Comparative Evaluation of Two Different Fiber-Reinforced Composite Materials in Class 1 Post-Endodontic Restorations in Molars—A Randomized Clinical Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Endodontic Treatment Procedure
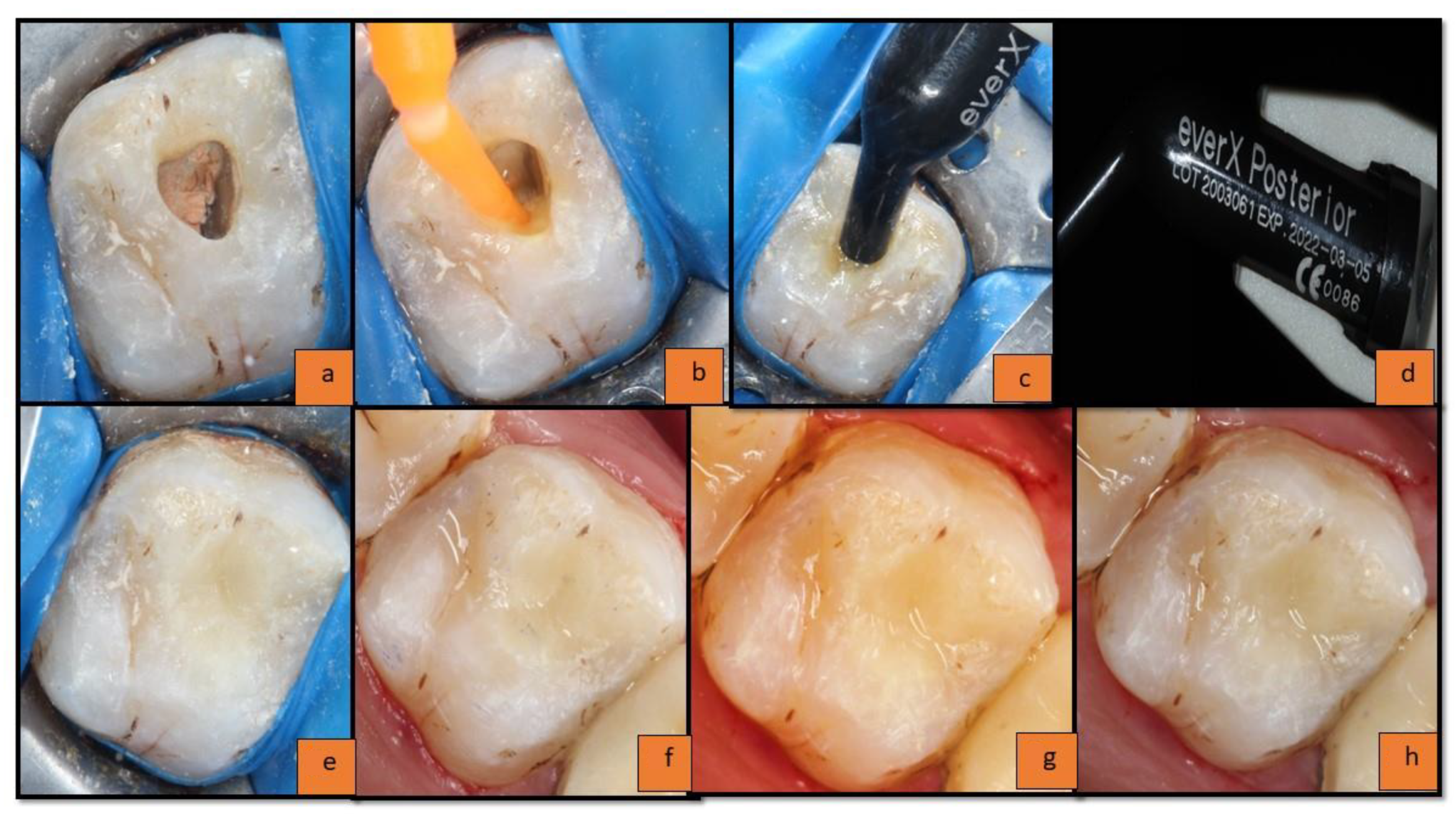
2.2. Group (A)—EverX Posterior Composite with Nanohybrid Solare-X Composite
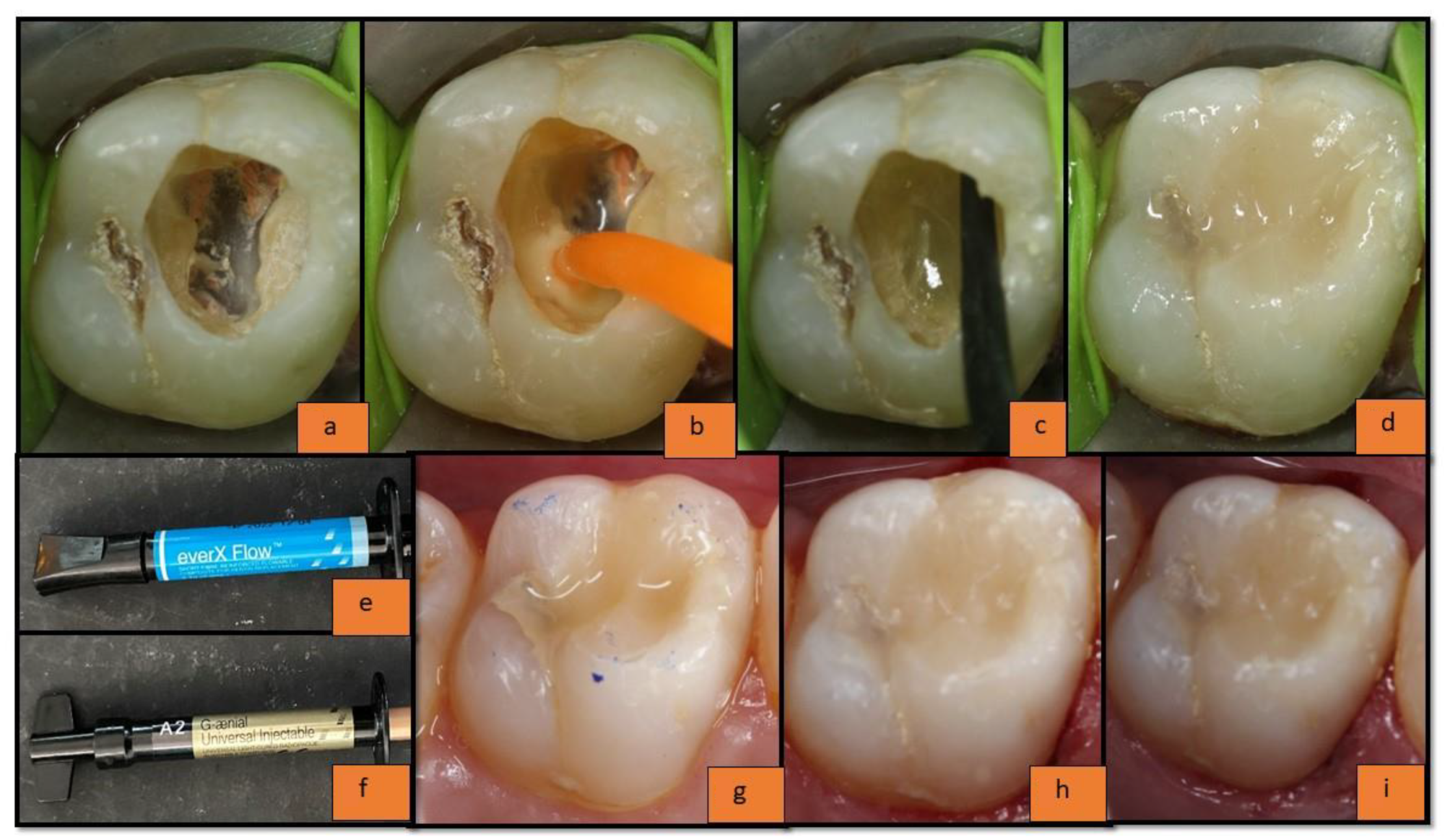
2.3. Group (B): EverX 12 Composite with G-Aenial Universal Injectable Composite
2.4. Evaluation of Restoration
3. Results
3.1. Results of Individual USPHS Criteria
3.1.1. Anatomic Contour
3.1.2. Cavo-Surface Marginal Discoloration
3.1.3. Marginal Integrity
3.1.4. Fracture of Restoration
3.1.5. Fracture of Tooth
3.1.6. Surface Texture
4. Discussion
4.1. Anatomic Contour
4.2. Cavo-Surface Marginal Discoloration
4.3. Marginal Integrity
4.4. Fracture of Restoration and Tooth
- Patient’s habits: If the patient had a habit of chewing betel nuts (or any other similar habit) or had hard consistency food in his routine diet; non-veg, seafood, etc. This might have caused cracks in the restoration leading to a complete fracture over 1 year.
- Location of the tooth in the arch: If there was any occlusal discrepancy already existing or developed later due to some other reasons, this might have shifted the occlusal forces to the tooth restored with FRC in this experimental study, leading to a possible fracture.
- Poor oral hygiene: Composite materials require good oral hygiene for their longevity in clinical conditions as the accumulation of plaque and subsequent microleakage around them might lead to various complications including the fracture of the restoration in the long run.
4.5. Surface Texture
5. Limitations of the Present Study
6. Conclusions
- Clinical performance of the combination of everX Flow with overlying G-aenial Universal Injectable Composite proved to be comparable with everX Posterior with overlying solareX composite as post-endodontic restorations in class I lesions in molars without having a statistically significant difference.
- Individually, the clinical performance of newly introduced materials such as everX Flow (as a substrate dentin replacement material) and G-aenial Universal Injectable Composite (as enamel replacement material) proved to be similar compared with their experimental counterparts, everX posterior and solareX Composite materials.
- Bilayer restorations, a combination of new dentin replacement material with overlying new enamel replacement materials with inherent advanced properties, can mimic the behavior of natural tooth tissues evidencing more conservative, less invasive, and long-lasting restorations, especially in endodontically treated teeth.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cheung, W. Review of the management of endodontically treated teeth. Am. J. Dent. 2005, 25, 52–57. [Google Scholar] [CrossRef] [PubMed]
- Faria, A.C.; Rodrigues, R.C.; de Almeida Antunes, R.P.; de Mattos, M.D.G.; Ribeiro, R.F. Endodontically treated teeth; characteristics and considerations to restore them. J. Prosthodont. Res. 2011, 55, 69–74. [Google Scholar] [CrossRef] [PubMed]
- Burke, F.J. Tooth fracture in vivo and in vitro. J. Dent. 1992, 20, 131–139. [Google Scholar] [CrossRef]
- Garlapati, T.G.; Krithikadatta, J.; Natanasabapathy, V. Fracture resistance of endodontically treated teeth restored with short fibre composite used as a core material—An in vitro study. J. Prosthodont. Res. 2017, 61, 464–470. [Google Scholar] [CrossRef]
- Luthria, A.; Srirekha, A.; Hegde, J.; Karale, R.; Tyagi, S.; Bhaskaran, S. The reinforcement effect of polyethylene fibre and composite impregnated glass fibre on fracture resistance of endodontically treated teeth: An in vitro study. J. Conserv. Dent. 2012, 15, 372–376. [Google Scholar]
- Goldstein, G.R. The longevity of direct and indirect posterior restorations is uncertain and may be affected by a number of dentist-, patient-, and material-related factors. J. Evid. Based Dent. Pract. 2010, 10, 30–31. [Google Scholar] [CrossRef]
- Nandini, S. Indirect resin composites. J. Conserv. Dent. 2010, 13, 184–194. [Google Scholar] [CrossRef]
- Santhosh, L.; Bashetty, K.; Nadig, G. The influence of different composite placement techniques on microleakage in preparations with high C-factor: An in vitro study. J. Conserv. Dent. 2008, 11, 112–116. [Google Scholar] [CrossRef]
- Hiremath, H.; Kulkarni, S.; Hiremath, V.; Kotipalli, M. Evaluation of different fibres and biodentine as alternates to crown coverage for endodontically treated molars: An in vitro study. J. Conserv. Dent. 2017, 20, 72–75. [Google Scholar] [CrossRef]
- Da Rosa Rodolpho, P.A.; Cenci, M.S.; Donassollo, T.A.; Loguércio, A.D.; Demarco, F.F. A clinical evaluation of posterior composite restorations: 17-year findings. J. Dent. 2006, 34, 427–435. [Google Scholar] [CrossRef]
- Fennis, W.M.; Kuijs, R.H.; Roeters, F.J.; Creugers, N.H.; Kreulen, C.M. Randomized control trial of composite cuspal restorations: Five-year results. J. Dent. Res. 2014, 93, 36–41. [Google Scholar] [CrossRef] [PubMed]
- Eapen, A.M.; Amirtharaj, L.V.; Sanjeev, K.; Mahalaxmi, S. Fracture resistance of endodontically treated teeth restored with 2 different fibre reinforced composite and 2 conventional composite resin core build up materials; An In vitro study. J. Endod. 2017, 43, 1499–1504. [Google Scholar] [CrossRef] [PubMed]
- Belli, S.; Cobankara, F.K.; Eraslan, O.; Eskitascioglu, G.; Karbhari, V. The effect of fibre insertion on fracture resistance of endodontically treated molars with MOD cavity and reattached fractured lingual cusps. J. Biomed. Mater. Res. Part B Appl. Biomater. 2006, 79, 35–41. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, F.B.; Paranhos, M.P.; Spohr, A.M.; Oshima, H.M.; Carlini, B.; Burnett, L.H., Jr. Fracture resistance of root filled molar teeth restored with glass fibre bundles. Int. Endod. J. 2010, 43, 356–362. [Google Scholar] [CrossRef] [PubMed]
- Bilgi, P.S.; Shah, N.C.; Patel, P.P.; Vaid, D.S. Comparison of fracture resistance of endodontically treated teeth restored with nanohybrid, silorane, and fibre reinforced composite: An in vitro study. J. Conserv. Dent. 2016, 19, 364. [Google Scholar] [PubMed]
- Butterworth, C.; Ellakwa, A.E.; Shortall, A. Fibre-reinforced composites in restorative dentistry. Dent. Update 2003, 30, 300–306. [Google Scholar] [CrossRef]
- Meenakumari, C.; Bhat, K.M.; Bansal, R.; Singh, N. Evaluation of mechanical properties of newer nanoposterior restorative resin composites: An In vitro study. Contemp. Clin. Dent. 2018, 9 (Suppl. 1), 142–146. [Google Scholar] [CrossRef]
- Ayna, B.; Elenk Sc Atakul, F.; Uysal, E. Three year clinical evaluation of endodontically treated anterior teeth restored with a polyethylene fibre reinforced composite. Aust. Dent. J. 2009, 54, 136–140. [Google Scholar] [CrossRef]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef] [PubMed]
- Gianordoli-Neto, R.; Padovani, G.C.; Mondelli, J.; de Lima Navarro, M.F.; Mendonça, J.S.; Santiago, S.L. Two-year clinical evaluation of resin composite in posterior teeth: A randomized controlled study. J. Conserv. Dent. 2016, 19, 306. [Google Scholar]
- Deliperi, S.; Bardwell, D.N. Reconstruction of nonvital teeth using direct fibre reinforced composite resin: A pilot clinical study. J. Adhes. Dent. 2009, 11, 71–78. [Google Scholar] [PubMed]
- Garoush, S.; Sungur, S.; Boz, Y.; Ozkan, P.; Vallittu, P.K.; Uctasli, S.; Lassila, L. Influence of short-fiber composite base on fracture behavior of direct and indirect restorations. Clin. Oral Investig. 2021, 25, 4543–4552. [Google Scholar] [CrossRef] [PubMed]
- Attavar, S.H.; Nadig, P.L. An in vitro evaluation of the fracture resistance of endodontically treated single rooted premolar fractured vertically and reattached using two different fibre reinforced composites. Indian J. Appl. Res. 2015, 5, 472–474. [Google Scholar]
- Loomans, B.; Hilton, T. Extended resin composite restorations: Techniques and procedures. Oper. Dent. 2016, 41, S58–S67. [Google Scholar] [CrossRef] [PubMed]
- Lempel, E.; Lovász, B.V.; Bihari, E.; Krajczár, K.; Jeges, S.; Tóth, Á.; Szalma, J. Long-term clinical evaluation of direct resin composite restorations in vital vs. endodontically treated posterior teeth—Retrospective study up to 13 years. Dent. Mater. 2019, 35, 1308–1318. [Google Scholar] [CrossRef]
- Tekçe, N.; Pala, K.; Tuncer, S.; Demirci, M.; Serim, M.E. Influence of polymerisation method and type of fibre on fracture strength of endodontically treated teeth. Aust. Endod. J. 2017, 43, 115–122. [Google Scholar] [CrossRef]
- Cheng, T.H.; Jones, F.R.; Wang, D. Effect of fibre conditioning on the interfacial shear strength of glass-fibre composite. Compos. Sci. Technol. 1993, 48, 89–96. [Google Scholar] [CrossRef]
- Chung, K.H. Effects of finishing and polishing procedures on the surface texture of resin composites. Dent. Mater. 1994, 10, 325–330. [Google Scholar] [CrossRef]
| Product Name | Manufacturer | Components | Batch | Expiry | Shade |
|---|---|---|---|---|---|
| Solare Universal Bond | GC India Dental Pvt. Ltd. Telangana, India | 4-MET, MDP, MDTP, Photoinitiator, Nano filler | 2007011 | June 2022 | - |
| everX Posterior | GC Corporation Tokyo, Japan | Bis-GMA, PMMA, TEGDMA, Salinated E-glass Fiber, Barium Glass | 2003061 | March 2022 | - |
| everX Flow | GC Corporation Tokyo, Japan | Bis—MEPP, TEGDMA, UDMA, E-glass Fiber, Barium Glass, Silicon Dioxide | 1912051 | December 2022 | - |
| G-aenial universal injectable | GC Corporation Tokyo, Japan | UDMA, Bis-MEPP, TEGDMA, Fillers: SiO2, Barium Glass | 1909051 | September 2022 | A2 |
| GROUP | Time Interval | Samples Present (No.) | Samples Lost to Follow-Up (No.) | Samples Lost to Follow-Up (%) |
|---|---|---|---|---|
| group A | At Baseline | 25 | 0 | 0% |
| At 6 months | 24 | 1 | 4% | |
| At 1 year | 23 | 2 | 8% | |
| group B | At Baseline | 25 | 0 | 0% |
| At 6 months | 24 | 1 | 4% | |
| At 1 year | 22 | 3 | 12% |
| Anatomic Contour | Baseline | 6 Months | 1 Year | |||
|---|---|---|---|---|---|---|
| group A (n = 25) | group B (n = 25) | group A (n = 24) | group B (n = 24) | group A (n = 23) | group B (n = 22) | |
| Alpha | 25 (100%) | 25 (100%) | 18 (75%) | 20 (83.3%) | 12 (52.2%) | 15 (68.2%) |
| Bravo | 0 (0%) | 0 (0%) | 6 (25%) | 4 (16.7%) | 11 (47.8%) | 5 (22.7%) |
| Charlie | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 2 (9.1%) |
| NA | Chi-square = 0.505, Exact p-value = 0.724 | Chi-square = 4.563, Exact p-value = 0.091 | ||||
| Cavo-Surface Marginal Discoloration | Baseline | 6 Months | 1 Year | |||
| group A (n = 25) | group B (n = 25) | group A (n = 24) | group B (n = 24) | group A (n = 23) | group B (n = 22) | |
| Alpha | 25 (100%) | 25 (100%) | 22 (91.7%) | 20 (83.3%) | 17 (73.9%) | 15 (68.2%) |
| Bravo | 0 (0%) | 0 (0%) | 2 (8.3%) | 4 (16.7%) | 5 (21.7%) | 5 (22.7%) |
| Charlie | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (4.3%) | 2 (9.1%) |
| NA | Chi-square = 0.762, Exact p-value = 0.666 | Chi-square = 0.436, Exact p-value = 0.890 | ||||
| Marginal Integrity | Baseline | 6 Months | 1 Year | |||
| group A (n = 25) | group B (n = 25) | group A (n = 24) | group B (n = 24) | group A (n = 23) | group B (n = 22) | |
| Alpha | 25 (100%) | 25 (100%) | 22 (91.7%) | 20 (83.3%) | 17 (73.9%) | 15 (68.2%) |
| Bravo | 0 (0%) | 0 (0%) | 2 (8.3%) | 4 (16.7%) | 5 (21.7%) | 5 (22.7%) |
| Charlie | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (4.3%) | 2 (9.1%) |
| NA | Chi-square = 0.762, Exact p-value = 0.666 | Chi-square = 0.436, Exact p-value = 0.890 | ||||
| Fracture of Restoration | Baseline | 6 Months | 1 Year | |||
| group A (n = 25) | group B (n = 25) | group A (n = 24) | group B (n = 24) | group A (n = 23) | group B (n = 22) | |
| Alpha | 25 (100%) | 25 (100%) | 24 (100%) | 23 (95.8%) | 22 (95.7%) | 19 (86.4%) |
| Bravo | 0 (0%) | 0 (0%) | 0 (0%) | 1 (4.2%) | 1 (4.3%) | 3 (13.6%) |
| Charlie | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| NA | Chi-square = 1.021, Exact p-value = 1.000 | Chi-square = 1.198, Exact p-value = 0.346 | ||||
| Tooth Fracture | Baseline | 6 Months | 1 Year | |||
| group A (n = 25) | group B (n = 25) | group A (n = 24) | group B (n = 24) | group A (n = 23) | group B (n = 22) | |
| Alpha | 25 (100%) | 25 (100%) | 23 (95.8%) | 23 (95.8%) | 22 (95.7%) | 20 (90.9%) |
| Bravo | 0 (0%) | 0 (0%) | 1 (4.2%) | 1 (4.2%) | 1 (4.3%) | 2 (9.1%) |
| Charlie | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| NA | Chi-square = 0, Exact p-value = 1.000 | Chi-square = 0.407, Exact p-value = 0.608 | ||||
| Surface Texture | Baseline | 6 Months | 1 Year | |||
| group A (n = 25) | group B (n = 25) | group A (n = 24) | group B (n = 24) | group A (n = 23) | group B (n = 22) | |
| Alpha | 24 (96%) | 25 (100%) | 21 (87.5%) | 19 (79.2%) | 7 (30.4%) | 10 (45.5%) |
| Bravo | 1 (4%) | 0 (0%) | 2 (8.3%) | 4 (16.7%) | 16 (69.6%) | 11 (50%) |
| Charlie | 0 (0%) | 0 (0%) | 1 (4.2%) | 1 (4.2%) | 0 (0%) | 1 (4.5%) |
| Chi-square = 1.020, Exact p-value = 1.000 | Chi-square = 0.767, Exact p-value = 0.829 | Chi-square = 2.434, Exact p-value = 0.283 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ranka, S.; Rao, A.S.; Shah, U.; Solanki, D.; Pawar, A.M.; Reda, R.; Zanza, A.; Testarelli, L. Comparative Evaluation of Two Different Fiber-Reinforced Composite Materials in Class 1 Post-Endodontic Restorations in Molars—A Randomized Clinical Study. Materials 2022, 15, 7858. https://doi.org/10.3390/ma15217858
Ranka S, Rao AS, Shah U, Solanki D, Pawar AM, Reda R, Zanza A, Testarelli L. Comparative Evaluation of Two Different Fiber-Reinforced Composite Materials in Class 1 Post-Endodontic Restorations in Molars—A Randomized Clinical Study. Materials. 2022; 15(21):7858. https://doi.org/10.3390/ma15217858
Chicago/Turabian StyleRanka, Suwidhi, Ajay Singh Rao, Unnati Shah, Dikshit Solanki, Ajinkya M. Pawar, Rodolfo Reda, Alessio Zanza, and Luca Testarelli. 2022. "Comparative Evaluation of Two Different Fiber-Reinforced Composite Materials in Class 1 Post-Endodontic Restorations in Molars—A Randomized Clinical Study" Materials 15, no. 21: 7858. https://doi.org/10.3390/ma15217858
APA StyleRanka, S., Rao, A. S., Shah, U., Solanki, D., Pawar, A. M., Reda, R., Zanza, A., & Testarelli, L. (2022). Comparative Evaluation of Two Different Fiber-Reinforced Composite Materials in Class 1 Post-Endodontic Restorations in Molars—A Randomized Clinical Study. Materials, 15(21), 7858. https://doi.org/10.3390/ma15217858











