Enhanced Release of Calcium Ions from Hydroxyapatite Nanoparticles with an Increase in Their Specific Surface Area
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials and Synthesis of Nanoparticles
2.2. Characterization of Nanoparticles
2.3. Determination of the Amount of Ca2+ Ions Released
3. Results
3.1. Synthesis of Nanoparticles
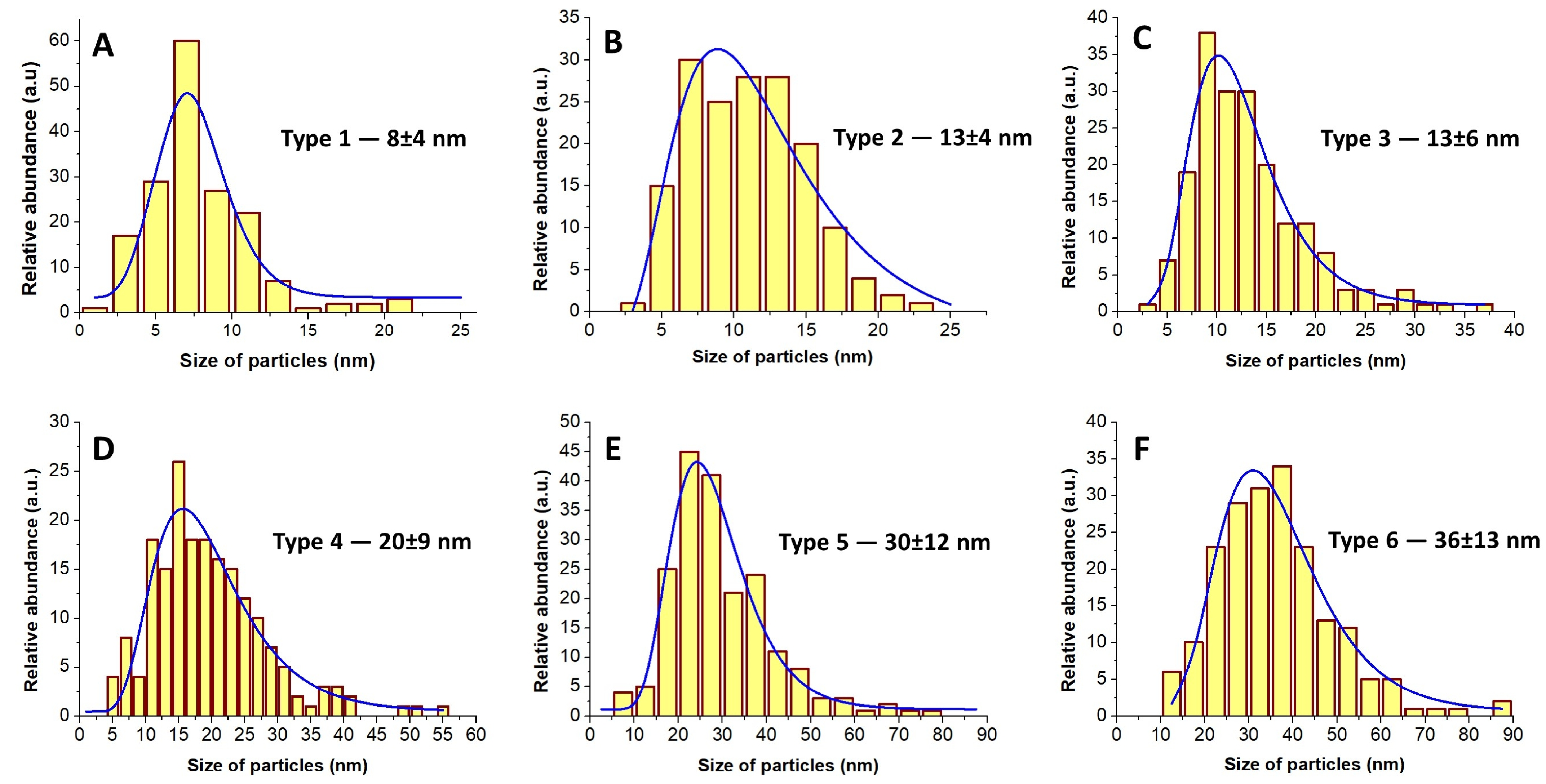
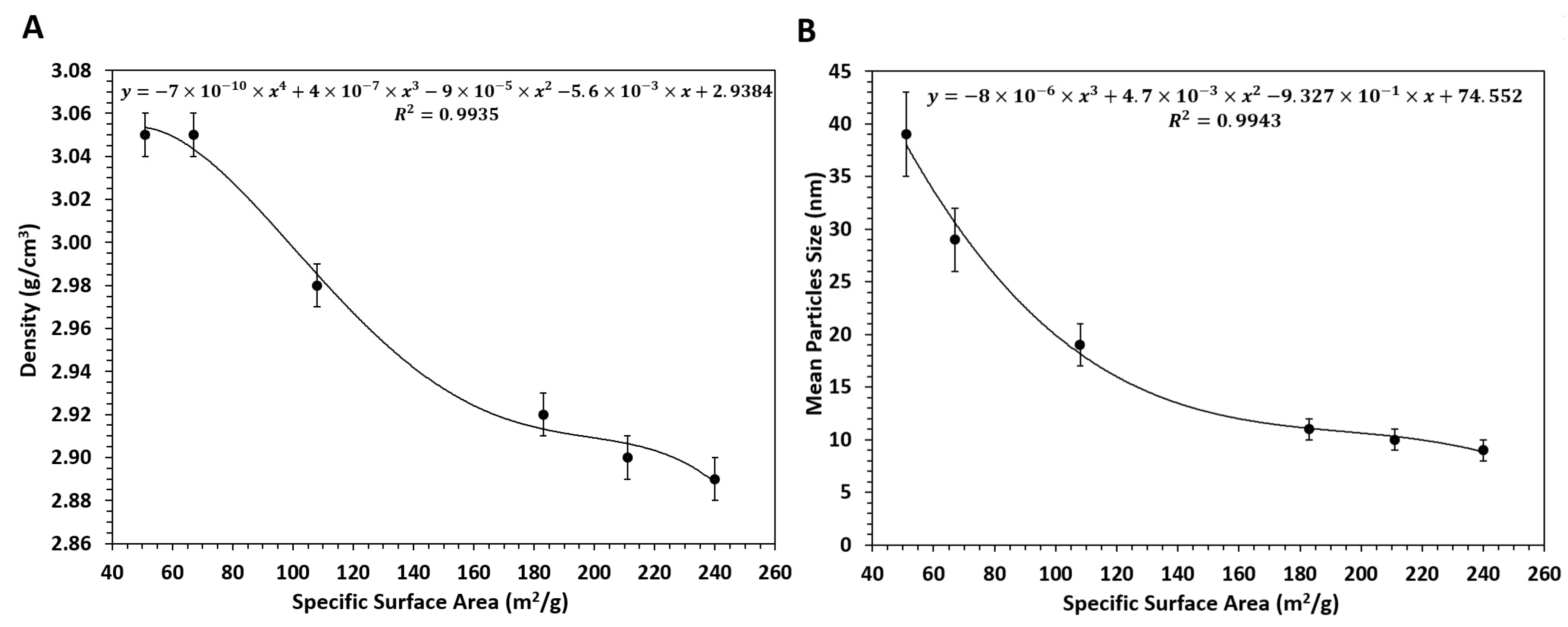
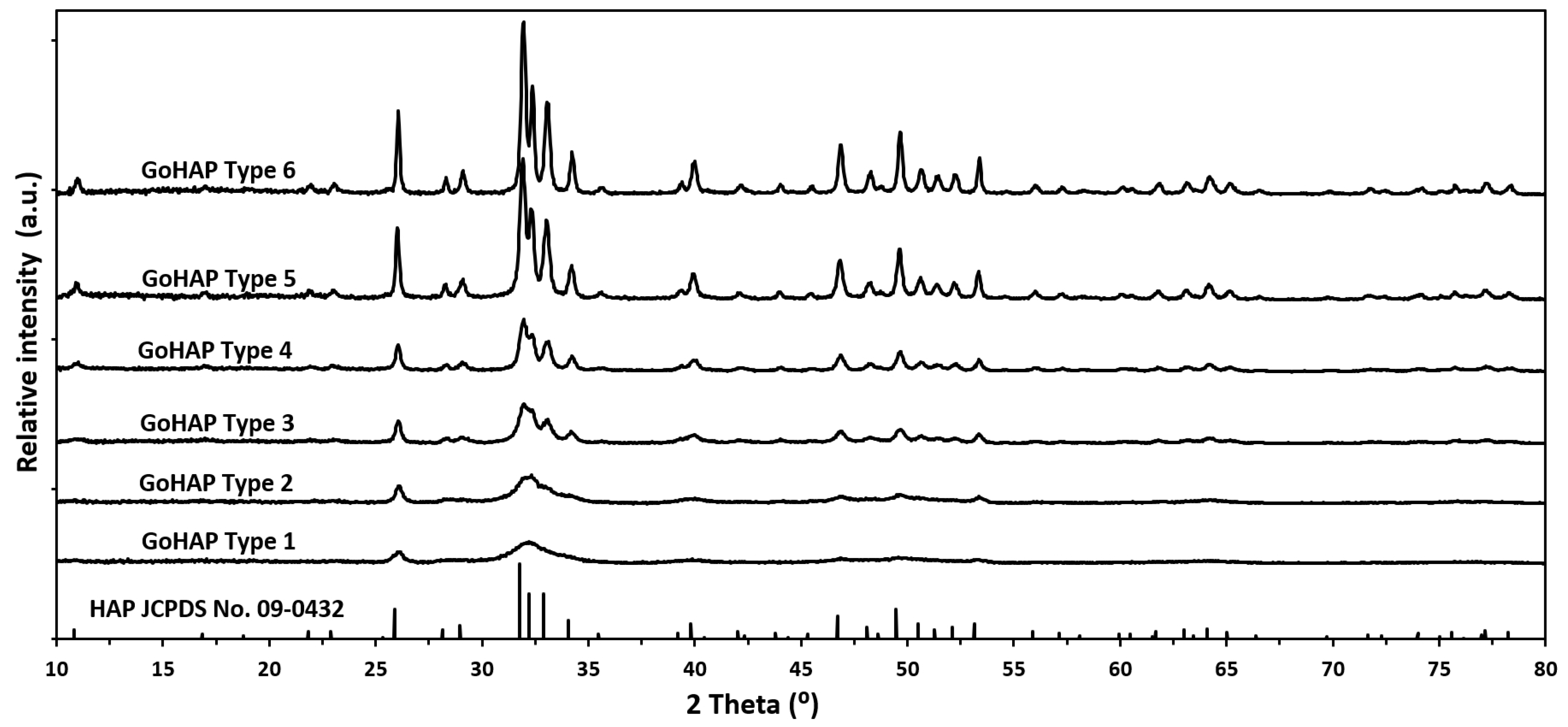
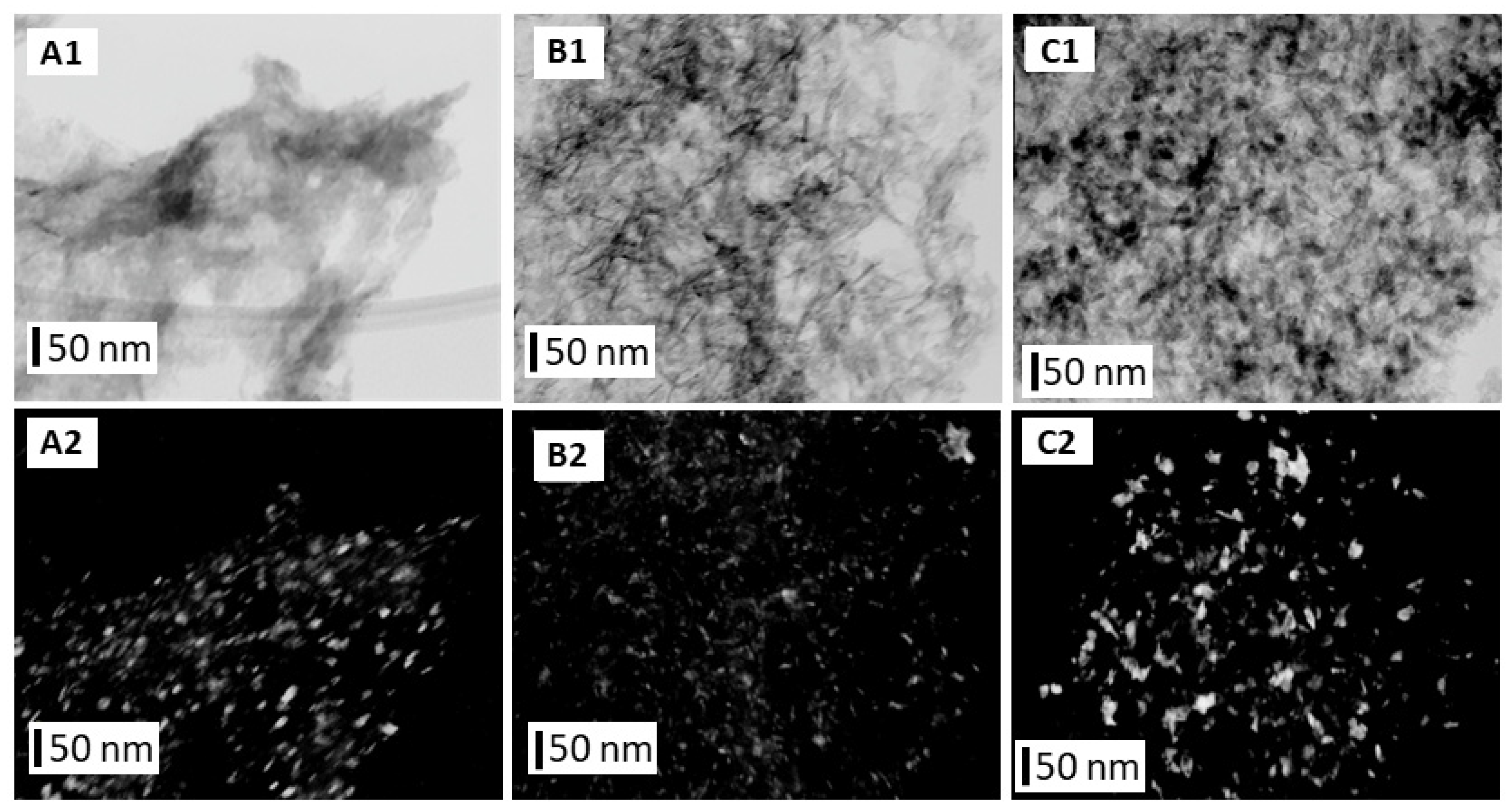
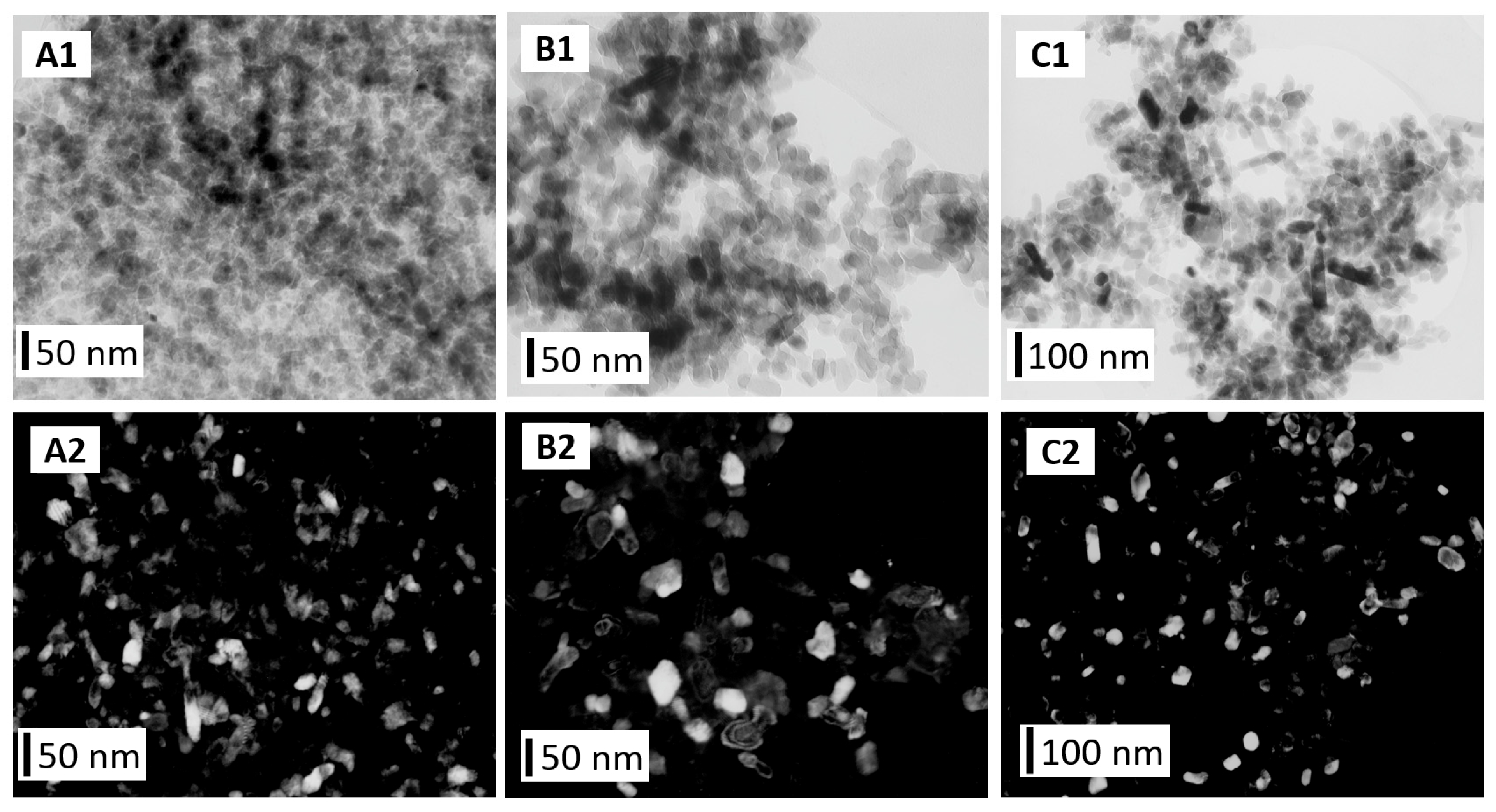
3.2. Characterization of Nanoparticles
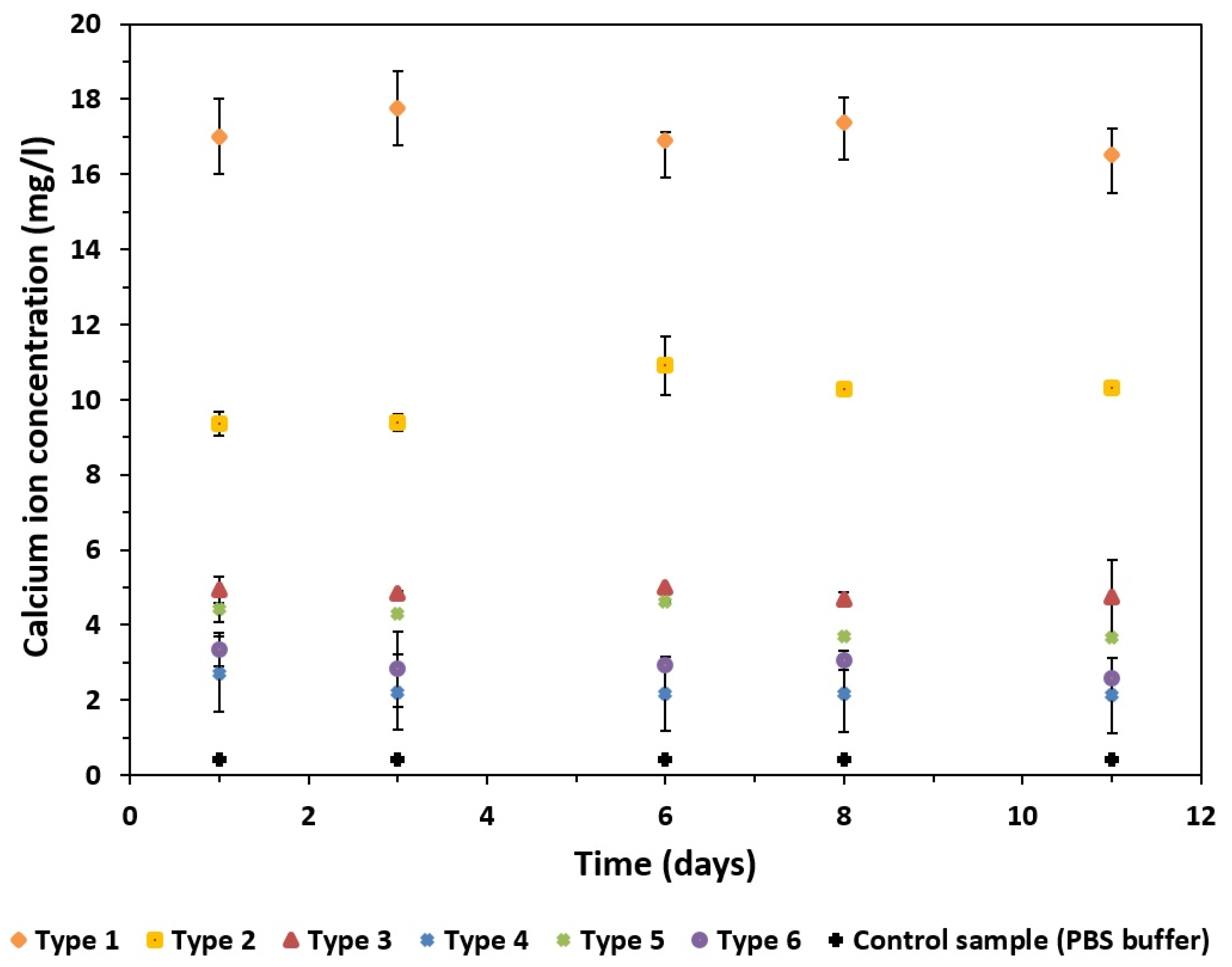
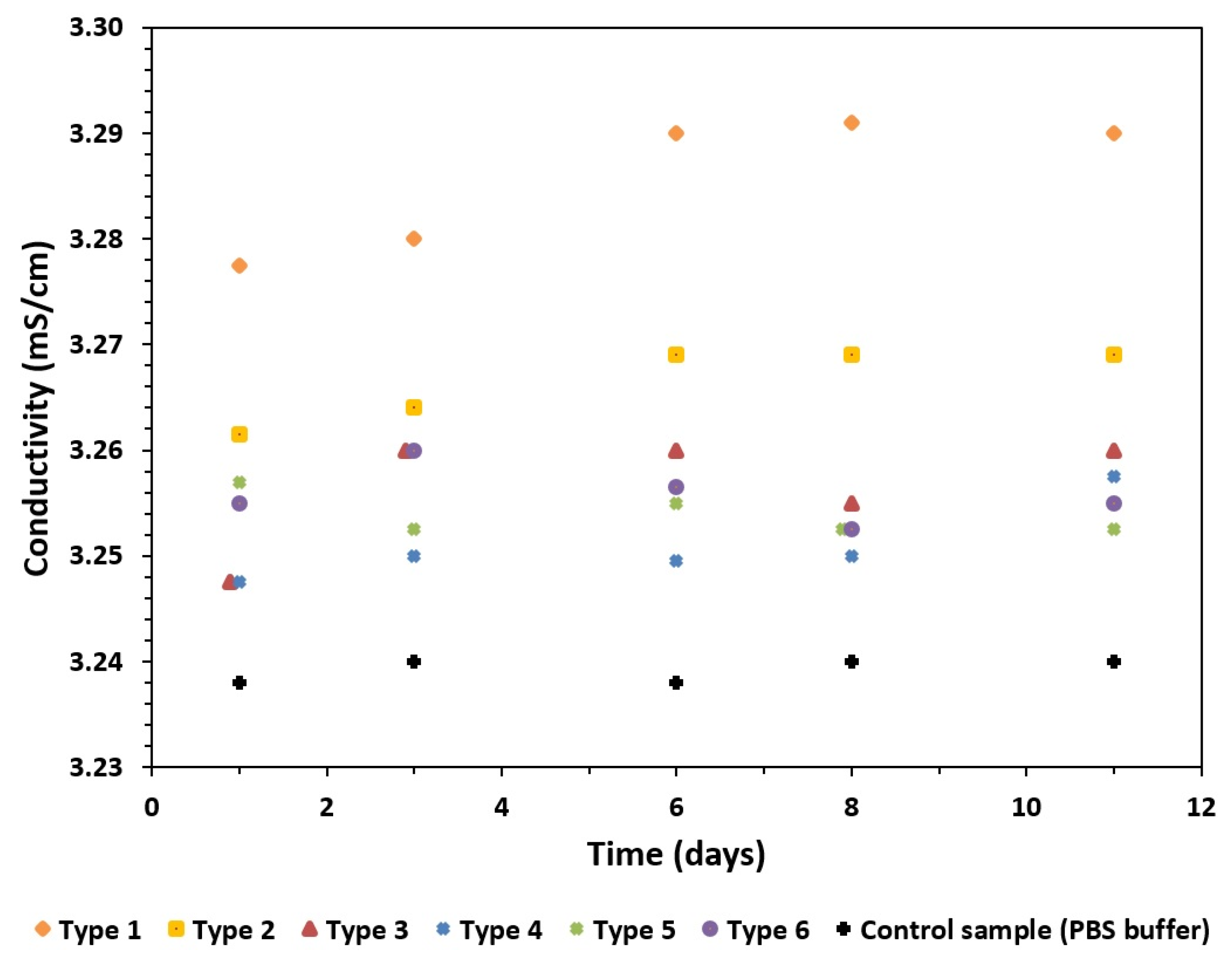
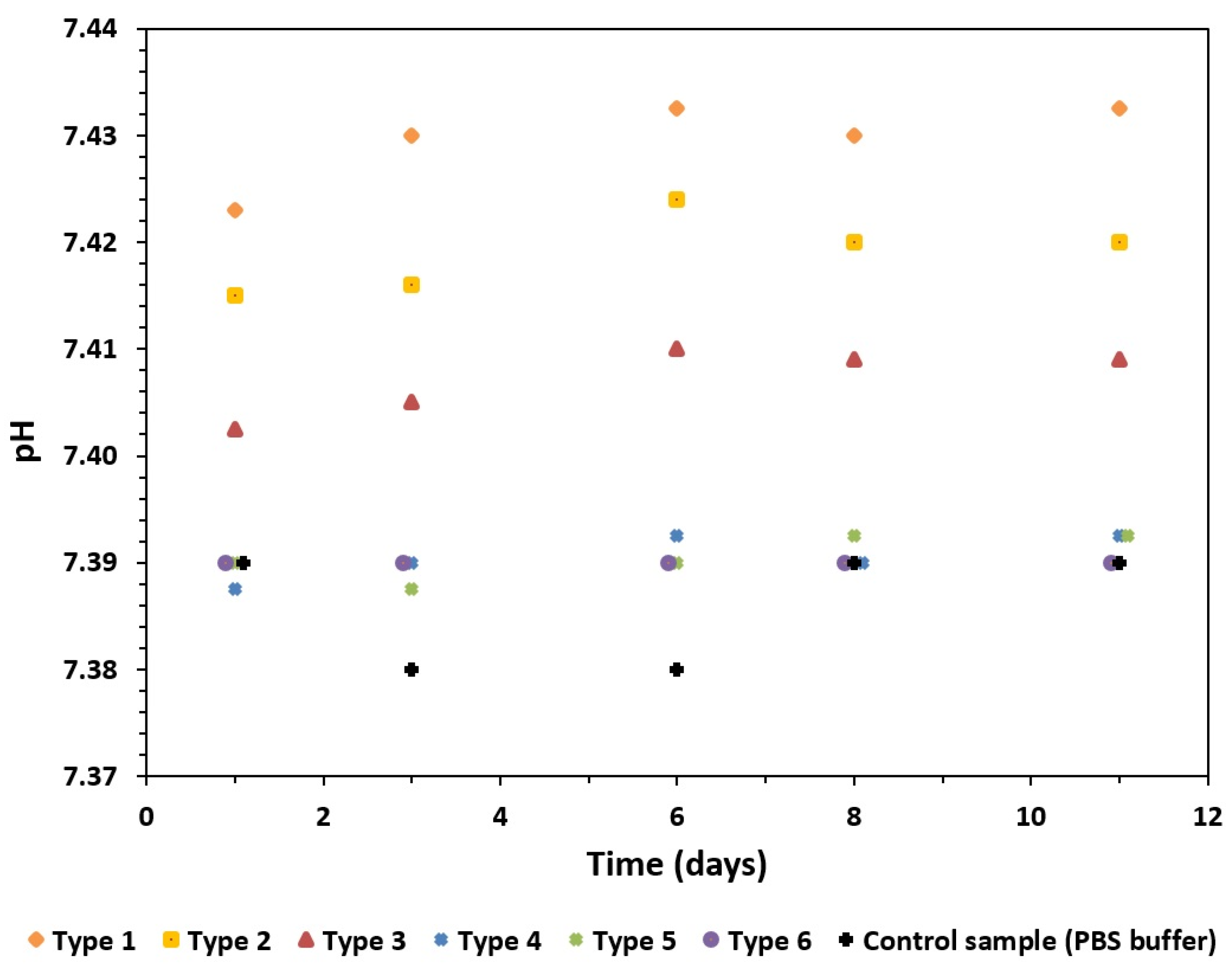
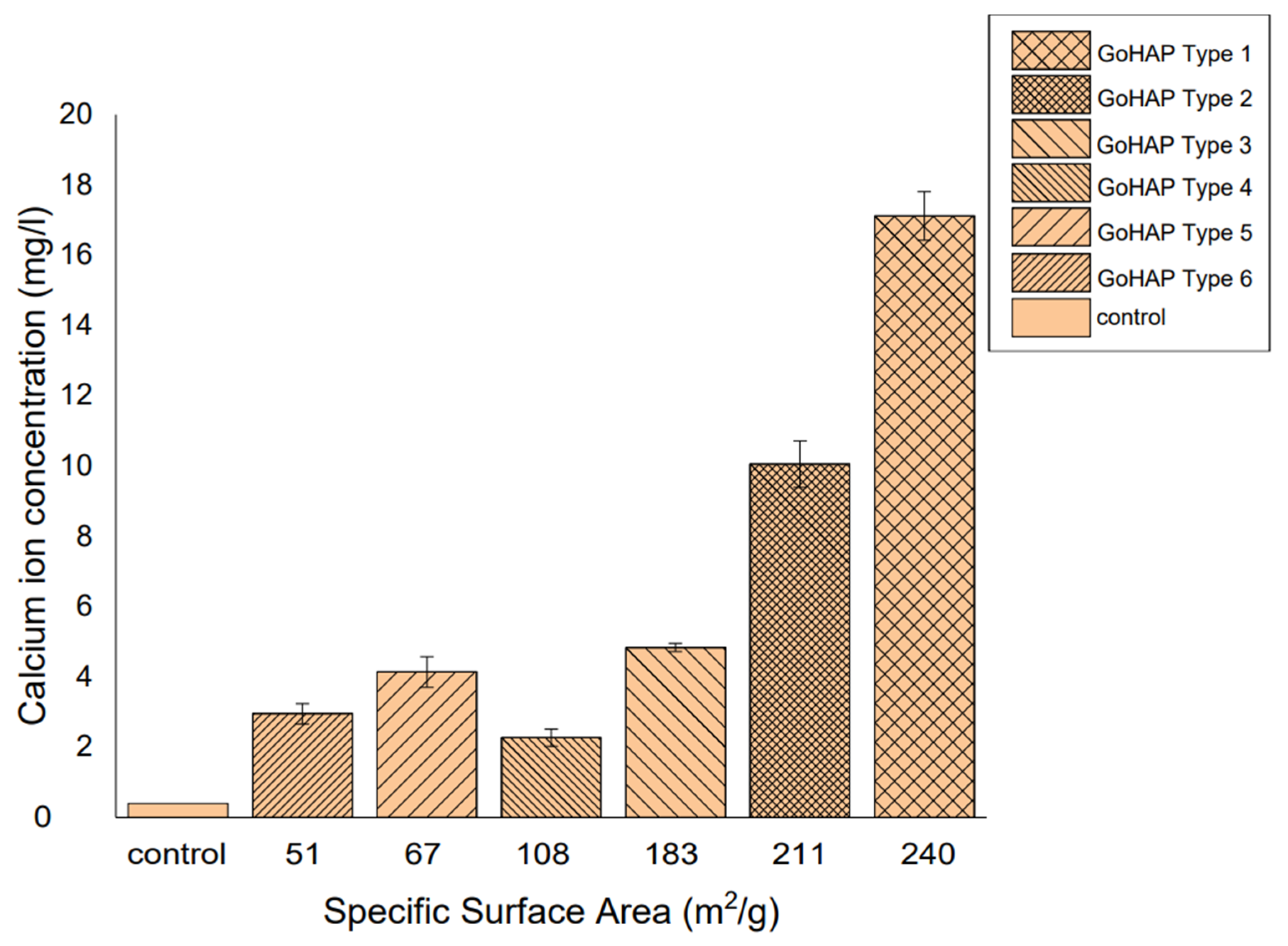
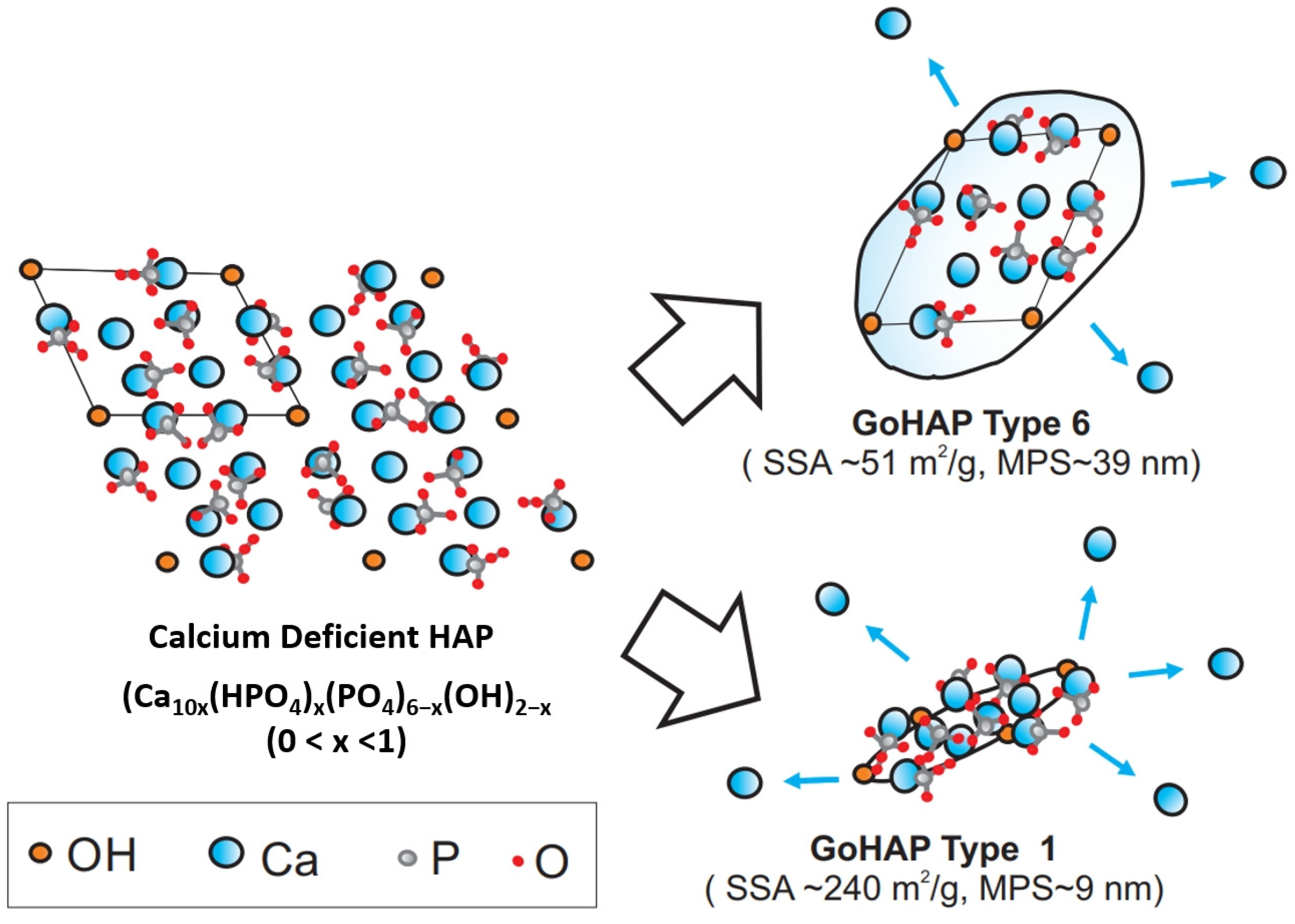
3.3. Calcium-Ion-Release Results
4. Discussion
4.1. Structural and Chemical Characterization
4.2. Ion-Release Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gimigliano, F.; Resmini, G.; Moretti, A.; Aulicino, M.; Gargiulo, F.; Gimigliano, A.; Liguori, S.; Paoletta, M.; Iolascon, G. Epidemiology of Musculoskeletal Injuries in Adult Athletes: A Scoping Review. Medicina 2021, 57, 1118. [Google Scholar] [CrossRef] [PubMed]
- Sebbag, E.; Felten, R.; Sagez, F.; Sibilia, J.; Devilliers, H.; Arnaud, L. The world-wide burden of musculoskeletal diseases: A systematic analysis of the World Health Organization Burden of Diseases Database. Ann. Rheum. Dis. 2019, 78, 844–848. [Google Scholar] [CrossRef] [PubMed]
- Kanczler, J.M.; Wells, J.A.; Gibbs, D.M.R.; Marshall, K.M.; Tang, D.K.O.; Oreffo, R.O.C. Chapter 50-Bone Tissue Engineering and Bone Regeneration. In Principles of Tissue Engineering, 5th ed.; Lanza, R., Langer, R., Vacanti, J.P., Atala, A., Eds.; Academic Press: San Diego, CA, USA, 2020; pp. 917–935. ISBN 9780128184226. [Google Scholar] [CrossRef]
- Feng, X. Chemical and Biochemical Basis of Cell-Bone Matrix Interaction in Health and Disease. Curr. Chem. Biol. 2009, 3, 189–196. [Google Scholar] [CrossRef]
- Cheng, H.; Chabok, R.; Guan, X.; Chawla, A.; Li, Y.; Khademhosseini, A.; Jang, H.L. Synergistic interplay between the two major bone minerals, hydroxyapatite and whitlockite nanoparticles, for osteogenic dierentiation of mesenchymal stem cells. Acta Biomater. 2018, 69, 342–351. [Google Scholar] [CrossRef] [PubMed]
- Batool, S.; Liaqat, U.; Hussain, Z.; Sohail, M. Synthesis, Characterization and Process Optimization of Bone Whitlockite. Nanomaterials 2020, 10, 1856. [Google Scholar] [CrossRef] [PubMed]
- Morgan, E.F.; Barnes, G.L.; Einhorn, T.A. The bone organ system: Form and function. In Osteoporosis, 3rd ed.; Marcus, R., Feldman, D., Nelson, D.A., Rosen, C.J., Eds.; Academic Press: San Diego, CA, USA, 2007; pp. 3–25. ISBN 978-0-12-370544-0. [Google Scholar]
- Zhu, W.; Robey, P.G.; Boskey, A.L. The Regulatory Role of Matrix Proteins in Mineralization of Bone. In Osteoporosis, 3rd ed.; Marcus, R., Feldman, D., Nelson, D.A., Rosen, C.J., Eds.; Academic Press: San Diego, CA, USA, 2007; pp. 191–240. ISBN 978-0-12-370544-0. [Google Scholar]
- Dorozhkin, S.V. Bioceramics of calcium orthophosphates. Biomaterials 2010, 31, 1465–1485. [Google Scholar] [CrossRef]
- Hench, L.L. Bioceramics. J. Am. Ceram. Soc. 1998, 81, 1705–1728. [Google Scholar] [CrossRef]
- Suchanek, W.; Yoshimura, M. Processing and properties of hydroxyapatite-based biomaterials for use as hard tissue replacement implants. J. Mater. Res. 1998, 13, 94–117. [Google Scholar] [CrossRef]
- Ojeda, E.; García-Barrientos, Á.; Martínez de Cestafe, N.; Alonso, J.M.; Pérez-González, R.; Sáez-Martínez, V. Nanometric Hydroxyapatite Particles as Active Ingredient for Bioinks: A Review. Macromol 2022, 2, 20–29. [Google Scholar] [CrossRef]
- Kuśnieruk, S.; Wojnarowicz, S.; Chodara, A.; Chudoba, T.; Gierlotka, S.; Lojkowski, W. Influence of hydrothermal synthesis parameters on the properties of hydroxyapatite nanoparticles. Beilstein J. Nanotechnol. 2016, 7, 1586–1601. [Google Scholar] [CrossRef]
- Ielo, I.; Calabrese, G.; De Luca, G.; Conoci, S. Recent Advances in Hydroxyapatite-Based Biocomposites for Bone Tissue Regeneration in Orthopedics. Int. J. Mol. Sci. 2022, 23, 9721. [Google Scholar] [CrossRef] [PubMed]
- Rogowska-Tylman, J.; Locs, J.; Salma, I.; Woźniak, B.; Pilmane, M.; Zalite, V.; Wojnarowicz, J.; Kędzierska-Sar, A.; Chudoba, T.; Szlązak, K.; et al. In Vivo and in Vitro Study of a Novel Nanohydroxyapatite Sonocoated Scaffolds for Enhanced Bone Regeneration. Mater. Sci. Eng. C 2019, 99, 669–684. [Google Scholar] [CrossRef] [PubMed]
- Cavalcante, M.D.; de Menezes, L.R.; Rodrigues, E.J.D.; Tavares, M.I.B. In vitro characterization of a biocompatible composite based on poly (3-hydroxybutyrate)/hydroxyapatite nanoparticles as a potential scaffold for tissue engineering. J. Mech. Behav. Biomed. 2022, 128, 105138. [Google Scholar] [CrossRef] [PubMed]
- Kavasi, R.-M.; Coelho, C.C.; Platania, V.; Quadros, P.A.; Chatzinikolaidou, M. In Vitro Biocompatibility Assessment of Nano-Hydroxyapatite. Nanomaterials 2021, 11, 1152. [Google Scholar] [CrossRef]
- Cintra, C.C.V.; Ferreira-Ermita, D.A.C.; Loures, F.H.; Araújo, P.M.A.G.; Ribeiro, I.M.; Araújo, F.R.; Valente, F.L.; Reis, E.C.C.; Costa, A.C.F.M.; Bicalho, S.M.C.M.; et al. In vitro characterization of hydroxyapatite and cobalt ferrite nanoparticles compounds and their biocompatibility in vivo. J. Mater. Sci. Mater. Med. 2022, 33, 21. [Google Scholar] [CrossRef]
- Biazar, E.; Daliri, J.M.; Heidari, S.K.; Navayee, A.D.; Kamalvand, M.; Sahebalzamani, M.; Royanian, F.; Shabankhah, M.; Farajpour, F.L. Characterization and biocompatibility of hydroxyapatite nanoparticles extracted from fish bone. J. Bioeng. Res. 2020, 2, 10–19. [Google Scholar] [CrossRef]
- Turon, P.; Del Valle, L.J.; Alemán, C.; Puiggalí, J. Biodegradable and Biocompatible Systems Based on Hydroxyapatite Nanoparticles. Appl. Sci. 2017, 7, 60. [Google Scholar] [CrossRef]
- Torres, E.C.L.; De Sousa, E.M.B.; Cipreste, M.F. A Brief Review on Hydroxyapatite Nanoparticles Interactions with Biological Constituents. J. Biomater. Nanobiotechnol. 2022, 13, 24–44. [Google Scholar] [CrossRef]
- Borkowski, L.; Jojczuk, M.; Belcarz, A.; Pawlowska-Olszewska, M.; Kruk-Bachonko, J.; Radzki, R.; Bienko, M.; Slowik, T.; Lübek, T.; Nogalski, A.; et al. Comparing the Healing Abilities of Fluorapatite and Hydroxyapatite Ceramics in Regenerating Bone Tissue: An In Vivo Study. Materials 2023, 16, 5992. [Google Scholar] [CrossRef]
- Nalesso, P.R.L.; Vedovatto, M.; Gregório, J.E.S.; Huang, B.; Vyas, C.; Santamaria-Jr, M.; Bártolo, P.; Caetano, G.F. Early In Vivo Osteogenic and Inflammatory Response of 3D Printed Polycaprolactone/Carbon Nanotube/Hydroxyapatite/Tricalcium Phosphate Composite Scaffolds. Polymers 2023, 15, 2952. [Google Scholar] [CrossRef]
- George, S.M.; Nayak, C.; Singh, I.; Balani, K. Multifunctional Hydroxyapatite Composites for Orthopedic Applications: A Review. ACS Biomater. Sci. Eng. 2022, 8, 3162–3186. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, H.L.; Da Rosa, W.L.O.; Cuevas-Suárez, C.E.; Carreño, N.L.V.; Da Silva, A.F.; Guim, T.N.; Dellagostin, O.A.; Piva, E. Histological Evaluation of Bone Repair with Hydroxyapatite: A Systematic Review. Calcif. Tissue. Int. 2017, 101, 341–354. [Google Scholar] [CrossRef] [PubMed]
- Bal, Z.; Kaito, T.; Korkusuz, F.; Yoshikawa, H. Bone regeneration with hydroxyapatite-based biomaterials. Emergent Mater. 2020, 3, 521–544. [Google Scholar] [CrossRef]
- Peacock, M. Calcium metabolism in health and disease. Clin. J. Am. Soc. Nephrol. 2010, 5 (Suppl. S1), S23–S30. [Google Scholar] [CrossRef]
- O’Neill, E.; Awale, G.; Daneshmandi, L.; Umerah, O.; Lo, K.W.-H. The roles of ions on bone regeneration. Drug Discov. Today 2018, 23, 879–890. [Google Scholar] [CrossRef] [PubMed]
- Liu, D.; Genetos, D.C.; Shao, Y.; Geist, D.J.; Li, J.; Ke, H.Z.; Turner, C.H.; Duncan, R.L. Activation of extracellular-signal regulated kinase (ERK 1/2) by fluid shear is Ca2+- and ATP-dependent in MC3T3-E1 osteoblasts. Bone 2008, 42, 644–652. [Google Scholar] [CrossRef] [PubMed]
- Danciu, T.E.; Adam, R.M.; Naruse, K.; Freeman, M.R.; Hauschka, P.V. Calcium regulates the PI3K-Akt pathway in stretched osteoblasts. FEBS Lett. 2003, 536, 193–197. [Google Scholar] [CrossRef]
- Foskett, J.K.; White, C.; Cheung, K.-H.; Mak, D.-O.D.; Lacruz, R.S.; Habelitz, S.; Wright, J.T.; Paine, M.L.; Hohendanner, F.; DeSantiago, J.; et al. Inositol trisphosphate receptor Ca2+ release channels. Physiol. Rev. 2007, 87, 593–658. [Google Scholar] [CrossRef]
- Lim, S.S.; Chai, C.Y.; Loh, H.-S. In vitro evaluation of osteoblast adhesion, proliferation and differentiation on chitosan-TiO2 nanotubes scaffolds with Ca2+ ions. Mater. Sci. Eng. C Mater. Biol. Appl. 2017, 76, 144–152. [Google Scholar] [CrossRef]
- Seol, Y.-J.; Park, J.Y.; Jung, J.W.; Jang, J.; Girdhari, R.; Kim, S.W.; Cho, D.-W. Improvement of Bone Regeneration Capability of Ceramic Scaffolds by Accelerated Release of Their Calcium Ions. Tissue. Eng. Part A 2014, 20, 2840–2849. [Google Scholar] [CrossRef]
- Sun, J.; Wang, F.; Sui, Y.; She, Z.; Zhai, W.; Wang, C.; Deng, Y. Effect of particle size on solubility, dissolution rate, and oral bioavailability: Evaluation using coenzyme Q10 as naked nanocrystals. Int. J. Nanomed. 2012, 7, 5733–5744. [Google Scholar] [CrossRef]
- Saentho, A.; Wisawapipat, W.; Lawongsa, P.; Aramrak, S.; Prakongkep, N.; Wantana, K.; Christl, I. Speciation and pH- and particle size-dependent solubility of phosphorus in tropical sandy soils. Geoderma 2022, 408, 115590. [Google Scholar] [CrossRef]
- Jinno, J.; Kamada, N.; Miyake, M.; Yamada, K.; Mukai, T.; Odomi, M.; Toguchi, H.; Liversidge, G.G.; Higaki, K.; Kimura, T. Effect of particle size reduction on dissolution and oral absorption of a poorly water-soluble drug, cilostazol, in beagle dogs. J. Control Release 2006, 111, 56–64. [Google Scholar] [CrossRef] [PubMed]
- Babu, V.R.; Areefulla, S.; Mallikarjun, V. Solubility and dissolution enhancement: An overview. J. Pharm. Res. 2010, 3, 141–145. [Google Scholar]
- Dinh, H.T.T.; Tran, P.H.L.; Duan, W.; Lee, B.-J.; Tran, T.T.D. Nano-sized solid dispersions based on hydrophobic-hydrophilic conjugates for dissolution enhancement of poorly water-soluble drugs. Int. J. Pharm. 2017, 533, 93–98. [Google Scholar] [CrossRef] [PubMed]
- Tang, R.; Wanga, L.; Nancollas, G.H. Size-effects in the dissolution of hydroxyapatite: An understanding of biological demineralization. J. Mater. Chem. 2004, 14, 2341–2346. [Google Scholar] [CrossRef]
- Jassim, Z.E.; Rajab, N.A. Review on preparation, characterization, and pharmaceutical application of nanosuspension as an approach of solubility and dissolution enhancement. J. Pharm. Res. 2018, 12, 771–774. [Google Scholar]
- Dizaj, S.M.; Vazifehasl, Z.H.; Salatin, S.; Adibkia, K.H.; Javadzadeh, Y. Nanosizing of drugs: Effect on dissolution rate. Res. Pharm. Sci. 2015, 10, 95–108. [Google Scholar]
- Hecq, J.; Deleers, M.; Fanara, D.; Vranckx, H.; Amighi, K. Preparation and characterization of nanocrystals for solubility and dissolution rate enhancement of nifedipine. Int. J. Pharm. 2005, 299, 167–177. [Google Scholar] [CrossRef]
- Smoleń, D.; Chudoba, T.; Gierlotka, S.; Kędzierska, A.; Łojkowski, W.; Sobczak, K.; Święszkowski, W.; Kurzydowski, K.J. Hydroxyapatite Nanopowder Synthesis with a Programmed Resorption Rate. J. Nanomater. 2012, 2012, 841971. [Google Scholar] [CrossRef]
- Wojnarowicz, J.; Chudoba, T.; Lojkowski, W. A Review of Microwave Synthesis of Zinc Oxide Nanomaterials: Reactants, Process Parameters and Morphologies. Nanomaterials 2020, 10, 1086. [Google Scholar] [CrossRef] [PubMed]
- Mohd Pu’ad, N.A.S.; Abdul Haq, R.H.; Mohd Noh, H.; Abdullah, H.Z.; Idris, M.I.; Lee, T.C. Synthesis method of hydroxyapatite: A review. Mater. Today Proc. 2020, 29, 233–239. [Google Scholar] [CrossRef]
- Gui, X.; Peng, W.; Xu, X.; Su, Z.; Liu, G.; Zhou, Z.; Liu, M.; Li, Z.; Song, G.; Zhou, C.; et al. Synthesis and application of nanometer hydroxyapatite in biomedicine. Nanotechnol. Rev. 2022, 11, 2154–2168. [Google Scholar] [CrossRef]
- DileepKumar, V.G.; Sridhar, M.S.; Aramwit, P.; Krut’ko, V.K.; Musskaya, O.N.; Glazov, I.E.; Reddy, N. A review on the synthesis and properties of hydroxyapatite for biomedical applications. J. Biomater. Sci. Polym. Ed. 2022, 33, 229–261. [Google Scholar] [CrossRef]
- Latocha, J.; Wojasinski, M.; Sobieszuk, P.; Ciach, T. Synthesis of hydroxyapatite in a continuous reactor: A review. Synthesis of hydroxyapatite in a continuous reactor: A review. Chem. Process Eng. 2018, 39, 281–293. [Google Scholar] [CrossRef]
- Baskaran, T.; Mohammad, N.F.; Md Saleh, S.S.; Mohd Nasir, N.F.; Mohd Daud, F.D. Synthesis Methods of Doped Hydroxyapatite: A Brief Review. J. Phys. Conf. Ser. 2021, 2071, 012008. [Google Scholar] [CrossRef]
- Haider, A.; Haider, S.; Han, S.S.; Kang, I.-K. Recent advances in the synthesis, functionalization and biomedical applications of hydroxyapatite: A review. RSC Adv. 2017, 7, 7442. [Google Scholar] [CrossRef]
- Alorku, K.; Manoj, M.; Yuan, A. A plant-mediated synthesis of nanostructured hydroxyapatite for biomedical applications: A review. RSC Adv. 2020, 10, 40923. [Google Scholar] [CrossRef]
- Ferraz, M.P.; Monteiro, F.J.; Manuel, C.M. Hydroxyapatite nanoparticles: A review of preparation methodologies. J. Appl. Biomater. Biomech. 2004, 2, 74–80. [Google Scholar]
- Munir, M.U.; Salman, S.; Ihsan, A.; Elsaman, T. Synthesis, Characterization, Functionalization and Bio-Applications of Hydroxyapatite Nanomaterials: An Overview. Int. J. Nanomed. 2022, 17, 1903–1925. [Google Scholar] [CrossRef]
- Burdusel, A.-C.; Neacsu, I.A.; Birca, A.C.; Chircov, C.; Grumezescu, A.-M.; Holban, A.M.; Curutiu, C.; Ditu, L.M.; Stan, M.; Andronescu, E. Microwave-Assisted Hydrothermal Treatment of Multifunctional Substituted Hydroxyapatite with Prospective Applications in Bone Regeneration. J. Funct. Biomater. 2023, 14, 378. [Google Scholar] [CrossRef] [PubMed]
- Koutsopoulos, S. Synthesis and characterization of hydroxyapatite crystals: A review study on the analytical methods. J. Biomed. Mater. Res. 2002, 62, 600–612. [Google Scholar] [CrossRef] [PubMed]
- Gani, M.A.; Budiatin, A.S.; Lestari, M.L.A.D.; Rantam, F.A.; Ardianto, C.; Khotib, J. Fabrication and Characterization of Submicron-Scale Bovine Hydroxyapatite: A Top-Down Approach for a Natural Biomaterial. Materials 2022, 15, 2324. [Google Scholar] [CrossRef] [PubMed]
- Qi, M.-L.; He, K.; Huang, Z.-N.; Shahbazian-Yassar, R.; Xiao, G.-Y.; Lu, Y.-P.; Shokuhfar, T. Hydroxyapatite Fibers: A Review of Synthesis Methods. JOM 2017, 69, 1354–1360. [Google Scholar] [CrossRef]
- Shavandi, A.; Bekhit, A.E.-D.A.; Sun, Z.F.; Ali, A. A Review of Synthesis Methods, Properties and Use of Hydroxyapatite as a Substitute of Bone. J. Biomim. Biomater. Biomed. Eng. 2015, 25, 98–117. [Google Scholar] [CrossRef]
- Firdaus Hussin, M.S.; Abdullah, H.Z.; Idris, M.I.; Abdul Wahap, M.A. Extraction of natural hydroxyapatite for biomedical applications—A review. Heliyon 2022, 8, e10356. [Google Scholar] [CrossRef]
- Radulescu, D.-E.; Vasile, O.R.; Andronescu, E.; Ficai, A. Latest Research of Doped Hydroxyapatite for Bone Tissue Engineering. Int. J. Mol. Sci. 2023, 24, 13157. [Google Scholar] [CrossRef]
- Prasad, P.S.; Marupalli, B.C.G.; Das, S.; Das, K. Surfactant-assisted synthesis of hydroxyapatite particles: A comprehensive review. J. Mater. Sci. 2023, 58, 6076–6105. [Google Scholar] [CrossRef]
- Method for of Producing Nano-Plates of Synthetic Hydroxyapatite and Nanopowder Comprising a Synthetic Hydroxyapatite Nano-Plates. Patent, Exclusive Right Number-Pat.235292. Available online: https://api-ewyszukiwarka.pue.uprp.gov.pl/api/collection/2f1684e27bedc23db247cb2a29fe4b67 (accessed on 15 September 2023).
- Alves Cardoso, D.; Jansen, J.A.; Leeuwenburgh, S.C.G. Synthesis and application of nanostructured calcium phosphate ceramics for bone regeneration. J. Biomed. Mater. Res. Part. B 2012, 100B, 2316–2326. [Google Scholar] [CrossRef]
- Singh, J.; Chatha, S.S.; Singh, H. In vitro assessment of plasma-sprayed reinforced hydroxyapatite coatings deposited on Ti6Al4V alloy for bio-implant applications. J. Mater. Res. 2022, 37, 2623–2634. [Google Scholar] [CrossRef]
- Ritwik, A.; Saju, K.K.; Vengellur, A.; Saipriya, P.P. Development of thin-film hydroxyapatite coatings with an intermediate shellac layer produced by dip-coating process on Ti6Al4V implant materials. J. Coat. Technol. Res. 2022, 19, 597–605. [Google Scholar] [CrossRef]
- Kubicki, G.; Leshchynsky, V.; Elseddawy, A.; Wisniewska, M.; Maev, R.G.; Jakubowicz, J.; Sulej-Chojnacka, J. Microstructure and Properties of Hydroxyapatite Coatings Made by Aerosol Cold Spraying-Sintering Technology. Coatings 2022, 12, 535. [Google Scholar] [CrossRef]
- Higuchi, J.; Fortunato, G.; Woźniak, B.; Chodara, A.; Domaschke, S.; Męczyńska-Wielgosz, S.; Kruszewski, M.; Dommann, A.; Łojkowski, W. Polymer Membranes Sonocoated and Electrosprayed with Nano-Hydroxyapatite for Periodontal Tissues Regeneration. Nanomaterials 2019, 9, 1625. [Google Scholar] [CrossRef]
- Higuchi, J.; Klimek, K.; Wojnarowicz, J.; Opalińska, A.; Chodara, A.; Szalaj, U.; Dąbrowska, S.; Fudala, D.; Ginalska, G. Electrospun Membrane Surface Modification by Sonocoating with HA and ZnO:Ag Nanoparticles-Characterization and Evaluation of Osteoblasts and Bacterial Cell Behavior In Vitro. Cells 2022, 11, 1582. [Google Scholar] [CrossRef] [PubMed]
- Majcher, A.; Wiejak, J.; Przybylski, J.; Chudoba, T.; Wojnarowicz, J. A novel reactor for microwave hydrothermal scale-up nanopowder synthesis. Int. J. Chem. React. Eng. 2013, 11, 361–368. [Google Scholar] [CrossRef]
- Holzwarth, U.; Gibson, N. The Scherrer equation versus the ‘Debye-Scherrer equation’. Nat. Nanotechnol. 2011, 6, 534. [Google Scholar] [CrossRef]
- ISO 9277; 2010-Determination of the Specific Surface Area of Solids by Gas Adsorption—BET Method. ISO: Geneva, Switzerland, 2023. Available online: https://www.iso.org/standard/44941.html (accessed on 24 August 2023).
- ISO 12154; 2014-Determination of Density by Volumetric Displacement—Skeleton Density by Gas Pycnometry. ISO: Geneva, Switzerland, 2023. Available online: https://www.iso.org/standard/54731.html (accessed on 24 August 2023).
- Szałaj, U.; Świderska-Środa, A.; Chodara, A.; Gierlotka, S.; Łojkowski, W. Nanoparticle Size Effect on Water Vapour Adsorption by Hydroxyapatite. Nanomaterials 2019, 9, 1005. [Google Scholar] [CrossRef]
- Polish Center for Accreditation, Testing Laboratories. Accreditation Number: AB 1503. Available online: https://www.pca.gov.pl/en/accredited-organizations/accredited-organizations/testing-laboratories/AB%201503,entity.html (accessed on 24 August 2023).
- PN-EN ISO/IEC 17025; 2018-02-Polish Version-General Requirements for the Competence of Testing and Calibration Laboratories. ISO: Geneva, Switzerland, 2023. Available online: https://sklep.pkn.pl/pn-en-iso-iec-17025-2018-02p.html (accessed on 24 August 2023).
- Legeros, R.Z. Calcium phosphates in oral biology and medicine. Monogr. Oral. Sci. 1991, 15, 1–201. [Google Scholar]
- Legeros, R.Z. Biological and Synthetic Apatites in Hydroxyapatite and Related Materials, 1st ed.; Brown, P.W., Constantz, B., Eds.; CRC Press: Boca Raton, FL, USA, 1994; pp. 3–28. [Google Scholar]
- Kozerozhets, I.V.; Panasyuk, G.P.; Semenov, E.A.; Avdeeva, V.V.; Danchevskaya, M.N.; Simonenko, N.P.; Vasiliev, M.G.; Kozlova, L.O.; Ivakin, Y.I. Recrystallization of nanosized boehmite in an aqueous medium. Powder Technol. 2023, 413, 118030. [Google Scholar] [CrossRef]
- Vdoviaková, K.; Jenca, A.; Jenca, A., Jr.; Danko, J.; Kresáková, L.; Simaiová, V.; Reichel, P.; Rusnák, P.; Pribula, J.; Vrzgula, M.; et al. Regenerative Potential of Hydroxyapatite-Based Ceramic Biomaterial on Mandibular Cortical Bone: An In Vivo Study. Biomedicines 2023, 11, 877. [Google Scholar] [CrossRef]
- ISO 13175-3; 2012(en) Implants for Surgery—Calcium Phosphates—Part 3: Hydroxyapatite and Beta-Tricalcium Phosphate Bone Substitutes. ISO: Geneva, Switzerland, 2023. Available online: https://www.iso.org/obp/ui/#iso:std:iso:13175:-3:ed-1:v1:en (accessed on 28 August 2023).
- Opalinska, A.; Malka, I.; Dzwolak, W.; Chudoba, T.; Presz, A.; Lojkowski, W. Size-dependent density of zirconia nanoparticles. Beilstein J. Nanotechnol. 2015, 6, 27–35. [Google Scholar] [CrossRef]
- Wojnarowicz, J.; Opalinska, A.; Chudoba, T.; Gierlotka, S.; Mukhovskyi, R.; Pietrzykowska, E.; Sobczak, K.; Lojkowski, W. Effect of water content in ethylene glycol solvent on the size of ZnO nanoparticles prepared using microwave solvothermal synthesis. J. Nanomater. 2016, 2016, 2789871. [Google Scholar] [CrossRef]
- Kusiak-Nejman, E.; Wojnarowicz, J.; Morawski, A.W.; Narkiewicz, U.; Sobczak, K.; Gierlotka, S.; Lojkowski, W. Size-dependent effects of ZnO nanoparticles on the photocatalytic degradation of phenol in a water solution. Appl. Surf. Sci. 2021, 541, 148416. [Google Scholar] [CrossRef]
- Wojnarowicz, J.; Chudoba, T.; Gierlotka, S.; Sobczak, K.; Lojkowski, W. Size Control of Cobalt-Doped ZnO Nanoparticles Obtained in Microwave Solvothermal Synthesis. Crystals 2018, 8, 179. [Google Scholar] [CrossRef]
- Tamari, S.; Aguilar-Chavez, A. Optimum Design of Gas Pycnometers for Determining the Volume of Solid Particles. J. Test. Eval. 2005, 33, JTE12674. [Google Scholar] [CrossRef]
- Tamari, S.; Aguilar-Chávez, A. Optimum design of the variable-volume gas pycnometer for determining the volume of solid particles. Meas. Sci. Technol. 2004, 15, 1146–1152. [Google Scholar] [CrossRef]
- Wilson, R.M.; Elliott, J.C.; Dowker, S.E.P. Rietveld Refinement of the Crystallographic Structure of Human Dental Enamel Apatites. Am. Mineral. 1999, 84, 1406–1414. [Google Scholar] [CrossRef]
- Okazaki, M.; Taira, M.; Takahashi, J. Rietveld Analysis and Fourier Maps of Hydroxyapatite. Biomaterials 1997, 18, 795–799. [Google Scholar] [CrossRef]
- Ma, G.; Liu, X.Y. Hydroxyapatite: Hexagonal or Monoclinic? Cryst. Growth Des. 2009, 9, 2991–2994. [Google Scholar] [CrossRef]
- Adam, M.; Ganz, C.; Xu, W.; Sarajian, H.; Götz, W.; Gerber, T. In vivo and in vitro investigations of a nanostructured coating material–a preclinical study. Int. J. Nanomed. 2014, 9, 975–984. [Google Scholar] [CrossRef]
- Shekhawat, D.; Vauth, M.; Pezoldt, J. Size Dependent Properties of Reactive Materials. Inorganics 2022, 10, 56. [Google Scholar] [CrossRef]
- Durkan, C. Size Really Does Matter: The Nanotechnology Revolution, 1st ed.; World Scientific Publishing: Singapore, 2019; ISBN 978-1-78634-661-2. [Google Scholar] [CrossRef]
- Navrotsky, A. Energetics of nanoparticle oxides: Interplay between surface energy and polymorphism. Geochem. Trans. 2003, 4, 34–37. [Google Scholar] [CrossRef] [PubMed]
- Kimmel, G.; Zabicky, J. Stability, Instability, Metastability and Grain Size in Nanocrystalline Ceramic Oxide Systems. Solid State Phenom. 2008, 140, 29–36. [Google Scholar] [CrossRef]
- Fu, Q.; Xue, Y.; Cui, Z. Size- and shape-dependent surface thermodynamic properties of nanocrystals. J. Phys. Chem. Solids 2018, 116, 79–85. [Google Scholar] [CrossRef]
- Wang, L.; Nancollas, G.H. Calcium orthophosphates: Crystallization and dissolution. Chem. Rev. 2008, 108, 4628–4669. [Google Scholar] [CrossRef]
- Wang, L.; Lu, J.; Xu, F.; Zhang, F. Dynamics of crystallization and dissolution of calcium orthophosphates at the near-molecular level. Chin. Sci. Bull. 2011, 56, 713–721. [Google Scholar] [CrossRef]
- Porter, A.E.; Patel, N.; Skepper, J.N.; Best, S.M.; Bonfield, W. Comparison of in vivo dissolution processes in hydroxyapatite and silicon-substituted hydroxyapatite bioceramics. Biomaterials 2003, 24, 4609–4620. [Google Scholar] [CrossRef]
- Hoppe, A.; Guldal, N.S.; Boccaccini, A.R. A review of the biological response to ionic dissolution products from bioactive glasses and glass-ceramics. Biomaterials 2011, 32, 2757–2774. [Google Scholar] [CrossRef]
- Nikolenko, M.V.; Vasylenko, K.V.; Myrhorodska, V.D.; Kostyniuk, A.; Likozar, B. Synthesis of Calcium Orthophosphates by Chemical Precipitation in Aqueous Solutions: The Effect of the Acidity, Ca/P Molar Ratio, and Temperature on the Phase Composition and Solubility of Precipitates. Processes 2020, 8, 1009. [Google Scholar] [CrossRef]
- Dorozhkin, S.V. Dissolution mechanism of calcium apatites in acids: A review of literature. World J. Methodol. 2012, 2, 1–17. [Google Scholar] [CrossRef]
- Dorozhkin, S.V. Surface reactions of apatite dissolution. J. Colloid Interface Sci. 1997, 191, 489–497. [Google Scholar] [CrossRef] [PubMed]
- Gayathri, B.; Muthukumarasamy, N.; Velauthapillai, D.; Santhosh, S.B. Magnesium incorporated hydroxyapatite nanoparticles: Preparation, characterization, antibacterial and larvicidal activity. Arab. J. Chem. 2018, 11, 645–654. [Google Scholar] [CrossRef]
- Zhu, Y.; Huang, B.; Zhu, Z.; Liu, H.; Huang, Y.; Zhao, X.; Liang, M. Characterization, dissolution and solubility of the hydroxypyromorphite–hydroxyapatite solid solution [(PbxCa1−x)5(PO4)3OH] at 25 °C and pH 2–9. Geochem. Trans 2016, 17, 2–9. [Google Scholar] [CrossRef]
- Prakash, K.H.; Kumar, R.; Ooi, C.P.; Cheang, P.; Khor, K.A. Apparent Solubility of Hydroxyapatite in Aqueous Medium and Its Influence on the Morphology of Nanocrystallites with Precipitation Temperature. Langmuir 2006, 22, 11002–11008. [Google Scholar] [CrossRef] [PubMed]
- Larsen, M.J.; Jensen, S.J. The hydroxyapatite solubility product of human dental enamel as a function of pH in the range 4.6–7.6 at 20 °C. Arch. Oral Biol. 1989, 34, 957–961. [Google Scholar] [CrossRef]
- Chen, Z.-F.; Darvell, B.W.; Leung, V.W.-H. Hydroxyapatite solubility in simple inorganic solutions. Arch. Oral Biol. 2004, 49, 359–367. [Google Scholar] [CrossRef]
- Arcos, D.; Vallet-Regí, M. Substituted hydroxyapatite coatings of bone implants. J. Mater. Chem. B 2020, 8, 1781–1800. [Google Scholar] [CrossRef]
- Kuranov, G.; Mikhelson, K.; Puzyk, A. Solubility of Hydroxyapatite as a Function of Solution Composition (Experiment and Modeling). In Processes and Phenomena on the Boundary between Biogenic and Abiogenic Nature; Lecture Notes in Earth System Sciences; Frank-Kamenetskaya, O., Vlasov, D., Panova, E., Lessovaia, S., Eds.; Springer: Cham, Switzerland, 2020. [Google Scholar] [CrossRef]
- Kamieniak, J.; Kelly, P.J.; Banks, C.E.; Doyle, A.M. Mechanical, pH and Thermal Stability of Mesoporous Hydroxyapatite. J. Inorg. Organomet. Polym. 2018, 28, 84–91. [Google Scholar] [CrossRef]
- Bell, L.C.; Mika, H.; Kruger, B.J. Synthetic hydroxyapatite-solubility product and stoichiometry of dissolution. Arch. Oral Biol. 1978, 23, 329–336. [Google Scholar] [CrossRef]
- Bengtsson, Å.; Shchukarev, A.; Persson, P.; Sjöberg, S. A solubility and surface complexation study of a non-stoichiometric hydroxyapatite. Geochim. Cosmochim. Acta 2009, 73, 257–267. [Google Scholar] [CrossRef]
- Bloebaum, R.D.; Lundeen, G.A.; Bachus, K.N.; Ison, I.; Hofmann, A.A. Dissolution of particulate hydroxyapatite in a macrophage organelle model. J. Biomed. Mater. Res. 1998, 40, 104–114. [Google Scholar] [CrossRef]
- Wang, D.; Xie, Y.; Jaisi, D.P.; Jin, Y. Effects of low-molecular-weight organic acids on the dissolution of hydroxyapatite nanoparticles. Environ. Sci. Nano 2016, 3, 768–779. [Google Scholar] [CrossRef]
- Capanema, N.S.V.; Mansur, A.A.P.; Carvalho, S.M.; Silva, A.R.P.; Ciminelli, V.S.; Mansur, H.S. Niobium-Doped Hydroxyapatite Bioceramics: Synthesis, Characterization and In Vitro Cytocompatibility. Materials 2015, 8, 4191–4209. [Google Scholar] [CrossRef] [PubMed]
- Mocanu, A.; Cadar, O.; Frangopol, P.T.; Petean, I.; Tomoaia, G.; Paltinean, G.-A.; Racz, C.P.; Horovitz, O.; Tomoaia-Cotisel, M. Ion release from hydroxyapatite and substituted hydroxyapatites in different immersion liquids: In vitro experiments and theoretical modelling study. Ion release from hydroxyapatite and substituted hydroxyapatites in different immersion liquids: In vitro experiments and theoretical modelling study. R. Soc. Open Sci. 2020, 8, 201785. [Google Scholar] [CrossRef]
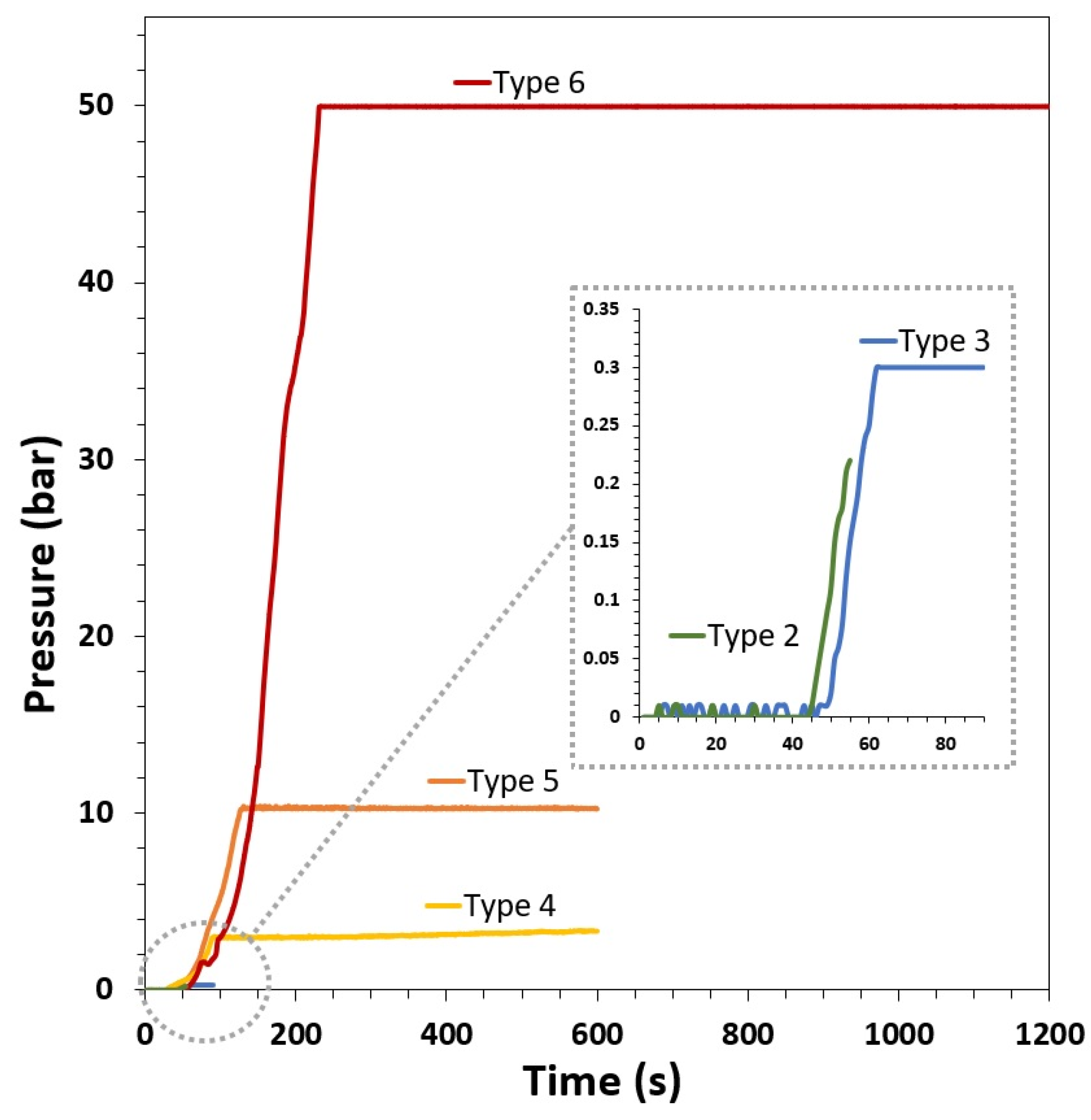
| GoHAP | Heating Time (s) | Total Reaction Time (s) | Pressure (bar) | Temperature (°C) |
|---|---|---|---|---|
| Type 1 | - | - | - | - |
| Type 2 | 55 | 55 | 0.2 | 115 |
| Type 3 | 60 | 90 | 0.3 | 125 |
| Type 4 | 100 | 600 | 3 | 130 |
| Type 5 | 120 | 600 | 10 | 175 |
| Type 6 | 200 | 1200 | 50 | 260 |
| GoHAP | Specific Surface Area, as (m2/g) | Skeleton Density, ρs ± SD (g/cm3) |
|---|---|---|
| Type 1 | 240 | 2.89 ± 0.01 |
| Type 2 | 211 | 2.90 ± 0.01 |
| Type 3 | 183 | 2.92 ± 0.01 |
| Type 4 | 108 | 2.98 ± 0.01 |
| Type 5 | 67 | 3.05 ± 0.01 |
| Type 6 | 51 | 3.05 ± 0.01 |
| GoHAPTM | Mean Particle Size Based on TEM Method, dTEM ± SD (nm) | Mean Particle Size Based on SSA, dSSA ± SD (nm) | Mean Size of Crystallites Based on Scherrer’s Formula | ||
|---|---|---|---|---|---|
| Length D(002) ± SD (nm) | Width D(300) ± SD (nm) | Aspect Ratio (D(002)/D(300)) | |||
| Type 1 | 8 ± 4 | 9 ± 1 | 14 ± 7 | 5 ± 1 | 2.8 |
| Type 2 | 13 ± 4 | 10 ± 1 | 21 ± 12 | 5 ± 2 | 4.2 |
| Type 3 | 13 ± 6 | 11 ± 1 | 29 ± 15 | 17 ± 7 | 1.7 |
| Type 4 | 20 ± 9 | 19 ± 2 | 33 ± 17 | 23 ± 8 | 1.4 |
| Type 5 | 30 ± 12 | 29 ± 3 | 43 ± 20 | 27 ± 10 | 1.6 |
| Type 6 | 36 ± 13 | 39 ± 4 | 51 ± 24 | 32 ± 11 | 1.6 |
| GoHAP | Calcium (mol) | Phosphorus (mol) | Calcium-Phosphorus (Ca/P) Ratio |
|---|---|---|---|
| Type 1 | 8.29 | 5.44 | 1.52 |
| Type 2 | 8.09 | 5.36 | 1.51 |
| Type 3 | 9.67 | 6.40 | 1.51 |
| Type 4 | 8.71 | 5.74 | 1.52 |
| Type 5 | 5.38 | 3.54 | 1.52 |
| Type 6 | 9.29 | 6.09 | 1.53 |
| GoHAP | Magnesium (wt%) | Silicon (wt%) | Aluminum (wt%) | Iron (wt%) | Sodium (wt%) | Sodium (wt%) |
|---|---|---|---|---|---|---|
| Type 1 | 0.225 | 0.053 | 0.019 | 0.021 | 0.082 | 0.0009 |
| Type 2 | 0.219 | 0.056 | 0.018 | 0.018 | 0.083 | 0.0009 |
| Type 3 | 0.258 | 0.049 | 0.019 | 0.020 | 0.074 | 0.010 |
| Type 4 | 0.232 | 0.054 | 0.019 | 0.020 | 0.087 | 0.010 |
| Type 5 | 0.144 | 0.043 | 0.013 | 0.014 | 0.073 | 0.006 |
| Type 6 | 0.252 | 0.050 | 0.019 | 0.026 | 0.083 | 0.010 |
| Mean value | 0.222 ± 0.041 | 0.051 ± 0.005 | 0.018 ± 0.002 | 0.020 ± 0.004 | 0.080 ± 0.006 | 0.006 ± 0.004 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Szałaj, U.; Chodara, A.; Gierlotka, S.; Wojnarowicz, J.; Łojkowski, W. Enhanced Release of Calcium Ions from Hydroxyapatite Nanoparticles with an Increase in Their Specific Surface Area. Materials 2023, 16, 6397. https://doi.org/10.3390/ma16196397
Szałaj U, Chodara A, Gierlotka S, Wojnarowicz J, Łojkowski W. Enhanced Release of Calcium Ions from Hydroxyapatite Nanoparticles with an Increase in Their Specific Surface Area. Materials. 2023; 16(19):6397. https://doi.org/10.3390/ma16196397
Chicago/Turabian StyleSzałaj, Urszula, Agnieszka Chodara, Stanisław Gierlotka, Jacek Wojnarowicz, and Witold Łojkowski. 2023. "Enhanced Release of Calcium Ions from Hydroxyapatite Nanoparticles with an Increase in Their Specific Surface Area" Materials 16, no. 19: 6397. https://doi.org/10.3390/ma16196397
APA StyleSzałaj, U., Chodara, A., Gierlotka, S., Wojnarowicz, J., & Łojkowski, W. (2023). Enhanced Release of Calcium Ions from Hydroxyapatite Nanoparticles with an Increase in Their Specific Surface Area. Materials, 16(19), 6397. https://doi.org/10.3390/ma16196397







