Middle East Respiratory Syndrome Coronavirus (MERS-CoV) Seropositive Camel Handlers in Kenya
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Zaki, A.M.; van Boheemen, S.; Bestebroer, T.M.; Osterhaus, A.D.M.E.; Fouchier, R.A.M. Isolation of a Novel Coronavirus from a Man with Pneumonia in Saudi Arabia. N. Engl. J. Med. 2012, 367, 1814–1820. [Google Scholar] [CrossRef] [PubMed]
- Dudas, G.; Carvalho, L.M.; Rambaut, A.; Bedford, T. MERS-CoV spillover at the camel-human interface. Elife 2018, 7, 1–23. [Google Scholar]
- Alraddadi, B.M.; Watson, J.T.; Almarashi, A.; Abedi, G.R.; Turkistani, A.; Sadran, M.; Housa, A.; Almazroa, M.A.; Alraihan, N.; Banjar, A.; et al. Risk factors for primary middle east respiratory syndrome coronavirus illness in humans, Saudi Arabia, 2014. Emerg. Infect. Dis. 2016, 22, 49–55. [Google Scholar] [CrossRef] [PubMed]
- Reusken, C.B.E.M.; Farag, E.A.B.A.; Haagmans, B.L.; Mohran, K.A.; Godeke, G.J.; Raj, V.S.; Alhajri, F.; Al-Marri, S.A.; Al-Romaihi, H.E.; Al-Thani, M.; et al. Occupational exposure to dromedaries and risk for MERS-CoV infection, Qatar, 2013–2014. Emerg. Infect. Dis. 2015, 21, 1422–1425. [Google Scholar] [CrossRef] [PubMed]
- Aly, M.; Elrobh, M.; Alzayer, M.; Aljuhani, S.; Balkhy, H. Occurrence of the Middle East Respiratory Syndrome Coronavirus (MERS-CoV) across the Gulf Corporation Council countries: Four years update. PLoS ONE 2017, 12, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Deem, S.L.; Fèvre, E.M.; Kinnaird, M.; Browne, A.S.; Muloi, D.; Godeke, G.J.; Koopmans, M.; Reusken, C.B. Serological evidence of MERS-CoV antibodies in dromedary camels (camelus dromedaries) in laikipia county, Kenya. PLoS ONE 2015, 10, 11–15. [Google Scholar] [CrossRef] [PubMed]
- Liljander, A.; Meyer, B.; Jores, J.; Müller, M.A.; Lattwein, E.; Njeru, I.; Bett, B.; Drosten, C.; Corman, V.M. MERS-CoV Antibodies in Humans, Africa, 2013-2014. Emerg. Infect. Dis. 2016, 22, 1086–1089. [Google Scholar] [CrossRef] [PubMed]
- Munyua, P.; Corman, V.M.; Bitek, A.; Osoro, E.; Meyer, B.; Müller, M.A.; Lattwein, E.; Thumbi, S.M.; Murithi, R.; Widdowson, M.A.; et al. No serologic evidence of middle east respiratory syndrome coronavirus infection among camel farmers exposed to highly seropositive camel herds: A household linked study, Kenya, 2013. Am. J. Trop. Med. Hyg. 2017, 96, 1318–1324. [Google Scholar] [CrossRef] [PubMed]
- Okba, N.M.A.; Raj, V.S.; Widjaja, I.; GeurtsvanKessel, C.H.; de Bruin, E.; Chandler, F.D.; Park, W.B.; Kim, N.-J.; Farag, E.A.B.A.; Al-Hajri, M.; et al. Sensitive and Specific Detection of Low-Level Antibody Responses in Mild Middle East Respiratory Syndrome Coronavirus Infections. Emerg. Infect. Dis. 2019, 25, 1868–1877. [Google Scholar] [CrossRef] [PubMed]
- Kiambi, S.; Corman, V.M.; Sitawa, R.; Githinji, J.; Ngoci, J.; Ozomata, A.S.; Gardner, E.; von Dobschuetz, S.; Morzaria, S.; Kimutai, J.; et al. Detection of distinct MERS-Coronavirus strains in dromedary camels from Kenya, 2017. Emerg. Microbes Infect. 2018, 7, 195. [Google Scholar] [CrossRef] [PubMed]
- Roess, A.; Carruth, L.; Lahm, S.; Salman, M. Camels, MERS-CoV, and other emerging infections in east Africa. Lancet Infect. Dis. 2016, 16, 14–15. [Google Scholar] [CrossRef]
- So Ray, T.Y.; Perera Ranawaka, A.P.M.; Oladipo Jamiu, O.; Chu Daniel, K.W.; Kuranga Sulyman, A.; Kin-Ho, C.; Lau Eric, H.Y.; Cheng Samuel, M.S.; Poon Leo, L.M.; Webby Richard, J.; et al. Lack of serological evidence of middle east respiratory syndrome coronavirus infection in virus exposed camel abattoir workers in Nigeria, 2016. Eurosurveillance 2018, 23, 2–5. [Google Scholar]
- Aburizaiza, A.S.; Mattes, F.M.; Azhar, E.I.; Hassan, A.M.; Memish, Z.A.; Muth, D.; Meyer, B.; Lattwein, E.; Müller, M.A.; Drosten, C. Investigation of anti-middle east respiratory syndrome antibodies in blood donors and slaughterhouse workers in Jeddah and Makkah, Saudi Arabia, Fall 2012. J. Infect. Dis. 2014, 209, 243–246. [Google Scholar] [CrossRef] [PubMed]
- Hemida, M.G.; Al-Naeem, A.; Perera, R.A.P.M.; Chin, A.W.H.; Poon, L.L.M.; Peiris, M. Lack of Middle East Respiratory Syndrome Coronavirus Transmission from Infected Camels. Emerg. Infect. Dis. 2015, 21, 699–701. [Google Scholar] [CrossRef] [PubMed]
- Dighe, A.; Jombart, T.; Kerkhove, M.D.v.; Ferguson, N. A systematic review of MERS-CoV seroprevalence and RNA prevalence in dromedary camels: Implications for animal vaccination. Epidemics 2019, 29, 100350. [Google Scholar] [CrossRef] [PubMed]
- Nicholas, D.E.; Jacobsen, K.H.; Waters, N.M. Risk factors associated with human Rift Valley fever infection: systematic review and meta-analysis. Trop. Med. Int. Health 2014, 19, 1420–1429. [Google Scholar] [CrossRef] [PubMed]
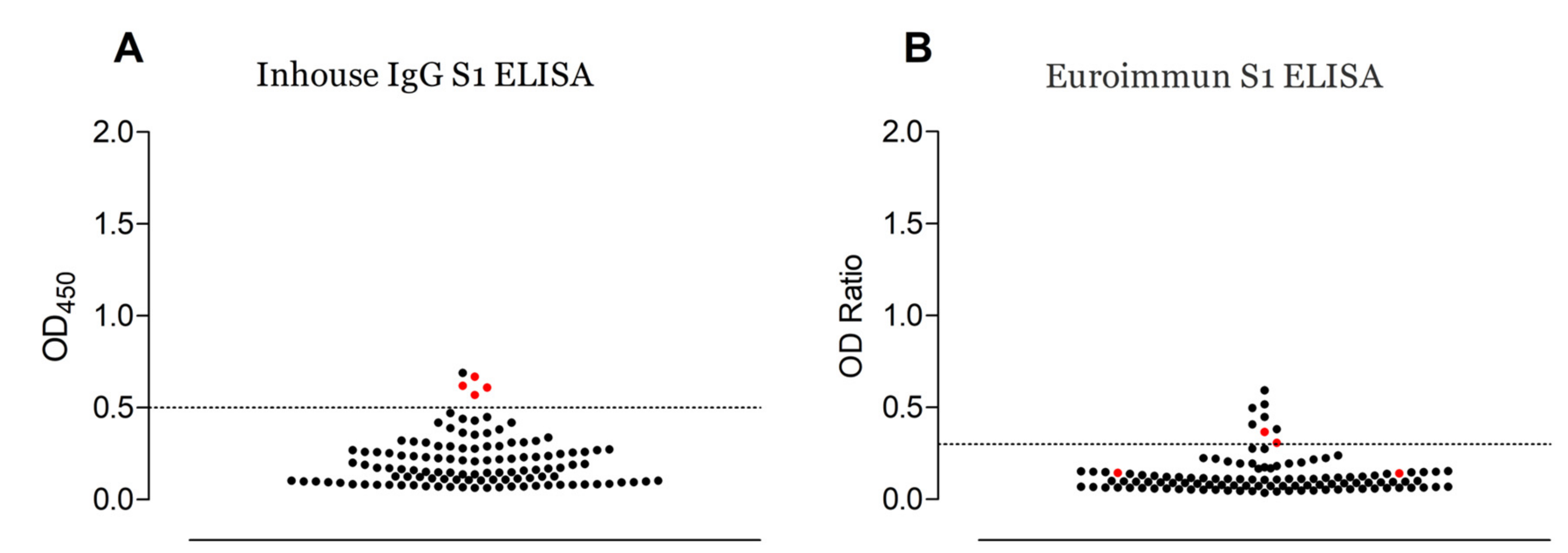
| Cohort | Number of Samples | Euroimmun S1 ELISA Positive Number (%) | In-house S1 ELISA Positive Number (%) | PRNT50 Positive Number | |
|---|---|---|---|---|---|
| Commercial S1 ELISA positive | In-House S1 ELISA Positive | ||||
| Slaughterhouse workers | 58 | 5 (8.6) | 4 (6.8) | 2/5 | 4/4 |
| Camel herders | 35 | 3 (8.6) | 1 (2.9) | 0/3 | 0/1 |
| Total | 93 | 8 (8.6) | 5 (5.4) | 2/8 | 4/5 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kiyong’a, A.N.; Cook, E.A.J.; Okba, N.M.A.; Kivali, V.; Reusken, C.; Haagmans, B.L.; Fèvre, E.M. Middle East Respiratory Syndrome Coronavirus (MERS-CoV) Seropositive Camel Handlers in Kenya. Viruses 2020, 12, 396. https://doi.org/10.3390/v12040396
Kiyong’a AN, Cook EAJ, Okba NMA, Kivali V, Reusken C, Haagmans BL, Fèvre EM. Middle East Respiratory Syndrome Coronavirus (MERS-CoV) Seropositive Camel Handlers in Kenya. Viruses. 2020; 12(4):396. https://doi.org/10.3390/v12040396
Chicago/Turabian StyleKiyong’a, Alice N., Elizabeth A. J. Cook, Nisreen M. A. Okba, Velma Kivali, Chantal Reusken, Bart L. Haagmans, and Eric M. Fèvre. 2020. "Middle East Respiratory Syndrome Coronavirus (MERS-CoV) Seropositive Camel Handlers in Kenya" Viruses 12, no. 4: 396. https://doi.org/10.3390/v12040396
APA StyleKiyong’a, A. N., Cook, E. A. J., Okba, N. M. A., Kivali, V., Reusken, C., Haagmans, B. L., & Fèvre, E. M. (2020). Middle East Respiratory Syndrome Coronavirus (MERS-CoV) Seropositive Camel Handlers in Kenya. Viruses, 12(4), 396. https://doi.org/10.3390/v12040396





