Hepatitis A: Epidemiology, High-Risk Groups, Prevention and Research on Antiviral Treatment
Abstract
:1. Background and Virology
2. Clinical Outcomes
3. Hepatitis A Diagnosis
4. Transmission Routes of Hepatitis A Virus and Epidemiology
5. Specific Risk Groups in Developed Countries
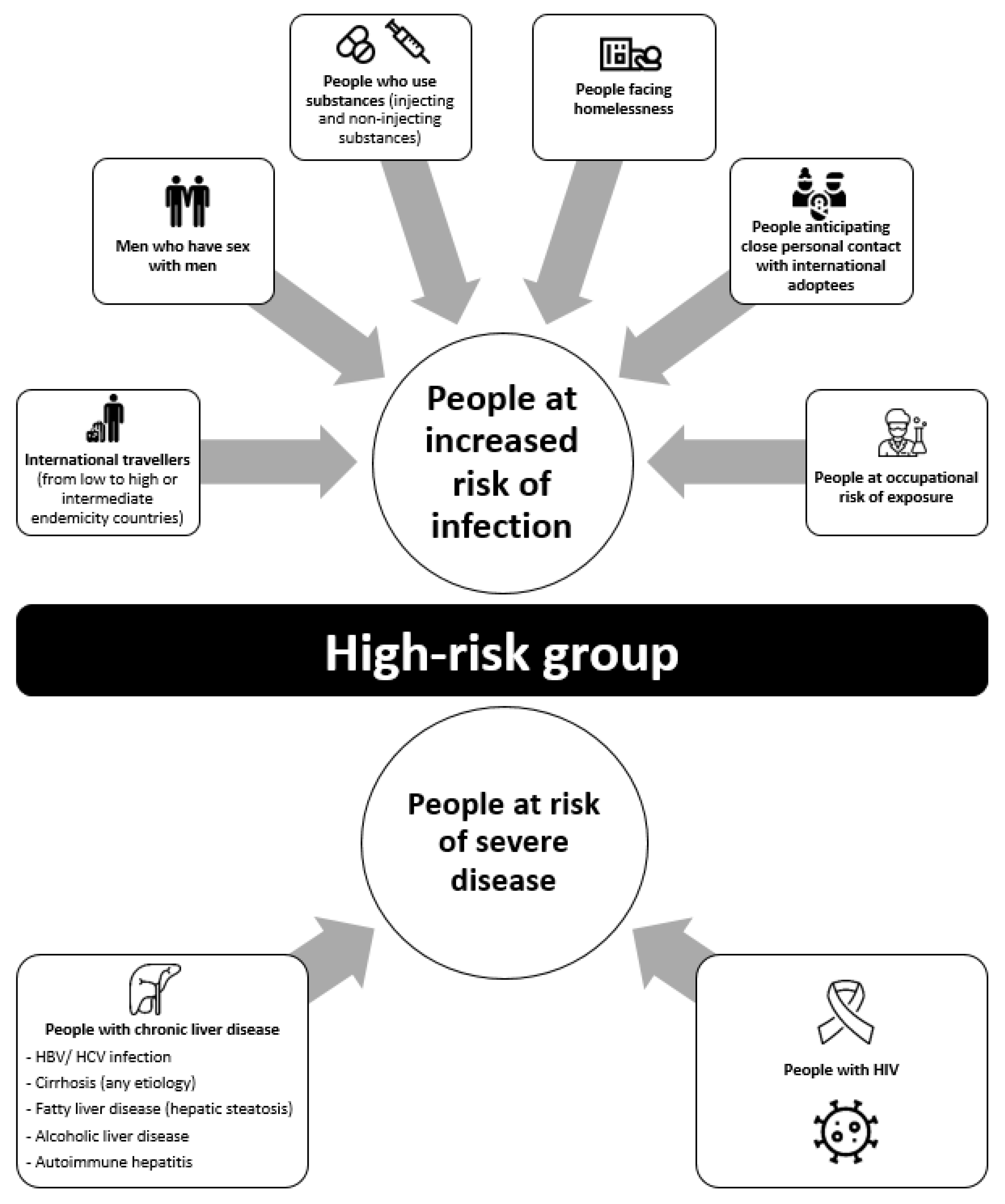
5.1. Increased Risk of HAV Infection
5.1.1. International Travellers
5.1.2. Men Who Have Sex with Men (MSM)
5.1.3. People Who Use Substances and Those Who Face Homelessness
5.2. People at Increased Risk of Severe Disease
6. Hepatitis A Prevention
7. Research on HAV Antiviral Treatment
8. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Wang, X.; Ren, J.; Gao, Q.; Hu, Z.; Sun, Y.; Li, X.; Rowlands, D.J.; Yin, W.; Wang, J.; Stuart, D.I.; et al. Hepatitis A Virus and the Origins of Picornaviruses. Nature 2015, 517, 85–88. [Google Scholar] [CrossRef]
- Feng, Z.; Hensley, L.; McKnight, K.L.; Hu, F.; Madden, V.; Ping, L.; Jeong, S.-H.; Walker, C.; Lanford, R.E.; Lemon, S.M. A Pathogenic Picornavirus Acquires an Envelope by Hijacking Cellular Membranes. Nature 2013, 496, 367–371. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hirai-Yuki, A.; Hensley, L.; Whitmire, J.K.; Lemon, S.M. Biliary Secretion of Quasi-Enveloped Human Hepatitis A Virus. mBio 2016, 7, e01998-16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Najarian, R.; Caput, D.; Gee, W.; Potter, S.J.; Renard, A.; Merryweather, J.; Van Nest, G.; Dina, D. Primary Structure and Gene Organization of Human Hepatitis A Virus. Proc. Natl. Acad. Sci. USA 1985, 82, 2627–2631. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Martin, A.; Lemon, S.M. Hepatitis A Virus: From Discovery to Vaccines. Hepatology 2006, 43, S164–S172. [Google Scholar] [CrossRef]
- Nainan, O.V.; Xia, G.; Vaughan, G.; Margolis, H.S. Diagnosis of Hepatitis A Virus Infection: A Molecular Approach. Clin. Microbiol. Rev. 2006, 19, 63–79. [Google Scholar] [CrossRef] [Green Version]
- Morace, G.; Kusov, Y.; Dzagurov, G.; Beneduce, F.; Gauss-Muller, V. The Unique Role of Domain 2A of the Hepatitis A Virus Precursor Polypeptide P1-2A in Viral Morphogenesis. BMB Rep. 2008, 41, 678–683. [Google Scholar] [CrossRef] [Green Version]
- Genus: Hepatovirus—Picornaviridae—Positive-Sense RNA Viruses—ICTV. Available online: https://talk.ictvonline.org/ictv-reports/ictv_online_report/positive-sense-rna-viruses/w/picornaviridae/709/genus-hepatovirus (accessed on 9 September 2021).
- Pérez-Sautu, U.; Costafreda, M.I.; Lite, J.; Sala, R.; Barrabeig, I.; Bosch, A.; Pintó, R.M. Molecular Epidemiology of Hepatitis A Virus Infections in Catalonia, Spain, 2005–2009: Circulation of Newly Emerging Strains. J. Clin. Virol. 2011, 52, 98–102. [Google Scholar] [CrossRef] [PubMed]
- Tong, M.J.; el-Farra, N.S.; Grew, M.I. Clinical Manifestations of Hepatitis A: Recent Experience in a Community Teaching Hospital. J. Infect. Dis. 1995, 171, S15–S18. [Google Scholar] [CrossRef]
- Koff, R.S. Clinical Manifestations and Diagnosis of Hepatitis A Virus Infection. Vaccine 1992, 10, S15–S17. [Google Scholar] [CrossRef]
- Lednar, W.M.; Lemon, S.M.; Kirkpatrick, J.W.; Redfield, R.R.; Fields, M.L.; Kelley, P.W. Frequency of Illness Associated with Epidemic Hepatitis A Virus Infections in Adults. Am. J. Epidemiol. 1985, 122, 226–233. [Google Scholar] [CrossRef] [PubMed]
- Lemon, S.M.; Ott, J.J.; Van Damme, P.; Shouval, D. Type A Viral Hepatitis: A Summary and Update on the Molecular Virology, Epidemiology, Pathogenesis and Prevention. J. Hepatol. 2018, 68, 167–184. [Google Scholar] [CrossRef] [Green Version]
- Pintó, R.M.; Pérez-Rodríguez, F.-J.; Costafreda, M.-I.; Chavarria-Miró, G.; Guix, S.; Ribes, E.; Bosch, A. Pathogenicity and Virulence of Hepatitis A Virus. Virulence 2021, 12, 1174–1185. [Google Scholar] [CrossRef]
- Willner, I.R.; Uhl, M.D.; Howard, S.C.; Williams, E.Q.; Riely, C.A.; Waters, B. Serious Hepatitis A: An Analysis of Patients Hospitalized during an Urban Epidemic in the United States. Ann. Intern. Med. 1998, 128, 111–114. [Google Scholar] [CrossRef] [PubMed]
- Gordon, S.C.; Reddy, K.R.; Schiff, L.; Schiff, E.R. Prolonged Intrahepatic Cholestasis Secondary to Acute Hepatitis A. Ann. Intern. Med. 1984, 101, 635–637. [Google Scholar] [CrossRef]
- Glikson, M.; Galun, E.; Oren, R.; Tur-Kaspa, R.; Shouval, D. Relapsing Hepatitis A. Review of 14 Cases and Literature Survey. Medicine 1992, 71, 14–23. [Google Scholar] [CrossRef] [PubMed]
- Inman, R.D.; Hodge, M.; Johnston, M.E.; Wright, J.; Heathcote, J. Arthritis, Vasculitis, and Cryoglobulinemia Associated with Relapsing Hepatitis A Virus Infection. Ann. Intern. Med. 1986, 105, 700–703. [Google Scholar] [CrossRef]
- Schiff, E.R. Atypical Clinical Manifestations of Hepatitis A. Vaccine 1992, 10, S18–S20. [Google Scholar] [CrossRef]
- Zikos, D.; Grewal, K.S.; Craig, K.; Cheng, J.C.; Peterson, D.R.; Fisher, K.A. Nephrotic Syndrome and Acute Renal Failure Associated with Hepatitis A Virus Infection. Am. J. Gastroenterol. 1995, 90, 295–298. [Google Scholar]
- Jung, Y.J.; Kim, W.; Jeong, J.B.; Kim, B.G.; Lee, K.L.; Oh, K.-H.; Yoon, J.-H.; Lee, H.-S.; Kim, Y.J. Clinical Features of Acute Renal Failure Associated with Hepatitis A Virus Infection. J. Viral Hepat. 2010, 17, 611–617. [Google Scholar] [CrossRef]
- World Health Organization. WHO Immunological Basis for Immunization Series, Module 18: Hepatitis A Update; WHO: Geneva, Switzerland, 2019. [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Positive Test Results for Acute Hepatitis A Virus Infection among Persons with No Recent History of Acute Hepatitis—United States, 2002—2004. MMWR Morb. Mortal. Wkly. Rep. 2005, 54, 453–456.
- Nelson, N.P.; Weng, M.K.; Hofmeister, M.G.; Moore, K.L.; Doshani, M.; Kamili, S.; Koneru, A.; Haber, P.; Hagan, L.; Romero, J.R.; et al. Prevention of Hepatitis A Virus Infection in the United States: Recommendations of the Advisory Committee on Immunization Practices, 2020. MMWR Recomm. Rep. 2020, 69, 1–38. [Google Scholar] [CrossRef] [PubMed]
- Bower, W.A.; Nainan, O.V.; Han, X.; Margolis, H.S. Duration of Viremia in Hepatitis A Virus Infection. J. Infect. Dis. 2000, 182, 12–17. [Google Scholar] [CrossRef]
- Costa-Mattioli, M.; Monpoeho, S.; Nicand, E.; Aleman, M.-H.; Billaudel, S.; Ferré, V. Quantification and Duration of Viraemia during Hepatitis A Infection as Determined by Real-Time RT-PCR. J. Viral. Hepat. 2002, 9, 101–106. [Google Scholar] [CrossRef] [PubMed]
- Yotsuyanagi, H.; Koike, K.; Yasuda, K.; Moriya, K.; Shintani, Y.; Fujie, H.; Kurokawa, K.; Iino, S. Prolonged Fecal Excretion of Hepatitis A Virus in Adult Patients with Hepatitis A as Determined by Polymerase Chain Reaction. Hepatology 1996, 24, 10–13. [Google Scholar] [CrossRef] [PubMed]
- Lowther, J.A.; Bosch, A.; Butot, S.; Ollivier, J.; Mäde, D.; Rutjes, S.A.; Hardouin, G.; Lombard, B.; In’t Veld, P.; Leclercq, A. Validation of EN ISO Method 15216—Part 1—Quantification of Hepatitis A Virus and Norovirus in Food Matrices. Int. J. Food Microbiol. 2019, 288, 82–90. [Google Scholar] [CrossRef] [PubMed]
- Siegl, G.; Weitz, M.; Kronauer, G. Stability of Hepatitis A Virus. Intervirology 1984, 22, 218–226. [Google Scholar] [CrossRef]
- Ramsay, C.N.; Upton, P.A. Hepatitis A and Frozen Raspberries. Lancet 1989, 1, 43–44. [Google Scholar] [CrossRef]
- McCaustland, K.A.; Bond, W.W.; Bradley, D.W.; Ebert, J.W.; Maynard, J.E. Survival of Hepatitis A Virus in Feces after Drying and Storage for 1 Month. J. Clin. Microbiol. 1982, 16, 957–958. [Google Scholar] [CrossRef] [Green Version]
- Costafreda, M.I.; Pérez-Rodriguez, F.J.; D’Andrea, L.; Guix, S.; Ribes, E.; Bosch, A.; Pintó, R.M. Hepatitis A Virus Adaptation to Cellular Shutoff Is Driven by Dynamic Adjustments of Codon Usage and Results in the Selection of Populations with Altered Capsids. J. Virol. 2014, 88, 5029–5041. [Google Scholar] [CrossRef] [Green Version]
- Tjon, G.M.S.; Coutinho, R.A.; van den Hoek, A.; Esman, S.; Wijkmans, C.J.; Hoebe, C.J.P.A.; Wolters, B.; Swaan, C.; Geskus, R.B.; Dukers, N.; et al. High and Persistent Excretion of Hepatitis A Virus in Immunocompetent Patients. J. Med. Virol. 2006, 78, 1398–1405. [Google Scholar] [CrossRef] [Green Version]
- Severi, E.; Verhoef, L.; Thornton, L.; Guzman-Herrador, B.R.; Faber, M.; Sundqvist, L.; Rimhanen-Finne, R.; Roque-Afonso, A.M.; Ngui, S.L.; Allerberger, F.; et al. Large and Prolonged Food-Borne Multistate Hepatitis A Outbreak in Europe Associated with Consumption of Frozen Berries, 2013 to 2014. Euro Surveill. 2015, 20, 21192. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garcia Vilaplana, T.; Leeman, D.; Balogun, K.; Ngui, S.L.; Phipps, E.; Khan, W.M.; Incident Team; Balasegaram, S. Hepatitis A Outbreak Associated with Consumption of Dates, England and Wales, January 2021 to April 2021. Euro Surveill. 2021, 26, 2100432. [Google Scholar] [CrossRef] [PubMed]
- Halliday, M.L.; Kang, L.-Y.; Zhou, T.-K.; Hu, M.-D.; Pan, Q.-C.; Fu, T.-Y.; Huang, Y.-S.; Hu, S.-L. An Epidemic of Hepatitis A Attributable to the Ingestion of Raw Clams in Shanghai, China. J. Infect. Dis. 1991, 164, 852–859. [Google Scholar] [CrossRef]
- Pintó, R.M.; Costafreda, M.I.; Bosch, A. Risk Assessment in Shellfish-Borne Outbreaks of Hepatitis A. Appl. Environ. Microbiol. 2009, 75, 7350–7355. [Google Scholar] [CrossRef] [Green Version]
- Di Cola, G.; Fantilli, A.C.; Pisano, M.B.; Ré, V.E. Foodborne Transmission of Hepatitis A and Hepatitis E Viruses: A Literature Review. Int. J. Food Microbiol. 2021, 338, 108986. [Google Scholar] [CrossRef]
- Foster, M.A.; Weil, L.M.; Jin, S.; Johnson, T.; Hayden-Mixson, T.R.; Khudyakov, Y.; Annambhotla, P.D.; Basavaraju, S.V.; Kamili, S.; Ritter, J.M.; et al. Transmission of Hepatitis A Virus through Combined Liver-Small Intestine-Pancreas Transplantation. Emerg. Infect. Dis. 2017, 23, 590–596. [Google Scholar] [CrossRef] [Green Version]
- Liu, Z.; Shi, O.; Zhang, T.; Jin, L.; Chen, X. Disease Burden of Viral Hepatitis A, B, C and E: A Systematic Analysis. J. Viral. Hepat. 2020, 27, 1284–1296. [Google Scholar] [CrossRef]
- Zeng, D.-Y.; Li, J.-M.; Lin, S.; Dong, X.; You, J.; Xing, Q.-Q.; Ren, Y.-D.; Chen, W.-M.; Cai, Y.-Y.; Fang, K.; et al. Global Burden of Acute Viral Hepatitis and Its Association with Socioeconomic Development Status, 1990–2019. J. Hepatol. 2021, S0168827821003007. [Google Scholar] [CrossRef]
- Jacobsen, K.H. Globalization and the Changing Epidemiology of Hepatitis A Virus. Cold Spring Harb. Perspect. Med. 2018, 8, a031716. [Google Scholar] [CrossRef] [Green Version]
- Lee, D.-Y.; Chae, S.-J.; Cho, S.-R.; Choi, W.; Kim, C.-K.; Han, M.-G. Nationwide Seroprevalence of Hepatitis A in South Korea from 2009 to 2019. PLoS ONE 2021, 16, e0245162. [Google Scholar] [CrossRef]
- Klevens, R.M.; Miller, J.T.; Iqbal, K.; Thomas, A.; Rizzo, E.M.; Hanson, H.; Sweet, K.; Phan, Q.; Cronquist, A.; Khudyakov, Y.; et al. The Evolving Epidemiology of Hepatitis a in the United States: Incidence and Molecular Epidemiology from Population-Based Surveill.ance, 2005-2007. Arch. Intern. Med. 2010, 170, 1811–1818. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Beauté, J.; Westrell, T.; Schmid, D.; Müller, L.; Epstein, J.; Kontio, M.; Couturier, E.; Faber, M.; Mellou, K.; Borg, M.-L.; et al. Travel-Associated Hepatitis A in Europe, 2009 to 2015. Euro Surveill. 2018, 23, 1700583. [Google Scholar] [CrossRef] [PubMed]
- Santé Publique France Hépatite A en France. Données Epidémiologiques 2019. Available online: https://www.santepubliquefrance.fr/maladies-et-traumatismes/hepatites-virales/hepatite-a/articles/hepatite-a-en-france.-donnees-epidemiologiques-2019 (accessed on 3 July 2021).
- Lu, P.-J.; Hung, M.-C.; Srivastav, A.; Grohskopf, L.A.; Kobayashi, M.; Harris, A.M.; Dooling, K.L.; Markowitz, L.E.; Rodriguez-Lainz, A.; Williams, W.W. Surveill.ance of Vaccination Coverage Among Adult Populations—United States, 2018. MMWR Surveill. Summ. 2021, 70, 1–26. [Google Scholar] [CrossRef]
- Narayanan, N.; Elsaid, M.I.; NeMoyer, R.E.; Trivedi, N.; Zeb, U.; Rustgi, V.K. Disparities in Hepatitis A Virus (HAV) Vaccination Coverage among Adult Travelers to Intermediate or High-Risk Countries: The Role of Birthplace and Race/Ethnicity. Vaccine 2019, 37, 4111–4117. [Google Scholar] [CrossRef]
- Doornekamp, L.; GeurtsvanKessel, C.; Slobbe, L.; Te Marvelde, M.R.; Scherbeijn, S.M.J.; van Genderen, P.J.J.; van Gorp, E.C.M.; Goeijenbier, M. Adherence to Hepatitis A Travel Health Guidelines: A Cross-Sectional Seroprevalence Study in Dutch Travelling Families—The Dutch Travel Vaccination Study (DiVeST). Travel Med. Infect. Dis. 2019, 32, 101511. [Google Scholar] [CrossRef] [PubMed]
- Pedersini, R.; Marano, C.; De Moerlooze, L.; Chen, L.; Vietri, J. HAV & HBV Vaccination among Travellers Participating in the National Health and Wellness Survey in Five European Countries. Travel Med. Infect. Dis. 2016, 14, 221–232. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Namikawa, K.; Iida, T.; Ouchi, K.; Kimura, M. Knowledge, Attitudes, and Practices of Japanese Travelers on Infectious Disease Risks and Immunization Uptake. J. Travel Med. 2010, 17, 171–175. [Google Scholar] [CrossRef] [Green Version]
- Gassowski, M.; Michaelis, K.; Wenzel, J.J.; Faber, M.; Figoni, J.; Mouna, L.; Friesema, I.H.; Vennema, H.; Avellon, A.; Varela, C.; et al. Two Concurrent Outbreaks of Hepatitis A Highlight the Risk of Infection for Non-Immune Travellers to Morocco, January to June 2018. Euro Surveill. 2018, 23, 1800329. [Google Scholar] [CrossRef]
- MacDonald, E.; Steens, A.; Stene-Johansen, K.; Lassen, S.G.; Midgley, S.E.; Lawrence, J.; Crofts, J.; Ngui, S.L.; Balogun, K.; Frank, C.; et al. Increase in Hepatitis A in Tourists from Denmark, England, Germany, the Netherlands, Norway and Sweden Returning from Egypt, November 2012 to March 2013. Euro Surveill. 2013, 18, 20468. [Google Scholar] [CrossRef]
- Corey, L.; Holmes, K.K. Sexual Transmission of Hepatitis A in Homosexual Men: Incidence and Mechanism. N. Engl. J. Med. 1980, 302, 435–438. [Google Scholar] [CrossRef] [PubMed]
- Stewart, T.; Crofts, N. An Outbreak of Hepatitis A among Homosexual Men in Melbourne. Med. J. Aust. 1993, 158, 519–521. [Google Scholar] [CrossRef]
- Christenson, B.; Broström, C.; Böttiger, M.; Hermanson, J.; Weiland, O.; Ryd, G.; Berg, J.V.; Sjöblom, R. An Epidemic Outbreak of Hepatitis A among Homosexual Men in Stockholm. Hepatitis A, a Special Hazard for the Male Homosexual Subpopulation in Sweden. Am. J. Epidemiol. 1982, 116, 599–607. [Google Scholar] [CrossRef]
- Henning, K.J.; Bell, E.; Braun, J.; Barker, N.D. A Community-Wide Outbreak of Hepatitis A: Risk Factors for Infection among Homosexual and Bisexual Men. Am. J. Med. 1995, 99, 132–136. [Google Scholar] [CrossRef] [Green Version]
- CDC MMWR Recommendations and Reports Prevention of Hepatitis A Through Active or Passive Immunization: Recommendations of the Advisory Committee on Immunization Practices. Available online: https://www.cdc.gov/mmwr/preview/mmwrhtml/00048084.htm (accessed on 21 July 2021).
- Katz, M.H.; Hsu, L.; Wong, E.; Liska, S.; Anderson, L.; Janssen, R.S. Seroprevalence of and Risk Factors for Hepatitis A Infection among Young Homosexual and Bisexual Men. J. Infect. Dis. 1997, 175, 1225–1229. [Google Scholar] [CrossRef] [Green Version]
- Bell, A.; Ncube, F.; Hansell, A.; Davison, K.L.; Young, Y.; Gilson, R.; Macdonald, N.; Heathcock, R.; Warburton, F.; Maguire, H. An Outbreak of Hepatitis A among Young Men Associated with Having Sex in Public Venues. Commun. Dis. Public Health 2001, 4, 163–170. [Google Scholar]
- Mazick, A.; Howitz, M.; Rex, S.; Jensen, I.P.; Weis, N.; Katzenstein, T.L.; Haff, J.; Molbak, K. Hepatitis A Outbreak among MSM Linked to Casual Sex and Gay Saunas in Copenhagen, Denmark. Euro Surveill. 2005, 10, 111–114. [Google Scholar] [CrossRef]
- Epidemiological Update: Hepatitis A Outbreak in the EU/EEA Mostly Affecting Men Who Have Sex with Men. Available online: https://www.ecdc.europa.eu/en/news-events/epidemiological-update-hepatitis-outbreak-eueea-mostly-affecting-men-who-have-sex-men-2 (accessed on 21 July 2021).
- Ndumbi, P.; Freidl, G.S.; Williams, C.J.; Mårdh, O.; Varela, C.; Avellón, A.; Friesema, I.; Vennema, H.; Beebeejaun, K.; Ngui, S.L.; et al. Hepatitis A Outbreak Disproportionately Affecting Men Who Have Sex with Men (MSM) in the European Union and European Economic Area, June 2016 to May 2017. Euro Surveill. 2018, 23, 1700641. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Freidl, G.S.; Sonder, G.J.; Bovée, L.P.; Friesema, I.H.; van Rijckevorsel, G.G.; Ruijs, W.L.; van Schie, F.; Siedenburg, E.C.; Yang, J.-Y.; Vennema, H. Hepatitis A Outbreak among Men Who Have Sex with Men (MSM) Predominantly Linked with the EuroPride, the Netherlands, July 2016 to February 2017. Euro Surveill. 2017, 22, 30468. [Google Scholar] [CrossRef]
- Chen, W.-C.; Chiang, P.-H.; Liao, Y.-H.; Huang, L.-C.; Hsieh, Y.-J.; Chiu, C.-M.; Lo, Y.-C.; Yang, C.-H.; Yang, J.-Y. Outbreak of Hepatitis A Virus Infection in Taiwan, June 2015 to September 2017. Euro Surveill. 2019, 24, 1800133. [Google Scholar] [CrossRef] [Green Version]
- Mello, V.; Lago, B.; Sousa, P.; Mello, F.; Souza, C.; Pinto, L.; Ginuino, C.; Fernandes, C.; Aguiar, S.; Villar, L.; et al. Hepatitis A Strain Linked to the European Outbreaks During Gay Events between 2016 and 2017, Identified in a Brazilian Homosexual Couple in 2017. Viruses 2019, 11, 281. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Foster, M.A.; Hofmeister, M.G.; Albertson, J.P.; Brown, K.B.; Burakoff, A.W.; Gandhi, A.P.; Glenn-Finer, R.E.; Gounder, P.; Ho, P.-Y.; Kavanaugh, T.; et al. Hepatitis A Virus Infections Among Men Who Have Sex with Men—Eight U.S. States, 2017–2018. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 875–878. [Google Scholar] [CrossRef] [PubMed]
- Srivastav, A.; O’Halloran, A.; Lu, P.-J.; Williams, W.W.; Hutchins, S.S. Vaccination Differences among U.S. Adults by Their Self-Identified Sexual Orientation, National Health Interview Survey, 2013–2015. PLoS ONE 2019, 14, e0213431. [Google Scholar] [CrossRef]
- Yin, S.; Barker, L.; Ly, K.N.; Kilmer, G.; Foster, M.A.; Drobeniuc, J.; Jiles, R.B. Susceptibility to Hepatitis A Virus Infection in the United States, 2007–2016. Clin. Infect. Dis. 2020, 71, e571–e579. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zimmermann, R.; Faber, M.; Dudareva, S.; Ingiliz, P.; Jessen, H.; Koch, J.; Marcus, U.; Michaelis, K.; Rieck, T.; Ruscher, C.; et al. Hepatitis A Outbreak among MSM in Berlin Due to Low Vaccination Coverage: Epidemiology, Management, and Successful Interventions. Int. J. Infect. Dis. 2021, 103, 146–153. [Google Scholar] [CrossRef]
- Penot, P.; Colombier, M.-A.; Maylin, S.; Molina, J.-M. Hepatitis A Infections in Men Who Have Sex with Men Using HIV PrEP in Paris. BMJ Case Rep. 2018, 2018, bcr-2017-222248. [Google Scholar] [CrossRef]
- Charre, C.; Ramière, C.; Roque-Afonso, A.-M.; Chidiac, C.; Zoulim, F.; Godinot, M.; Koffi, J.; Scholtès, C.; Livrozet, J.-M.; Cotte, L.; et al. Hepatitis A outbreak in HIV-infected MSM and in PrEP-using MSM despite a high level of immunity, Lyon, France, January to June 2017. Euro Surveill. 2017, 22, 1700742. [Google Scholar] [CrossRef] [Green Version]
- Boucher, A.; Meybeck, A.; Alidjinou, K.; Huleux, T.; Viget, N.; Baclet, V.; Valette, M.; Alcaraz, I.; Sauser, E.; Bocket, L.; et al. Clinical and Virological Features of Acute Hepatitis A during an Ongoing Outbreak among Men Who Have Sex with Men in the North of France. Sex Transm. Infect. 2019, 95, 75–77. [Google Scholar] [CrossRef]
- Migueres, M.; Ducours, M.; Dimeglio, C.; Trimoulet, P.; Abravanel, F.; Delobel, P.; Cazanave, C.; Izopet, J. No Evidence of Sexual Transmission of HEV among Individuals Using HIV Pre-Exposure Prophylaxis. J. Viral. Hepat. 2020, 27, 1495–1501. [Google Scholar] [CrossRef]
- O’Donovan, D.; Cooke, R.P.D.; Joce, R.; Eastbury, A.; Waite, J.; Stene-Johansen, K. An Outbreak of Hepatitis A amongst Injecting Drug Users. Epidemiol. Infect. 2001, 127, 469–473. [Google Scholar] [CrossRef]
- Roy, K.; Howie, H.; Sweeney, C.; Parry, J.; Molyneaux, P.; Goldberg, D.; Taylor, A. Hepatitis A Virus and Injecting Drug Misuse in Aberdeen, Scotland: A Case-Control Study. J. Viral. Hepat. 2004, 11, 277–282. [Google Scholar] [CrossRef]
- Lugoboni, F.; Pajusco, B.; Albiero, A.; Quaglio, G. Hepatitis A Virus among Drug Users and the Role of Vaccination: A Review. Front. Psychiatry 2012, 2. [Google Scholar] [CrossRef] [Green Version]
- Hutin, Y.J.; Sabin, K.M.; Hutwagner, L.C.; Schaben, L.; Shipp, G.M.; Lord, D.M.; Conner, J.S.; Quinlisk, M.P.; Shapiro, C.N.; Bell, B.P. Multiple Modes of Hepatitis A Virus Transmission among Methamphetamine Users. Am. J. Epidemiol. 2000, 152, 186–192. [Google Scholar] [CrossRef] [Green Version]
- Spada, E.; Genovese, D.; Tosti, M.E.; Mariano, A.; Cuccuini, M.; Proietti, L.; Giuli, C.D.; Lavagna, A.; Crapa, G.E.; Morace, G.; et al. An Outbreak of Hepatitis A Virus Infection with a High Case-Fatality Rate among Injecting Drug Users. J. Hepatol. 2005, 43, 958–964. [Google Scholar] [CrossRef]
- Samala, N.; Abdallah, W.; Poole, A.; Shamseddeen, H.; Are, V.; Orman, E.; Patidar, K.R.; Vuppalanchi, R. Insight into an Acute Hepatitis A Outbreak in Indiana. J. Viral. Hepat. 2021, 28, 964–971. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention Widespread Outbreaks of Hepatitis A across the U.S. CDC. Available online: https://www.cdc.gov/hepatitis/outbreaks/2017March-HepatitisA.htm (accessed on 20 July 2021).
- Hofmeister, M.G.; Xing, J.; Foster, M.A.; Augustine, R.J.; Burkholder, C.; Collins, J.; McBee, S.; Thomasson, E.D.; Thoroughman, D.; Weng, M.K.; et al. Hepatitis A Person-to-Person Outbreaks: Epidemiology, Morbidity Burden, and Factors Associated with Hospitalization—Multiple States, 2016–2019. J. Infect. Dis. 2021, 223, 426–434. [Google Scholar] [CrossRef] [PubMed]
- Lin, K.-Y.; Fang, C.-T. Public Health Responses to Person-to-Person Hepatitis A Outbreaks. J. Infect. Dis. 2021, 223, 359–361. [Google Scholar] [CrossRef] [PubMed]
- Foster, M. Hepatitis A Virus Outbreaks Associated with Drug Use and Homelessness—California, Kentucky, Michigan, and Utah, 2017. MMWR Morb. Mortal. Wkly. Rep. 2018, 67. [Google Scholar] [CrossRef]
- Peak, C.M.; Stous, S.S.; Healy, J.M.; Hofmeister, M.G.; Lin, Y.; Ramachandran, S.; Foster, M.A.; Kao, A.; McDonald, E.C. Homelessness and Hepatitis A—San Diego County, 2016–2018. Clin. Infect. Dis. 2020, 71, 14–21. [Google Scholar] [CrossRef] [PubMed]
- Tjon, G.M.S.; Götz, H.; Koek, A.G.; de Zwart, O.; Mertens, P.L.J.M.; Coutinho, R.A.; Bruisten, S.M. An Outbreak of Hepatitis A among Homeless Drug Users in Rotterdam, The Netherlands. J. Med. Virol. 2005, 77, 360–366. [Google Scholar] [CrossRef]
- Hennessey, K.A.; Bangsberg, D.R.; Weinbaum, C.; Hahn, J.A. Hepatitis A Seroprevalence and Risk Factors among Homeless Adults in San Francisco: Should Homelessness Be Included in the Risk-Based Strategy for Vaccination? Public Health Rep. 2009, 124, 813–817. [Google Scholar] [CrossRef] [PubMed]
- Doshani, M. Recommendations of the Advisory Committee on Immunization Practices for Use of Hepatitis A Vaccine for Persons Experiencing Homelessness. MMWR Morb. Mortal. Wkly. Rep. 2019, 68, 153–156. [Google Scholar] [CrossRef]
- Vento, S.; Garofano, T.; Renzini, C.; Cainelli, F.; Casali, F.; Ghironzi, G.; Ferraro, T.; Concia, E. Fulminant Hepatitis Associated with Hepatitis A Virus Superinfection in Patients with Chronic Hepatitis C. N. Engl. J. Med. 1998, 338, 286–290. [Google Scholar] [CrossRef] [PubMed]
- Hofmeister, M.G.; Xing, J.; Foster, M.A.; Augustine, R.J.; Burkholder, C.; Collins, J.; McBee, S.; Thomasson, E.D.; Thoroughman, D.; Weng, M.K.; et al. Factors Associated with Hepatitis A Mortality During Person-to-Person Outbreaks: A Matched Case-Control Study-United States, 2016–2019. Hepatology 2020, 74, 28–40. [Google Scholar] [CrossRef] [PubMed]
- Lin, K.-Y.; Chen, G.-J.; Lee, Y.-L.; Huang, Y.-C.; Cheng, A.; Sun, H.-Y.; Chang, S.-Y.; Liu, C.-E.; Hung, C.-C. Hepatitis A Virus Infection and Hepatitis A Vaccination in Human Immunodeficiency Virus-Positive Patients: A Review. WJG 2017, 23, 3589–3606. [Google Scholar] [CrossRef] [PubMed]
- Ida, S.; Tachikawa, N.; Nakajima, A.; Daikoku, M.; Yano, M.; Kikuchi, Y.; Yasuoka, A.; Kimura, S.; Oka, S. Influence of Human Immunodeficiency Virus Type 1 Infection on Acute Hepatitis A Virus Infection. Clin. Infect. Dis. 2002, 34, 379–385. [Google Scholar] [CrossRef] [PubMed]
- Tram, J.; Le Baccon-Sollier, P.; Bolloré, K.; Ducos, J.; Mondain, A.-M.; Pastor, P.; Pageaux, G.-P.; Makinson, A.; de Perre, P.V.; Tuaillon, E. RNA Testing for the Diagnosis of Acute Hepatitis A during the 2017 Outbreak in France. J. Viral. Hepat. 2020, 27, 540–543. [Google Scholar] [CrossRef]
- Lee, Y.-L.; Chen, G.-J.; Chen, N.-Y.; Liou, B.-H.; Wang, N.-C.; Lee, Y.-T.; Yang, C.-J.; Huang, Y.-S.; Tang, H.-J.; Huang, S.-S.; et al. Less Severe but Prolonged Course of Acute Hepatitis A in Human Immunodeficiency Virus (HIV)–Infected Patients Compared With HIV-Uninfected Patients During an Outbreak: A Multicenter Observational Study. Clin. Infect. Dis. 2018, 67, 1595–1602. [Google Scholar] [CrossRef]
- Werzberger, A.; Mensch, B.; Kuter, B.; Brown, L.; Lewis, J.; Sitrin, R.; Miller, W.; Shouval, D.; Wiens, B.; Calandra, G. A Controlled Trial of a Formalin-Inactivated Hepatitis A Vaccine in Healthy Children. N. Engl. J. Med. 1992, 327, 453–457. [Google Scholar] [CrossRef]
- Mao, J.S.; Dong, D.X.; Zhang, H.Y.; Chen, N.L.; Zhang, X.Y.; Huang, H.Y.; Xie, R.Y.; Zhou, T.J.; Wan, Z.J.; Wang, Y.Z. Primary Study of Attenuated Live Hepatitis A Vaccine (H2 Strain) in Humans. J. Infect. Dis. 1989, 159, 621–624. [Google Scholar] [CrossRef]
- Victor, J.C.; Monto, A.S.; Surdina, T.Y.; Suleimenova, S.Z.; Vaughan, G.; Nainan, O.V.; Favorov, M.O.; Margolis, H.S.; Bell, B.P. Hepatitis A Vaccine versus Immune Globulin for Postexposure Prophylaxis. N. Engl. J. Med. 2007, 357, 1685–1694. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shouval, D. Immunization against Hepatitis A. Cold Spring Harb. Perspect. Med. 2019, 9, a031682. [Google Scholar] [CrossRef] [PubMed]
- Nelson, N.P.; Link-Gelles, R.; Hofmeister, M.G.; Romero, J.R.; Moore, K.L.; Ward, J.W.; Schillie, S.F. Update: Recommendations of the Advisory Committee on Immunization Practices for Use of Hepatitis A Vaccine for Postexposure Prophylaxis and for Preexposure Prophylaxis for International Travel. MMWR Morb. Mortal. Wkly. Rep. 2018, 67, 1216–1220. [Google Scholar] [CrossRef] [Green Version]
- Ojeda-Martinez, H.I.; McGowan, J.P.; Fine, S.M.; Vail, R.; Merrick, S.T.; Radix, A.; Hoffmann, C.J.; Gonzalez, C.J. Prevention and Management of Hepatitis A Virus in Adults With HIV; New York State Department of Health AIDS Institute Clinical Guidelines; Johns Hopkins University: Baltimore, MD, USA, 2021. [Google Scholar]
- Stuurman, A.L.; Marano, C.; Bunge, E.M.; De Moerlooze, L.; Shouval, D. Impact of Universal Mass Vaccination with Monovalent Inactivated Hepatitis A Vaccines—A Systematic Review. Hum. Vaccin. Immunother. 2017, 13, 724–736. [Google Scholar] [CrossRef]
- D’Andrea, L.; Pérez-Rodríguez, F.J.; de Castellarnau, M.; Manzanares, S.; Lite, J.; Guix, S.; Bosch, A.; Pintó, R.M. Hepatitis A Virus Genotype Distribution during a Decade of Universal Vaccination of Preadolescents. Int. J. Mol. Sci. 2015, 16, 6842–6854. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Andani, A.; van Damme, P.; Bunge, E.M.; Salgado, F.; van Hoorn, R.C.; Hoet, B. One or Two Doses of Hepatitis A Vaccine in Universal Vaccination Programs in Children in 2020: A Systematic Review. Vaccine 2021, 29, S0264410X21000542. [Google Scholar] [CrossRef]
- Vizzotti, C.; González, J.; Gentile, A.; Rearte, A.; Ramonet, M.; Cañero-Velasco, M.C.; Pérez Carrega, M.E.; Urueña, A.; Diosque, M. Impact of the Single-Dose Immunization Strategy Against Hepatitis A in Argentina. Pediatr. Infect. Dis. J. 2014, 33, 84–88. [Google Scholar] [CrossRef] [Green Version]
- Sabrià, A.; Gregori, J.; Garcia-Cehic, D.; Guix, S.; Pumarola, T.; Manzanares-Laya, S.; Caylà, J.A.; Bosch, A.; Quer, J.; Pintó, R.M. Evidence for Positive Selection of Hepatitis A Virus Antigenic Variants in Vaccinated Men-Having-Sex-with Men Patients: Implications for Immunization Policies. EBio Med. 2018, 39, 348–357. [Google Scholar] [CrossRef]
- Kanda, T.; Nakamoto, S.; Wu, S.; Nakamura, M.; Jiang, X.; Haga, Y.; Sasaki, R.; Yokosuka, O. Direct-Acting Antivirals and Host-Targeting Agents against the Hepatitis A Virus. J. Clin. Transl. Hepatol. 2015, 3, 205–210. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kanda, T.; Sasaki, R.; Masuzaki, R.; Matsumoto, N.; Ogawa, M.; Moriyama, M. Cell Culture Systems and Drug Targets for Hepatitis A Virus Infection. Viruses 2020, 12, 533. [Google Scholar] [CrossRef]
- Debing, Y.; Neyts, J.; Thibaut, H.J. Molecular Biology and Inhibitors of Hepatitis A Virus. Med. Res. Rev. 2014, 34, 895–917. [Google Scholar] [CrossRef] [Green Version]
- Crance, J.M.; Deloince, R.; Leveque, F.; Jouan, A.; Trépo, C. Antiviral effect of recombinant interferon-alpha on hepatitis A virus replication in human liver cells. C R Acad. Sci. III 1994, 317, 94–97. [Google Scholar] [PubMed]
- Berthillon, P.; Crance, J.-M.; Leveque, F.; Jouan, A.; Petit, M.-A.; Deloince, R.; Trepo, C. Inhibition of the Expression of Hepatitis A and B Viruses (HAV and HBV) Proteins by Interferon in a Human Hepatocarcinoma Cell Line (PLC/PRF/5). J. Hepatol. 1996, 25, 15–19. [Google Scholar] [CrossRef]
- Yoshiba, M.; Inoue, K.; Sekiyama, K. Interferon for Hepatitis A. Lancet 1994, 343, 288–289. [Google Scholar] [CrossRef]
- Kanda, T.; Wu, S.; Kiyohara, T.; Nakamoto, S.; Jiang, X.; Miyamura, T.; Imazeki, F.; Ishii, K.; Wakita, T.; Yokosuka, O. Interleukin-29 Suppresses Hepatitis A and C Viral Internal Ribosomal Entry Site-Mediated Translation. Viral. Immunol. 2012, 25, 379–386. [Google Scholar] [CrossRef] [PubMed]
- Jiang, X.; Kanda, T.; Nakamoto, S.; Saito, K.; Nakamura, M.; Wu, S.; Haga, Y.; Sasaki, R.; Sakamoto, N.; Shirasawa, H.; et al. The JAK2 Inhibitor AZD1480 Inhibits Hepatitis A Virus Replication in Huh7 Cells. Biochem. Biophys. Res. Commun. 2015, 458, 908–912. [Google Scholar] [CrossRef] [PubMed]
- Jiang, X.; Kanda, T.; Wu, S.; Nakamoto, S.; Saito, K.; Shirasawa, H.; Kiyohara, T.; Ishii, K.; Wakita, T.; Okamoto, H.; et al. Suppression of La Antigen Exerts Potential Antiviral Effects against Hepatitis A Virus. PLoS ONE 2014, 9, e101993. [Google Scholar] [CrossRef] [Green Version]
- Kanda, T.; Sasaki, R.; Masuzaki, R.; Takahashi, H.; Fujisawa, M.; Matsumoto, N.; Okamoto, H.; Moriyama, M. Additive Effects of Zinc Chloride on the Suppression of Hepatitis A Virus Replication by Interferon in Human Hepatoma Huh7 Cells. In Vivo 2020, 34, 3301–3308. [Google Scholar] [CrossRef]
- Ogawa, M.; Kanda, T.; Suganami, A.; Nakamoto, S.; Win, N.N.; Tamura, Y.; Nakamura, M.; Matsuoka, S.; Yokosuka, O.; Kato, N.; et al. Antiviral Activity of Zinc Sulfate against Hepatitis A Virus Replication. Future Virol. 2019, 14, 399–406. [Google Scholar] [CrossRef]
- Kanda, T.; Sasaki-Tanaka, R.; Masuzaki, R.; Matsumoto, N.; Okamoto, H.; Moriyama, M. Knockdown of Mitogen-Activated Protein Kinase Kinase 3 Negatively Regulates Hepatitis A Virus Replication. IJMS 2021, 22, 7420. [Google Scholar] [CrossRef]
- Kim, D.-H.; Ahn, H.-S.; Go, H.-J.; Kim, D.-Y.; Kim, J.-H.; Lee, J.-B.; Park, S.-Y.; Song, C.-S.; Lee, S.-W.; Choi, I.-S. Heme Oxygenase-1 Exerts Antiviral Activity against Hepatitis A Virus In Vitro. Pharmaceutics 2021, 13, 1229. [Google Scholar] [CrossRef]
- Chaudhary, R.K.; Andonov, A.P. Effect of Ribavirin on Hepatitis A Virus Replication in Vitro. Can. J. Infect. Dis. 1992, 3, 67–70. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Widell, A.; Hansson, B.G.; Öberg, B.; Nordenfelt, E. Influence of Twenty Potentially Antiviral Substances on in Vitro Multiplication of Hepatitis a Virus. Antivir. Res. 1986, 6, 103–112. [Google Scholar] [CrossRef]
- Jiang, W.; Muhammad, F.; Ma, P.; Liu, X.; Long, G. Sofosbuvir Inhibits Hepatitis A Virus Replication In Vitro Assessed by a Cell-Based Fluorescent Reporter System. Antivir. Res. 2018, 154, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Kanda, T.; Imazeki, F.; Nakamoto, S.; Okitsu, K.; Fujiwara, K.; Yokosuka, O. Internal Ribosomal Entry-Site Activities of Clinical Isolate-Derived Hepatitis A Virus and Inhibitory Effects of Amantadine. Hepatol. Res. 2010, 40, 415–423. [Google Scholar] [CrossRef] [PubMed]
- Kanda, T.; Zhang, B.; Kusov, Y.; Yokosuka, O.; Gauss-Müller, V. Suppression of Hepatitis A Virus Genome Translation and Replication by SiRNAs Targeting the Internal Ribosomal Entry Site. Biochem. Biophys. Res. Commun. 2005, 330, 1217–1223. [Google Scholar] [CrossRef]
- Konduru, K.; Kaplan, G.G. Determinants in 3Dpol Modulate the Rate of Growth of Hepatitis A Virus. J. Virol. 2010, 84, 8342–8347. [Google Scholar] [CrossRef] [Green Version]
- Morris, T.S.; Frormann, S.; Shechosky, S.; Lowe, C.; Lall, M.S.; Gauss-Müller, V.; Purcell, R.H.; Emerson, S.U.; Vederas, J.C.; Malcolm, B.A. In Vitro and Ex Vivo Inhibition of Hepatitis A Virus 3C Proteinase by a Peptidyl Monofluoromethyl Ketone. Bioorg. Med. Chem. 1997, 5, 797–807. [Google Scholar] [CrossRef]
- Lall, M.S.; Ramtohul, Y.K.; James, M.N.G.; Vederas, J.C. Serine and Threonine Beta-Lactones: A New Class of Hepatitis A Virus 3C Cysteine Proteinase Inhibitors. J. Org. Chem. 2002, 67, 1536–1547. [Google Scholar] [CrossRef]
- Blaum, B.S.; Wünsche, W.; Benie, A.J.; Kusov, Y.; Peters, H.; Gauss-Müller, V.; Peters, T.; Sczakiel, G. Functional Binding of Hexanucleotides to 3C Protease of Hepatitis A Virus. Nucleic. Acids Res. 2012, 40, 3042–3055. [Google Scholar] [CrossRef] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Migueres, M.; Lhomme, S.; Izopet, J. Hepatitis A: Epidemiology, High-Risk Groups, Prevention and Research on Antiviral Treatment. Viruses 2021, 13, 1900. https://doi.org/10.3390/v13101900
Migueres M, Lhomme S, Izopet J. Hepatitis A: Epidemiology, High-Risk Groups, Prevention and Research on Antiviral Treatment. Viruses. 2021; 13(10):1900. https://doi.org/10.3390/v13101900
Chicago/Turabian StyleMigueres, Marion, Sébastien Lhomme, and Jacques Izopet. 2021. "Hepatitis A: Epidemiology, High-Risk Groups, Prevention and Research on Antiviral Treatment" Viruses 13, no. 10: 1900. https://doi.org/10.3390/v13101900
APA StyleMigueres, M., Lhomme, S., & Izopet, J. (2021). Hepatitis A: Epidemiology, High-Risk Groups, Prevention and Research on Antiviral Treatment. Viruses, 13(10), 1900. https://doi.org/10.3390/v13101900






