Adhesive-Ceramic Interface Behavior in Dental Restorations. FEM Study and SEM Investigation
Abstract
1. Introduction
2. Materials and Methods
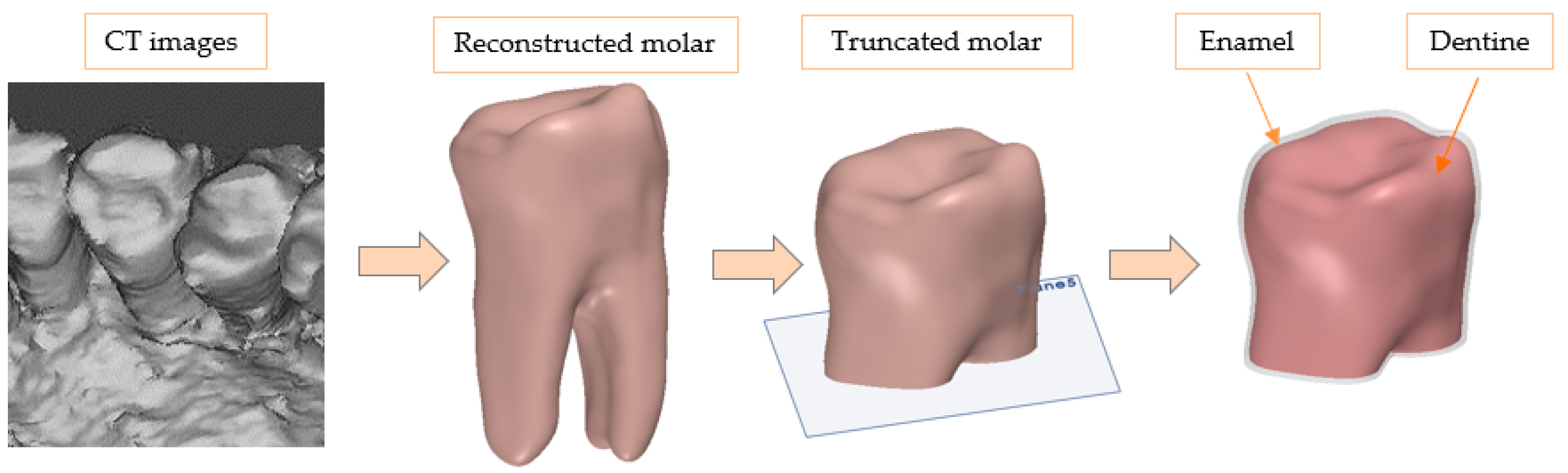
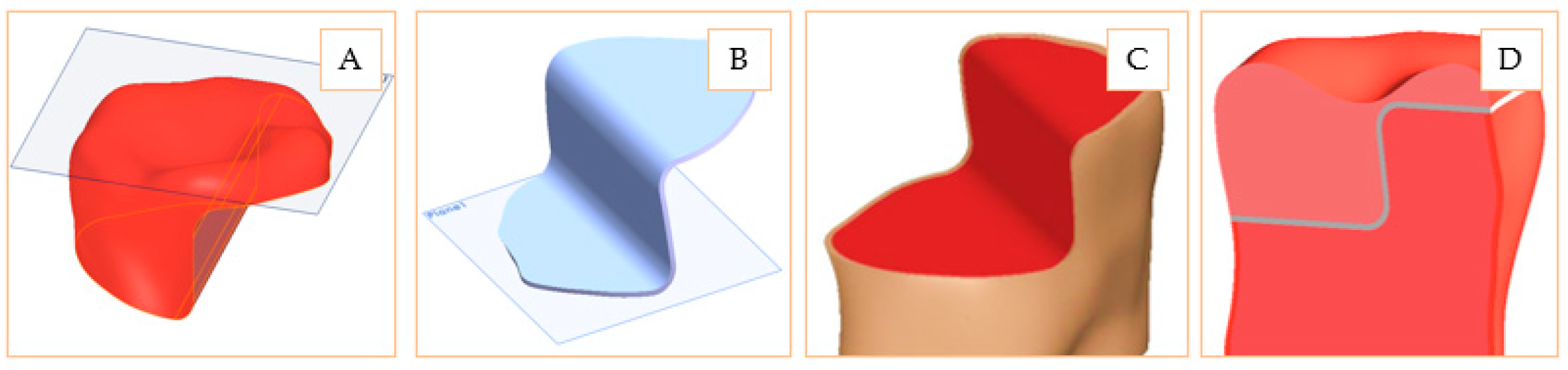
2.1. Design of Inlay and Onlay Restorations
2.2. Defining the Materials and Model Association
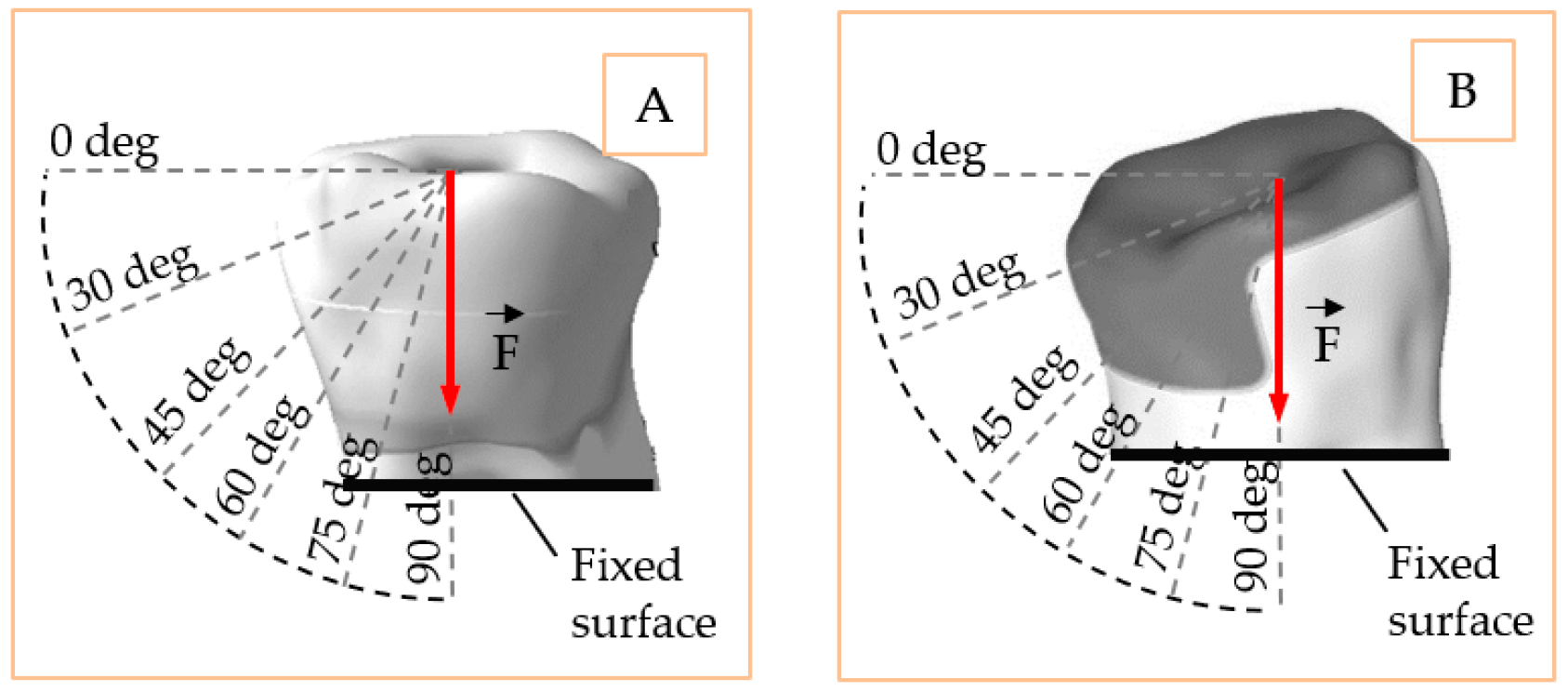
2.3. Loading, Fixing Conditions, Contacts and Discretization of the Models
2.4. Scanning Light Microscopy Analysis
3. Results
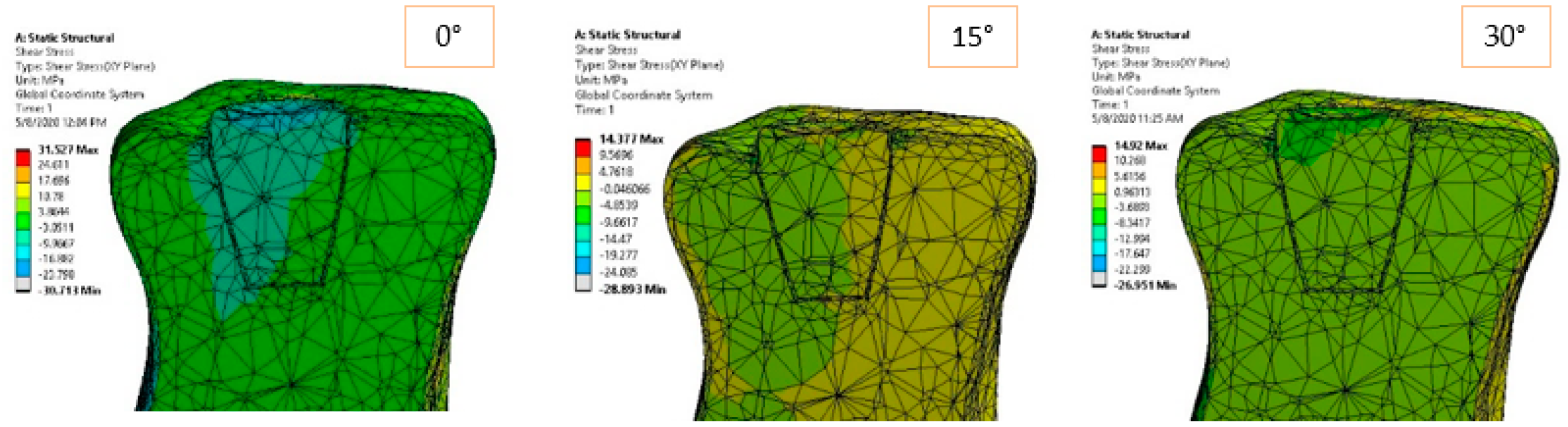
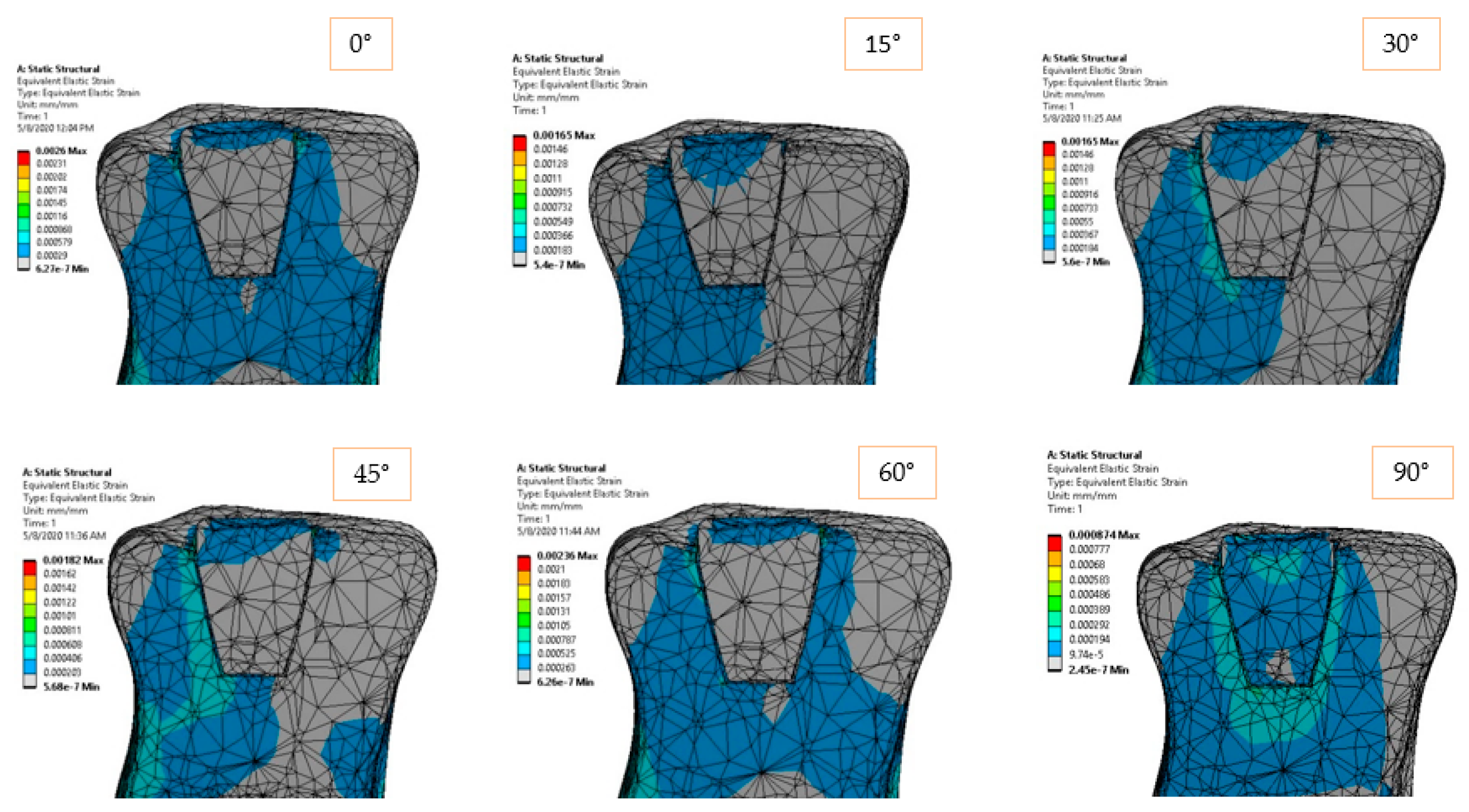
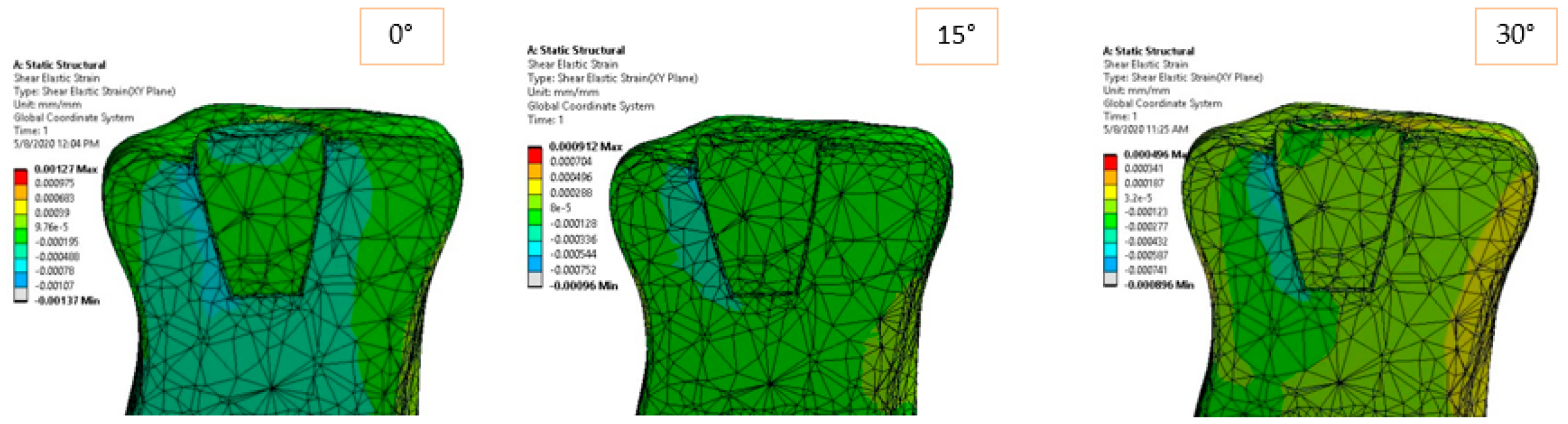
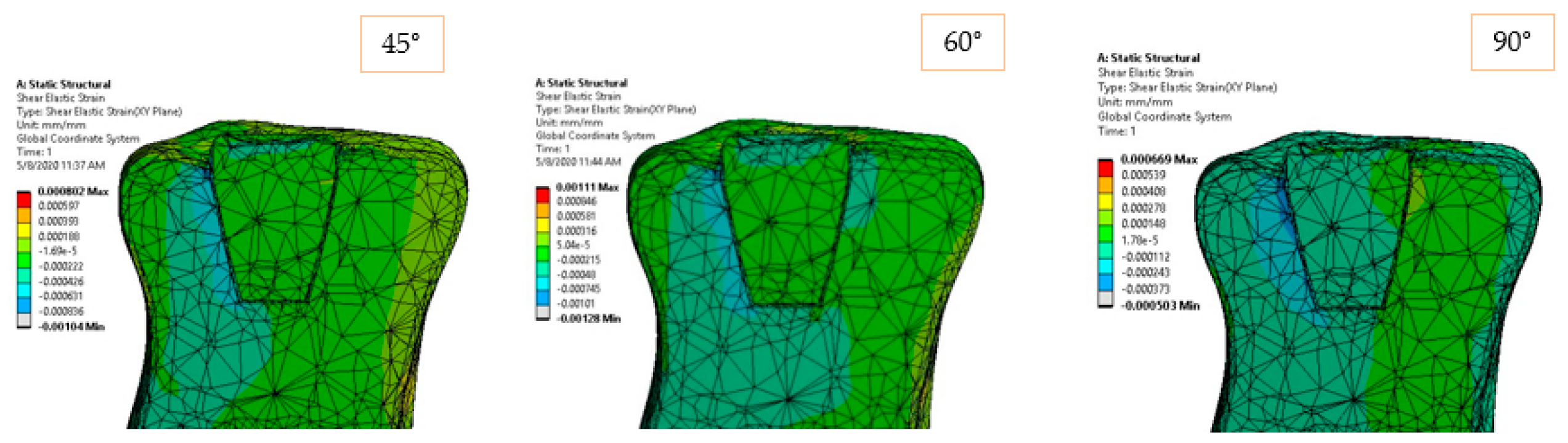
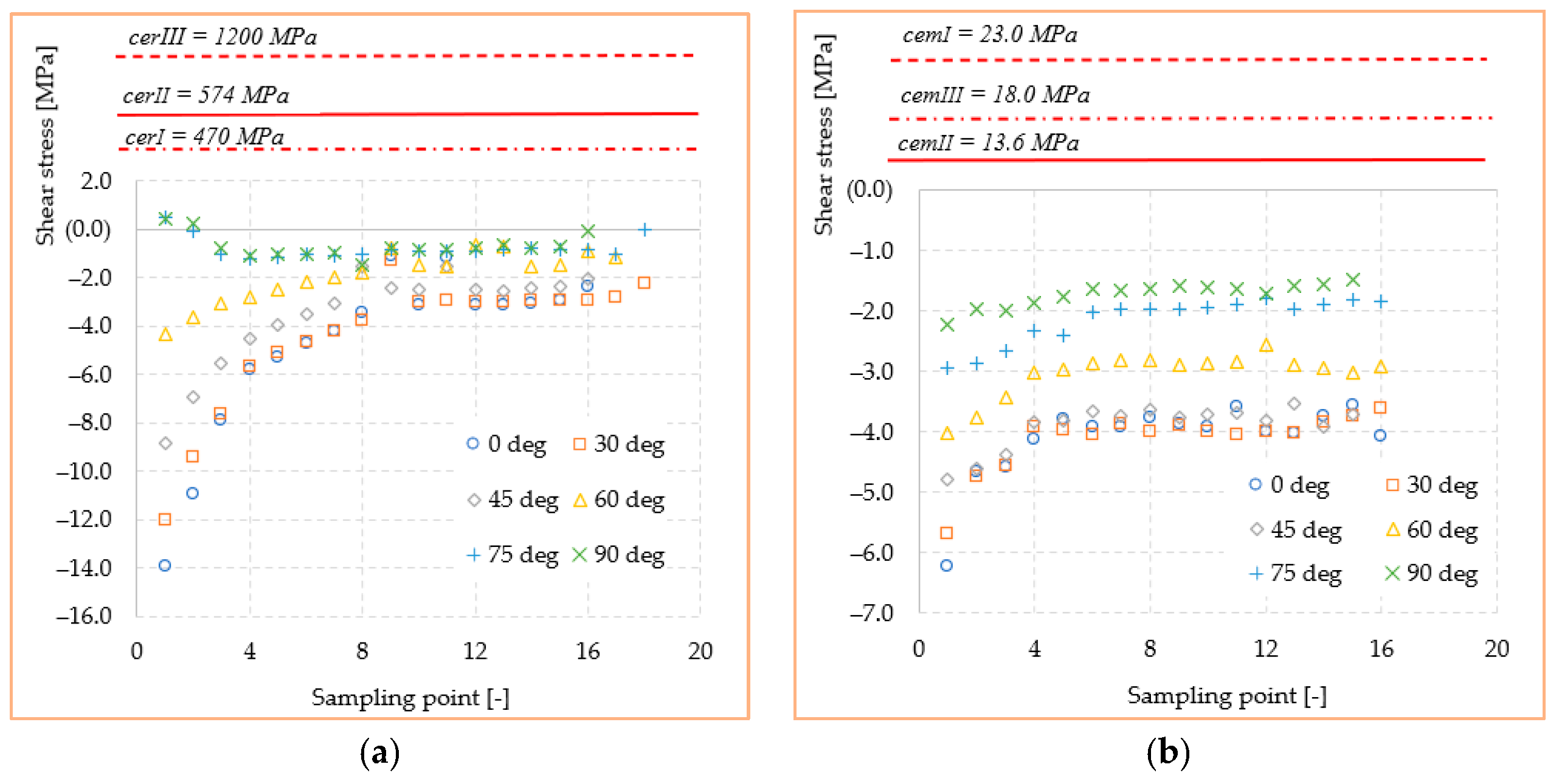
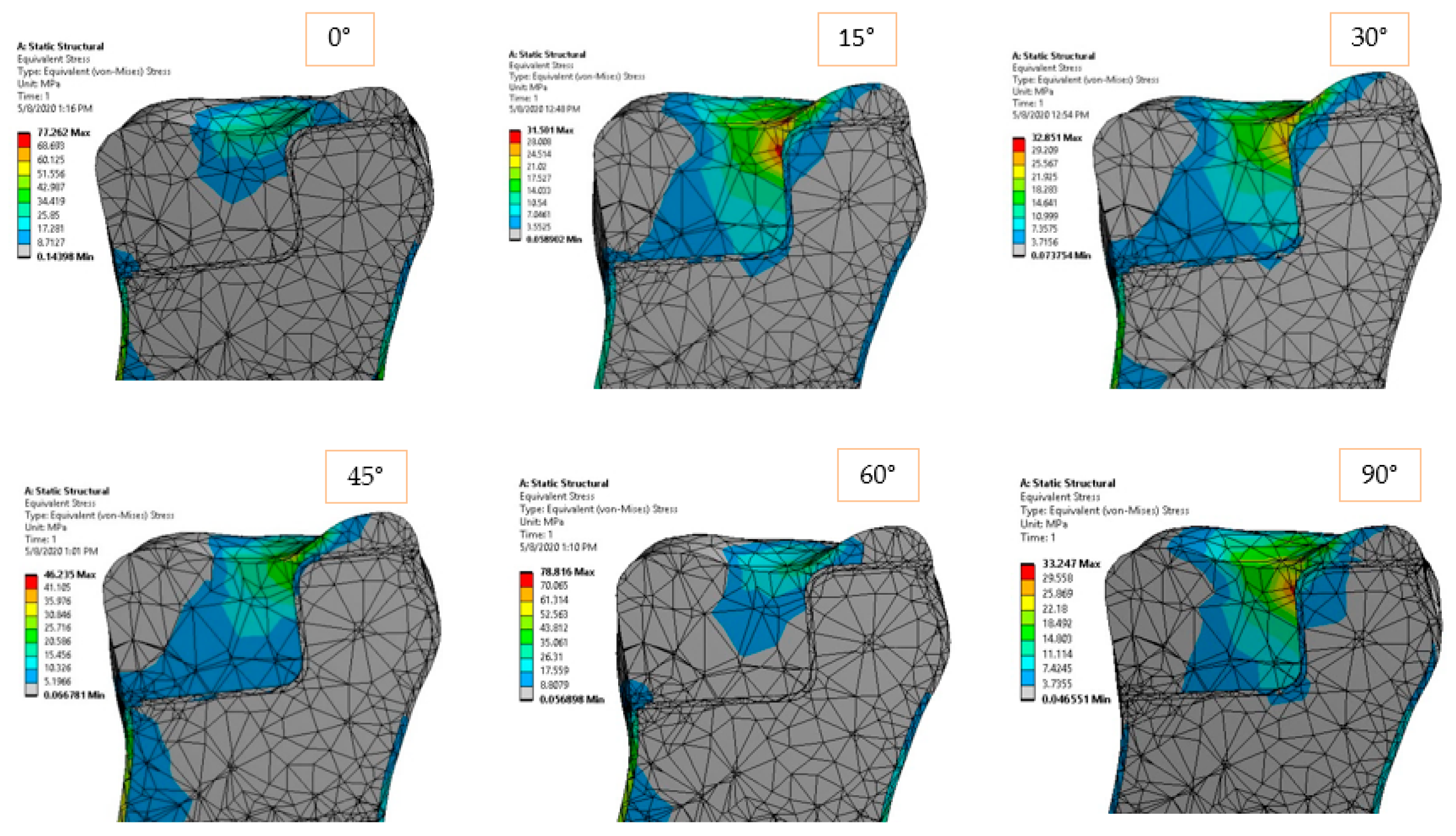
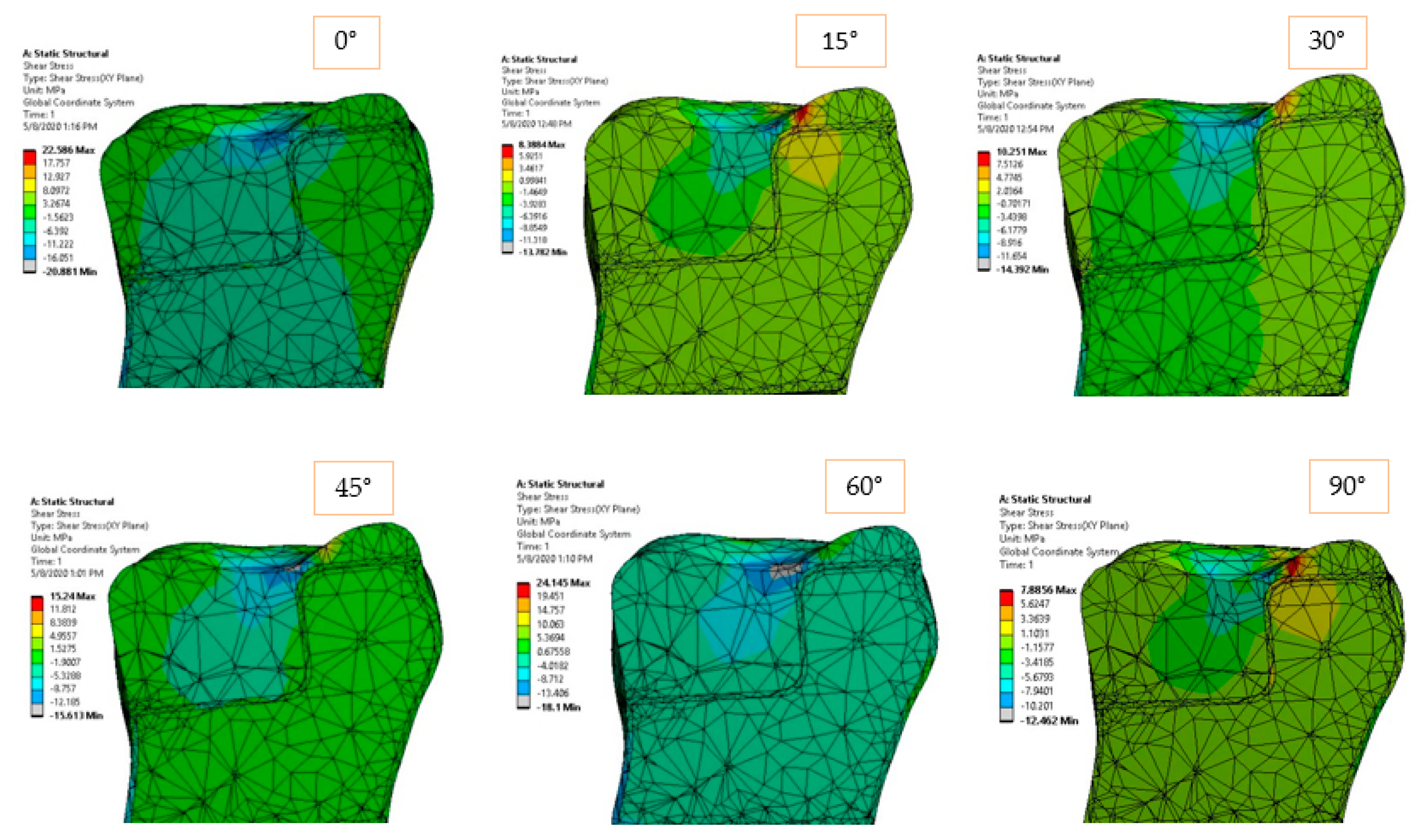
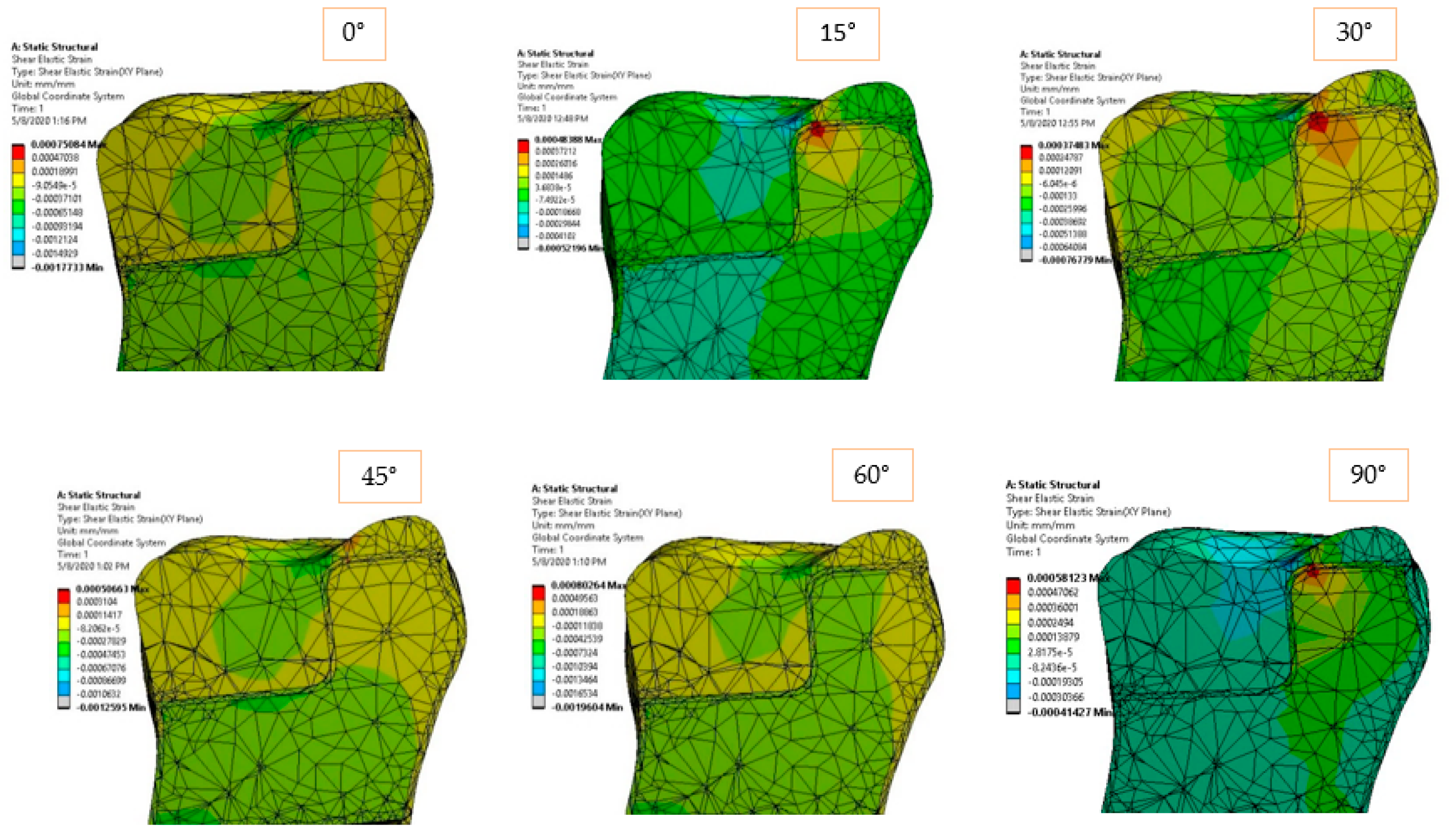
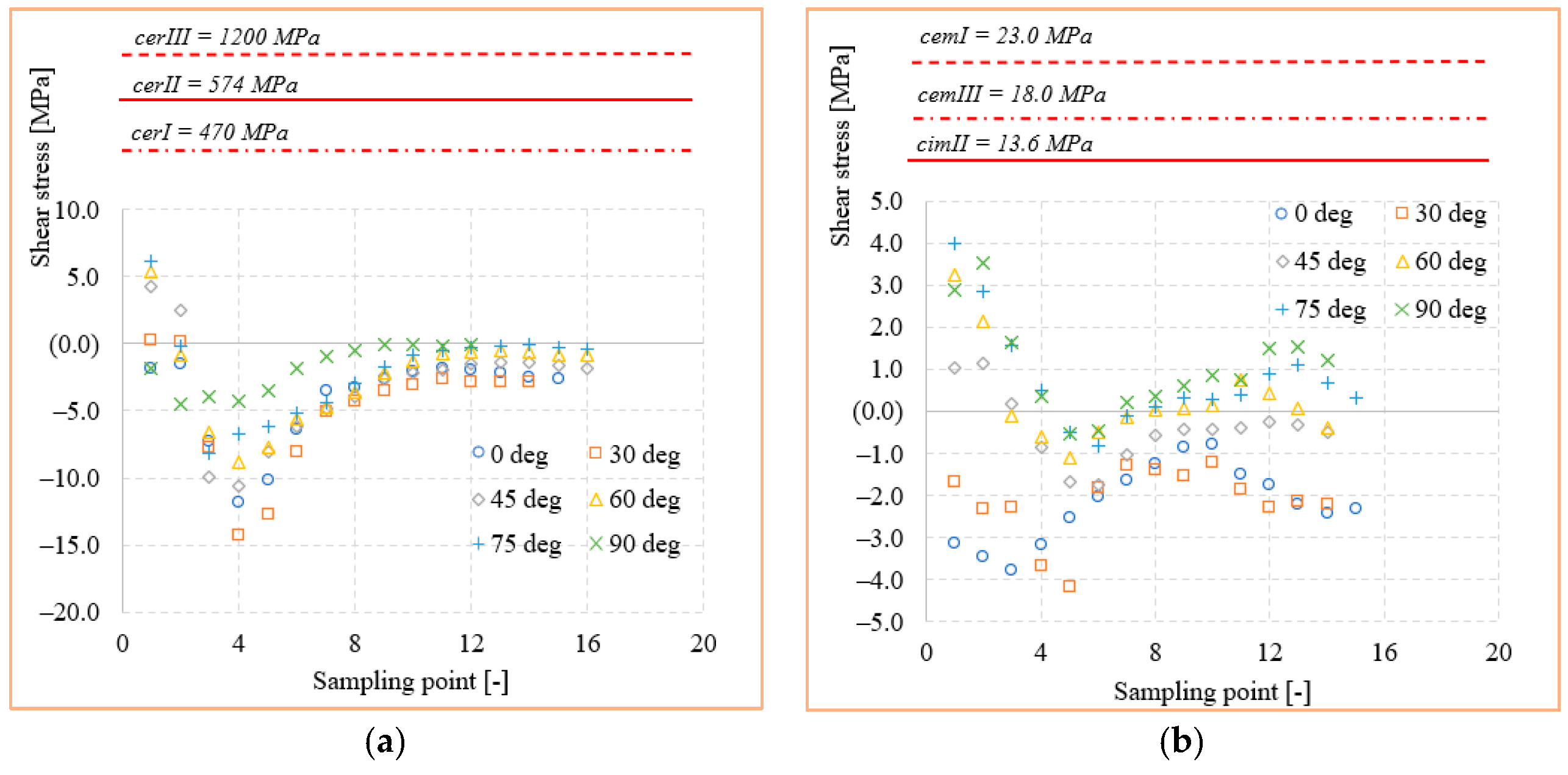
3.1. Inlay Model Simulation
3.2. Onlay Model Simulation
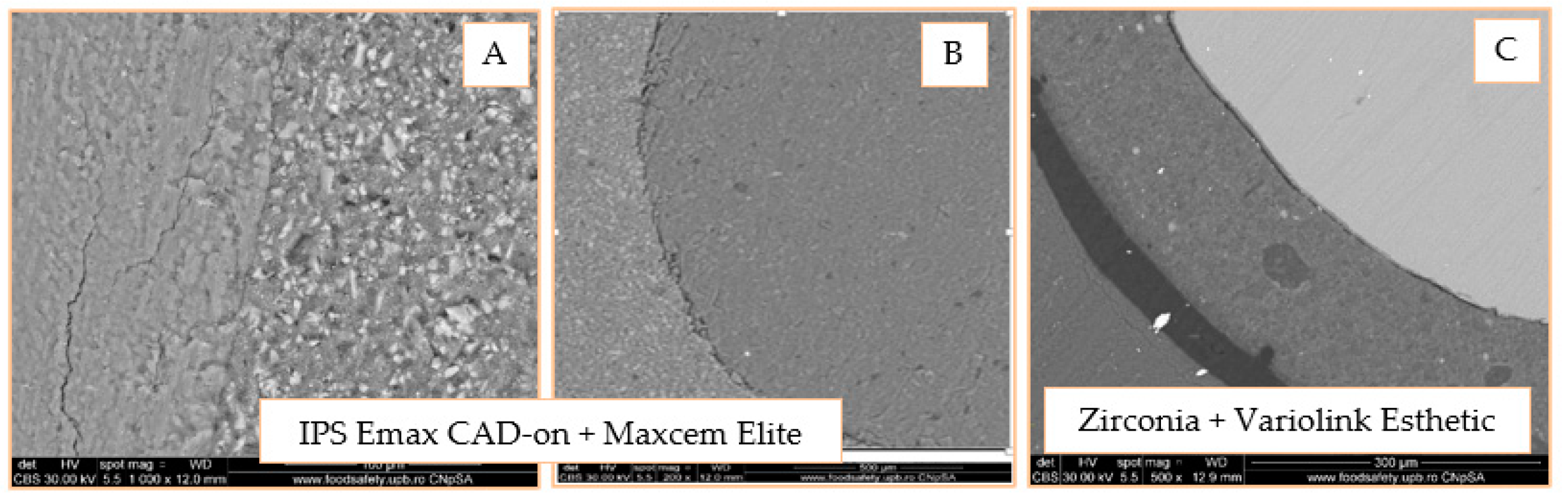
3.3. SEM Analysis of Inlay Model
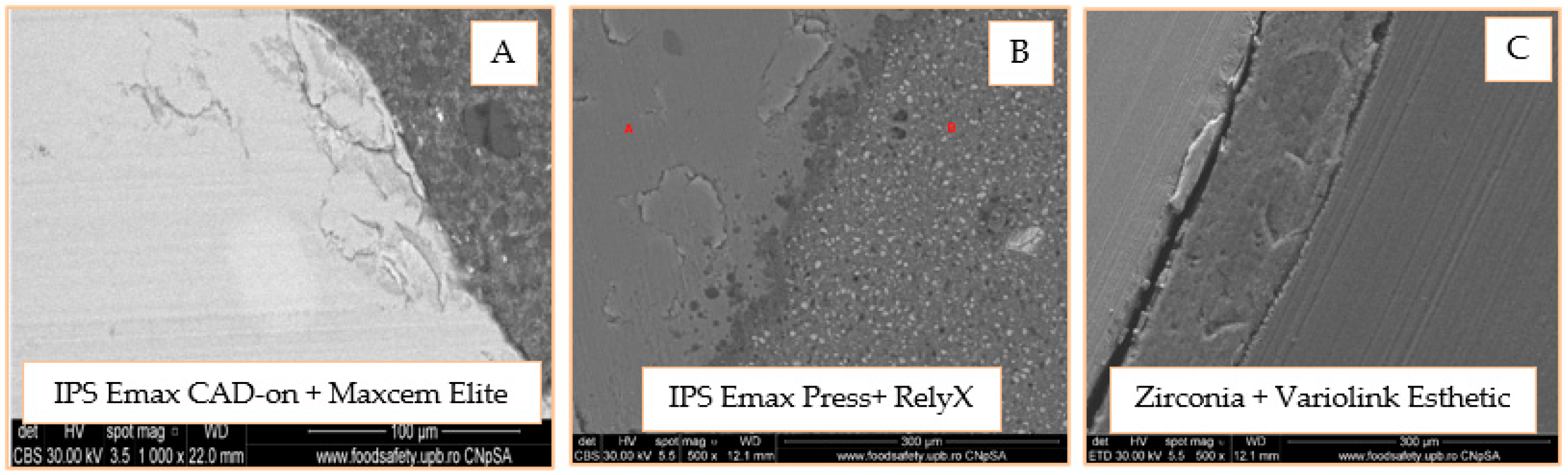
3.4. SEM Analysis of Onlay Model
4. Discussions
5. Conclusions
- The mechanical strength values of the ceramics (cerI, cerII, cerIII) are superior by at least one order of magnitude to the equivalent and shear stress values in either inlay and onlay models. This confirms that a real loading value similar to a simulated one cannot produce a mechanical failure of any of the ceramics.
- The adhesive cements, especially dual-cure cemIII, had a mechanical strength limit very close to the stress values obtained in the critical points of the structures. This could lead in practice to fracture initiation sites, especially when the applied load is oblique or tangent to the molar.
- Shear stresses show jumps of 100–200% due to the dimensional leap of onlay reconstruction. This type of structure is at least geometrically inferior to the inlay, making it a good candidate for crack failure when accidental force occurs.
- The adhesion between the restorations and the tooth structure can stabilize the ceramic restorations, resulting in higher resistance to the action of external forces.
- The adhesive cement/restoration interface seems to be more difficult to achieve in inlay; self-adhesive and universal cements seem to be more efficient in onlay type restorations.
- The adhesive cement/dental structure interface is much more efficient both for the types of design and for all types of cementing techniques.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Yang, H.; Park, C.; Shin, J.H.; Yun, K.D.; Lim, H.P.; Park, S.W.; Chung, H. Stress distribution in premolars restored with inlays or onlays: 3D finite element analysis. J. Adv. Prosthodont. 2018, 10, 90. [Google Scholar] [CrossRef] [PubMed]
- Baciu, S.; Berece, C.; Florea, A.; Burde, A.V.; Negrutiu, M.L.; Szuhanek, C.; Sinescu, C.; Duma, V.F.; Manole, M.A. Comparative Three- and Bi-dimensional Research of the Marginal Fit of Pressed Lithium Disilicate Inlays. Rev. Chim. 2017, 68, 1316. [Google Scholar] [CrossRef]
- Amesti-Garaizabal, A.; Agustín-Panadero, R.; Verdejo-Solá, B.; Fons-Font, A.; Fernández-Estevan, L.; Montiel-Company, J.; Solá-Ruíz, M.F. Fracture Resistance of Partial Indirect Restorations Made with CAD/CAM Technology. A Systematic Review and Meta-Analysis. J. Clin. Med. 2019, 8, 1932. [Google Scholar] [CrossRef] [PubMed]
- Flávia, B.W.R.; Özcan, M.; Gimenez, T.C.; Moreira, M.S.C.A.; Tedesco, T.K.; Morimoto, S. Effects of manufacturing methods on the survival rate of ceramic and indirect composite restorations: A systematic review and meta-analysis. JERD 2019, 31, 561–571. [Google Scholar]
- Silva, L.H.; Miranda, R.; Favero, S.S.; Lohbauer, U.; Cesar, P.F. Dental ceramics: A review of new materials and processing methods. Braz. Oral Res. 2017, 31 (Suppl. S1), e58. [Google Scholar] [CrossRef]
- Dietschi, D.; Spreafico, R. Current clinical concepts for adhesive cementation of tooth–colored posterior restorations. Pract. Periodontics Aesthet. Dent. 1998, 10, 47–55. [Google Scholar]
- Subramanian, D. All ceramic cementation protocols and resin cements for bonding: A key to success. JIDAM 2019, 6, 58–65. [Google Scholar]
- Al-Assaf, K.; Chakmakchi, M.; Palaghias, G.; Karanika-Kouma, A.; Eliades, G. Interfacial characteristics of adhesive luting resins and composites with dentin. Dent. Mater. 2007, 23, 829–839. [Google Scholar] [CrossRef]
- Navez, L.Z.; Soares, C.J.; Moraes, R.R.; Goncalves, L.S.; Sinhoreti, M.A.; Correr-Sobrinho, L. Surface/Interface morphology and bond strength to glass ceramic etched for different periods. Oper. Dent. 2010, 35, 420–427. [Google Scholar] [CrossRef]
- Gloria, A.; Maietta, S.; Richetta, M.; Ausiello, P.; Martorelli, M. Metal posts and the effect of material–shape combination on the mechanical behavior of endodontically treated anterior teeth. Metals 2019, 9, 125. [Google Scholar] [CrossRef]
- Koc, D.; Dogan, A.; Bek, B. Bite Force and Influential Factors on Bite Force Measurements: A Literature Review. Eur. J. Dent. 2010, 4, 223–232. [Google Scholar] [CrossRef]
- Zhao, Y.; Ye, D. Measurement of biting force of normal teeth at different ages. Hua Xi Yi Ke Da Xue Xue Bao J. West China Univ. Med Sci. Huaxi Yike Daxue Xuebao 1994, 25, 414–417. (In Chinese) [Google Scholar]
- Takaki, P.; Vieira, M.; Bommarito, S. Maximum bite force analysis in different age groups. Int. Arch. Otorhinolaryngol. 2014, 18, 272–276. [Google Scholar]
- Magne, P. Virtual prototyping of adhesively restored, endodontically treated molars. J. Prosthet. Dent. 2010, 103, 343.e51. [Google Scholar] [CrossRef]
- Abo-Hamar, S.E.; Hiller, K.A.; Jung, H.; Federlin, M.; Friedl, K.H.; Schmalz, G. Bond strength of a new universal self-adhesive resin luting cement to dentin and enamel. Clin. Oral Investig. 2005, 9, 161–167. [Google Scholar] [CrossRef]
- Sessle, B.J. Neural Basis of Oral and Facial Function; Reference Module in Biomedical Sciences; Elsevier: Amsterdam, The Netherlands, 2014. [Google Scholar]
- Dawod, N.; Florescu, A.; Antoniac, I.V.; Stoia, D.I.; Hancu, V.; Biclesanu, F.C. The FEA Study of the Biomecanic Behavior of Canine Reconstructed with Composite Resin. Rev. Chim. 2019, 70, 2456–2462. [Google Scholar]
- Antoniac, I.V.; Stoia, D.I.; Ghiban, B.; Tecu, C.; Miculescu, F.; Vigaru, C.; Saceleanu, V. Failure analysis of a Humeral Shaft Locking Compression Plate—Surface Investigations and FEM Simulation by Finite Element Method. Materials 2019, 12, 1128. [Google Scholar] [CrossRef]
- Marinescu, R.; Antoniac, V.I.; Stoia, D.I.; Laptoiu, D.C. Clavicle anatomical osteosynthesis plate breakage-failure analysis report based on patient morphological parameters. Rom. J. Morphol. Embryol. 2017, 58, 593–598. [Google Scholar]
- Toth-Tascau, M.; Stoia, D.I. Modeling and Numerical Analysis of a Cervical Spine Unit. In Biologically Responsive Biomaterials for Tissue Engineering; Springer: Berlin/Heidelberg, Germany, 2012; pp. 137–171. [Google Scholar]
- Kandziora, F.; Ludwing, K. Biomechanical assessment of four different anterior atlanto axial plates. In Proceedings of the North American Spine Society 15th Annual Meeting, New Orleans, LA, USA, 26 October 2000. [Google Scholar]
- Brinckmann, P.; Frobin, W.; Gunnar, W.E. Musculoskeletal Biomechanics; Thieme: Stuttgart, Germany; New York, NY, USA, 2000. [Google Scholar]
- Drăgulescu, D. Modelarea în Biomecanică; Editura Didactică şi Pedagogică: Bucureşti, Romania, 2005. [Google Scholar]
- Trindade, F.Z.; Valandro, L.F.; de Jager, N.; Bottino, M.A.; Kleverlaan, C.J. Elastic Properties of Lithium Disilicate Versus Feldspathic Inlays: Effect on the Bonding by 3D Finite Element Analysis. J. Prosthodont. 2018, 27, 741–747. [Google Scholar] [CrossRef]
- Furuichi, T.; Takamizawa, T.; Tsujimoto, A.; Miyazaki, M.; Barkmeier, W.W.; Latta, M.A. Mechanical Properties and Sliding-impact Wear Resistance of Self-adhesive Resin Cements. Oper. Dent. 2016, 41, E83–E92. [Google Scholar] [CrossRef]
- Walls, A.W.G.; Lee, J.; McCabe, J.F. The bonding of composite resin to moist enamel. Br. Dent. J. 2001, 191, 148–150. [Google Scholar] [CrossRef][Green Version]
- Kimmes, N.S.; Barkmeier, W.W.; Erickson, R.L.; Latta, M.A. Adhesive Bond Strengths to Enamel and Dentin Using Recommended and Extended Treatment Times. Oper. Dent. 2010, 35, 112–119. [Google Scholar] [CrossRef] [PubMed]
- Malek, S.; Darendeliler, M.A.; Swain, M.V. Physical properties of root cementum: Part I. A new method for 3-dimensional evaluation. Am. J. Orthod. Dentofac. Orthop. 2001, 120, 198–208. [Google Scholar] [CrossRef] [PubMed]
- Sarr, M.; Leye-Benoist, F.; Aidara, A.W.; Faye, B.; Bane, K.; Touré, B. Characterization of the Resin Luting Materials: Percentage, Morphology and Mechanical Properties. J. Dent. Oral Care Med. 2016, 2, 303. [Google Scholar]
- Dal Piva, A.M.O.; Tribst, J.P.M.; Bottino, M.A. Evaluation of shear bond strength and shear stress on zirconia reinforced lithium silicate and high translucency zirconia. J. Oral Res. 2018. In Press. [Google Scholar] [CrossRef][Green Version]
- Dejak, B.; Młotkowski, A. A comparison of mvM stress of inlays, onlays and endocrowns made from various materials and their bonding with molars in a computer simulation of mastication—FEA. Dent. Mater. 2020, 36, 854–864. [Google Scholar] [CrossRef]
- Huang, X.; Hong, N.; Zou, L.; Wu, S.; Li, Y. Estimation of stress distribution and risk of failure for maxillary premolar restored by occlusal veneer with different CAD/CAM materials and preparation designs. Clin. Oral Investig. 2020, 24, 3157–3167. [Google Scholar] [CrossRef]
- Özkir, S.E. Effect of restoration material on stress distribution on partial crowns: A 3D finite element analysis. J. Dent. Sci. 2018, 13, 311–317. [Google Scholar] [CrossRef]
- Wiedenmann, F.; Becker, F.; Eichberger, M.; Stawarczyk, B. Measuring the polymerization stress of self-adhesive resin composite cements by crack propagation. Clin. Oral Investig. 2021, 25, 1011–1018. [Google Scholar] [CrossRef]
- Fabianelli, A.; Pollington, S.; Papacchini, F.; Goracci, C.; Can-Toro, A.; Ferrari, M.; van Noort, R. The effect of different surface treatments on bond strength between leucite rein-forced feldspathic ceramic and composite resin. J. Dent. 2010, 38, 39–43. [Google Scholar] [CrossRef]
- Aguiar, T.R.; Vermelho, P.M.; André, C.B.; Giannini, M. Interfacial ultramorphology evaluation of resin luting cements to dentin: A correlative scanning electron microscopy and transmission electron microscopy analysis: Ultramorphology of Resin Cements to Dentin. Microsc. Res. Tech. 2013, 76, 1234–1239. [Google Scholar] [CrossRef] [PubMed]








| Cement Type | Code | Ceramic Type | Code | Restoration |
|---|---|---|---|---|
| Universal RelyX Ultimate Clicker | cemI | Pressed IPS e.max Press, Ivoclar Vivadent | cerI | inlay, onlay |
| Self-adhesive Maxcem | cemII | Carbonat IPS e.max CAD-on, Ivoclar Vivadent | cerII | inlay, onlay |
| Duble cure Variolink | cemIII | Zirconium oxide Zirconia Novodent GS | cerIII | inlay, onlay |
| Material | Structure | Density [kg/m3] | Young Modulus/ Bending Modulus [MPa] | Poisson’s Ratio [-] |
|---|---|---|---|---|
| cerI | inlay/onlay restoration | 2480 | 82,300 | 0.22 |
| cerII | inlay/onlay restoration | 2480 | 82,300 | 0.23 |
| cerIII | inlay/onlay restoration | 2480 | 88,000 | 0.34 |
| cemI | adhesive cement | 2400 | 7700 | 0.24 |
| cemII | adhesive cement | 2350 | 4400 | 0.24 |
| cemIII | adhesive cement | 2400 | 8100 | 0.25 |
| dentine | dentine | 2000 | 17,000 | 0.30 |
| enamel | enamel | 2750 | 74,000 | 0.23 |
| Material | Group 1 | Group 2 | Group 3 |
|---|---|---|---|
| Restaurative material | IPS e.max CAD-on Ivoclar Vivadent | IPS e.max Press Ivoclar Vivadent | Novodent GS Zirconia |
| Adhesive cement | Maxcem Elite Kerr | RelyX Ultimate 3M ESPE | Variolink Esthetic |
| No. | Loading Direction | Average Stress [MPa] | Standard Deviation [MPa] | |||||
|---|---|---|---|---|---|---|---|---|
| 0° | 30° | 45° | 60° | 75° | 90° | |||
| 1 | 34.37 | 31.53 | 24.34 | 18.60 | 15.45 | 11.78 | 22.68 | 9.01 |
| 2 | 29.08 | 26.28 | 22.17 | 18.60 | 16.56 | 13.33 | 21.00 | 5.98 |
| 3 | 24.18 | 22.02 | 20.01 | 18.02 | 17.96 | 18.22 | 20.07 | 2.56 |
| 4 | 19.00 | 16.03 | 16.31 | 15.62 | 18.19 | 17.17 | 17.05 | 1.32 |
| 5 | 14.67 | 13.23 | 14.19 | 14.43 | 16.82 | 15.93 | 14.88 | 1.29 |
| 6 | 13.33 | 12.17 | 12.68 | 13.36 | 15.54 | 14.46 | 13.59 | 1.23 |
| 7 | 11.96 | 10.78 | 11.55 | 11.89 | 14.44 | 11.84 | 12.08 | 1.24 |
| 8 | 10.48 | 9.51 | 10.20 | 8.30 | 13.32 | 10.51 | 10.39 | 1.66 |
| 9 | 9.23 | 3.72 | 9.60 | 9.90 | 11.63 | 9.29 | 8.89 | 2.68 |
| 10 | 3.55 | 8.20 | 4.02 | 8.70 | 10.66 | 8.29 | 7.24 | 2.82 |
| 11 | 7.90 | 7.91 | 8.44 | 7.70 | 9.33 | 7.64 | 8.15 | 0.64 |
| 12 | 7.73 | 3.35 | 7.97 | 7.29 | 8.36 | 6.99 | 6.95 | 1.83 |
| 13 | 3.42 | 7.45 | 4.42 | 6.91 | 8.10 | 8.48 | 6.46 | 2.06 |
| 14 | 7.61 | 7.19 | 5.02 | 6.78 | 7.55 | 3.92 | 6.34 | 1.52 |
| 15 | 7.58 | 6.78 | 7.48 | 7.12 | 4.45 | 6.92 | 6.72 | 1.16 |
| No. | Loading Direction | Average Stress [MPa] | Standard Deviation [MPa] | |||||
|---|---|---|---|---|---|---|---|---|
| 0° | 30° | 45° | 60° | 75° | 90° | |||
| 1 | 17.04 | 13.69 | 13.35 | 9.58 | 8.54 | 4.27 | 11.08 | 4.53 |
| 2 | 9.83 | 10.98 | 10.29 | 8.53 | 6.60 | 4.55 | 8.47 | 2.46 |
| 3 | 10.38 | 10.40 | 10.04 | 6.43 | 5.77 | 4.69 | 7.95 | 2.61 |
| 4 | 8.49 | 8.90 | 8.54 | 7.34 | 5.81 | 4.67 | 7.29 | 1.71 |
| 5 | 8.82 | 9.26 | 8.69 | 7.54 | 5.71 | 4.73 | 7.46 | 1.85 |
| 6 | 8.78 | 9.15 | 8.76 | 7.32 | 5.77 | 4.72 | 7.42 | 1.83 |
| 7 | 8.63 | 8.76 | 8.40 | 7.28 | 5.82 | 4.68 | 7.26 | 1.68 |
| 8 | 8.84 | 9.10 | 8.86 | 7.36 | 5.03 | 4.74 | 7.32 | 1.99 |
| 9 | 8.97 | 9.25 | 8.95 | 7.40 | 5.03 | 5.13 | 7.45 | 1.95 |
| 10 | 8.80 | 8.06 | 8.79 | 7.39 | 5.69 | 4.72 | 7.24 | 1.69 |
| 11 | 8.81 | 7.91 | 7.75 | 7.31 | 5.45 | 6.15 | 7.23 | 1.23 |
| 12 | 7.96 | 9.10 | 8.16 | 7.32 | 5.40 | 6.92 | 7.48 | 1.27 |
| 13 | 8.03 | 9.38 | 9.39 | 6.69 | 6.37 | 6.93 | 7.80 | 1.35 |
| 14 | 10.92 | 9.51 | 9.88 | 6.42 | 6.67 | 6.94 | 8.39 | 1.94 |
| 15 | 9.68 | 9.90 | 11.18 | 8.40 | 7.54 | 6.94 | 8.94 | 1.60 |
| No. | Loading Direction | Average Stress [MPa] | Standard Deviation [MPa] | |||||
|---|---|---|---|---|---|---|---|---|
| 0° | 30° | 45° | 60° | 75° | 90° | |||
| 1 | 12.98 | 11.89 | 6.64 | 7.41 | 11.42 | 14.91 | 10.88 | 3.22 |
| 2 | 22.54 | 23.34 | 13.78 | 15.74 | 15.40 | 22.03 | 18.81 | 4.27 |
| 3 | 24.94 | 22.76 | 22.32 | 24.47 | 21.50 | 23.48 | 23.24 | 1.31 |
| 4 | 21.92 | 26.94 | 25.17 | 23.92 | 23.99 | 26.63 | 24.76 | 1.89 |
| 5 | 16.48 | 21.68 | 22.00 | 24.80 | 25.51 | 24.81 | 22.55 | 3.37 |
| 6 | 10.51 | 14.66 | 18.91 | 21.79 | 22.77 | 17.74 | 17.73 | 4.58 |
| 7 | 8.44 | 9.87 | 15.44 | 16.91 | 17.89 | 13.22 | 13.63 | 3.83 |
| 8 | 6.82 | 7.86 | 10.92 | 11.88 | 12.84 | 12.01 | 10.39 | 2.46 |
| 9 | 6.16 | 6.53 | 9.48 | 10.41 | 11.64 | 10.94 | 9.20 | 2.32 |
| 10 | 5.36 | 5.48 | 8.64 | 9.61 | 10.61 | 10.16 | 8.31 | 2.33 |
| 11 | 5.40 | 4.75 | 7.30 | 8.80 | 9.52 | 9.27 | 7.51 | 2.04 |
| 12 | 5.71 | 5.14 | 6.56 | 7.89 | 8.58 | 8.78 | 7.11 | 1.53 |
| 13 | 5.84 | 5.43 | 6.56 | 7.61 | 8.23 | 8.64 | 7.05 | 1.31 |
| 14 | 5.96 | 5.47 | 6.47 | 7.42 | 8.10 | 8.56 | 7.00 | 1.23 |
| 15 | 6.01 | 4.42 | 6.46 | 7.35 | 7.98 | 8.26 | 6.75 | 1.43 |
| No. | Loading Direction | Average Stress [MPa] | Standard Deviation [MPa] | |||||
|---|---|---|---|---|---|---|---|---|
| 0° | 30° | 45° | 60° | 75° | 90° | |||
| 1 | 6.22 | 5.77 | 4.74 | 5.07 | 6.63 | 9.76 | 6.37 | 1.80 |
| 2 | 7.42 | 5.89 | 7.19 | 8.85 | 10.15 | 11.20 | 8.45 | 1.99 |
| 3 | 7.67 | 6.23 | 7.92 | 9.26 | 10.10 | 12.50 | 8.94 | 2.20 |
| 4 | 7.42 | 4.18 | 7.37 | 9.84 | 10.03 | 10.81 | 8.27 | 2.46 |
| 5 | 9.47 | 3.36 | 7.44 | 9.11 | 8.26 | 9.43 | 7.84 | 2.33 |
| 6 | 3.97 | 2.75 | 6.12 | 3.23 | 6.83 | 7.96 | 5.14 | 2.12 |
| 7 | 2.98 | 5.37 | 5.11 | 6.47 | 5.74 | 6.96 | 5.44 | 1.39 |
| 8 | 6.14 | 2.25 | 3.96 | 5.25 | 4.60 | 6.02 | 4.70 | 1.46 |
| 9 | 2.40 | 2.61 | 3.07 | 4.40 | 4.16 | 5.02 | 3.61 | 1.07 |
| 10 | 3.05 | 3.30 | 2.54 | 3.59 | 3.86 | 4.58 | 3.49 | 0.70 |
| 11 | 6.44 | 3.60 | 2.16 | 3.25 | 3.78 | 4.32 | 3.93 | 1.43 |
| 12 | 4.84 | 3.67 | 1.98 | 3.03 | 4.01 | 4.51 | 3.67 | 1.04 |
| 13 | 5.02 | 3.82 | 1.81 | 3.15 | 4.28 | 4.59 | 3.78 | 1.16 |
| 14 | 6.11 | 3.79 | 2.12 | 2.59 | 5.28 | 6.85 | 4.46 | 1.92 |
| 15 | 6.03 | 3.66 | 4.41 | 4.09 | 4.99 | 5.88 | 4.84 | 0.96 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chirca, O.; Biclesanu, C.; Florescu, A.; Stoia, D.I.; Pangica, A.M.; Burcea, A.; Vasilescu, M.; Antoniac, I.V. Adhesive-Ceramic Interface Behavior in Dental Restorations. FEM Study and SEM Investigation. Materials 2021, 14, 5048. https://doi.org/10.3390/ma14175048
Chirca O, Biclesanu C, Florescu A, Stoia DI, Pangica AM, Burcea A, Vasilescu M, Antoniac IV. Adhesive-Ceramic Interface Behavior in Dental Restorations. FEM Study and SEM Investigation. Materials. 2021; 14(17):5048. https://doi.org/10.3390/ma14175048
Chicago/Turabian StyleChirca, Otilia, Cornelia Biclesanu, Anamaria Florescu, Dan Ioan Stoia, Anna Maria Pangica, Alexandru Burcea, Marius Vasilescu, and Iulian Vasile Antoniac. 2021. "Adhesive-Ceramic Interface Behavior in Dental Restorations. FEM Study and SEM Investigation" Materials 14, no. 17: 5048. https://doi.org/10.3390/ma14175048
APA StyleChirca, O., Biclesanu, C., Florescu, A., Stoia, D. I., Pangica, A. M., Burcea, A., Vasilescu, M., & Antoniac, I. V. (2021). Adhesive-Ceramic Interface Behavior in Dental Restorations. FEM Study and SEM Investigation. Materials, 14(17), 5048. https://doi.org/10.3390/ma14175048








