On-Demand Patient-Specific Phenotype-to-Genotype Ebola Virus Characterization
Abstract
:1. Introduction
2. Materials and Methods
2.1. Cell Culture
2.2. Viruses
2.3. Recombinant EBOV Templates
2.4. Synthesis of the EBOV Genome-Encoding Plasmids and Helper Plasmids
2.4.1. Genome Plasmids
2.4.2. Helper Plasmids
2.4.3. Plasmid Sequencing
2.5. EBOV/Mak-G3864.1 Minigenome
2.6. Recombinant EBOV Rescue
2.7. Small Molecules
2.8. EBOV Assay in HeLa Cells
2.9. Immunostaining
2.10. Image and Data Analysis
2.11. Sequencing Data Analysis
2.12. Laboratory Mouse Experiments
3. Results
3.1. Recombinant EBOV Rescue
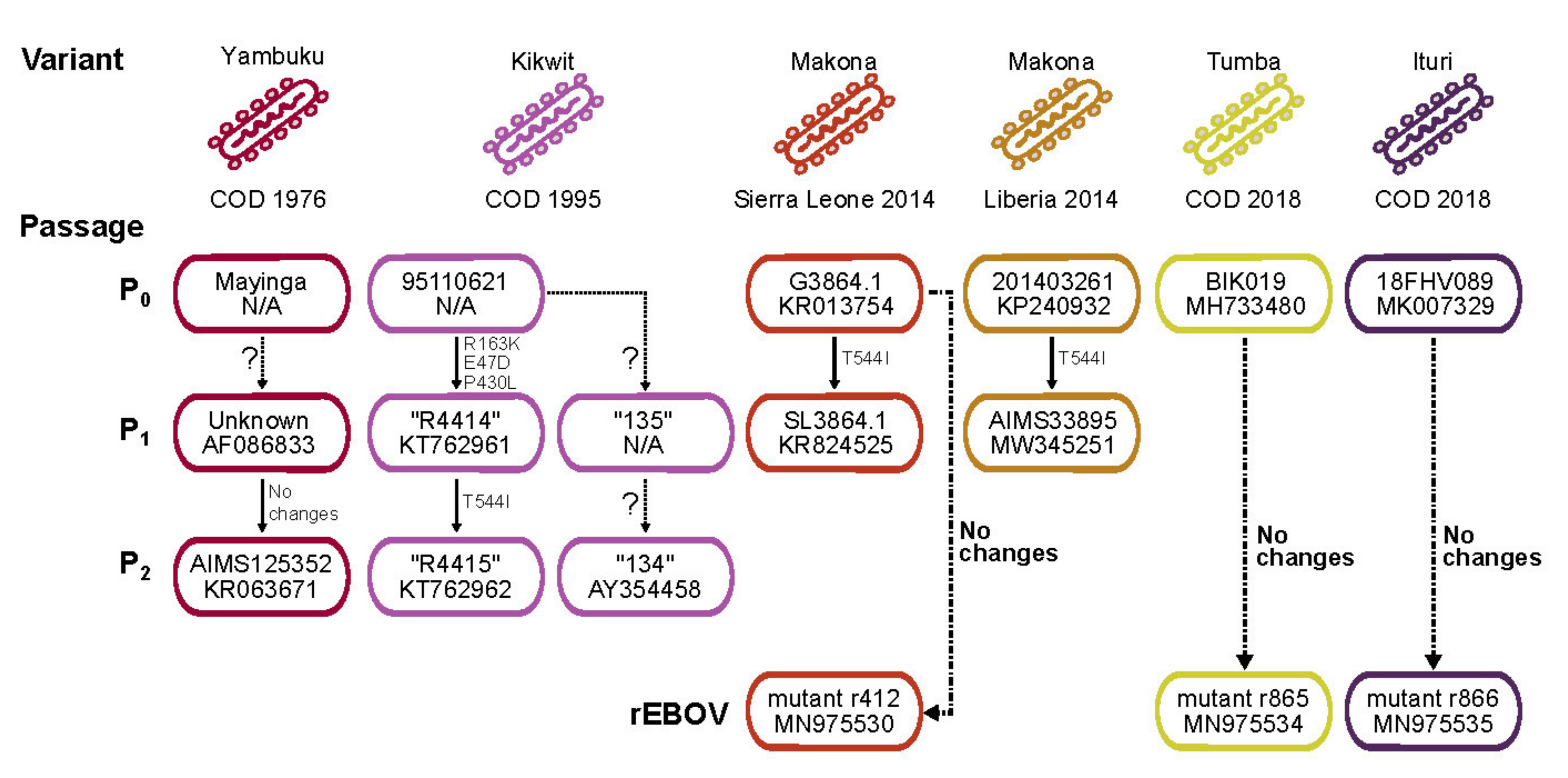
3.1.1. Selection of EBOV Isolate Sequences for De Novo Genome Synthesis and Rescue
3.1.2. Plasmid Establishment and Sequence Verification
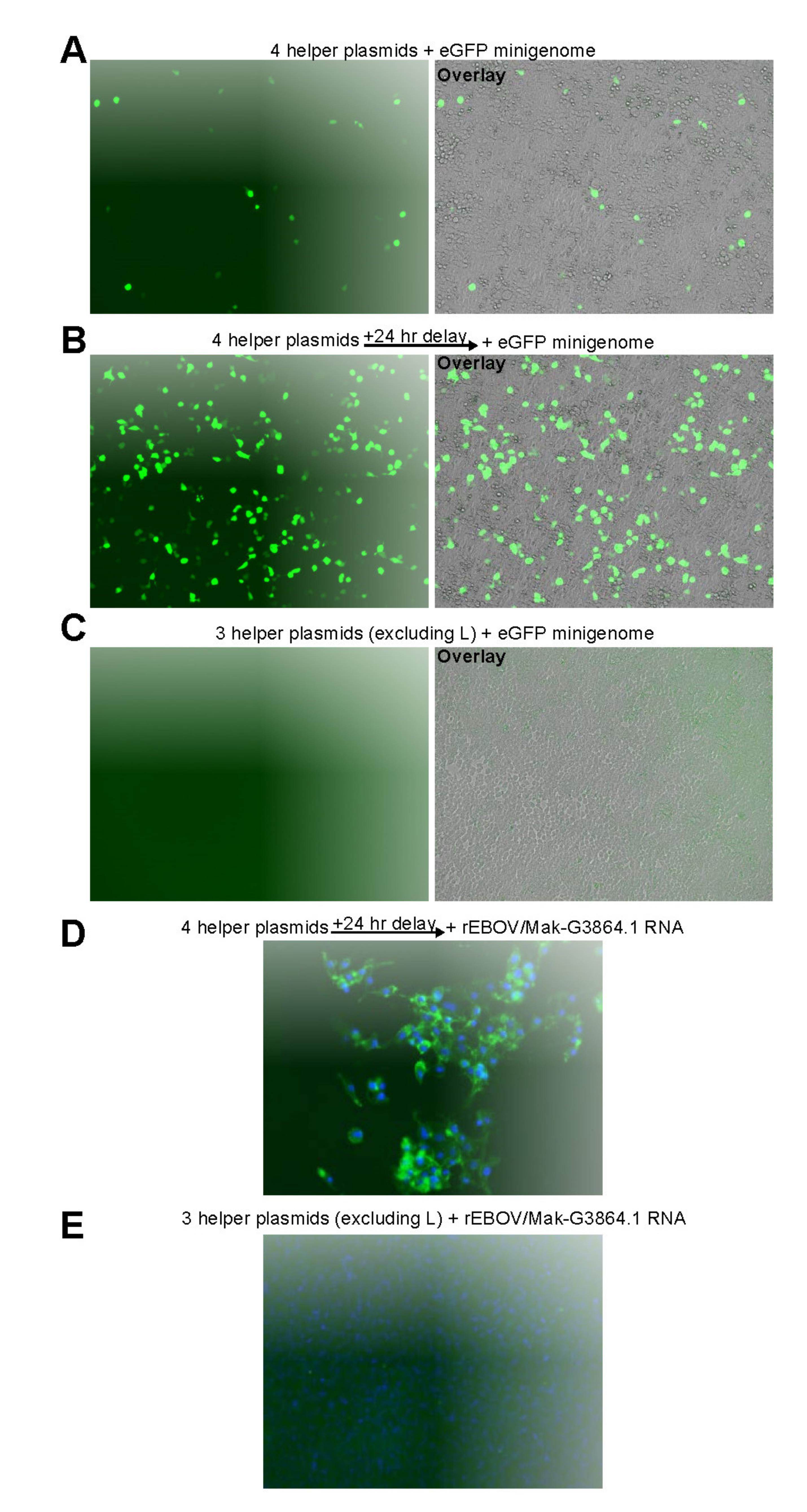
3.2. EBOV Rescue
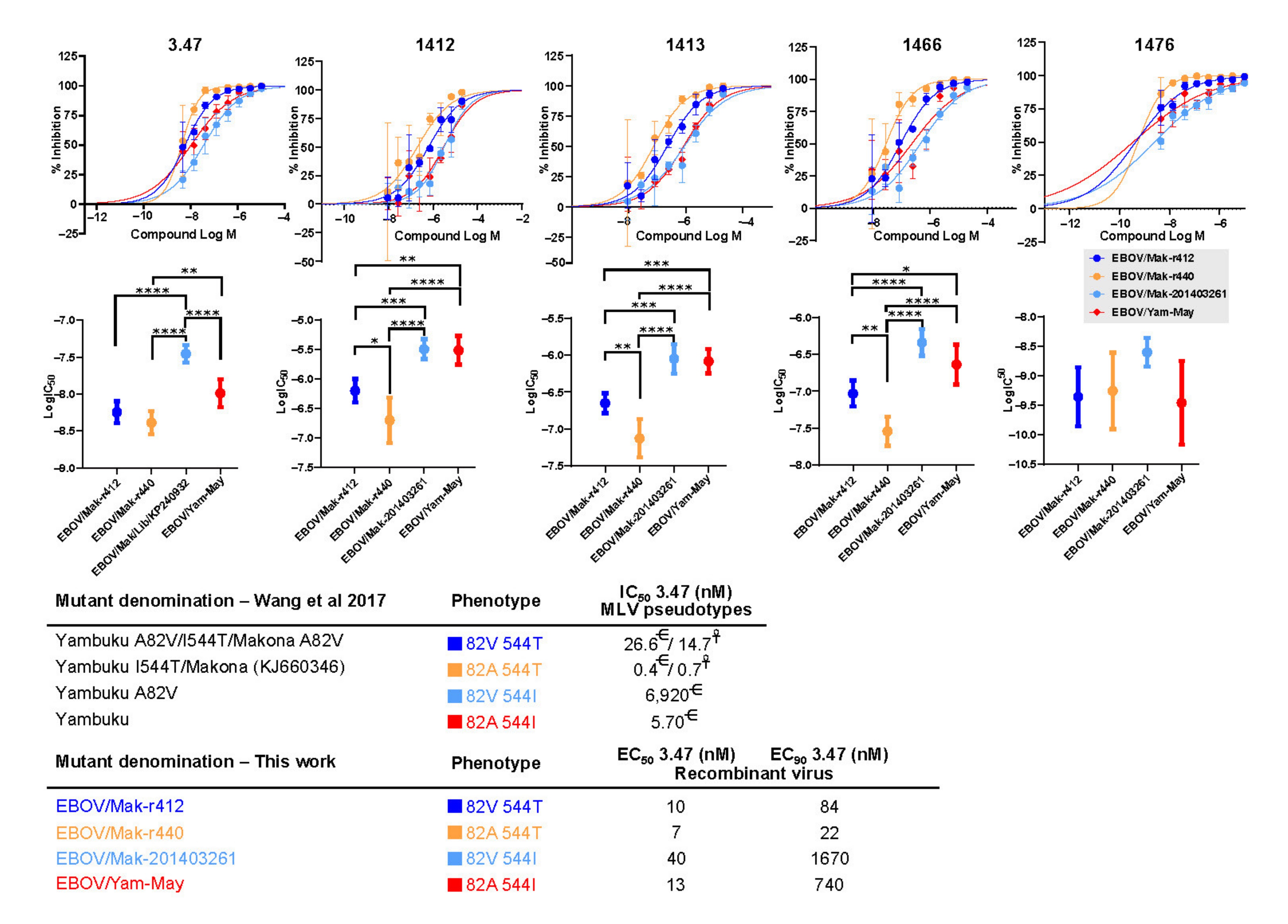
3.2.1. Cell Culture Adaptations Can Alter Susceptibility to MCMs
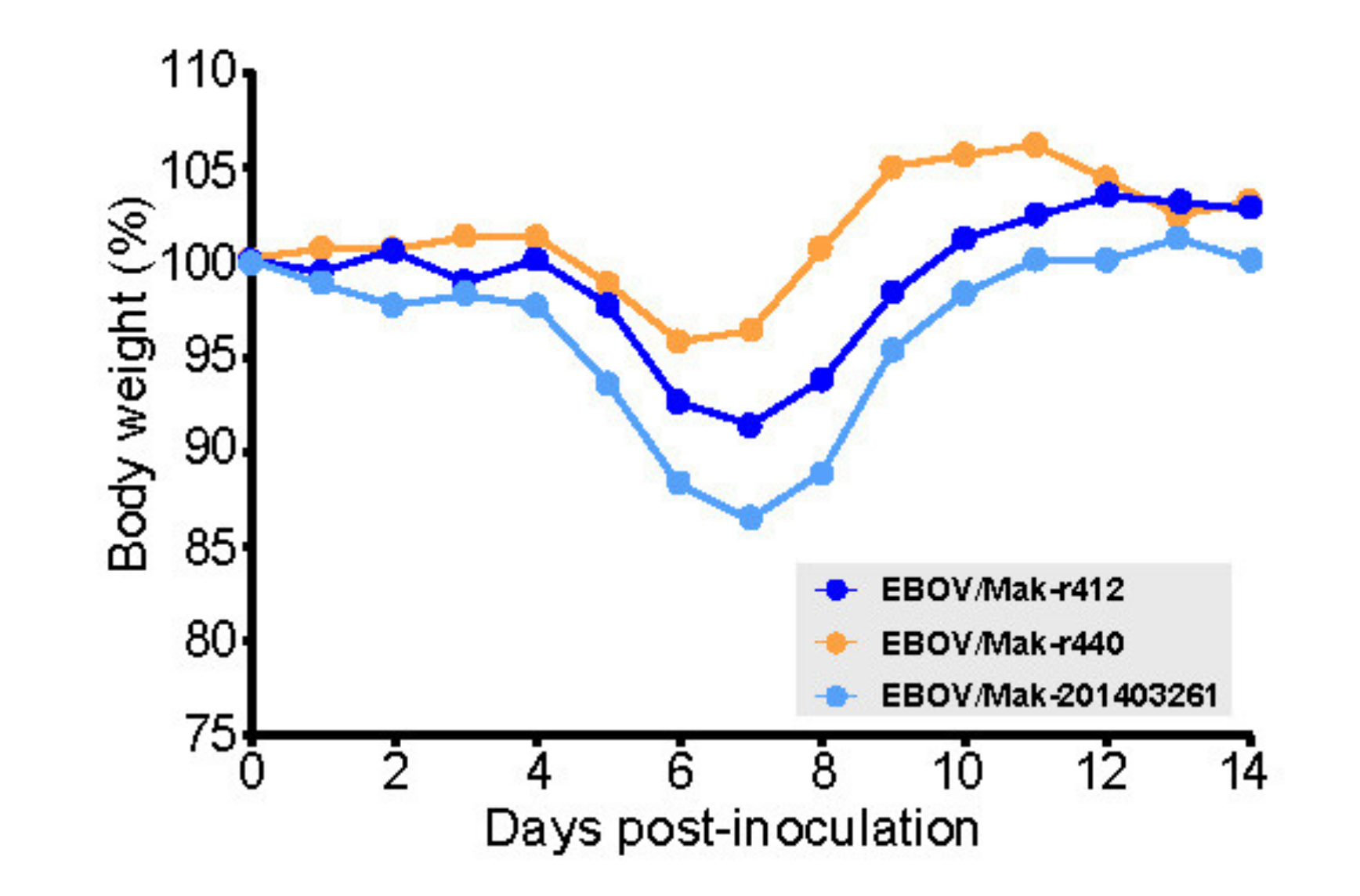
3.2.2. Recombinant EBOV/Mak-G3864.1 Mutants Cause Weight Loss in Interferon-Alpha/Beta Receptor Knockout (INFAR−/−) Laboratory Mice
4. Discussion
5. Conclusions
Disclaimer
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Ebola haemorrhagic fever in Zaire, 1976. Report of an International Commission. Bull. World Health Organ. 1978, 56, 271–293. [Google Scholar]
- Bowen, E.T.W.; Lloyd, G.; Harris, W.J.; Platt, G.S.; Baskerville, A.; Vella, E.E. Viral hæmorrhagic fever in southern Sudan and northern Zaire. Preliminary studies on the aetiological agent. Lancet 1977, 309/i, 571–573. [Google Scholar] [CrossRef]
- Johnson, K.M.; Lange, J.V.; Webb, P.A.; Murphy, F.A. Isolation and partial characterisation of a new virus causing acute hæmorrhagic fever in Zaire. Lancet 1977, 309/i, 569–571. [Google Scholar] [CrossRef]
- Pattyn, S.; van der Groen, G.; Jacob, W.; Piot, P.; Courteille, G. Isolation of Marburg-like virus from a case of hæmorrhagic fever in Zaire. Lancet 1977, 309/i, 573–574. [Google Scholar] [CrossRef]
- World Health Organization. Ebola haemorrhagic fever in Sudan, 1976. Report of a WHO/International Study Team. Bull. World Health Organ. 1978, 56, 247–270. [Google Scholar]
- Kuhn, J.H.; Amarasinghe, G.K.; Perry, D.L. Filoviridae. In Fields Virology, 7th ed.; Howley, P.M., Knipe, D.M., Whelan, S.P.J., Eds.; Wolters Kluwer/Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2020; Volume 1, pp. 449–503. [Google Scholar]
- Bullard, S.G. A Day-by-Day Chronicle of the 2013–2016 Ebola Outbreak; Springer: Cham, Switzerland, 2018. [Google Scholar]
- Mbala-Kingebeni, P.; Pratt, C.B.; Wiley, M.R.; Diagne, M.M.; Makiala-Mandanda, S.; Aziza, A.; Di Paola, N.; Chitty, J.A.; Diop, M.; Ayouba, A.; et al. 2018 Ebola virus disease outbreak in Equateur Province, Democratic Republic of the Congo: A retrospective genomic characterisation. Lancet Infect. Dis. 2019, 19, 641–647. [Google Scholar] [CrossRef] [Green Version]
- Maganga, G.D.; Kapetshi, J.; Berthet, N.; Kebela Ilunga, B.; Kabange, F.; Mbala Kingebeni, P.; Mondonge, V.; Muyembe, J.-J.; Bertherat, E.; Briand, S.; et al. Ebola virus disease in the Democratic Republic of Congo. N. Engl. J. Med. 2014, 371, 2083–2091. [Google Scholar] [CrossRef]
- Nsio, J.; Kapetshi, J.; Makiala, S.; Raymond, F.; Tshapenda, G.; Boucher, N.; Corbeil, J.; Okitandjate, A.; Mbuyi, G.; Kiyele, M.; et al. 2017 outbreak of Ebola virus disease in northern Democratic Republic of Congo. J. Infect. Dis. 2020, 221, 701–706. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mbala-Kingebeni, P.; Aziza, A.; di Paola, N.; Wiley, M.R.; Makiala-Mandanda, S.; Caviness, K.; Pratt, C.B.; Ladner, J.T.; Kugelman, J.R.; Prieto, K.; et al. Medical countermeasures during the 2018 Ebola virus disease outbreak in the North Kivu and Ituri Provinces of the Democratic Republic of the Congo: A rapid genomic assessment. Lancet Infect. Dis. 2019, 19, 648–657. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Ebola in the Democratic Republic of the Congo. Health Emergency Update. 2020. Available online: https://www.who.int/emergencies/situations/Ebola-2019-drc- (accessed on 20 September 2021).
- World Health Organization. End of the 11th Ebola Outbreak. Democratic Republic of the Congo. 2020. Available online: https://www.afro.who.int/health-topics/ebola-virus-disease/end-ebola-11-drc (accessed on 20 September 2021).
- Bell, A.; Lewandowski, K.; Myers, R.; Wooldridge, D.; Aarons, E.; Simpson, A.; Vipond, R.; Jacobs, M.; Gharbia, S.; Zambon, M. Genome sequence analysis of Ebola virus in clinical samples from three British healthcare workers, August 2014 to March 2015. Eurosurveillance 2015, 20, 21131. [Google Scholar] [CrossRef]
- Diallo, B.; Sissoko, D.; Loman, N.J.; Bah, H.A.; Bah, H.; Worrell, M.C.; Conde, L.S.; Sacko, R.; Mesfin, S.; Loua, A.; et al. Resurgence of Ebola virus disease in Guinea linked to a survivor with virus persistence in seminal fluid for more than 500 Days. Clin. Infect. Dis. 2016, 63, 1353–1356. [Google Scholar] [CrossRef]
- EVIDENT Consortium. EBOV Sequences. 2017. Available online: http://evident-project.eu/newsevents/ebov-sequences/ (accessed on 20 September 2021).
- Gire, S.K.; Goba, A.; Andersen, K.G.; Sealfon, R.S.; Park, D.J.; Kanneh, L.; Jalloh, S.; Momoh, M.; Fullah, M.; Dudas, G.; et al. Genomic surveillance elucidates Ebola virus origin and transmission during the 2014 outbreak. Science 2014, 345, 1369–1372. [Google Scholar] [CrossRef] [Green Version]
- Goodfellow, I.; Arias, A.; Caddy, S.; Thorne, L.; Kargbo, B.; Kamara, B.O.; Jah, U.; Cooper, D.; Newport, M.; Horby, P.; et al. Recent Evolution Patterns of Ebola Virus from December 2014–June 2015 Obtained by Direct Sequencing in Sierra Leone. 2015. Available online: http://virological.org/t/recent-evolution-patterns-of-ebola-virus-obtained-by-direct-sequencing-in-sierra-leone/35 (accessed on 20 September 2021).
- Hoenen, T.; Safronetz, D.; Groseth, A.; Wollenberg, K.R.; Koita, O.A.; Diarra, B.; Fall, I.S.; Haidara, F.C.; Diallo, F.; Sanogo, M.; et al. Mutation rate and genotype variation of Ebola virus from Mali case sequences. Science 2015, 348, 117–119. [Google Scholar] [CrossRef]
- Institut Pasteur. EBOV Sequences from Guinea. 2015. Available online: https://www.pasteur.fr/en/ebov-sequences-guinea (accessed on 20 September 2021).
- Kugelman, J.R.; Wiley, M.R.; Mate, S.; Ladner, J.T.; Beitzel, B.; Fakoli, L.; Taweh, F.; Prieto, K.; Diclaro, J.W.; Minogue, T.; et al. Monitoring of Ebola virus Makona evolution through establishment of advanced genomic capability in Liberia. Emerg. Infect. Dis. 2015, 21, 1135–1143. [Google Scholar] [CrossRef] [PubMed]
- Park, D.J.; Dudas, G.; Wohl, S.; Goba, A.; Whitmer, S.L.M.; Andersen, K.G.; Sealfon, R.S.; Ladner, J.T.; Kugelman, J.R.; Matranga, C.B.; et al. Ebola virus epidemiology, transmission, and evolution during seven months in Sierra Leone. Cell 2015, 161, 1516–1526. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Quick, J.; Loman, N.J.; Duraffour, S.; Simpson, J.T.; Severi, E.; Cowley, L.; Bore, J.A.; Koundouno, R.; Dudas, G.; Mikhail, A.; et al. Real-time, portable genome sequencing for Ebola surveillance. Nature 2016, 530, 228–232. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tong, Y.-G.; Shi, W.-F.; Liu, D.; Qian, J.; Liang, L.; Bo, X.-C.; Liu, J.; Ren, H.-G.; Fan, H.; Ni, M.; et al. China Mobile Laboratory Testing Team in Sierra Leone, Genetic diversity and evolutionary dynamics of Ebola virus in Sierra Leone. Nature 2015, 524, 93–96. [Google Scholar] [CrossRef]
- Virus Pathogen Resource, Filoviridae. 2017. Available online: https://www.viprbrc.org/brc/vipr_genome_search.spg?method=SubmitForm&blockId=2718&decorator=filo (accessed on 20 September 2021).
- Diehl, W.E.; Lin, A.E.; Grubaugh, N.D.; Carvalho, L.M.; Kim, K.; Kyawe, P.P.; McCauley, S.M.; Donnard, E.; Kucukural, A.; McDonel, P.; et al. Ebola virus glycoprotein with increased infectivity dominated the 2013-2016 epidemic. Cell 2016, 167, 1088–1098.e6. [Google Scholar] [CrossRef] [Green Version]
- Urbanowicz, R.A.; McClure, C.P.; Sakuntabhai, A.; Sall, A.A.; Kobinger, G.; Müller, M.A.; Holmes, E.C.; Rey, F.A.; Simon-Loriere, E.; Ball, J.K. Human adaptation of Ebola virus during the West African outbreak. Cell 2016, 167, 1079–1087.e5. [Google Scholar] [CrossRef] [Green Version]
- Ueda, M.T.; Kurosaki, Y.; Izumi, T.; Nakano, Y.; Oloniniyi, O.K.; Yasuda, J.; Koyanagi, Y.; Sato, K.; Nakagawa, S. Functional mutations in spike glycoprotein of Zaire ebolavirus associated with an increase in infection efficiency. Genes Cells 2017, 22, 148–159. [Google Scholar] [CrossRef] [Green Version]
- Kugelman, J.R.; Lee, M.S.; Rossi, C.A.; McCarthy, S.E.; Radoshitzky, S.R.; Dye, J.M.; Hensley, L.E.; Honko, A.; Kuhn, J.H.; Jahrling, P.B.; et al. Ebola virus genome plasticity as a marker of its passaging history: A comparison of in vitro passaging to non-human primate infection. PLoS ONE 2012, 7, e50316. [Google Scholar] [CrossRef] [PubMed]
- Ruedas, J.B.; Ladner, J.T.; Ettinger, C.R.; Gummuluru, S.; Palacios, G.; Connor, J.H. Spontaneous mutation at amino acid 544 of the Ebola virus glycoprotein potentiates virus entry and selection in tissue culture. J. Virol. 2017, 91, e00392-17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Volchkova, V.A.; Dolnik, O.; Martinez, M.J.; Reynard, O.; Volchkov, V.E. Genomic RNA editing and its impact on Ebola virus adaptation during serial passages in cell culture and infection of guinea pigs. J. Infect. Dis 2011, 204 (Suppl. S3), S941–S946. [Google Scholar] [CrossRef]
- Trefry, J.C.; Wollen, S.E.; Nasar, F.; Shamblin, J.D.; Kern, S.J.; Bearss, J.J.; Jefferson, M.A.; Chance, T.B.; Kugelman, J.R.; Ladner, J.T.; et al. Ebola virus infections in nonhuman primates are temporally influenced by glycoprotein poly-U editing site populations in the exposure material. Viruses 2015, 7, 6739–6754. [Google Scholar] [CrossRef]
- Alfson, K.J.; Avena, L.E.; Beadles, M.W.; Worwa, G.; Amen, M.; Patterson, J.L.; Carrion, R., Jr.; Griffiths, A. Intramuscular exposure of Macaca fascicularis to low doses of low passage- or cell culture-adapted Sudan virus or Ebola virus. Viruses 2018, 10, 642. [Google Scholar] [CrossRef] [Green Version]
- Volchkov, V.E.; Volchkova, V.A.; Mühlberger, E.; Kolesnikova, L.V.; Weik, M.; Dolnik, O.; Klenk, H.-D. Recovery of infectious Ebola virus from complementary DNA: RNA editing of the GP gene and viral cytotoxicity. Science 2001, 291, 1965–1969. [Google Scholar] [CrossRef]
- Neumann, G.; Feldmann, H.; Watanabe, S.; Lukashevich, I.; Kawaoka, Y. Reverse genetics demonstrates that proteolytic processing of the Ebola virus glycoprotein is not essential for replication in cell culture. J. Virol. 2002, 76, 406–410. [Google Scholar] [CrossRef] [Green Version]
- Mühlberger, E.; Weik, M.; Volchov, V.E.; Klenk, H.-D.; Becker, S. Comparison of the transcription and replication strategies of marburg virus and Ebola virus by using artificial replication systems. J. Virol. 1999, 73, 2333–2342. [Google Scholar] [CrossRef] [Green Version]
- Hoenen, T.; Brandt, J.; Caì, Y.; Kuhn, J.H.; Finch, C. Reverse genetics of filoviruses. Curr. Top. Microbiol. Immunol. 2017, 411, 421–445. [Google Scholar] [PubMed]
- McMullan, L.K.; Flint, M.; Chakrabarti, A.; Guerrero, L.; Lo, M.K.; Porter, D.; Nichol, S.T.; Spiropoulou, C.F.; Albariño, C. Characterisation of infectious Ebola virus from the ongoing outbreak to guide response activities in the Democratic Republic of the Congo: A phylogenetic and in vitro analysis. Lancet Infect. Dis. 2019, 19, 1023–1032. [Google Scholar] [CrossRef] [Green Version]
- Ladner, J.T.; Wiley, M.R.; Mate, S.; Dudas, G.; Prieto, K.; Lovett, S.; Nagle, E.R.; Beitzel, B.; Gilbert, M.L.; Fakoli, L.; et al. Evolution and spread of Ebola virus in Liberia, 2014–2015. Cell Host Microbe 2015, 18, 659–669. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ladner, J.T.; Beitzel, B.; Chain, P.S.G.; Davenport, M.G.; Donaldson, E.F.; Frieman, M.; Kugelman, J.R.; Kuhn, J.H.; O’Rear, J.; Sabeti, P.C.; et al. Standards for sequencing viral genomes in the era of high-throughput sequencing. MBio 2014, 5, e01360-14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blackley, D.J.; Wiley, M.R.; Ladner, J.T.; Fallah, M.; Lo, T.; Gilbert, M.L.; Gregory, C.; D’ambrozio, J.; Coulter, S.; Mate, S.; et al. Reduced evolutionary rate in reemerged Ebola virus transmission chains. Sci. Adv. 2016, 2, e1600378. [Google Scholar] [CrossRef] [Green Version]
- Ni, M.; Chen, C.; Qian, J.; Xiao, H.-X.; Shi, W.-F.; Luo, Y.; Wang, H.-Y.; Li, Z.; Wu, J.; Xu, P.-S.; et al. Intra-host dynamics of Ebola virus during 2014. Nat. Microbiol. 2016, 1, 16151. [Google Scholar] [CrossRef]
- Dietzel, E.; Schudt, G.; Krähling, V.; Matrosovich, M.; Becker, S. Functional characterization of adaptive mutations during the West African Ebola virus outbreak. J. Virol. 2017, 91, e01913-16. [Google Scholar] [CrossRef] [Green Version]
- Hoffmann, M.; Crone, L.; Dietzel, E.; Paijo, J.; González-Hernández, M.; Nehlmeier, I.; Kalinke, U.; Becker, S.; Pöhlmann, S. A polymorphism within the internal fusion loop of the Ebola virus glycoprotein modulates host cell entry. J. Virol. 2017, 91, e00177-17. [Google Scholar] [CrossRef] [Green Version]
- Kurosaki, Y.; Ueda, M.T.; Nakano, Y.; Yasuda, J.; Koyanagi, Y.; Sato, K.; Nakagawa, S. Different effects of two mutations on the infectivity of Ebola virus glycoprotein in nine mammalian species. J. Gen. Virol. 2018, 99, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.K.; Lim, S.-Y.; Lee, S.M.; Cunningham, J.M. Biochemical basis for increased activity of Ebola glycoprotein in the 2013-16 epidemic. Cell Host Microbe 2017, 21, 367–375. [Google Scholar] [CrossRef] [Green Version]
- Marzi, A.; Chadinah, S.; Haddock, E.; Feldmann, F.; Arndt, N.; Martellaro, C.; Scott, D.P.; Hanley, P.W.; Nyenswah, T.G.; Sow, S.; et al. Recently identified mutations in the Ebola virus-Makona genome do not alter pathogenicity in animal models. Cell Rep. 2018, 23, 1806–1816. [Google Scholar] [CrossRef] [Green Version]
- Kinganda Lusamaki, E.; Pratt, C. Genomic Epidemiology of the 2018-20 Ebola Epidemic. 2021. Available online: https://nextstrain.org/community/inrb-drc/ebola-nord-kivu (accessed on 20 September 2021).
- Schmaljohn, C.; VanderZanden, L.; Bray, M.; Custer, D.; Meyer, B.; Li, D.; Rossi, C.; Fuller, D.; Fuller, J.; Haynes, J.; et al. Naked DNA vaccines expressing the prM and E genes of Russian spring summer encephalitis virus and Central European encephalitis virus protect mice from homologous and heterologous challenge. J. Virol. 1997, 71, 9563–9569. [Google Scholar] [CrossRef] [Green Version]
- Côté, M.; Misasi, J.; Ren, T.; Bruchez, A.; Lee, K.; Filone, C.M.; Hensley, L.; Li, Q.; Ory, D.; Chandran, K.; et al. Small molecule inhibitors reveal Niemann-Pick C1 is essential for Ebola virus infection. Nature 2011, 477, 344–348. [Google Scholar] [CrossRef]
- Liu, H.; Tian, Y.; Lee, K.; Krishnan, P.; Wang, M.K.-M.; Whelan, S.; Mevers, E.; Soloveva, V.; Dedic, B.; Liu, X.; et al. Identification of potent Ebola virus entry inhibitors with suitable properties for in vivo studies. J. Med. Chem. 2018, 61, 6293–6307. [Google Scholar] [CrossRef]
- Pessi, A.; Bixler, S.L.; Soloveva, V.; Radoshitzky, S.; Retterer, C.; Kenny, T.; Zamani, R.; Gomba, G.; Gharabeih, D.; Wells, J.; et al. Cholesterol-conjugated stapled peptides inhibit Ebola and Marburg viruses in vitro and in vivo. Antiviral Res. 2019, 171, 104592. [Google Scholar] [CrossRef] [PubMed]
- Kugelman, J.R.; Wiley, M.R.; Nagle, E.R.; Reyes, D.; Pfeffer, B.P.; Kuhn, J.H.; Sanchez-Lockhart, M.; Palacios, G.F. Error baseline rates of five sample preparation methods used to characterize RNA virus populations. PLoS ONE 2017, 12, e0171333. [Google Scholar] [CrossRef]
- Ruedas, J.B.; Arnold, C.E.; Palacios, G.; Connor, J.H. Growth-adaptive mutations in the Ebola virus Makona glycoprotein alter different steps in the virus entry pathway. J. Virol 2018, 92, e00820-18. [Google Scholar] [CrossRef] [Green Version]
- Bray, M.; Davis, K.; Geisbert, T.; Schmaljohn, C.; Huggins, J. A mouse model for evaluation of prophylaxis and therapy of Ebola hemorrhagic fever. J. Infect. Dis. 1998, 178, 651–661. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brannan, J.M.; Froude, J.W.; Prugar, L.I.; Bakken, R.R.; Zak, S.E.; Daye, S.P.; Wilhelmsen, C.E.; Dye, J.M. Interferon α/β receptor-deficient mice as a model for Ebola virus disease. J. Infect. Dis. 2015, 212 (Suppl. S2), S282–S294. [Google Scholar] [CrossRef] [PubMed]
- Albariño, C.G.; Guerrero, L.W.; Chakrabarti, A.K.; Kainulainen, M.H.; Whitmer, S.L.M.; Welch, S.R.; Nichol, S.T. Virus fitness differences observed between two naturally occurring isolates of Ebola virus Makona variant using a reverse genetics approach. Virology 2016, 496, 237–243. [Google Scholar] [CrossRef]
- Tsuda, Y.; Hoenen, T.; Banadyga, L.; Weisend, C.; Ricklefs, S.M.; Porcella, S.F.; Ebihara, H. An improved reverse genetics system to overcome cell-type-dependent Ebola virus genome plasticity. J. Infect. Dis. 2015, 212 (Suppl. S2), S129–S137. [Google Scholar] [CrossRef] [Green Version]
- Lin, A.E.; Diehl, W.E.; Cai, Y.; Finch, C.L.; Akusobi, C.; Kirchdoerfer, R.N.; Bollinger, L.; Schaffner, S.F.; Brown, E.A.; Saphire, E.O.; et al. Reporter assays for Ebola virus nucleoprotein oligomerization, virion-like particle budding, and minigenome activity reveal the importance of nucleoprotein amino acid position 111. Viruses 2020, 12, 105. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fels, J.M.; Spence, J.S.; Bortz, R.H., III.; Bornholdt, Z.A.; Chandran, K. A hyperstabilizing mutation in the base of the Ebola virus glycoprotein acts at multiple steps to abrogate viral entry. MBio 2019, 10, e01408-19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Misasi, J.; Gilman, M.S.; Kanekiyo, M.; Gui, M.; Cagigi, A.; Mulangu, S.; Corti, D.; Ledgerwood, J.E.; Lanzavecchia, A.; Cunningham, J.; et al. Structural and molecular basis for Ebola virus neutralization by protective human antibodies. Science 2016, 351, 1343–1346. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smither, S.J.; Eastaugh, L.; Ngugi, S.; O’Brien, L.; Phelps, A.; Steward, J.; Lever, M.S. Ebola virus Makona shows reduced lethality in an immune-deficient mouse model. J. Infect. Dis. 2016, 214 (Suppl. S3), S268–S274. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Designation for This Study | Genotype Compared to EBOV/ Mak-G3864.1 Sequence 412 | Characteristics | GenBank Accession Number |
|---|---|---|---|
| rEBOV/Mak-G3864.1 mutant r412 (parental) | C3579A (VP35 gene, silent) | MN975530 | |
| rEBOV/Mak-G3864.1 mutant r414 | C1498T (NP gene, silent) | Detected during a flare-up of seven EVD cases that occurred in June and July of 2015 in Liberia [41]. The genome sequence of this virus indicated a markedly reduced rate of genome evolution compared to previously circulating viruses. | MN975531 |
| G9355A (nonsense, truncation of last 7 amino acids of VP30) | |||
| A10130G (VP24 gene UTR) | |||
| rEBOV/Mak-G3864.1 mutant r424 | T3008C (NP gene UTR) | The double NP mutation was first identified in viruses from September 2014 and affects expression of NP in an EBOV minigenome assay [42]. | MN975532 |
| T3011C (NP gene UTR) | |||
| C3579A (VP35 gene, silent) | |||
| rEBOV/Mak-G3864.1 mutant r440 | C6283T (GP1,2, V82A) | EBOV/Mak genome sequences obtained at the very beginning of the 2013–2016 EVD were all of the 82A genotype, but the 82V genotype quickly emerged and >90% of all of the sequenced EBOV genomes from the outbreak are of the 82V genotype [39]. The A82V change enhances EBOV infection in nonhuman primate cells [26,27,28,43,44,45,46], but it does not appear to alter virulence in an interferon alpha receptor knock-out (IFNAR−/−) laboratory mouse model and a rhesus monkey (Macaca mulatta) model of EVD [47]. | MN975533 |
| C3579A (VP35 gene, silent) | |||
| rEBOV/Itu mutant r865 | N/A | MN975534 | |
| rEBOV/Tum mutant r866 | N/A | MN975535 |
| Sample | Variants >5% | % 8U |
|---|---|---|
| HeLa 1 | G7692A (31.5%): GP1,2 D552N | 0.8 |
| HeLa 2 | T331C (26%) in NP UTR | 1.8 |
| ins11514A (38.9%) in VP24/L UTR | ||
| Huh7D-12/T7 | none | 1.1 |
| Vero E6 (1) | none | 0.9 |
| Vero E6 (2) | A670G (25.8%): NP Q67R | 9.1 |
| C16881T (7.9%): L T1767I | ||
| Huh7 plus T7 * | none | 1.2 |
| Huh7D-12/T7 plus T7 * | none | 1.4 |
| VeroE6 plus T7 * | A4943T (100%): VP40 Q155L | 2.4 |
| A9124C (68.1%): VP30 E205D |
| Virus | Phenotype | Compound ID | EC50 (μM) | SD | EC90 | CC50 (μM) | SI |
|---|---|---|---|---|---|---|---|
| EBOV/Mak-r440 | 82A 544T | 3.47 | 0.007 | 0.0004 | 0.02 | >10 | >1423 |
| EBOV/Mak-r412 | 82V 544T | 0.01 | 0.001 | 0.08 | >10 | >1014 | |
| EBOV/Mak-201403261 | 82V 544I | 0.04 | 0.008 | 1.67 | >10 | >248 | |
| EBOV/May-tc | 82A 544I | 0.01 | 0.005 | 0.74 | >10 | >792 | |
| EBOV/Mak-r440 | 82A 544T | 1412 | 0.15 | 0.12 | 5.65 | >20 | >131 |
| EBOV/Mak-r412 | 82V 544T | 0.77 | 0.23 | 16 | >20 | >26 | |
| EBOV/Mak-201403261 | 82V 544I | 2.93 | 1.21 | 79.7 | >20 | >7 | |
| EBOV/May-tc | 82A 544I | 2.64 | 1.14 | 106 | >20 | >8 | |
| EBOV/Mak-r440 | 82A 544T | 1413 | 0.08 | 0.02 | 0.68 | >20 | >266 |
| EBOV/Mak-r412 | 82V 544T | 0.24 | 0.06 | 4.03 | >20 | >85 | |
| EBOV/Mak-201403261 | 82V 544I | 0.85 | 0.33 | 27,8 | >20 | >24 | |
| EBOV/May-tc | 82A 544I | 0.76 | 0.27 | 18.7 | >20 | >26 | |
| EBOV/Mak-r440 | 82A 544T | 1466 | 0.04 | 0.007 | 0.14 | >20 | >497 |
| EBOV/Mak-r412 | 82V 544T | 0.13 | 0.02 | 1.39 | >20 | >159 | |
| EBOV/Mak-201403261 | 82V 544I | 0.39 | 0.17 | 24.4 | >20 | >52 | |
| EBOV/May-tc | 82A 544I | 0.30 | 0.13 | 11.1 | >20 | >67 | |
| EBOV/Mak-r440 | 82A 544T | 1476 | 0.001 | 0.0004 | 0.05 | >10 | >14,169 |
| EBOV/Mak-r412 | 82V 544T | 0.002 | 0.001 | 0.17 | >10 | >5985 | |
| EBOV/Mak-201403261 | 82V 544I | 0.005 | 0.002 | 0.4 | >10 | >2018 | |
| EBOV/May-tc | 82A 544I | 0.002 | 0.002 | 0.37 | >10 | >4262 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Beitzel, B.F.; Radoshitzky, S.R.; Di Paola, N.; Brannan, J.M.; Kimmel, D.; Caviness, K.; Soloveva, V.; Yu, S.; Postnikova, E.N.; Finch, C.L.; et al. On-Demand Patient-Specific Phenotype-to-Genotype Ebola Virus Characterization. Viruses 2021, 13, 2010. https://doi.org/10.3390/v13102010
Beitzel BF, Radoshitzky SR, Di Paola N, Brannan JM, Kimmel D, Caviness K, Soloveva V, Yu S, Postnikova EN, Finch CL, et al. On-Demand Patient-Specific Phenotype-to-Genotype Ebola Virus Characterization. Viruses. 2021; 13(10):2010. https://doi.org/10.3390/v13102010
Chicago/Turabian StyleBeitzel, Brett F., Sheli R. Radoshitzky, Nicholas Di Paola, Jennifer M. Brannan, David Kimmel, Katie Caviness, Veronica Soloveva, Shuiqing Yu, Elena N. Postnikova, Courtney L. Finch, and et al. 2021. "On-Demand Patient-Specific Phenotype-to-Genotype Ebola Virus Characterization" Viruses 13, no. 10: 2010. https://doi.org/10.3390/v13102010
APA StyleBeitzel, B. F., Radoshitzky, S. R., Di Paola, N., Brannan, J. M., Kimmel, D., Caviness, K., Soloveva, V., Yu, S., Postnikova, E. N., Finch, C. L., Liu, H., Prugar, L., Bakken, R., Dye, J. M., Kugelman, J. R., Cunningham, J. M., Sanchez-Lockhart, M., Kuhn, J. H., & Palacios, G. (2021). On-Demand Patient-Specific Phenotype-to-Genotype Ebola Virus Characterization. Viruses, 13(10), 2010. https://doi.org/10.3390/v13102010







