Healing of Post-Extraction Sockets Filled with Anorganic Bovine Bone and Covered with a Xenogeneic Collagen Matrix. Radiological 2D and 3D Results of a Pilot Study to Assess Dimensional Stability
Abstract
1. Introduction
2. Materials and Methods
- Radiological Assessment
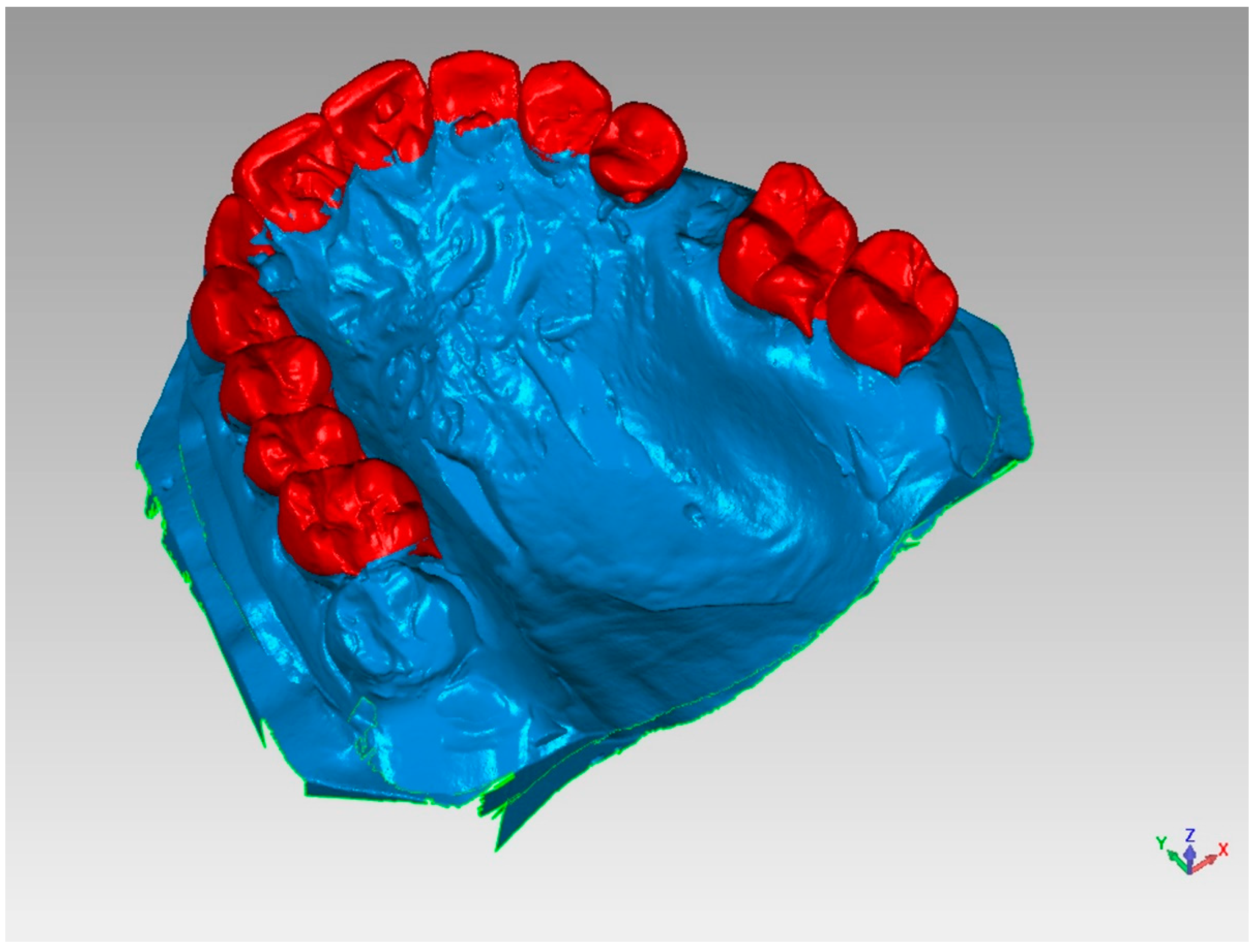
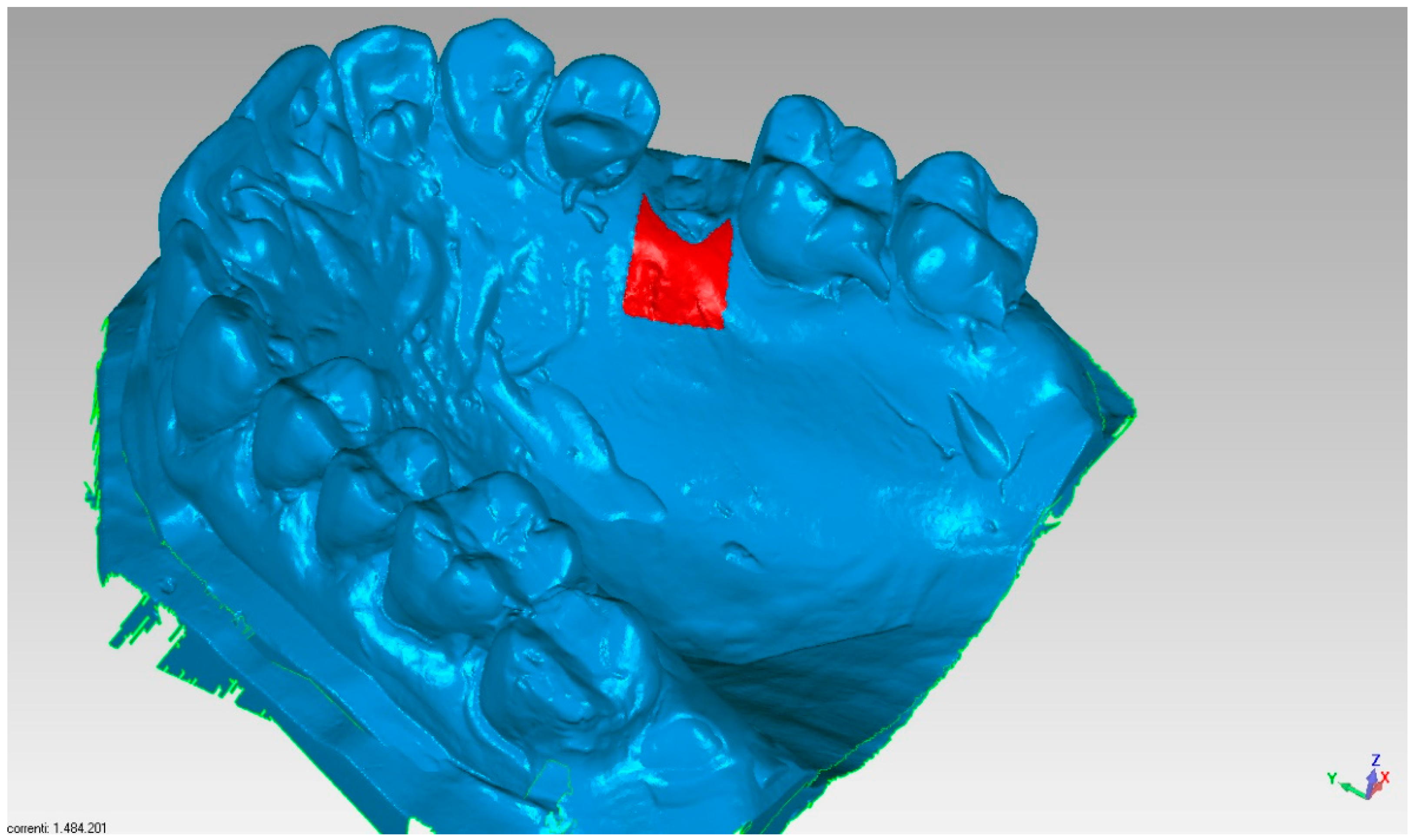
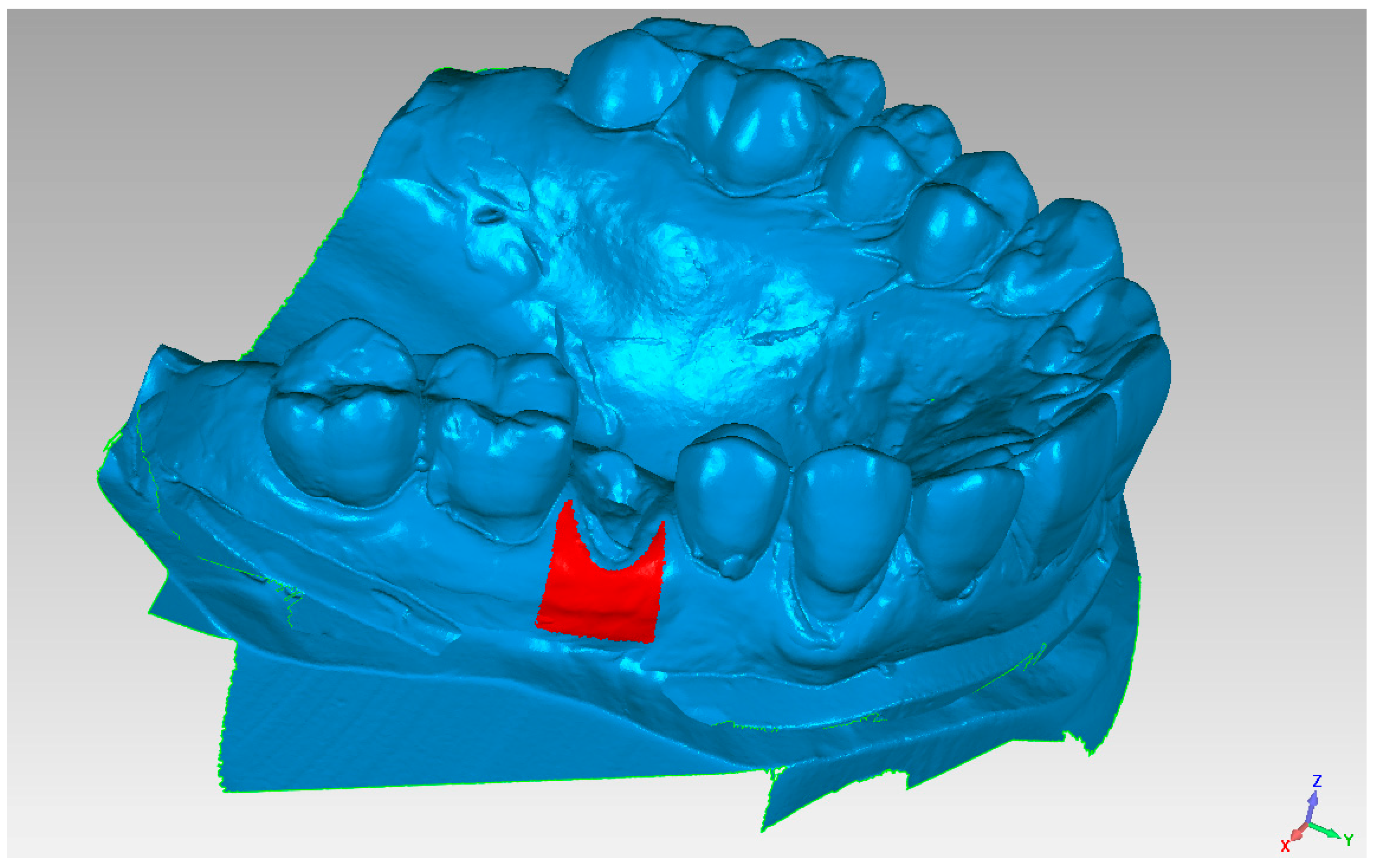
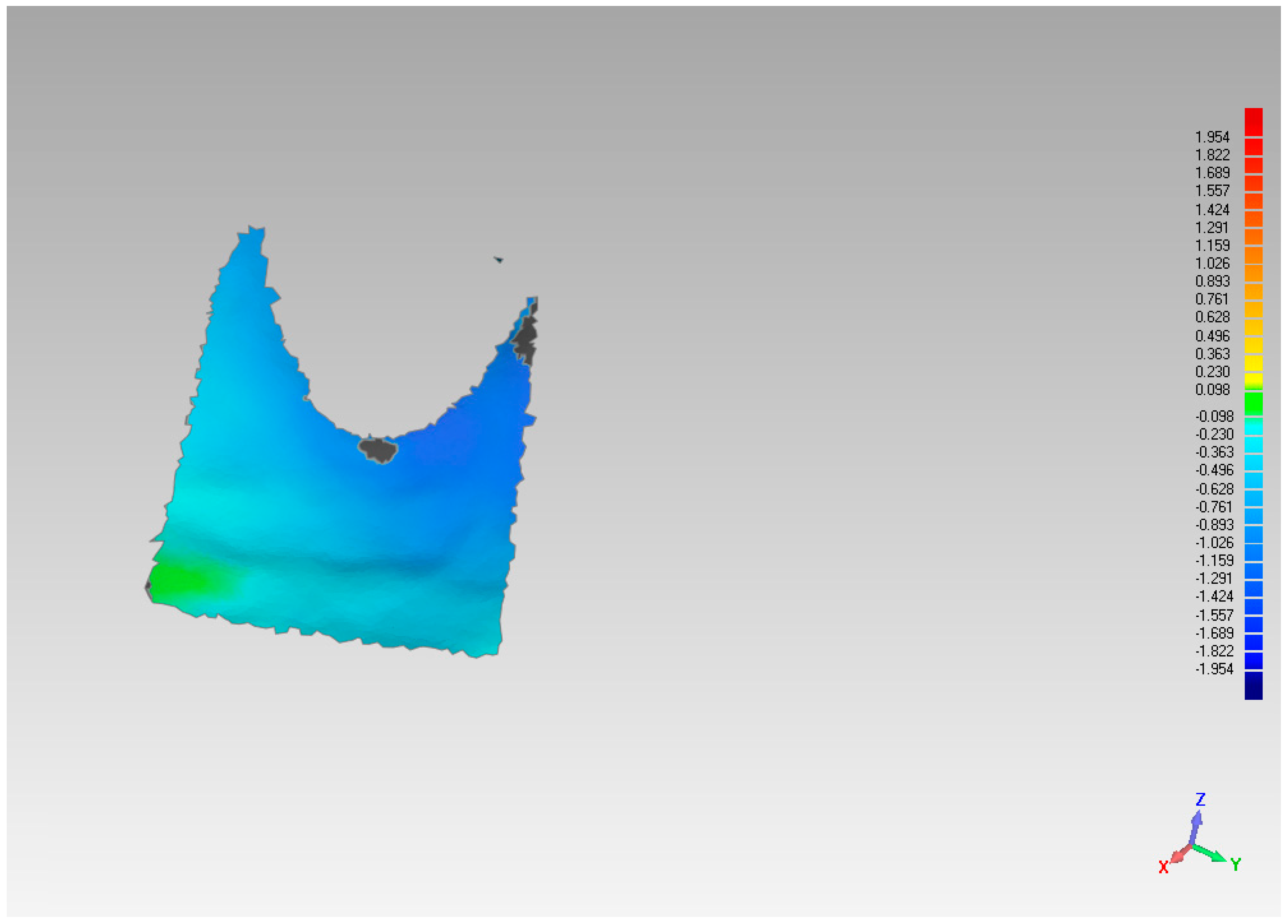
- Analysis of Models
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cardaropoli, G.; Araújo, M.; Lindhe, J. Dynamics of bone tissue formation in tooth extraction sites. An experimental study in dogs. J. Clin. Periodontol. 2003, 30, 809–818. [Google Scholar] [CrossRef]
- Araujo, M.G.; Lindhe, J. Dimensional ridge alterations following tooth extraction. An experimental study in the dog. J. Clin. Periodontol. 2005, 32, 212–218. [Google Scholar] [CrossRef] [PubMed]
- Araújo, M.G.; Wennström, J.L.; Lindhe, J. Modeling of the buccal and lingual bone walls of fresh extraction sites following implant installation. Clin. Oral Implant. Res. 2006, 17, 606–614. [Google Scholar] [CrossRef]
- Fickl, S.; Zuhr, O.; Wachtel, H.; Bolz, W.; Huerzeler, M. Tissue alterations after tooth extraction with and without surgical trauma: A volumetric study in the beagle dog. J. Clin. Periodontol. 2008, 35, 356–363. [Google Scholar] [CrossRef]
- Fickl, S.; Zuhr, O.; Wachtel, H.; Bolz, W.; Huerzeler, M.B. Hard tissue alterations after socket preservation: An experimental study in the beagle dog. Clin. Oral Implant. Res. 2008, 19, 1111–1118. [Google Scholar] [CrossRef] [PubMed]
- Lekovic, V.; Camargo, P.M.; Klokkevold, P.R.; Weinlaender, M.; Kenney, E.B.; Dimitrijevic, B.; Nedic, M. Preservation of Alveolar Bone in Extraction Sockets Using Bioabsorbable Membranes. J. Periodontol. 1998, 69, 1044–1049. [Google Scholar] [CrossRef] [PubMed]
- Capelli, M.; Testori, T.; Galli, F.; Zuffetti, F.; Motroni, A.; Weinstein, R.; Del Fabbro, M. Implant–Buccal Plate Distance as Diagnostic Parameter: A Prospective Cohort Study on Implant Placement in Fresh Extraction Sockets. J. Periodontol. 2013, 84, 1768–1774. [Google Scholar] [CrossRef]
- Barone, A.; Aldini, N.N.; Fini, M.; Giardino, R.; Guirado, J.L.C.; Covani, U. Xenograft Versus Extraction Alone for Ridge Preservation After Tooth Removal: A Clinical and Histomorphometric Study. J. Periodontol. 2008, 79, 1370–1377. [Google Scholar] [CrossRef]
- Schropp, L.; Wenzel, A.; Kostopoulos, L.; Karring, T. Bone healing and soft tissue contour changes following single-tooth extraction: A clinical and radiographic 12-month prospective study. Int. J. Periodont. Restor. Dent. 2003, 23, 313–323. [Google Scholar]
- Chen, S.T.; Buser, D. Clinical and esthetic outcomes of implants placed in postextraction sites. Int. J. Oral Maxillofac. Implant. 2009, 24, 186–217. [Google Scholar]
- Chen, S.T.; Buser, D. Esthetic Outcomes Following Immediate and Early Implant Placement in the Anterior Maxilla—A Systematic Review. Int. J. Oral Maxillofac. Implant. 2014, 29, 186–215. [Google Scholar] [CrossRef]
- Maiorana, C.; Poli, P.P.; Deflorian, M.; Testori, T.; Mandelli, F.; Nagursky, H.; Vinci, R. Alveolar socket preservation with demineralised bovine bone mineral and a collagen matrix. J. Periodont. Implant. Sci. 2017, 47, 194–210. [Google Scholar] [CrossRef] [PubMed]
- ImageJ; Version 1.51, Processing Software; National Institute of Health (NIH): Bethesda, MD, USA, 2018.
- Hämmerle, C.H.; Araújo, M.G.; Simion, M. Evidence-based knowledge on the biology and treatment of extraction sockets. Clin. Oral Implant. Res. 2012, 5, 80–82. [Google Scholar] [CrossRef]
- Weng, D.; Nagata, M.J.H.; Bosco, A.F.H.; De Melo, L.G.N. Influence of microgap location and configuration on radiographic bone loss around submerged implants: An experimental study in dogs. Int. J. Oral Maxillofac. Implant. 2011, 26, 941–946. [Google Scholar]
- Vignoletti, F.; Matesanz, P.; Rodrigo, D.; Figuero, E.; Martin, C.; Sanz, M. Surgical protocols for ridge preservation after tooth extraction. A systematic review. Clin. Oral Implant. Res. 2011, 23, 22–38. [Google Scholar] [CrossRef]
- Vignoletti, F.; Discepoli, N.; Müller, A.; Sanctis, M.; Muñoz, F.; Sanz, M. Bone modelling at fresh extraction sockets: Immediate implant placement versus spontaneous healing. An experimental study in the beagle dog. J. Clin. Periodontol. 2011, 39, 91–97. [Google Scholar] [CrossRef] [PubMed]
- Avila-Ortiz, G.; Elangovan, S.; Kramer, K.W.; Blanchette, D.; Dawson, D.V. Effect of alveolar ridge preservation after tooth extraction: A systematic review and meta-analysis. J. Dent. Res. 2014, 93, 950–958. [Google Scholar] [CrossRef]
- Morjaria, K.R.; Wilson, R.; Palmer, R.M. Bone Healing after Tooth Extraction with or without an Intervention: A Systematic Review of Randomized Controlled Trials. Clin. Implant. Dent. Relat. Res. 2012, 16, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Horváth, A.; Mardas, N.; Mezzomo, L.A.; Needleman, I.G.; Donos, N. Alveolar ridge preservation. A systematic review. Clin. Oral. Investig. 2013, 17, 341–363. [Google Scholar] [CrossRef] [PubMed]
- Vittorini Orgeas, G.; Clementini, M.; De Risi, V.; De Sanctis, M. Surgical techniques for alveolar socket preservation: A systematic review. Int. J. Oral. Maxillofac. Implant. 2013, 28, 1049–1061. [Google Scholar] [CrossRef]
- Jung, R.E.; Philipp, A.; Annen, B.M.; Signorelli, L.; Thoma, D.S.; Hämmerle, C.H.; Attin, T.; Schmidlin, P.R. Radiographic evaluation of different techniques for ridge preservation after tooth extraction: A randomized controlled clinical trial. J. Clin. Periodontol. 2013, 40, 90–98. [Google Scholar] [CrossRef] [PubMed]
- Magne, P.; Magne, M.; Belser, U. The Esthetic Width in Fixed Prosthodontics. J. Prosthodont. 1999, 8, 106–118. [Google Scholar] [CrossRef] [PubMed]



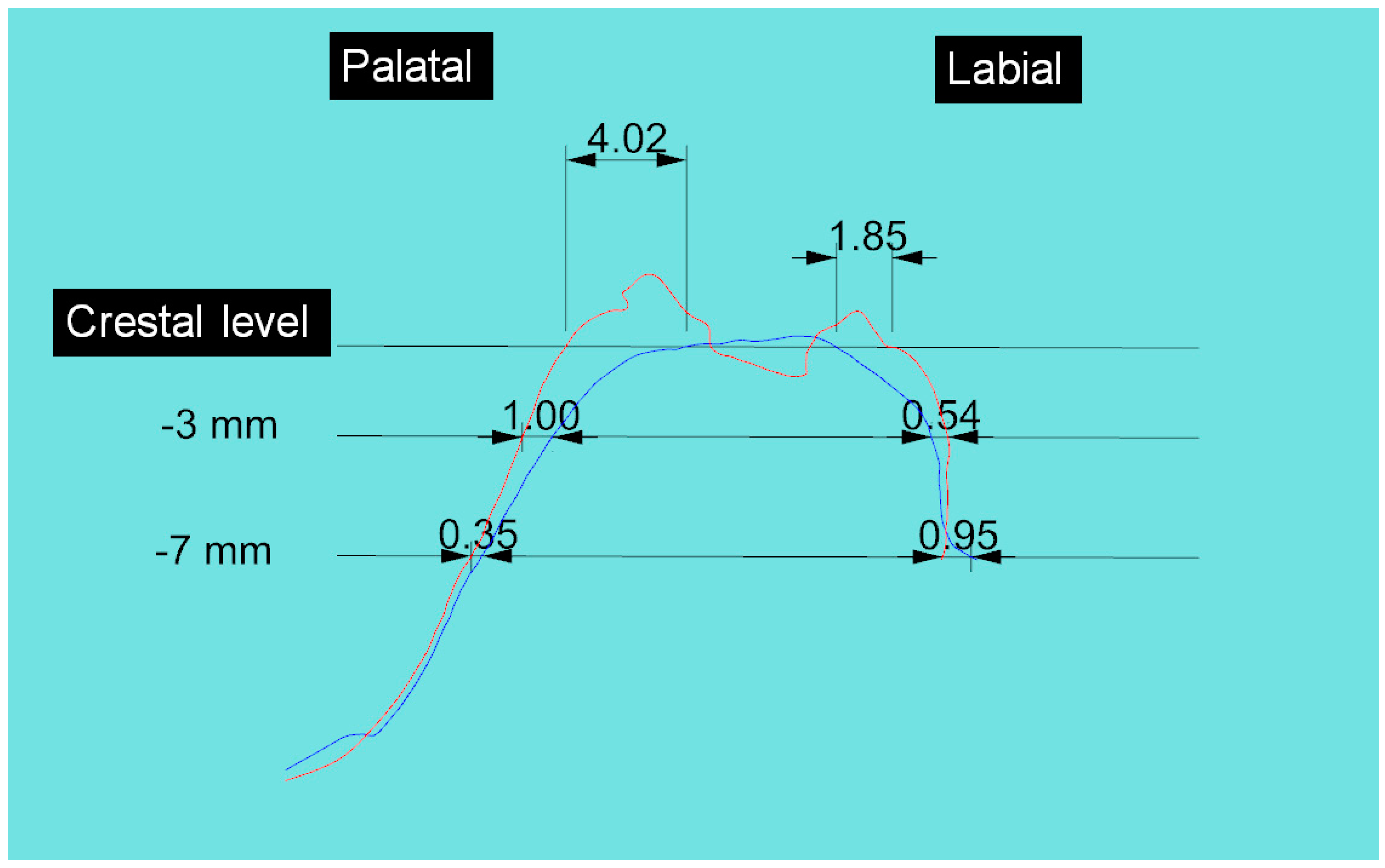
| Case n | Palatal/Lingual Section | Vestib/Sagittal Section | ||||
|---|---|---|---|---|---|---|
| crest | 3 mm | 7 mm | crest | 3 mm | 7 mm | |
| 1 | 1.6 | 0.11 | 0.22 | 1.68 | 1.27 | 0.41 |
| 2 | 0.89 | 0.48 | 0.00 | 1.04 | 0.68 | 0.65 |
| 3 | 4.02 | 1.00 | 0.35 | 1.85 | 0.54 | 0.95 |
| 4 | 3.24 | 0.43 | 0.08 | 2.74 | 0.89 | 0.25 |
| 5 | 0.93 | 0.41 | 0.26 | 4.07 | 2.92 | 0.46 |
| 6 | 1.28 | 0.63 | 1.79 | 1.78 | 0.88 | 0.69 |
| 7 | 2.54 | 0.26 | 0.8 | 1.89 | 0.87 | 1.08 |
| 8 | 2.11 | 0.38 | 0.14 | 1.48 | 0.93 | 0.91 |
| 9 | 1.72 | 0.12 | 0.03 | 1.83 | 1.01 | 0.64 |
| 10 | 2.46 | 0.48 | 0.41 | 2.57 | 1.81 | 1.04 |
| 11 | 1.69 | 0.24 | 0.00 | 1.52 | 0.68 | 0.33 |
| 12 | 0.41 | 0.71 | 0.15 | 1.92 | 1.25 | 0.86 |
| 13 | 0.73 | 0.61 | 0.06 | 1.79 | 1.41 | 0.99 |
| 14 | 2.61 | 0.58 | 0.18 | 2.48 | 1.78 | 1.18 |
| 15 | 1.41 | 0.43 | 0.21 | 1.73 | 1.58 | 1.35 |
| mean | 1.84 | 0.46 | 0.31 | 2.02 | 1.23 | 0.79 |
| st.dev | 0.99 | 0.23 | 0.46 | 0.71 | 0.61 | 0.33 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Testori, T.; Deflorian, M.A.; Mandelli, F.; Attardo, G.; Maiorana, C.; Del Fabbro, M.; Vinci, R. Healing of Post-Extraction Sockets Filled with Anorganic Bovine Bone and Covered with a Xenogeneic Collagen Matrix. Radiological 2D and 3D Results of a Pilot Study to Assess Dimensional Stability. Materials 2021, 14, 2473. https://doi.org/10.3390/ma14102473
Testori T, Deflorian MA, Mandelli F, Attardo G, Maiorana C, Del Fabbro M, Vinci R. Healing of Post-Extraction Sockets Filled with Anorganic Bovine Bone and Covered with a Xenogeneic Collagen Matrix. Radiological 2D and 3D Results of a Pilot Study to Assess Dimensional Stability. Materials. 2021; 14(10):2473. https://doi.org/10.3390/ma14102473
Chicago/Turabian StyleTestori, Tiziano, Matteo Antonio Deflorian, Federico Mandelli, Giulia Attardo, Carlo Maiorana, Massimo Del Fabbro, and Raffaele Vinci. 2021. "Healing of Post-Extraction Sockets Filled with Anorganic Bovine Bone and Covered with a Xenogeneic Collagen Matrix. Radiological 2D and 3D Results of a Pilot Study to Assess Dimensional Stability" Materials 14, no. 10: 2473. https://doi.org/10.3390/ma14102473
APA StyleTestori, T., Deflorian, M. A., Mandelli, F., Attardo, G., Maiorana, C., Del Fabbro, M., & Vinci, R. (2021). Healing of Post-Extraction Sockets Filled with Anorganic Bovine Bone and Covered with a Xenogeneic Collagen Matrix. Radiological 2D and 3D Results of a Pilot Study to Assess Dimensional Stability. Materials, 14(10), 2473. https://doi.org/10.3390/ma14102473








