Utilisation of Chimeric Lyssaviruses to Assess Vaccine Protection against Highly Divergent Lyssaviruses
Abstract
1. Introduction
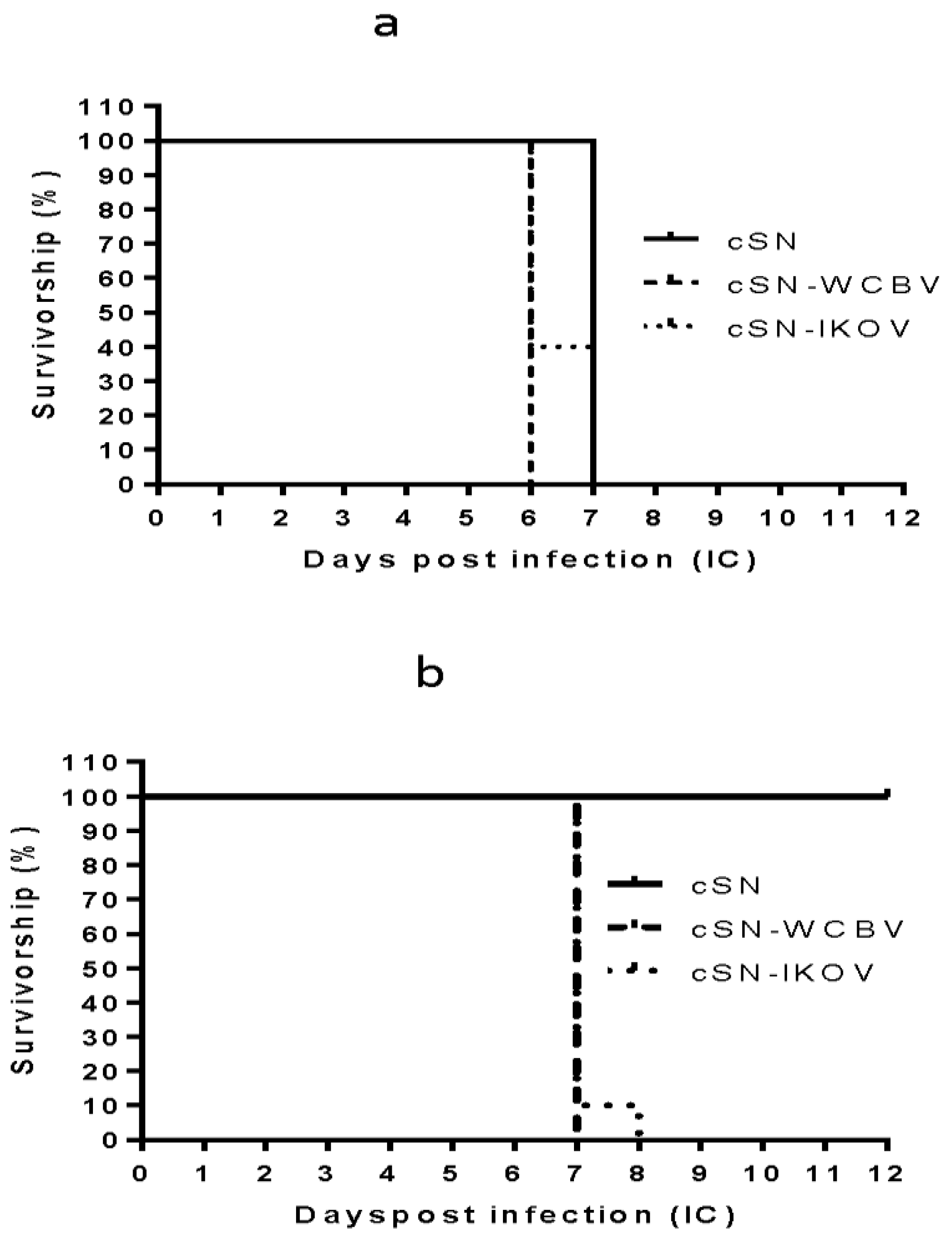
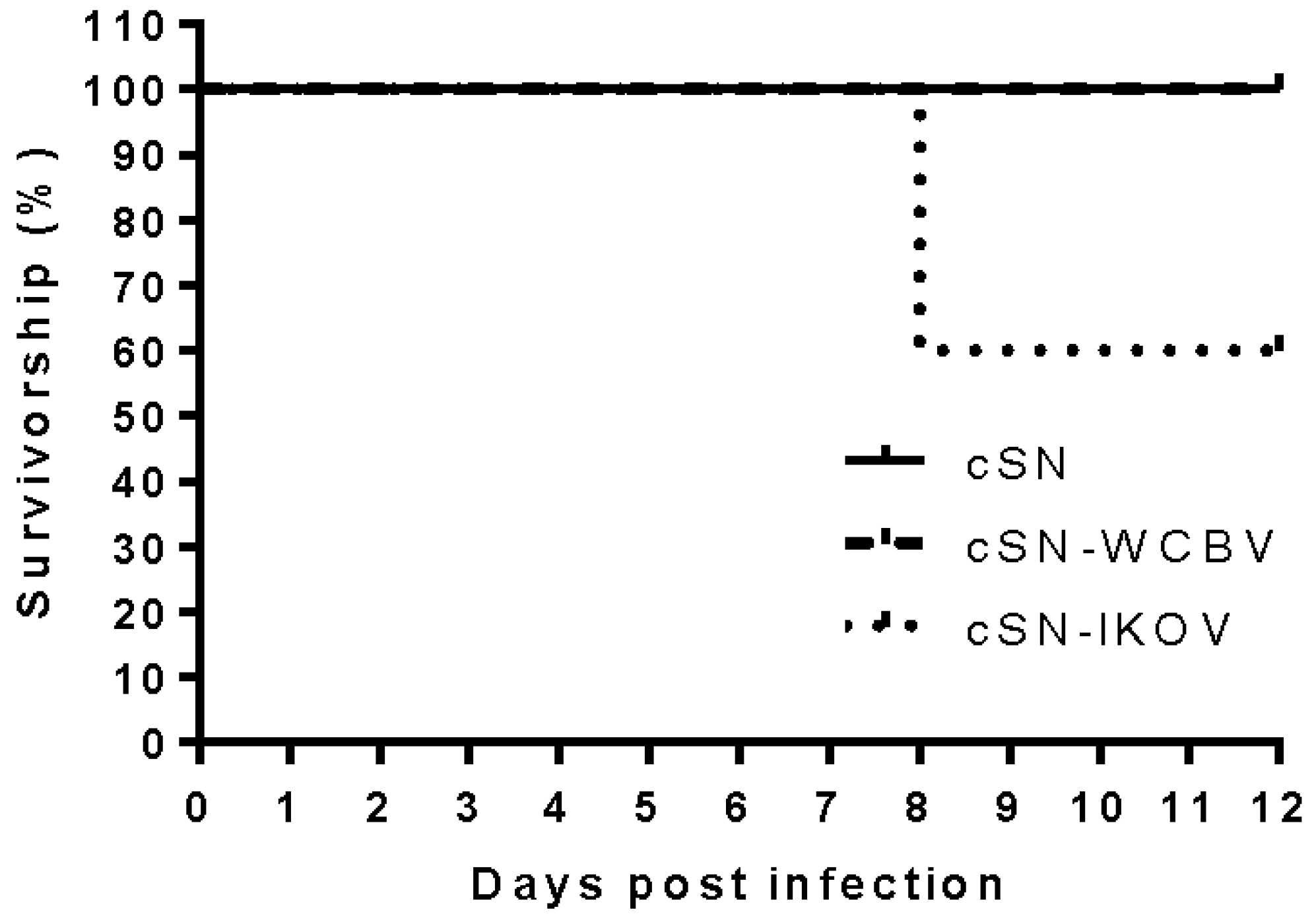
2. Materials and Methods
2.1. Full Length Plasmid Construction
2.2. Virus Rescue, Titration, and Growth Curves
2.3. In Vivo Experimentation
2.4. Serology
3. Results
4. Discussion
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Fooks, A.R.; Banyard, A.C.; Horton, D.L.; Johnson, N.; McElhinney, L.M.; Jackson, A.C. Current status of rabies and prospects for elimination. Lancet 2014, 384, 1389–1399. [Google Scholar] [CrossRef]
- Hampson, K.; Coudeville, L.; Lembo, T.; Sambo, M.; Kieffer, A.; Attlan, M.; Barrat, J.; Blanton, J.D.; Briggs, D.J.; Cleaveland, S.; et al. Estimating the global burden of endemic canine rabies. PLoS Negl. Trop. Dis. 2015, 9, e0003709. [Google Scholar]
- Banyard, A.C.; Horton, D.; Freuling, C.; Müller, T.; Fooks, A.R. Control and prevention of canine rabies: The need for building laboratory based surveillance capacity. Antivir. Res. 2013, 98, 357–364. [Google Scholar] [CrossRef] [PubMed]
- Mani, R.S.; Anand, A.M.; Madhusudana, S.N. Human rabies in India: An audit from a rabies diagnostic laboratory. Trop. Med. Int. Health 2016, 21, 556–563. [Google Scholar] [CrossRef] [PubMed]
- Rupprecht, C.; Kuzmin, I.; Meslin, F. Lyssaviruses and rabies: Current conundrums, concerns, contradictions and controversies. F1000Res. 2017, 6. [Google Scholar] [CrossRef] [PubMed]
- Banyard, A.C.; Fooks, A.R. The impact of novel lyssavirus discovery. Microbiol. Aust. 2017, 38, 18–21. [Google Scholar] [CrossRef]
- Banyard, A.C.; Evans, J.S.; Luo, T.R.; Fooks, A.R. Lyssaviruses and bats: Emergence and zoonotic threat. Viruses 2014, 6, 2974–2990. [Google Scholar] [CrossRef] [PubMed]
- Streicker, D.G.; Turmelle, A.S.; Vonhof, M.J.; Kuzmin, I.V.; McCracken, G.F.; Rupprecht, C.E. Host phylogeny constrains cross-species emergence and establishment of rabies virus in bats. Science 2010, 329, 676–679. [Google Scholar] [CrossRef] [PubMed]
- Moore, S.M.; Hanlon, C.A. Rabies-specific antibodies: Measuring surrogates of protection against a fatal disease. PLoS Negl. Trop. Dis. 2010, 4, e595. [Google Scholar] [CrossRef] [PubMed]
- Hanlon, C.A.; Kuzmin, I.V.; Blanton, J.D.; Weldon, W.C.; Manangan, J.S.; Rupprecht, C.E. Efficacy of rabies biologics against new lyssaviruses from Eurasia. Virus Res. 2005, 111, 44–54. [Google Scholar] [CrossRef] [PubMed]
- Brookes, S.M.; Healy, D.M.; Fooks, A.R. Ability of rabies vaccine strains to elicit cross-neutralising antibodies. Dev. Biol. (Basel) 2006, 125, 185–193. [Google Scholar] [PubMed]
- Badrane, H.; Bahloul, C.; Perrin, P.; Tordo, N. Evidence of two Lyssavirus phylogroups with distinct pathogenicity and immunogenicity. J. Virol. 2001, 75, 3268–3276. [Google Scholar] [CrossRef] [PubMed]
- Nolden, T.; Banyard, A.C.; Finke, S.; Fooks, A.R.; Hanke, D.; Hoper, D.; Horton, D.L.; Mettenleiter, T.C.; Muller, T.; Teifke, J.P.; et al. Comparative studies on the genetic, antigenic and pathogenic characteristics of Bokeloh bat lyssavirus. J. Gen. Virol. 2014, 95, 1647–1653. [Google Scholar] [CrossRef] [PubMed]
- Fekadu, M.; Shaddock, J.H.; Sanderlin, D.W.; Smith, J.S. Efficacy of rabies vaccines against Duvenhage virus isolated from European house bats (Eptesicus serotinus), classic rabies and rabies-related viruses. Vaccine 1988, 6, 533–539. [Google Scholar] [CrossRef]
- Kuzmin, I.V.; Niezgoda, M.; Franka, R.; Agwanda, B.; Markotter, W.; Beagley, J.C.; Urazova, O.Y.; Breiman, R.F.; Rupprecht, C.E. Possible emergence of West Caucasian bat virus in Africa. Emerg. Infect. Dis. 2008, 14, 1887–1889. [Google Scholar] [CrossRef] [PubMed]
- Arechiga Ceballos, N.; Vazquez Moron, S.; Berciano, J.M.; Nicolas, O.; Aznar Lopez, C.; Juste, J.; Rodriguez Nevado, C.; Aguilar Setien, A.; Echevarria, J.E. Novel lyssavirus in bat, Spain. Emerg. Infect. Dis. 2013, 19, 793–795. [Google Scholar] [CrossRef] [PubMed]
- Horton, D.L.; Banyard, A.C.; Marston, D.A.; Wise, E.; Selden, D.; Nunez, A.; Hicks, D.; Lembo, T.; Cleaveland, S.; Peel, A.J.; et al. Antigenic and genetic characterization of a divergent African virus, Ikoma lyssavirus. J. Gen. Virol. 2014, 95, 1025–1032. [Google Scholar] [CrossRef] [PubMed]
- Horton, D.L.; McElhinney, L.M.; Marston, D.A.; Wood, J.L.; Russell, C.A.; Lewis, N.; Kuzmin, I.V.; Fouchier, R.A.; Osterhaus, A.D.; Fooks, A.R.; et al. Quantifying antigenic relationships among the Lyssaviruses. J. Virol. 2010. [Google Scholar] [CrossRef] [PubMed]
- Gaudin, Y.; Ruigrok, R.W.; Tuffereau, C.; Knossow, M.; Flamand, A. Rabies virus glycoprotein is a trimer. Virology 1992, 187, 627–632. [Google Scholar] [CrossRef]
- Faber, M.; Pulmanausahakul, R.; Nagao, K.; Prosniak, M.; Rice, A.B.; Koprowski, H.; Schnell, M.J.; Dietzschold, B. Identification of viral genomic elements responsible for rabies virus neuroinvasiveness. Proc. Natl. Acad. Sci. USA 2004, 101, 16328–16332. [Google Scholar] [CrossRef] [PubMed]
- Marston, D.A.; McElhinney, L.M.; Banyard, A.C.; Horton, D.L.; Nunez, A.; Koser, M.L.; Schnell, M.J.; Fooks, A.R. Interspecies protein substitution to investigate the role of the lyssavirus glycoprotein. J. Gen. Virol. 2013, 94, 284–292. [Google Scholar] [CrossRef] [PubMed]
- McGettigan, J.P.; Foley, H.D.; Belyakov, I.M.; Berzofsky, J.A.; Pomerantz, R.J.; Schnell, M.J. Rabies virus-based vectors expressing human immunodeficiency virus type 1 (HIV-1) envelope protein induce a strong, cross-reactive cytotoxic T-lymphocyte response against envelope proteins from different HIV-1 isolates. J. Virol. 2001, 75, 4430–4434. [Google Scholar] [CrossRef] [PubMed]
- Morimoto, K.; Foley, H.D.; McGettigan, J.P.; Schnell, M.J.; Dietzschold, B. Reinvestigation of the role of the rabies virus glycoprotein in viral pathogenesis using a reverse genetics approach. J. Neurovirol. 2000, 6, 373–381. [Google Scholar] [CrossRef] [PubMed]
- Pulmanausahakul, R.; Li, J.; Schnell, M.J.; Dietzschold, B. The glycoprotein and the matrix protein of rabies virus affect pathogenicity by regulating viral replication and facilitating cell-to-cell spread. J. Virol. 2008, 82, 2330–2338. [Google Scholar] [CrossRef] [PubMed]
- Schnell, M.; Mebatsion, T.; Conzelmann, K.-K. Infectious rabies virus from cloned cDNA. EMBO J. 1994, 13, 4195–4203. [Google Scholar] [PubMed]
- Healy, D.M.; Brookes, S.M.; Banyard, A.C.; Nunez, A.; Cosby, S.L.; Fooks, A.R. Pathobiology of rabies virus and the European bat lyssaviruses in experimentally infected mice. Virus Res. 2013, 172, 46–53. [Google Scholar] [CrossRef] [PubMed]
- Wright, E.; Temperton, N.J.; Marston, D.A.; McElhinney, L.M.; Fooks, A.R.; Weiss, R.A. Investigating antibody neutralization of lyssaviruses using lentiviral pseudotypes: A cross-species comparison. J. Gen. Virol. 2008, 89, 2204–2213. [Google Scholar] [CrossRef] [PubMed]
- Winkler, W.G.; Fashinell, T.R.; Leffingwell, L.; Howard, P.; Conomy, P. Airborne rabies transmission in a laboratory worker. JAMA 1973, 226, 1219–1221. [Google Scholar] [CrossRef] [PubMed]
- Basavaraju, S.V.; Kuehnert, M.J.; Zaki, S.R.; Sejvar, J.J. Encephalitis caused by pathogens transmitted through organ transplants, United States, 2002-2013. Emerg. Infect. Dis. 2014, 20, 1443. [Google Scholar] [CrossRef] [PubMed]
- Marston, D.A.; Ellis, R.; Wise, E.; Aréchiga-Ceballos, N.; Freuling, C.; Banyard, A.C.; McElhinney, L.M.; de Lamballerie, X.; Müller, T.; Fooks, A.R.; et al. Complete Genomic Sequence of Lleida bat Lyssavirus. Genome Announc. 2017, 5, e01427-16. [Google Scholar] [CrossRef] [PubMed]
- De Benedictis, P.; Minola, A.; Rota Nodari, E.; Aiello, R.; Zecchin, B.; Salomoni, A.; Foglierini, M.; Agatic, G.; Vanzetta, F.; Lavenir, R.; et al. Development of broad-spectrum human monoclonal antibodies for rabies post-exposure prophylaxis. EMBO Mol. Med. 2016, 8, 407–421. [Google Scholar] [CrossRef] [PubMed]
- Ghildyal, R.; Li, D.; Peroulis, I.; Shields, B.; Bardin, P.G.; Teng, M.N.; Collins, P.L.; Meanger, J.; Mills, J. Interaction between the respiratory syncytial virus G glycoprotein cytoplasmic domain and the matrix protein. J. Gen. Virol. 2005, 86, 1879–1884. [Google Scholar] [CrossRef] [PubMed]
- Enami, M.; Enami, K. Influenza virus hemagglutinin and neuraminidase glycoproteins stimulate the membrane association of the matrix protein. J. Virol. 1996, 70, 6653–6657. [Google Scholar] [PubMed]
- Lyles, D.S.; McKenzie, M.; Parce, J.W. Subunit interactions of vesicular stomatitis virus envelope glycoprotein stabilized by binding to viral matrix protein. J. Virol. 1992, 66, 349–358. [Google Scholar] [PubMed]
- Mebatsion, T.; Weiland, F.; Conzelmann, K.K. Matrix protein of rabies virus is responsible for the assembly and budding of bullet-shaped particles and interacts with the transmembrane spike glycoprotein G. J. Virol. 1999, 73, 242–250. [Google Scholar] [PubMed]
- Genz, B.; Nolden, T.; Negatsch, A.; Teifke, J.P.; Conzelmann, K.K.; Finke, S. Chimeric rabies viruses for trans-species comparison of lyssavirus glycoprotein ectodomain functions in virus replication and pathogenesis. Berl. Munch. Tierarztl. Wochenschr. 2012, 125, 219–227. [Google Scholar] [PubMed]
- Finke, S.; Conzelmann, K.K. Dissociation of rabies virus matrix protein functions in regulation of viral RNA synthesis and virus assembly. J. Virol. 2003, 77, 12074–12082. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, K.; Ito, N.; Mita, T.; Yamada, K.; Hosokawa-Muto, J.; Sugiyama, M.; Minamoto, N. Involvement of nucleoprotein, phosphoprotein, and matrix protein genes of rabies virus in virulence for adult mice. Virus Res. 2007, 123, 154–160. [Google Scholar] [CrossRef] [PubMed]
- Kuzmin, I.V.; Franka, R.; Rupprecht, C.E. Experimental infection of big brown bats (Eptesicus fuscus) with West Caucasian bat virus (WCBV). Dev. Biol. (Basel) 2008, 131, 327–337. [Google Scholar] [PubMed]
- Banyard, A.C.; Healy, D.M.; Brookes, S.M.; Voller, K.; Hicks, D.J.; Nunez, A.; Fooks, A.R. Lyssavirus infection: ‘low dose, multiple exposure’ in the mouse model. Virus Res. 2014, 181, 35–42. [Google Scholar] [CrossRef] [PubMed]
- Turmelle, A.S.; Jackson, F.R.; Green, D.; McCracken, G.F.; Rupprecht, C.E. Host immunity to repeated rabies virus infection in big brown bats. J. Gen. Virol. 2010, 91, 2360–2366. [Google Scholar] [CrossRef] [PubMed]
- Johnson, N.; Vos, A.; Neubert, L.; Freuling, C.; Mansfield, K.L.; Kaipf, I.; Denzinger, A.; Hicks, D.; Nunez, A.; Franka, R.; et al. Experimental study of European bat lyssavirus type-2 infection in Daubenton’s bats (Myotis daubentonii). J. Gen. Virol. 2008, 89, 2662–2672. [Google Scholar] [CrossRef] [PubMed]
- Freuling, C.; Vos, A.; Johnson, N.; Kaipf, I.; Denzinger, A.; Neubert, L.; Mansfield, K.; Hicks, D.; Nunez, A.; Tordo, N.; et al. Experimental infection of serotine bats (Eptesicus serotinus) with European bat lyssavirus type 1a. J. Gen. Virol. 2009, 90, 2493–2502. [Google Scholar] [CrossRef] [PubMed]
- Franka, R.; Johnson, N.; Muller, T.; Vos, A.; Neubert, L.; Freuling, C.; Rupprecht, C.E.; Fooks, A.R. Susceptibility of North American big brown bats (Eptesicus fuscus) to infection with European bat lyssavirus type 1. J. Gen. Virol. 2008, 89, 1998–2010. [Google Scholar] [CrossRef] [PubMed]
- Seif, I.; Coulon, P.; Rollin, P.E.; Flamand, A. Rabies Virulence: Effect on pathogenicity and sequence characterisation of rabies virus mutations affaecting antigenic site III of the glycoprotein. J. Virol. 1985, 53, 926–934. [Google Scholar] [PubMed]
- Mebatsion, T. Extensive attenuation of rabies virus by simultaneously modifying the dynein light chain binding site in the P protein and replacing Arg333 in the G protein. J. Virol. 2001, 75, 11496–11502. [Google Scholar] [CrossRef] [PubMed]
- Faber, M.; Faber, M.L.; Papaneri, A.; Bette, M.; Weihe, E.; Dietzschold, B.; Schnell, M.J. A single amino acid change in rabies virus glycoprotein increases virus spread and enhances virus pathogenicity. J. Virol. 2005, 79, 14141–14148. [Google Scholar] [CrossRef] [PubMed]
- Ito, H.; Minamoto, N.; Watanabe, T.; Goto, H.; Rong, L.T.; Sugiyama, M.; Kinjo, T.; Mannen, K.; Mifune, K.; Konobe, T.; et al. A unique mutation of glycoprotein gene of the attenuated RC-HL strain of rabies virus, a seed virus used for production of animal vaccine in Japan. Microbiol. Immunol. 1994, 38, 479–482. [Google Scholar] [CrossRef] [PubMed]

© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Evans, J.S.; Wu, G.; Selden, D.; Buczkowski, H.; Thorne, L.; Fooks, A.R.; Banyard, A.C. Utilisation of Chimeric Lyssaviruses to Assess Vaccine Protection against Highly Divergent Lyssaviruses. Viruses 2018, 10, 130. https://doi.org/10.3390/v10030130
Evans JS, Wu G, Selden D, Buczkowski H, Thorne L, Fooks AR, Banyard AC. Utilisation of Chimeric Lyssaviruses to Assess Vaccine Protection against Highly Divergent Lyssaviruses. Viruses. 2018; 10(3):130. https://doi.org/10.3390/v10030130
Chicago/Turabian StyleEvans, Jennifer S., Guanghui Wu, David Selden, Hubert Buczkowski, Leigh Thorne, Anthony R. Fooks, and Ashley C. Banyard. 2018. "Utilisation of Chimeric Lyssaviruses to Assess Vaccine Protection against Highly Divergent Lyssaviruses" Viruses 10, no. 3: 130. https://doi.org/10.3390/v10030130
APA StyleEvans, J. S., Wu, G., Selden, D., Buczkowski, H., Thorne, L., Fooks, A. R., & Banyard, A. C. (2018). Utilisation of Chimeric Lyssaviruses to Assess Vaccine Protection against Highly Divergent Lyssaviruses. Viruses, 10(3), 130. https://doi.org/10.3390/v10030130




