Biomarkers Predictive for In-Hospital Mortality in Patients with Diabetes Mellitus and Prediabetes Hospitalized for COVID-19 in Austria: An Analysis of COVID-19 in Diabetes Registry
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Population and Inclusion Criteria
2.3. Data Collection
2.4. Study Variables
2.4.1. Outcome
2.4.2. Predictors
2.5. Ethical Considerations
2.6. Statistical Analysis
3. Results
3.1. Characteristics of Study Participants, Overall and by In-Hospital Mortality
3.2. Biomarker of COVID-19 Mortality
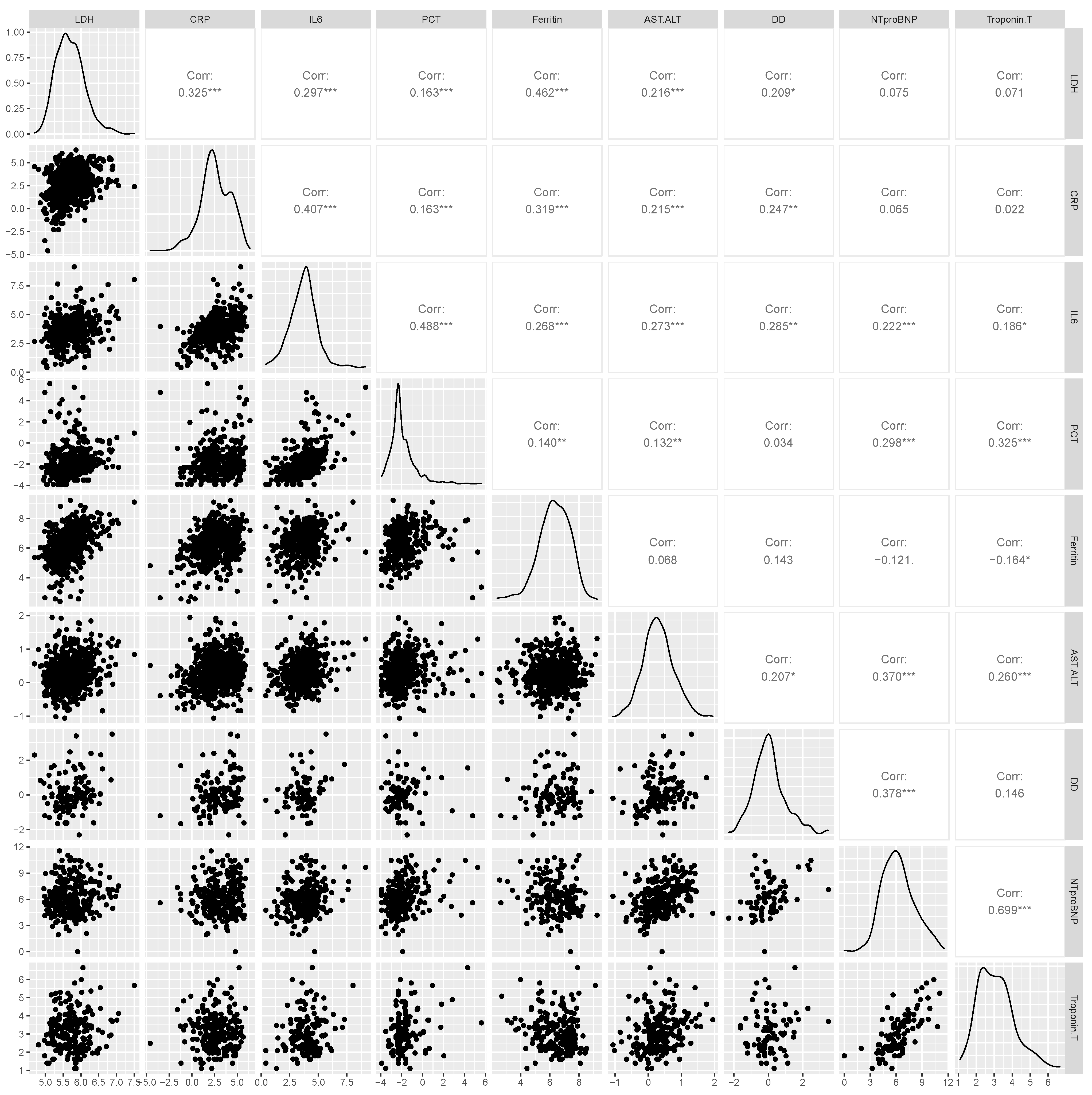
3.3. Correlation between Biomarkers
3.4. Association of Biomarkers with In-Hospital Mortality
3.5. Predictive Performance of Biomarkers
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int (accessed on 25 January 2022).
- Lim, S.; Bae, J.H.; Kwon, H.-S.; Nauck, M.A. COVID-19 and diabetes mellitus: From pathophysiology to clinical management. Nat. Rev. Endocrinol. 2020, 17, 11–30. [Google Scholar] [CrossRef] [PubMed]
- Ejaz, H.; Alsrhani, A.; Zafar, A.; Javed, H.; Junaid, K.; Abdalla, A.E.; Abosalif, K.O.A.; Ahmed, Z.; Younas, S. COVID-19 and comorbidities: Deleterious impact on infected patients. J. Infect. Public Health 2020, 13, 1833–1839. [Google Scholar] [CrossRef] [PubMed]
- Grasselli, G.; Zangrillo, A.; Zanella, A.; Antonelli, M.; Cabrini, L.; Castelli, A.; Cereda, D.; Coluccello, A.; Foti, G.; Fumagalli, R.; et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the lombardy region, Italy. JAMA 2020, 323, 1574–1581. [Google Scholar] [CrossRef] [Green Version]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Richardson, S.; Hirsch, J.S.; Narasimhan, M.; Crawford, J.M.; McGinn, T.; Davidson, K.W.; the Northwell COVID-19 Research Consortium; Barnaby, D.P.; Becker, L.B.; Chelico, J.D.; et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA 2020, 323, 2052–2059. [Google Scholar] [CrossRef]
- Aziz, F.; Aberer, F.; Bräuer, A.; Ciardi, C.; Clodi, M.; Fasching, P.; Karolyi, M.; Kautzky-Willer, A.; Klammer, C.; Malle, O.; et al. COVID-19 in-hospital mortality in people with diabetes is driven by comorbidities and age–propensity score-matched analysis of austrian national public health institute data. Viruses 2021, 13, 2401. [Google Scholar] [CrossRef]
- Aggarwal, G.; Lippi, G.; Lavie, C.J.; Henry, B.M.; Sanchis-Gomar, F. Diabetes mellitus association with coronavirus disease 2019 (COVID-19) severity and mortality: A pooled analysis. J. Diabetes 2020, 12, 851–855. [Google Scholar] [CrossRef]
- Samprathi, M.; Jayashree, M. Biomarkers in COVID-19: An up-to-date review. Front. Pediatrics 2021, 8, 972. [Google Scholar] [CrossRef]
- Bavishi, C.; Bonow, R.O.; Trivedi, V.; Abbott, J.D.; Messerli, F.H.; Bhatt, D.L. Special article-Acute myocardial injury in patients hospitalized with COVID-19 infection: A review. Prog. Cardiovasc. Dis. 2020, 63, 682–689. [Google Scholar] [CrossRef]
- Lavie, C.J.; Sanchis-Gomar, F.; Lippi, G. Cardiac injury in COVID-19-echoing prognostication. J. Am. Coll. Cardiol. 2020, 76, 2056–2059. [Google Scholar] [CrossRef]
- Miri, C.; Charii, H.; Bouazzaoui, M.-A.; Brem, F.L.; Boulouiz, S.; Abda, N.; Kouismi, H.; Bazid, Z.; Ismaili, N.; Ouafi, N.E. D-Dimer level and diabetes in the COVID-19 infection. Clin. Appl. Thromb. 2021, 27. [Google Scholar] [CrossRef] [PubMed]
- Koh, H.; Moh, A.M.C.; Yeoh, E.; Lin, Y.; Low, S.K.M.; Ooi, S.T.; Tan, S.K.; Lin, J.H.X.; Hoong, C.W.S. Diabetes predicts severity of COVID-19 infection in a retrospective cohort: A mediatory role of the inflammatory biomarker C-reactive protein. J. Med. Virol. 2021, 93, 3023–3032. [Google Scholar] [CrossRef] [PubMed]
- Sourij, H.; Aziz, F.; Bräuer, A.; Ciardi, C.; Clodi, M.; Fasching, P.; Karolyi, M.; Kautzky-Willer, A.; Klammer, C.; Malle, O.; et al. COVID-19 fatality prediction in people with diabetes and prediabetes using a simple score upon hospital admission. Diabetes Obes. Metab. 2021, 23, 589–598. [Google Scholar] [CrossRef] [PubMed]
- Harreiter, J.; Roden, M. Diabetes mellitus-definition, classification, diagnosis, screening and prevention (Update 2019). Wien. Klin. Wochenschr. 2019, 131, 6–15. [Google Scholar] [CrossRef]
- Acharya, D.; Lee, K.; Lee, D.S.; Lee, Y.S.; Moon, S.-S. Mortality rate and predictors of mortality in hospitalized COVID-19 patients with diabetes. Healthcare 2020, 8, 338. [Google Scholar] [CrossRef]
- Hammad, M.O.; Alseoudy, M.M. The sex-related discrepancy in laboratory parameters of severe COVID-19 patients with diabetes: A retrospective cohort study. Prim. Care Diabetes 2021, 15, 713–718. [Google Scholar] [CrossRef]
- Bhatti, R.; Khamis, A.H.; Khatib, S.; Shiraz, S.; Matfin, G. Clinical characteristics and outcomes of patients with diabetes admitted for COVID-19 treatment in dubai: Single-centre cross-sectional study. JMIR Public Health Surveill. 2020, 6, e22471. [Google Scholar] [CrossRef]
- Ceriello, A.; Standl, E.; Catrinoiu, D.; Itzhak, B.; Lalic, N.M.; Rahelic, D.; Schnell, O.; Škrha, J.; Valensi, P.; the “Diabetes and Cardiovascular Disease (D&CVD)” Study Group of the European Association for the Study of Diabetes (EASD). Issues for the Management of People with Diabetes and COVID-19 in ICU. Cardiovasc. Diabetol. 2020, 19. [Google Scholar] [CrossRef]
- Lippi, G.; Sanchis-Gomar, F.; Henry, B.M.; Lavie, C.J. Cardiac biomarkers in COVID-19: A narrative review. EJIFCC 2021, 32, 337–346. [Google Scholar]
- Lippi, G.; Lavie, C.J.; Sanchis-Gomar, F. Cardiac troponin I in patients with coronavirus disease 2019 (COVID-19): Evidence from a meta-analysis. Prog. Cardiovasc. Dis. 2020, 63, 390–391. [Google Scholar] [CrossRef]
- Wang, F.; Yang, Y.; Dong, K.; Yan, Y.; Zhang, S.; Ren, H.; Yu, X.; Shi, X. Clinical characteristics of 28 patients with diabetes and COVID-19 in Wuhan, China. Endocr. Pract. 2020, 26, 668–674. [Google Scholar] [CrossRef] [PubMed]
- Cunningham, J.W.; Claggett, B.L.; Jering, K.S.; Vaduganathan, M.; Bhatt, A.S.; Rosenthal, N.; Solomon, S.D. Prognostic value of natriuretic peptides and cardiac troponins in COVID-19. Circulation 2021, 144, 177–179. [Google Scholar] [CrossRef] [PubMed]
- Guo, T.; Fan, Y.; Chen, M.; Wu, X.; Zhang, L.; He, T.; Wang, H.; Wan, J.; Wang, X.; Lu, Z. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol. 2020, 5, 811–818. [Google Scholar] [CrossRef] [Green Version]
- Yap, L.B.; Mukerjee, D.; Timms, P.M.; Ashrafian, H.; Coghlan, J.G. Natriuretic peptides, respiratory disease, and the right heart. Chest 2004, 126, 1330–1336. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ramesh, J.; Reddy, S.L.S.; Rajesh, M.; Varghese, J. Evaluation of simple and cost-effective immuno- haematological markers to predict outcome in hospitalized severe COVID-19 patients, with a focus on diabetes mellitus-A retrospective study in Andhra Pradesh, India. Diabetes Metab. Syndr. 2021, 15, 739–745. [Google Scholar] [CrossRef] [PubMed]
- Lemkes, B.A.; Hermanides, J.; Devries, J.H.; Holleman, F.; Meijers, J.C.M.; Hoekstra, J.B.L. Hyperglycemia: A prothrombotic factor? J. Thromb. Haemost. 2010, 8, 1663–1669. [Google Scholar] [CrossRef]
- Phipps, M.M.; Barraza, L.H.; LaSota, E.D.; Sobieszczyk, M.E.; Pereira, M.R.; Zheng, E.X.; Fox, A.N.; Zucker, J.; Verna, E.C. Acute liver injury in COVID-19: Prevalence and association with clinical outcomes in a large, U.S. cohort. Hepatology 2020, 72, 807–817. [Google Scholar] [CrossRef]


| Variables | n | All | In-Hospital Mortality | p-Value | |
|---|---|---|---|---|---|
| Yes | No | ||||
| All, n (%) | 747 | -- | 142 (19.0) | 605 (81.0) | -- |
| Characteristics | |||||
| Age—years, mean ± SD | 717 | 70.3 ±13.3 | 78.63 ±10.0 | 68.3 ±13.2 | <0.001 |
| Sex, n (%) | 747 | ||||
| Male | 518 (69.3) | 95 (66.9) | 423 (69.9) | 0.483 | |
| Female | 229 (30.7) | 47 (33.1) | 182 (30.1) | ||
| Smoking status, n (%) | 747 | ||||
| Non-smoker | 372 (49.8) | 70 (49.3) | 302 (49.9) | 0.399 | |
| Former smoker | 97 (13.0) | 24 (16.9) | 73 (12.1) | ||
| Current smoker | 23 (3.1) | 5 (3.5) | 18 (3.0) | ||
| Unknown | 255 (34.1) | 43 (30.3) | 212 (35.0) | ||
| Body mass index—kg/m2, mean ± SD | 390 | 29.0 ±5.9 | 29.52 ±6.7 | 28.9 ±5.7 | 0.439 |
| Type of diabetes mellitus, n (%) | 747 | ||||
| Prediabetes | 111 (14.9) | 12 (8.5) | 99 (16.4) | 0.010 | |
| Type 1 diabetes mellitus | 43 (5.8) | 5 (3.5) | 38 (6.3) | ||
| Type 2 diabetes mellitus | 529 (70.8) | 117 (82.4) | 412 (68.1) | ||
| Other diabetes mellitus | 64 (8.6) | 8 (5.6) | 56 (9.3) | ||
| Comorbidities | |||||
| Hypertension, n (%) | 747 | 508 (68.0) | 112 (78.9) | 396 (65.5) | 0.002 |
| Coronary heart disease, n (%) | 747 | 198 (26.5) | 52 (36.6) | 146 (24.1) | 0.002 |
| Myocardial infarction, n (%) | 747 | 90 (12.1) | 25 (17.6) | 65 (10.7) | 0.024 |
| Heart failure, n (%) | 747 | 91 (12.2) | 38 (26.8) | 53 (8.8) | <0.001 |
| Peripheral artery disease, n (%) | 747 | 104 (13.9) | 38 (26.8) | 66 (10.9) | <0.001 |
| Stroke, n (%) | 747 | 57 (7.6) | 16 (11.3) | 41 (6.8) | 0.070 |
| Chronic kidney disease, n (%) | 747 | 160 (21.4) | 52 (36.6) | 108 (17.9) | <0.001 |
| Cancer, n (%) | 747 | 90 (12.1) | 28 (19.7) | 62 (10.3) | 0.002 |
| Respiratory disease, n (%) | 747 | 147 (19.7) | 35 (24.7) | 112 (18.5) | 0.098 |
| Liver disease, n (%) | 747 | 57 (7.6) | 14 (9.9) | 43 (7.1) | 0.266 |
| Inflammatory biomarkers | |||||
| LDH—U/L, median [IQR] | 681 | 288.0 [160.0] | 311.5 [165.0] | 281.0 [159.0] | 0.147 |
| CRP—mg/dL, median [IQR] | 711 | 12.1 [43.5] | 20.4 [66.9] | 10.7 [34.2] | <0.001 |
| IL6—pg/mL, median [IQR] | 489 | 41.8 [56.8] | 67.7 [80.7] | 38.5 [49.3] | <0.001 |
| PCT—ng/mL, median [IQR] | 503 | 0.1 [0.1] | 0.2 [0.4] | 0.1 [0.1] | <0.001 |
| Ferritin—ng/mL, median [IQR] | 555 | 568.0 [938.0] | 562.0 [864.0] | 570.0 [944.0] | 0.559 |
| Hepatic biomarkers | |||||
| AST—U/L, median [IQR] | 565 | 38.0 [29.0] | 42.0 [34.5] | 36.0 [28.0] | 0.027 |
| ALT—U/L, median [IQR] | 578 | 29.0 [25.0] | 27.0 [20.0] | 29.0 [27.0] | 0.037 |
| AST–ALT ratio | 564 | 1.33 [0.8] | 1.67 [1.0] | 1.28 [0.7] | <0.001 |
| Coagulation biomarkers | |||||
| D-dimer—mcg/mL, median [IQR] | 140 | 0.99 [0.97] | 1.28 [4.08] | 0.90 [0.98] | 0.016 |
| Cardiac biomarkers | |||||
| NT-proBNP—pg/mL, median [IQR] | 296 | 418.5 [1464.0] | 1333.5 [5003.5] | 297.0 [730.0] | <0.001 |
| Troponin T—pg/mL, median [IQR] | 242 | 20.0 [31.0] | 43.0 [44.0] | 16.0 [22.0] | <0.001 |
| Biomarkers | Simple Logistic Regression | Multiple Logistic Regression | ||||
|---|---|---|---|---|---|---|
| OR | 95%CI | p-Value | AOR | 95%CI | p-Value | |
| Inflammatory biomarkers | ||||||
| LDH—U/L | 1.4 | 0.88–2.25 | 0.158 | 2.03 | 1.21–3.42 | 0.008 |
| CRP—mg/dL | 1.3 | 1.15–1.47 | <0.001 | 1.33 | 1.16–1.52 | <0.001 |
| IL6—pg/mL | 1.66 | 1.34–2.06 | <0.001 | 1.6 | 1.27–2.01 | <0.001 |
| PCT—ng/mL | 1.31 | 1.13–1.51 | <0.001 | 1.25 | 1.06–1.48 | 0.007 |
| Ferritin—ng/mL | 0.9 | 0.74–1.10 | 0.3 | 1.07 | 0.86–1.35 | 0.541 |
| Coagulation biomarkers | ||||||
| D-dimer—mcg/mL | 1.93 | 1.22–3.03 | 0.005 | 1.66 | 0.97–2.82 | 0.063 |
| Hepatic biomarkers | ||||||
| AST–ALT ratio | 3 | 1.97–4.56 | <0.001 | 1.89 | 1.19–3.01 | 0.007 |
| Cardiac biomarkers | ||||||
| NT-proBNP—pg/mL | 1.59 | 1.35–1.86 | <0.001 | 1.5 | 1.24–1.80 | <0.001 |
| Troponin T—pg/mL | 2.78 | 1.90–4.07 | <0.001 | 2.2 | 1.44–3.35 | <0.001 |
| Biomarkers | Hosmer–Lemeshow Test | |
|---|---|---|
| Statistics | p-Value | |
| Inflammatory biomarkers | ||
| LDH—U/L | 3.22 | 0.920 |
| CRP—mg/dL | 5.82 | 0.667 |
| IL6—pg/mL | 3.81 | 0.874 |
| PCT—ng/mL | 6.63 | 0.577 |
| Ferritin—ng/mL | 6.42 | 0.600 |
| Coagulation biomarkers | ||
| D-dimer—mcg/mL | 6.19 | 0.626 |
| Hepatic biomarkers | ||
| AST–ALT ratio | 7.96 | 0.437 |
| Cardiac biomarkers | ||
| NT-proBNP—pg/mL | 9.50 | 0.302 |
| Troponin T—pg/mL | 20.03 | 0.010 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aziz, F.; Stöcher, H.; Bräuer, A.; Ciardi, C.; Clodi, M.; Fasching, P.; Karolyi, M.; Kautzky-Willer, A.; Klammer, C.; Malle, O.; et al. Biomarkers Predictive for In-Hospital Mortality in Patients with Diabetes Mellitus and Prediabetes Hospitalized for COVID-19 in Austria: An Analysis of COVID-19 in Diabetes Registry. Viruses 2022, 14, 1285. https://doi.org/10.3390/v14061285
Aziz F, Stöcher H, Bräuer A, Ciardi C, Clodi M, Fasching P, Karolyi M, Kautzky-Willer A, Klammer C, Malle O, et al. Biomarkers Predictive for In-Hospital Mortality in Patients with Diabetes Mellitus and Prediabetes Hospitalized for COVID-19 in Austria: An Analysis of COVID-19 in Diabetes Registry. Viruses. 2022; 14(6):1285. https://doi.org/10.3390/v14061285
Chicago/Turabian StyleAziz, Faisal, Hannah Stöcher, Alexander Bräuer, Christian Ciardi, Martin Clodi, Peter Fasching, Mario Karolyi, Alexandra Kautzky-Willer, Carmen Klammer, Oliver Malle, and et al. 2022. "Biomarkers Predictive for In-Hospital Mortality in Patients with Diabetes Mellitus and Prediabetes Hospitalized for COVID-19 in Austria: An Analysis of COVID-19 in Diabetes Registry" Viruses 14, no. 6: 1285. https://doi.org/10.3390/v14061285
APA StyleAziz, F., Stöcher, H., Bräuer, A., Ciardi, C., Clodi, M., Fasching, P., Karolyi, M., Kautzky-Willer, A., Klammer, C., Malle, O., Aberer, F., Pawelka, E., Peric, S., Ress, C., Sourij, C., Stechemesser, L., Stingl, H., Stulnig, T., Tripolt, N., ... for the COVID-19 in Diabetes in Austria. (2022). Biomarkers Predictive for In-Hospital Mortality in Patients with Diabetes Mellitus and Prediabetes Hospitalized for COVID-19 in Austria: An Analysis of COVID-19 in Diabetes Registry. Viruses, 14(6), 1285. https://doi.org/10.3390/v14061285










