Adaptation of the H7N2 Feline Influenza Virus to Human Respiratory Cell Culture
Abstract
1. Introduction
2. Materials and Methods
2.1. Cells and Viruses
2.2. Passages of H7N2 Feline Influenza Virus in A549 Cells
2.3. Growth Kinetics of the Virus in A549 Cells
2.4. Sequence Analysis
2.5. Reverse Genetics
2.6. Syncytium Assay for Cell Fusion
2.7. Thermostability Assay
2.8. Virus Release Assay
2.9. Statistical Analysis
3. Results
3.1. Adaptation of H7N2 Feline Influenza Virus to A549 Cells
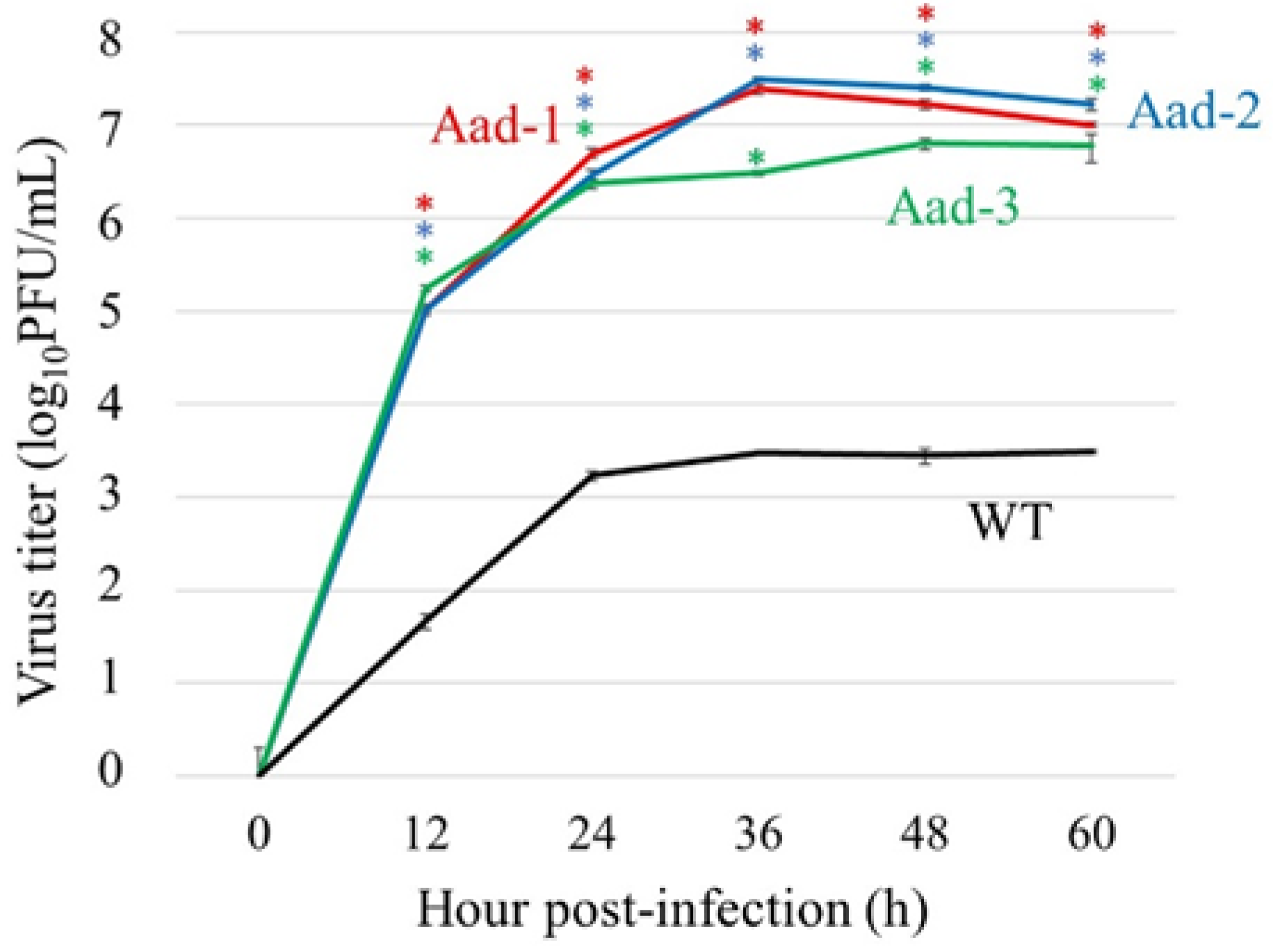
3.2. Replication of Aad Viruses in A549 Cells
3.3. Sequence Analysis of A549-Adapted Viruses
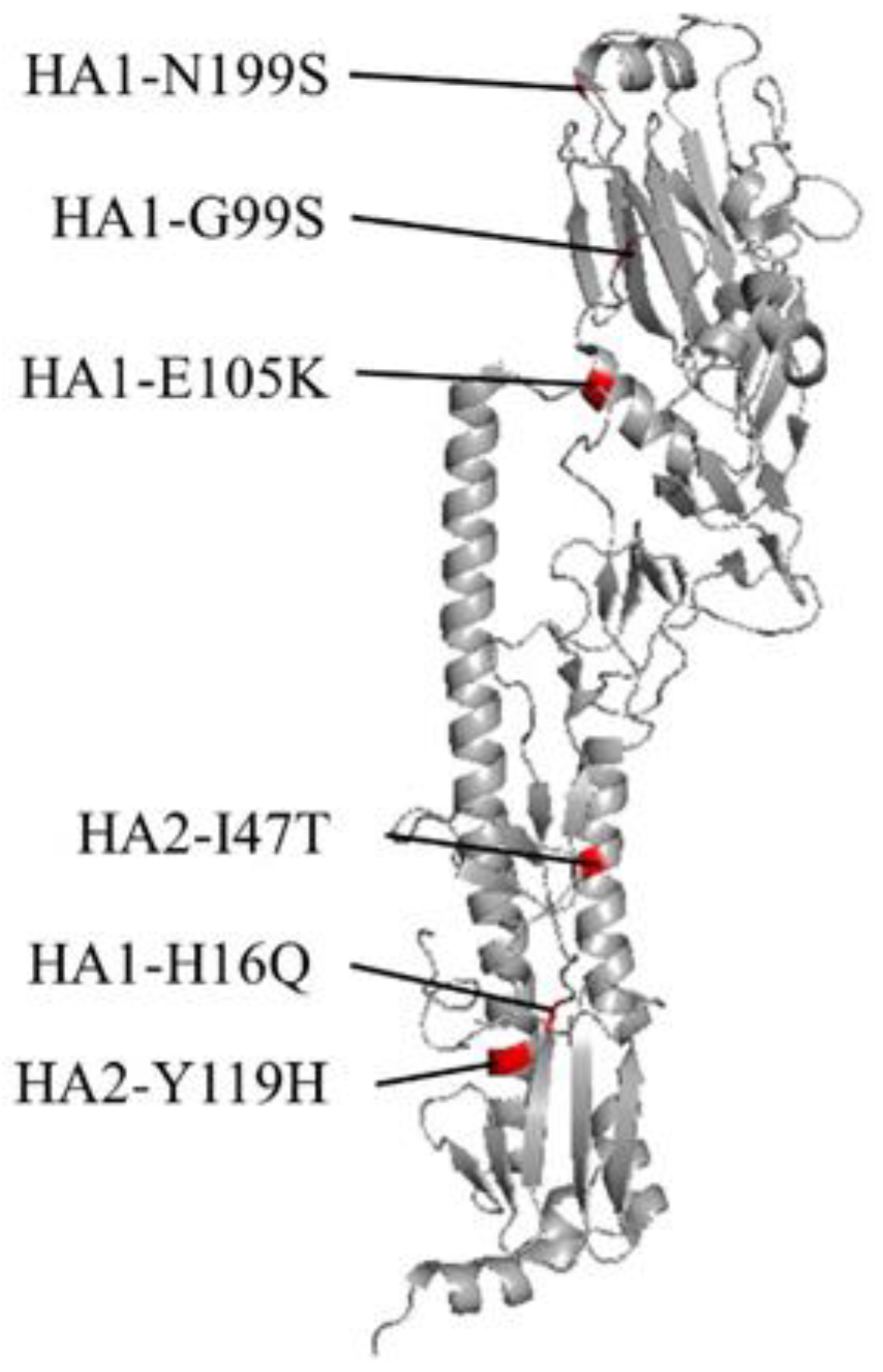
3.4. Generation and Replication of Recombinant Aad Viruses
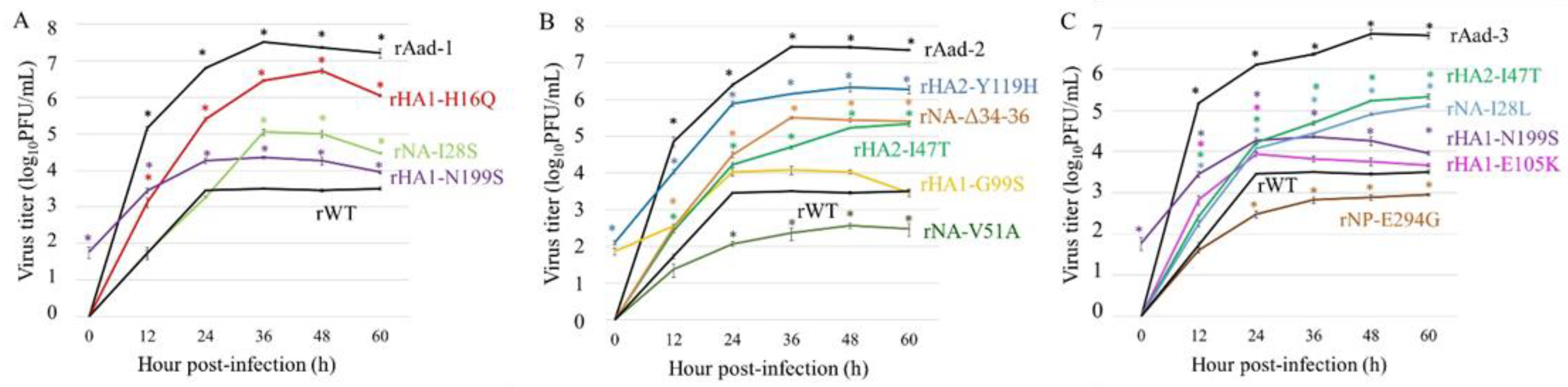
3.5. Effects of Mutations on Virus Growth in A549 Cells
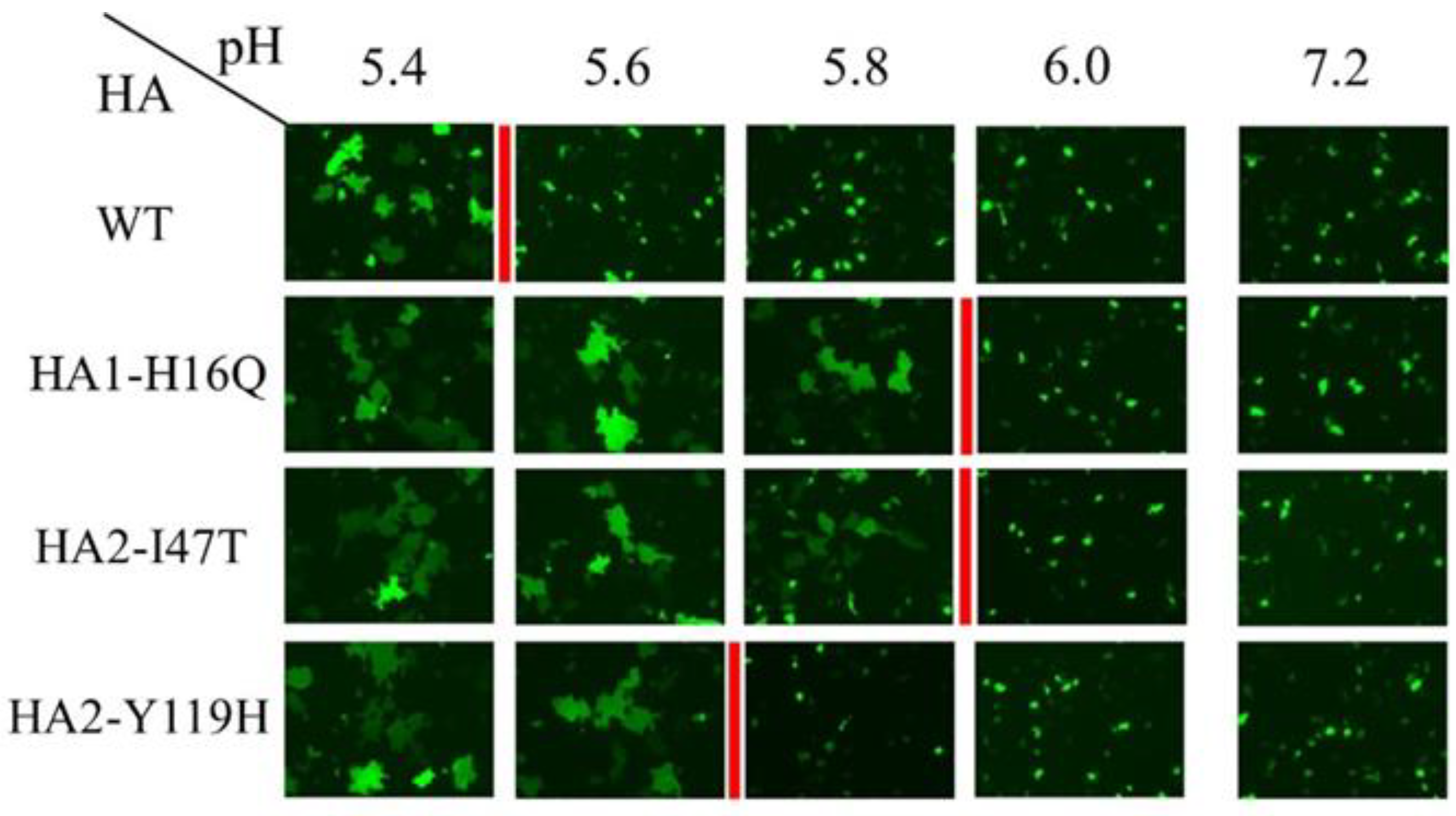
3.6. Change in the pH Threshold of Syncytium Formation by HA Mutations
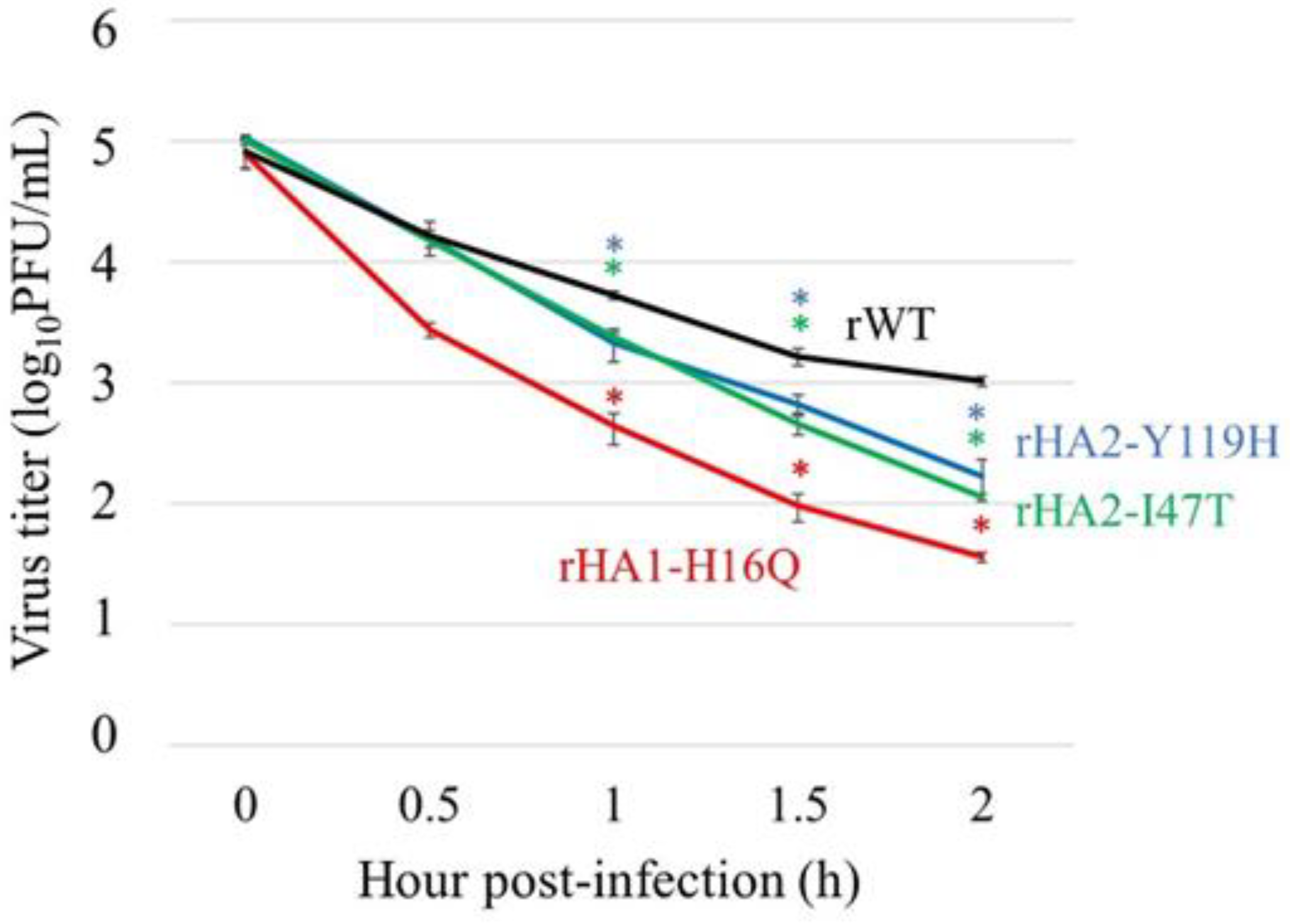
3.7. Thermostability of HA Mutants
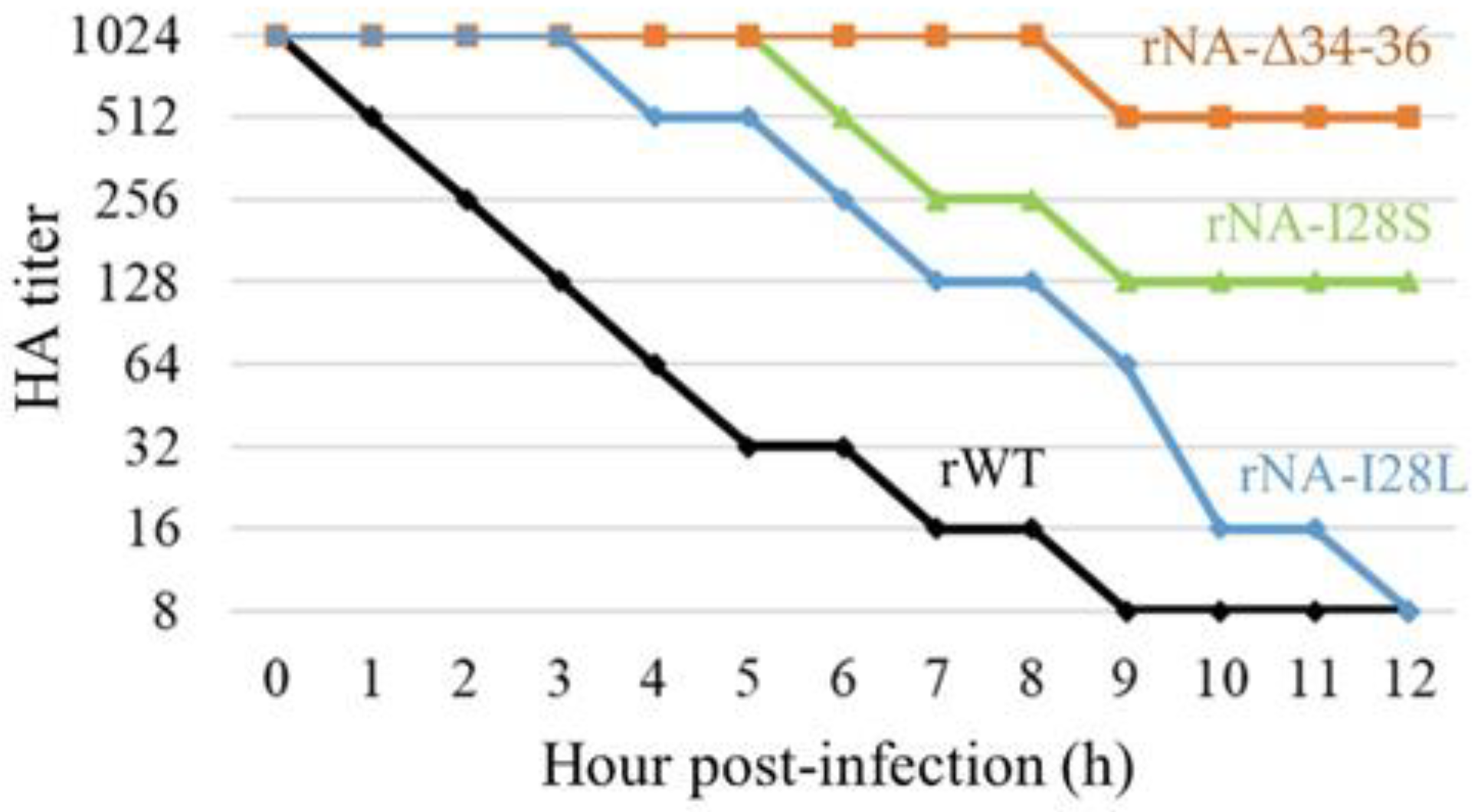
3.8. Change in HA–NA Functional Balance by NA Mutations
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wright, P.F.; Neumann, G.; Kawaoka, Y. Orthomyxoviruses. In Fields Virology, 6th ed.; Knipe, D.M., Howley, P.M., Eds.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2013; pp. 1186–1243. [Google Scholar]
- Long, J.S.; Mistry, B.; Haslam, S.M.; Barclay, W.S. Host and viral determinants of influenza A virus species specificity. Nat. Rev. Microbiol. 2019, 17, 67–81. [Google Scholar] [CrossRef] [PubMed]
- Neumann, G.; Kawaoka, Y. Transmission of influenza A viruses. Virology 2015, 479–480, 234–246. [Google Scholar] [CrossRef] [PubMed]
- Newbury, S.P.; Cigel, F.; Killian, M.L.; Leutenegger, C.M.; Seguin, M.A.; Crossley, B.; Brennen, R.; Suarez, D.L.; Torchetti, M.; Toohey-Kurth, K. First Detection of Avian Lineage H7N2 in Felis catus. Genome Announc. 2017, 5, e00457-17. [Google Scholar] [CrossRef]
- Lee, C.T.; Slavinski, S.; Schiff, C.; Merlino, M.; Daskalakis, D.; Liu, D.; Rakeman, J.L.; Misener, M.; Thompson, C.; Leung, Y.L.; et al. Influenza A(H7N2) Response Team. Outbreak of Influenza A(H7N2) among cats in an animal shelter with cat-to-human transmission—New York City, 2016. Clin. Infect. Dis. 2017, 65, 1927–1929. [Google Scholar] [CrossRef] [PubMed]
- Marinova-Petkova, A.; Laplante, J.; Jang, Y.; Lynch, B.; Zanders, N.; Rodriguez, M.; Jones, J.; Thor, S.; Hodges, E.; Cruz, J.A.D.L.; et al. Avian influenza A(H7N2) virus in human exposed to sick cats, New York, USA, 2016. Emerg. Infect. Dis. 2017, 23, 2046–2049. [Google Scholar] [CrossRef]
- Poirot, E.; Levine, M.Z.; Russell, K.; Stewart, R.J.; Pompey, J.M.; Chiu, S.; Fry, A.M.; Gross, L.; Havers, F.P.; Li, Z.N.; et al. Detection of avian influenza A(H7N2) virus infection among animal shelter workers using a novel serological approach—New York City, 2016–2017. J. Infect. Dis. 2018, 219, 1688–1696. [Google Scholar] [CrossRef]
- Wasik, B.R.; Voorhees, I.E.H.; Parrish, C.R. Canine and feline influenza. Cold Spring Harb. Perspect. Med. 2021, 11, a038562. [Google Scholar] [CrossRef]
- Weber, S.; Harder, T.; Starick, E.; Beer, M.; Werner, O.; Hoffmann, B.; Mettenleiter, T.C.; Mundt, E. Molecular analysis of highly pathogenic avian influenza virus of subtype H5N1 isolated from wild birds and mammals in northern Germany. J. Gen. Virol. 2007, 88, 554–558. [Google Scholar] [CrossRef]
- Kuiken, T.; Rimmelzwaan, G.; Riel, D.; Amerongen, G.; Baars, M.; Foucheur, B.; Osterhaus, A. Avian H5N1 influenza in cats. Science 2004, 306, 241. [Google Scholar] [CrossRef]
- Songserm, T.; Amonsin, A.; Jam-on, R.; Sae-Heng, N.; Meemak, N.; Pariyothorn, N.; Payungporn, S.; Theamboonlers, A.; Poovorawan, Y. Avian influenza H5N1 in naturally infected domestic cat. Emerg. Infect. Dis. 2006, 12, 681–683. [Google Scholar] [CrossRef]
- Amonsin, A.; Songserm, T.; Chutinimitkul, S.; Jam-On, R.; Sae-Heng, N.; Pariyothorn, N.; Payungporn, S.; Theamboonlers, A.; Poovorawan, Y. Genetic analysis of influenza A virus (H5N1) derived from domestic cat and dog in Thailand. Arch. Virol. 2007, 152, 1925–1933. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.; Lee, E.-K.; Lee, H.; Heo, G.-B.; Lee, Y.-N.; Jung, J.-Y.; Bae, Y.-C.; So, B.; Lee, Y.-J.; Choi, E.-J. Highly pathogenic avian influenza A(H5N6) in domestic cats, south Korea. Emerg. Infect. Dis. 2018, 24, 2343–2347. [Google Scholar] [CrossRef] [PubMed]
- Sponseller, B.A.; Strait, E.; Jergens, A.; Harmon, K.; Koster, L.; Jenkins-Moore, M.; Killian, M.; Swenson, S.; Bender, H.; Waller, K.; et al. Influenza A pandemic (H1N1) 2009 virus infection in domestic cat. Emerg. Infect. Dis. 2010, 16, 534–537. [Google Scholar] [CrossRef] [PubMed]
- Zhao, S.; Schuurman, N.; Tieke, M.; Quist, B.; Zwinkels, S.; van Kuppeveld, F.J.M.; de Haan, C.A.M.; Egberink, H. Serological screening of influenza A virus antibodies in cats and dogs indicates frequent infection with different subtypes. J. Clin. Microbiol. 2020, 58, e01689-20. [Google Scholar] [CrossRef]
- Lee, C.-W.; Lee, Y.-J.; Senne, D.A.; Suarez, D.L. Pathogenic potential of North American H7N2 avian influenza virus: A mutagenesis study using reverse genetics. Virology 2006, 353, 388–395. [Google Scholar] [CrossRef][Green Version]
- Watanabe, T.; Watanabe, S.; Maher, E.A.; Neumann, G.; Kawaoka, Y. Pandemic potential of avian influenza A (H7N9) viruses. Trends Microbiol. 2014, 22, 623–631. [Google Scholar] [CrossRef]
- Hatta, M.; Zhong, G.; Gao, Y.; Nakajima, N.; Fan, S.; Chiba, S.; Deering, K.M.; Ito, M.; Imai, M.; Kiso, M.; et al. Characterization of a feline influenza A(H7N2) virus. Emerg. Infect. Dis. 2018, 24, 75–86. [Google Scholar] [CrossRef]
- Hoffmann, E.; Stech, J.; Guan, Y.; Webster, R.G.; Perez, D.R. Universal primer set for the full-length amplification of all influenza A viruses. Arch. Virol. 2001, 146, 2275–2289. [Google Scholar] [CrossRef]
- Neumann, G.; Watanabe, T.; Ito, H.; Watanabe, S.; Goto, H.; Gao, P.; Hughes, M.; Perez, D.R.; Donis, R.; Hoffman, E.; et al. Generation of influenza A viruses entirely from cloned cDNAs. Proc. Natl. Acad. Sci. USA 1999, 96, 9345–9350. [Google Scholar] [CrossRef]
- Murakami, S.; Horimoto, T.; Ito, M.; Takano, R.; Katsura, H.; Shimojima, M.; Kawaoka, Y. Enhanced growth of influenza vaccine seed viruses in vero cells mediated by broadening the optimal pH range for virus membrane fusion. J. Virol. 2012, 86, 1405–1410. [Google Scholar] [CrossRef]
- Hanson, A.; Imai, M.; Hatta, M.; Mcbrige, R.; Imai, H.; Taft, A.; Zhong, G.; Watanabe, T.; Suzuki, Y.; Neumann, G.; et al. Identification of stabilizing mutations in an H5 hemagglutinin influenza virus protein. J. Virol. 2016, 90, 2981–2992. [Google Scholar] [CrossRef] [PubMed]
- Zhou, H.; Yu, Z.; Hu, Z.; Tu, J.; Zou, W.; Peng, Y.; Zhu, J.; Li, Y.; Zhang, A.; Yu, Z.; et al. The special neuraminidase stalk-motif responsible for increased virulence and pathogenesis of H5N1 influenza A virus. PLoS ONE 2009, 4, e6277. [Google Scholar] [CrossRef] [PubMed]
- Cotter, C.R.; Jin, H.; Chen, Z. A single amino acid in the stalk region of the H1N1pdm influenza virus HA protein affects viral fusion, stability and infectivity. PLoS Pathog. 2014, 10, e1003831. [Google Scholar] [CrossRef] [PubMed]
- Russell, C.J.; Hu, M.; Okda, F.A. Influenza hemagglutinin protein stability, activation, and pandemic risk. Trends Microbiol. 2018, 26, 841–853. [Google Scholar] [CrossRef]
- Mostafa, A.; Abdelwhab, E.M.; Mettenleiter, T.C.; Pleschka, S. Zoonotic potential of 1nfluenza A airuses: A comprehensive overview. Viruses 2018, 10, 497. [Google Scholar] [CrossRef]
- Kilbourne, E.D. Influenza pandemics of the 20th century. Emerg. Infect. Dis. 2006, 12, 9–14. [Google Scholar] [CrossRef]
- Ito, T.; Couceiro, J.N.S.S.; Kelm, S.; Baum, L.G.; Krauss, S.; Castrucci, M.R.; Donatelli, I.; Kida, H.; Paulson, J.C.; Webster, R.G.; et al. Molecular basis for the generation in pigs of influenza A viruses with pandemic potential. J. Virol. 1998, 72, 7367–7373. [Google Scholar] [CrossRef]
- Imai, M.; Kawaoka, Y. The role of receptor binding specificity in interspecies transmission of influenza viruses. Curr. Opin. Virol. 2012, 2, 160–167. [Google Scholar] [CrossRef]
- Shi, Y.; Wu, Y.; Zhang, W.; Qi, J.; Gao, G.F. Enabling the “host jump”: Structural determinants of receptor-binding specificity in influenza A viruses. Nat. Rev. Microbiol. 2014, 12, 822–831. [Google Scholar] [CrossRef]
- Rogers, G.N.; Paulson, J.C. Receptor determinants of human and animal influenza virus isolates: Differences in receptor specificity of the H3 hemagglutinin based on species of origin. Virology 1983, 127, 361–373. [Google Scholar] [CrossRef]
- Thongratsakul, S.; Suzuki, Y.; Hiramatsu, H.; Sakpuaram, T.; Sirinarumitr, T.; Poolkhet, C.; Moonjit, P.; Yodsheewan, R.; Songserm, T. Avian and human influenza A virus receptors in trachea and lung of animals. Asian Pac. J. Allergy Immunol. 2010, 28, 294–301. [Google Scholar] [PubMed]
- Ujie, M.; Takada, K.; Kiso, M.; Sakai-Tagawa, Y.; Ito, M.; Nakamura, K.; Watanabe, S.; Imai, M.; Kawaoka, Y. Long-term culture of human lung adenocarcinoma A549 cells enhances the replication of human influenza A viruses. J. Gen. Virol. 2019, 100, 1345–1349. [Google Scholar] [CrossRef] [PubMed]
- Shi, Y.-Q.; He, Q.; Zhao, Y.-J.; Wang, E.-H.; Wu, G.-P. Lectin microarrays differentiate carcinoma cells from reactive mesothelial cells in pleural effusions. Cytotechnology 2013, 65, 355–362. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Shinya, K.; Ebina, M.; Yamada, S.; Ono, M.; Kasai, N.; Kawaoka, Y. Influenza virus receptors in the human airway. Nature 2006, 440, 435–436. [Google Scholar] [CrossRef]
- Watanabe, Y.; Arai, Y.; Kawashita, N.; Ibrahim, M.S.; Elgendy, E.M.; Daidoji, T.; Kajikawa, J.; Hiramatsu, H.; Sriwilaijaroen, N.; Ono, T.; et al. Characterization of H5N1 influenza virus quasispecies with adaptive hemagglutinin mutations from single-virus infections of human airway cells. J. Virol. 2018, 92, e02004-17. [Google Scholar] [CrossRef]
- Xu, R.; Zhu, X.; McBride, R.; Nycholat, C.M.; Yu, W.; Paulson, J.C.; Wilson, I.A. Functional balance of the hemagglutinin and neuraminidase activities accompanies the emergence of the 2009 H1N1 influenza pandemic. J. Virol. 2012, 86, 9221–9232. [Google Scholar] [CrossRef]
- Diederich, S.; Berhane, Y.; Embury-Hyatt, C.; Hisanaga, T.; Handel, K.; Cottam-Birt, C.; Ranadheera, C.; Kobasa, D.; Pasick, J. Hemagglutinin-neuraminidase balance influences the virulence phenotype of a recombinant H5N3 influenza A virus possessing a polybasic HA0 cleavage site. J. Virol. 2015, 89, 10724–10734. [Google Scholar] [CrossRef]
- Yen, H.L.; Liang, C.H.; Wu, C.Y.; Forrest, H.L.; Ferguson, A.; Choy, K.T.; Jones, J.; Wong, D.D.; Cheung, P.P.; Hsu, C.H.; et al. Hemagglutinin-neuraminidase balance confers respiratory-droplet transmissibility of the pandemic H1N1 influenza virus in ferrets. Proc. Natl. Acad. Sci. USA 2011, 108, 14264–14269. [Google Scholar] [CrossRef]
- McAuley, J.L.; Gilbertson, B.P.; Trifkovic, S.; Brown, L.E.; McKimm-Breschkin, J.L. Influenza virus neuraminidase structure and functions. Front. Microbiol. 2019, 10, 39. [Google Scholar] [CrossRef]
- Barman, S.; Nayak, D.P. Analysis of the transmembrane domain of influenza virus neuraminidase, a type II transmembrane glycoprotein, for apical sorting and raft association. J. Virol. 2000, 74, 6538–6545. [Google Scholar] [CrossRef]
- Ernst, A.M.; Zacherl, S.; Herrmann, A.; Hacke, M.; Nickel, W.; Wieland, F.T.; Brügger, B. Differential transport of Influenza A neuraminidase signal anchor peptides to the plasma membrane. FEBS Lett. 2013, 587, 1411–1417. [Google Scholar] [CrossRef] [PubMed]

| Virus | HA1 | HA2 | NP | NA | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 16 1 | 99 | 105 | 199 | 47 | 119 | 294 | 28 | 34 | 35 | 36 | 51 | |
| Wild-type | H | G | E | N | I | Y | E | I | T | L | H | V |
| Aad-1 | Q2 | G | E | S | I | Y | E | S | T | L | H | V |
| Aad-2 | H | S | E | N | T | H | E | I | –3 | – | – | A |
| Aad-3 | H | G | K | S | T | Y | G | L | T | L | H | V |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sekine, W.; Takenaka-Uema, A.; Kamiki, H.; Ishida, H.; Matsugo, H.; Murakami, S.; Horimoto, T. Adaptation of the H7N2 Feline Influenza Virus to Human Respiratory Cell Culture. Viruses 2022, 14, 1091. https://doi.org/10.3390/v14051091
Sekine W, Takenaka-Uema A, Kamiki H, Ishida H, Matsugo H, Murakami S, Horimoto T. Adaptation of the H7N2 Feline Influenza Virus to Human Respiratory Cell Culture. Viruses. 2022; 14(5):1091. https://doi.org/10.3390/v14051091
Chicago/Turabian StyleSekine, Wataru, Akiko Takenaka-Uema, Haruhiko Kamiki, Hiroho Ishida, Hiromichi Matsugo, Shin Murakami, and Taisuke Horimoto. 2022. "Adaptation of the H7N2 Feline Influenza Virus to Human Respiratory Cell Culture" Viruses 14, no. 5: 1091. https://doi.org/10.3390/v14051091
APA StyleSekine, W., Takenaka-Uema, A., Kamiki, H., Ishida, H., Matsugo, H., Murakami, S., & Horimoto, T. (2022). Adaptation of the H7N2 Feline Influenza Virus to Human Respiratory Cell Culture. Viruses, 14(5), 1091. https://doi.org/10.3390/v14051091






