Infection, Dissemination, and Transmission Potential of North American Culex quinquefasciatus, Culex tarsalis, and Culicoides sonorensis for Oropouche Virus
Abstract
1. Introduction
2. Materials and Methods
2.1. Insects
2.2. Infection
2.3. Collections
2.4. Sample Testing
2.5. Data Analysis
3. Results
3.1. Infection, Dissemination, and Transmission Potential
3.2. Statistical Analyses of Viral Titers and Infections between Vectors
3.3. Survival Rates of Experimental and Control Insects
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Travassos da Rosa, J.F.; Marciel de Souza, W.; Pinheiro, F.P.; Figueiredo, M.L.; Cardoso, J.F.; Acrani, G.O.; Nunes, M.R.T. Oropouche virus: Clinical, epidemiological, and molecular aspects of a neglected Orthobunyavirus. Am. J. Trop. Med. Hyg. 2017, 96, 1019–1030. [Google Scholar]
- Pinheiro, F.P.; Travassos da Rosa, A.P.A.; Travassos da Rosa, J.F.S.; Ishak, R.; Freitas, R.B.; Gomes, M.L.C.; LeDuc, J.W.; Oliva, O.F.; Oropouche Virus, I. A review of clinical, epidemiological, and ecological findings. Am. J. Trop. Med. Hyg. 1981, 30, 149–160. [Google Scholar] [CrossRef] [PubMed]
- Mourão, M.P.G.; Bastos, M.S.; Gimaque, J.B.L.; Mota, B.R.; Souza, G.S.; Grimmer, G.H.N.; Galusso, E.S.; Arruda, E.; Figueiredo, L.T.M. Oropouche fever outbreak, Manaus, Brazil, 2007–2008. Emerg Infect. Dis. 2009, 15, 2063–2064. [Google Scholar] [CrossRef] [PubMed]
- Tesh, R.B. The emerging epidemiology of Venezuelan hemorrhagic fever and Oropouche fever in tropical South America. Ann. N. Y. Acad. Sci. 1994, 740, 129–137. [Google Scholar] [CrossRef] [PubMed]
- Baisley, K.J.; Watts, D.M.; Munstermann, L.E.; Wilson, M.L. Epidemiology of endemic Oropouche virus transmission in upper Amazonian Peru. Am. J. Trop. Med. Hyg. 2001, 59, 710–716. [Google Scholar] [CrossRef] [PubMed]
- Romero-Alvarez, D.; Escobar, L.E. Oropouche fever, an emergent disease from the Americas. Microbes Infect. 2018, 20, 135–146. [Google Scholar] [CrossRef] [PubMed]
- Wise, E.L.; Pullan, S.T.; Márquez, S.; Paz, V.; Mosquera, J.D.; Zapata, S.; Jackson, S.K.; Fejer, G.; Trueba, G.; Logue, C.H. Isolation of Oropouche virus from febrile patient, Ecuador. Emerg Infect. Dis. 2018, 24, 935–937. [Google Scholar] [CrossRef] [PubMed]
- LeDuc, J.W.; Hoch, A.L.; Pinheiro, F.P.; Travassos da Rosa, A.P.A. Epidemic Oropouche virus disease in Northern Brazil. Bull. Pan Am. Health Organ. 1981, 15, 97–103. [Google Scholar] [PubMed]
- Pinheiro, F.P.; Hoch, A.L.; Gomes, M.L.; Roberts, D.R. Oropouche virus IV. Laboratory transmission by Culicoides paraensis. Am. J. Trop. Med. Hyg. 1980, 30, 172–176. [Google Scholar] [CrossRef]
- Pinheiro, F.P.; Travassos da Rosa, A.P.A.; Travassos da Rosa, J.F.; Bensabath, G. An outbreak of Oropouche virus disease in the vicinity of Santarem, Para, Brazil. Tropenmed. Parasit. 1976, 27, 213–223. [Google Scholar]
- Owen, J.; Moore, F.; Panella, N.; Edwards, E.; Bru, R.; Hughes, M.; Komar, N. Migrating birds as dispersal vehicles for West Nile virus. EcoHealth 2006, 3, 79. [Google Scholar] [CrossRef]
- Smith, R.P.; Rand, P.W.; Lacombe, E.H.; Morris, S.R.; Holmes, D.W.; Caporale, D.A. Role of bird migration in the long-distance dispersal of Ixodes dammini, the vector of Lyme disease. J. Infect. Dis. 1996, 174, 221–224. [Google Scholar] [CrossRef] [PubMed]
- Elfving, K.; Olsen, B.; Bergström, S.; Waldenström, J.; Lundkvist, Å.; Mejlon, H.; Nilsson, K. Dissemination of spotted fever Rickettsia agents in Europe by migrating birds. PLoS ONE 2010, 5, e8572. [Google Scholar] [CrossRef] [PubMed]
- Bingham, A.M.; Burkett-Cadena, N.D.; Hassan, H.K.; McClure, C.J.W.; Unnasch, T.R. Field investigations of winter transmission of Eastern Equine Encephalitis virus in Florida. Am. J. Trop. Med. Hyg. 2014, 91, 685–693. [Google Scholar] [CrossRef]
- Calisher, C.H.; Maness, K.S.C.; Lord, R.D.; Coleman, P.H. Identification of two South American strains of Eastern Equine Encephalomyelitis virus from migrant birds captured on the Mississippi Delta. Am. J. Epidem. 1971, 94, 172–178. [Google Scholar] [CrossRef]
- Likos, A.; Griffin, I.; Bingham, A.M.; Stanek, D.; Fischer, M.; White, S.; Hamilton, J.; Eisenstein, L.; Atrubin, D.; Mulay, P.; et al. Local mosquito-borne transmission of Zika virus-Miami-Dade and Broward counties, Florida, June-August 2016. MMWR 2016, 65, 1032–1038. [Google Scholar] [CrossRef]
- Tsetsarkin, K.A.; Vanlandingham, D.L.; McGee, C.E.; Higgs, S. A single mutation in Chikungunya virus affects vector specificity and epidemic potential. PLoS Path. 2007, 3, e201. [Google Scholar] [CrossRef]
- Navarro, J.C.; Giambalyo, D.; Hernandez, R.; Auguste, A.J.; Tesh, R.B.; Weaver, S.C.; Montañez, H.; Liria, J.; Lima, A.; Travassos da Rosa, J.F.S.; et al. Isolation of Madre de Dios virus (Orthobunyavirus; Bunyaviridae), an Oropouche Virus species reassortant, from a monkey in Venezuela. Am. J. Trop. Med. Hyg. 2016, 95, 328–338. [Google Scholar] [CrossRef]
- Aguilar, P.V.; Barrett, A.D.; Saeed, M.F.; Watts, D.M.; Russell, K.; Guevara, C.; Ampuero, J.S.; Suarez, L.; Cespedes, M.; Montgomery, J.M.; et al. Iquitos virus: A novel reassortant Orthobunyavirus associated with human illness in Peru. PLoS Neg. Trop. Dis. 2011, 5, e1315. [Google Scholar] [CrossRef]
- Wilson, A.L.; Courtenay, O.; Kelly-Hope, L.A.; Scott, T.W.; Takken, W.; Torr, S.J.; Lindsay, S.W. The importance of vector control for the control and elimination of vector-borne diseases. PLoS Neg. Trop. Dis. 2020, 14, e0007831. [Google Scholar] [CrossRef]
- Rosenberg, R.; Lindsey, N.P.; Fischer, M.; Gregory, C.J.; Hinckley, A.F.; Mead, P.S. Paz-Bailey, G.; Waterman, S.H.; Drexler, N.A.; Kersh, G.J.; et al. Vital Signs: Trends in reported vectorborne disease cases—United States and territories, 2004–2016. MMWR 2018, 67, 496–501. [Google Scholar]
- Petersen, L.R.; Beard, C.B.; Visser, S.N. Combatting the increasing threat of vector-borne disease in the United States with a national vector-borne disease prevention and control system. Am. J. Trop. Med. Hyg. 2019, 100, 242–245. [Google Scholar] [CrossRef]
- Pfannenstiel, R.S.; Mullens, B.A.; Ruder, M.G.; Zurek, L.; Cohnstaedt, L.W.; Nayduch, D. Management of North American Culicoides biting midges: Current knowledge and research needs. Vector-Borne Zoonotic Dis. 2015, 15, 374–384. [Google Scholar] [CrossRef]
- Anderson, S.L.; Richards, S.L.; Smartt, C.T. A simple method for determining arbovirus transmission in mosquitoes. J. Am. Mosq. Control Assoc. 2010, 26, 108–111. [Google Scholar] [CrossRef]
- Richards, S.L.; Lord, C.C.; Pesko, K.; Tabachnick, W.J. Environmental and biological factors influencing Culex pipiens quinquefasciatus Say (Diptera: Culicidae) vector competence for Saint Louis encephalitis virus. Am. J. Trop. Med. Hyg. 2009, 81, 264–272. [Google Scholar] [CrossRef]
- Alto, B.W.; Wiggins, K.; Eastmond, B.; Velez, D.; Lounibos, L.P.; Lord, C.C. Transmission risk of two chikungunya lineages by invasive mosquito vectors from Florida and the Dominican Republic. PLoS Neg. Trop. Dis. 2017, 11, e0005724. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2019. [Google Scholar]
- Darsie, R.F., Jr.; Ward, R.A. Identification and Geographical Distribution of the Mosquitoes of North America, North of Mexico; University Press of Florida: Gainesville, FL, USA, 2005; pp. 300–303. [Google Scholar]
- Burkett-Cadena, N.D. Mosquitoes of the Southeastern United States; The University of Alabama Press: Tuscaloosa, AL, USA, 2013; pp. 141–147. [Google Scholar]
- Borkent, A.; Grogan, W.L., Jr. Catalog of the New World Biting Midges North of Mexico. Zootaxa 2009, 2273, 1–48. [Google Scholar] [CrossRef]
- Jewiss-Gaines, A.; Barelli, L.; Hunter, F.F. First records of Culicoides sonorensis (Diptera: Ceratopogonidae), a known vector of bluetongue virus, in Southern Ontario. J. Med. Entomol. 2017, 54, 757–762. [Google Scholar]
- Huerta, H.; Castrejón, A.M.R.; Grogan, W.L., Jr.; Ibáñez-Bernal, S. Culicoides (Monoculicoides) variipennis complex. In New records of biting midges of the genus Culicoides Latreille from Mexico (Diptera: Ceratopogonidae). Insecta Mundi 2012, 0211, 12–14. [Google Scholar]
- Price, D.A.; Hardy, W.T. Isolation of the bluetongue virus from Texas sheep-Culicoides shown to be a vector. J. Am. Vet. Med. Assoc. 1954, 124, 255–258. [Google Scholar]
- Foster, N.M.; Breckon, R.D.; Luedke, A.J.; Jones, R.H. Transmission of two strains of epizootic hemorrhagic disease virus in deer by Culicoides variipennis. J. Wild Dis. 1977, 13, 9–16. [Google Scholar] [CrossRef] [PubMed]
- Veronesi, E.; Henstock, M.; Gubbins, S.; Batten, C.; Manley, R.; Barber, J.; Hoffmann, B.; Beer, M.; Attoui, H.; Mertens, P.P.C.; et al. Implicating Culicoides biting midges as vectors of Schmallenberg virus using semi-quantitative RT-PCR. PLoS ONE 2013, 8, e57747. [Google Scholar] [CrossRef] [PubMed]
- Drolet, B.S.; Campbell, C.L.; Stuart, M.A.; Wilson, W.C. Vector competence of Culicoides sonorensis (Diptera: Ceratopogonidae) for vesicular stomatitis virus. J. Med. Entomol. 2005, 42, 409–418. [Google Scholar] [CrossRef] [PubMed]
- Wellby, M.P.; Baylis, M.; Rawlings, P.; Mellor, P.S. Effect of temperature on survival and rate of virogenesis of African horse sickness virus in Culicoides variipennis sonorensis (Diptera: Ceratopogonidae) and its significance in relation to the epidemiology of the disease. Bull. Entomol. Res. 1996, 86, 715–720. [Google Scholar] [CrossRef]
- Franz, A.W.E.; Kantor, A.M.; Passarelli, A.L.; Clem, R.J. Tissue barriers to arbovirus infection in mosquitoes. Viruses 2015, 7, 3741–3767. [Google Scholar] [CrossRef]
- Langner, K.F.A.; Darpel, K.E.; Denison, E.; Drolet, B.S.; Leibold, W.; Mellor, P.S.; Mertens, P.P.C.; Nimtz, M.; Nimtz, G.W.I. Collection and analysis of salivary proteins from the biting midge Culicoides nebeculosus (Diptera: Ceratopogonidae). J. Med. Entomol. 2007, 44, 238–248. [Google Scholar] [CrossRef]
- McGregor, B.L.; Erram, D.; Acevedo, C.; Alto, B.W.; Burkett-Cadena, N.D. Vector competence of Culicoides sonorensis (Diptera: Ceratopogonidae) for epizootic hemorrhagic disease virus serotype 2 strains from Canada and Florida. Viruses 2019, 11, 367. [Google Scholar] [CrossRef]
- Smith, D.R.; Carrara, A.; Aguilar, P.V.; Weaver, S.C. Evaluation of methods to assess transmission potential of Venezuelan equine encephalitis virus by mosquitoes and estimation of mosquito salivary titers. Am. J. Trop. Med. Hyg. 2005, 73, 33–39. [Google Scholar] [CrossRef]
- Kenney, J.L.; Adams, A.P.; Weaver, S.C. Transmission potential of two chimeric western equine encephalitis vaccine candidates in Culex tarsalis. Am. J. Trop. Med. Hyg. 2010, 82, 354–359. [Google Scholar] [CrossRef]
- Roberts, D.R.; Pinheiro, F.P.; Hoch, A.L.; LeDuc, J.W.; Peterson, N.E.; Santos, M.A.V.; Western, K.A. Vectors and Natural Reservoirs of Oropouche Virus in The Amazon Region; Pan American Health Organization: Washington, DC, USA, 1977. [Google Scholar]
- Hoch, A.L.; Pinheiro, F.P.; Roberts, D.R.; Gomes, M.L.C. Laboratory transmission of Oropouche virus by Culex quinquefasciatus. Bull. Pan Am. Health Organ. 1987, 21, 55–61. [Google Scholar]
- Sakkas, H.; Bozidis, P.; Franks, A.; Papadopoulou, C. Oropouche fever: A review. Viruses 2018, 10, 175. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, B.F.; Serra, O.P.; Heinen, L.B.S.; Zuchi, N.; Souza, V.C.; Naveca, F.G.; Santos, M.A.M.; Slhessarenko, R.D. Detection of Oropouche virus segment S in patients and in Culex quinquefasciatus in the state of Mato Grosso, Brazil. Mem. Inst. Oswaldo Cruz 2015, 110, 745–754. [Google Scholar] [CrossRef] [PubMed]
- David, M.R.; Ribeiro, G.S.; de Freitas, R.M. Bionomics of Culex quinquefasciatus within urban areas of Rio de Janeiro, Southeastern Brazil. Rev. Saúde Pública 2012, 46, 858–865. [Google Scholar] [CrossRef] [PubMed]
- Kramer, L.D.; Ciota, A.T. Dissecting vectorial capacity for mosquito-borne viruses. Curr. Opin. Virol. 2015, 15, 112–118. [Google Scholar] [CrossRef]
- Weaver, S.C.; Scott, T.W.; Lorenz, L.H.; Lerdthusnee, K.; Romoser, W.S. Togavirus-associated pathologic changes in the midgut of a natural mosquito vector. J. Virol. 1988, 62, 2083–2090. [Google Scholar] [CrossRef]
- Pinheiro, F.P.; Travassos Da Rosa, A.P.A.; Gomes, M.L.C.; LeDuc, J.W.; Hoch, A.L. Transmission of Oropouche virus from man to hamster by the midge Culicoides paraensis. Science 1982, 215, 1251–1253. [Google Scholar] [CrossRef]
- Anderson, C.R.; Spence, L.; Downs, W.G.; Aitken, T.H.G. Oropouche Virus: A new human disease agent from Trinidad, West Indies. Am. J. Trop. Med. Hyg. 1961, 10, 574–578. [Google Scholar] [CrossRef]
- Molaei, G.; Andreadis, T.G.; Armstrong, P.M.; Anderson, J.F.; Vossbrinck, C.R. Host feeding patterns of Culex mosquitoes and West Nile virus transmission, Northeastern United States. Emerg. Infect. Dis. 2006, 12, 468–474. [Google Scholar] [CrossRef]
- Molaei, G.; Andreadis, T.G. Identification of avian- and mammalian-derived bloodmeals in Aedes vexans and Culiseta melanura (Diptera: Culicidae) and its implication for West Nile virus transmission in Connecticut, U.S.A. J. Med. Entomol. 2006, 43, 1088–1093. [Google Scholar] [CrossRef]
- Edman, J.D. Host-feeding patterns of Florida mosquitoes I. Aedes, Anopheles, Coquillettidia, Mansonia, and Psorophora. J. Med. Entomol. 1971, 8, 687–695. [Google Scholar] [CrossRef]
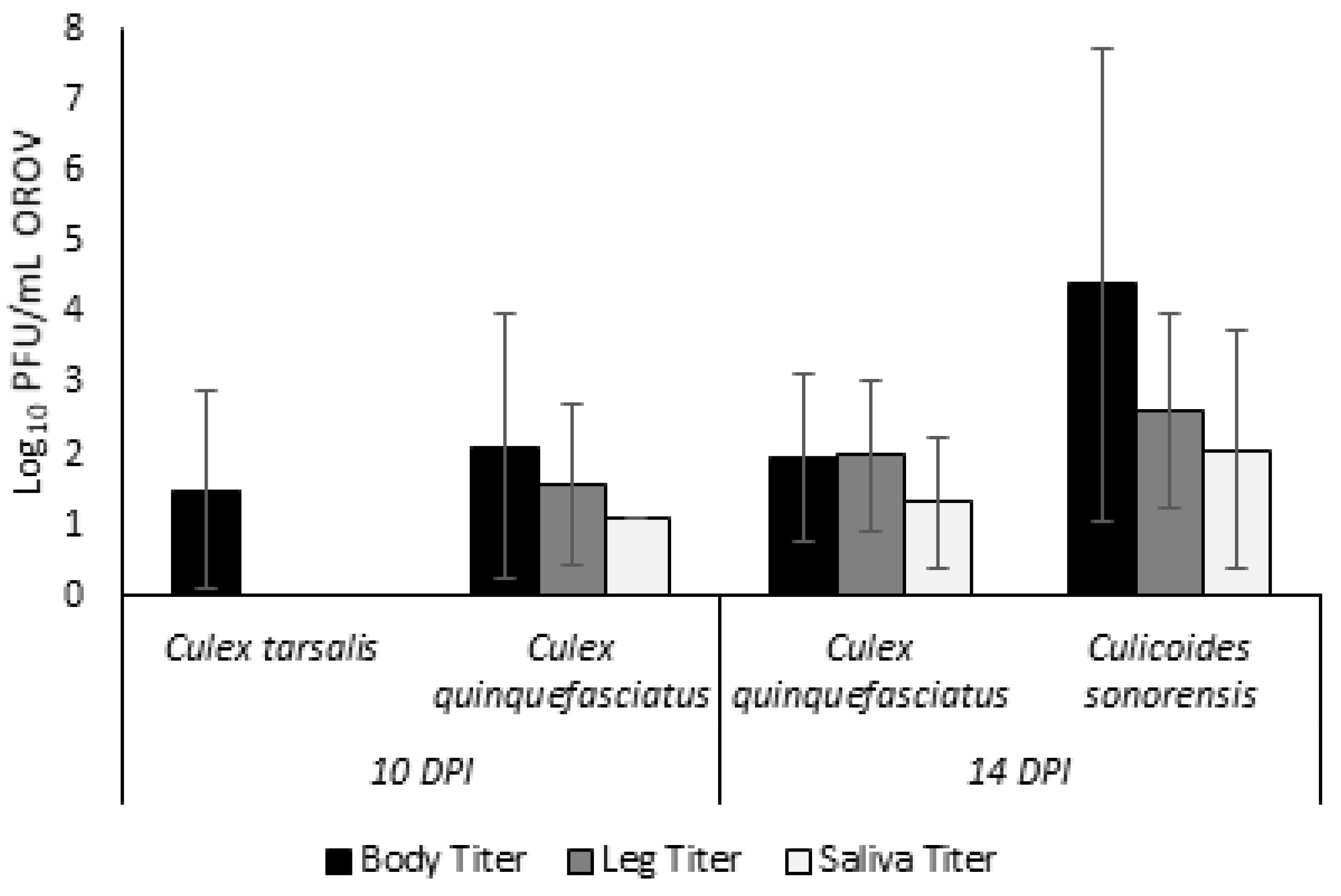
| DPI | Species | N | Infection | Dissemination | Transmission |
|---|---|---|---|---|---|
| 10 | Culex tarsalis | 96 | 3 (3.13) | 0 (0) | 0 (0) |
| Culex quinquefasciatus | 103 | 10 (9.71) | 3 (2.91) | 1 (0.97) | |
| 14 | Culex quinquefasciatus | 244 | 47 (19.3) | 3 (1.23) | 2 (0.82) |
| Culicoides sonorensis | 172 | 149 (86.63) | 143 (83.14) | 34 (19.77) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
McGregor, B.L.; Connelly, C.R.; Kenney, J.L. Infection, Dissemination, and Transmission Potential of North American Culex quinquefasciatus, Culex tarsalis, and Culicoides sonorensis for Oropouche Virus. Viruses 2021, 13, 226. https://doi.org/10.3390/v13020226
McGregor BL, Connelly CR, Kenney JL. Infection, Dissemination, and Transmission Potential of North American Culex quinquefasciatus, Culex tarsalis, and Culicoides sonorensis for Oropouche Virus. Viruses. 2021; 13(2):226. https://doi.org/10.3390/v13020226
Chicago/Turabian StyleMcGregor, Bethany L., C. Roxanne Connelly, and Joan L. Kenney. 2021. "Infection, Dissemination, and Transmission Potential of North American Culex quinquefasciatus, Culex tarsalis, and Culicoides sonorensis for Oropouche Virus" Viruses 13, no. 2: 226. https://doi.org/10.3390/v13020226
APA StyleMcGregor, B. L., Connelly, C. R., & Kenney, J. L. (2021). Infection, Dissemination, and Transmission Potential of North American Culex quinquefasciatus, Culex tarsalis, and Culicoides sonorensis for Oropouche Virus. Viruses, 13(2), 226. https://doi.org/10.3390/v13020226







