Analysis of the Risk of Wear on Cemented and Uncemented Polyethylene Liners According to Different Variables in Hip Arthroplasty
Abstract
1. Introduction
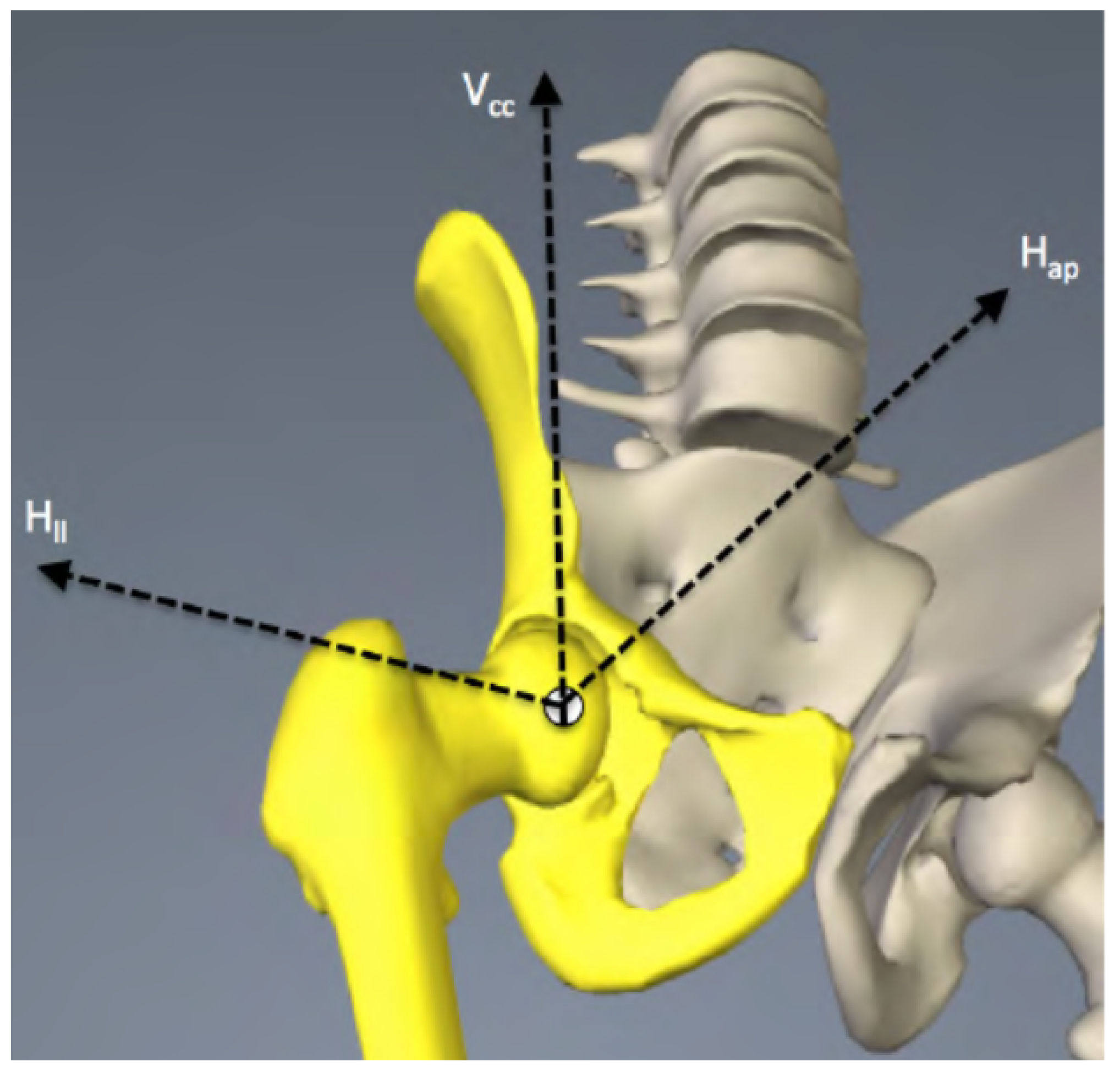
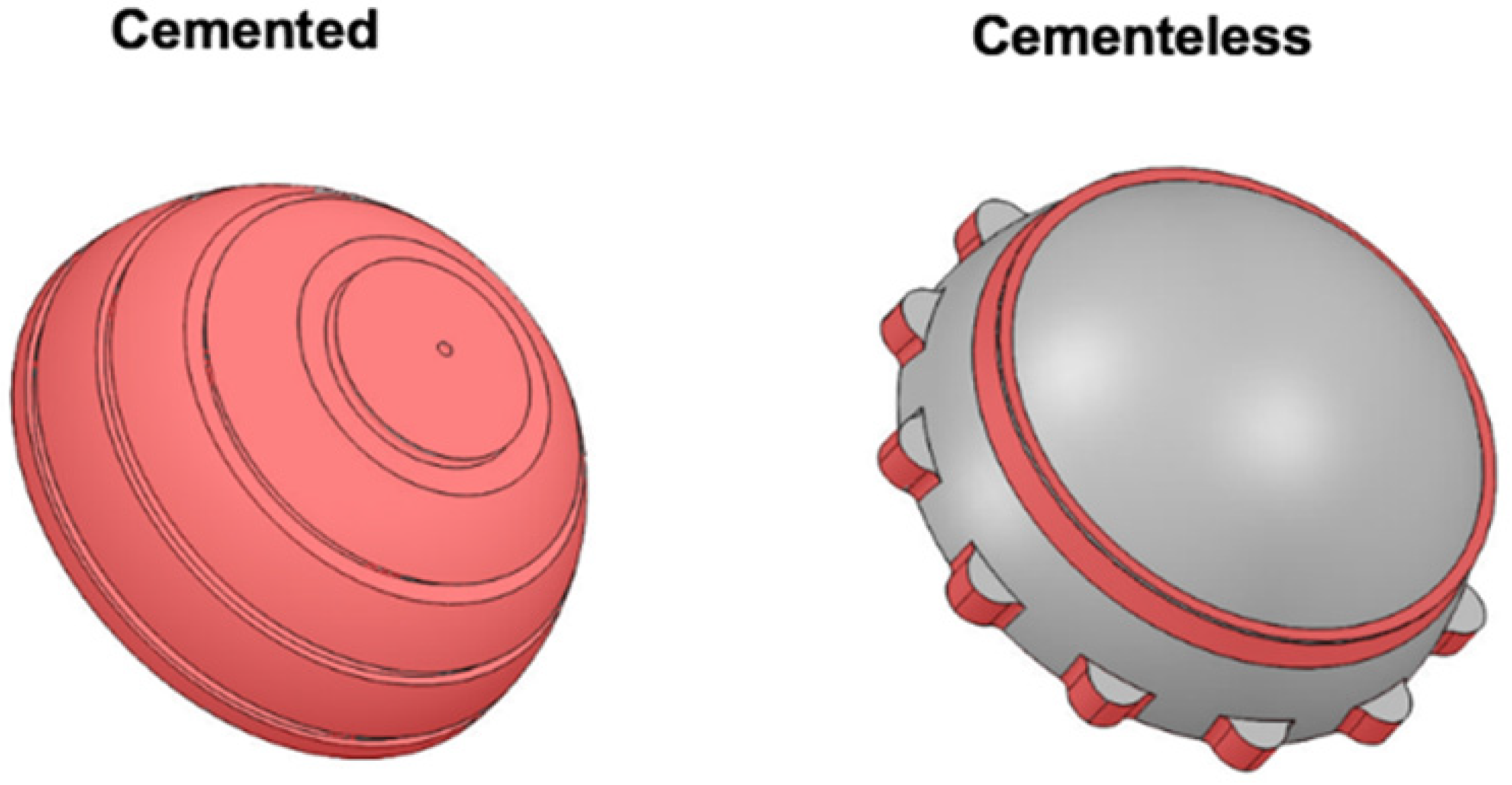
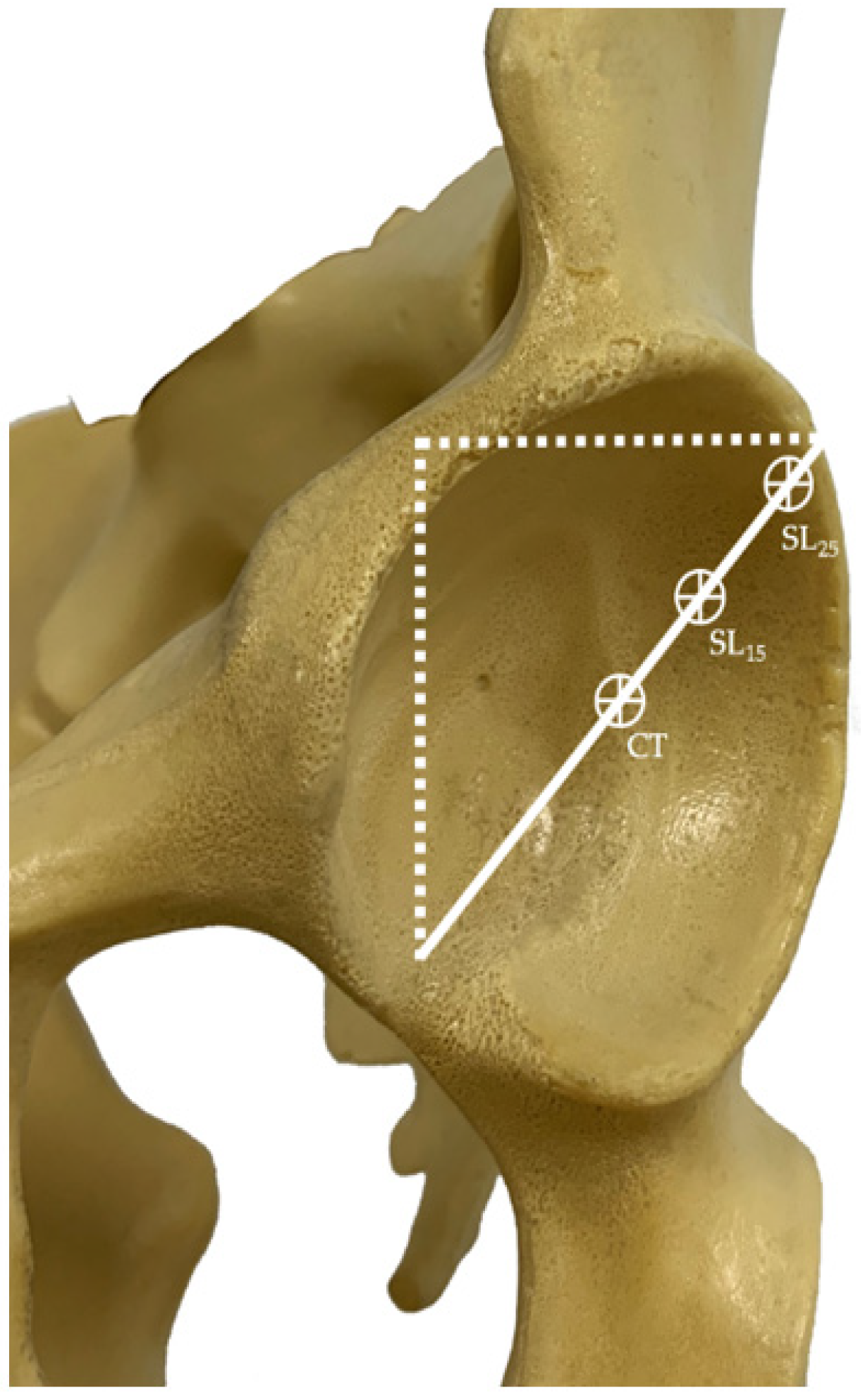
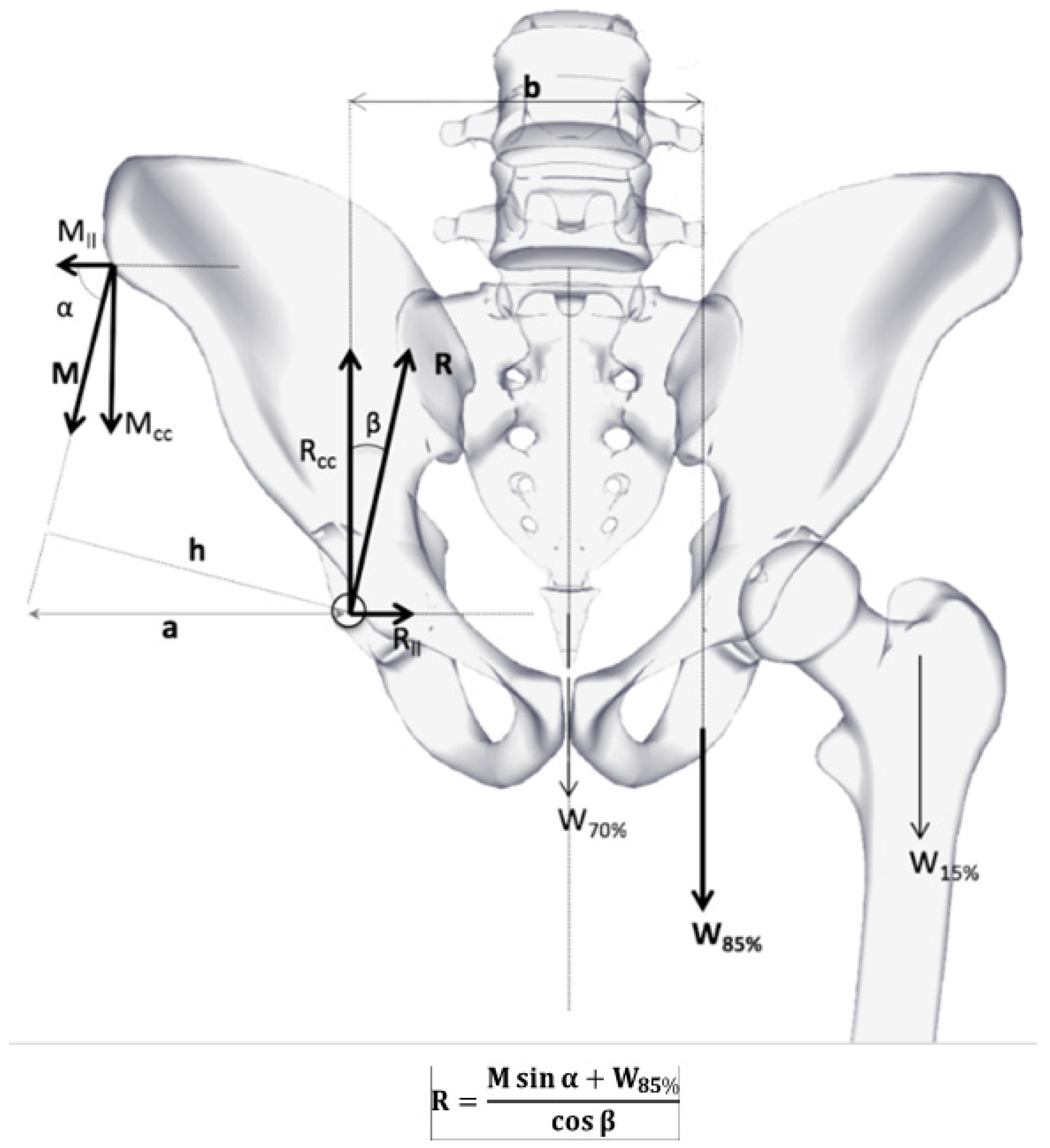
2. Materials and Methods
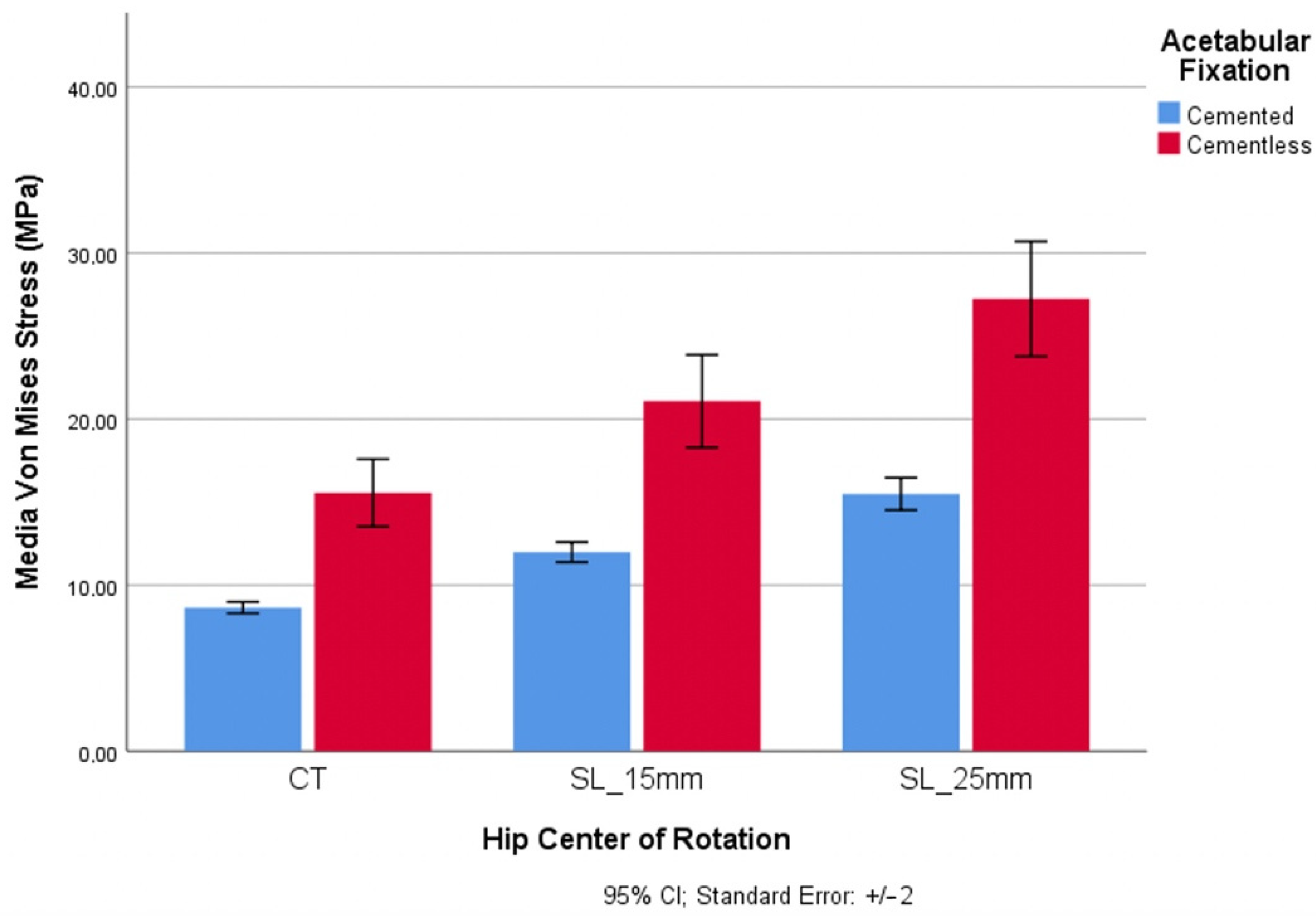
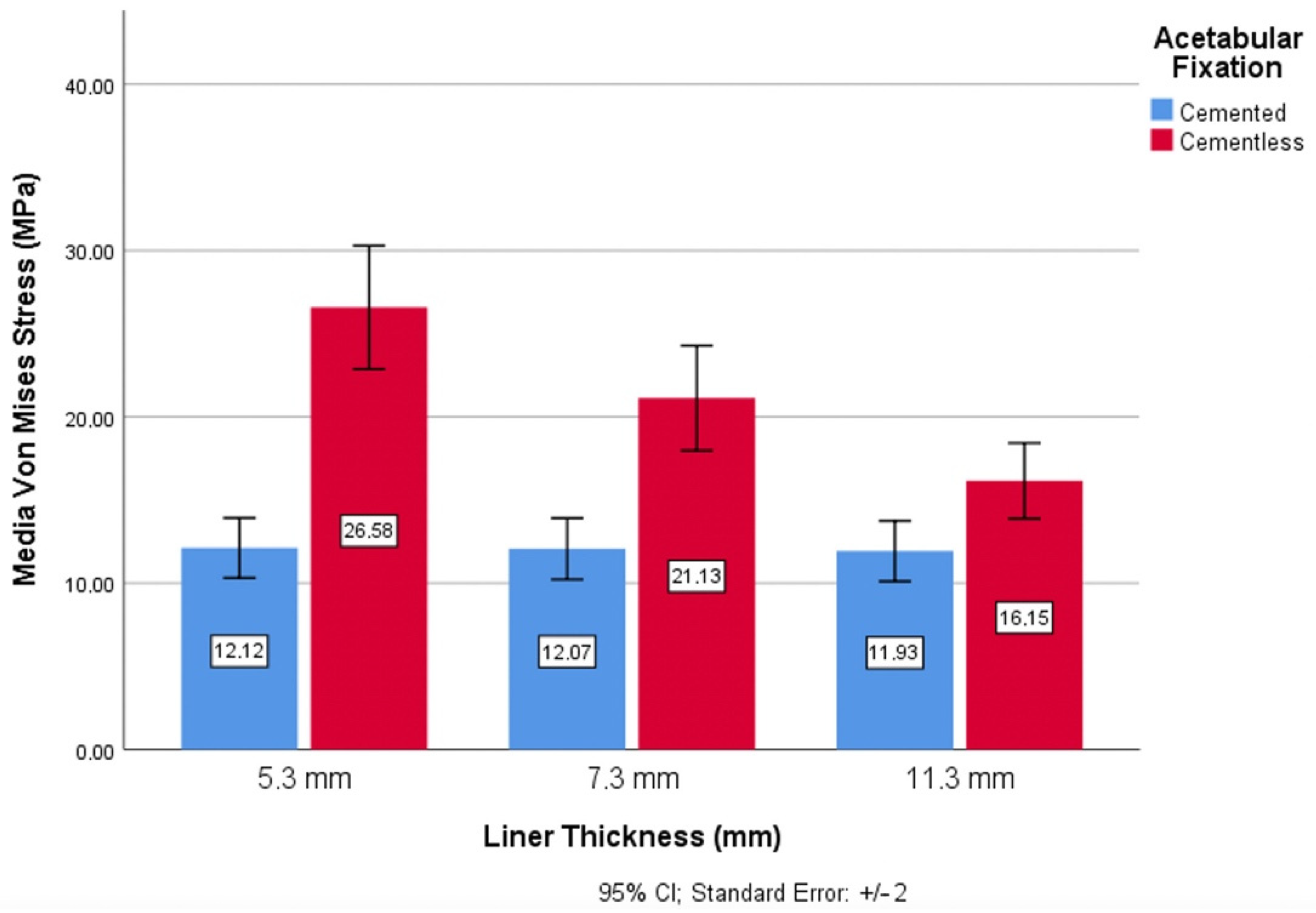
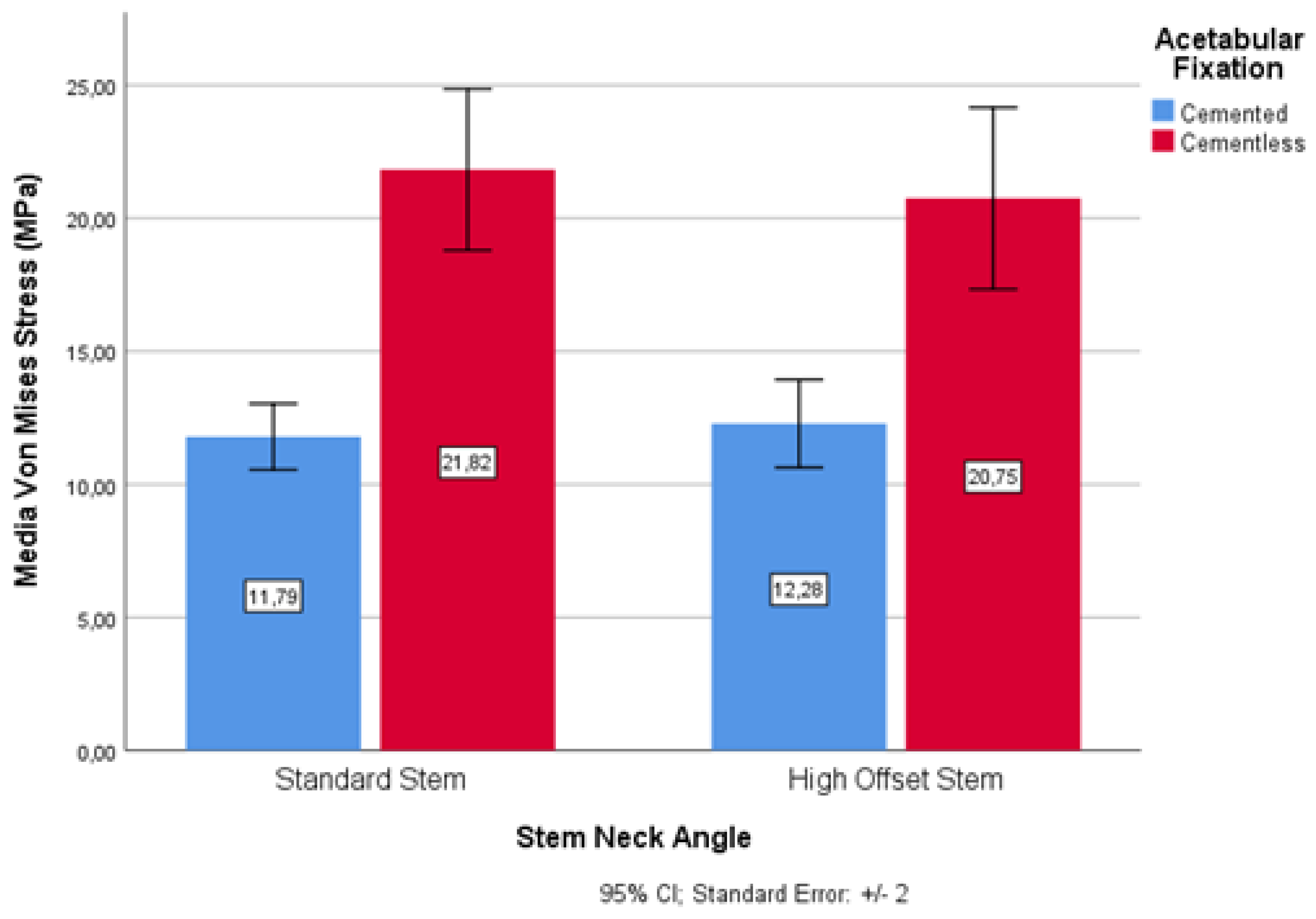
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Learmonth, I.D.; Young, C.; Rorabeck, C. The operation of the century: Total hip replacement. Lancet 2007, 370, 1508–1519. [Google Scholar] [CrossRef]
- Sloan, M.; Premkumar, A.; Sheth, N.P. Projected volume of primary total joint arthroplasty in the US, 2014 to 2030. JBJS 2018, 100, 1455–1460. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Glassman, A.H. What’s new in hip replacement. JBJS 2018, 100, 1616–1624. [Google Scholar] [CrossRef] [PubMed]
- Charnley, J. The long-term results of low-friction arthroplasty of the hip performed as a primary intervention. J. Bone Jt. Surg. Br. Vol. 1972, 54, 61–76. [Google Scholar] [CrossRef]
- García-Cimbrelo, E.; Munuera, L. Early and late loosening of the acetabular cup after low-friction arthroplasty. J. Bone Jt. Surg. Am. Vol. 1992, 74, 1119–1129. [Google Scholar] [CrossRef]
- Irie, T.; Oyama, M.; Kita, A.; Sakamoto, T.; Funayama, K. Medium-term result of Elite Plus hip arthroplasty: The second modular evolution of the original Charnley low-friction arthroplasty. J. Orthop. Sci. 2012, 17, 699–704. [Google Scholar] [CrossRef]
- McCombe, P.; Williams, S.A. A comparison of polyethylene wear rates between cemented and cementless cups: A prospective, randomised trial. J. Bone Jt. Surg. Br. Vol. 2004, 86, 344–349. [Google Scholar] [CrossRef] [PubMed]
- Hailer, N.P.; Garellick, G.; Kärrholm, J. Uncemented and cemented primary total hip arthroplasty in the Swedish Hip Arthroplasty Register: Evaluation of 170,413 operations. Acta Orthop. 2010, 81, 34–41. [Google Scholar] [CrossRef] [PubMed]
- Bragdon, C.R.; Doerner, M.; Martell, J.; Jarrett, B.; Palm, H.; Malchau, H. The 2012 John Charnley Award: Clinical multicenter studies of the wear performance of highly crosslinked remelted polyethylene in THA. Clin. Orthop. Relat. Res. 2013, 471, 393–402. [Google Scholar] [CrossRef]
- Scheerlinck, T. Cup positioning in total hip arthroplasty. Acta Orthop. Belg. 2014, 80, 336–347. [Google Scholar]
- Wang, A. A unified theory of wear for ultra-high molecular weight polyethylene in multi-directional sliding. Wear 2001, 248, 38–47. [Google Scholar] [CrossRef]
- Liu, F.; Leslie, I.; Williams, S.; Fisher, J.; Jin, Z. Development of computational wear simulation of metal-on-metal hip resurfacing replacements. J. Biomech. 2008, 41, 686–694. [Google Scholar] [CrossRef] [PubMed]
- Saikko, V.; Calonius, O. An improved method of computing the wear factor for total hip prostheses involving the variation of relative motion and contact pressure with location on the bearing surface. J. Biomech. 2003, 36, 1819–1827. [Google Scholar] [CrossRef]
- Zietz, C.; Fabry, C.; Baum, F.; Bader, R.; Kluess, D. The Divergence of Wear Propagation and Stress at Steep Acetabular Cup Positions Using Ceramic Heads and Sequentially Cross-Linked Polyethylene Liners. J. Arthroplast. 2015, 30, 1458–1463. [Google Scholar] [CrossRef]
- Barbour, P.S.M.; Barton, D.C.; Fisher, J. The influence of contact stress on the wear of UHMWPE for total replacement hip prostheses. Wear 1995, 181–183, 250–257. [Google Scholar] [CrossRef]
- Taylor, M.; Prendergast, P.J. Four decades of finite element analysis of orthopaedic devices: Where are we now and what are the opportunities? J. Biomech. 2015, 48, 767–778. [Google Scholar] [CrossRef]
- Bevill, S.L.; Bevill, G.R.; Penmetsa, J.R.; Petrella, A.J.; Rullkoetter, P.J. Finite element simulation of early creep and wear in total hip arthroplasty. J. Biomech. 2005, 38, 2365–2374. [Google Scholar] [CrossRef] [PubMed]
- Kurtz, S.M.; Edidin, A.A.; Bartel, D.L. The role of backside polishing, cup angle, and polyethylene thickness on the contact stresses in metal-backed acetabular components. J. Biomech. 1997, 30, 639–642. [Google Scholar] [CrossRef]
- Wang, L.; Isaac, G.; Wilcox, R.; Jones, A.; Thompson, J. Finite element analysis of polyethylene wear in total hip replacement: A literature review. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2019, 233, 1067–1088. [Google Scholar] [CrossRef]
- Carreiras, A.R.; Fonseca, E.M.M.; Martins, D.; Couto, R. The axisymmetric computational study of a femoral component to analysis the effect of titanium alloy and diameter variation. J. Comput. Appl. Mech. 2020, 51, 403–410. [Google Scholar]
- Higgins, S.W.; Spratley, E.M.; A Boe, R.; Hayes, C.W.; Jiranek, W.A.; Wayne, J.S. A novel approach for determining three-dimensional acetabular orientation: Results from two hundred subjects. JBJS 2014, 96, 1776–1784. [Google Scholar] [CrossRef]
- Tsikandylakis, G.; Kärrholm, J.; Hailer, N.P.; Eskelinen, A.; Mäkelä, K.; Hallan, G.; Nord Furnes, O.; Pedersen, A.B.; Overgaard, S.; Mohaddes, M. No increase in survival for 36-mm versus 32-mm femoral heads in metal-on-polyethylene THA: A registry study. Clin. Orthop. Relat. Res. 2018, 476, 2367. [Google Scholar] [CrossRef]
- Ranawat, C.S.; Dorr, L.D.; Inglis, A.E. Total hip arthroplasty in protrusio acetabuli of rheumatoid arthritis. J. Bone Joint Surg. Am. 1980, 62, 1059–1065. [Google Scholar] [CrossRef]
- Doehring, T.C.; Rubash, H.E.; Dore, D.E. Micromotion measurements with hip center and modular neck length alterations. Clin. Orthop. Relat. Res. 1999, 362, 230–239. [Google Scholar] [CrossRef]
- Pauwels, F. Biomechanics of the Normal and Diseased Hip; Springer: Berlin, Heidelberg, 1976. [Google Scholar] [CrossRef]
- Li, G.; Peng, Y.; Zhou, C.; Jin, Z.; Bedair, H. The effect of structural parameters of total hip arthroplasty on polyethylene liner wear behavior: A theoretical model analysis. J. Orthop. Res. 2020, 38, 1587–1595. [Google Scholar] [CrossRef]
- Maggs, J.L.; Smeatham, A.; Whitehouse, S.L.; Charity, J.; Timperley, A.J.; Gie, G.A. The Exeter Contemporary flanged cemented acetabular component in primary total hip arthroplasty. Bone Jt. J. 2016, 98, 307–312. [Google Scholar] [CrossRef] [PubMed]
- Gwynne-Jones, D.P.; Gray, A.R. Cemented or uncemented acetabular fixation in combination with the Exeter Universal cemented stem: Long-term survival to 18 years. Bone Jt. J. 2020, 102, 414–422. [Google Scholar] [CrossRef] [PubMed]
- Van Praet, F.; Mulier, M. To cement or not to cement acetabular cups in total hip arthroplasty: A systematic review and re-evaluation. SICOT-J. 2019, 5, 35. [Google Scholar] [CrossRef]
- Van Der Veen, H.C.; Van Jonbergen, H.P.W.; Poolman, R.W.; Bulstra, S.K.; Van Raay, J.J.A.M. Is there evidence for accelerated polyethylene wear in uncemented compared to cemented acetabular components? A systematic review of the literature. Int. Orthop. 2013, 37, 9–14. [Google Scholar] [CrossRef] [PubMed]
- Hartofilakidis, G.; Georgiades, G.; Babis, G.C. A comparison of the outcome of cemented all-polyethylene and cementless metal-backed acetabular sockets in primary total hip arthroplasty. J. Arthroplast. 2009, 24, 217–225. [Google Scholar] [CrossRef]
- Teeter, M.G.; Lanting, B.A.; Naudie, D.D.; McCalden, R.W.; Howard, J.L.; MacDonald, S.J. Highly crosslinked polyethylene wear rates and acetabular component orientation: A minimum ten-year follow-up. Bone Jt. J 2018, 100, 891–897. [Google Scholar] [CrossRef] [PubMed]
- Georgiades, G.; Babis, G.C.; Kourlaba, G.; Hartofilakidis, G. Effect of cementless acetabular component orientation, position, and containment in total hip arthroplasty for congenital hip disease. J. Arthroplast. 2010, 25, 1143–1150. [Google Scholar] [CrossRef] [PubMed]
- Antoniades, J.; Pellegrini, V.D. Cross-sectional anatomy of the ilium: Implications for acetabular component placement in total hip arthroplasty. Clin. Orthop. Relat. Res. 2012, 470, 3537–3541. [Google Scholar] [CrossRef][Green Version]
- Vigdorchik, J.M.; Sharma, A.K.; Elbuluk, A.M.; Carroll, K.M.; Mayman, D.J.; Lieberman, J.R. High offset stems are protective of dislocation in high-risk total hip arthroplasty. J. Arthroplast. 2021, 36, 210–216. [Google Scholar] [CrossRef] [PubMed]
- Weber, M.; Merle, C.; Nawabi, D.H.; Dendorfer, S.; Grifka, J.; Renkawitz, T. Inaccurate offset restoration in total hip arthroplasty results in reduced range of motion. Sci. Rep. 2020, 10, 13208. [Google Scholar] [CrossRef]
- Muratoglu, O.K.; Bragdon, C.R.; O’Connor, D.; Perinchief, R.S.; Estok, D.M.; Jasty, M.; Harris, W.H. Larger diameter femoral heads used in conjunction with a highly cross-linked ultra-high molecular weight polyethylene: A new concept. J. Arthroplast. 2001, 16, 24–30. [Google Scholar] [CrossRef] [PubMed]
- Johnson, A.J.; Loving, L.; Herrera, L.; Delanois, R.E.; Wang, A.; Mont, M.A. Short-term wear evaluation of thin acetabular liners on 36-mm femoral heads. Clin. Orthop. Relat. Res. 2014, 472, 624–629. [Google Scholar] [CrossRef]
- Shen, F.-W.; Lu, Z.; McKellop, H.A. Wear versus thickness and other features of 5-Mrad crosslinked UHMWPE acetabular liners. Clin. Orthop. Relat. Res. 2011, 469, 395–404. [Google Scholar] [CrossRef]
- Tower, S.S.; Currier, J.H.; Currier, B.H.; Lyford, K.A.; Van Citters, D.W.; Mayor, M.B. Rim cracking of the cross-linked longevity polyethylene acetabular liner after total hip arthroplasty. JBJS 2007, 89, 2212–2217. [Google Scholar] [CrossRef]


| Liner Thickness (mm) | Element Type/Mesh Quality | Elements Size (mm) | Total Elements | Total Nodes | Element Accept. Ratio < 3 (%) |
|---|---|---|---|---|---|
| 5.3 | Solid Hexahedron/High quality | 1.14319 | 55,010 | 82,156 | 99.1 |
| 7.3 | 77,960 | 113,960 | 99.1 | ||
| 11.3 | 137,728 | 196,708 | 99.5 |
| E 1 (MPa) | G 2 (MPa) | ν 3 | Fy 4 (MPa) | fu 5 (MPa) 2 | Strain Max (%) |
|---|---|---|---|---|---|
| 940 | 322 | 0.46 | 25 | 40 | 500 |
| Head Femoral Material | E 1 (GPa) | ν 2 | μ (32) 3 |
|---|---|---|---|
| CoCr | 210 | 0.30 | 0.133 |
| ZrO2 | 358 | 0.24 | 0.096 |
| Std. Error | p-Value | |
|---|---|---|
| Acetabular Fixation | 0.672 | <0.0001 |
| Cervical–Diaphyseal Morphology | 0.672 | 0.664 |
| Thickness Liner | 0.412 | <0.0001 |
| Acetabular Component Positioning | 0.273 | <0.0001 |
| Head Material | 0.943 | 0.01 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
De la Torre, B.; Barrios, L.; De la Torre-Mosquera, J.; Bujan, J.; Ortega, M.A.; González-Bravo, C. Analysis of the Risk of Wear on Cemented and Uncemented Polyethylene Liners According to Different Variables in Hip Arthroplasty. Materials 2021, 14, 7243. https://doi.org/10.3390/ma14237243
De la Torre B, Barrios L, De la Torre-Mosquera J, Bujan J, Ortega MA, González-Bravo C. Analysis of the Risk of Wear on Cemented and Uncemented Polyethylene Liners According to Different Variables in Hip Arthroplasty. Materials. 2021; 14(23):7243. https://doi.org/10.3390/ma14237243
Chicago/Turabian StyleDe la Torre, Basilio, Loreto Barrios, Juan De la Torre-Mosquera, Julia Bujan, Miguel A. Ortega, and Carlos González-Bravo. 2021. "Analysis of the Risk of Wear on Cemented and Uncemented Polyethylene Liners According to Different Variables in Hip Arthroplasty" Materials 14, no. 23: 7243. https://doi.org/10.3390/ma14237243
APA StyleDe la Torre, B., Barrios, L., De la Torre-Mosquera, J., Bujan, J., Ortega, M. A., & González-Bravo, C. (2021). Analysis of the Risk of Wear on Cemented and Uncemented Polyethylene Liners According to Different Variables in Hip Arthroplasty. Materials, 14(23), 7243. https://doi.org/10.3390/ma14237243








