Bovine Ephemeral Fever in Asia: Recent Status and Research Gaps
Abstract
1. Introduction
2. Bovine Ephemeral Fever Virus and Its Susceptible Species
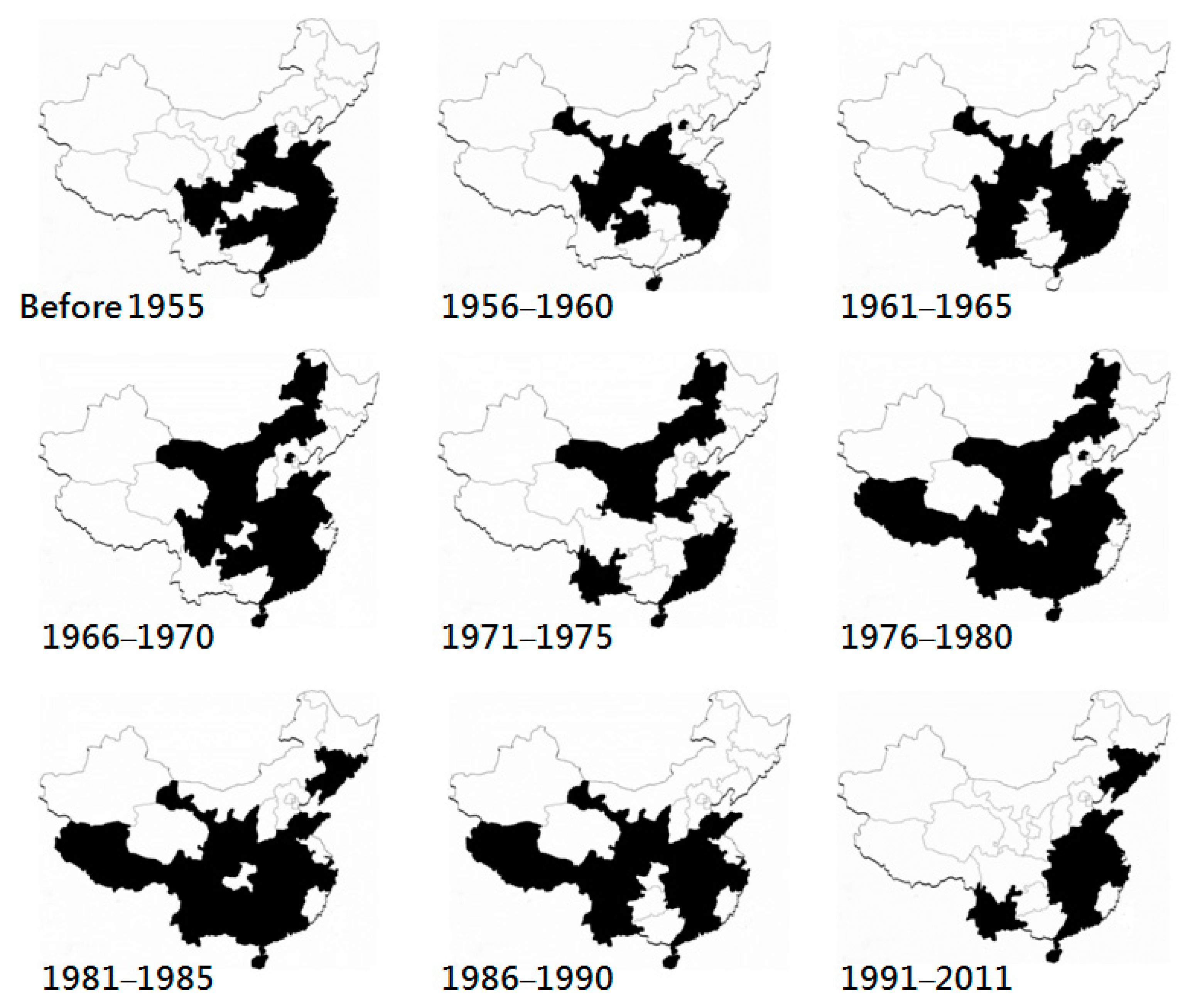
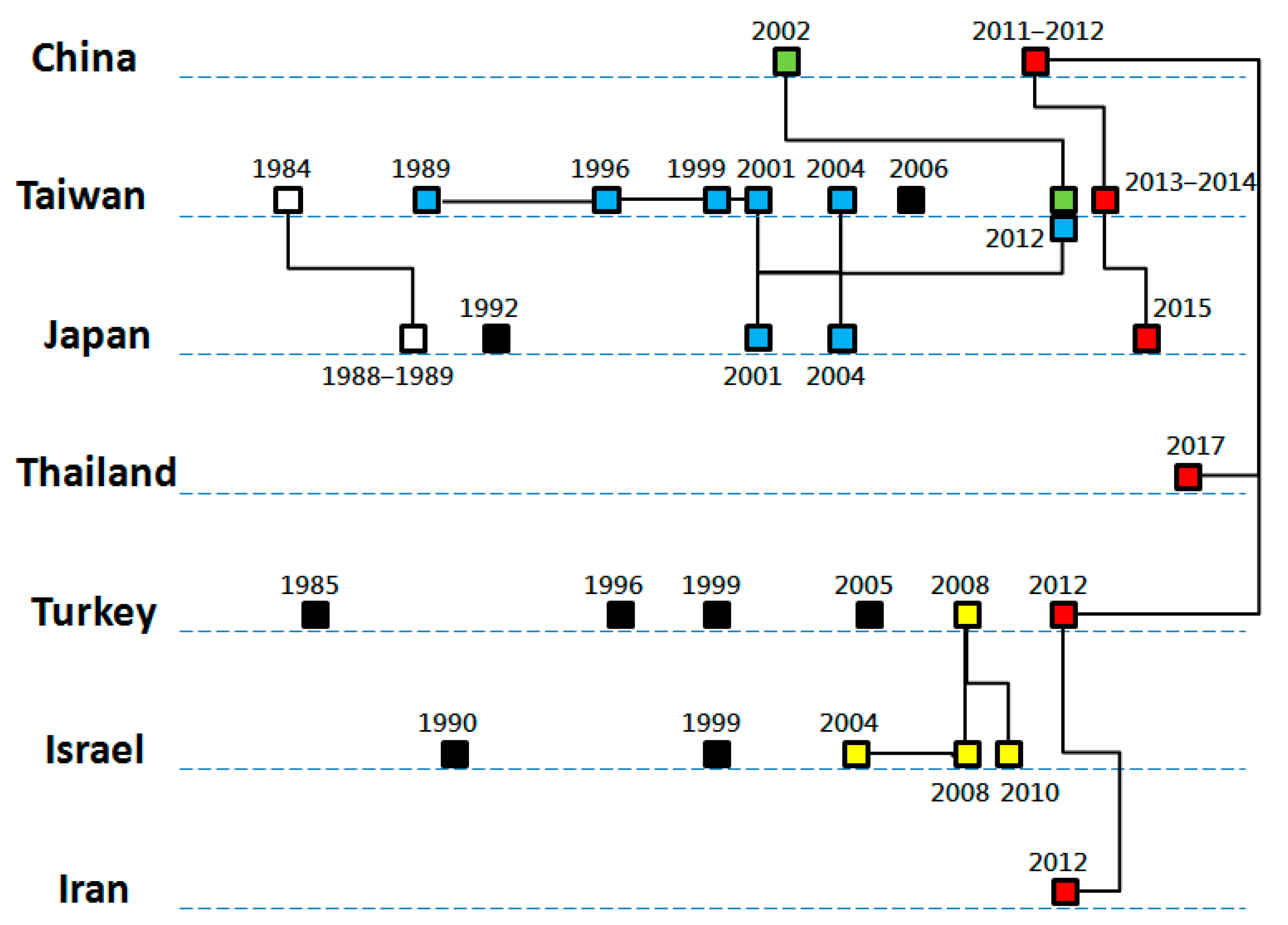
3. History and Geographical Distribution
3.1. Eastern Asia
3.2. South and Southeastern Asia
3.3. Middle East
4. Relationships between Epidemics
5. Vectors
6. Discussion
7. Conclusions
Conflicts of Interest
References
- Akakpo, A.J. Three-day fever. Rev. Sci. Tech. 2015, 34, 533–538. [Google Scholar] [PubMed]
- Inaba, Y.; Tanaka, Y.; Omori, T.; Matumoto, M. Serological relation between bovine epizootic fever and ephemeral fever. Japan J. Microbiol. 1969, 13, 129–130. [Google Scholar] [CrossRef]
- Walker, P.J. Bovine ephemeral fever in Australia and the world. Curr. Top. Microbiol. Immunol. 2005, 292, 57–80. [Google Scholar] [PubMed]
- Momtaz, H.; Nejat, S.; Moazeni, M.; Riahi, M. Molecular epidemiology of bovine ephemeral fever virus in cattle and buffaloes in Iran. Rev. Méd. Vét. 2012, 8–9, 415–418. [Google Scholar]
- Zaghawa, A.; Housawi, F.M.T.; Al-Naeem, A.; Al-Nakhly, H.; Kamr, A.; Toribio, R. Risk analysis and seroprevalence of bovine ephemeral fever virus in cattle in the Kingdom of Saudi Arabia. Trop. Anim. Health Prod. 2016, 48, 487–492. [Google Scholar] [CrossRef]
- Liu, D.; Zhang, L.; Li, K.; Han, Z.; Wang, X.; Zhang, H.; Li, J. Seroprevalence investigation of bovine ephemeral fever in yaks from Tibetan region of 2015. Dairy Health 2016, 317, 24–26. [Google Scholar]
- Holmes, I.H.; Doherty, R.L. Morphology and development of bovine ephemeral fever virus. J. Virol. 1970, 5, 91–96. [Google Scholar] [PubMed]
- Murphy, F.A.; Taylor, W.P.; Mims, C.A.; Whitfield, S.G. Bovine ephemeral fever virus in cell culture and mice. Arch. Gesamte Virusforsch 1972, 38, 234–249. [Google Scholar] [CrossRef] [PubMed]
- Liu, D.; Li, K.; Zhang, L.; Lan, Y.; Wang, X.; Zhang, H.; Wang, L.; Gui, R.; Han, Z.; Jang, W.; Sizhu, S.; Li, J. Seroprevalence investigation of bovine ephemeral fever in yaks in Tibetan Plateau of China from 2012 to 2015. Trop. Anim. Health Prod. 2017, 49, 227–230. [Google Scholar] [CrossRef] [PubMed]
- Davies, F.G.; Shaw, T.; Ochieng, P. Observations on the epidemiology of ephemeral fever in Kenya. J. Hyg. Camb. 1975, 75, 231–235. [Google Scholar] [CrossRef] [PubMed]
- Anderson, E.C.; Rowe, L.W. The prevalence of antibody to the viruses of bovine virus diarrhoea, bovine herpes virus 1, rift valley fever, ephemeral fever and bluetongue and to Leptospira sp in free-ranging wildlife in Zimbabwe. Epidemiol. Infect. 1998, 121, 441–449. [Google Scholar] [CrossRef] [PubMed]
- Van Vuuren, M.; Penzhorn, B.L. Geographic range of vector-borne infections and their vectors: The role of African wildlife. Rev. Sci. Tech. Off. Int. Epiz. 2015, 34, 139–149. [Google Scholar] [CrossRef]
- Tzipori, S.; Spradbrow, P.B. Development and behavior of a strain of bovine ephemeral fever virus with unusual hosts. J. Comp. Pathol. 1974, 84, 1–8. [Google Scholar] [CrossRef]
- Hall, W.T.; Daddow, K.N.; Dimmock, C.K.; St Goerge, T.D.; Standfast, H.A. The infection of Merino sheep with bovine ephemeral fever virus. Aust. Vet. J. 1975, 51, 344–346. [Google Scholar] [CrossRef]
- Lim, S.I.; Kweon, C.H.; Tark, D.S.; Kim, S.H.; Yang, D.K. Sero-survey on Aino, Akabane, Chuzan, bovine ephemeral fever, and Japanese encephalitis virus of cattle and swine in Korea. J. Vet. Sci. 2007, 8, 45–49. [Google Scholar] [CrossRef]
- Sato, K. A history of bovine influenza in Japan. J. Japan. Soc. Vet. Hist. 2016, 53, 14–23. (In Japanese) [Google Scholar]
- Inaba, Y.; Kurogi, H.; Sato, K.; Goto, Y.; Omori, T.; Matumoto, M. Formalin-inactivated, aluminum phosphate gel-adsorbed vaccine of bovine ephemeral fever virus. Arch. Gesamte Virusforsch. 1973, 42, 42–53. [Google Scholar] [CrossRef] [PubMed]
- Hirashima, Y.; Nojiri, M.; Ohtsuka, Y.; Kato, T.; Shirafuji, H.; Kurazono, M.; Imafuji, T.; Yanase, T. Resurgence of bovine ephemeral fever in mainland Japan in 2015 after a 23-year absence. J. Vet. Med. Sci. 2017, 79, 9047–9911. [Google Scholar] [CrossRef]
- Bai, W.B.; Jiang, C.L.; Davis, S.S. Preliminary observations on the epidemiology of bovine ephemeral fever in China. Trop. Anim. Health Prod. 1991, 23, 22–26. [Google Scholar]
- Wang, F.I.; Hsu, A.M.; Huang, K.J. Bovine ephemeral fever in Taiwan. J. Vet. Diagn. Invest. 2001, 13, 462–467. [Google Scholar] [CrossRef]
- Zheng, F.; Qiu, C. Phylogenetic relationships of the glycoprotein gene of bovine ephemeral fever virus isolated from mainland China, Taiwan, Japan, Turkey, Israel and Australia. Virol. J. 2012, 9, 268. [Google Scholar] [CrossRef]
- Tian, L.K.; Li, J.P. Treatment of bovine ephemeral fever. Heilongjiang Anim. Sci. Vet. Med. 2005, 2, 76. (In Chinese) [Google Scholar]
- Nuerbahat, N.; Zhang, T.; Liu, S.; Ding, M.; Jin, H.; Chen, Y.; Zhang, Y.; Gu, W. An epidemiological investigation of three important arbovirus diseases in some areas of Xingjiang cattle. Grass-Feed. Livest. 2018, 4, 59–62. (In Chinese) [Google Scholar]
- Li, Z.; Zheng, F.; Gao, S.; Wang, S.; Wang, J.; Liu, Z.; Du, J.; Yin, H. Large-scale serological survey of bovine ephemeral fever in China. Vet. Microbiol. 2015, 176, 155–160. [Google Scholar] [CrossRef]
- Yang, D.; Yang, M.S.; Rhim, H.; Han, J.I.; Oem, J.K.; Kim, Y.H.; Lee, K.K.; Lim, C.W.; Kim, B. Analysis of five arboviruses and Culicoides distribution on cattle farms in Jeollabuk-do, Korea. Korean J. Parasitol. 2018, 56, 477–485. [Google Scholar] [CrossRef]
- Ting, L.J.; Lee, M.S.; Lin, Y.L.; Cheng, M.C.; Lee, F. Invasion of exotic bovine ephemeral fever virus into Taiwan in 2013–2014. Vet. Microbiol. 2016, 182, 15–17. [Google Scholar] [CrossRef]
- Daniels, P.W.; Sendow, I.; Soleha, E.; Sukarsih; Hunt, N.T.; Bahri, S. Australian-Indonesia collaboration in veterinary arbovirology-a review. Vet. Microbiol. 1995, 46, 151–174. [Google Scholar] [CrossRef]
- Chaisirirat, T.; Sangthong, P.; Arunvipas, P.; Petcharat, N.; Thangthamniyom, N.; Chumsing, W.; Lekcharoensuk, P. Molecular characterization of bovine ephemeral fever virus in Thailand between 2013 and 2017. Vet. Microbiol. 2018, 227, 1–7. [Google Scholar] [CrossRef]
- Lapira, J.E.E.; Balbin, M.M.; Belotindos, L.P.; Viloria, V.V.; Abes, N.S.; Mingala, C.N. Molecular detection of ephemeral fever virus among large ruminants in the Philippines. Virus Dis. 2018, 29, 400–404. [Google Scholar] [CrossRef] [PubMed]
- Bakhshesh, M.; Abdollahi, D. Bovine ephemeral fever in Iran: Diagnosis, isolation and molecular characterization. J. Arthropod-Borne Dis. 2015, 9, 195–203. [Google Scholar]
- Yeruham, I.; Ham, M.V.; Stram, Y.; Friedgut, O.; Yadin, H.; Mumcuoglu, K.Y.; Braverman, Y. Epidemiological investigation of bovine ephemeral fever outbreaks in Israel. Vet. Med. Int. 2010, 290541. [Google Scholar] [CrossRef] [PubMed]
- Abu Elzein, E.M.; Gameel, A.A.; al-Afaleq, A.I.; al-Gundi, O.; al-Bashier, A.M.; Zeedan, A.; al-Mageed, H.A.; Abu Khadra, H. Obervations on the recent epizootic of bovine ephemeral fever in Saudi Arabia. Rev. Sci. Tech. 1999, 18, 672–680. [Google Scholar] [CrossRef]
- Alkan, F.; Albayrak, H.; Timurkan, M.O.; Ozan, E.; Coskun, N. Assessment of the molecular epidemiology of bovine ephemeral fever in Turkey. Vet. Arch. 2017, 87, 665–675. [Google Scholar] [CrossRef]
- Aziz-Boaron, O.; Klausner, Z.; Hasoksuz, M.; Shenkar, J.; Gafni, O.; Gelman, B.; David, D.; Klement, E. Circulation of bovine ephemeral fever in the Middle East-Strong evidence for transmission by winds and animal transport. Vet. Microbiol. 2012, 158, 300–307. [Google Scholar] [CrossRef]
- Hazrati, A.; Hessami, M.; Roustai, M.; Dayhim, F. Isolation of bovine ephemeral fever virus in Iran. Arch. Razi Inst. 1975, 27, 80–81. [Google Scholar]
- Bazargani, T.T.; Movassaghi, A.R.; Bahonar, A.R.; Hassan, E.B.; Hemmatzadeh, F.; Khedmati, K. Identification of bovine ephemeral fever (BEF) outbreak in a large dairy farm in Varamin, Iran. Iran. J. Vet. Sci. Tech. 2013, 5, 35–44. [Google Scholar]
- Mirzaie, K.; Bahonar, A.; Mehrabadi, M.F.; Hajilu, G.; Yoghoubi, M. Determinants of bovine ephemeral fever outbreak during 2013, in Qazvin Province, Iran. Asian Pac. J. Trop. Dis. 2017, 7, 744–747. [Google Scholar] [CrossRef]
- Al-Sultany, H.A.O.; Hassan, I.Q. Molecular investigation of bovine ephemeral fever in Iraq. Mirror Res. Vet. Sci. Anim. 2013, 2, 42–50. [Google Scholar]
- Trinidad, L.; Blasdell, K.R.; Albert Joubert, D.; Davis, S.S.; Melville, L.; Kirkland, P.D.; Coulibaly, F.; Holmes, E.C.; Walker, P.J. Evolution of bovine ephemeral fever viruses in the Australian episystem. J. Virol. 2014, 88, 1525–1535. [Google Scholar] [CrossRef]
- Abu-Elzein, E.M.E.; Al-Afaleq, A.I.; Housawi, F.M.T.; Al-Basheir, A.M. A study on bovine ephemeral fever involving sentinel herds ans serosurveillance in Saudi Arabia. Rev. Sci. Tech. Off. Int. Epiz. 2006, 25, 1147–1151. [Google Scholar]
- Abu Elzein, E.M.E.; Gameel, A.A.; Al Afaleq, A.I.; Al Gundi, O.; Bukhari, A. Bovine ephemeral fever in Saudi Arabia. Vet. Rec. 1997, 140, 630–631. [Google Scholar] [CrossRef] [PubMed]
- Tonbak, S.; Berber, E.; Yoruk, M.D.; Azkur, A.K.; Pestil, Z.; Bulut, H. A large-scale outbreak of bovine ephemrqal fever in Turkey, 2012. J. Vet. Med. Sci. 2013, 75, 1511–1514. [Google Scholar] [CrossRef] [PubMed]
- Nabila, S.N.; Hassan, H.Y.; El-Sanousi, A.A.; Salem, S.A.; Beshir, E.; Hanan, A.E. Recent trials for diagnosis of bovine ephemeral fever in Egypt. Animal hygiene and sustainable livestock production. In Proceedings of the XVth International Congress of the International Society for Animal Hygiene, Vienna, Austria, 3–7 July 2011. [Google Scholar]
- Mahmoud, A. Comparative sequence analysis and epitope prediction of the partial glycoprotein G gene of bovine ephemeral fever virus isolate in Egypt. Egypt. J. Virol. 2012, 9, 49–60. [Google Scholar]
- Ibrahim, M.M.; Amany, E.Z.; Christine, A.M.; Soliman, Y.A. Further evaluation of locally prepared live attenuated bovine ephemeral fever vaccine in cattle. J. Vet. Med. Res. 2017, 24, 339–348. [Google Scholar]
- St George, T.D. Bovine ephemeral fever: A review. Trop. Anim. Health Prod. 1988, 20, 194–202. [Google Scholar] [CrossRef]
- Shirakawa, H.; Ishibashi, K.; Ogawa, T. A comparison of the epidemiology of bovine ephemeral fever in South Korea and south-western Japan. Aust. Vet. J. 1994, 71, 50–52. [Google Scholar] [CrossRef]
- Melville, L.; Weir, R.; Hunt, N.; Davis, S.; Walsh, S. Forty years continous monitoring for bluetongue virus at an Australian site of high arbovirus activity. What have we achieved? Vet. Ital. 2015, 51, 263–267. [Google Scholar] [PubMed]
- Seddon, H.R. The spread of ephemeral fever (three-day sickness) in Australia in 1936–1937. Aus. Vet. J. 1938, 14, 90–101. [Google Scholar] [CrossRef]
- Standfast, H.A.; Dyce, A.L.; St George, T.D.; Muller, M.J.; Doherty, R.L.; Carley, J.G.; Filippich, C. Isolation of arboviruses from insects collected at Beatrice Hill, Northern Territory of Australia. Aust. J. Biol. Sci. 1984, 37, 351–366. [Google Scholar] [CrossRef]
- Doherty, R.L.; Carley, J.G.; Standfast, H.A.; Dyce, A.L.; Snowdon, W.A. Virus strains isolated from arthropods during an epizootic of bovine ephemeral fever in Queensland. Aust. Vet. J. 1972, 48, 81–86. [Google Scholar] [CrossRef]
- Davies, F.G.; Walker, A.R. The isolation of ephemeral fever virus from cattle and Culicoides midges in Kenya. Vet. Rec. 1974, 95, 63–64. [Google Scholar] [CrossRef]
- Uren, M.F.; St George, T.D.; Kirkland, P.D.; Stranger, R.S.; Murray, M.D. Epidemiology of bovine ephemeral fever in Australian 1981–1985. Aust. J. Biol. Sci. 1987, 40, 125–136. [Google Scholar] [CrossRef]
- Blackburn, N.K.; Searle, L.; Phelps, R.J. Viruses isolated from Culicoides (Dipt.: Cerat.) caught at the Veterinary Research Farm, Mazowe, Zimbabwe. J. Entomol. Soc. S. Afr. 1985, 48, 331–336. [Google Scholar]
- Kay, B.H.; Carley, J.G.; Filippich, C. The multiplication of Queensland and New Guinean arboviruses in Culex annulirostris (Skuse) (Diptera: Culicidae). J. Med. Entomol. 1975, 12, 279–283. [Google Scholar] [CrossRef]
- Beef2Live. Available online: http://beef2live.com/story-world-cattle-inventory-ranking-countries-0 -106905 (accessed on 10 March 2019).
- Wilson, A.J.; Mellor, P.S. Bluetongue in Europe: Past, present and future. Phil. Trans. R. Soc. B 2009, 364, 2669–2681. [Google Scholar] [CrossRef]
- Hsieh, Y.C.; Chen, S.H.; Chou, C.C.; Ting, L.J.; Itakura, C.; Wang, F.I. Bovine ephemeral fever in Taiwan (2001–2002). J. Vet. Med. Sci. 2005, 67, 411–416. [Google Scholar] [CrossRef] [PubMed]
- Carpenter, S.; Mellor, P.S.; Torr, S.J. Control techniques for Culicoides biting midges and their application in the U. K. and northwestern Palaearctic. Med. Vet. Entomol. 2008, 22, 175–187. [Google Scholar] [CrossRef]
- Nayduch, D.; Lee, M.B.; Saski, C.A. The reference transcriptome of the adult female biting midge (Culicoides sonorensis) and differential expression profiling during teneral, blood, and sucrose feeding conditions. PLoS ONE 2014, 9, e98123. [Google Scholar] [CrossRef] [PubMed]
- Nayduch, D.; Erram, D.; Lee, M.B.; Zurek, L.; Saski, C.A. Impact of the blood meal on humoral immunity and microbiota in the gut of the female Culicoides sonorensis. Vet. Ital. 2015, 51, 385–392. [Google Scholar]
- Morii, T.; Kitaoka, S. The laboratory colonization of Culicoides arakawae (Diptera: Ceratopogonidae). Natl. Inst. Anim. Health Quart. 1968, 8, 26–30. [Google Scholar]
- Lien, J.C.; Peng, H.K. Laboratory colonization of Culicoides arakawae. Chin. J. Entomol. 1989, 9, 211–216. [Google Scholar]
- Yu, C.Y.; Chang, V.S.; Wang, J.S. Improvement of culture effect of Leucocytozoon caulleryi and Culicoides arakawae. Taiwan Vet. J. 2006, 32, 129–135. [Google Scholar]
- Li, G.; Qin, Z.; Lin, H.; Weng, Y.; Zhu, J. Colonization of Culicoides arakawae in laboratory. Acta Vet. Zootech. Sin. 2001, 32, 525–529. (In Chinese) [Google Scholar]
- Ronderos, M.M.; Diaz, F. Rearing Culicoides bambusicola (Lutz, 1913) (Diptera: Ceratopogonidae) in laboratory. Obsevations and new records. Bio. Mus. Nac. Histo. Nat. Parag. 2002, 14, 43–48. [Google Scholar]
- Koch, H.G.; Axtell, R.C. Autogeny and rearing of C. furens, C. hollensis and C. melleus (Diptera: Ceratopogonidae) from coastal North Carolina. Mosquito News 1978, 38, 240–244. [Google Scholar]
- Gazeau, L.J.; Messersmith, D.H. Rearing and distribution of Maryland Culicoides (Depteria: Ceratopogonidae). Mosquito News. 1970, 30, 30–34. [Google Scholar]
- Megahed, M.M. A culture method for Culicoides nubeculosus (Meigen) (Diptera: Ceratopogonidae) in the laboratory, with notes on the biology. Bull. Entomol. Res. 1956, 47, 107–114. [Google Scholar] [CrossRef]
- Fahrner, J.; Barthelmess, C. Rearing Culicoides nubeculosus (Diptera: Ceratopogonidae) by natural or artificial feeding in the laboratory. Vet. Parasitol. 1988, 28, 307–313. [Google Scholar] [CrossRef]
- Harsha, R.; Mazumdar, A. Laboratory rearing of immature Culicoides peregrines Kieffer, a potential vector of bluetongue virus. Med. Vet. Entomol. 2015, 29, 434–438. [Google Scholar] [CrossRef]
- Hunt, G.J. A Procedural Manual for the Large-Scale Rearing of the Biting Midge, Culicoides Variipennis (Deptera: Ceratopogonidae); United States Department of Agriculture: Washington, DC, USA, 1994; pp. 4–22.
- Carpenter, S.; Veronesi, E.; Mullens, B.; Venter, G. Vecter competence of Culicoids for arboviruses: Three major periods of research, their influence on current studies and future direction. Rev. Sci. Tech. Off. Int. Epiz. 2015, 34, 97–112. [Google Scholar] [CrossRef]
- Tuffereau, C.; Leblois, H.; Benejean, J.; Coulon, P.; Lafay, F.; Flamand, A. Arginine or lysine in position 333 of ERA and CVS glycoprotein in necessary for rabies virulence in adult mice. Virology 1989, 172, 206–212. [Google Scholar] [CrossRef]
- Morimoto, K.; Foley, H.D.; McGettigan, J.P.; Schnell, M.J.; Dietzscholld, B. Reinvestigation of the role of the rabies virus glycoprotein in viral pathogenesis using a reverse genetics approach. J. Neurovirol. 2000, 6, 373–381. [Google Scholar] [CrossRef] [PubMed]
- Faber, M.; Faber, M.L.; Papaneri, A.; Bette, M.; Weihe, E.; Dietzscholld, B.; Schnell, M.J. A single amino acid change in rabies virus glycoprotein increases virus spread and enhances virus pathogenicity. J. Virol. 2005, 79, 14141–14148. [Google Scholar] [CrossRef] [PubMed]
- Kato, T.; Aizawa, M.; Takayoshi, K.; Kokuba, T.; Yanase, T.; Shirafuji, H.; Tsuda, T.; Yamakawa, M. Phylogenetic relationships of the G gene sequence of bovine ephemeral fever virus isolated in Japan, Taiwan and Australia. Vet. Microbiol. 2009, 137, 217–223. [Google Scholar] [CrossRef]
- Braverman, Y.; Chechik, F. Air streams and the introduction of animal diseases borne on Culicoides (Deptera: Ceratopogonidae) into Israel. Rev. Sci. Tech. Off. Int. Epiz. 1996, 15, 1037–1052. [Google Scholar] [CrossRef]
- Jacquet, S.; Huber, K.; Pages, N.; Talavera, S.; Burgin, L.E.; Carpenter, S.; Sanders, C.; Dicko, A.H.; Djerbal, M.; Goffredo, M.; et al. Range expansion of the bluetongue virus vector, Culicoides imicola, in continental France likely due to rare win-transport events. Sci. Rep. 2016, 6, 21247. [Google Scholar] [CrossRef] [PubMed]
- McGrath, G.; More, S.J.; O’Neill, R. Hypothetical route of the introduction of Schmallenberg virus into Ireland using two complementary analyses. Vet. Rec. 2017. [CrossRef] [PubMed]
- Nie, W.; Bo, J.; Liu, E.; Yu, Y. The imported living midges and a new species Brachypogon (Isohelea) edelweiss commected on an entry ship. Chin. J. Hyg. Insect Equip. 2015, 21, 618–619. (In Chinese) [Google Scholar]
- Himeidan, Y.E.; Kweka, E.J.; Mahgoub, M.M.; El Rayah, E.A.; Ouma, J.O. Ecent outbreaks of Rift Valley fever in East Africa and the Middle East. Front. Pub. Health 2014, 2, 169. [Google Scholar] [CrossRef]
- Qiu, Y.; Abila, R.; Rodtian, P.; King, P.D.; Knowles, N.J.; Ngo, L.T.; Le, V.T.; Khounsy, S.; Bounma, P.; Lwin, S.; et al. Emergence of an exotic strain of serotype O foot-and-mouth disease virus O/ME-SA/Ind-2001d in South-East Asia in 2015. Transbound. Emerg. Dis. 2017, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Di Nardo, A.; Knowles, N.J.; Paton, D.J. Combining live stock trade patterns and phylogenetics to help understand the spread of foot and mouth disease in sub-Saharan Africa, the Middle East and the Southeast Asia. Rev. Sci. Tech. Off. Int. Opiz. 2011, 30, 63–85. [Google Scholar] [CrossRef]
- Hindustan Times. Cross-Border Arms, Cattle, Narcotics Smuggling Cases Rose over 3 Years: Data till 2017. Available online: https://www.hindustantimes.com/india-news/cross-border-arms-cattle-narcotics-smuggling-cases-rose-over-3-years-data-till-2017/story-DIptEAJVkJRc8CPykk232O.html (accessed on 15 March 2019).
| Insect | Place/Year of Sampling | Methods | References |
|---|---|---|---|
| Mosquitoes: | |||
| Anopleles bancroftii | Australia/1974–1976 | Virus isolation | [50] |
| Culex annulirostris | Australia/1968 | Virus isolation | [51] |
| Biting midges: | |||
| Culicoides arakawae | Korea/2016–2017 | RT-PCR | [25] |
| Culicoides bedfordi | Kenya/1972–1973 | Virus isolation | [52] |
| Culicoides brevitarsis | Australia/1984 | Virus isolation | [51,53] |
| Culicoides coarctatus | Zimbabwe | Virus isolation | [54] |
| Culicoides cornutus | Kenya/1972–1973 | Virus isolation | [52] |
| Culicoides kingi | Kenya/1972–1973 | Virus isolation | [52] |
| Culicoides imicola | Kenya/1972–1973 | Virus isolation | [52] |
| Culicoides nivosus | Kenya/1972–1973 | Virus isolation | [52] |
| Year | Country | Morbidity (%) | Case Fatality (%) | References |
|---|---|---|---|---|
| 1967 | Taiwan | 26.6 | 5.2 | [58] |
| 1983–1984 | Taiwan | 20.1 | 6.0 | [58] |
| 1989–1990 | Taiwan | 14.5 | 5.0 | [58] |
| 1990 | Israel | 8.3–20.0 | 2.0 | [31] |
| 1996 | Saudi Arabia | 59 | >1.0 | [41] |
| 1996 | Taiwan | 13.6 | 11.3 | [58] |
| 1999 | Taiwan | 5.6 | 21.9 | [58] |
| 1999 | Israel | 5.4–38.7 | 8.6–28.0 | [31] |
| 2001 | Taiwan | 7.4 | 9.7 | [58] |
| 2001 | Taiwan | 15.0 | 50.0 | [58] |
| 2004 | Israel | 14.9–22.2 | 3.5–5.4 | [31] |
| Before 2000 | China | 10.0–20.0 | >1.0 | [21] |
| 2011 | China | 30.0 | 5.0 | [21] |
| 2012 | Turkey | 35.0 | 15.0–20.0 | [42] |
| 2013 | Iran | 17.0 | 25.8 | [37] |
| 2015 | Japan | 28.9 | 0.0 | [18] |
© 2019 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, F. Bovine Ephemeral Fever in Asia: Recent Status and Research Gaps. Viruses 2019, 11, 412. https://doi.org/10.3390/v11050412
Lee F. Bovine Ephemeral Fever in Asia: Recent Status and Research Gaps. Viruses. 2019; 11(5):412. https://doi.org/10.3390/v11050412
Chicago/Turabian StyleLee, Fan. 2019. "Bovine Ephemeral Fever in Asia: Recent Status and Research Gaps" Viruses 11, no. 5: 412. https://doi.org/10.3390/v11050412
APA StyleLee, F. (2019). Bovine Ephemeral Fever in Asia: Recent Status and Research Gaps. Viruses, 11(5), 412. https://doi.org/10.3390/v11050412




