M.; McGinn, T.; Davidson, K.W.; The Northwell COVID-19 Research Consortium. Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area. JAMA 2020, 323, 2052–2059. [Google Scholar] [CrossRef]
- Selim, S. Leukocyte count in COVID-19: An important consideration. Egypt J. Bronchol. 2020, 14, 43. [Google Scholar] [CrossRef]
- Urrechaga, E.; Ponga, C.; Fernández, M.; España, P.P.; Haider, R.Z.; Aguirre, U. Diagnostic potential of leukocyte differential and cell population data in prediction of COVID-19 among related viral and bacterial infections at Emergency Department. Clin. Chem. Lab. Med. 2022, 60, e104–e107. [Google Scholar] [CrossRef]
- Van Elden, L.J.; van Essen, G.A.; Boucher, C.A.; van Loon, A.M.; Nijhuis, M.; Schipper, P.; Verheij, T.J.; Hoepelman, I.M. Clinical diagnosis of influenza virus infection: Evaluation of diagnostic tools in general practice. Br. J. Gen. Pract. 2001, 51, 630–634. [Google Scholar]
- Sahu, K.K.; Mishra, A.K.; Raturi, M.; Lal, A. Current Perspectives of convalescent plasma therapy in COVID-19. Acta Biomed. 2020, 91, e2020175. [Google Scholar]
- Marionneaux, S. Nonmalignant leukocyte disorders. Rodaks Hematol. 2020, 445–465. [Google Scholar] [CrossRef]
- Tanni, F.; Akker, E.; Zaman, M.M.; Figueroa, N.; Tharian, B.; Hupart, K.H. Eosinopenia and COVID-19. J. Am. Osteopath. Assoc. 2020; accepted. [Google Scholar] [CrossRef] [PubMed]
- Arora, P.; Gupta, P.K.; Lingaiah, R.; Mukhopadhyay, A.K. Volume, conductivity, and scatter parameters of leukocytes as early markers of sepsis and treatment response. J. Lab. Physicians 2019, 11, 29–33. [Google Scholar] [CrossRef] [PubMed]
- Manley, H.R.; Keightley, M.C.; Lieschke, G.J. The Neutrophil Nucleus: An Important Influence on Neutrophil Migration and Function. Front. Immunol. 2018, 9, 2867. [Google Scholar] [CrossRef] [PubMed]
- Guo, Z.; Zhang, Z.; Prajapati, M.; Li, Y. Lymphopenia Caused by Virus Infections and the Mechanisms Beyond. Viruses 2021, 13, 1876. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Liao, D.; Jiang, J.; Sun, T.; Deng, S. The VCS Parameters of Lymphocytes may Improve Discrimination between Bacterial Infection and Viral Infection. Clin. Lab. 2021, 67, 11. [Google Scholar] [CrossRef] [PubMed]
- Seyit, M.; Avci, E.; Nar, R.; Senol, H.; Yilmaz, A.; Ozen, M.; Oskay, A.; Aybek, H. Neutrophil to lymphocyte ratio, lymphocyte to monocyte ratio and platelet to lymphocyte ratio to predict the severity of COVID-19. Am. J. Emerg. Med. 2021, 40, 110–114. [Google Scholar] [CrossRef]
- Liu, J.; Liu, Y.; Xiang, P.; Pu, L.; Xiong, H.; Li, C.; Zhang, M.; Tan, J.; Xu, Y.; Song, R.; et al. Neutrophil-to-lymphocyte ratio predicts critical illness patients with 2019 coronavirus disease in the early stage. J. Transl. Med. 2020, 18, 206. [Google Scholar] [CrossRef]
- Carbonell-Sahuquillo, S.; LAzaro-Carreno, M.I.; Camacho, J.; Barres-Fernandez, A.; Albert, E.; Torres, I.; Bretón-Martínez, J.R.; Martínez-Costa, C.; Navarro, D. Evaluation of a Rapid Antigen Detection test (Panbio COVID-19 Ag Rapid test device) as a point-of-care diagnostic tool for COVID-19 in a pediatric emergency department. J. Med. Virol. 2021, 93, 6803–6807. [Google Scholar] [CrossRef]
- Villarreal, A.; Rangel, G.; Zhang, X.; Wong, D.; Britton, G.; Fernandez, P.L.; Perez, A.; Oviedo, D.; Restrepo, C.; Carreirra, M.B.; et al. Performance of a Point of Care Test for Detecting IgM and IgG Antibodies Against SARS-CoV-2 and Seroprevalence in Blood Donors and Health Care Workers in Panama. Front. Med. 2021, 8, 616106. [Google Scholar] [CrossRef]
- Ozaras, R.; Cirpin, R.; Duran, A.; Duman, H.; Arslan, O.; Bakcan, Y.; Kaya, M.; Mutlu, H.; Isayeva, L.; Kebanli, F.; et al. Influenza and COVID-19 coinfection: Report of six cases and review of the literature. J. Med. Virol. 2020, 92, 2657–2665. [Google Scholar] [CrossRef] [PubMed]

| Parameters | COVID-19 (N = 169) | Control (N = 140) | Non-COVID-19 Influenza-like Illnesses (N = 113) | Pa | Pb |
|---|---|---|---|---|---|
| Age, Y | 55 ± 14.6 | 38.14 ± 8.7 | 50.19 ± 16.5 | 0 | 0.009 |
| Male, n (%) | 134(70.9) | 92(65.7) | 79(69.9) | 0.31 | 0.85 |
| WBC (×109) | 9.9 ± 6.1 | 6.8 ± 1.4 | 9.06 ± 4.5 | 0 | 0.197 |
| RBC (×1012/L) | 4.1 ± 0.8 | 4.5 ± 0.5 | 4.1 ± 0.767 | 0 | 0.67 |
| HB (g/L) | 12.01 ± 2.2 | 13.8 ± 1.6 | 12.1 ± 2.21 | 0 | 0.85 |
| PLT (×109/L) | 207.2 ± 121.5 | 195 ± 75.7 | 233.5 ± 136 | 0.32 | 0.084 |
| NE % | 75.8 ± 15.2 | 56.7 ± 8.05 | 71.5 ± 11.3 | 0 | 0.014 |
| LY % | 13.1(7.1–21.2) | 30.9(26.7–36.7) | 17.7(12.1–23.7) | 0 | 0.001 |
| MO % | 6.7(4.5–8.8) | 7.3(6.4–8.8) | 7.9(5.3–10.2) | 0.005 | 0.001 |
| EO % | 0.19(0.0–0.8) | 2.6(1.6–4.2) | 0.37(0.09–1.5) | 0 | 0.01 |
| BA % | 0.3(0.2–0.5) | 0.6(0.4–0.8) | 0.35(0.29–0.52) | 0 | 0.02 |
| NE # (×109/L) | 6.4(4.7–10.5) | 3.7(3.1–4.5) | 6.09(3.67–8.1) | 0 | 0.06 |
| LY # (×109/L) | 1.08(0.7–1.57) | 2.0(1.7–2.4) | 1.2(0.93–1.8) | 0 | 0.011 |
| MO # (×109/L) | 0.5(0.4–0.74) | 0.5(0.4–0.6) | 0.6(0.4–0.86) | 0.109 | 0.012 |
| EO # (×109/L) | 0.007(0.0–0.1) | 0.2(0.1–0.3) | 0.15(0.0–0.13) | 0 | 0.123 |
| BA # (×109/L) | 0.015(0.0–0.04) | 0.0(0.0–0.1) | 0.02(0.0–0.04) | 0.003 | 0.305 |
| MN-V-NE | 152(146–158) | 149(146–153.7) | 148(143.5–156) | 0.002 | 0.009 |
| MN-C-NE | 145(141–147) | 145(143–149) | 145(143–146) | 0.004 | 0.667 |
| MN-MALS-NE | 141(136–145) | 141(137–144) | 138(131–144) | 0.965 | 0.017 |
| MN-UMALS-NE | 142(136–145) | 141(139–144) | 141(134–145) | 0.449 | 0.024 |
| MN-LMALS-NE | 136(129–141) | 136(131–140) | 133(124–140) | 0.688 | 0.023 |
| MN-LALS-NE | 196(146–208) | 157(144–204.7) | 176(141–205) | 0.062 | 0.015 |
| MN-AL2-NE | 138(133.5–143) | 136(134–140) | 137(133–140) | 0.006 | 0.042 |
| MN-V-LY | 90(86–94) | 89(87–90.7) | 89(85–92) | 0.051 | 0.434 |
| MN-C-LY | 118(114–120) | 113(111–118) | 118(115–121) | 0 | 0.73 |
| MN-MALS-LY | 75(67.5–79) | 70(67–75) | 76(72.5–78) | 0 | 0.344 |
| MN-UMALS-LY | 80(69–86) | 73(69–79) | 80(77–85) | 0 | 0.176 |
| MN-LMALS-LY | 65(60–70) | 61(58–66) | 66(61–68) | 0 | 0.942 |
| MN-LALS-LY | 40(34–43.5) | 36(35–43) | 37(33.5–42) | 0.577 | 0.036 |
| MN-AL2-LY | 65(61–69) | 65(63–70) | 64(62–68) | 0.126 | 0.13 |
| MN-V-MO | 182(175–188) | 170(167–175) | 179(172–185) | 0 | 0.047 |
| MN-C-MO | 124(121–127) | 123(121–127) | 124(122–126) | 0.284 | 0.517 |
| MN-MALS-MO | 94(88–97) | 90(87–94) | 93(87–960 | 0 | 0.411 |
| MN-UMALS-MO | 105(98–109) | 100(96–103) | 104(98.5–107) | 0 | 0.579 |
| MN-LMALS-MO | 79(72–84) | 78(74–80.7) | 78(72–82) | 0.05 | 0.209 |
| MN-LALS-MO | 92(73–115) | 95(90–123.5) | 85(72.5–102.5) | 0 | 0.77 |
| MN-AL2-MO | 122(115–127) | 119(115.2–125.7) | 118(113–125) | 0.122 | 0.009 |
| NLR | 6.00(3.27–12.30) | 1.87(1.39–2.26) | 4.02(2.82–6.48) | 0 | 0.001 |
| PLR | 14.17(7.84–30.71) | 6.19(4.07–7.99) | 12.55(7.17–26.47) | 0 | 0.173 |
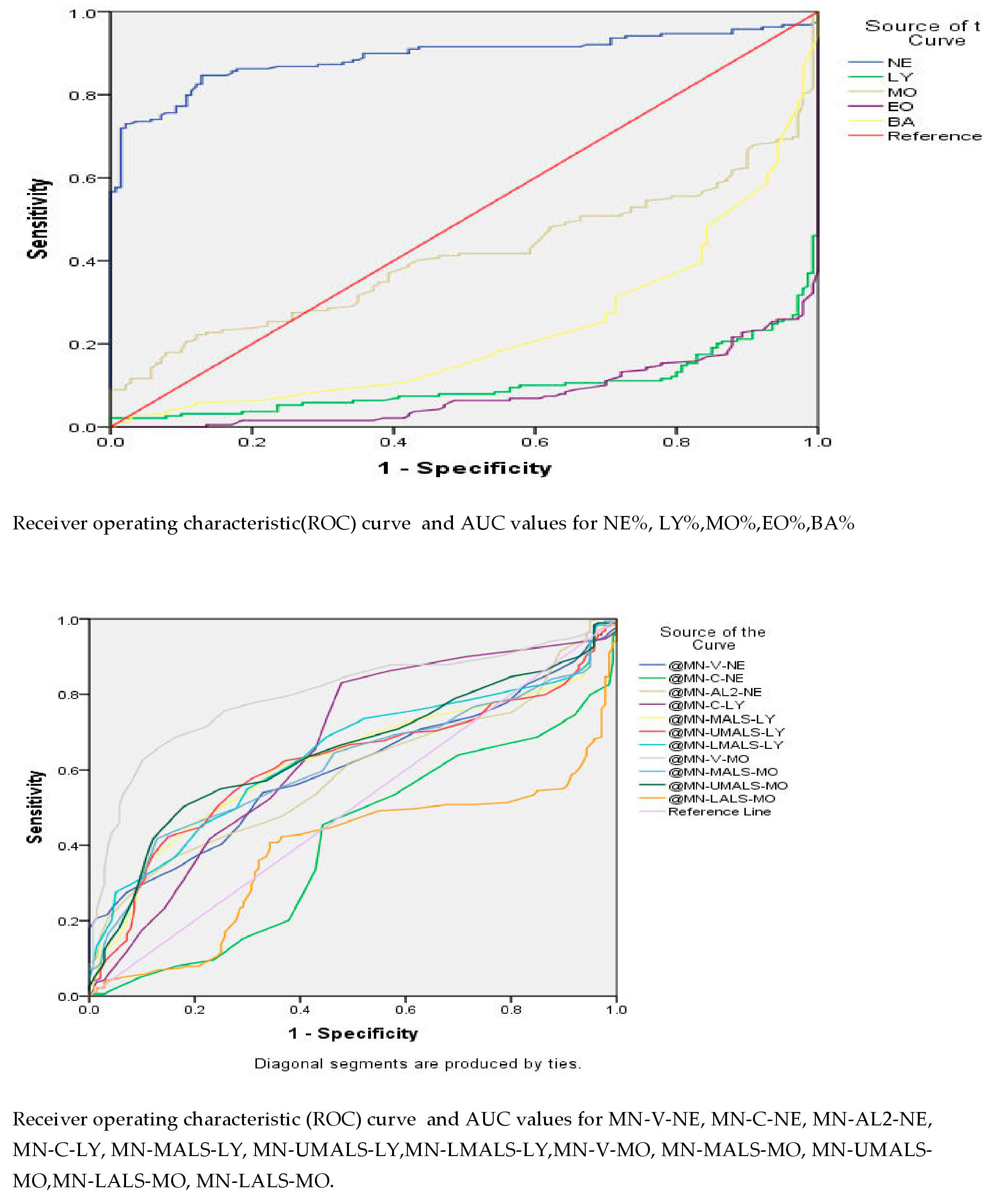
| Test Result Variable(s) | Area Under Curve | Sensitivity | Specificity | Cutoff | CI | p Value | |
|---|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||||
| NE # | 0.816 | 76% | 70% | 4.35 | 0.769 | 0.863 | 0 |
| MO # | 0.553 | 62% | 42% | 0.44 | 0.491 | 0.615 | 0.109 |
| BA # | 0.587 | 48% | 67% | 0.016 | 0.522 | 0.652 | 0.003 |
| NE % | 0.890 | 86% | 82% | 63.34 | 0.853 | 0.928 | 0 |
| MN-V-NE | 0.600 | 59% | 55% | 149.5 | 0.539 | 0.660 | 0.002 |
| MN-AL2-NE | 0.589 | 53% | 57% | 137.5 | 0.529 | 0.651 | 0.006 |
| MN-C-LY | 0.659 | 59% | 61% | 46.5 | 0598 | 0.720 | 0 |
| MN-MALS-LY | 0.625 | 62% | 60% | 71.5 | 0.565 | 0.686 | 0 |
| MN-UMALS-LY | 0.618 | 62% | 63% | 75.5 | 0.557 | 0.679 | 0 |
| MN-LMALS-LY | 0.641 | 59% | 64% | 63.5 | 0.582 | 0.701 | 0 |
| MN-V-MO | 0.798 | 75% | 74% | 174.5 | 0.749 | 0.846 | 0 |
| MN-MALS-MO | 0.614 | 64% | 53% | 90.5 | 0.554 | 0.675 | 0 |
| MN-UMALS-MO | 0.648 | 63% | 58% | 101.5 | 0.589 | 0.708 | 0 |
| Test Result Variable(s) | Area Under Curve | Sensitivity | Specificity | Cutoff | CI | p Value | |
|---|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||||
| NE % | 0.630 | 72% | 54% | 72.1 | 0.566 | 0694 | 0.014 |
| NE # | 0.565 | 67% | 44% | 5.14 | 0.497 | 0.631 | 0.060 |
| MN-V-NE | 0.589 | 64% | 54% | 148.5 | 0.657 | 0.522 | 0.009 |
| MN-MALS-NE | 0.582 | 64% | 54% | 138.5 | 0.515 | 0.649 | 0.017 |
| MN-UMALS-NE | 0.578 | 52% | 57% | 141.5 | 0.511 | 0644 | 0.024 |
| MN-LMALS-NE | 0.578 | 59% | 57% | 134.5 | 0.512 | 0.645 | 0.023 |
| MN-LALS-NE | 0.584 | 62% | 56% | 184.5 | 0.519 | 0.649 | 0.015 |
| MN-AL2-NE | 0.570 | 53% | 53% | 137.5 | 0.505 | 0.635 | 0.042 |
| MN-LALS-LY | 0.572 | 59% | 54% | 37.5 | 0.507 | 0.636 | 0.036 |
| MN-V-MO | 0.568 | 53% | 54% | 180.5 | 0.502 | 0.635 | 0.047 |
| MN-AL2-MO | 0.590 | 60% | 54% | 119.5 | 0.524 | 0.655 | 0.009 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kala, M.; Ahmad, S.; Dhebane, M.; Das, K.; Raturi, M.; Tyagi, M.; Kusum, A. A Cross-Sectional Comparative Characterization of Hematological Changes in Patients with COVID-19 Infection, Non-COVID Influenza-like Illnesses and Healthy Controls. Viruses 2023, 15, 134. https://doi.org/10.3390/v15010134
Kala M, Ahmad S, Dhebane M, Das K, Raturi M, Tyagi M, Kusum A. A Cross-Sectional Comparative Characterization of Hematological Changes in Patients with COVID-19 Infection, Non-COVID Influenza-like Illnesses and Healthy Controls. Viruses. 2023; 15(1):134. https://doi.org/10.3390/v15010134
Chicago/Turabian StyleKala, Mansi, Sohaib Ahmad, Meghali Dhebane, Kunal Das, Manish Raturi, Meghna Tyagi, and Anuradha Kusum. 2023. "A Cross-Sectional Comparative Characterization of Hematological Changes in Patients with COVID-19 Infection, Non-COVID Influenza-like Illnesses and Healthy Controls" Viruses 15, no. 1: 134. https://doi.org/10.3390/v15010134
APA StyleKala, M., Ahmad, S., Dhebane, M., Das, K., Raturi, M., Tyagi, M., & Kusum, A. (2023). A Cross-Sectional Comparative Characterization of Hematological Changes in Patients with COVID-19 Infection, Non-COVID Influenza-like Illnesses and Healthy Controls. Viruses, 15(1), 134. https://doi.org/10.3390/v15010134








