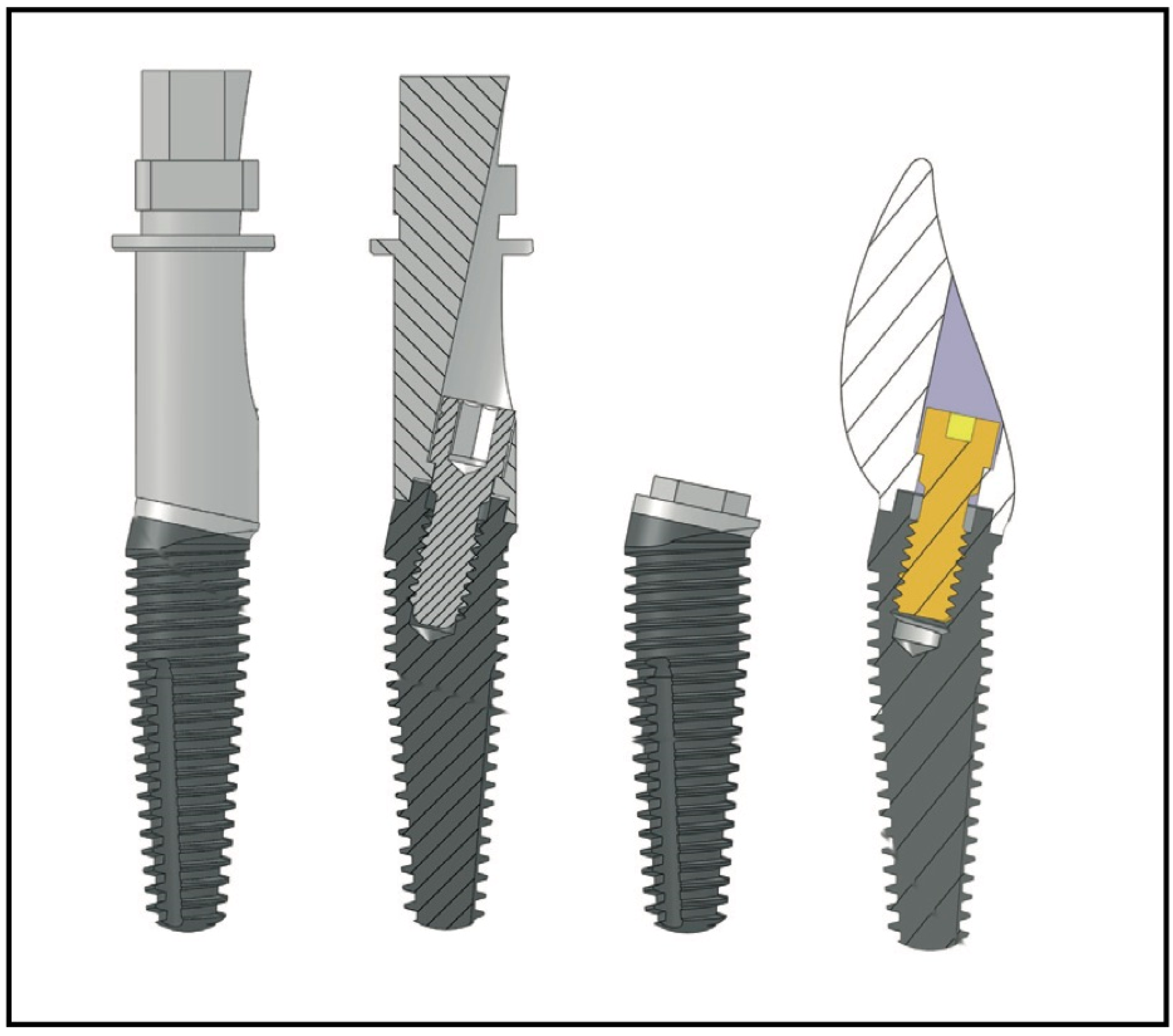
Clinical Evidence on a Novel Macrohybrid Design Dental Implant with 12° Angled Platform: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Protocol and Registration
2.2. Search Strategy
2.3. Eligibility Criteria
- Publications in English.
- Human studies—retrospective and prospective clinical studies, cross-sectional studies, and cohort studies.
- Reporting on outcomes of a novel implant with a 12° angled prosthodontic platform.
- Articles including data on the survival rate of the implants and/or marginal bone loss at final follow-up.
- 5.
- Studies reporting outcomes of a novel implant with 24° angled prosthodontic platform.
- 6.
- In vitro studies.
- 7.
- Animal studies.
- 8.
- Case series.
2.4. Study Selection
2.5. Data Extraction
2.6. Data Analysis
2.7. Risk of Bias
2.8. Quality of the Studies
2.9. Statistical Analysis
3. Results
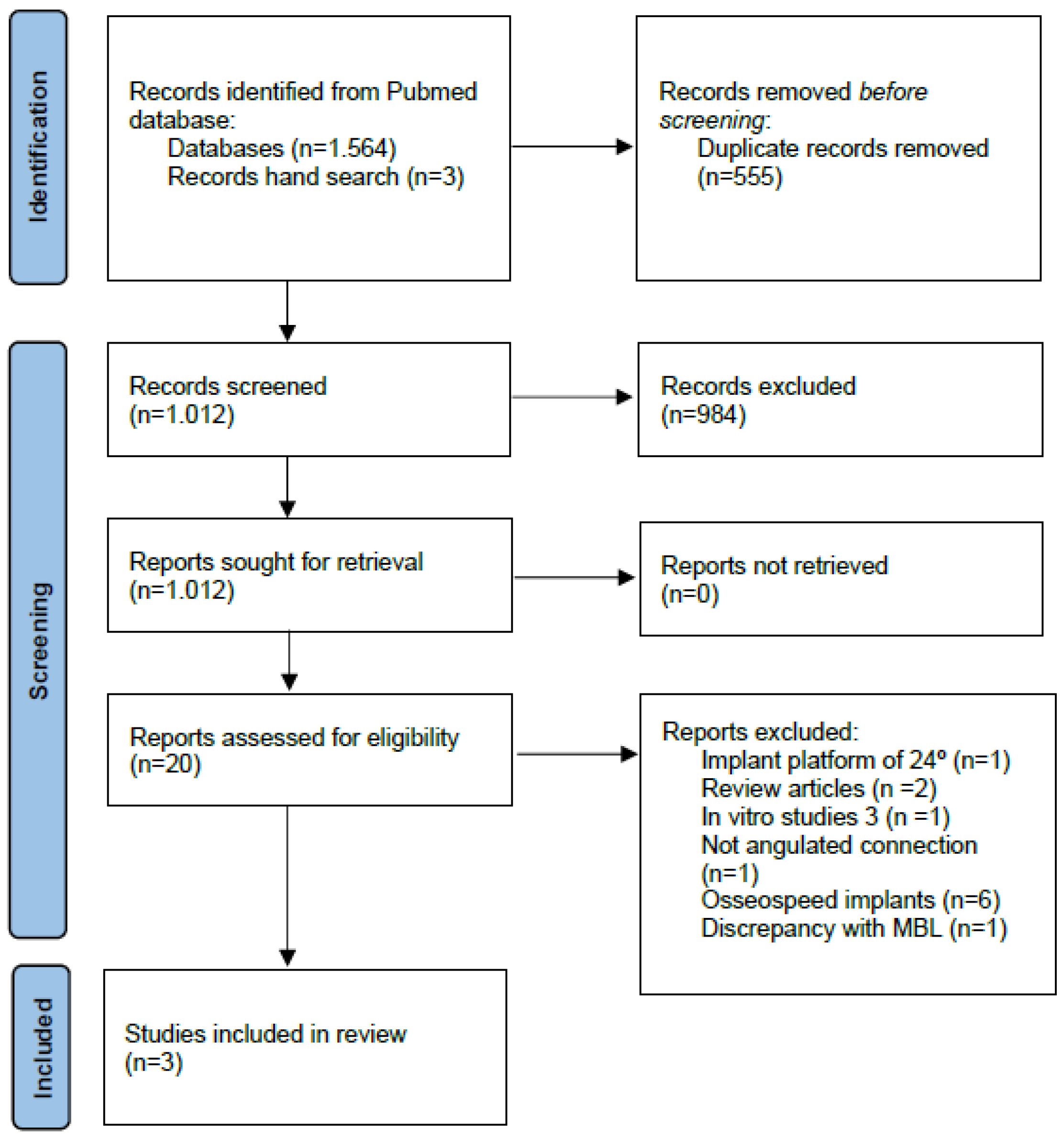
3.1. Study Selection
3.2. Characteristics of the Studies
3.2.1. Intervention Category and Sample Characteristics
3.2.2. Outcomes Methodology
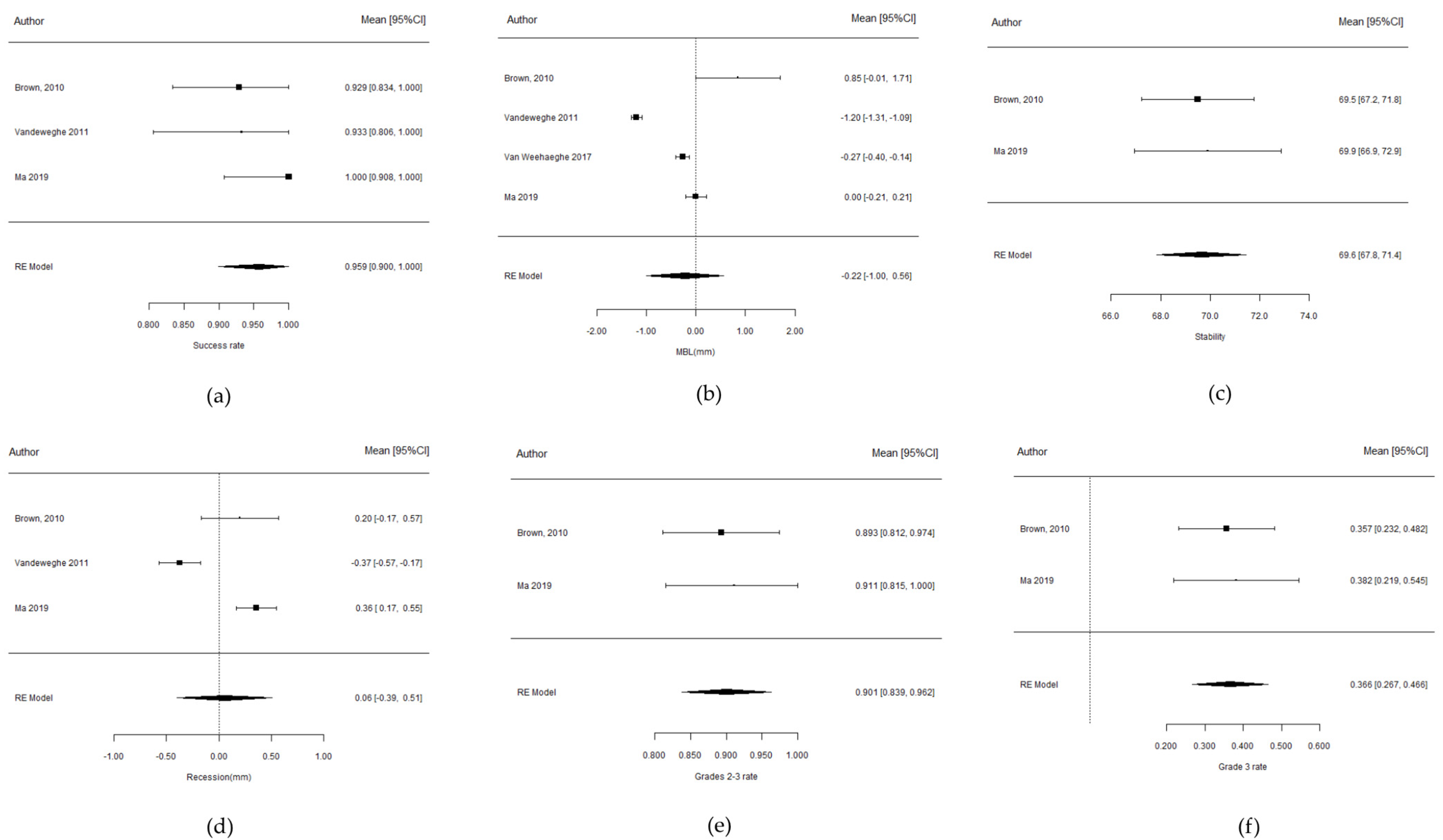
3.3. Success Rate
3.4. Marginal Bone Loss
3.5. Implant Stability
3.6. Soft Tissue Recession
3.7. Papilla Index
4. Discussion
5. Conclusions
Funding
Institutional Review Board statement
Informed Consent Statement
Data availability statement
Acknowledgments
Conflicts of Interest
References
- Nevins, M.; Chu, S.J.; Jang, W.; Kim, D.M. Evaluation of an Innovative Hybrid Macrogeometry Dental Implant in Immediate Extraction Sockets: A Histomorphometric Pilot Study in Foxhound Dogs. Int. J. Periodontics Restor. Dent. 2019, 39, 29–37. [Google Scholar] [CrossRef] [PubMed]
- Kan, J.Y.K.; Rungcharassaeng, K.; Deflorian, M.; Weinstein, T.; Wang, H.-L.; Testori, T. Immediate implant placement and provisionalization of maxillary anterior single implants. Periodontology 2000 2018, 77, 197–212. [Google Scholar] [CrossRef]
- Kan, J.Y.K.; Roe, P.; Rungcharassaeng, K.; Patel, R.D.; Waki, T.; Lozada, J.L.; Zimmerman, G. Classification of sagittal root position in relation to the anterior maxillary osseous housing for immediate implant placement: A cone beam computed tomography study. Int. J. Oral Maxillofac. Implant. 2011, 26, 873–876. [Google Scholar]
- Buser, D.; Martin, W.; Belser, U.C. Optimizing esthetics for implant restorations in the anterior maxilla: Anatomic and surgical considerations. Int. J. Oral Maxillofac. Implant. 2004, 19, 43–61. [Google Scholar]
- Vetromilla, B.M.; Brondani, L.P.; Pereira-Cenci, T.; Bergoli, C.D. Influence of different implant-abutment connection designs on the mechanical and biological behavior of single-tooth implants in the maxillary esthetic zone: A systematic review. J. Prosthet. Dent. 2019, 121, 398–403.e3. [Google Scholar] [CrossRef]
- Lops, D.; Stellini, E.; Sbricoli, L.; Cea, N.; Romeo, E.; Bressan, E. Influence of abutment material on peri-implant soft tissues in anterior areas with thin gingival biotype: A multicentric prospective study. Clin. Oral Implant. Res. 2017, 28, 1263–1268. [Google Scholar] [CrossRef]
- Ahmad, M.; Dhanasekar, B.; Aparna, I.N.; Naim, H. Replacement of missing anterior tooth using screw retained implant prosthesis in the esthetic zone: A case report with 3 years of follow up. J. Indian Prosthodont. Soc. 2014, 14, 297–300. [Google Scholar] [CrossRef]
- Hotinski, E.; Dudley, J. Abutment screw loosening in angulation-correcting implants: An in vitro study. J. Prosthet. Dent. 2019, 121, 151–155. [Google Scholar] [CrossRef]
- Chu, S.J.; Östman, P.-O.; Nicolopoulos, C.; Yuvanoglu, P.; Chow, J.; Nevins, M.; Tarnow, D.P. Prospective Multicenter Clinical Cohort Study of a Novel Macro Hybrid Implant in Maxillary Anterior Postextraction Sockets: 1-Year Results. Int. J. Periodontics Restor. Dent. 2018, 38, s17–s27. [Google Scholar] [CrossRef]
- Bennardo, F.; Barone, S.; Vocaturo, C.; Nucci, L.; Antonelli, A.; Giudice, A. Usefulness of Magnetic Mallet in Oral Surgery and Implantology: A Systematic Review. J. Pers. Med. 2022, 12, 108. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ 2009, 339, b2700. [Google Scholar] [CrossRef] [PubMed]
- Miller, S.A.; Forrest, J.L. Enhancing your practice through evidence-based decision making: PICO, learning how to ask good questions. J. Evid. Based Dent. Pract. 2001, 1, 136–141. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. Int. J. Surg. 2014, 12, 1495–1499. [Google Scholar] [CrossRef] [PubMed]
- Brown, S.D.K.; Payne, A.G.T. Immediately restored single implants in the aesthetic zone of the maxilla using a novel design: 1-year report. Clin. Oral Implant. Res. 2011, 22, 445–454. [Google Scholar] [CrossRef]
- Vandeweghe, S.; Cosyn, J.; Thevissen, E.; Van den Berghe, L.; De Bruyn, H. A 1-year prospective study on Co-Axis implants immediately loaded with a full ceramic crown. Clin. Implant Dent. Relat. Res. 2012, 14 (Suppl. 1), e126–e138. [Google Scholar] [CrossRef]
- Ma, S.; Tawse-Smith, A.; Brown, S.D.K.; Duncan, W. Immediately restored single implants in the aesthetic zone of the maxilla using a novel design: 5-year results from a prospective single-arm clinical trial. Clin. Implant Dent. Relat. Res. 2019, 21, 344–351. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. MetaArXiv 2020. [Google Scholar] [CrossRef]
- Van Weehaeghe, M.; De Bruyn, H.; Vandeweghe, S. A prospective, split-mouth study comparing tilted implants with angulated connection versus conventional implants with angulated abutment. Clin. Implant Dent. Relat. Res. 2017, 19, 989–996. [Google Scholar] [CrossRef]
- Egbert, N.; Ahuja, S.; Selecman, A.; Wicks, R. Angulated Implants for Fabrication of Implant Supported Fixed Partial Denture in the Maxilla. J. Dent. 2017, 18, 304–313. [Google Scholar]
- Ahuja, S.; Egbert, N.; Jain, V.; Cagna, D. Managing maxillary proclination with novel designed angulated implants. J. Indian Prosthodont. Soc. 2017, 17, 203–206. [Google Scholar] [CrossRef]
- Chu, S.J.; Tan-Chu, J.H.P.; Levin, B.P.; Sarnachiaro, G.O.; Lyssova, V.; Tarnow, D.P. A Paradigm Change in Macro Implant Concept: Inverted Body-Shift Design for Extraction Sockets in the Esthetic Zone. Compendium 2019, 40, 444–452. [Google Scholar] [PubMed]
- Howes, D. Angled Implant Design to Accommodate Screw-retained Implant-supported Prostheses. Compend. Contin. Educ. Dent. (Jamesburg NJ 1995) 2017, 38, 458–463. [Google Scholar]
- Kurtzman, G.; Dompkowski, D.; Mahler, B.A.; Howes, D. Off-Axis Implant Placement for Anatomical Considerations Using the Co-Axis Implant. Inside Dent. 2008, 5, 96–102. [Google Scholar]
- Abrahamsson, I.; Welander, M.; Linder, E.; Berglundh, T. Healing at implants placed in an alveolar ridge with a sloped configuration: An experimental study in dogs. Clin. Implant Dent. Relat. Res. 2014, 16, 62–69. [Google Scholar] [CrossRef]
- Lofaj, F.; Kučera, J.; Németh, D.; Minčík, J. Optimization of Tilted Implant Geometry for Stress Reduction in All-on-4 Treatment Concept: Finite Element Analysis Study. Int. J. Oral Maxillofac. Implant. 2018, 33, 1287–1295. [Google Scholar] [CrossRef]
- Noelken, R.; Donati, M.; Fiorellini, J.; Gellrich, N.-C.; Parker, W.; Wada, K.; Berglundh, T. Soft and hard tissue alterations around implants placed in an alveolar ridge with a sloped configuration. Clin. Oral Implant. Res. 2014, 25, 3–9. [Google Scholar] [CrossRef]
- Noelken, R.; Oberhansl, F.; Kunkel, M.; Wagner, W. Immediately provisionalized OsseoSpeed(TM) Profile implants inserted into extraction sockets: 3-year results. Clin. Oral Implant. Res. 2016, 27, 744–749. [Google Scholar] [CrossRef]
- Rojas-Vizcaya, F.; Zadeh, H.H. Minimizing the discrepancy between implant platform and alveolar bone for tilted implants with a sloped implant platform: A clinical report. J. Prosthet. Dent. 2018, 119, 319–324. [Google Scholar] [CrossRef]
- Schiegnitz, E.; Noelken, R.; Moergel, M.; Berres, M.; Wagner, W. Survival and tissue maintenance of an implant with a sloped configurated shoulder in the posterior mandible-a prospective multicenter study. Clin. Oral Implant. Res. 2017, 28, 721–726. [Google Scholar] [CrossRef]
- Jemt, T. Regeneration of gingival papillae after single-implant treatment. Int. J. Periodontics Restor. Dent. 1997, 17, 326–333. [Google Scholar]
- Kamperos, G.; Zambara, I.; Petsinis, V.; Zambaras, D. The Impact of Buccal Bone Defects and Immediate Placement on the Esthetic Outcome of Maxillary Anterior Single-Tooth Implants. J. Oral Implantol. 2016, 42, 337–341. [Google Scholar] [CrossRef] [PubMed]
- Buser, D.; Chappuis, V.; Belser, U.C.; Chen, S. Implant placement post extraction in esthetic single tooth sites: When immediate, when early, when late? Periodontol. 2000 2017, 73, 84–102. [Google Scholar] [CrossRef] [PubMed]
- Gallucci, G.O.; Hamilton, A.; Zhou, W.; Buser, D.; Chen, S. Implant placement and loading protocols in partially edentulous patients: A systematic review. Clin. Oral Implants Res. 2018, 29 (Suppl. 16), 106–134. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.-Y.; Park, H.-J.; Kim, J.-E.; Choi, Y.-G.; Kim, Y.-S.; Huh, J.-B.; Shin, S.-W. A 5-year retrospective clinical study of the Dentium implants. J. Adv. Prosthodont. 2011, 3, 229–235. [Google Scholar] [CrossRef]
- Camps-Font, O.; Rubianes-Porta, L.; Valmaseda-Castellón, E.; Jung, R.E.; Gay-Escoda, C.; Figueiredo, R. Comparison of external, internal flat-to-flat, and conical implant abutment connections for implant-supported prostheses: A systematic review and network meta-analysis of randomized clinical trials. J. Prosthet. Dent. 2021; in press. [Google Scholar] [CrossRef]
- Esposito, M.; Maghaireh, H.; Pistilli, R.; Grusovin, M.G.; Lee, S.T.; Trullenque-Eriksson, A.; Gualini, F. Dental implants with internal versus external connections: 5-year post-loading results from a pragmatic multicenter randomised controlled trial. Eur. J. Oral Implantol. 2016, 9 (Suppl. 1), 129–141. [Google Scholar] [CrossRef]
- Menini, M.; Pesce, P.; Bagnasco, F.; Carossa, M.; Mussano, F.; Pera, F. Evaluation of internal and external hexagon connections in immediately loaded full-arch rehabilitations: A within-person randomised split-mouth controlled trial. Eur. J. Oral Implantol. 2019, 12, 169–179. [Google Scholar]
- Seyssens, L.; Eeckhout, C.; Cosyn, J. Immediate implant placement with or without socket grafting: A systematic review and meta-analysis. Clin. Implant Dent. Relat. Res. 2022, 24, 339–351. [Google Scholar] [CrossRef]
- Park, W.; Park, Y.; Park, H.; Yoo, S.; Chung, S.; Han, J.; Kim, S.-W.; Kim, D.M. A 10-year retrospective radiographic study of implantium dental implants. Int. J. Periodontics Restor. Dent. 2015, 35, 49–54. [Google Scholar] [CrossRef][Green Version]

| Study Design | No. of Patients | No. of Implants | Tooth Replacement | Implant System | Length and Diameter (mm) | Immediate Implant | Biomaterial | Flap/Flapless | CTG | Immediate Provisionalization | Type of Prosthesis | Follow-Up (Months) | Outcomes | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Brown et al., 2010 [14] | Prospective clinical study | 27 | 28 | 15–25 | Co-axis 12° Southern external connection | Length: 13–15 Diameter: 4–4.7 | Yes | No | 26 Flapless 2 Flap | No | Yes (without loading) | Screw-retained | 12 (4 h provisional, 8 weeks definitive crown, 1 year follow-up) | Primary: (1) Implant success. (2) Marginal bone loss. Secondary: (1) Implant stability. (2) Peri-implant tissue stability. (3) Prosthodontic success. |
| Vandeweghe et al., 2011 [18] | Prospective clinical study | 14 | 15 | 15–25 | Co-axis 12° Southern external connection | Length: 10–13–15 Diameter: 4–5 | No | No | Flap | No | Yes (with loading) | Screw-retained | 12 | (1) Marginal bone loss. (2) Implant survival and success. (3) Plaque and bleeding. (4) Soft tissue changes. (5) Patient satisfaction. (6) Esthetic outcomes. (7) Complications. |
| Ma et al., 2019 [16] | Prospective clinical study (single-arm) | 16 | 17 | 15–25 | Co-axis 12° Southern external connection | Not reported | Yes | No | Not reported | No | Yes (with loading) | Screw-retained | 60 (4 h provisional, 8 weeks definitive, follow-up 5 years) | Primary: (1) Implant success. (2) Marginal bone loss. Secondary: (1) Implant stability. (2) Peri-implant tissue stability. (3) Prosthodontic success. |
| WMP | SE | 95%CI | I2 | QH (p-Value) | Egger (p-Value) |
|---|---|---|---|---|---|
| 0.959 | 0.030 | 0.900–1.017 | 0.0% | 0.521 | 0.585 |
| WMP | SE | 95% CI | I2 | QH (p-Value) | Egger (p-Value) |
|---|---|---|---|---|---|
| 0.901 | 0.032 | 0.839–0.962 | 0.0% | 0.778 | - |
| WMP | SE | 95% CI | I2 | QH (p-Value) | Egger (p-Value) |
|---|---|---|---|---|---|
| 0.366 | 0.051 | 0.267–0.466 | 0.0% | 0.812 | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Galve-Huertas, A.; Zilleruelo-Pozo, M.J.; García-González, S.; Ortíz-Puigpelat, O.; Hernández-Alfaro, F.; Aboul-Hosn Centenero, S. Clinical Evidence on a Novel Macrohybrid Design Dental Implant with 12° Angled Platform: A Systematic Review. Materials 2022, 15, 5011. https://doi.org/10.3390/ma15145011
Galve-Huertas A, Zilleruelo-Pozo MJ, García-González S, Ortíz-Puigpelat O, Hernández-Alfaro F, Aboul-Hosn Centenero S. Clinical Evidence on a Novel Macrohybrid Design Dental Implant with 12° Angled Platform: A Systematic Review. Materials. 2022; 15(14):5011. https://doi.org/10.3390/ma15145011
Chicago/Turabian StyleGalve-Huertas, Andrea, Maria José Zilleruelo-Pozo, Susana García-González, Octavi Ortíz-Puigpelat, Federico Hernández-Alfaro, and Samir Aboul-Hosn Centenero. 2022. "Clinical Evidence on a Novel Macrohybrid Design Dental Implant with 12° Angled Platform: A Systematic Review" Materials 15, no. 14: 5011. https://doi.org/10.3390/ma15145011
APA StyleGalve-Huertas, A., Zilleruelo-Pozo, M. J., García-González, S., Ortíz-Puigpelat, O., Hernández-Alfaro, F., & Aboul-Hosn Centenero, S. (2022). Clinical Evidence on a Novel Macrohybrid Design Dental Implant with 12° Angled Platform: A Systematic Review. Materials, 15(14), 5011. https://doi.org/10.3390/ma15145011






