The Impact of Dental Implant Length on Failure Rates: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Objective
2.2. Search Strategies
2.3. Inclusion and Exclusion Criteria
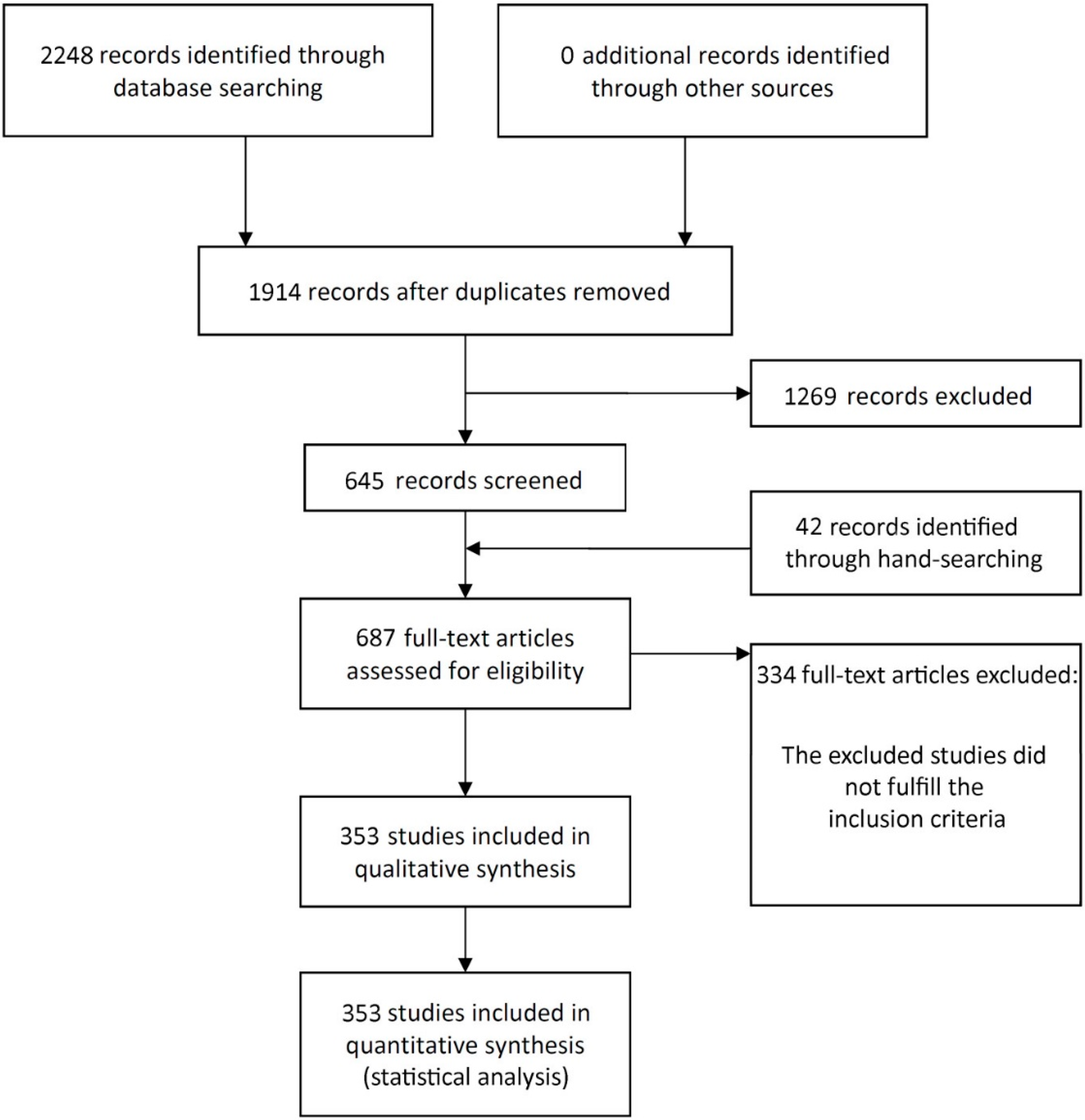
2.4. Study Selection
2.5. Quality Assessment
2.6. Data Extraction
2.7. Analyses
3. Results
3.1. Literature Search
3.2. Description of the Studies
3.3. Quality Assessment
3.4. Meta-Analyses
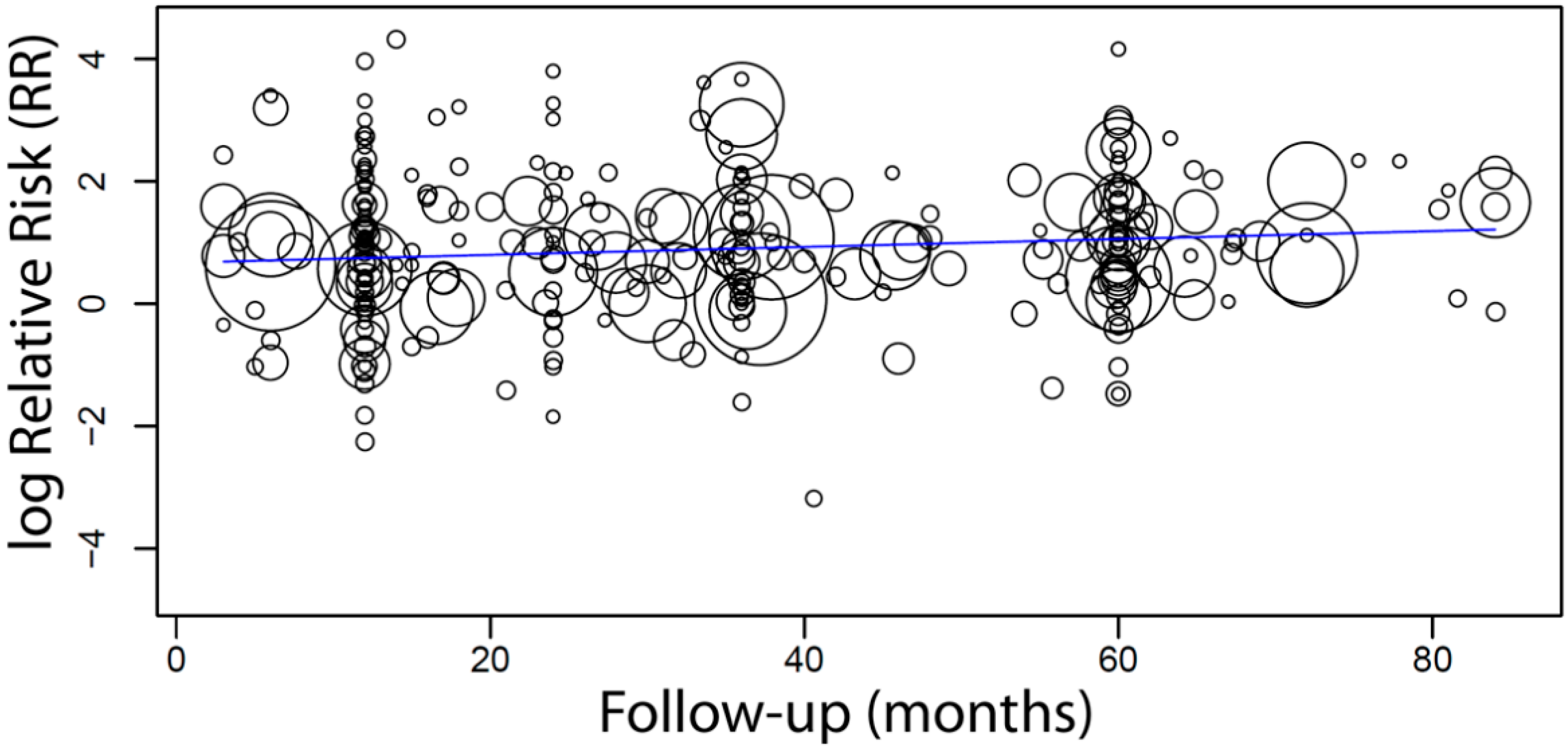
3.5. Meta-Regression
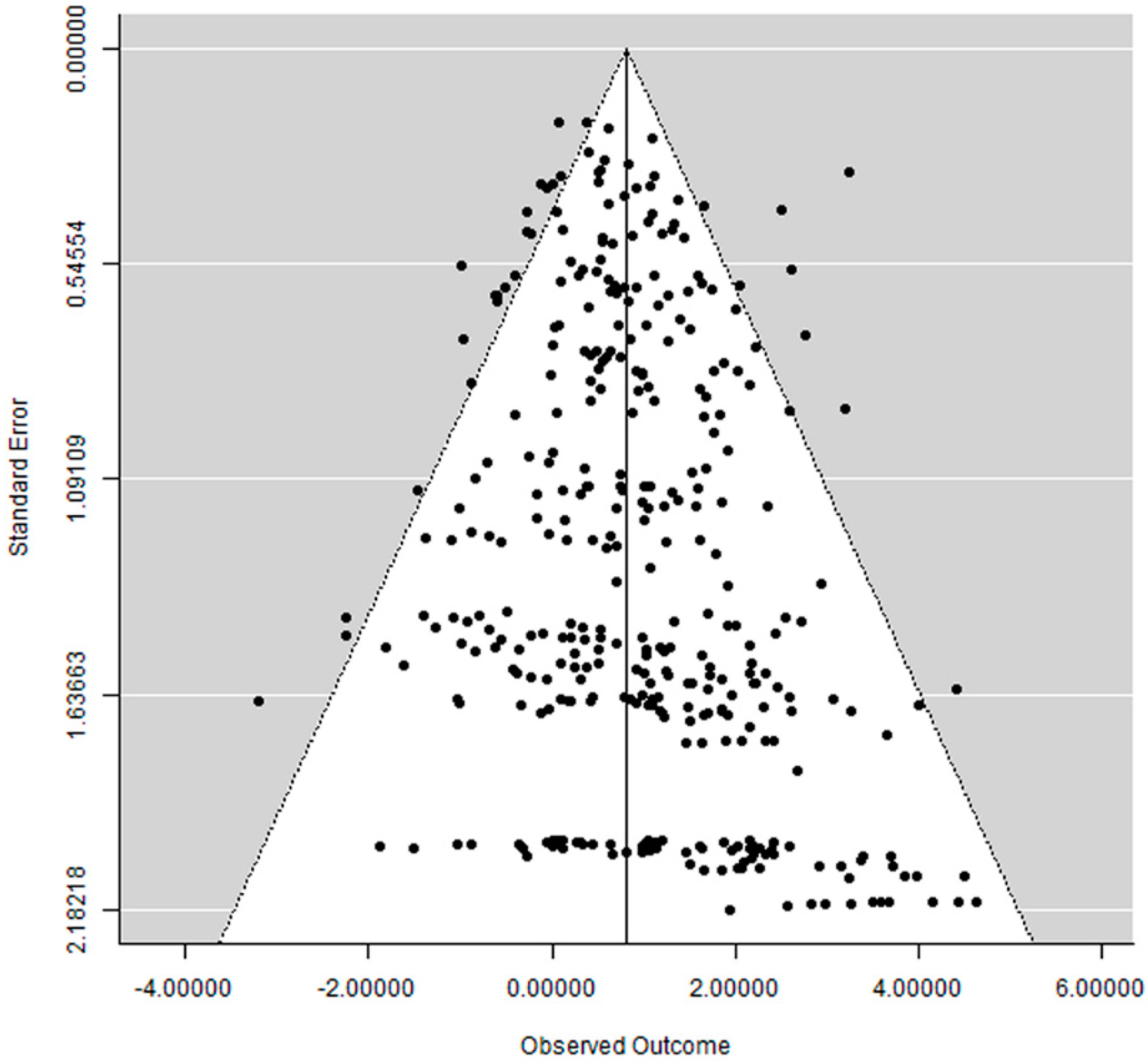
3.6. Publication Bias
4. Discussion
Limitations of the Present Study
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Schropp, L.; Wenzel, A.; Kostopoulos, L.; Karring, T. Bone healing and soft tissue contour changes following single-tooth extraction: A clinical and radiographic 12-month prospective study. Int. J. Periodontics Restor. Dent. 2003, 23, 313–323. [Google Scholar]
- Amato, F.; Polara, G.; Spedicato, G.A. Immediate Loading of Fixed Partial Dental Prostheses on Extra-Short and Short Implants in Patients with Severe Atrophy of the Posterior Maxilla or Mandible: An Up-to-4-year Clinical Study. Int. J. Oral Maxillofac. Implant. 2020, 35, 607–615. [Google Scholar] [CrossRef]
- Chrcanovic, B.R.; Albrektsson, T.; Wennerberg, A. Survival and Complications of Zygomatic Implants: An Updated Systematic Review. J. Oral Maxillofac. Surg. 2016, 74, 1949–1964. [Google Scholar] [CrossRef] [Green Version]
- Nedir, R.; Bischof, M.; Briaux, J.M.; Beyer, S.; Szmukler-Moncler, S.; Bernard, J.P. A 7-year life table analysis from a prospective study on ITI implants with special emphasis on the use of short implants. Results from a private practice. Clin. Oral Implant. Res. 2004, 15, 150–157. [Google Scholar] [CrossRef] [PubMed]
- Raghoebar, G.M.; Timmenga, N.M.; Reintsema, H.; Stegenga, B.; Vissink, A. Maxillary bone grafting for insertion of endosseous implants: Results after 12–124 months. Clin. Oral Implant. Res. 2001, 12, 279–286. [Google Scholar] [CrossRef]
- Chrcanovic, B.R.; Custodio, A.L. Inferior alveolar nerve lateral transposition. Oral Maxillofac. Surg. 2009, 13, 213–219. [Google Scholar] [CrossRef]
- Thoma, D.S.; Zeltner, M.; Hüsler, J.; Hämmerle, C.H.; Jung, R.E. EAO Supplement Working Group 4—EAO CC 2015 Short implants versus sinus lifting with longer implants to restore the posterior maxilla: A systematic review. Clin. Oral Implant. Res. 2015, 26 (Suppl. S11), 154–169. [Google Scholar] [CrossRef]
- Kotsovilis, S.; Fourmousis, I.; Karoussis, I.K.; Bamia, C. A systematic review and meta-analysis on the effect of implant length on the survival of rough-surface dental implants. J. Periodontol. 2009, 80, 1700–1718. [Google Scholar] [CrossRef]
- Ravida, A.; Wang, I.C.; Barootchi, S.; Askar, H.; Tavelli, L.; Gargallo-Albiol, J.; Wang, H.L. Meta-analysis of randomized clinical trials comparing clinical and patient-reported outcomes between extra-short (</=6 mm) and longer (>/=10 mm) implants. J. Clin. Periodontol. 2019, 46, 118–142. [Google Scholar] [CrossRef]
- Lemos, C.A.; Ferro-Alves, M.L.; Okamoto, R.; Mendonça, M.R.; Pellizzer, E.P. Short dental implants versus standard dental implants placed in the posterior jaws: A systematic review and meta-analysis. J. Dent. 2016, 47, 8–17. [Google Scholar] [CrossRef] [Green Version]
- Papaspyridakos, P.; De Souza, A.; Vazouras, K.; Gholami, H.; Pagni, S.; Weber, H.P. Survival rates of short dental implants (</=6 mm) compared with implants longer than 6 mm in posterior jaw areas: A meta-analysis. Clin. Oral Implant. Res. 2018, 29 (Suppl. S16), 8–20. [Google Scholar] [CrossRef]
- Chrcanovic, B.R.; Kisch, J.; Albrektsson, T.; Wennerberg, A. Factors Influencing Early Dental Implant Failures. J. Dent. Res. 2016, 95, 995–1002. [Google Scholar] [CrossRef] [PubMed]
- Chrcanovic, B.R.; Kisch, J.; Albrektsson, T.; Wennerberg, A. A retrospective study on clinical and radiological outcomes of oral implants in patients followed up for a minimum of 20 years. Clin. Implant Dent. Relat. Res. 2018, 20, 199–207. [Google Scholar] [CrossRef]
- NIH. Quality Assessment Tool for Case Series Studies. Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed on 15 January 2020).
- DerSimonian, R.; Laird, N. Meta-analysis in clinical trials. Control. Clin. Trials 1986, 7, 177–188. [Google Scholar] [CrossRef]
- Wallace, B.C.; Dahabreh, I.J.; Trikalinos, T.A.; Lau, J.; Trow, P.; Schmid, C.H. Closing the Gap between Methodologists and End-Users: R as a Computational Back-End. J. Stat. Softw. 2012, 49, 1–15. [Google Scholar] [CrossRef] [Green Version]
- Wallace, B.C.; Lajeunesse, M.J.; Dietz, G.; Dahabreh, I.J.; Trikalinos, T.A.; Schmid, C.H.; Gurevitch, J. OpenMEE: Intuitive, open-source software for meta-analysis in ecology and evolutionary biology. Methods Ecol. Evol. 2017, 8, 941–947. [Google Scholar] [CrossRef] [Green Version]
- Tan, W.L.; Wong, T.L.; Wong, M.C.; Lang, N.P. A systematic review of post-extractional alveolar hard and soft tissue dimensional changes in humans. Clin. Oral Implant. Res. 2012, 23 (Suppl. S5), 1–21. [Google Scholar] [CrossRef] [PubMed]
- Zhao, K.; Wang, F.; Huang, W.; Wu, Y. Clinical Outcomes of Vertical Distraction Osteogenesis for Dental Implantation: A Systematic Review and Meta-Analysis. Int. J. Oral Maxillofac. Implant. 2018, 33, 549–564. [Google Scholar] [CrossRef]
- Tonetti, M.S.; Hämmerle, C.H. Advances in bone augmentation to enable dental implant placement: Consensus Report of the Sixth European Workshop on Periodontology. J. Clin. Periodontol. 2008, 35, 168–172. [Google Scholar] [CrossRef] [Green Version]
- Chrcanovic, B.R.; Albrektsson, T.; Wennerberg, A. Bone Quality and Quantity and Dental Implant Failure: A Systematic Review and Meta-analysis. Int. J. Prosthodont. 2017, 30, 219–237. [Google Scholar] [CrossRef] [PubMed]
- Koc, D.; Dogan, A.; Bek, B. Bite force and influential factors on bite force measurements: A literature review. Eur. J. Dent. 2010, 4, 223–232. [Google Scholar] [CrossRef] [Green Version]
- De Santis, D.; Cucchi, A.; Longhi, C.; Vincenzo, B. Short threaded implants with an oxidized surface to restore posterior teeth: 1- to 3-year results of a prospective study. Int. J. Oral Maxillofac. Implant. 2011, 26, 393–403. [Google Scholar]
- Pieri, F.; Aldini, N.N.; Fini, M.; Marchetti, C.; Corinaldesi, G. Preliminary 2-year report on treatment outcomes for 6-mm-long implants in posterior atrophic mandibles. Int. J. Prosthodont. 2012, 25, 279–289. [Google Scholar] [PubMed]
- Anitua, E.; Alkhraist, M.H.; Pinas, L.; Begona, L.; Orive, G. Implant survival and crestal bone loss around extra-short implants supporting a fixed denture: The effect of crown height space, crown-to-implant ratio, and offset placement of the prosthesis. Int. J. Oral Maxillofac. Implant. 2014, 29, 682–689. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blanes, R.J. To what extent does the crown-implant ratio affect the survival and complications of implant-supported reconstructions? A systematic review. Clin. Oral Implant. Res. 2009, 20 (Suppl. S4), 67–72. [Google Scholar] [CrossRef]
- Verri, F.R.; Batista, V.E.; Santiago, J.F., Jr.; Almeida, D.A.; Pellizzer, E.P. Effect of crown-to-implant ratio on peri-implant stress: A finite element analysis. Mater. Sci. Eng. C Mater. Biol. Appl. 2014, 45, 234–240. [Google Scholar] [CrossRef]
- Verri, F.R.; Junior, J.F.S.; de Faria Almeida, D.A.; de Oliveira, G.B.; de Souza Batista, V.E.; Honório, H.M.; Noritomi, P.Y.; Pellizzer, E.P. Biomechanical influence of crown-to-implant ratio on stress distribution over internal hexagon short implant: 3-D finite element analysis with statistical test. J. Biomech. 2015, 48, 138–145. [Google Scholar] [CrossRef] [PubMed]
- Sotto-Maior, B.S.; Senna, P.M.; da Silva-Neto, J.P.; de Arruda Nóbilo, M.A.; Del Bel Cury, A.A. Influence of crown-to-implant ratio on stress around single short-wide implants: A photoelastic stress analysis. J. Prosthodont. 2015, 24, 52–56. [Google Scholar] [CrossRef]
- Quaranta, A.; Piemontese, M.; Rappelli, G.; Sammartino, G.; Procaccini, M. Technical and biological complications related to crown to implant ratio: A systematic review. Implant Dent. 2014, 23, 180–187. [Google Scholar] [CrossRef]
- Telleman, G.; Raghoebar, G.M.; Vissink, A.; den Hartog, L.; Huddleston Slater, J.J.; Meijer, H.J. A systematic review of the prognosis of short (<10 mm) dental implants placed in the partially edentulous patient. J. Clin. Periodontol. 2011, 38, 667–676. [Google Scholar] [CrossRef]
- Chrcanovic, B.R.; Albrektsson, T.; Wennerberg, A. Smoking and dental implants: A systematic review and meta-analysis. J. Dent. 2015, 43, 487–498. [Google Scholar] [CrossRef]
- Alsaadi, G.; Quirynen, M.; Komarek, A.; van Steenberghe, D. Impact of local and systemic factors on the incidence of oral implant failures, up to abutment connection. J. Clin. Periodontol. 2007, 34, 610–617. [Google Scholar] [CrossRef]
- Chrcanovic, B.R.; Albrektsson, T.; Wennerberg, A. Periodontally compromised vs. periodontally healthy patients and dental implants: A systematic review and meta-analysis. J. Dent. 2014, 42, 1509–1527. [Google Scholar] [CrossRef] [PubMed]
- Chrcanovic, B.R.; Albrektsson, T.; Wennerberg, A. Dental implants in irradiated versus nonirradiated patients: A meta-analysis. Head Neck 2016, 38, 448–481. [Google Scholar] [CrossRef] [PubMed]
- Chrcanovic, B.R.; Albrektsson, T.; Wennerberg, A. Dental implants inserted in fresh extraction sockets versus healed sites: A systematic review and meta-analysis. J. Dent. 2015, 43, 16–41. [Google Scholar] [CrossRef]
- Chrcanovic, B.R.; Kisch, J.; Albrektsson, T.; Wennerberg, A. Is the intake of selective serotonin reuptake inhibitors associated with an increased risk of dental implant failure? Int. J. Oral Maxillofac. Surg. 2017, 46, 782–788. [Google Scholar] [CrossRef]
- Chrcanovic, B.R.; Kisch, J.; Albrektsson, T.; Wennerberg, A. Intake of Proton Pump Inhibitors Is Associated with an Increased Risk of Dental Implant Failure. Int. J. Oral Maxillofac. Implant. 2017, 32, 1097–1102. [Google Scholar] [CrossRef] [Green Version]
- Chrcanovic, B.R.; Albrektsson, T.; Wennerberg, A. Bruxism and Dental Implants: A Meta-Analysis. Implant Dent. 2015, 24, 505–516. [Google Scholar] [CrossRef]
- Chrcanovic, B.R.; Kisch, J.; Albrektsson, T.; Wennerberg, A. Bruxism and dental implant failures: A multilevel mixed effects parametric survival analysis approach. J. Oral Rehabil. 2016, 43, 813–823. [Google Scholar] [CrossRef]
- Chrcanovic, B.R.; Kisch, J.; Albrektsson, T.; Wennerberg, A. Bruxism and dental implant treatment complications: A retrospective comparative study of 98 bruxer patients and a matched group. Clin. Oral Implant. Res. 2017, 28, e1–e9. [Google Scholar] [CrossRef]
- Chrcanovic, B.R.; Albrektsson, T.; Wennerberg, A. Diabetes and oral implant failure: A systematic review. J. Dent. Res. 2014, 93, 859–867. [Google Scholar] [CrossRef] [PubMed]
- Chrcanovic, B.R.; Kisch, J.; Albrektsson, T.; Wennerberg, A. Impact of Different Surgeons on Dental Implant Failure. Int. J. Prosthodont. 2017, 30, 445–454. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chrcanovic, B.R.; Kisch, J.; Albrektsson, T.; Wennerberg, A. Analysis of risk factors for cluster behavior of dental implant failures. Clin. Implant Dent. Relat. Res. 2017, 19, 632–642. [Google Scholar] [CrossRef]
- Klokkevold, P.R.; Han, T.J. How do smoking, diabetes, and periodontitis affect outcomes of implant treatment? Int. J. Oral Maxillofac. Implant. 2007, 22, 173–202. [Google Scholar]
| Length Group (mm) | Studies (n) | Failure/Total of Implants | Probability of Failure * (95% CI), SE, p Value | Heterogeneity |
|---|---|---|---|---|
| 4–6.5 | 72 | 108/2549 | 4.6% (3.3, 6.0), 0.7%, p < 0.001 | τ2 = 0001, Chi2 = 157.702, I2 = 54.98%, p < 0.001 |
| 7–9.5 | 307 | 573/11,940 | 3.8% (3.3, 4.3), 0.3%, p < 0.001 | τ2 = 0.000, Chi2 = 646.944, I2 = 52.70%, p < 0.001 |
| 10–12 | 316 | 1588/47,196 | 2.7% (2.4, 2.9), 0.1%, p < 0.001 | τ2 = 0.000, Chi2 = 1273.409, I2 = 75.26%, p < 0.001 |
| 13–15 | 225 | 1312/40,033 | 2.5% (2.2, 2.8), 0.2%, p < 0.001 | τ2 = 0.000, Chi2 = 970.310, I2 = 76.92%, p < 0.001 |
| 16–20 | 119 | 212/8486 | 1.8% (1.4, 2.1), 0.2%, p < 0.001 | τ2 = 0.000, Chi2 = 136.446, I2 = 13.52%, p = 0.118 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abdel-Halim, M.; Issa, D.; Chrcanovic, B.R. The Impact of Dental Implant Length on Failure Rates: A Systematic Review and Meta-Analysis. Materials 2021, 14, 3972. https://doi.org/10.3390/ma14143972
Abdel-Halim M, Issa D, Chrcanovic BR. The Impact of Dental Implant Length on Failure Rates: A Systematic Review and Meta-Analysis. Materials. 2021; 14(14):3972. https://doi.org/10.3390/ma14143972
Chicago/Turabian StyleAbdel-Halim, Maha, Dalia Issa, and Bruno Ramos Chrcanovic. 2021. "The Impact of Dental Implant Length on Failure Rates: A Systematic Review and Meta-Analysis" Materials 14, no. 14: 3972. https://doi.org/10.3390/ma14143972
APA StyleAbdel-Halim, M., Issa, D., & Chrcanovic, B. R. (2021). The Impact of Dental Implant Length on Failure Rates: A Systematic Review and Meta-Analysis. Materials, 14(14), 3972. https://doi.org/10.3390/ma14143972






