Residual Bone Height and New Bone Formation after Maxillary Sinus Augmentation Procedure Using Biomaterials: A Network Meta-Analysis of Clinical Trials
Abstract
1. Introduction
2. Materials and Methods
2.1. Design and Registration
2.2. Search Strategy and Selection Criteria
2.3. Data Collection
2.4. Outcome Variables
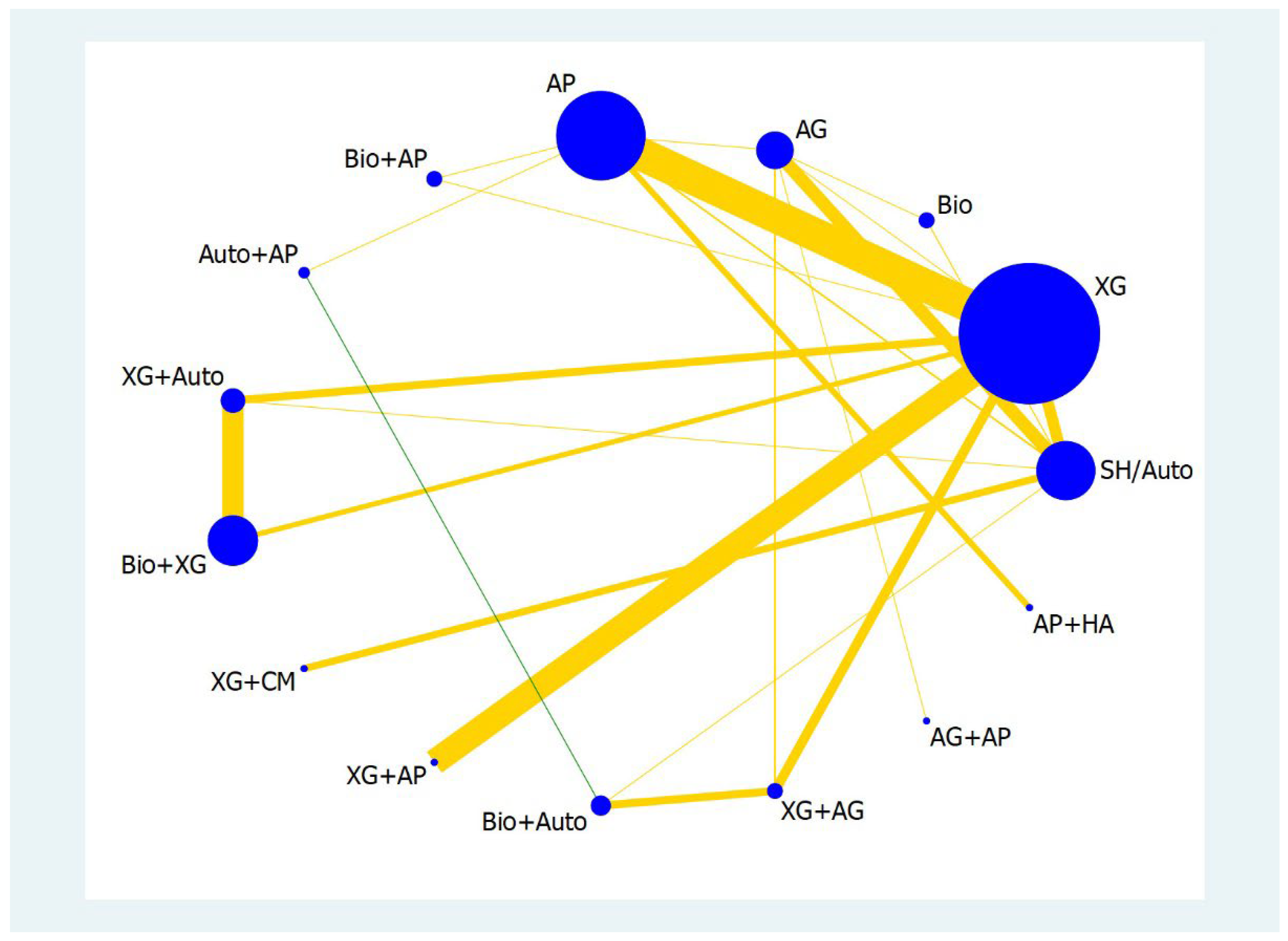
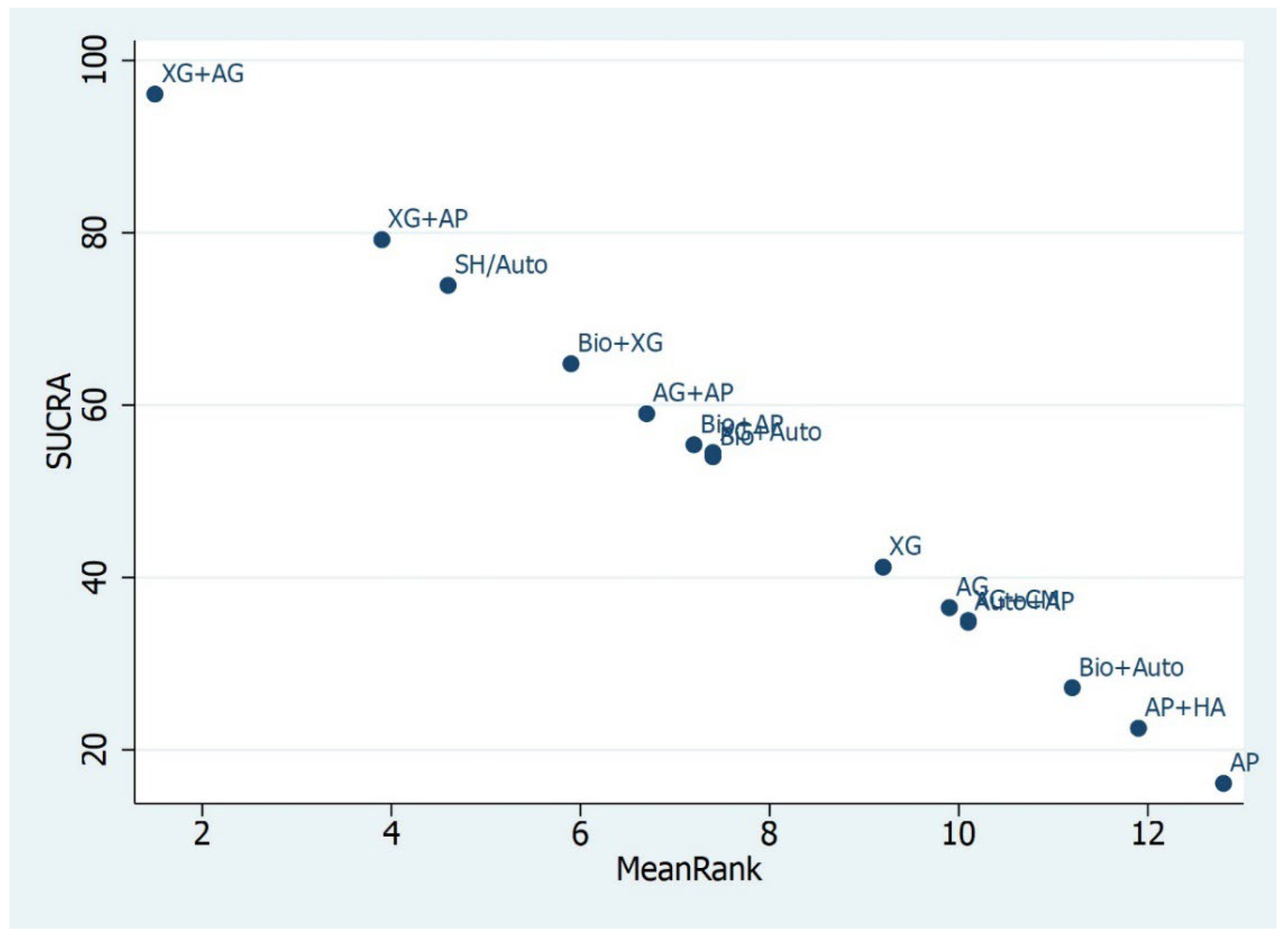
2.5. Data Analysis for Network Meta-Analysis
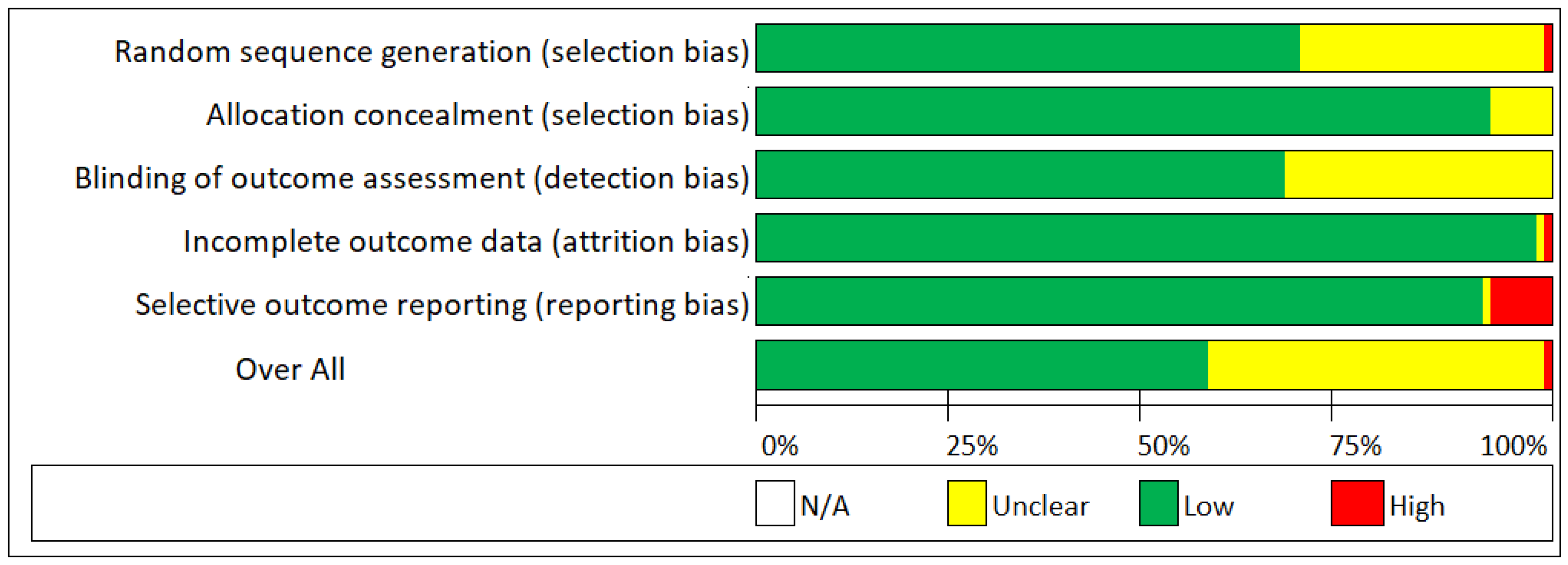
2.6. Risk of Bias
2.7. Heterogeneity
3. Results
Quality of Evidence
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Del Fabbro, M.; Rosano, G.; Taschieri, S. Implant survival rates after maxillary sinus augmentation. Eur. J. Oral Sci. 2008, 116, 497–506. [Google Scholar] [CrossRef] [PubMed]
- Wallace, S.S.; Tarnow, D.P.; Froum, S.J.; Cho, S.C.; Zadeh, H.H.; Stoupel, J.; Del Fabbro, M.; Testori, T. Maxillary sinus elevation by lateral window approach: Evolution of technology and technique. J. Evid. Based Dent. Pract. 2012, 12, 161–171. [Google Scholar] [CrossRef] [PubMed]
- Del Fabbro, M.; Wallace, S.S.; Testori, T. Long-term implant survival in the grafted maxillary sinus: A systematic review. Int. J. Periodontics Restor. Dent. 2013, 33, 773–783. [Google Scholar] [CrossRef] [PubMed]
- Danesh-Sani, S.A.; Loomer, P.M.; Wallace, S.S. A comprehensive clinical review of maxillary sinus floor elevation: Anatomy, techniques, biomaterials and complications. Br. J. Oral Maxillofac. Surg. 2016, 54, 724–730. [Google Scholar] [CrossRef] [PubMed]
- Corbella, S.; Taschieri, S.; Weinstein, R.; Del Fabbro, M. Histomorphometric outcomes after lateral sinus floor elevation procedure: A systematic review of the literature and meta-analysis. Clin. Oral Implant. Res. 2016, 27, 1106–1122. [Google Scholar] [CrossRef]
- Al-Moraissi, E.A.; Alkhutari, A.S.; Abotaleb, B.; Altairi, N.H.; Del Fabbro, M. Do osteoconductive bone substitutes result in similar bone regeneration for maxillary sinus augmentation when compared to osteogenic and osteoinductive bone grafts? A systematic review and frequentist network meta-analysis. Int. J. Oral Maxillofac. Surg. 2020, 49, 107–120. [Google Scholar] [CrossRef]
- Zhou, W.; Wang, F.; Magic, M.; Zhuang, M.; Sun, J.; Wu, Y. The effect of anatomy on osteogenesis after maxillary sinus floor augmentation: A radiographic and histological analysis. Clin. Oral Investig. 2021, 11, 5197–5204. [Google Scholar] [CrossRef]
- Stacchi, C.; Lombardi, T.; Ottonelli, R.; Berton, F.; Perinetti, G.; Traini, T. New bone formation after transcrestal sinus floor elevation was influenced by sinus cavity dimensions: A prospective histologic and histomorphometric study. Clin. Oral Implant. Res. 2018, 29, 465–479. [Google Scholar] [CrossRef]
- Avila--Ortiz, G.; Neiva, R.; Galindo--Moreno, P.; Rudek, I.; Benavides, E.; Wang, H.L. Analysis of the influence of residual alveolar bone height on sinus augmentation outcomes. Clin. Oral Implant. Res. 2012, 23, 1082–1088. [Google Scholar] [CrossRef]
- Pignaton, T.B.; Wenzel, A.; Ferreira, C.E.; Borges Martinelli, C.; Oliveira, G.J.; Marcantonio, E., Jr.; Spin--Neto, R. Influence of residual bone height and sinus width on the outcome of maxillary sinus bone augmentation using anorganic bovine bone. Clin. Oral Implant. Res. 2019, 30, 315–323. [Google Scholar] [CrossRef]
- Pignaton, T.B.; Spin-Neto, R.; Ferreira, C.E.; Martinelli, C.B.; de Oliveira, G.J.; Marcantonio, E., Jr. Remodelling of sinus bone grafts according to the distance from the native bone: A histomorphometric analysis. Clin. Oral Implant. Res. 2020, 31, 959–967. [Google Scholar] [CrossRef] [PubMed]
- Pesce, P.; Menini, M.; Canullo, L.; Khijmatgar, S.; Modenese, L.; Gallifante, G.; Del Fabbro, M. Radiographic and histomorphometric evaluation of biomaterials used for lateral sinus augmentation: A systematic review on the effect of residual bone height and vertical graft size on new bone formation and graft shrinkage. J. Clin. Med. 2021, 10, 4996. [Google Scholar] [CrossRef] [PubMed]
- Chao, Y.L.; Chen, H.H.; Mei, C.C.; Tu, Y.K.; Lu, H.K. Meta--regression analysis of the initial bone height for predicting implant survival rates of two sinus elevation procedures. J. Clin. Periodontol. 2010, 37, 456–465. [Google Scholar] [CrossRef] [PubMed]
- Chaimani, A.J.P.T.; Higgins, D.; Mavridis, P.; Spyridonos, G. Salanti. Graphical tools for network meta-analysis in Stata. PLoS ONE 2013, 8, e76654. [Google Scholar] [CrossRef]
- Jansen, J.P.; Naci, H. Is network meta-analysis as valid as standard pairwise meta-analysis? It all depends on the distribution of effect modifiers. BMC. Med. 2013, 11, 159. [Google Scholar] [CrossRef]
- Salanti, G. Indirect and mixed-treatment comparison, network, or multiple-treatments meta-analysis: Many names, many benefits, many concerns for the next generation evidence synthesis tool. Res. Synth. Methods 2012, 3, 80–97. [Google Scholar] [CrossRef]
- Velasco-Torres, M.; Padial-Molina, M.; Avila-Ortiz, G.; García-Delgado, R.; O’Valle, F.; Catena, A.; Galindo-Moreno, P. Maxillary sinus dimensions decrease as age and tooth loss increase. Implant. Dent. 2017, 26, 288–295. [Google Scholar] [CrossRef]
- Mendes, B.C.; Pereira, R.D.S.; Mourão, C.F.A.B.; Montemezzi, P.; Santos, A.M.S.; Moreno, J.M.L.; Okamoto, R.; Hochuli-Vieira, E. Evaluation of two Beta-Tricalcium Phosphates with Different Particle Dimensions in Human Maxillary Sinus Floor Elevation: A Prospective, Randomized Clinical Trial. Materials 2022, 15, 1824. [Google Scholar] [CrossRef]
- Harlos, M.M.; da Silva, T.B.; Montagner, P.G.; Teixeira, L.N.; Gomes, A.V.; Martinez, E.F. Histomorphometric evaluation of different graft associations for maxillary sinus elevation in wide antral cavities: A randomized controlled clinical trial. Clin. Oral Investig. 2022, 26, 1–9. [Google Scholar] [CrossRef]
- Arshad, M.; Ghanavati, Z.; Aminishakib, P.; Rasouli, K.; Shirani, G. Effect of Light-Emitting Diode Phototherapy on Allograft Bone After Open Sinus Lift Surgery: A Randomized Clinical Trial (Concurrent Parallel). J. Lasers Med. Sci. 2021, 12, e16. [Google Scholar] [CrossRef]
- Beck, F.; Reich, K.M.; Lettner, S.; Heimel, P.; Tangl, S.; Redl, H.; Ulm, C. The vertical course of bone regeneration in maxillary sinus floor augmentations: A histomorphometric analysis of human biopsies. J. Periodontol. 2021, 92, 263–272. [Google Scholar] [CrossRef] [PubMed]
- Zahedpasha, A.; Ghassemi, A.; Bijani, A.; Haghanifar, S.; Majidi, M.S.; Ghorbani, Z.M. Comparison of bone formation after sinus membrane lifting without graft or using bone substitute “histologic and radiographic evaluation”. J. Oral Maxillofac. Surg. 2021, 79, 1246–1254. [Google Scholar] [CrossRef] [PubMed]
- Trimmel, B.; Gyulai-Gaál, S.; Kivovics, M.; Jákob, N.P.; Hegedűs, C.; Szabó, B.T.; Dobó-Nagy, C.; Szabó, G. Evaluation of the Histomorphometric and Micromorphometric Performance of a Serum Albumin-Coated Bone Allograft Combined with A-PRF for Early and Conventional Healing Protocols after Maxillary Sinus Augmentation: A Randomized Clinical Trial. Materials 2021, 14, 1810. [Google Scholar] [CrossRef] [PubMed]
- Correia, F.; Pozza, D.H.; Gouveia, S.; Felino, A.C.; Faria-Almeida, R. Advantages of porcine xenograft over autograft in sinus lift: A randomised clinical trial. Materials 2021, 21, 3439. [Google Scholar] [CrossRef]
- Chaushu, L.; Chaushu, G.; Kolerman, R.; Vered, M.; Naishlos, S.; Nissan, J. Histomorphometrical Assessment of Sinus Augmentation Using Allograft (Particles or Block) and Simultaneous Implant Placement. Sci. Rep. 2020, 10, 9046. [Google Scholar] [CrossRef]
- da Silva, H.F.; Goulart, D.R.; Sverzut, A.T.; Olate, S.; de Moraes, M. Comparison of two anorganic bovine bone in maxillary sinus lift: A split-mouth study with clinical, radiographical, and histomorphometrical analysis. Int. J. Implant. Dent. 2020, 6, 1. [Google Scholar] [CrossRef]
- Grasso, G.; Mummolo, S.; Bernardi, S.; Pietropaoli, D.; D’Ambrosio, G.; Iezzi, G.; Piattelli, A.; Bianchi, S.; Marchetti, E. Histological and histomorphometric evaluation of new bone formation after maxillary sinus augmentation with two different osteoconductive materials: A randomized, parallel, double-blind clinical trial. Materials 2020, 13, 5520. [Google Scholar] [CrossRef]
- Kim, H.W.; Lim, K.O.; Lee, W.P.; Seo, Y.S.; Shin, H.I.; Choi, S.H.; Kim, B.O.; Yu, S.J. Sinus floor augmentation using mixture of mineralized cortical bone and cancellous bone allografts: Radiographic and histomorphometric evaluation. J. Dent. Sci. 2020, 15, 257–264. [Google Scholar] [CrossRef]
- Velasco--Ortega, E.; Valente, N.A.; Iezzi, G.; Petrini, M.; Derchi, G.; Barone, A. Maxillary sinus augmentation with three different biomaterials: Histological, histomorphometric, clinical, and patient--reported outcomes from a randomized controlled trial. Clin. Implant. Dent. Relat. Res. 2021, 23, 86–95. [Google Scholar] [CrossRef]
- Pereira, R.D.; Bonardi, J.P.; Ouverney, F.R.; Campos, A.B.; Griza, G.L.; Okamoto, R.; Hochuli-Vieira, E. The new bone formation in human maxillary sinuses using two bone substitutes with different resorption types associated or not with autogenous bone graft: A comparative histomorphometric, immunohistochemical and randomized clinical study. J. Appl. Oral Sci. 2020, 29, e20200568. [Google Scholar] [CrossRef]
- Tanaka, K.; Iezzi, G.; Piattelli, A.; Ferri, M.; Mesa, N.F.; Alccayhuaman, K.A.; Botticelli, D. Sinus floor elevation and antrostomy healing: A histomorphometric clinical study in humans. Implant. Dent. 2019, 28, 537–542. [Google Scholar] [CrossRef] [PubMed]
- Pang, K.M.; Lee, J.K.; Choi, S.H.; Kim, Y.K.; Kim, B.J.; Lee, J.H. Maxillary sinus augmentation with calcium phosphate double-coated anorganic bovine bone: Comparative multicenter randomized clinical trial with histological and radiographic evaluation. Implant. Dent. 2019, 28, 39–45. [Google Scholar] [CrossRef] [PubMed]
- Batas, L.; Tsalikis, L.; Stavropoulos, A. PRGF as adjunct to DBB in maxillary sinus floor augmentation: Histological results of a pilot split-mouth study. Int. J. Implant. Dent. 2019, 5, 14. [Google Scholar] [CrossRef] [PubMed]
- Oh, J.S.; Seo, Y.S.; Lee, G.J.; You, J.S.; Kim, S.G. A Comparative Study with Biphasic Calcium Phosphate to Deproteinized Bovine Bone in Maxillary Sinus Augmentation: A Prospective Randomized and Controlled Clinical Trial. Int. J. Oral Maxillofac. Implant. 2019, 34, 233–242. [Google Scholar] [CrossRef]
- Scarano, A.; de Oliveira, P.S.; Traini, T.; Lorusso, F. Sinus Membrane Elevation with Heterologous Cortical Lamina: A Randomized Study of a New Surgical Technique for Maxillary Sinus Floor Augmentation without Bone Graft. Materials 2018, 17, 11, 1457. [Google Scholar] [CrossRef]
- Nizam, N.; Eren, G.; Akcali, A.; Donos, N. Maxillary sinus augmentation with leukocyte and platelet-rich fibrin and deprotei nized bovine bone mineral: A split-mouth histological and histomorphometric study. Clin. Oral Implants. Res. 2018, 29, 67–75. [Google Scholar] [CrossRef]
- Taschieri, S.; Corbella, S.; Weinstein, R.; Di Giancamillo, A.; Mortellaro, C.; Del Fabbro, M. Maxillary Sinus Floor Elevation using Platelet-Rich Plasma Combined with either Biphasic Calcium Phosphate or Deproteinized Bovine Bone. J. Craniofac. Surg. 2016, 27, 702–707. [Google Scholar] [CrossRef]
- Menezes, J.D.; Pereira, R.D.S.; Bonardi, J.P.; Griza, G.L.; Okamoto, R.; Hochuli-Vieira, E. Bioactive glass added to autogenous bone graft in maxillary sinus augmentation: A prospective histomorphometric, immunohistochemical, and bone graft resorption assessment. J. Appl. Oral Sci. 2018, 26, e20170296. [Google Scholar] [CrossRef]
- Theodoro, L.H.; Rocha, G.S.; Ribeiro Junior, V.L.; Sakakura, C.E.; de Mello Neto, J.M.; Garcia, V.G.; Ervolino, E.; Marcantonio Junior, E. Bone Formed After Maxillary Sinus Floor Augmentation by Bone Autografting with Hydroxyapatite and Low-Level Laser Therapy: A Randomized Controlled Trial With Histomorphometrical and Immunohistochemical Analyses. Implant. Dent. 2018, 27, 547–554. [Google Scholar] [CrossRef]
- Pereira, R.S.; Gorla, L.F.; Boos, F.B.; Okamoto, R.; Júnior, I.G.; Hochuli-Vieira, E. Use of autogenous bone and beta-tricalcium phosphate in maxillary sinus lifting: Histomorphometric study and immunohistochemical assessment of RUNX2 and VEGF. Int. J. Oral Maxillofac. Surg. 2017, 46, 503–510. [Google Scholar] [CrossRef]
- Stacchi, C.; Lombardi, T.; Oreglia, F.; Alberghini Maltoni, A.; Traini, T. Histologic and histomorphometric comparison between sintered nanohydroxyapatite and anorganic bovine xenograft in maxillary sinus grafting: A split-mouth randomized controlled clinical trial. BioMed Res. Int. 2017, 2017, 9489825. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.S.; Shin, H.K.; Yun, J.H.; Cho, K.S. Randomized clinical trial of maxillary sinus grafting using deproteinized porcine and bovine bone mineral. Clin. Implant. Dent. Relat. Res. 2017, 19, 140–150. [Google Scholar] [CrossRef] [PubMed]
- Rodriguezy Baena, R.; Pastorino, R.; Gherlone, E.F.; Perillo, L.; Lupi, S.M.; Lucchese, A. Histomorphometric evaluation of two different bone substitutes in sinus augmentation procedures: A randomized controlled trial in humans. Int. J. Oral Maxillofac. Implant. 2017, 32, 188–194. [Google Scholar] [CrossRef] [PubMed]
- Comert Kilic, S.; Gungormus, M.; Parlak, S.N. Histologic and histomorphometric assess ment of sinus-floor augmentation with be ta-tricalcium phosphate alone or in combination with pure-platelet-rich plasma or platelet-rich fibrin: A randomized clinical trial. Clin. Implant. Dent. Relat. Res. 2017, 19, 959–967. [Google Scholar] [CrossRef]
- Dogan, E.; Dursun, E.; Tosun, E.; Bilgic, E.; Akman, A.C.; Orhan, K.; Celik, H.H.; Korkusuz, P.; Caglayan, F. Evaluation of hyaluronic matrix efficacy in sinus augmentation: A randomized-controlled histomorphometric and micro-computed tomography analysis. Int. J. Oral Maxillofac. Surg. 2017, 46, 931–937. [Google Scholar] [CrossRef]
- Kolerman, R.; Nissan, J.; Rahmanov, M.; Vered, H.; Cohen, O.; Tal, H. Comparison between mineralized cancellous bone allograft and an alloplast material for sinus augmentation: A split mouth histomorphometric study. Clin. Implant. Dent. Relat. Res. 2017, 19, 812–820. [Google Scholar] [CrossRef]
- Meimandi, M.; Moghaddam, A.A.; Gholami, G.A.; Abbass, F.M.; Solati, M. Histomorphometric and histologic evaluation of nano-HA with and without PRGF in bilateral sinus lift augmentation: A randomized clinical trial. J. Res. Med. Dent. Sci. 2017, 5, 69–81. [Google Scholar]
- Portelli, M.; Cicciù, M.; Lauritano, F.; Cervino, G.; Manuelli, M.; Gherlone, E.F.; Lucchese, A. Histomorphometric Evaluation of Two Different Bone Substitutes in Sinus Floor Augmentation Procedures. J. Craniofacial Surg. 2017, 22. [Google Scholar] [CrossRef]
- Meymandi, M.; Solati, M.; Talebi, M.; Mashadi, F.A.; Abbas, M.; Moghaddam, A.A. Histologic and Histomorphometric Evaluation of Maxillary Sinus Floor Elevation Using Nanobone® and EasyGrafttm Crystal: A Split-Mouth Clinical Trial. J. Res. Med. Dent. Sci. 2017, 5, 35–43. [Google Scholar]
- Nery, J.C.; Pereira, L.A.V.D.; Guimarães, G.F.; Scardueli, C.R.; França, F.M.G.; SpinNeto, R.; Stavropoulos, A. β-TCP/HA with or without enamel matrix proteins for maxillary sinus floor augmentation: A histomorphometric analysis of human biopsies. Int. J. Implant. Dent. 2017, 3, 18. [Google Scholar] [CrossRef]
- Pereira, R.D.; Menezes, J.D.; Bonardi, J.P.; Griza, G.L.; Okamoto, R.; Hochuli--Vieira, E. Histomorphometric and immunohistochemical assessment of RUNX2 and VEGF of Biogran™ and autogenous bone graft in human maxillary sinus bone augmentation: A prospective and randomized study. Clin. Implant. Dent. Relat. Res. 2017, 19, 867–875. [Google Scholar] [CrossRef] [PubMed]
- Amoian, B.; Seyedmajidi, M.; Safipor, H.; Ebrahimipour, S. Histologic and histomorphometric evaluation of two grafting materials Cenobone and ITB-MBA in open sinus lift surgery. J. Int. Soc. Prev. Community Dent. 2016, 6, 480–486. [Google Scholar]
- Jelusic, D.; Zirk, M.L.; Fienitz, T.; Plancak, D.; Puhar, I.; Rothamel, D. Monophasic ß-TCP vs. biphasic HA/ß-TCP in two-stage sinus floor augmentation procedures—A prospective randomized clinical trial. Clin. Oral Implant. Res. 2017, 28, e175–e183. [Google Scholar] [CrossRef] [PubMed]
- Nappe, C.E.; Rezuc, A.B.; Montecinos, A.; Donoso, F.A.; Vergara, A.J.; Martinez, B. Histological comparison of an allograft, a xenograft and alloplastic graft as bone substitute materials. J. Osseointegr. 2016, 8, 20–26. [Google Scholar]
- Duque Netto, H.; Miranda Chaves, M.D.; Aatrstrup, B.; Guerra, R.; Olate, S. Bone formation in maxillary sinus lift using autogenous bone graft at 2 and 6 months. Int. J. Morphol. 2016, 34, 69–75. [Google Scholar] [CrossRef]
- Ahmet, S.; Alper Gultekin, B.; Karabuda, Z.C.; Olgac, V. Two composite bone graft substitutes for maxillary sinus floor augmentation: Histological, histomorphometric, and radiographic analyses. Implant. Dent. 2016, 25, 313–321. [Google Scholar] [CrossRef] [PubMed]
- Badr, M.; Oliver, R.; Pemberton, P.; Coulthard, P. Platelet-rich plasma in grafted maxillae: Growth factor quantification and dynamic histomorphometric evaluation. Implant. Dent. 2016, 25, 492–498. [Google Scholar] [CrossRef]
- Kim, E.S.; Kang, J.Y.; Kim, J.J.; Kim, K.W.; Lee, E.Y. Space maintenance in autogenous fresh demineralized tooth blocks with platelet-rich plasma for maxillary sinus bone formation: A prospective study. SpringerPlus 2016, 5, 274. [Google Scholar] [CrossRef]
- Alayan, J.; Vaquette, C.; Farah, C.; Ivanovski, S. A histomorphometric assessment of collagen--stabilized anorganic bovine bone mineral in maxillary sinus augmentation–a prospective clinical trial. Clin. Oral Implant. Res. 2016, 27, 850–858. [Google Scholar] [CrossRef]
- Danesh-Sani, S.A.; Wallace, S.S.; Movahed, A.; El Chaar, E.S.; Cho, S.C.; Khouly, I.; Testori, T. Maxillary Sinus Grafting With Biphasic Bone Ceramic or Autogenous Bone: Clinical, Histologic, and Histomorphometric Results From a Randomized Controlled Clinical Trial. Implant. Dent. 2016, 25, 588–593. [Google Scholar] [CrossRef]
- de Oliveira, T.A.; Aloise, A.C.; Orosz, J.E.; de Melloe Oliveira, R.; de Carvalho, P.; Pelegrine, A.A. Double Centrifugation Versus Single Centrifugation of Bone Marrow Aspirate Concentrate in Sinus Floor Elevation: A Pilot Study. Int. J. Oral Maxillofac. Implant. 2016, 31, 216–222. [Google Scholar] [CrossRef] [PubMed]
- Payer, M.; Lohberger, B.; Strunk, D.; Reich, K.M.; Acham, S.; Jakse, N. Effects of directly autotransplanted tibial bone marrow aspirates on bone regeneration and osseointegration of dental implants. Clin. Oral Implant. Res. 2014, 25, 468–474. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Chung, J.H.; Shin, S.Y.; Shin, S.I.; Kye, S.B.; Kim, N.K.; Kwon, T.G.; Paeng, J.Y.; Kim, J.W.; OH, O.H.; et al. Efficacy of rhBMP-2/hydroxyapatite on si nus floor augmentation: A multicenter, ran domized controlled clinical trial. J. Dent. Res. 2015, 94, 158s–165s. [Google Scholar] [CrossRef]
- Kim, M.S.; Lee, J.S.; Shin, H.K.; Kim, J.S.; Yun, J.H.; Cho, K.S. Prospective randomized, controlled trial of sinus grafting using Escherichia coli-produced rhBMP-2 with a biphasic calcium phosphate carrier compared to deproteinized bovine bone. Clin. Oral Implant. Res. 2015, 26, 1361–1368. [Google Scholar] [CrossRef]
- Sehn, F.P.; Dias, R.R.; de Santana Santos, T.; Silva, E.R.; Salata, L.A.; Chaushu, G.; Xavier, S.P. Fresh-frozen allografts combined with bo vine bone mineral enhance bone formation in sinus augmentation. J. Biomater. Appl. 2015, 29, 1003–1013. [Google Scholar] [CrossRef]
- Taschieri, S.; Testori, T.; Corbella, S.; Weinstein, R.; Francetti, L.; Di Giancamillo, A.; Del Fabbro, M. Platelet-rich plasma and deproteinized bovine bone matrix in maxillary sinus lift surgery: A split-mouth histomor phometric evaluation. Implant. Dent. 2015, 24, 592–597. [Google Scholar] [CrossRef]
- Xavier, S.P.; Dias, R.R.; Sehn, F.P.; Kahn, A.; Chaushu, L.; Chaushu, G. Maxillary sinus grafting with autograft vs. fresh frozen allograft: A split-mouth histomorphometric study. Clin. Oral Implant. Res. 2015, 26, 1080–1085. [Google Scholar] [CrossRef]
- Pasquali, P.J.; Teixeira, M.L.; de Oliveira, T.A.; de Macedo, L.G.; Aloise, A.C.; Pelegrine, A.A. Maxillary sinus augmentation combining Bio Oss with the bone marrow aspirate concen trate: A histomorphometric study in humans. Int. J. Biomater. 2015, 2015, 121286. [Google Scholar] [CrossRef]
- de Lange, G.L.; Overman, J.R.; Farré-Guasch, E.; Korstjens, C.M.; Hartman, B.; Langenbach, G.E.; Van Duin, M.A.; Klein-Nulend, J. A histomorphometric and micro–computed tomography study of bone regeneration in the maxillary sinus comparing biphasic calcium phosphate and deproteinized cancellous bovine bone in a human split-mouth model. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2014, 117, 8–22. [Google Scholar] [CrossRef]
- Correia, F.; Pozza, D.; Gouveia, S. Sinus lift with two different grafts—Histological and radiological findings—Preliminary reports. Clin. Oral Implant. Res. 2014, 25 (Suppl. 10), 444. [Google Scholar]
- Garlini, G.; Redemagni, M.; Canciani, E.; Del lavia, C. Maxillary sinus floor augmentation with vegetal hydroxyapatite “versus” demi neralized bovine bone: A randomized clinical study with a split-mouth design. J. Dent. Implant. 2014, 4, 118–125. [Google Scholar] [CrossRef]
- Wildburger, A.; Payer, M.; Jakse, N.; Strunk, D.; Etchard-Liechtenstein, N.; Sauerbier, S. Impact of autogenous concentrated bone mar row aspirate on bone regeneration after sinus floor augmentation with a bovine bone sub stitute—A split-mouth pilot study. Clin. Oral Implant. Res. 2014, 25, 1175–1181. [Google Scholar] [CrossRef] [PubMed]
- Torres García--Denche, J.; Wu, X.; Martinez, P.P.; Eimar, H.; Ikbal, D.J.; Hernández, G.; López--Cabarcos, E.; Fernandez--Tresguerres, I.; Tamimi, F. Membranes over the lateral window in sinus augmentation procedures: A two--arm and split--mouth randomized clinical trials. J. Clin. Periodontol. 2013, 40, 1043–1051. [Google Scholar] [CrossRef] [PubMed]
- Froum, S.J.; Wallace, S.; Cho, S.C.; Khouly, I.; Rosenberg, E.; Corby, P.; Froum, S.; Bromage, T.; Schoor, R.; Norman, R.; et al. Histomorphometric comparison of different concentrations of recombinant human bone morphogenetic protein with allogeneic bone compared to the use of 100% mineralized cancellous bone allograft in maxillary sinus grafting. Int. J. Periodontics Restor. Dent. 2013, 33, 721–730. [Google Scholar] [CrossRef]
- Froum, S.J.; Wallace, S.; Cho, S.C.; Rosenburg, E.; Froum, S.; Schoor, R.; Mascarenhas, P.; Tarnow, D.P.; Corby, P.; Elian, N.; et al. A histomorphometric comparison of Bio-Oss alone versus Bio-Oss and platelet-derived growth factorforsinus aug mentation: A postsurgical assessment. Int. J. Periodontics Restor. Dent. 2013, 33, 269. [Google Scholar] [CrossRef]
- Khairy, N.M.; Shendy, E.E.; Askar, N.A.; El Rouby, D.H. Effect of platelet rich plasma on bone regeneration in maxillary sinus aug mentation (randomized clinical trial). Int. J. Oral Maxillofac. Surg. 2013, 42, 249–255. [Google Scholar] [CrossRef]
- Schmitt, C.M.; Doering, H.; Schmidt, T.; Lutz, R.; Neukam, F.W.; Schlegel, K.A. Histological results after maxillary sinus augmentation with Straumann (R) BoneCeramic, Bio-Oss (R), Puros(R), and autologous bone. A ran domized controlled clinical trial. Clin. Oral Implant. Res. 2013, 24, 576–585. [Google Scholar] [CrossRef]
- Tosta, M.; Cortes, A.R.; Correa, L.; Pinto Ddos, S., Jr.; Tumenas, I.; Katchburian, E. Histologic and histomorphometric evaluation of a synthetic bone substitute for maxillary sinus grafting in humans. Clin. Oral Implant. Res. 2013, 24, 866–870. [Google Scholar] [CrossRef]
- Anitua, E.; Prado, R.; Orive, G. Bilateral sinus elevation evaluating plasma rich in growth factors technology: A report of five cases. Clin. Implant. Dent. Relat. Res. 2012, 14, 51–60. [Google Scholar] [CrossRef]
- Kao, D.W.; Kubota, A.; Nevins, M.; Fiorellini, J.P. The negative effect of combining rhBMP-2 and Bio-Oss on bone formation for maxillary sinus augmentation. Int. J. Periodontics Restor. Dent. 2012, 32, 61–67. [Google Scholar]
- Kurkcu, M.; Benlidayi, M.E.; Cam, B.; Sertdemir, Y. Anorganic bovine-derived hydroxyapatite vs beta-tricalcium phosphate in sinus augmenta tion: A comparative histomorphometric study. J. Oral Implant. 2012, 38, 519–526. [Google Scholar] [CrossRef] [PubMed]
- Lindgren, C.; Mordenfeld, A.; Johansson, C.B.; Hallman, M. A 3-year clinical follow-up of implants placed in two different biomaterials used for sinus augmentation. Int. J. Oral Maxillofac. Implant. 2012, 27, 1151–1162. [Google Scholar]
- Zhang, Y.; Tangl, S.; Huber, C.D.; Lin, Y.; Qiu, L.; Rausch-Fan, X. Effects of Choukroun’s plate let-rich fibrin on bone regeneration in com bination with deproteinized bovine bone mineral in maxillary sinus augmentation: A histological and histomorphometric study. J. Craniomaxillofac. Surg. 2012, 40, 321–328. [Google Scholar] [CrossRef]
- Wagner, W.; Wiltfang, J.; Pistner, H.; Yildirim, M.; Ploder, B.; Chapman, M.; Schiestl, N.; Hanak, E. Bone formation with a biphasic calci um phosphate combined with fibrin sealant in maxillary sinus floor elevation for delayed dental implant. Clin. Oral Implant. Res. 2012, 23, 1112–1117. [Google Scholar] [CrossRef] [PubMed]
- Pikdöken, L.; Gürbüzer, B.; Küçükodacı, Z.; Urhan, M.; Barış, E.; Tezulaş, E. Scintigraphic, histologic, and histomorphometric analyses of bovine bone mineral and autogenous bone mixture in sinus floor augmentation: A randomized controlled trial—Results after 4 months of healing. J. Oral Maxillofac. Surg. 2011, 69, 160–169. [Google Scholar] [CrossRef] [PubMed]
- Stavropoulos, A.; Becker, J.; Capsius, B.; Açil, Y.; Wagner, W.; Terheyden, H. Histological evaluation of maxillary sinus floor augmentation with recombinant human growth and differentiation factor--5--coated β--tricalcium phosphate: Results of a multicenter randomized clinical trial. J. Clin. Periodontol. 2011, 38, 966–974. [Google Scholar] [CrossRef] [PubMed]
- Rickert, D.; Sauerbier, S.; Nagursky, H.; Menne, D.; Vissink, A.; Raghoebar, G.M. Maxillary sinus floor elevation with bovine bone min eral combined with either autogenous bone or autogenous stem cells: A prospective ran domized clinical trial. Clin. Oral Implant. Res. 2011, 22, 251–258. [Google Scholar] [CrossRef]
- Sauerbier, S.; Rickert, D.; Gutwald, R.; Nagursky, H.; Oshima, T.; Xavier, S.P.; Christmann, J.; Kurz, P.; Menne, D.; Vissink, A.; et al. Bone marrow concentrate and bovine bone mineral for sinus floor augmentation: A controlled, randomized, single-blinded clinical and histological trial—Per-protocol analysis. Tissue Eng. Part A 2011, 17, 2187–2197. [Google Scholar] [CrossRef]
- Galindo--Moreno, P.; Moreno--Riestra, I.; Avila, G.; Padial-Molina, M.; Paya, J.A.; Wang, H.L.; O’Valle, F. Effect of anorganic bovine bone to autogenous cortical bone ratio upon bone remodeling patterns following maxillary sinus augmentation. Clin. Oral Implant. Res. 2011, 22, 857–864. [Google Scholar] [CrossRef]
- de Vicente, J.C.; Hernández-Vallejo, G.; Braña-Abascal, P.; Peña, I. Maxillary sinus augmentation with autologous bone harvested from the lateral maxillary wall combined with bovine-derived hydroxyapatite: Clinical and histologic observations. Clin. Oral Implant. Res. 2010, 21, 430–438. [Google Scholar] [CrossRef]
- Felice, P.; Scarano, A.; Pistilli, R.; Checchi, L.; Piattelli, M.; Pellegrino, G.; Esposito, M. A comparison of two techniques to augment maxillary sinuses using the lateral window approach: Rigid synthetic resorbable barriers versus anorganic bovine bone. Five-month post-loading clinical and histological results of a pilot randomised controlled clinical trial. Eur. J. Oral Implantol. 2009, 2, 293–306. [Google Scholar] [PubMed]
- Cordaro, L.; Bosshardt, D.D.; Palattella, P.; Rao, W.; Serino, G.; Chiapasco, M. Maxillary sinus grafting with Bio--Oss® or Straumann® Bone Ceramic: Histomorphometric results from a randomized controlled multicenter clinical trial. Clin. Oral Implant. Res. 2008, 19, 796–803. [Google Scholar] [CrossRef] [PubMed]
- Froum, S.J.; Wallace, S.S.; Cho, S.C.; Elian, N.; Tarnow, D.P. Histomorphometric Comparison of a Biphasic Bone Ceramic to Anorganic anorganic bovine bone for sinus augmentation: 6- to 8-month postsurgical assessment of vital bone formation. A pilot study. Int. J. Periodontics Restor. Dent. 2008, 28, 273–281. [Google Scholar]
- Galindo--Moreno, P.; Ávila, G.; Fernández--Barbero, J.E.; Aguilar, M.; Sánchez--Fernández, E.; Cutando, A.; Wang, H.L. Evaluation of sinus floor elevation using a composite bone graft mixture. Clin. Oral Implant. Res. 2007, 18, 376–382. [Google Scholar] [CrossRef]
- Froum, S.J.; Wallace, S.S.; Elian, N.; Cho, S.C.; Tarnow, D.P. Comparison of mineralized cancellous bone allograft (Puros) and anorganic bovine bone matrix (Bio-Oss) for sinus augmentation: Histomorphometry at 26 to 32 weeks after grafting. Int. J. Periodontics Restor. Dent. 2006, 26, 543–551. [Google Scholar]
- Zijderveld, S.A.; Zerbo, I.R.; van den Bergh, J.; Schulten, E.; Bruggenkate, C.M. Maxillary Sinus Floor Augmentation Using a β3-Tricalcium Phosphate (Cerasorb) Alone Compared to Autogenous Bone Grafts. Int. J. Oral Maxillofac. Implant. 2005, 20, 432–440. [Google Scholar]
- Raghoebar, G.M.; Schortinghuis, J.; Liem, R.S.; Ruben, J.L.; Van Der Wal, J.E.; Vissink, A. Does platelet--rich plasma promote remodeling of autologous bone grafts used for augmentation of the maxillary sinus floor? Clin. Oral Implant. Res. 2005, 16, 349–356. [Google Scholar] [CrossRef]
- Szabó, G.; Huys, L.; Coulthard, P.; Malorana, C.; Garagiola, U.; Barabás, J.; Németh, Z.; Hrabák, K.; Suba, Z. A Prospective Multicenter Randomized Clinical Trial of Autogenous Bone Versus β-Tricalcium Phosphate Graft Alone for Bilateral Sinus Elevation: Histologic and Histomorphometric Evaluation. Int. J. Oral Maxillofac. Implant. 2005, 20, 371–381. [Google Scholar] [CrossRef]
- Zerbo, I.R.; Zijderveld, S.A.; De Boer, A.; Bronckers, A.L.; De Lange, G.; Ten Bruggenkate, C.M.; Burger, E.H. Histomorphometry of human sinus floor augmentation using a porous β--tricalcium phosphate: A prospective study. Clin. Oral Implant. Res. 2004, 15, 724–732. [Google Scholar] [CrossRef]
- Wiltfang, J.; Schlegel, K.A.; Schultze--Mosgau, S.; Nkenke, E.; Zimmermann, R.; Kessler, P. Sinus floor augmentation with β--tricalciumphosphate (β--TCP): Does platelet--rich plasma promote its osseous integration and degradation? Clin. Oral Implant. Res. 2003, 14, 213–218. [Google Scholar] [CrossRef]
- Hallman, M.; Sennerby, L.; Lundgren, S. A clinical and histologic evaluation of implant integration in the posterior maxilla after sinus floor augmentation with autogenous bone, bovine hydroxyapatite, or a 20: 80 mixture. Int. J. Oral Maxillofac. Implant. 2002, 17, 635–643. [Google Scholar]
- Velasco-Torres, M.; Padial-Molina, M.; Alarcón, J.A.; O’Valle, F.; Catena, A.; Galindo-Moreno, P. Maxillary sinus dimensions with respect to the posterior superior alveolar artery decrease with tooth loss. Implant. Dent. 2016, 25, 464–470. [Google Scholar] [CrossRef] [PubMed]
- Zheng, X.; Huang, L.; Huang, S.; Mo, A.; Zhu, J. Influence of anatomical factors related to maxillary sinus on outcomes of transcrestal sinus floor elevation. J. Dent. Sci. 2022, 17, 438–443. [Google Scholar] [CrossRef] [PubMed]
- Stacchi, C.; Rapani, A.; Lombardi, T.; Bernardello, F.; Nicolin, V.; Berton, F. Does new bone formation vary in different sites within the same maxillary sinus after lateral augmentation? A prospective histomorphometric study. Clin. Oral. Implants. Res. 2022, 33, 322–332. [Google Scholar] [CrossRef] [PubMed]
- Rong, Q.; Li, X.; Chen, S.L.; Zhu, S.X.; Huang, D.Y. Effect of the Schneiderian membrane on the formation of bone after lifting the floor of the maxillary sinus: An experimental study in dogs. Br. J. Oral Maxillofac. Surg. 2015, 53, 607–612. [Google Scholar] [CrossRef]
- Higgins, J.P.; Jackson, D.; Barrett, J.K.; Lu, G.; Ades, A.; White, I.R. Consistency and inconsistency in network meta-analysis: Concepts and models for multi-arm studies. Res. Synth. Methods 2012, 3, 98–110. [Google Scholar] [CrossRef]
- Lin, L. Use of prediction intervals in network meta-analysis. JAMA Netw. Open 2019, 2, e199735. [Google Scholar] [CrossRef]
- Puhan, M.A.; Schünemann, H.J.; Murad, M.H.; Li, T.; Brignardello-Petersen, R.; Singh, J.A.; Kessels, A.G.; Guyatt, G.H. A GRADE Working Group approach for rating the quality of treatment effect estimates from network meta-analysis. BMJ 2014, 24, 349. [Google Scholar] [CrossRef]



| 1st Author, Year | No. of Patients | No. of Sinus Lifts | Age, Years Mean ± SD (Range) | Residual Bone Height (mm) | Months (Follow-Up) | CTR Material | Test Material/Technique |
|---|---|---|---|---|---|---|---|
| Mendes, 2022 [18] | 30 | 30 | (50–70) | <5 | 6 | Autogenous bone | G2: β-TCP ChronOS; G3: Beta-TCP |
| Harlos, 2022 [19] | 36 | 36 | 53.8 | <3 | 8 | DBBM+Autogenous bone | G2: Auto+PRF; G3: XG |
| Arshad, 2021 [20] * | 44 | 44 | 40.5 ± 8.5 | ۔ | 1 | AG | Allograft (+LED Group) |
| Beck, 2021 [21] * | 55 | 85 | 51.82 ± 9.93 | 4.58 ± 2.5 | 6 | DBBM | XG+auto; XG+bio |
| Zahedpasha, 2021 [22] | 10 | 20 | 45.65 ± 5.74 (39–51) | G1:4.88 ± 1.63; G2:5.36 ± 1.55 | 6 | Self-healing (no graft) | Bovine bone (Cerabone) |
| Trimmel, 2021 [23] | 26 | 30 | 57.93 ± 7.79 (test); 55.33 ± 8.55 (ctr) | 2.93 ± 1.14 (test); 3.48 ± 1.04 (ctr) | 3 (test) 6 (ctr) | A-PRF | Albumin-coated bone allograft (SACBA) |
| Correia, 2021 [24] | 12 | 24 | 59.7 ± 8.7 | 3.20 ± 0.93 | 6 | Autologous bone | Porcine bone |
| Chaushu, 2020 [25] * | 29 | 38 | 55.5 ± 10 (39–74) | <3 | 9 | Allograft particles | Allograft block |
| da Silva, 2020 [26] * | 13 | 30 | 55 ± 8.1 | 3.11 ± 0.83 (ctr); 2.38 ± 0.75 (test) | 6 | DBBM | XG (granules 1–2 mm) (Lumina porous) |
| Grasso, 2020 [27] * | 16 | 23 | 54 ± 7 | <4 | 6 | Deproteinized equine bone mineral (DEBM) | Anorganic bovine bone (DBBM) |
| Kim, 2020 [28] | 37 | 51 | 53.0 ± 8.17; 51.07 ± 9.67; 54.15 ± 8.24 | <5 | 6 | Anorganic bovine bone | Mineralized cancellous bone allograft |
| Velasco-Ortega, 2020 [29] | 24 | 24 | BCP: 57.63 ± 13.97; BCP+HA: 60.63 ± 11.21; ABBM: 49.5 ± 11.28 | <3 | 9 | Demineralized bovine bone | Test 1: TCP (particle size 250 to 1000 μm); Test 2: TCP as in test 1 + crosslinked HA 2:1 |
| Pereira, 2020 [30] | 40 | 40 | 32–65 | <5 | 6 | Autologous bone (G1) | G2: Bioactive glass; G3: Bioactive glass +Autologous bone; G4: Bio-Oss; G5: Bio-Oss+Auto |
| Tanaka, 2019 [31] * | 12 | 12 | 55.3 ± 11.7 | <4 | 9 | Collagenated corticocancellous porcine bone (Alveolar Crest Sites) | Collagenated corticocancellous porcine bone (Antrostomy sites) |
| Pang, 2019 [32] * | 25 | 28 | 56.67 ± 10.53 | 2.92 ± 2.17 (Inducera)/3.69 ± 4.85 | 6 | DBBM (Bio-Oss) | Calcium phosphate crystal double-coated bovine bone |
| Batas, 2019 [33] | 6 | 12 | ۔ | <3 | 6 | DBBM | DBBM+PRGF |
| Oh, 2019 [34] | 56 | 60 | 54.3 (20–69) | 2–6 | 6 | DBBM | Biphasic calcium phosphate |
| Scarano, 2018 [35] | 23 | 27 | 52 | NR | 6 | Group 1: Collagen porcine bone + CM | Autologous bone |
| Nizam, 2018 [36] | 13 | 26 | 49.92 ± 10.37 | <5 | 6 | DBBM+L-PRF | DBBM |
| Taschieri, 2016 [37] | 20 | 20 | 49–69 | <4 | 6 | DBBM | BCP+PRP |
| Menezes, 2018 [38] | 21 | 27 | NR | <5 | 6 | Autogenous bone graft | Biogran (AP) + Autologous bone |
| Theodoro, 2018 [39] * | 12 | 12 | 48.12 ± 6.24 | 4 to 5 | 6 | AB/HA | AB/HA+LLLT |
| Pareira, 2017 [40] | 22 | 36 | NR | <5 | 6 | Autogenous bone | Test 1: Auto; Test 2: Auto+Biogran |
| Stacchi, 2017 [41] | 28 | 52 | 60.1 | 2 | 6 | ABB | NHA |
| Lee, 2017 [42] * | 16 | 20 | 44.04 ± 4.48 | Ctr: (2.06 ± 0.43 mm)/Test: (1.90 ± 0.80 mm) | 6 | XG (DBBM, ctr) | XG (DPBM, test) |
| Rodriguez y Baena, 2017 [43] | 8 | 12 | 56 ± 13 | <4 | 6 | Deproteinized bovine bone | Poly(lactic-co-glycolic acid/Hydroxyapatite |
| Comert Kiliç, 2017 [44] | 26 | 18 | 31.51 ± 8.52 (ctr); 34.01 ± 9.59 (test) | <7 | 6 | β-TCP | β-TCP+PRP |
| Dogan, 2017 [45] | 13 | 26 | (33–69) | <4 | 4 | Collagenated heterologous bone graft | Hyaluronic matrix and collagenated heterologous bone graft |
| Kolerman, 2017 [46] | 13 | 26 | 58 | <5 | 9 | BCP | Freeze dried bone allografts |
| Meimandi, 2017 [47] | 10 | 20 | (30–60) | 2 to 4 | 6 | Alloplast | Bone graft + Growth factors |
| Portelli, 2017 [48] | 8 | 12 | 56 | 4 to 5 | 8 | Xenografts | Alloplast |
| Meymandi, 2017 [49] * | 9 | 18 | (42–57) | 12 to 13 | 6 | Easy Graft Crystal (Alloplast) | Nano Bone (Alloplast) |
| Nery, 2017 [50] | 10 | 20 | (35–75) | 3 and 5 | 6 | β-TCP/HA (BC) | β-TCP/HA mixed with EMD (BC+EMD) |
| Pereira, 2017 [51] | 30 | 30 | NR | <5 | 6 | Biogran | Biogran with autogenous bone graft and Autogenous bone graft |
| Amoian, 2016 [52] * | 20 | 20 | 49 ± 4.32 | NR | 6 | DFDBA | DFDBA |
| Jelusic, 2016 [53] * | 60 | 67 | 55.92 | NR | 6 | Monophasic (100% ß-TCP) | Biphasic (60% HA and 40% ß-TCP) |
| Nappe CE 2016 [54] * | 18 | 25 | 67 | NR | 6 | XG | Alloplast + Allograft |
| Duque Netto, 2016 [55] * | 10 | 20 | NR | <4 | 2 and 6 | Auto 6 months | Auto 2 months |
| Ahmet, 2016 [56] | 20 | 20 | 53.8 (47–65) | <5 | 5 | Biphasic CS + Alloplast (60%HA, 40% β-TCP) | Biphasic CS + DBBM |
| Badr, 2016 [57] * | 22 | 22 | 36 (17–73) | NR | 6 | Autograft | Auto+PRP |
| Kim, 2016 [58] | 30 | 30 | 54.6 ± 0.42 | 2.50 ± 1.01/2.87 ± 0.74 | 6 | Auto+PC | AG+XG+PC |
| Alayan, 2016 [59] | 16 | 40 | 57.7 ± 0.43 (ctr);54.6 ± 0.33 (test) | <5 and >1 | 5 | Anorganic bovine bone + Autogenous bone | Collagen-stabilized anorganic bovine bone |
| Danesh-Sani, 2016 [60] | 10 | 20 | (25–72) | <5 | 6 to 8 | Autogenous bone | BCP (60% hydroxyapatite and 40% β-TCP) |
| de Oliveira, 2016 [61] | 15 | 21 | 2,2 | 6 | Bovine bone | Bovine+BMC (bone marrow concentrate) | |
| Payer, 2015 [62] | 6 | 12 | 58.2 | <3 | 6 | Bovine bone | Bovine bone + Tibial BM aspirate |
| Kim, 2015 [63] | 41 | 41 | 52.37 | <3 | 6 | Xenografts | rhBMP-2 + Microporous BCP |
| Kim, 2015 [64] | 127 | 127 | 53.19 (test); 53.15 (ctr) | <4 | 3 | Xenografts | rhBMP-2 + Microporous BCP |
| Sehn, 2015 [65] | 29 | 34 | 51.32 ± 6.44 | <5 | 6 | Fresh-frozen bone allograft | Bovine bone mineral + Fresh-frozen bone allograft |
| Taschieri, 2015 [66] | 6 | 12 | (48–71) | <4 | 6 | Xenografts | Alloplast |
| Xavier, 2015 [67] | 15 | 30 | 6 | <3 | Autogenous | Allograft | |
| Pasquali, 2015 [68] | 8 | 16 | 55.4 ± 9.2 | <4 | 6 | Bio-Oss | BMAC |
| de Lange, 2014 [69] | 5 | 10 | 66 (64–71) | 2,4 | 12 | DBA | BCP (Straumann BoneCeramic; Institut Straumann AG) |
| Correia, 2014 [70] | 6 | 12 | (42–64) | 2–4.6 | 6 | Autogenous bone | Xenograft |
| Garlini, 2014 [71] | 5 | 10 | 57 | <5 | 6 to 8 | Xenograft | Algipore |
| Wildburger, 2014 [72] | 7 | 14 | 58 (47–72) | <3 | 3 and 6 | Bovine bone | BOVINE Bone + MSC |
| Torres, 2013 [73] | 93 | 13 | <65:38; >65:55 | <7 | 6 | DBBM + membrane | DBBM |
| Froum, 2013 [74] | 24 | 48 | 61.2 ± 7.7 | 4 to 5 | 6 to 9 | Allografts | Bone grafts + bioactive protein |
| Froum, 2013 [75] | 24 | 24 | 61.2 | 4 to 5 | 4–5 and 7–9 | Xenograft | XG+PDGF |
| Khairy, 2013 [76] | 15 | 10 | 38 (22–54) | <5 | 6/4 and 6 | Autogenous bone | Autologous bone + PRP |
| Schmitt, 2013 [77] | 30 | 36 | (38–79) | <4 | 5 | Autologous bone | Mineralized cancellous bone Allograft |
| Tosta, 2013 [78] | 30 | 30 | (18–70) | 3 and 6 | 9 | Autogenous | BCP |
| Anitua, 2012 [79] | 5 | 10 | 52 ± 11 (29–73) | 1–3 | 5 | DBBM | DBBM+PRGF |
| Kao, 2012 [80] | 22 | 20 | 50.8 | <5 | 6 | Bio-Oss | Bio-Oss + rhBMP-2/ACS |
| Kurkcu, 2012 [81] | 23 | 23 | 48.65 | <5 | 6,5 | Xenografts | Alloplast |
| Lindgren, 2012 [82] | 11 | 22 | 67 (50–79) | <5 | 36 | Xenografts | Alloplast |
| Zhang, 2012 [83] | 10 | 11 | 43.5 (test);46.2 (ctr) | 6 | <5 | Xenografts | Bone Grafts and Growth Factors |
| Wagner, 2012 [84] | 85 | 117 | 52.5 (22.7–82.6) | 2 to 5 | 6 | Biphasic Ca(PO)4 + Fibrin sealant | Autogenous bone graft with Bovine Xenograft |
| Pikdöken, 2011 [85] | 24 | 24 | 59.83 (57.92) | 4 | <5 | Xenografts | Autogenous + XG |
| Stavropoulos, 2011 [86] | 31 | 31 | 53.8 ± 12.1 | <5 | 4 | rhGDF-5/b-TCP/3-month | Biologics |
| Rickert, 2011 [87] | 23 | 22 | 60.8 ± 5.9 | 1 to 3 | 4 | Bovine bone mineral + Autogenous bone | Bovine bone mineral + Autogenous stem cells |
| Sauerbier, 2011 [88] | 36 | 44 | 56.6 | 2 to 3 | 3 to 4 | Autogenous + Xenograft | Bone grafts + mesenchymal cells |
| Galindo-Moreno, 2011 [89] | 28 | 28 | 47.3 ± 9.8 | <5 | 6 | Bovine+AB 1:1 | Bovine + AB 4:1 |
| de Vicente, 2010 [90] * | 35 | 42 | (34–69) | <4 (severely atrophic) | 9 | Bovine-derived hydroxyapatite (2-stage) | Bovine-derived hydroxyapatite (1-stage) |
| Felice, 2009 [91] | 10 | 20 | 50 (35–60) | 1–5 | 6 | DBBM | No graft + rigid synthetic resorbable membrane |
| Cordaro, 2008 [92] | 37 | 48 | NR | ≥3 and <8 mm | 8 | Straumann Bone Ceramic | Anorganic bovine bone |
| Froum, 2008 [93] | 12 | 21 | NR | <5 | 6 to 8 | Xenograft | Alloplast |
| Galindo-Moreno, 2008 [94] | 5 | 10 | 62 (45–78) | <5 | 6 | Bovine+AB | Bioglass + AB |
| Froum, 2006 [95] | 13 | 22 | 59 | <5 | 8 | Mineralized cancellous bone allograft | Anorganic bovine bone |
| Zijderveld, 2005 [96] | 10 | 16 | (18–70) | 5 ± 2.05 | 12 | Autologous chin bone | β-TCP |
| Raghoebar, 2005 [97] | 5 | 10 | 58.4 ± 1.9 | <5 | 3 | Autogenous bone | Autogenous bone + PRP |
| Szabo, 2005 [98] | 20 | 40 | 52 | <5 | 6 | Autogenous | Alloplast |
| Zerbo, 2004 [99] | 9 | 14 | 52 | 6 | <4 | Autogenous bone | TCP |
| Wiltfang, 2003 [100] | 35 | 35 | 45 (37–54) (test); 47 (32–64) (ctr) | 2 to 7 | 6 | B-TCP | B-TCP + PRP |
| Hallman, 2002 [101] | 21 | 22 | 54 | <5 | 12 to 15 | Autogenous bone | Autogenous + XG |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khijmatgar, S.; Del Fabbro, M.; Tumedei, M.; Testori, T.; Cenzato, N.; Tartaglia, G.M. Residual Bone Height and New Bone Formation after Maxillary Sinus Augmentation Procedure Using Biomaterials: A Network Meta-Analysis of Clinical Trials. Materials 2023, 16, 1376. https://doi.org/10.3390/ma16041376
Khijmatgar S, Del Fabbro M, Tumedei M, Testori T, Cenzato N, Tartaglia GM. Residual Bone Height and New Bone Formation after Maxillary Sinus Augmentation Procedure Using Biomaterials: A Network Meta-Analysis of Clinical Trials. Materials. 2023; 16(4):1376. https://doi.org/10.3390/ma16041376
Chicago/Turabian StyleKhijmatgar, Shahnavaz, Massimo Del Fabbro, Margherita Tumedei, Tiziano Testori, Niccolò Cenzato, and Gianluca Martino Tartaglia. 2023. "Residual Bone Height and New Bone Formation after Maxillary Sinus Augmentation Procedure Using Biomaterials: A Network Meta-Analysis of Clinical Trials" Materials 16, no. 4: 1376. https://doi.org/10.3390/ma16041376
APA StyleKhijmatgar, S., Del Fabbro, M., Tumedei, M., Testori, T., Cenzato, N., & Tartaglia, G. M. (2023). Residual Bone Height and New Bone Formation after Maxillary Sinus Augmentation Procedure Using Biomaterials: A Network Meta-Analysis of Clinical Trials. Materials, 16(4), 1376. https://doi.org/10.3390/ma16041376










