Clinical Evaluation of Flowable Composite Materials in Permanent Molars Small Class I Restorations: 3-Year Double Blind Clinical Study
Abstract
1. Introduction
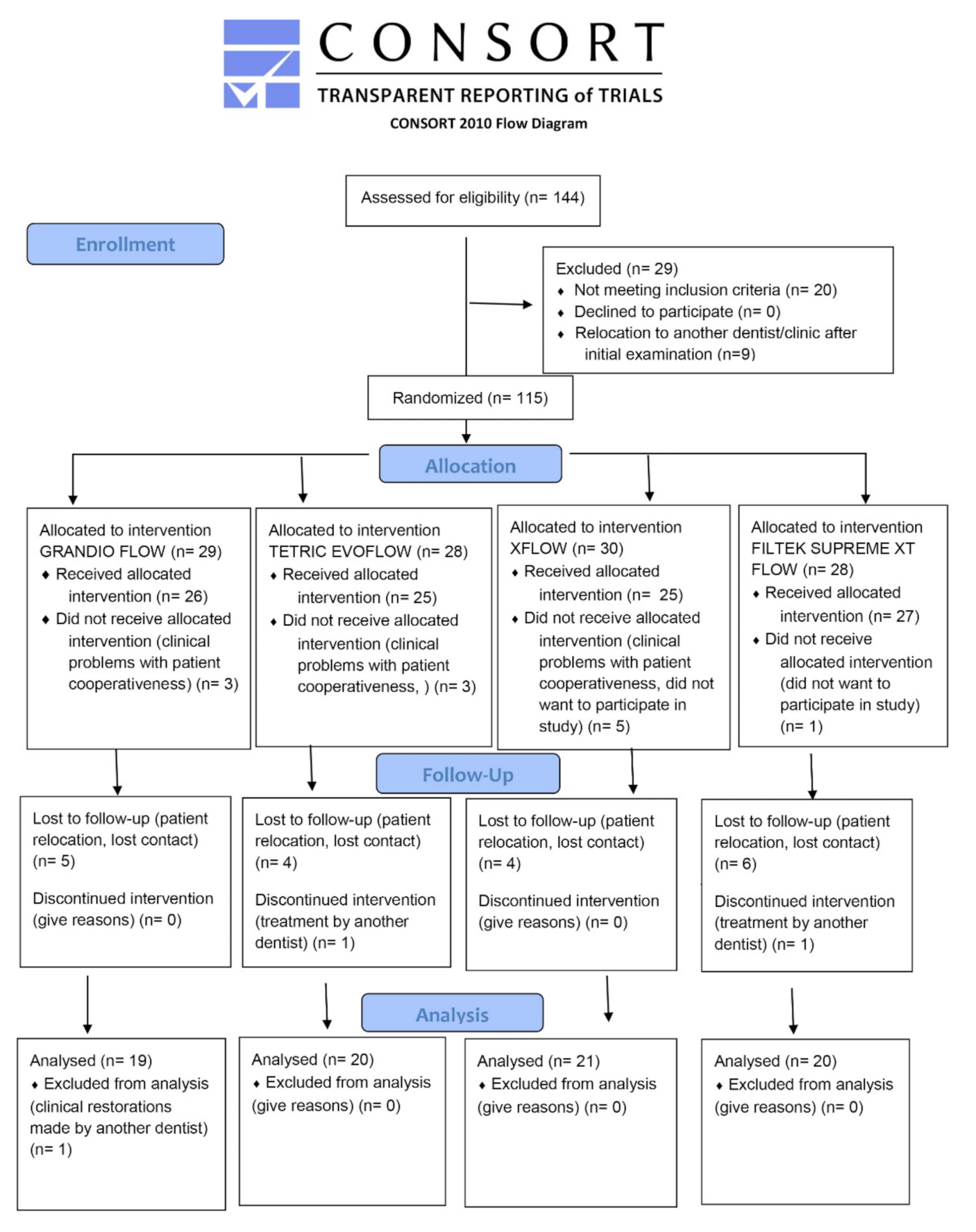
2. Materials and Methods
2.1. Selection Criteria
2.2. Restorative Procedures
2.3. Clinical Evaluation Criteria
2.4. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Donly, K.J.; García-Godoy, F. The Use of Resin-based Composite in Children: An Update. Pediatr. Dent. 2015, 37, 136–143. [Google Scholar]
- U.S. Public Health Service National; Institute of Dental Research. The Prevalence of Dental Caries in United States Children 1979–1980; National Institutes of Health: Bethesda, MD, USA, 1981; pp. 82–2245.
- Swift, E.J., Jr. The effect of sealants on dental caries: A review. J. Am. Dent. Assoc. 1988, 116, 700–704. [Google Scholar] [CrossRef] [PubMed]
- Ripa, L.W. Occlusal sealing: Rationale of the technique and historical review. J. Am. Soc. Prev. Dent. 1973, 3, 32–39. [Google Scholar]
- Ericson, D. The concept of minimally invasive dentistry. Dent. Update 2007, 34, 9–18. [Google Scholar] [CrossRef] [PubMed]
- Peters, M.C.; McLean, M.E. Minimally invasive operative care. I. Minimal intervention and concepts for minimally invasive cavity preparations. J Adhes. Dent. 2001, 3, 7–16. [Google Scholar]
- Peters, M.C.; McLean, M.E. Minimally invasive operative care. II. Contemporary techniques and materials: An overview. J. Adhes. Dent. 2001, 3, 7–16. [Google Scholar]
- Yazici, A.R.; Baseren, M.; Gorucu, J. Clinical comparison of bur- and laser prepared minimally invasive occlusal resin com-posite restorations: Two-year follow-up. Oper. Dent. 2010, 35, 500–507. [Google Scholar] [CrossRef]
- Murdoch-Kinch, C.A.; McLean, M.E. Minimally invasive dentistry. J. Am. Dent. Assoc. 2003, 134, 87–95. [Google Scholar] [CrossRef]
- Simonsen, R.J. Preventive resin restorations (I). Quintessence Int. Dent. Dig. 1978, 9, 69–76. [Google Scholar]
- Simonsen, R.J. Conservation of tooth structure in restorative dentistry. Quintessence Int. 1985, 16, 15–24. [Google Scholar]
- Qin, M.; Liu, H. Clinical evaluation of a flowable resin composite and flowable compomer for preventive resin restorations. Oper. Dent. 2005, 30, 580–587. [Google Scholar]
- Lawson, N.; Radhakrishnan, R.; Givan, D.; Ramp, L.; Burgess, J. Two-year Randomized, Controlled Clinical Trial of a Flowable and Conventional Composite in Class I Restorations. Oper. Dent. 2015, 40, 594–602. [Google Scholar] [CrossRef]
- Seemann, R.; Pfefferkorn, F.; Hickel, R. Behaviour of general dental practitioners in Germany regarding posterior restorations with flowable composites. Int. Dent. J. 2011, 61, 252–256. [Google Scholar] [CrossRef] [PubMed]
- MacKenzie, L.; Banerjee, A. Minimally invasive direct restorations: A practical guide. Br. Dent. J. 2017, 223, 163–171. [Google Scholar] [CrossRef]
- Baroudi, K.; Rodrigues, J.C. Flowable Resin Composites: A Systematic Review and Clinical Considerations. J. Clin. Diagn. Res. 2015, 9, ZE18–ZE24. [Google Scholar] [CrossRef]
- Firla, M.T. Seventeen Years of Using Flowable Resin Restoratives—A Dental Practitioner’s Personal Clinical Review. Dent. Update 2017, 42, 261–268. [Google Scholar] [CrossRef] [PubMed]
- Jang, J.-H.; Park, S.-H.; Hwang, I.-N. Polymerization Shrinkage and Depth of Cure of Bulk-Fill Resin Composites and Highly Filled Flowable Resin. Oper. Dent. 2015, 40, 172–180. [Google Scholar] [CrossRef]
- Chung, K.-H.; Greener, E.H. Correlation between degree of conversion, filler concentration and mechanical properties of posterior composite resins. J. Oral Rehabil. 1990, 17, 487–494. [Google Scholar] [CrossRef]
- Condon, J.R.; Ferracane, J.L. In vitro wear of composite with varied cure, filler level, and filler treatment. J. Dent. Res. 1997, 76, 1405–1411. [Google Scholar] [CrossRef]
- Munksgaard, E.C.; Hansen, E.K.; Kato, H. Wall-to-wall polymerization contraction of composite resins versus filler content. Eur. J. Oral Sci. 1987, 95, 526–531. [Google Scholar] [CrossRef]
- Opdam, N.; Bronkhorst, E.; Loomans, B.; Huysmans, M.C. 12-year Survival of Composite vs. Amalgam Restorations. J. Dent. Res. 2010, 89, 1063–1067. [Google Scholar] [CrossRef]
- Sabbagh, J.; Dagher, S.; El Osta, N.; Souhaid, P. Randomized Clinical Trial of a Self-Adhering Flowable Composite for Class I Restorations: 2-Year Results. Int. J. Dent. 2017, 2017, 5041529. [Google Scholar] [CrossRef]
- Shaalan, O.O.; Abou-Auf, E.; El Zoghby, A.F. Clinical evaluation of self-adhering flowable composite versus conventional flowable composite in conservative Class I cavities: Randomized controlled trial. J. Conserv. Dent. 2018, 21, 485–490. [Google Scholar] [CrossRef]
- Oz, F.D.; Ergin, E.; Cakir, F.Y.; Gurgan, S. Clinical Evaluation of a Self-Adhering Flowable Resin Composite in Minimally Invasive Class I Cavities: 5-year Results of a Double Blind Randomized, Controlled Clinical Trial. Acta Stomatol. Croat. 2020, 5, 10–21. [Google Scholar]
- Hamilton, J.C.; Dennison, J.B.; Stoffers, K.W.; Welch, K.B. A clinical evaluation of air-abrasion treatment of questionable carious lesions. A 12-month report. J. Am. Dent. Assoc. 2001, 132, 762–769. [Google Scholar] [CrossRef] [PubMed]
- Zhegova, G.; Rashkova, M.; Rocca, J.-P. Minimally invasive treatment of dental caries in primary teeth using an Er:YAG Laser. Laser Ther. 2014, 23, 249–254. [Google Scholar] [CrossRef] [PubMed]
- Gallo, J.R.; Burgess, J.O.; Ripps, A.H.; Walker, R.S.; Bell, M.J.; Turpin-Mair, J.S.; Mercante, D.E.; Davidson, J.M. Clinical evaluation of 2 flowable composites. Quintessence Int. 2006, 37, 225–231. [Google Scholar]
- Gallo, J.R.; Burgess, J.O.; Ripps, A.H.; Walker, R.S.; Bell, M.J.; Turpin-Mair, J.S.; Mercante, D.E.; Davidson, J.M. Three-year clinical evaluation of two flowable composites. Quintessence Int. 2010, 41, 497–503. [Google Scholar] [PubMed]
- Ekstrand, K.; Ricketts, D.N.J.; Kidd, E.A.M. Reproducibility and Accuracy of Three Methods for Assessment of Demineralization Depth on the Occlusal Surface: An in vitro Examination. Caries Res. 1997, 31, 224–231. [Google Scholar] [CrossRef]
- Bryant, R.W.; Hodge, K.L.A. Clinical evaluation of posterior composite resin restorations. Aust. Dent. J. 1994, 39, 77–81. [Google Scholar] [CrossRef]
- Dukić, W.; Dukic, O.L.; Milardović, S.; Delija, B. Clinical Evaluation of Indirect Composite Restorations at Baseline and 36 Months After Placement. Oper. Dent. 2010, 35, 156–164. [Google Scholar] [CrossRef][Green Version]
- Dresch, W.; Volpato, S.; Gomes, J.C.; Ribeiro, N.R.; Reis, A.; Loguercio, A.D. Clinical Evaluation of a Nanofilled Composite in Posterior Teeth: 12-month Results. Oper. Dent. 2006, 31, 409–417. [Google Scholar] [CrossRef]
- Simonsen, R.J. From prevention to therapy: Minimal intervention with sealants and resin restorative materials. J. Dent. 2011, 39, S27–S33. [Google Scholar] [CrossRef]
- Strassler, H.E.; Goodman, H.S. A durable flowable composite resin for preventive resin restorations. Dent. Today 2002, 21, 116–121. [Google Scholar] [PubMed]
- Kitasako, Y.; Sadr, A.; Burrow, M.F.; Tagami, J. Thirty six-month clinical evaluation of a highly-filled flowable composite for direct posterior restorations. Aust. Dent. J. 2016, 61, 366–373. [Google Scholar] [CrossRef] [PubMed]
- Savage, B.; McWhorter, A.G.; Kerins, C.A.; Seale, S.N. Preventive resin restorations: Practice and billing patterns of pediatric dentists. Pediatr. Dent. 2009, 31, 210–215. [Google Scholar]
- Banerjee, A.; Frencken, J.E.; Schwendicke, F.; Innes, N.P.T. Contemporary operative caries management: Consensus recommendations on minimally invasive caries removal. Br. Dent. J. 2017, 223, 215–222. [Google Scholar] [CrossRef]
- MacKenzie, L.; Banerjee, A. The Minimally Invasive Management of Early Occlusal Caries: A Practical Guide. Prim. Dent. J. 2014, 3, 34–41. [Google Scholar] [CrossRef] [PubMed]
- Shaalan, O.O.; Abou-Auf, E.; El Zoghby, A.F. Clinical evaluation of flowable resin composite versus conventional resin composite in carious and noncarious lesions: Systematic review and meta-analysis. J. Conserv. Dent. 2017, 20, 380–385. [Google Scholar] [CrossRef]
| Flowable Material/Adhesive System/GROUPS | Composition | Mode of Clinical Application |
|---|---|---|
| Grandio Flow (Voco, Cuxhaven, Germany) Voco Solobond M (Voco, Cuxhaven, Germany) GROUP GF | Inorganic glass ceramic fillers, Bis-GMA, TEGDMA, HEDMA, inorganic filler 80% loading by weight. Bis-GMA, HEMA, BHT, acetone organic acids. | Acid etching 34.5% phosphoric acid (30 s enamel, 15 s dentine), rinsing (20 s), gently air drying (2 s) of dentine leaving it moist, adhesive application Solobond, light blowing (2 s), light curing (20 s), application of resin composite, light cure (40 s). |
| Tetric Evoflow (Vivadent, Schaan, Liechtenstein) Excite (Vivadent, Schaan, Liechtenstein GROUP TF | Bis-GMA, UDMA, Barium glass filler, Ytterbiumtrifluoride, Mixed oxide, Highly dispersed silica, 62% inorganic filler loading by weight. Phosphonic acid acrylate, HEMA, Bis-GMA Dimethacrylate, Highly dispersed silicon dioxide, Ethanol. | Acid etching 37% phosphoric acid (30 s enamel, 15 s dentine), rinsing (20 s), gently air drying of dentine (2 s) leaving it moist, adhesive application Excite, light blowing (2 s), light curing (20 s), application of resin composite, light cure (40 s). |
| Xflow (Dentsply Sirona, York, PA, USA) Prime&Bond NT (Dentsply Sirona, York, PA, USA) GROUP XF | Urethane modified BisGMA-adduct, Bis-GMA and diluents, nanofiller silica, 62% inorganic filler loading by weight. PENTA, UDMA, Resin R5-62-1, T-resin, D-resin, nanofiller, acetone, and cetylaminehydrofluoride. | Acid etching 37% phosphoric acid (30 s enamel, 15 s dentine), rinsing (20 s), gently air drying of dentine (2 s) leaving it moist adhesive application Prime&Bond NT, light blowing (2 s), light curing (20 s), application of resin composite, light cure (40 s). |
| Filtek Supreme XT Flow (3M/Espe, St. Paul, MN, USA) Scotchbond Universal (3M/Espe, St. Paul, MN, USA) GROUP FS | Bis-GMA, TEGDMA, and Bis-EMA, dimethacrylate polymer, silica and zirconia nanofiller, 65% inorganic filler loading by weight. MDP Phosphate Monomer, Dimethacrylate resins, HEMA, silane, Ethanol. | Acid etching 37% phosphoric acid (30 s enamel, 15 s dentine), rinsing (20 s), gently air drying of dentine (2 s) leaving it moist, adhesive application Scotchbond Universal, light blowing (2 s), light curing (20 s), application of resin composite, light cure (40 s). |
| Score/ Criteria | Retention | Color Match | Marginal Discoloration | Marginal Adaptation | Anatomic Form | Surface Texture | Postoperative Sensitivity | Secondary Caries |
|---|---|---|---|---|---|---|---|---|
| A | restoration is present | Excellent match of color and translucency compared to the neighboring tooth tissue, restoration almost invisible | No discoloration | No visible gap or crevice, probe does not catch or penetrate | The restoration is continuous with tooth anatomy, ideal | restoration surface is smooth as the surrounding enamel | no postoperative sensitivity | no caries is present at the margin of the restoration, as evidenced by softness and opacity |
| B | partial loss of retention | Slight mismatch, only visible by close examination | Minor staining, can be polished | Visible gap or crevice, slight catching or penetration of probe | Slightly under or over contoured restoration, no dentin exposed | surface rougher than the surrounding enamel | Slight and mild occasional sensitivity | |
| C | restoration absent | Moderate mismatch in color, shade or translucency | Moderate surface staining, not aesthetically unacceptable | Visible gap or extensive probe penetration between cavity wall and restoration | Restoration is under contoured, dentin or base exposed, restorative material missing, failure | |||
| D | Extensive color mismatch, outside the limits of acceptable appearance | Surface staining present on the restoration, intervention necessary | Loose restoration, secondary caries | constant sensitivity | caries present | |||
| Material | Baseline | 12 Months | 24 Months | 36 Months | p * | p ** |
|---|---|---|---|---|---|---|
| GF | 61(100%) | 57(93.4%) | 50 (81.9%) | 43 (70.5%) | 0.996 | 0.999 |
| TF | 55 (100%) | 53 (96.3%) | 47 (85.5%) | 42 (76.3%) | 0.996 | |
| XF | 57 (100%) | 53 (92.5%) | 48 (84.2%) | 41 (71.9%) | 1.000 | |
| FS | 56 (100%) | 53 (94.6%) | 48 (85.7%) | 42 (75%) | 0.999 | |
| Total | 229 (100%) | 216 (94.3%) | 193 (84.2%) | 168 (73.3%) |
| Measurement | p * | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 12 Months | 24 Months | 36 Months | |||||||
| A | B | A | B | A | B | A | B | C | ||
| GF | n (%) | n (%) | n (%) | n (%) | ||||||
| Retention | 43 (100.0) | 0 (0.0) | 42 (97.7) | 1 (2.3) | 42 (97.7) | 1 (2.3) | 41 (95.3) | 1 (2.3) | 1 (2.3) | 0.750 |
| Color match | 35 (81.4) | 8 (18.6) | 35 (81.4) | 8 (18.6) | 35 (81.4) | 8 (18.6) | 34 (79.1) | 8 (18.6) | 1 (2.3) | 1.000 |
| Marginal discoloration | 41 (95.3) | 2 (4.7) | 41 (95.3) | 2 (4.7) | 41 (95.3) | 2 (4.7) | 40 (93.0) | 2 (4.7) | 1 (2.3) | 1.000 |
| Marginal adaptation | 43 (100.0) | 0 (0.0) | 41 (95.3) | 2 (4.7) | 41 (95.3) | 2 (4.7) | 40 (93.0) | 3 (7.0) | 0 (0.0) | 0.188 |
| Caries | 43 (100.0) | 0 (0.0) | 43 (100.0) | 0 (0.0) | 43 (100.0) | 0 (0.0) | 43 (100.0) | 0 (0.0) | 0 (0.0) | 1.000 |
| Surface texture | 43 (100.0) | 0 (0.0) | 43 (100.0) | 0 (0.0) | 43 (100.0) | 0 (0.0) | 42 (97.7) | 1 (2.3) | 0 (0.0) | 1.000 |
| Anatomic form | 43 (100.0) | 0 (0.0) | 43 (100.0) | 0 (0.0) | 43 (100.0) | 0 (0.0) | 43 (100.0) | 0 (0.0) | 0 (0.0) | 1.000 |
| Postoperative sensitivity | 39 (90.7) | 4 (9.3) | 41 (95.3) | 2 (4.7) | 43 (100.0) | 0 (0.0) | 43 (100.0) | 0 (0.0) | 0 (0.0) | 0.021 * |
| TF | n (%) | n (%) | n (%) | n (%) | ||||||
| Retention | 42 (100.0) | 0 (0.0) | 41 (97.6) | 1 (2.4) | 39 (92.9) | 3 (7.1) | 37 (88.1) | 4 (9.5) | 1 (2.4) | 0.010 * |
| Color match | 36 (85.7) | 6 (14.3) | 36 (85.7) | 6 (14.3) | 36 (85.7) | 6 (14.3) | 32 (76.2) | 6 (14.3) | 4 (9.5) | 0.004 * |
| Marginal discoloration | 42 (100.0) | 0 (0.0) | 41 (97.6) | 1 (2.4) | 39 (92.9) | 3 (7.1) | 38 (90.5) | 4 (9.5) | 0 (0.0) | 0.042 * |
| Marginal adaptation | 42 (100.0) | 0 (0.0) | 42 (100.0) | 0 (0.0) | 41 (97.6) | 1 (2.4) | 40 (95.2) | 2 (4.8) | 0 (0.0) | 0.500 |
| Caries | 42 (100.0) | 0 (0.0) | 42 (100.0) | 0 (0.0) | 42 (100.0) | 0 (0.0) | 42 (100.0) | 0 (0.0) | 0 (0.0) | 1.000 |
| Surface texture | 42 (100.0) | 0 (0.0) | 42 (100.0) | 0 (0.0) | 42 (100.0) | 0 (0.0) | 42 (100.0) | 0 (0.0) | 0 (0.0) | 1.000 |
| Anatomic form | 42 (100.0) | 0 (0.0) | 42 (100.0) | 0 (0.0) | 42 (100.0) | 0 (0.0) | 42 (100.0) | 0 (0.0) | 0 (0.0) | 1.000 |
| Postoperative sensitivity | 39 (92.9) | 3 (7.1) | 40 (95.2) | 2 (4.8) | 39 (92.9) | 3 (7.1) | 39 (92.9) | 3 (7.1) | 0 (0.0) | 1.000 |
| XF | n (%) | n (%) | n (%) | n (%) | ||||||
| Retention | 41 (100.0) | 0 (0.0) | 41 (100.0) | 0 (0.0) | 41 (100.0) | 0 (0.0) | 40 (97.6) | 1 (2.4) | 0 (0.0) | 1.000 |
| Color match | 36 (87.8) | 5 (12.2) | 36 (87.8) | 5 (12.2) | 36 (87.8) | 5 (12.2) | 36 (87.8) | 5 (12.2) | 0 (0.0) | 1.000 |
| Marginal discoloration | 41 (100.0) | 0 (0.0) | 41 (100.0) | 0 (0.0) | 39 (95.1) | 2 (4.9) | 39 (95.1) | 2 (4.9) | 0 (0.0) | 0.167 |
| Marginal adaptation | 41 (100.0) | 0 (0.0) | 41 (100.0) | 0 (0.0) | 41 (100.0) | 0 (0.0) | 40 (97.6) | 1 (2.4) | 0 (0.0) | 1.000 |
| Caries | 41 (100.0) | 0 (0.0) | 41 (100.0) | 0 (0.0) | 41 (100.0) | 0 (0.0) | 41 (100.0) | 0 (0.0) | 0 (0.0) | 1.000 |
| Surface texture | 41 (100.0) | 0 (0.0) | 41 (100.0) | 0 (0.0) | 41 (100.0) | 0 (0.0) | 40 (97.6) | 1 (2.4) | 0 (0.0) | 1.000 |
| Anatomic form | 41 (100.0) | 0 (0.0) | 41 (100.0) | 0 (0.0) | 41 (100.0) | 0 (0.0) | 41 (100.0) | 0 (0.0) | 0 (0.0) | 1.000 |
| Postoperative sensitivity | 39 (95.1) | 2 (4.9) | 39 (95.1) | 2 (4.9) | 39 (95.1) | 2 (4.9) | 39 (95.1) | 2 (4.9) | 0 (0.0) | 1.000 |
| FS | n (%) | n (%) | n (%) | n (%) | ||||||
| Retention | 42 (100.0) | 0 (0.0) | 40 (95.2) | 2 (4.8) | 38 (90.5) | 4 (9.5) | 37 (88.1) | 4 (9.5) | 1 (2.4) | 0.010 * |
| Color match | 35 (83.3) | 7 (16.7) | 35 (83.3) | 7 (16.7) | 35 (83.3) | 7 (16.7) | 34 (81.0) | 7 (16.7) | 1 (2.4) | 1.000 |
| Marginal discoloration | 40 (95.2) | 2 (4.8) | 40 (95.2) | 2 (4.8) | 40 (95.2) | 2 (4.8) | 39 (92.9) | 3 (7.1) | 0 (0.0) | 1.000 |
| Marginal adaptation | 42 (100.0) | 0 (0.0) | 36 (85.7) | 6 (14.3) | 35 (83.3) | 7 (16.7) | 35 (83.3) | 7 (16.7) | 0 (0.0) | <0.001 * |
| Caries | 42 (100.0) | 0 (0.0) | 42 (100.0) | 0 (0.0) | 42 (100.0) | 0 (0.0) | 42 (100.0) | 0 (0.0) | 0 (0.0) | 1.000 |
| Surface texture | 42 (100.0) | 0 (0.0) | 42 (100.0) | 0 (0.0) | 42 (100.0) | 0 (0.0) | 42 (100.0) | 0 (0.0) | 0 (0.0) | 1.000 |
| Anatomic form | 42 (100.0) | 0 (0.0) | 42 (100.0) | 0 (0.0) | 42 (100.0) | 0 (0.0) | 42 (100.0) | 0 (0.0) | 0 (0.0) | 1.000 |
| Postoperative sensitivity | 39 (92.9) | 3 (7.1) | 40 (95.2) | 2 (4.8) | 42 (100.0) | 0 (0.0) | 42 (100.0) | 0 (0.0) | 0 (0.0) | 0.083 |
| Material | GF | TF | XF | FS | |||||
|---|---|---|---|---|---|---|---|---|---|
| Tooth Location | Mean Rank | p * | Mean Rank | p * | Mean Rank | p * | Mean Rank | p * | |
| Retention: 36 months—Baseline | maxilla | 21.85 | 0.785 | 23.04 | 0.065 | 21.39 | 0.376 | 22.62 | 0.386 |
| mandible | 22.24 | 19.00 | 20.50 | 20.74 | |||||
| Color Match: 36 months—Baseline | maxilla | 22.33 | 0.419 | 20.60 | 0.279 | 21.00 | 1.000 | 21.00 | 0.410 |
| mandible | 21.50 | 22.97 | 21.00 | 21.84 | |||||
| Marginal discoloration: 36 months—Baseline | maxilla | 22.33 | 0.419 | 22.73 | 0.103 | 20.89 | 0.860 | 21.00 | 0.410 |
| mandible | 21.50 | 19.50 | 21.14 | 21.84 | |||||
| Marginal adaptation: 36 months—Baseline | maxilla | 22.15 | 0.822 | 22.12 | 0.261 | 20.50 | 0.258 | 20.47 | 0.487 |
| mandible | 21.76 | 20.50 | 21.64 | 22.20 | |||||
| Caries: 36 months—baseline | maxilla | 22.00 | 1.000 | 21.50 | 1.000 | 21.00 | 1.000 | 21.50 | 1.000 |
| mandible | 22.00 | 21.50 | 21.00 | 21.50 | |||||
| Surface texture: 36 months—Baseline | maxilla | 22.33 | 0.419 | 21.50 | 1.000 | 20.50 | 0.258 | 21.50 | 1.000 |
| mandible | 21.50 | 21.50 | 21.64 | 21.50 | |||||
| Anatomic form: 36 months—Baseline | maxilla | 22.00 | 1.000 | 21.50 | 1.000 | 21.00 | 1.000 | 21.50 | 1.000 |
| mandible | 22.00 | 21.50 | 21.00 | 21.50 | |||||
| Postoperative sensitivity: 36 months—Baseline | maxilla | 21.52 | 0.537 | 21.50 | 1.000 | 21.00 | 1.000 | 20.53 | 0.343 |
| mandible | 22.74 | 21.50 | 21.00 | 22.16 | |||||
| Material | GF | TF | XF | FS | |||||
|---|---|---|---|---|---|---|---|---|---|
| Tooth | Mean Rank | p * | Mean Rank | p * | Mean Rank | p * | Mean Rank | p * | |
| Retention: 36 months—Baseline | 1st molar | 22.00 | 1.000 | 22.25 | 0.369 | 21.26 | 0.471 | 22.13 | 0.427 |
| 2nd molar | 22.00 | 20.28 | 20.50 | 20.37 | |||||
| Color match: 36 months—Baseline | 1st molar | 22.48 | 0.329 | 21.35 | 0.854 | 21.00 | 1.000 | 21.78 | 0.456 |
| 2nd molar | 21.50 | 21.75 | 21.00 | 21.00 | |||||
| Marginal discoloration: 36 months—Baseline | 1st molar | 21.50 | 0.306 | 21.12 | 0.611 | 21.52 | 0.302 | 21.00 | 0.180 |
| 2nd molar | 22.52 | 22.13 | 20.00 | 22.40 | |||||
| Marginal adaptation: 36 months—Baseline | 1st molar | 23.43 | 0.083 | 21.31 | 0.726 | 21.26 | 0.471 | 19.56 | 0.033 * |
| 2nd molar | 20.50 | 21.81 | 20.50 | 25.00 | |||||
| Caries: 36 months—Baseline | 1st molar | 22.00 | 1.000 | 21.50 | 1.000 | 21.00 | 1.000 | 21.50 | 1.000 |
| 2nd molar | 22.00 | 21.50 | 21.00 | 21.50 | |||||
| Surface texture: 36 months—Baseline | 1st molar | 21.50 | 0.306 | 21.50 | 1.000 | 21.26 | 0.471 | 21.50 | 1.000 |
| 2nd molar | 22.52 | 21.50 | 20.50 | 21.50 | |||||
| Anatomic form: 36 months—Baseline | 1st molar | 22.00 | 1.000 | 21.50 | 1.000 | 21.00 | 1.000 | 21.50 | 1.000 |
| 2nd molar | 22.00 | 21.50 | 21.00 | 21.50 | |||||
| Postoperative sensitivity: 36 months—Baseline | 1st molar | 21.07 | 0.322 | 21.50 | 1.000 | 21.00 | 1.000 | 20.67 | 0.186 |
| 2nd molar | 22.98 | 21.50 | 21.00 | 23.00 | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dukić, W.; Majić, M.; Prica, N.; Oreški, I. Clinical Evaluation of Flowable Composite Materials in Permanent Molars Small Class I Restorations: 3-Year Double Blind Clinical Study. Materials 2021, 14, 4283. https://doi.org/10.3390/ma14154283
Dukić W, Majić M, Prica N, Oreški I. Clinical Evaluation of Flowable Composite Materials in Permanent Molars Small Class I Restorations: 3-Year Double Blind Clinical Study. Materials. 2021; 14(15):4283. https://doi.org/10.3390/ma14154283
Chicago/Turabian StyleDukić, Walter, Mia Majić, Natalija Prica, and Ivan Oreški. 2021. "Clinical Evaluation of Flowable Composite Materials in Permanent Molars Small Class I Restorations: 3-Year Double Blind Clinical Study" Materials 14, no. 15: 4283. https://doi.org/10.3390/ma14154283
APA StyleDukić, W., Majić, M., Prica, N., & Oreški, I. (2021). Clinical Evaluation of Flowable Composite Materials in Permanent Molars Small Class I Restorations: 3-Year Double Blind Clinical Study. Materials, 14(15), 4283. https://doi.org/10.3390/ma14154283






