Immediate Post-Extraction Short Implant Placement with Immediate Loading and without Extraction of an Impacted Maxillary Canine: Two Case Reports
Abstract
1. Introduction
2. Case Reports
2.1. Clinical Presentation
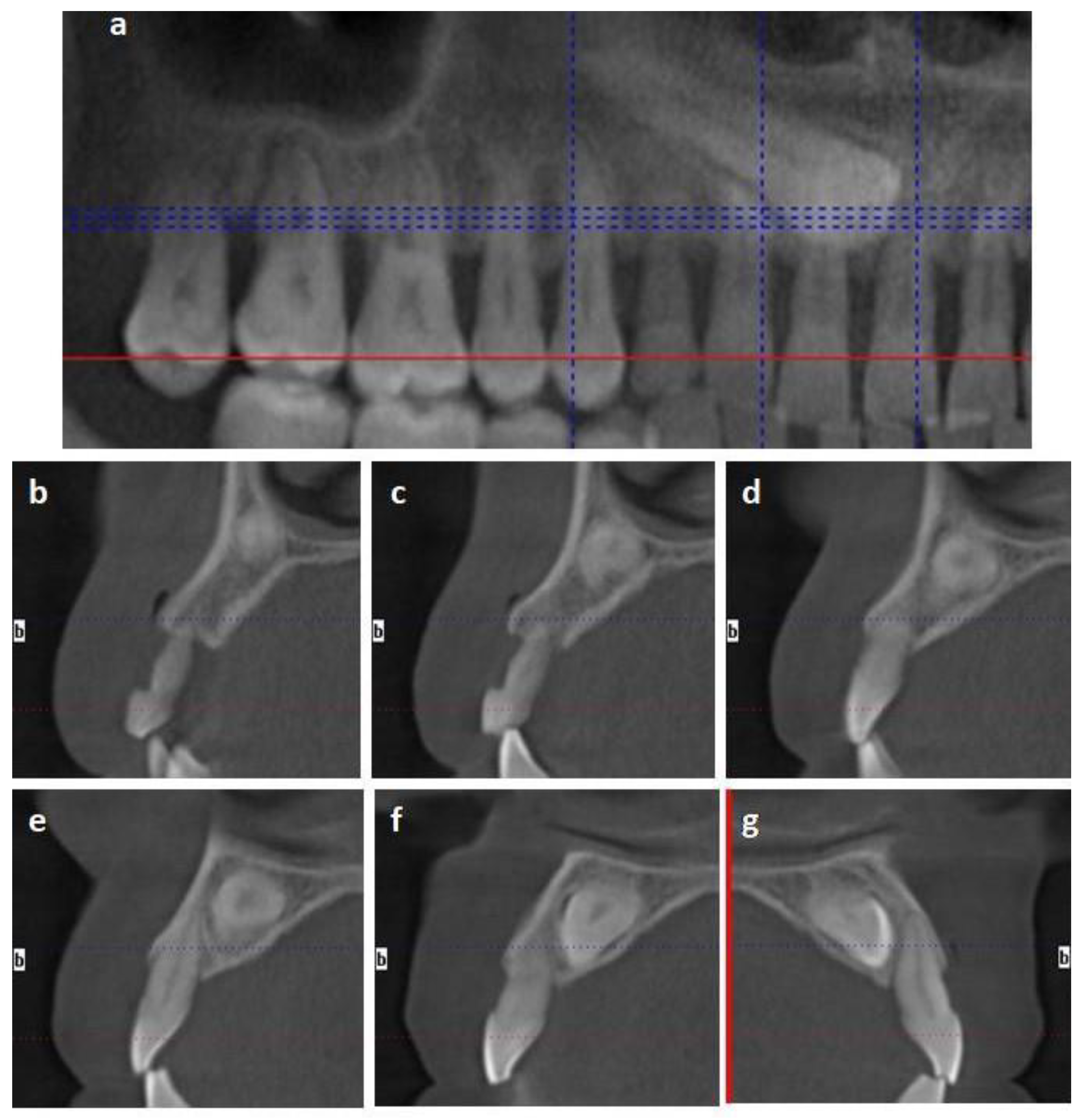
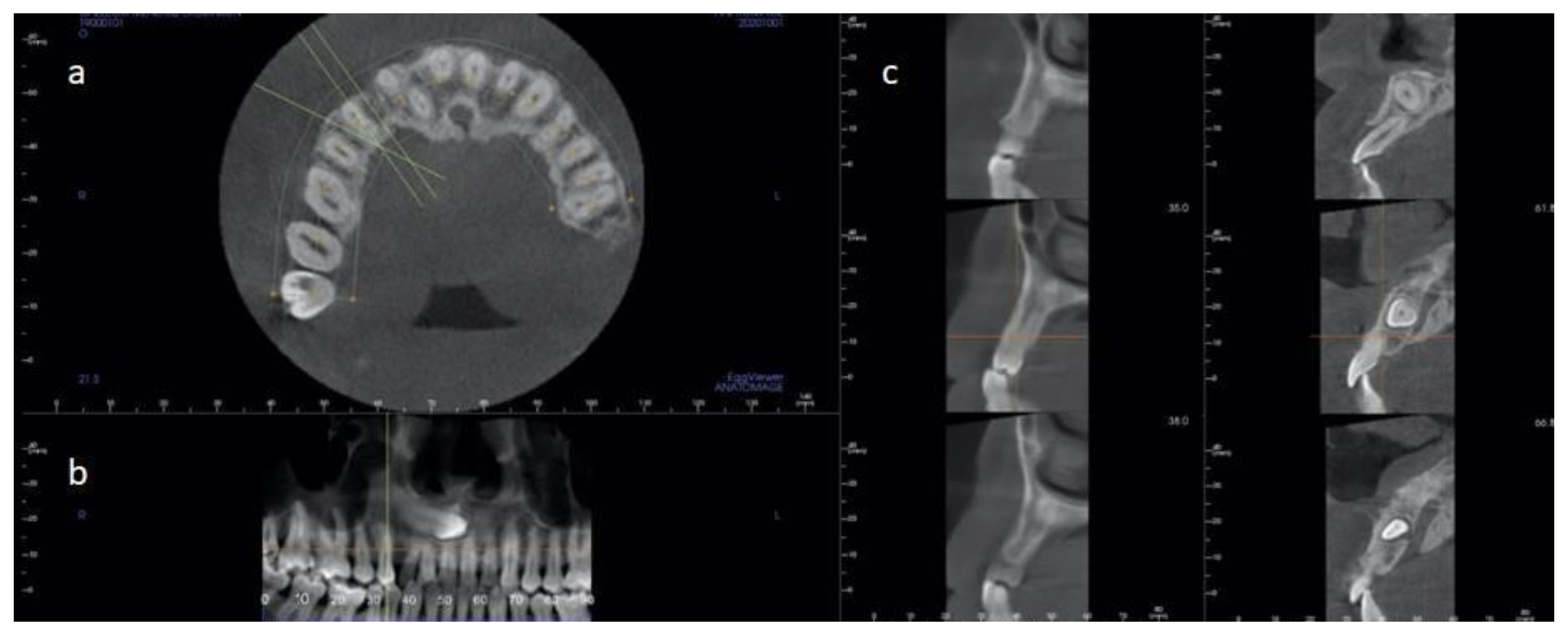
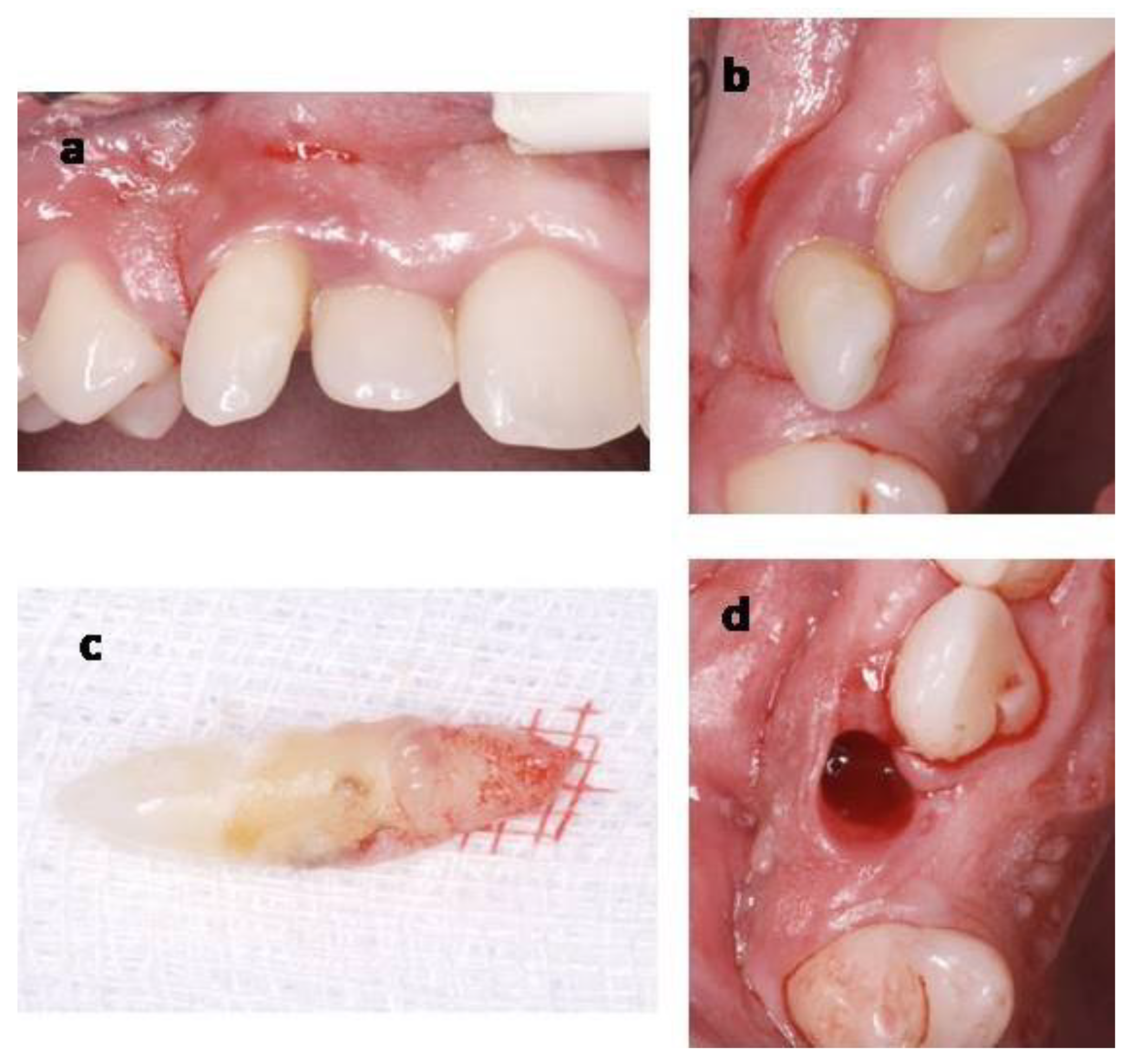
2.1.1. Case 1
2.1.2. Case 2
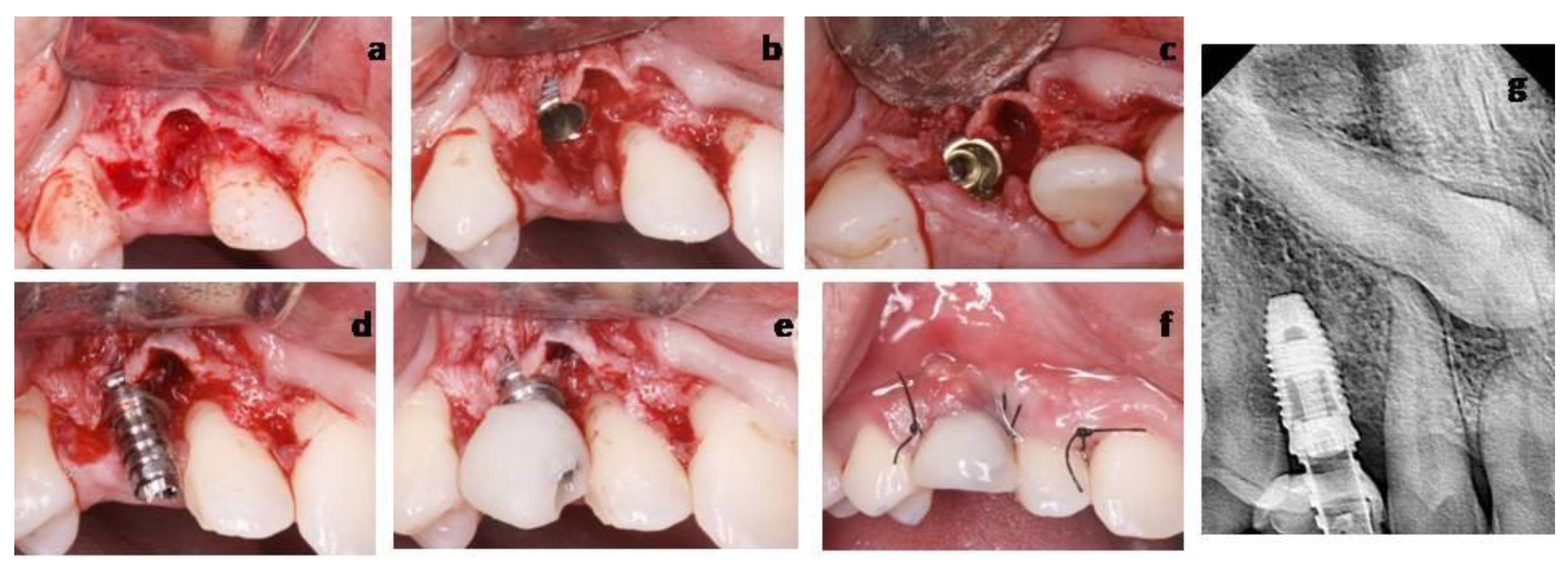
2.2. Clinical Procedures and Outcomes
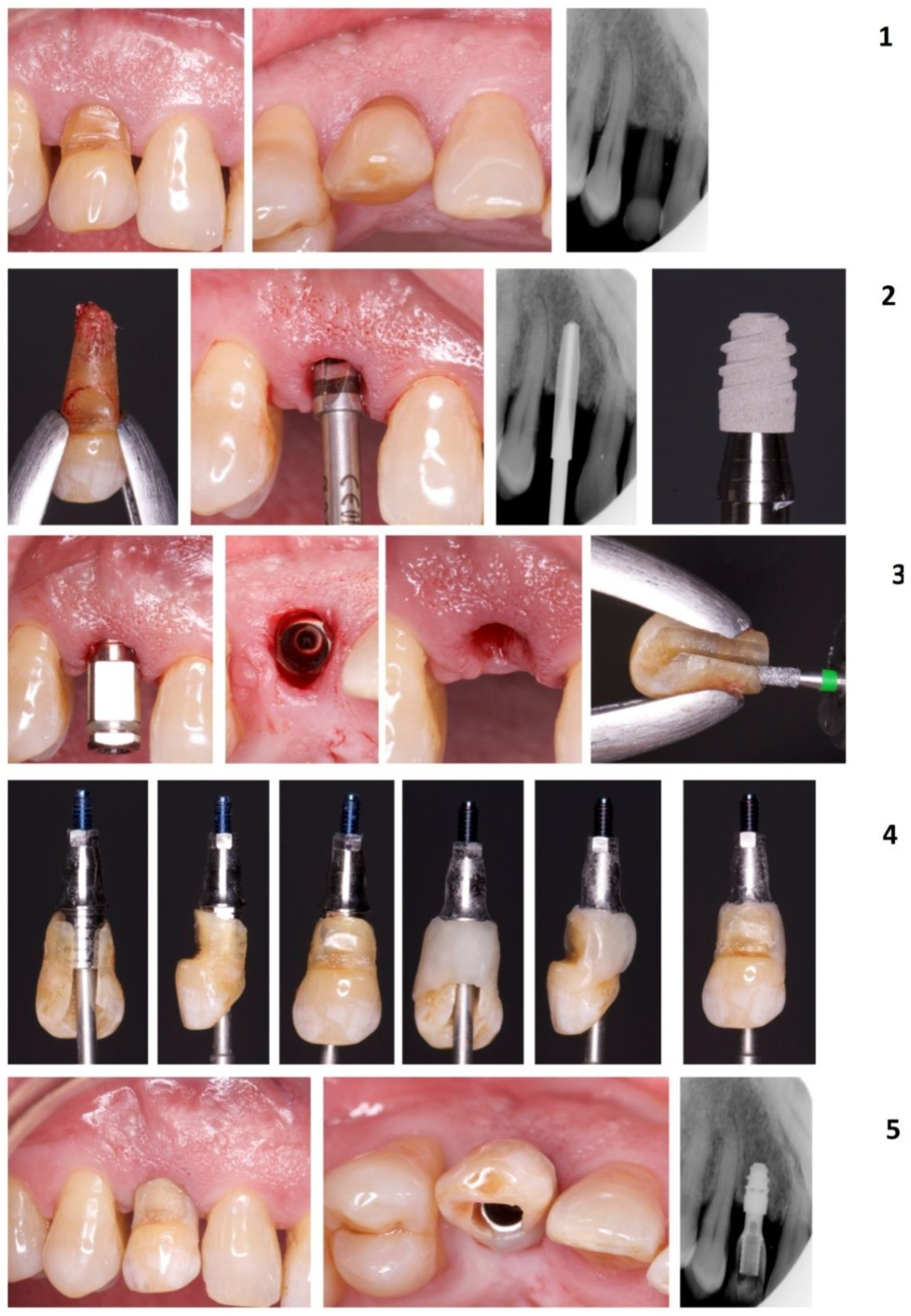
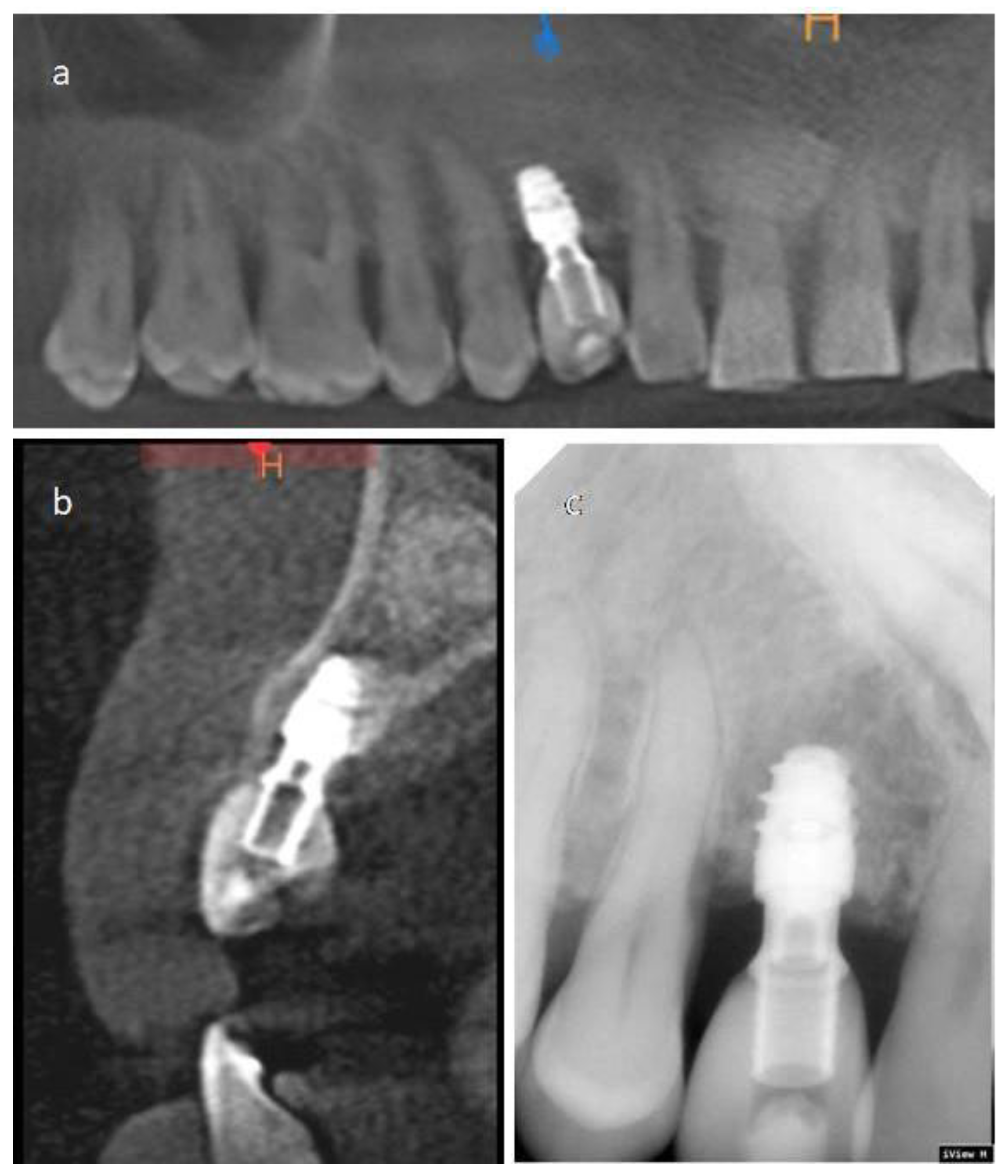
2.2.1. Case 1
2.2.2. Case 2
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pico, C.L.; do Vale, F.J.; Caramelo, F.J.; Corte-Real, A.; Pereira, S.M. Comparative analysis of impacted upper canines: Panoramic radiograph Vs Cone Beam Computed Tomography. J. Clin. Exp. Dent. 2017, 9, e1176–e1182. [Google Scholar] [CrossRef]
- Al-Zoubi, H.; Alharbi, A.A.; Ferguson, D.J.; Zafar, M.S. Frequency of impacted teeth and categorization of impacted canines: A retrospective radiographic study using orthopantomograms. Eur. J. Dent. 2017, 11, 117–121. [Google Scholar] [CrossRef]
- D´Oleo-Aracena, M.F.; Arriola-Guillen, L.E.; Rodriguez-Cardenas, Y.A.; Ruiz-Mora, G.A. Skeletal and dentoalveolar bilateral dimensions in unilateral palatally impacted canine using cone beam computed tomography. Prog. Orthod. 2017, 18, 7. [Google Scholar] [CrossRef]
- Bishara, S.E. Impacted maxillary canines: A review. Am. J. Orthod. Dentofac. Orthop. 1992, 101, 159–171. [Google Scholar] [CrossRef]
- Ericson, S.; Kurol, J. Early treatment of palatally erupting maxillary canines by extraction of the primary canines. Eur. J. Orthod. 1988, 10, 283–295. [Google Scholar] [CrossRef] [PubMed]
- Gunduz, K.; Acikgoz, A.; Egrioglu, E. Radiologic investigation of prevalence, associated pathologies and dental anomalies of non-third molar impacted teeth in Turkish oral patients. Chin. J. Dent. Res. 2011, 14, 141–146. [Google Scholar] [PubMed]
- Manne, R.; Gandikota, C.; Juvvadi, S.R.; Rama, H.R.; Anche, S. Impacted canines: Etiology, diagnosis, and orthodontic management. J. Pharm. Bioallied Sci. 2012, 4, S234–S238. [Google Scholar] [CrossRef] [PubMed]
- Becker, A.; Chaushu, S. Success rate and duration of orthodontic treatment for adult patients with palatally impacted maxillary canines. Am. J. Orthod. Dentofac. Orthop. 2003, 124, 509–514. [Google Scholar] [CrossRef]
- Sajnani, A.K.; King, N.M. Complications associated with the occurrence and treatment of impacted maxillary canines. Singapore Dent. J. 2014, 35, 53–57. [Google Scholar] [CrossRef]
- Alberto, P.L. Management of the impacted canine and second molar. Oral Maxillofac. Surg. Clin. N. Am. 2007, 19, 59–68. [Google Scholar] [CrossRef]
- Del Fabbro, M.; Testori, T.; Kekovic, V.; Goker, F.; Tumedei, M.; Wang, H.L. A Systematic Review of Survival Rates of Osseointegrated Implants in Fully and Partially Edentulous Patients Following Immediate Loading. J. Clin. Med. 2019, 8, 2142. [Google Scholar] [CrossRef]
- Clark, D.; Levin, L. Dental implant management and maintenance: How to improve long-term implant success? Quintessence Int. 2016, 47, 417–423. [Google Scholar] [CrossRef]
- Smith, M.M.; Knight, E.T.; Al-Harthi, L.; Leichter, J.W. Chronic periodontitis and implant dentistry. Periodontol. 2000 2017, 74, 63–73. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, F.; Derks, J.; Monje, A.; Wang, H.L. Peri-implantitis. J. Clin. Periodontol. 2018, 45 (Suppl. 20), S246–S266. [Google Scholar] [CrossRef] [PubMed]
- Patel, R.M. Dental Implants for Patients with Periodontitis. Prim. Dent. J. 2020, 8, 54–61. [Google Scholar] [CrossRef] [PubMed]
- Papapanou, P.N.; Sanz, M.; Buduneli, N.; Dietrich, T.; Feres, M.; Fine, D.H.; Flemmig, T.F.; Garcia, R.; Giannobile, W.V.; Graziani, F.; et al. Periodontitis: Consensus report of workgroup 2 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J. Periodontol. 2018, 89 (Suppl. 1), S173–S182. [Google Scholar] [CrossRef] [PubMed]
- Linkevicius, T.; Puisys, A.; Steigmann, M.; Vindasiute, E.; Linkeviciene, L. Influence of Vertical Soft Tissue Thickness on Crestal Bone Changes Around Implants with Platform Switching: A Comparative Clinical Study. Clin. Implant. Dent. Relat. Res. 2015, 17, 1228–1236. [Google Scholar] [CrossRef]
- Puisys, A.; Linkevicius, T. The influence of mucosal tissue thickening on crestal bone stability around bone-level implants. A prospective controlled clinical trial. Clin. Oral Implants Res. 2015, 26, 123–129. [Google Scholar] [CrossRef] [PubMed]
- Suarez-Lopez Del Amo, F.; Lin, G.H.; Monje, A.; Galindo-Moreno, P.; Wang, H.L. Influence of Soft Tissue Thickness on Peri-Implant Marginal Bone Loss: A Systematic Review and Meta-Analysis. J. Periodontol. 2016, 87, 690–699. [Google Scholar] [CrossRef]
- Bressan, E.; Grusovin, M.G.; D’Avenia, F.; Neumann, K.; Sbricoli, L.; Luongo, G.; Esposito, M. The influence of repeated abutment changes on peri-implant tissue stability: 3-year post-loading results from a multicentre randomised controlled trial. Eur J Oral Implantol 2017, 10, 373–390. [Google Scholar]
- Cruz, R.M. Orthodontic traction of impacted canines: Concepts and clinical application. Dental Press J Orthod 2019, 24, 74–87. [Google Scholar] [CrossRef] [PubMed]
- Arriola-Guillen, L.E.; Aliaga-Del Castillo, A.; Ruiz-Mora, G.A.; Rodriguez-Cardenas, Y.A.; Dias-Da Silveira, H.L. Influence of maxillary canine impaction characteristics and factors associated with orthodontic treatment on the duration of active orthodontic traction. Am. J. Orthod. Dentofacial Orthop. 2019, 156, 391–400. [Google Scholar] [CrossRef] [PubMed]
- Becker, A.; Chaushu, S. Surgical Treatment of Impacted Canines: What the Orthodontist Would Like the Surgeon to Know. Oral Maxillofac. Surg. Clin. N. Am. 2015, 27, 449–458. [Google Scholar] [CrossRef]
- Grisar, K.; Piccart, F.; Al-Rimawi, A.S.; Basso, I.; Politis, C.; Jacobs, R. Three-dimensional position of impacted maxillary canines: Prevalence, associated pathology and introduction to a new classification system. Clin. Exp. Dent. Res. 2019, 5, 19–25. [Google Scholar] [CrossRef]
- Mazor, Z.; Segal, P.; Levin, L. Computer-guided implant placement for rehabilitation of the edentulous maxilla with two impacted canines: An approach without extraction of the impacted teeth. Int. J. Periodontics Restor. Dent. 2015, 35, 93–97. [Google Scholar] [CrossRef]
- Mithridade, D.; Serge, S.M.; Keyvan, D.; Nedjoua, C.O.; Georgy, D.; Philippe, R. Unconventional Implant Placement IV. Implant Placement through Impacted Teeth to Avoid Invasive Surgery. Long-term Results of 3 Cases. Open Dent. J. 2015, 9, 15–20. [Google Scholar] [CrossRef] [PubMed]
- Nisand, D.; Renouard, F. Short implant in limited bone volume. Periodontol. 2000 2014, 66, 72–96. [Google Scholar] [CrossRef] [PubMed]
- Lemos, C.A.; Ferro-Alves, M.L.; Okamoto, R.; Mendonca, M.R.; Pellizzer, E.P. Short dental implants versus standard dental implants placed in the posterior jaws: A systematic review and meta-analysis. J. Dent. 2016, 47, 8–17. [Google Scholar] [CrossRef]
- Altaib, F.H.; Alqutaibi, A.Y.; Al-Fahd, A.; Eid, S. Short dental implant as alternative to long implant with bone augmentation of the atrophic posterior ridge: A systematic review and meta-analysis of RCTs. Quintessence Int. 2019, 50, 636–650. [Google Scholar] [CrossRef]
- Cruz, R.S.; Lemos, C.A.A.; Batista, V.E.S.; Oliveira, H.; Gomes, J.M.L.; Pellizzer, E.P.; Verri, F.R. Short implants versus longer implants with maxillary sinus lift. A systematic review and meta-analysis. Braz. Oral Res. 2018, 32, e86. [Google Scholar] [CrossRef]
- Hasanoglu Erbasar, G.N.; Hocaoglu, T.P.; Erbasar, R.C. Risk factors associated with short dental implant success: A long-term retrospective evaluation of patients followed up for up to 9 years. Braz. Oral Res. 2019, 33, e030. [Google Scholar] [CrossRef] [PubMed]
- Felice, P.; Barausse, C.; Stefanini, M.; Pistilli, R.; Zucchelli, G. A Minimally Invasive Approach Using a 4-mm Implant Without Extraction of Impacted Maxillary Canine: Four-Year Postloading Results. Int. J. Periodontics Restor. Dent. 2017, 37, 819–824. [Google Scholar] [CrossRef] [PubMed]
- Kan, J.Y.K.; Rungcharassaeng, K.; Deflorian, M.; Weinstein, T.; Wang, H.L.; Testori, T. Immediate implant placement and provisionalization of maxillary anterior single implants. Periodontol. 2000 2018, 77, 197–212. [Google Scholar] [CrossRef]
- Bassir, S.H.; El Kholy, K.; Chen, C.Y.; Lee, K.H.; Intini, G. Outcome of early dental implant placement versus other dental implant placement protocols: A systematic review and meta-analysis. J. Periodontol. 2019, 90, 493–506. [Google Scholar] [CrossRef] [PubMed]
- Weigl, P.; Strangio, A. The impact of immediately placed and restored single-tooth implants on hard and soft tissues in the anterior maxilla. Eur. J. Oral Implantol. 2016, 9 (Suppl. 1), S89–S106. [Google Scholar] [PubMed]
- Bramanti, E.; Norcia, A.; Cicciu, M.; Matacena, G.; Cervino, G.; Troiano, G.; Zhurakivska, K.; Laino, L. Postextraction Dental Implant in the Aesthetic Zone, Socket Shield Technique Versus Conventional Protocol. J. Craniofac. Surg. 2018, 29, 1037–1041. [Google Scholar] [CrossRef] [PubMed]
- Naseri, R.; Yaghini, J.; Feizi, A. Levels of smoking and dental implants failure: A systematic review and meta-analysis. J. Clin. Periodontol. 2020, 47, 518–528. [Google Scholar] [CrossRef]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moreno-Rodríguez, J.A.; Guerrero-Gironés, J.; Rodríguez-Lozano, F.J.; Pecci-Lloret, M.R. Immediate Post-Extraction Short Implant Placement with Immediate Loading and without Extraction of an Impacted Maxillary Canine: Two Case Reports. Materials 2021, 14, 2757. https://doi.org/10.3390/ma14112757
Moreno-Rodríguez JA, Guerrero-Gironés J, Rodríguez-Lozano FJ, Pecci-Lloret MR. Immediate Post-Extraction Short Implant Placement with Immediate Loading and without Extraction of an Impacted Maxillary Canine: Two Case Reports. Materials. 2021; 14(11):2757. https://doi.org/10.3390/ma14112757
Chicago/Turabian StyleMoreno-Rodríguez, José Antonio, Julia Guerrero-Gironés, Francisco Javier Rodríguez-Lozano, and Miguel Ramón Pecci-Lloret. 2021. "Immediate Post-Extraction Short Implant Placement with Immediate Loading and without Extraction of an Impacted Maxillary Canine: Two Case Reports" Materials 14, no. 11: 2757. https://doi.org/10.3390/ma14112757
APA StyleMoreno-Rodríguez, J. A., Guerrero-Gironés, J., Rodríguez-Lozano, F. J., & Pecci-Lloret, M. R. (2021). Immediate Post-Extraction Short Implant Placement with Immediate Loading and without Extraction of an Impacted Maxillary Canine: Two Case Reports. Materials, 14(11), 2757. https://doi.org/10.3390/ma14112757






